Medical Studies > QUESTIONS & ANSWERS > CPC Exam Questions Prep & Answers. Verified. (All)
CPC Exam Questions Prep & Answers. Verified.
Document Content and Description Below
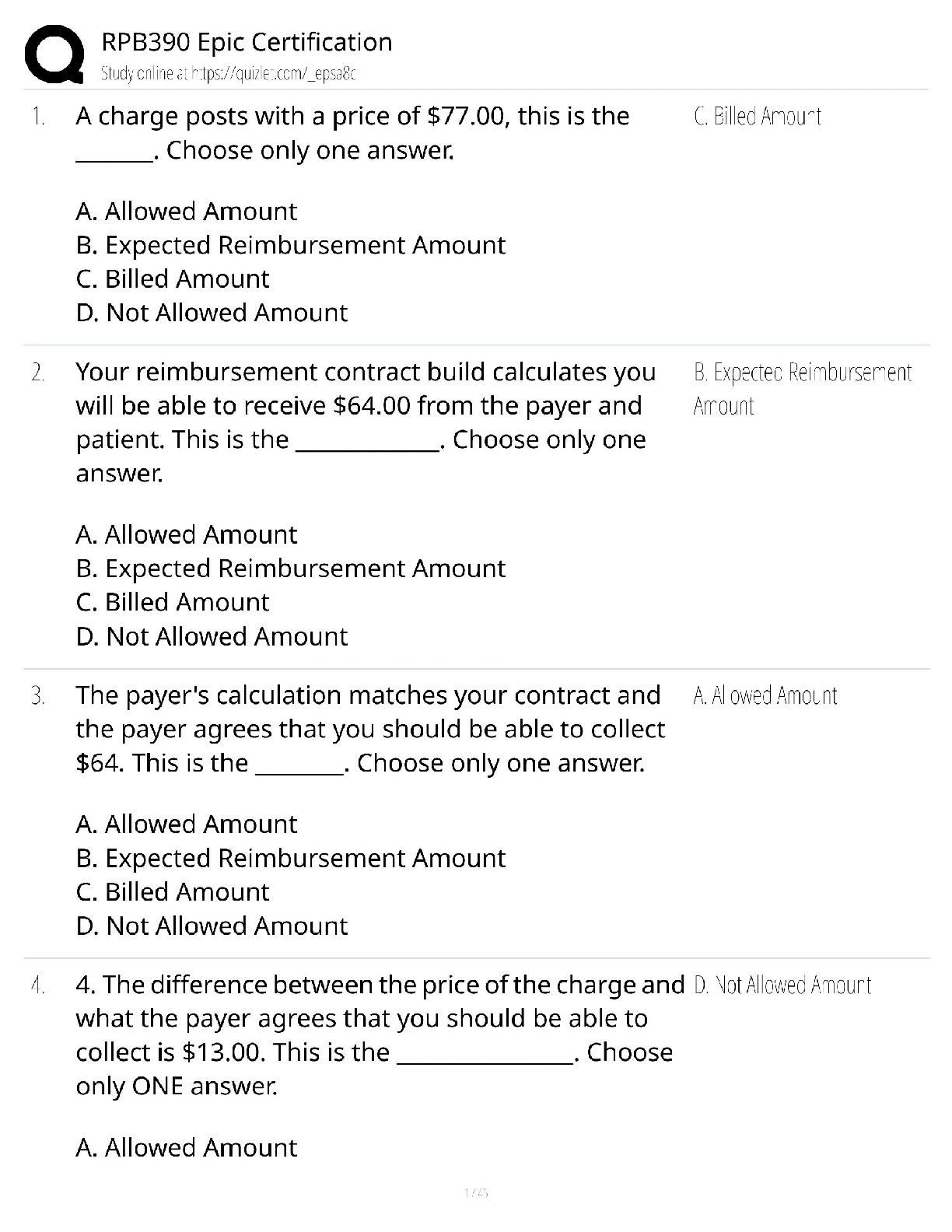
CPC Exam Questions Prep & Answers. Verified. Abstractor - ✔✔-hospital employee who converts documented procedurs and diangoses into medical codes Abuse - ✔✔-coding practices that lead to ... improper reimbursement by error because they do not meet medical necessity, ex. changing diagnosis to be covered by insurance Accreditation - ✔✔-an examination process the healthcare facility goes through to evaluate the facilities policies, procedures, and performance to meet higher standards. Accredited - ✔✔-Having seal of approval after being evaluated and demonstrating quality standards Act/ Law/ Statute - ✔✔-Legislation passed through Congress and signed by President or passed over his veto Actual Charge - ✔✔-The amount the provider charges for medical services or supplies. Not always paid in full. Additional Benefits - ✔✔-Health care services not covered by Medicare and are offered through the Medicare Advantage Organization for no additional premium. The benefits must equal the ACR (Adjusted Community Rating) Adjudication - ✔✔-Health Insurance Claims process at the insurance company Adjusted Average Per Capita Cost (AAPCC) - ✔✔-Estimate of how much Medicare will spend in a year for an average beneficiary Administrative Code Sets - ✔✔-Non medical code sets that characterize a general business situation rather than a medical condition. Administrative Costs - ✔✔-Medicare, Medicaid, CMS refer to this as their expenses to have the program, operating expenses, program management, etc. Administrative Data - ✔✔-Health insurance information stored in automated information system about enrollment, eligibility, claims, etc. Administrative Law Judge (ALJ) - ✔✔-hearing officer who presides over appeal conflicts between providers or beneficiaries, and Medicare contractors (MAC's) Administrative Simplification - ✔✔-Part of HIPAA authorizing HHS (Health and Human Services) to 1. adopt standards for transactions & code sets; 2. adopt standard identifiers for health plans; 3. adopt standards to protect security & privacy of personally identifiable health information. Administrative Simplification Act - ✔✔-Signed 12/17/01 allows HHS (Health & Human Services) to exclude providers from Medicare for HIPAA non-compliance of electronic claims and prohibit paper claims except in certain situations Admission Date - ✔✔-The date the patient was admitted for inpatient care, outpatient, or start of care.For hospice, enter effective date of election of hospice benefits. Admitting Diagnosis - ✔✔-Diagnosis code indicating patient's diagnosis at admission Admitting Physician - ✔✔-The doctor responsible for admitting a patient to the hospital or other inpatient health facility Advance Beneficiary Notification (ABN) - ✔✔-A notice from provider to patient that Medicare may deny payment. Patient must sign before services are provider, otherwise patient is not responsible if Medicare does not cover. Advanced Directive - ✔✔-Statement written by patient on how they want medical decisions to be made. May include a Living Will or Durable Power of Attorney for healthcare. Allowed Charge - ✔✔-Individual charge determination by carrier for a covered service or supply. Ambulatory Care - ✔✔-All types of health services that do not require an overnight stay. Ambulatory Care Sensitive Conditions (ACSC) - ✔✔-Medical condtions that if treated immediatly and managed properly should not require hospitalization. Ambulatory Payment Classification (APC) - ✔✔-Medicare's outpatient prospective payment system in which services are grouped based on the resources needed and payment is fixed within each group Ambulatory Surgery Center (ASC) - ✔✔-Outpatient surgery center not located in the hospital. Patient's may stay a few hours up to 1 night. American Hospital Association (AHA) - ✔✔-Represents concerns of instituitional providers. They host the National Uniform Billing Committee (NUBC) which consults under HIPAA American Medical Association (AMA) - ✔✔-Professional organization maintains CPT code sets, secretariat to National Uniform Claim Committee (NUCC) which consults under HIPAA. ASC payment group rate. ASHIM - ✔✔-American Society of Health Informatics Managers, Inc. is a non-profit group of computer professionals that specialize in health information technology (HIT). They are certified through Certified Health Informatics System Professionals (CHISP) Ancillary Services - ✔✔-Professional services by a hospital or inpatient facility. Xrays, drugs, labs, etc. Appeal - ✔✔-Complaint by hospital or patient about a health care payment Approved Amount - ✔✔-The fee Medicare sets as reasonable and pays to the provider. Assigned Claim - ✔✔-Claim submittted by a provider who accepts Medicare Assignment - ✔✔-Agreeing to acccept Medicare fees as payment in full Attending Physician - ✔✔-Licensed physician who certifies the patient services via medical necessity and is primarily responsible for the patient's medical care and treatment. Automated Claim Review - ✔✔-Claim review and etermination via system edits and don't require human intervention Basic Benefit - ✔✔-Includes Medicare covered benefits (except hospice) and additional benefits Beneficiary - ✔✔-The name of a person who has health care insurance through the insurance program Benefit Payment - ✔✔-Amount paid by insurance after the deductible and coinsurance have been deducted Benefit Period - ✔✔-Episode of care within hospitals & skilled nursing facilities (SNF). Begins on admission and ends 60 days after care has ended Benefits - ✔✔-The money or services provided through an insurance policy Board Certified - ✔✔-Doctor specializing in certain area of medicine and who passes an advanced exam. Primary care and specialists can both be board certified Business Associate - ✔✔-Someone performs a function on behalf of a covered entity but is not part of the covered entity's workforce, outside business manager. Capitation - ✔✔-Specified amount of money is paid to a health plan or doctor regardless of the services rendered in that period. One lump sum. Care Plan - ✔✔-Written plan of services patient will receive to ensure the patient's best care physically, mentally & socially Caregiver - ✔✔-Someone who cares for a patient who is ill, disabled, or aged. Can be relatives, friends or someone who is paid. Case Management - ✔✔-Physician, nurse, or other person tracks use of facilities and resources of a patient to be sure they are receiving the care they need. Case Mix - ✔✔-Distribution of patients into categories reflecting severity of illness or resource uses. Case Mix Index - ✔✔-The average Diagnostic Related Groups (DRG) relative weight for all Medicare admissions Catastrophic Illness - ✔✔-Serious and costly health problem that could be life-threatening or cause disability. Costs can cause patient financial hardship. Catastrophic Limit - ✔✔-The highest amount a beneficiary is required to pay out of pocket during a certain period of time for certain covered charges. Center for Disease Control and Prevention (CDC) - ✔✔-Organization that protects public health through monitoring disease trends, investigation outbreaks, implementing illness, and injury control. Center for Medicare & Medicaid Services (CMS) - ✔✔-The Heath & Human Services (HHS) agency responsible for Medicare & parts of Medicaid. Maintains UB-04, oversight of HIPAA and maintains HCPCS code set & Medicare remittance advice (RA) remark codes. They promote higher quality care Certification - ✔✔-the hospital passed a survey done by a state government agency. Medicare only covers hospital stays in hospitals that are certified or accredited. Civilian Health and Medical Program (CHAMPUS) - ✔✔-Run by department of defense. Used to give medical care to active duty but now this is called TRICARE Charge Description Master (CDM) - ✔✔-Electronic billing table where charge amounts are kept in a centralized place. Claim - ✔✔-Request for payment for services or benefits received. Claims are called bills through Medicare Part A Claim Adjustment Reason Codes - ✔✔-Identifies the reason for any difference in charge and payment. This code set is used in the X12 835 Claim Payment & Remittance Advice and the X12 837 Claim transactions and is maintained by Health Care Code Maintenance Committee Claim Status Code - ✔✔-Identifies the status of a claim. This code set is used in the X12N 277 Claim Status Inquiry and Response transactions and is mainted by the Health Care Code Maintenance Committee CMS Agent - ✔✔-State survey agency who participates in Medicare surveys and certification process. ex. private physician consulting with the State Agency (SA) or CMS regional office. UB-04 - ✔✔-Claim form used by hospitals and facilities for billing procedures and services. CMS1500 - ✔✔-Claim form used for billing physiicans and other services, ex physical therapy. Code of Federal Regulations - ✔✔-Official compiliation of federal rul [Show More]
Last updated: 2 years ago
Preview 1 out of 13 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 15, 2023
Number of pages
13
Written in
All
Additional information
This document has been written for:
Uploaded
Mar 15, 2023
Downloads
0
Views
44