Health Care > EXAM > NUR 155 EXAM ONE EXAM 2023 Full and Revised Study Guide with Complete solutions (All)
NUR 155 EXAM ONE EXAM 2023 Full and Revised Study Guide with Complete solutions
Document Content and Description Below
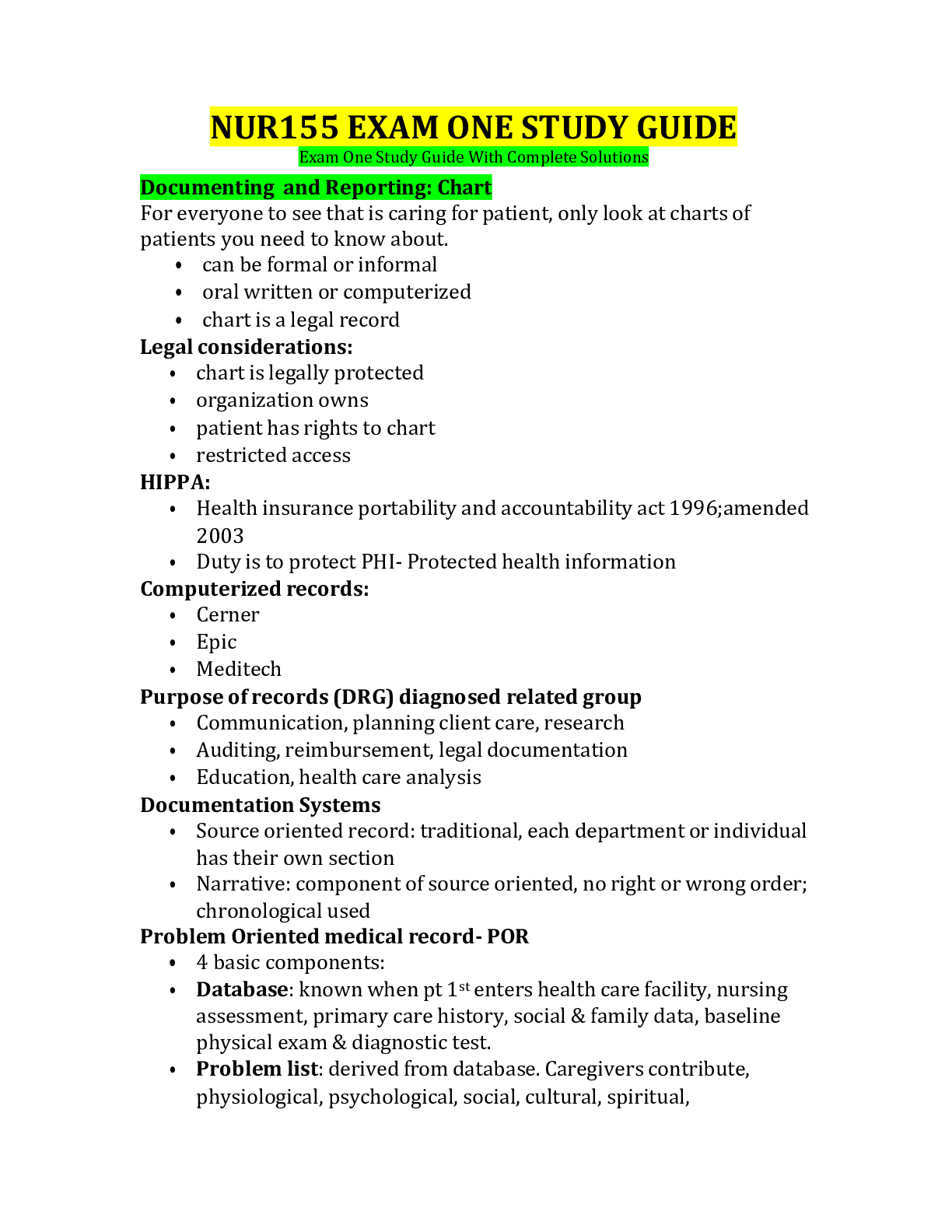
NUR155 EXAM ONE STUDY GUIDE Exam One Study Guide With Complete Solutions Documenting and Reporting: Chart For everyone to see that is caring for patient, only look at charts of patients you need to... know about. • can be formal or informal • oral written or computerized • chart is a legal record Legal considerations: • chart is legally protected • organization owns • patient has rights to chart • restricted access HIPPA: • Health insurance portability and accountability act 1996;amended 2003 • Duty is to protect PHI- Protected health information Computerized records: • Cerner • Epic • Meditech Purpose of records (DRG) diagnosed related group • Communication, planning client care, research • Auditing, reimbursement, legal documentation • Education, health care analysis Documentation Systems • Source oriented record: traditional, each department or individual has their own section • Narrative: component of source oriented, no right or wrong order; chronological used Problem Oriented medical record- POR • 4 basic components: • Database: known when pt 1st enters health care facility, nursing assessment, primary care history, social & family data, baseline physical exam & diagnostic test. • Problem list: derived from database. Caregivers contribute, physiological, psychological, social, cultural, spiritual, development, and environmental needs. Medical problems, diagnoses, surgical procedures, symptoms; nurse diagnoses. (ex impaired mobility, urinary incontinence). • Plan of Care- Initial list of orders or plan of care. • Progress notes- chart entry’s made by ALL Health care professionals involved in patients care. SOAP or SOAPIER- Subjective- obtained from client, Objective-information measured or observed (vital signs, lab, x-ray). Assessment- conclusions drawn subjective and objective from data (clients condition and level of progress). Plan- plan designed to resolve stated problem. I- intervention, E- evaluation, R- revision. PIE- Problems Interventions Evaluation • Consists or patient flow sheets and progress notes DAR- Data Action Response • Focus charting- intended to make patient concerns and strengths the focus of care CBE- Charting by Exception • Only abnormal or significant findings, exceptions to the norms recorded. 3 key elements: Flow sheets (vitals, head and face assessment) Standards of care- unconscious patient oral care q4h. Beside access chart forms- all flow sheets kept at patients bedside for immediate recording. *Guidelines for recording • Date/ time • Legibility • Permanence-Ink • Accepted terminology • Signature, Accuracy and completeness *SBAR • S- situation- state your name, unit, patient name, briefly state problem • B- background- admission diagnoses, medical history, summary of tx to date, code status • A- assessment- vital signs, pain scale, change from prior assessment [Show More]
Last updated: 2 years ago
Preview 1 out of 15 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$6.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 24, 2023
Number of pages
15
Written in
Additional information
This document has been written for:
Uploaded
Apr 24, 2023
Downloads
0
Views
61







.png)

