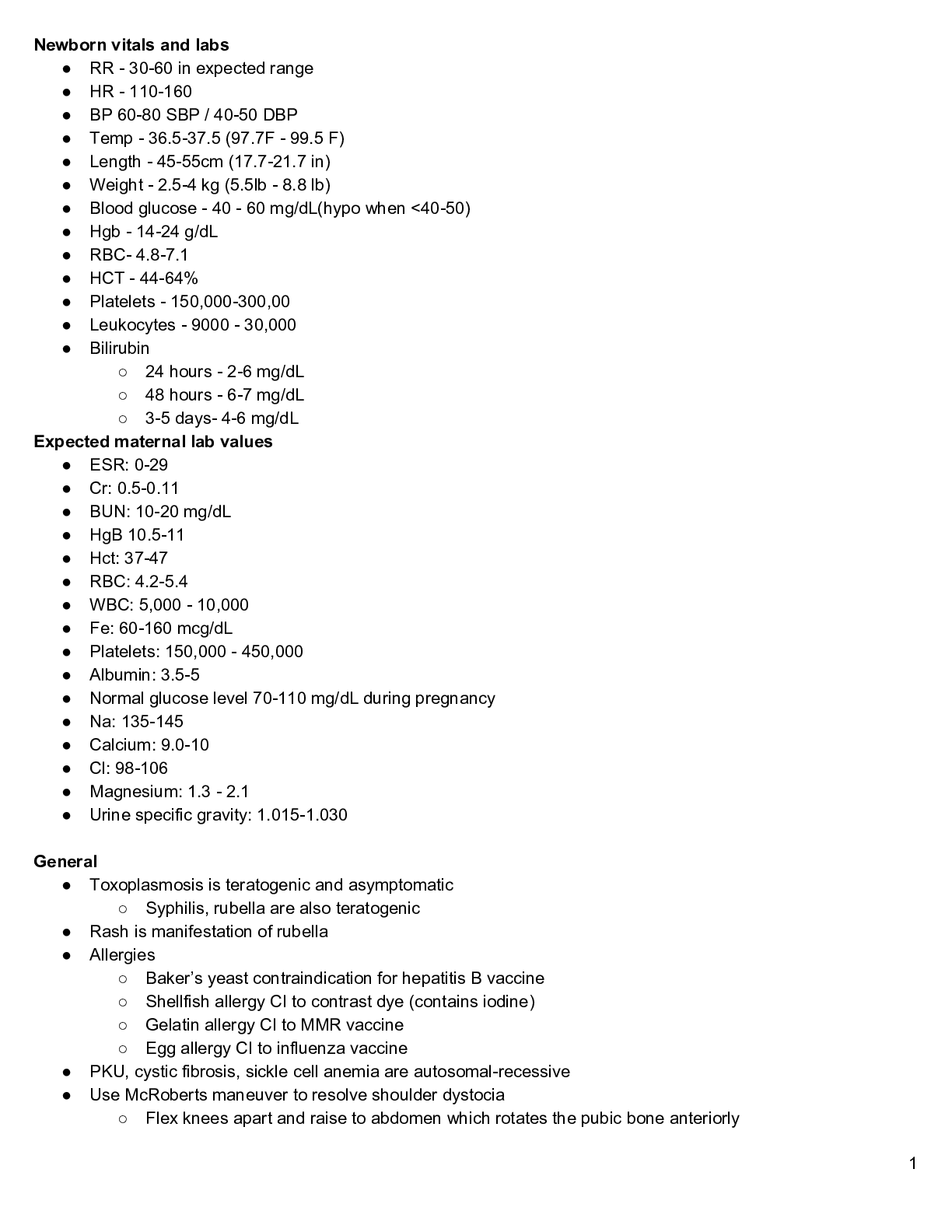
Newborn vitals and labs
● RR - 30-60 in expected range
● HR - 110-160
● BP 60-80 SBP / 40-50 DBP
● Temp - 36.5-37.5 (97.7F - 99.5 F)
● Length - 45-55cm (17.7-21.7 in)
● Weight - 2.5-4 kg (5.5lb - 8.8 lb)
● Blood g
...
Newborn vitals and labs
● RR - 30-60 in expected range
● HR - 110-160
● BP 60-80 SBP / 40-50 DBP
● Temp - 36.5-37.5 (97.7F - 99.5 F)
● Length - 45-55cm (17.7-21.7 in)
● Weight - 2.5-4 kg (5.5lb - 8.8 lb)
● Blood glucose - 40 - 60 mg/dL(hypo when <40-50)
● Hgb - 14-24 g/dL
● RBC- 4.8-7.1
● HCT - 44-64%
● Platelets - 150,000-300,00
● Leukocytes - 9000 - 30,000
● Bilirubin
○ 24 hours - 2-6 mg/dL
○ 48 hours - 6-7 mg/dL
○ 3-5 days- 4-6 mg/dL
Expected maternal lab values
● ESR: 0-29
● Cr: 0.5-0.11
● BUN: 10-20 mg/dL
● HgB 10.5-11
● Hct: 37-47
● RBC: 4.2-5.4
● WBC: 5,000 - 10,000
● Fe: 60-160 mcg/dL
● Platelets: 150,000 - 450,000
● Albumin: 3.5-5
● Normal glucose level 70-110 mg/dL during pregnancy
● Na: 135-145
● Calcium: 9.0-10
● Cl: 98-106
● Magnesium: 1.3 - 2.1
● Urine specific gravity: 1.015-1.030
General
● Toxoplasmosis is teratogenic and asymptomatic
○ Syphilis, rubella are also teratogenic
● Rash is manifestation of rubella
● Allergies
○ Baker’s yeast contraindication for hepatitis B vaccine
○ Shellfish allergy CI to contrast dye (contains iodine)
○ Gelatin allergy CI to MMR vaccine
○ Egg allergy CI to influenza vaccine
● PKU, cystic fibrosis, sickle cell anemia are autosomal-recessive
● Use McRoberts maneuver to resolve shoulder dystocia
○ Flex knees apart and raise to abdomen which rotates the pubic bone anteriorly
1○ This releases anterior shoulder
○ Can also position patient on hands and knees to help rotate fetus from a posterior to anterior position
for dystocia
● Indications for CS: abnormal FHR, malpresentation, HIV, active herpes, congenital anomalies
● Isotretinoin cream is used to treat acne and is teratogenic
● Graafian follicle expels ovum
● Frequent cough during pregnancy indicates cardiac decompensation, must be reported to provider
● Gastric bypass puts clients at risk for folate deficiency
● Sickle cell anemia iron levels are usually 6-8
● In bladder distention, bladder sounds dull with percussion, uterus is above umbilicus, displaced to the right
and fluctuates with palpation
● Pelvis shape
○ Gynecoid is well-rounded with a wide pubic arch, ideal for vaginal birth
○ Android, anthropoid, or platypelloid might have difficult with vaginal birth and may need CS
● Newborn with congenital diaphragmatic hernia will have a barrel-shaped chest
● Couvade syndrome is pregnancy like manifestations experienced by the expectant father - nausea, weight
gain
● SSRI withdrawal includes irritability, agitation, tremors, diarrhea, vomiting
○ Fetus experiences hypoglycemia, lbw, tachycardia
● For DVT place on bed rest and use warm compresses
● Intrauterine pressure catheter is necessary to determine uterine contraction intensity and if they’re adequate
for progression of labor
● Hispanic birth practices
○ Protect client’s head and feet from cold air
○ Delay bathing for 14 days following delivery
○ Bed rest for 3 days following delivery
○ Drink warm beverages following birth
● For a client with parvovirus, schedule ultrasound to detect fetal hydrops
● For maternal PKU, avoid foods high in protein
Contraception
● Barrier methods: condoms, diaphragms
○ Client must be re-fitted by provider every 2 years for diaphragm or if they have a 20% weight change
or have a full-term pregnancy or 2nd term abortion
○ When using diaphragm have to use spermicide for each act of coitus
○ Diaphragm must remain in place for 6 hours after sex
○ Can insert up to 6 hours before intercourse
● Hormonal methods (OCPs)
○ Side effects: chest pain, SOB, leg pain (DVT), headache/eye problems (stroke/HTN)
○ Want to pay attention to these side effects
○ If someone smokes, don’t recommend hormonal contraceptives (OCPs)
○ CI: hx of blood clots, stroke, cardiac problems, breast cancers, smoker, cholecystitis, HTN, migraines
○ Can’t use if on anticonvulsants, antifungals, and HIV protease inhibitors
● Depo-provera
○ Can cause decreased bone mineral density/loss of calcium
○ Make sure client has adequate calcium/vitamin D intake
● IUD
2○ Increase risk of PID
○ Can cause uterine perforation/ectopic pregnancy
○ Increases risk for ectopic pregnancy
○ Pay attention to change in string length, foul smelling discharge, pain with discharge, fever, chills
○ CI: menorrhagia, severe dysmenorrhea, history of ectopic pregnancy
● Levonorgestrel
○ Emergency contraception, inhibits ovulation
○ Must take within 72 hours after sexual intercourse
Infertility
● Inability to conceive for at least 12 months
● Work up - start with guy/sperm analysis, then turn to women
● Tests with female - make sure woman doesn’t have allergy to iodine or seafood for tests with dye
Maternal newborn nursing video 2 - Ch 3
Signs of pregnancy
● Presumptive signs
○ Things that can be explained by a reason other than pregnancy
○ Ex: amenorrhea, fatigue, n/v, urinary frequency, breast changes, fluttering in stomach
● Positive signs
○ Very distinct things
○ Ex: fetal heart signs, see baby with ultrasound, feel movement in uterus
● Probably signs
○ Signs that are in-between
○ Ex: abdominal enlargement,
■ Hegar's sign (softening/compressibility of uterus),
■ chadwick's sign (bluish color of the cervix), 6-8 weeks
■ goodell’s sign (softening of the cervical tip), 4 weeks
■ bolatment (rebound of unengaged fetus),
■ braxton-hicks,
■ positive pregnancy test (hormones could just be jacked up),
■ fetal outline felt by examiner, increased sensitivity of cervix
● Common physiological adaptation to pregnancy
○ Breast tenderness, larger and darker areolas
○ Spotting should be reported to provider
○ Increase in vaginal secretion (thin, white, odorless)
○ Dependent edema on the feet
○ Cardiovascular: increase in output (30-50%), blood volume (30-45%, and HR
○ Respiratory: oxygen needs increase, lung capacity decreases, RR increase
○ Cervical: becomes softer, blue/purple color
○ Skin: chloasma (brown patches on face, lines nigra, striae gravidarum
○ Will use new sexual positions for intercourse based on pregnancy weight change
Naegele's rule
● Due date based on last menstrual cycle
● SUbtract three months, add 7 days
● Cathy's rule: add 9 months + 1 week
3GT- PAW acronym (florida power and light)
● Gravity - number of pregnancies
● Term births - 36 weeks and more
● Pre-term - less than 36 weeks
● Abortions and miscarriages
● Living children
Maternal newborn nursing video 3 - Ch 5,6
Weight gain
● Normal - weight gain 25-35 pounds
● Overweight - 15-25 pounds
● Underweight - 28-40 pounds
● During 1st trimester shouldn’t gain more than 1-2kg (2-4 lbs)
● After 1st trimester, expect 1lb per week for last two trimesters
Nutrition
● 340 extra calories per day second trimester
● 452 extra calories per day last trimester
● If breastfeeding, need 300-500 extra calories per day
● Folic acid:
○ Need 600 mcg a day
○ huge deal, prevents fetal neural tube defects
○ Dark green leafy vegetables, orange juice
● Increase protein intake to 71mg 2nd and 3rd trimester
● Drink 2-3L water per day
● Limit caffeine intake 300 mg per day
● Do not eat swordfish, shark, or other fishes
● No ETOH
● To prevent n/v: eat cool foods that are salty/tart and carbohydrates in morning
Exercise
● Vigorous or strenuous activities limited to no longer than 20 minutes
● Should exercise 3 times per week for 30 minutes
Pregnancy interventions
● Backpain
○ Pelvic tilt exercises, resting, sleeping on firm mattress ease back pain
○ Avoid lying on back (supine hypotension)
● UTIs
○ Avoid bubble baths
●
Diagnostics during pregnancy
● Ultrasound (non-invasive)
○ Want bladder full, helps sound levels resonate
○ Have patient drink a quart of water prior
● Amniocentesis (invasive)
○ Empty bladder
● BPP
○ Score between 0-10
4■ 8-10 normal, healthy baby
○ Measures:
■ Reactive HR: reactive=2, non-reactive=0
■ Breathing: 1 or more >30 seconds=2, absent or <30=0
■ Body movements: 3 or more body/limb extensions return to flexsion=2, less than 3=0
■ Fetal tone: 1 or more extensions return to flexion=2, lack of or absent movement=0
■ Amniotic fluid volume: 1 pocket >2cm in 2 perpendicular planes=2, absent or <2cm pockets=0
○ Mother will be delivered if score of 4 or lower or at 36 weeks ga with a score of 6
● NST
○ Non-invasive
○ Measures fetal well-being in last trimester of pregnancy
○ MEasures response of fetal HR to fetal movement and uterine contractions
■ Frequency - evaluating time from beginning of one contraction to the next
■ Duration - length from beginning to end of contraction
○ Considered reactive (normal) if fetal HR accelerates during movement - positive
○ Non-reactive if FHR (not-normal) does not accelerate adequately - negative
○ Fetal heart rate should increase 15 bpm while fetus moves and remain increased for 15 seconds
○ Orange juice before test promotes fetal movement
○ Use vibroacoustic stimulation on abdomen for 3 sec if no fetal movement detected
○ Considered non-reactive after 40 minutes of continuous monitoring with no accelerations in FHR
Other diagnostics
● Contraction stress test
○ Bring contractions through oxytocin/pitocin/nipple stimulate
○ Late decelerations are never good
○ If no late decelerations - negative test result (GOOD)
■ No late deceleration of FHR with 3 contractions in 10 min. Period
○ If late decelerations - positive test result (BAD)
■ Late deceleration present in 50% or more of contractions, indicative of uteroplacental
insufficiency
○ Can send women into preterm labor
● Amniocentesis
○ Want empty bladder
○ Tests genetic fluid for fetal genetic abnormalities
○ Done around 14 weeks GA
○ Ultrasound done first to locate pocket of fluid
○ Testing for levels of AFP, alphafoto protein
■ If AFP high, associated with neural tube defects
■ If AFP low, associated with chromosomal disorders - down syndrome
■ This test is done around 15-22 weeks
○ Tests for LS ratio
■ Leucotin sphingomyelin
■ Tests for fetal lung maturity
○ Risks: amniotic fluid emboli, hemorrhaging, infection, leaking of fluid, rupture of membranes,
miscarriage
○ Might cause uterine cramping or mild discomfort
○ Asses fetal heart tones and uterine tone prior to and throughout procedure to establish a baseline
5○ Priority After: monitor FHR
○ After procedure administer Rhogham for Rh-negative moms, encourage rest and plenty of fluids for 24
hours
○ Complications: amniotic fluid emboli, hemorrhage, infection, leakage of amniotic fluid, PROM,
miscarriage
● Corianc viliv sampling (CVS) - alternative to amniocentesis
○ 10-12 weeks GA
○ Take tiny piece of placenta and test that
○ Advantage: done earlier
○ Complications: PROM, miscarriage
● Kleinheur-Betke test
○ Used to determine the amount of fetal blood circulating in the maternal blood when there is a risk of
Rh-isoimmunization
● Cordiocentesis
○ Used to identify fetal blood type and RBC when there is a risk of isoimmune hemolytic anemia
● Intermittent auscultation
○ Does NOT determine variability, need continuous FHR monitoring
○ Can determine baseline
○ Can reveal auditory accelerations and decelerations
○ Nurse should palpate and count the maternal pulse while listening to the fetal heart rate to validate
findings and distinguish maternal pulse from the fetal heart
○ Establish baseline fetal heart rate by counting for 30-60 seconds after each contraction
○ Listening device should be placed over the fetal back
● Kick count
○ Daily fetal movement count (DFMC)
○ Before bedtime or after meals for 2 hours or until 10 movements are counted
○ Or client can count all movements in a 12 hour period
○ Can be done once a day but should be for 60 minutes
● Bishop score
○ Indicates cervial favorability for labor inducibility by assessing cervical dilation, effacement, station,
consistency, position
○ Score of 8 or more favors successful induction
○ Dinoprostone - a cervical ripening agent, used for scores less than 8
Other tests before labor
● Strep B
○ Done at 35-37 weeks
○ Provide penicillin intrapartum
○ If status unknown, fever >38 degrees C, or ROM > 18 hours give antibiotics
● Urinalysis
○ Check for protein in urine
● Indirect Coombs:
○ Determines if mother is Rh negative or positive
○ For negative, repeat at 24-28 weeks
○ Administer rhogam for negative at 28 weeks
Contractions
6● True
○ Beginning irregular then become predictable
○ Will continue regardless of activity
○ Become stronger with walking and more reg with a change in activity
○ Frequency and duration increases
○ Begin in lower back and spread to abdomen
■ Lower abdomen
● False
○ Begin and remain irregular
○ Will go away if client walks or goes to sleep
○ Will not increase in frequency or duration
○ Begin in abdomen and stay in abdomen and groin area
■ Upper abdomen
● Tachysystole
○ Contractions lasting longer than 2 minutes or 5 contractions in 10 minutes
○ Leads to fetal hypoxia
○ Apply facemask at 10L
○ Turn in side lying position before discontinuing oxytocin and see if that resolves
External cephalic version
● Provider attempts to turn around fetus externally
● Receives tocolytic prior to allow uterus to relax
● This is high-risk procedure and is performed in hospital setting
● High risk of umbilical cord compression or placental abruption
● Administer Rhogham after
● FHR monitored continuously because fetus at risk of bradycardia and variable decelerations
● Nurse monitors FHR 60 minutes following procedure
Ectopic pregnancy
● Ovum implanted outside uterus, usually in fallopian tube
○ Usually result of scarring caused by previous tubal infection or surgery
● S/S: unilateral stabbing pain and tenderness in LLQ or RLQ of abdomen, vaginal spotting/bleeding, referred
shoulder pain with tubal rupture
● Fallopian tube can burst
● Procedure:Salpingostomy
● Risk factors: PID
Molar pregnancy (hydatidiform mole)- Gestational Trophoblastic Disease
● Proliferation and degeneration of trophoblastic villi in placenta
● Grape-like clusters
● Vaginal discharge is usually dark brown
● S/S: bleeding that resembles prune juice, abnormally high hCG levels
● Increased incidence of melanoma
● With hydatidiform moles pregnancy must be avoided for 1 year
● hCG should be obtained following evacuation of mole and then weekly until levels are normal for 3 weeks.
Then every 4 weeks for the next 6-10 months
● Can cause HTN
Spontaneous abortion
● termination of pregnancy before 20 weeks
● Threatened: spotting, no tissue passed, cervix closed
7● Inevitable: mild to severe bleeding, no tissue passed, dilated cervix
● Incomplete: severe bleeding, partial fetal tissue passed, dilated cervix
● Complete: minimal bleeding, complete uterine contents passed, closed cervix
● Procedures: dilation and curettage (D&C), administration of prostaglandins and oxytocin for inevitable or
incomplete abortion
Placenta previa
● Placenta abnormally implants in lower segment of uterus by uterus
● Complete, incomplete or partial
○ Complete: cervix completely covered by placental attachment
○ incomplete/partial: partially covered
○ Marginal/low-lying: placenta attached to lower uterus, but does not cover the cervical os
● S/S: painless bright red vaginal bleeding during 2nd/3rd trimester
● Mothers measure slightly larger because fetus is higher in uterus
● Fundal height can be larger
● Abdomen and uterus is soft and non-tender
● Do not perform vaginal exams
Abruptio placenta
● Premature separation of placenta from uterus
● High rate of fetal and maternal mortality
● Sudden onset of intense and localized uterine pain with dark red blood
● Rigid abdomen
● Firm board-like uterus (uterine hypertonicity)
TORCH
● Often causes flu-like symptoms
● Toxoplasmosis: r/t consumption of raw or undercooked meat, handling of cat feces (cook meats thoroughly,
don’t touch cat litter)
● Other: Hepatis A and B, syphilis, mumps
● Rubella (German Measles): vaccine CI during pregnancy
● Cytomegalovirus: member of the HSV family transmitted via droplet
● HSV: transmission to baby can occur during vaginal birth if mom has active lesions ::::::::::::::::::::::::::::::::::::::::CONTENT CONTINUED IN THE ATTACHMENT:::::::::::::::::::::::::::::::::::::::::::::::::::
[Show More]