healthcare > EXAM > CHFP Module 1 Certification Test (GRADED A) Test Bank (100% Guaranteed Pass) (All)
CHFP Module 1 Certification Test (GRADED A) Test Bank (100% Guaranteed Pass)
Document Content and Description Below
is a pre-determined amount that the patient pays before the insurer begins to pay for services deductible a percentage of the insurance payment amount that is paid by the patient, along with the ... amount paid by the insurer. coinsurance a flat amount that the patient pays at each time of service copayment payment also includes amounts for services that are not included in the patient's benefit design and amounts for services balance billed by out-of-network providers. Payments typically does not include premium sharing by the patient. Out-of-pocket payment The amount payable out of pocket for healthcare services, which may includes deductibles, copayments, coinsurance, amounts payable by the patient for services that are not included in the patient's benefit design, and amounts "balance billed" by out-of-network providers. Health insurance premiums constitute a separate category of healthcare costs for patients, independent of healthcare utilization. Cost (to the patient) The expense (direct and indirect) incurred to deliver healthcare services to patients. Costs (to the provider) The amount payable to the provider (or reimbursable to the patient) for services rendered. Cost (to the health plan/insurer) The expense related to provided health benefits (premiums or claims paid) Cost (to the employer) The dollar amount a provider sets for services rendered before negotiating any discounts. The charge can be different from the amount paid. Charge The total amount a provider expects to be paid by health plans/payers and patients for healthcare services. Price An organization that negotiates or sets rates for provider services, collects revenue through premium payments or tax dollars, processes provider claims for service, and pays provider claims using collected premium or tax revenues. Health Plan/Payer An entity, organization, or individual that furnishes a healthcare service. Provider Occurs when a healthcare provider bills a patient for charges (other than copayments, coinsurance or any amounts that may remain on the patient's annual deductible) that exceed the health plan's payment for a covered service. In-network providers are contractually prohibited from balance billing health plan members, but balance billing by out-of-network providers is common. Balance Billing In healthcare, readily available information on the price of healthcare services that, together with other information, helps define the value of those services and enables patients and other care purchasers to identify, compare and choose providers that offer the desired level of value Price Transparency The quality of a healthcare service in relation to the total price paid for the service by care purchasers. Value the flow of money between the patient, the insurer, and the provider of healthcare services Revenue Cycle function between a healthcare facility or physician and an insurer is one of the most important resource management challenges in today's healthcare industry. Billing and Collection An older term used to describe payment by an insurer to a healthcare facility or physician. This term is used because a physician or healthcare facility provider render services to a patient and then submits claims a claim to an insurer. The healthcare facility or physician waits for processing of that claim by the insurer, and ultimately recieves payment, a determination of payment or a denial by the insurer. Today it is more common to use the term payment. Reimbursement The price set by a healthcare facility or physician for their services is referred to as Charges or Billed Charges The charges by a healthcare facility or physician represent the retail price and are usually compiled in a price listing known as Chargemaster a charge-based payment mechanism in which a provider is paid either list price (full charges) or a percentage of charges (full charges less a discount) for the specific services rendered. Fee-for-service What does fee for service payment provides? more units of service in order to receive more payments. Why do Healthcare Facilities set Retail prices significantly above rates actually paid by commercial insurers or the government? 1. Access to Contracted Payment Rates. -Rare not all insurers participate in provider networks that give them access to contracted payment rates. Some auto insurers, liability insurers or companies providing travel insurance to visitors from abroad still pay a provider's full charges. 2. Percent-of-Charge Contracts -In markets with little competition, percent-of-charge contracts are still common. The higher the price, the higher the percent-of-charge payment, unless the contract limits a provider's annual price increases. 3. Outlier Provisions -Some insurance contacts contain an outlier provision that entitles providers to an additional payment (a lump-sum payment or a percentage of actual charges above a threshold) for particularly sick and high-cost patients. What is the use and benefits of Cost Based Payments? The only use of this method today is in a limited set of small, rural healthcare facilities known as critical access hospitals. This mechanism has rarely been used for physicians. Cost-based payment calls for the insurer to pay the healthcare provider based on the costs of providing services, with a nominal allowance for margin. What is the Medicare program began with a payment mechanism to healthcare facilities that has since been nearly eliminated from the healthcare industry — Cost based Payment Which of the following would benefit the most from a cost-based payment method? The healthcare provider That's right! Let's understand how. The payment mechanism is advantageous for healthcare providers, as there is a higher likelihood that all costs will be paid, and there is no incentive to be efficient in providing care, since costs will be reimbursed by the insurer. The rapid escalation of healthcare costs in the U.S. after the start of cost-based payment in Medicare and Medicaid programs led to the implementation of the Prospective Payment System (PPS) of paying acute care healthcare providers for inpatient services in 1983 and outpatient services in 2000. Since then, CMS has introduced prospective payment systems for most other types of institutional healthcare providers Cost-Based payment decreased need for providers to be efficient. Mountainside Health Plan is evaluating its payment of hospitals in its current service area. It is looking to reduce its costs per patient and stabilize its overall payments to hospitals. Which of the following payment methods would be least effective for the health plan to meet these objectives? Cost-based payment You selected the correct answer. Cost-based payment is the least predictable model for a health plan and has the greatest risk of increased cost because it is dependent on the hospital's ability to manage operating costs. The table below shows the methods ranked from most predictable to least predictable. What are the 5 main types of prospective payments used in today's healthcare market? 1. DRG healthcare provider 2. Per Procedure 3. Case rate - healthcare provider or physician 4. Per diem - healthcare provider 5. Bundled payment - healthcare provider, physicians and post-acute providers A payment based on the patient's diagnosis is known as a (DRG) Diagnosis Related Group What is the most widely used in payments to healthcare providers. (DRG)'s is a classification of a disease or injury into one of approximately 750 different categories. The amount paid is a flat rate per discharge and is adjusted based on: Relative severity of the patient's condition Resources used to treat the condition as determined by the DRG for that condition (DRG) defines the increase or decrease adjustment to the payment. Relative weight (each DRG is assigned relative weight) The average level of severity of conditions of patients in a healthcare provider during a specified period is known as case mix index A _________ pays a specified fee for each procedure performed on a patient in a healthcare provider or ambulatory care facility, or by a physician. Health plan What 2 payment approaches are used in the per-procedure payment plan? (APC) Ambulatory Payment Classification and Resource Based Relative Value Scale (RBRVS) What payment approach is similar to the inpatient DRG in that the amount paid is based on the specific procedure or service provided to the patient? (APC) Ambulatory Payment Classification What payment approach is the physician payment per procedure or service, varies based on the amount of resources (usually time and effort) needed by the physician. Resource Based Relative Value Scale (RBRVS) __________ at 100% of the per-procedure fee Primary procedure _________ at 50% of the normal per-procedure fee Secondary procedure _________ 25% of the normal per-procedure fee Third and Subsequent procedure What are the common discounting approches? primary , secondary, and third/subsequent procedures Affiliated Health Plan is negotiating a new contract with a local ambulatory surgery center. Previously, Affiliated paid that surgery center on a discount-off-of-billed charges basis and is trying to change to a per-procedure method of payment. Which of the following mechanisms must Affiliated have in place in order to control its risk of increased costs? A utilization management program Because a per-procedure method creates an incentive for providers to bill for more procedures, the health plan must monitor utilization and make sure that only medically necessary services are provided. Predetermined amount paid to a healthcare provider for a specified service or range of services. Case rate What is the difference between case rate and DRG The difference between case rate and DRG is that the case rate encompasses a group of similar procedures while the DRG can be specific to a unique diagnosis and may or may not include a procedure. Where is a common area where case rates would be used? Cardiac surgery which is used primarily for payment to long-term care facilities. Per diem (or per day) payment system What health plan reimburses a facility a fixed amount per day for care to a patient per diem payment system Cons of per diem system The rate may be higher or lower depending on the type of service the patient receives; that is, per diem or per-day payment for an intensive care unit (ICU) may be higher than the payment for a day in a medical/surgical unit. This differing level of payment recognizes that a provider will spend more to care for a patient in ICU than for the more routine level of care provided in a medical/surgical unit. What are benefits of Per Diem system the per diem payment is administratively easy for the health plan and provides a predictable payment rate that is useful in setting competitive premium rates. However, the facility has a strong incentive to keep a patient longer, since an additional day of service increases payments. This requires the health plan to monitor patient length of stay to verify that the patient stay is only for the number of days that are medically necessary. This process is referred to as concurrent review. involves staff from the facility working with the health plan to review the medical justification and obtaining a certification of necessity for the patient's continued stay. This process can be resource intensive for both the health plan and provider. As with other prospective payment methods, the facility bears the risk of the cost of care possibly exceeding the per diem payment. Consequently, the facility has the incentive to limit costs and services provided to the patient to only those services deemed necessary for care during that occasion of service. Concurrent review A form of episodic payment in which the health plan pays a single prospective rate for all services provided by physicians, the healthcare provider and post-acute providers. bundled payment what are forms of risk based contracts bundles payments and other shared savings what is a step toward aligning the incentives of healthcare providers and physicians and reducing the sources of this conflict? value-based payment Inland Medical Center is contemplating a per diem payment contract for inpatient services with a local health plan. Which of the following mechanisms must be in place in order for the hospital and the payer to have acceptable financial results from this contractual relationship? A. Concurrent review What pays a fixed amount Per Member Per Month (PMPM) to a provider in advance as payment for all service necessary to the patient. Capitation What is the most common in relationships between primary care physicians and managed care plans such as health maintenance organizations (HMOs)? Capitation-However, it is also used for specialty physicians as well. _________ at 50% of the normal per-procedure fee Secondary procedure _________ at 50% of the normal per-procedure fee Secondary procedure The average level of severity of conditions of patients in a healthcare provider during a specified period is known as case mix index are examples of risk-based contracts. medicare Shared Savings Accountable Care Organizations (MSSP ACOs) established by the Affordable Care Act and the Quality Payment Program (QPP) established by the Medicare and CHIP Reauthorization Act ______ _________ contracts generally overlay a conventional payment methodology (such as fee-for-service, per diem, per case or episodic) with a retrospective settlement mechanism that shares savings (known as upside risk) or losses (downside risk) from the negotiated target. Risk-based contracts may also include provisions that reward providers for achieving certain non-cost related metrics such as quality goals or penalize them for not meeting (or reporting) them. risk based _________ the payer (government or commercial) and the provider (or group of providers) share financially in both the risks and the rewards of providing healthcare services at a negotiated rate, giving all parties a financial stake in the contract's performance. (definition) risk based contract From the perspective of the medical group, charge-based payment poses the least financial risk since the group has control over the amount of services provided and can influence payments by increasing the prices charged to an insurer. charge based payment least to greatest risk to healthcare providers. least risk - charge based payment RBRVS Per procedure payment Bundled payment greatest risk - Capitation greatest and least financial risk for the hospital greatest risk- cost based payment charge based payment DRG Payment Case rate Bundled Payment Payment based on a pre-determined amount for a specified service case rate Payment based on billed charges or a percentage discount of charges charge based Payment based on a patient's diagnosis drg Payment based on a fixed amount per day per diem Ambulatory Payment Classification (APC) and Resource-Based Relative Value Scale (RBRVS) are both approaches to which type of payment? A. Per procedure The payment category that utilizes a payment based on a fixed amount per member per month (PMPM) is: A. Capitation Susan works in the patient registration area at Chase Memorial Hospital. She has a patient at her registration station that has arrived for an upper GI procedure. Susan will need to complete several steps before the patient will be seen for care. Place the following items in order in which they should be accomplished. 1. gather demographic data from patient 2. verify that the patient's information is updated and complete 3. contact the insurer 4.educate the patient about their financial responsibility to pay 5. ask how they would like to pay 6. collect the payment Put the following during-visit activities in the correct order by dragging the activity to the correct numbered position. 1. provide and document care to the patient 2. utilization review 3. change capture 4. discharge 5. medical record completion` Paul is reviewing a claim that was denied for payment by an insurer to the physician clinic where he is employed. Which of the following items might have been an error that resulted in the claim not being paid by the insurer? C. There were duplicate E&M charges on the claim the ----- process the medical record to assign codes that describe the diagnosis of the patient's condition and the procedures performed during the patient visit. coding Paul reviews another claim that has been denied payment by an insurer. A problem with coding accuracy was the reason for the denial. Which of the following would be an obvious error in coding accuracy? Showing a hysterectomy for a male patient showing a hysterectomy for a male patient is an obvious coding error since hysterectomies are not performed on male patients. the claim for payment (or bill) is referred to as the ------ ANSI 837 Healthcare Claim Format, or more commonly as the 837 record. remittance advice sent from the health plan to the provider explaining the payment decision is also a standard ANSI format, referred to as the ANSI 835 Healthcare Claim Payment/Advice is called ------- 835 record. w at terms means: Upon receipt of the claim, the health plan will record the claim in its inventory of claims pending processing in a step known as claim logging. It is customary with the use of electronic billing for the health plan to send an electronic acknowledgment of the claim to the provider. claim logging The steps required by the health plan to process the claim for payment is collectively referred to as claims adjudication. what is the payment processing steps? 1. CLAIM LOGGING 2. ELIGIBILITY 3. ADJUDICATION 4. REMITTANCE Kate prepares claims for Palm Coast Orthopedics. Which of the following items would not be needed to be in order for her to send a clean claim? B. Copies of the patient's previous medical records Ryan is reviewing the net days in receivables data and noted that it has increased in the past month. Which of the following would be unimportant in determining why net days in receivables have increased over the past month? The amount of time required for a new patient to get an appointment has no bearing on why net days in receivables have increased. The combined activities of pre-visit, during-visit, post-visit are known collectively as the: A. Revenue cycle part of the process for clean review by a payer Adjucation cycle Which of the activities below is not a part of the pre-visit portion of the revenue cycle? C. Coding -coding occurs when the patient recieves care Which of the terms below represent the payer's steps involved in payment processing (claims adjudication)? A. Claims logging, eligibility, adjudication, remittance _____ the intentional deception or misrepresentation of facts for gain. _____ carries criminal penalties. The burden of proof is high. (beyond reasonable doubt) fraud ________ involves unintentional actions (errors) that are inconsistent with accepted, sound medical, business or fiscal practices. Abuse carries civil monetary penalties. The burden of proof is lower (preponderance of evidence) abuse What is the goal of the compliance program? to prevent fraud and abuse What is a chief enforcement vehicle of the federal govenment that allows the US Department of Health and Human Services to recover monetary damages of up to $11,000 per false claim? False Claim Act Who is someone who discloses information he or she reasonably believes evidences: -a violation of any law, rule, or regulation -gross mismanagement -gross waste of funds -abuse of authority -substantial and specific danger to public health and public safety whistleblower What does the following: Protects patients' health and demographic information (protected health information or PHI) Applies to covered entities (health plans, clearing houses, and healthcare providers) Requires signed authorization by the patient for any use or disclosure not explicitly required or permitted Limits disclosures to minimum necessary information HIPPA Health Insurance Portability and Accountability Act What does the following: prohibits physician self-referrals for health services to entities with which the physician or their family has a financial relationship. Stark I and II What does the following: makes it a criminal offense to knowingly and willfully offer, pay, solicit or receive any remuneration for, or in order to induce, referrals. Anti-Kickback Statute Which of the following is NOT a law or regulation with which healthcare entities must comply? CHIP (Childresns Health Insurance Program) provides health insurance to eligible children. This program is administered by the CMS and individual states What term is: The sources of cash given here (working capital management) cash s the definition shows, working capital is not the same as cash. It is, rather, the surplus of cash- near-cash items such as accounts receivable and liquid short-term investments, over current obligations. Working capital management entails not only keeping working capital levels adequate for day-to-day operations but also maximizing available cash. Prairie Family Care currently has a contract with Premier Health Plan to provide primary healthcare services to about 5,000 Premier members. Prairie has been paid 75% of charges for services but the contract will expire soon. Which of the following items represents a potential risk to Prairie Family Care if they accept capitation from Premier? . Potential losses from increases in service utilization Charles Medical Center is interested in forming an Accountable Care Organization (ACO) with the Medicare program. Which of the following would be a priority for Charles Medical Center in forming a Medicare ACO? A. Develop information systems As part of its strategy to become a low-cost, high-value provider that is attractive to health plans in the community, Valley Medical Center is exploring use of bundled payments in a contract with Amalgamated Health Plans. Valley Medical Center has operated in a fee-for-service relationship with Amalgamated for the past twenty years, and has been paid on DRG and case rates during that time. Physicians in the community have admitted patients to the medical center and billed Amalgamated for their services. What areas should Valley Medical Center be attentive to in accepting bundled payments? D. Identifying an equitable allocation of bundled payments among providers under the contract Which of the following describes the organization of primary care providers into a coordinated team to meet a patient's healthcare needs? medical home The Affordable Care Act encourages providers to form entities called _________ which encourages them to work together to keep patients healthy. ACO's is a payment and care delivery model, included in the affordable care act that ties provider reimbrusements based on quality metrics and expected cost reductions for the care of a defined population of patients Which of the reimbursement models below establishes a single prospective rate to all providers involved in a patient's care for the providers to divide equitably among themselves? bundled payment are payments for specific healthcare services that are intended to be shared among treatement care teams What are the drivers of consumerism 1. availiability of information about diseases, treatments, physicians, and other health professionals on the internet 2. expectations of consumers for convenience and levels of service they have become accustomed to in other sectors of the economy 3. Increased patient cost sharing (high- deductible health plans) turns patients into shopperthat demand price transparency What is the outcomes-based payment model about? about aligning incentives between health plans and providers and reconfiguring the delivery system. What are the 3 ways both must understand and engage patients? for the outcomes based payment model to succeed? 1. Health plan and providers must learn how to attract patients and increase the number of lives under mgmt 2. health pland and providers must eliminate unnceessary utlization 3. health plan and providers with the assistance of employers must learn how to help patients change behaviors that drive adverse outcomes A process by which organizational data is analyzed and converted into information usable by decision-makers business intelligence What is the business intelligence implementation process? 1. Data strategy 2. Data availability 3. Data integrity A critical first step in implementing a business intelligence function is to agree on a data strategy that specifies: What data is gathered What is measured A process to protect the accuracy of such data Once this strategy is established, management must decide what metrics will be monitored. In some cases, the metrics monitored will be dictated by government regulators or private health plans. Also, the organization may want to measure other metrics that indicate progress toward strategic objectives. Data strategy For business intelligence data to be useful, it must be available to decision-makers in time for them to take action on it. Clinical measures indicating the quality of patient care should be reported as frequently as possible (almost in real time if possible). Other metrics, such as performance on a capitation contract or income, do not need to be reported as often. A schedule of priorities for the business intelligence function should be established so that managers know when to expect information. Data availiability A final critical element in business intelligence, particularly in health [1] care, is a process for maintaining the integrity of data. Data integrity is important not only for accurate reporting of clinical data that could influence patient care, but also for evaluating the costs of care under fixed or prospective payment methodologies. As healthcare information systems become more sophisticated, the amount of data available is increasing rapidly. Business intelligence personnel must closely monitor data accuracy, implement data integrity checks and work with clinical and administrative system users to address user error that could compromise data quality. data integrity Karen White is Chief Financial Officer of Midwestern Health Plan. Karen and the CEO have agreed to implement a business intelligence function in the Plan. They want to gain a better understanding of payments and quality outcomes. What items should Karen consider as she begins to implement this function at Midwestern? A. Bring financial and clinical staff together to plan and execute analyses for the plan There are three steps in implementing business intelligence. Which of the groups of steps below represent these three steps? A. Data strategy, data availability, data integrity Payment in this definition of value is the "amount paid by all purchasers of healthcare, including the insurer and patient." payment for care Quality in this context is defined as a "composite of clinical outcomes, safety and patient experiences with healthcare services." Healthcare quality Mary Jones is CFO of Island Health System. She and the system CEO believe that it is time for the system to start focusing on value-based payments with health plans in the community. To do so, they will have to shift the way the system sets its strategic objectives. Which of the following statements best describes the changes needed at Island Health System? B. Reduce emphasis on increasing volume and increase focus on demonstrating high-quality outcomes and patient satisfaction Essential elements of the cooperative relationship between clinical and financial staff include: -common set of objectives -agreement on communication strategies -sense of trust and transparency between the two disciplines Bob Garcia is CEO of La Vida Medical Center and has just ended a meeting with his Chief Financial Officer and Chief Medical Officer. The discussion focused on the need to begin analyzing outcomes and cost. Bob is discouraged after the meeting because of a lack of buy-in from the CFO and CMO. Which of the following might represent a challenge that Bob will have to overcome in order to get analyses done on an ongoing basis? D. Breaking down silos between finance and clinical staff There are three essential elements required for clinical and financial staff to build a cooperative relationship. Choose the group of terms below that represent these elements. Jerry Weir is CEO of the Mountains Health System and is about to meet with the Board of Directors to establish management objectives for the coming year. Historically, these objectives have been set based on growth in service volumes. The sytem has consistently met those volume growth objectives under Jerry's tenure as CEO. Jerry is aware of new opportunities for Mountains Health in the areas of population health and would like to introduce some of those initiatives into future management objectives. Which of the following statements best characterizes the challenge that Jerry may have in setting objectives with his board? D. Communicating with the Board and educating them about the need to change from objectives based on volume to objectives based on value Population Health Management can best be defined as: A. A concept which promotes the overall health of a group of patients through the cooperation of providers and a health plan. Most of the challenges in population health management come from managing: E. All of the above (chronic diseases, duplicate services, risk adjustment, collaboration) Healthcare sector makes up the nations ______ % of GDP 20% gdp Examples of facility providers include hospitals, skilled nursing facilities, assisted living facilities, home health agencies, and ambulatory surgery centers. Professional providers include physicians, pharmacists, nurses, and allied health professionals (APPs) such as physical therapists, clinical social workers, and others. The broadest classification is between facility and professional providers. What are the 2 different types of physicians? Primary and Specialists What type of physicians are usually trained as family practice, general practice, general internal medicine, and pediatrics. Physicians serving in primary care roles usually treat common medical conditions or injuries, and often provide preventive health screenings. Their role is often viewed as: a coordinator of a patient's care, assessing a patient's condition (and treating if simple) or referring a patient to a specialist physician. Primary What type of physicians normally do not provide primary care services, instead focusing their work based on in-depth training in different diseases, body systems or types of healthcare service. Specialists Who are examples of Primary care physicians:? Family prac, General, General Internal, and Pediatrics Who are examples of Specialists? Cardiology, OB/GN, Pathology, and Radiology Which of the doctors and/or facilities involved in Maria's care should she expect to receive a bill from for their services? A. Primary care physician B. Radiologist C. Hospital D. Surgeon E. Anesthesiologist F. Pathologist (all correct) Which of the doctors involved in Maria's care are considered to be hospital-based physicians? a. primary care b. radiologist c. surgeon d. anesthesiologist e. pathologst b. radiologist d. anesthesiologist e. pathologist The three largest third party payers by annual expenditures are: Private health insurance, Medicare and Medicaid. Which group of words below represents participants in the healthcare system that are NOT directly involved with patient care? A. Insurers, regulators, suppliers B. Insurers, providers, regulators C. Providers, regulators, suppliers D. Insurers, providers, suppliers A. Insurers, regulators, suppliers Insurers, regulators, and suppliers are pivotal in the business environment in which care is provided. None of these entities provides medical treatment to patients. Which of the following statements is NOT true regarding fees provided for service? Select the best response. A. There is always only one provider to which fees are paid. B. There can be multiple providers involved in treatment to which fees are owed. C. There is often a third party payer which pays for services. A. There is always only one provider to which fees are paid. Explanation: It is common for several different types of providers to be involved in treatment and consequently are due fees. 50% Americans receive healthcare as a benefit through their employers. 14% of elderly Americans receive their care through Medicare. The second largest group, low-income adults and children, pregnant women and people with disabilities (20%), is covered by Medicaid or CHIP (Children's Health Insurance Program) About 6% purchase health insurance on the individual market or through the Affordable Care Act's federal and state Health Insurance Marketplaces (also known as Exchanges) Currently, approximately 9% of individuals are uninsured. Illustration: Joe does not have insurance. He is showing signs of the flu. He visits a local clinic where he is examined and learns he needs some medicine to relieve his illness. This is Joe. We will be following Joe as his circumstances change to see what effect the changes have on how he pays for his health care. Under these circumstances, Joe will in all probability: Select the best response. A. Pay the full fee to the provider. B. Pay a discounted fee to the provider. C. Both A and B depending on the provider's policies. D. Neither A or B are correct. C. Both A and B depending on the provider's policies. You selected the correct response. Joe probably will need to pay all or part of the charges he has incurred. While many providers are offering discounted prices to those who pay at the time of service, this is not always the case. About 85% of people who purchase health insurance through the Insurance Marketplaces are eligible for premium subsidies Ted's hospital bill is $50,000, the surgeon fees are $10,000 and physical therapy is $5,000. Based on the information provided in his profile, what will his total out-of-pocket expense be? a. 1260 b. 2000 c. 4316 d. 10000 c. 4316 You selected the correct response. Ted pays $1,316 for the hospital deductible + (surgeon fee of $10,000 X 20% = $2,000) + (therapy of $5,000 X 20% = $1,000) = $4,316 Medicaid and the Children's Health Insurance Program (CHIP) provide health insurance for low-income Americans, people with disabilities, pregnant mothers, and eligible children. Medicaid and CHIP are administered as joint programs between the federal government (CMS) and the individual states, with the federal government picking up about half the costs. Medicaid is the third largest domestic program in the federal budget after Social Security and Medicare and Medicaid is often the largest program in the state budget. Each state has its own Medicaid program that is financed through tax revenues and contributions from the federal government through CMS. CMS pays 50% of each state's administrative costs for administering the Medicaid program. Regarding the costs for care to Medicaid beneficiaries, CMS pays a higher share in poor states and a lower share in more affluent states (as measured by per capita income in the state). Medicaid services must include: -Inpatient hospitalization -Outpatient care -Physician services -Diagnostic lab and x-ray -Family planning -Prenatal and obstetrical care -Home health -Transportation for the medically needy to obtain healthcare services Some states administer their Medicaid program through a state government agency while other states use private managed care contractors. Again, each state Medicaid program is different from that of other states. Term which include injuries or infections incurred while the patient is hospitalized. Hospital Acquired Conditions (HAC) HAC Services to treat such conditions will not be paid by Medicare and most commercial insurers. A medical condition on the HAC list is considered to be hospital acquired if it is not shown as present on admission on the claim. Which of the following statements describes how healthcare can be financed?. A. Patient pays fees directly to the provider. B. Patient pays premiums for individual insurance. The insurer then pays the provider. C. Patient has employer provided insurance. D. All of the above. D. All of the above. Health care in the U.S. is funded by multiple payers - the patient, commercial insurers and government insurance programs. Which of the following statements is true regarding Medicare? . A. Medicare provides insurance to the poor and medically needy. B. Medicare provides insurance coverage to people over 65, persons with disabilities and persons with end-stage renal disease. C. Medicare provides insurance to people over 65 and older. D. All of the above. B. Medicare provides insurance coverage to people over 65, persons with disabilities and persons with end-stage renal disease. Medicare was established to insure persons over 65, persons with disabilities and those with end-stage renal disease. Which of the statements below is NOT true regarding provider networks? A. Insurers pay a higher portion of the patient's costs in exchange for the patient using providers within the network. B. There is a perception among patients that networks do not provide a high level of quality care. C. Provider networks were established by insurers to seek discounts on fees. D. Even in emergency situations, the patient must use an in-network provider to receive the highest benefit. D. Even in emergency situations, the patient must use an in-network provider to receive the highest benefit. Explanation: In a true emergency, patients may seek services with any appropriate provider and still receive agreed-upon benefits the cost of health insurance increases the expenses for employers, which leads to increased prices for consumer goods and services, which in turn makes U.S. employers less competitive in a world economy. increased cost of government insurance programs creates pressure on legislatures to reduce funding to non-healthcare programs or increase taxes. Generally, there is some concern that the rate of increase for healthcare expenditures in the U.S. is not sustainable over the long term. Therefore, there is some pressure on legislators in the U.S. to reform the healthcare system. In 2019, U.S. healthcare spending totaled $3.8 trillion, or $11,582 per person. The overall share of the U.S. economy devoted to health care spending was 17.7 percent, and growing at an annual rate of 4.6%. Congress passed the Patient Protection and Affordable Care Act (ACA or Obamacare) in March 2010 along narrow partisan lines. Its key provisions are what? Health insurance market reform Medicaid healthcare delivery system transformation Health insurance market reform Guaranteed issue and renewability (no exclusion for pre-existing conditions) Rating variation based on age limited to 3 to 1 ratio Medical loss ratio requirements for insurers (the proportion of premium dollars spent on clinical services must be 85 percent or higher) Individual mandate and employer requirement to provide coverage with penalties for non-compliance (note: the penalty for not obtaining insurance under the individual mandate was eliminated by the Tax Cuts and Jobs Act of 2017) Creation of state and federal Health Insurance Marketplaces (11.4 million enrollees in 2019) Benefit category standardization (bronze, silver, gold, and platinum plans) Subsidies for 85 percent of enrollees with incomes between 133 and 400 percent of the federal poverty level (FPL) Elimination of individual and health insurance plans not offering standardized benefits Imposition of a "Cadillac tax" on benefit-rich plans Medicaid -Eligibility raised from 100 percent of FPL to 133 percent in the 37 states including the District of Columbia that elected to expand Medicaid (8.5 million newly covered lives in 2016, with the federal government picking up 100 percent of the extra cost initially, then 90% thereafter) Healthcare delivery system transformation -Medicare Shared Savings Program (Accountable Care Organizations or ACOs) -Hospital Value Based Purchasing (VBP) -Bundled Payments Initiative (some voluntary, others mandatory) -Center for Medicare and Medical Innovation (CMMI) Medicaid eligibility criteria were also expanded under the affordable care act by increasing the income limits for persons to qualify for this program. The decision to expand medicaid lies with each state. The intent of increasing the number of persons eligible for medicaid to reduce the number of persons seeking care for healthcare emergencies who have no ability to pay. With more of the population covered by medicaid, providers would no longer have to shift the costs of care for the uninsured to other patients and other insurance plans. Groups of providers that agree to work together to manage the care of patients and share, sometimes with payers, the savings of achieving the Triple Aim of: (1) improving the individual experience of care, (2) improving the health of populations (population health), and (3) reducing the per capita cost of care for populations. The Affordable Care Act also introduced a new payment mechanism called bundled payments that pays a single amount for an episode of care. The last provision of the Affordable Care Act aimed at rewarding quality is Value Based Purchasing (VBP) or pay for performance (P4P). VBP pays incentives to providers for attaining predetermined quality metrics called one sided risk or places a portion of the payments to the provider at risk of loss if specified quality objectives are not met or exceeded called two sided risk. The amount of risk has been increasing year by year since implementation of the Affordable Care Act and is applied to hospital and physician provider entities. VBP has placed payments at risk of loss and the amount of potential loss could reduce or erase the income earned by a healthcare provider, greater emphasis is being placed on achieving the quality and patient satisfaction goals as a means of maintaining financial performance. costs paid by insurers to healthcare providers has a significant impact on the price an insurer charges to employees and consumers. It is important for insurers to balance the need to compete based on cost with the need to maintain relationships with providers that provide access to care. The Affordable Care Act has placed insurers in the position of competing against each other for market share in the insurance exchanges on the basis of lowest price to consumers. Which of the following terms is not a part of the Affordable Care Act's reforms? A. Medical Loss ratio B. Pre-Existing Conditions C. Non-Resiccion D. Spend Down D. Spend Down Spend down: Refers to the option to use up any existing asset or income to become poor enough to meet medicaid eligibility. This was not addressed in the affordable care act. The Affordable Care Act has created the necessity of competition between which of the following? A. Healthcare providers and consumers B. Healthcare Providers with each other C. Insurers and Healthcare providers D. Insurers and Consumers B. Healthcare Providers with each other Providers compete for consumers' choices by competing on value (cost and quality outcomes). Value = Quality (Quality is the composite of patient outcomes, safety, and patient satisfaction) / Cost (The amount paid by all purchasers of care) Which of the following activities does not occur in the financial department itself? Select the best response. A. Payroll B. Accounting/bookkeeping C. Accounts payable D. Ordering Supplies Which of the following activities does not occur in the financial department itself? Select the best response. A. Payroll B. Accounting/bookkeeping C. Accounts payable D. Ordering supplies D. Ordering supplies Finance provides needed fiscal resources for ordering supplies but does not directly place orders for supplies. Select the formula below that reflects the value proposition. A. Value = Quality/Payment B. Quality = Value/Payment C. Value = Payment/Quality A. Value = Quality/Payment Value is defined as quality (quality patient outcomes, patient satisfaction, safety and cost) and payment is the amount paid by all purchasers of care. Which of the situations listed below does NOT put inflationary pressure on expenses in the healthcare industry? A. Salaries of healthcare specialty providers B. Healthcare technology C. Risk contracting D. Increased patient volume D. Increased patient volume Increased patient volume does not create inflationary pressure. However, expenses/costs will increase as more resources are utilized. Within a hospital or physician practice, this interaction between finance and clinical staff must focus on -improving operational efficiency -quantifying the extent and benefits of clinical outcomes -proactively projecting the impact of future payment system changes. A myriad of gFacility Providers Examples of facility providers include hospitals, skilled nursing facilities, assisted living facilities, home health agencies, and ambulatory surgery centers. Facility providers Professional Providers Professional providers include physicians, pharmacists, nurses, and allied health professionals (APPs) such as physical therapists, clinical social workers, and others. Professional Providers Primary care physicians are usually trained as family practice, general practice, general internal medicine, and pediatrics. Physicians serving in primary care roles usually treat common medical conditions or injuries, and often provide preventive health screenings. Their role is often viewed as: a coordinator of a patient's care, assessing a patient's condition (and treating if simple) or referring a patient to a specialist physician. Primary Care Close Specialists Specialists normally do not provide primary care services, instead focusing their work based on in-depth training in different diseases, body systems or types of healthcare service. Examples of specialist physicians include anesthesiology, radiology, pathology, cardiology, obstetrics/gynecology, ophthalmology, orthopedics, psychiatry, general surgery, oncology, neurology, or hospitalist medicine. Specialists The specialties of radiology, anesthesiology, pathology - along with emergency room physicians and hospitalists - are commonly referred to as hospital-based physicians, since the majority of their work is done within a hospital facility. Other physician specialties may also provide care within a facility provider, such as when a surgeon operates on a patient in an ambulatory surgery center or an obstetrician/gynecologist delivers a baby in the hospital. Note - While hospitalists are hospital-based physicians, "Hospitalist" and "Hospital-based physician" are not synonyms: "Hospital medicine is a medical specialty dedicated to the delivery of comprehensive medical care to hospitalized patients." Mary wakes up this morning with a fever and some severe pain in her abdomen. She senses that something is not right and calls her family physician, a general internal medicine specialist (the primary care physician). She gets an appointment right away. Her family physician examines her and performs an ultrasound test that suggests something may be amiss in her gallbladder. The family physician asks a radiologist (a hospital based physician) to examine the test results. The radiologist determines that there is a gallstone creating the problem and that Mary will need surgery to remove the gallbladder. Mary's family physician refers her to a surgeon (the specialist) physician for surgery. Mary immediately goes to the hospital where an anesthesiologist (another hospital based physician) prepares her for the surgery. The surgeon then performs the surgery that relieves Mary's condition. After the surgery, a pathologist (yet another hospital based physician) examined the gallbladder and confirmed the diagnosis of gallstones. In the healthcare system the relationship normally seen between a buyer and seller of goods or services (such as with purchase of an appliance or home cleaning services) is unlike many other sectors of the U.S. economy. In healthcare, the patient is the consumer of services, and the provider of services is a physician or pharmacy, facility or other provider, and a third party payer (such as a government or commercial health insurance plan) pays for the services. As illustrated later in this course and again in course 5 - Managing Financial Resources - this can introduce some complication into how healthcare physicians, hospitals, and other healthcare providers operate their businesses. The three largest third party payers by annual expenditures are: Private health insurance, Medicare and Medi The "business of healthcare" is unique in that less than 11 percent of the U.S. healthcare expenditures are paid for directly by the recipients or beneficiaries of care (known as out-of-pocket). The remainder of costs are paid by someone else: employers, federal and state governments, and the healthcare industry itself (through free care and through taxes on providers, pharmaceutical manufacturers and insurers). Indirectly, of course, the cost of healthcare is borne by everyone through higher prices, lower wages, higher taxes, and an increase in the national debt. All in all, 55 percent of U.S. healthcare is financed privately, and 45 percent is financed with public funds. patient > insurer > provider Approximately 50% of Americans receive healthcare as a benefit through their employers. The second largest group, low-income adults and children, pregnant women and people with disabilities (20%), is covered by Medicaid or CHIP (Children's Health Insurance Program) ; 14% of elderly Americans receive their care through Medicare. About 6% purchase health insurance on the individual market or through the Affordable Care Act's federal and state Health Insurance Marketplaces (also known as Exchanges) Currently, approximately 9% of individuals are uninsured. Still, the cost of healthcare is a significant factor for many people. 20 percent of workers have high-deductible health plans (HDHPs). Medical debt remains a significant factor in personal bankruptcies. Premiums, deductibles, coinsurance and copays can be steep and add up despite annual out-of-pocket limits. The American healthcare system is expensive. While we have made some progress in bending the cost curve, a significant portion of healthcare spending is still wasteful and has no benefit to patients. The Commonwealth Fund has calculated that we could have saved $15.5 trillion between 1980 and 2010 if we had matched the per capita spending on healthcare of the next highest country (Switzerland) and several studies have concluded that about one-third of US healthcare expenditures are unnecessary and are due to consumer demand, defensive medicine, and medical error. 2 As a result of the Patient Protection and Affordable Care Act (also known as the ACA), more than 90% of patients in the U.S. now have health insurance. Employer-provided health insurance is still the dominant form of insurance. It remains popular with employers and employees because the tax code allows it to be provided as a pre-tax employee benefit. The Affordable Care Act has also expanded the number of people on Medicaid and made it possible for uninsured Americans who do not qualify for Medicaid to purchase subsidized health insurance through the Health Insurance Marketplace ("exchange"). It is also still possible to buy unsubsidized health insurance on the individual market. Individuals that do not get insurance from their employer can obtain individual coverage from an insurer through state or federal health insurance exchanges under the ACA. About 85% of people who purchase health insurance through the Insurance Marketplaces are eligible for premium subsidies. Part A Medicare Part A is funded primarily by Medicare taxes paid by current workers to fund the costs of current beneficiaries. Patients are usually eligible for Medicare Part A if they are a U.S. citizen over age 65, disabled or have ESRD and have paid Medicare wage taxes for at least forty (40) calendar quarters - known as categorical eligibility. Medicare Part A covers inpatient hospital services, certain organ transplants, ESRD treatment, inpatient skilled nursing facility care, home health care and hospice care. The government also acts as one of the largest insurers in the U.S. healthcare system through two major health insurance initiatives started in 1965. The Medicare program is a federal insurance program for senior citizens over age 65, persons with disabilities, and persons with End Stage Renal Disease (ESRD). Medicare has four parts. Medicare Part B is a voluntary program where a patient that meets the age or medical condition requirements for Medicare Part A (but not the requirement to pay taxes for 40 calendar quarters) may participate in this insurance benefit. It is possible for a patient to be covered by Medicare Part B but not Medicare Part A. These persons are referred to as Part B Only beneficiaries. Conversely, it is possible for a patient to have only Medicare Part A coverage but not Medicare Part B With Medicare Part A, the patient usually has only a deductible to pay for each occasion of service (a hospitalization or illness requiring home health care). The deductible changes each year but is supposed to approximate the cost of the first day of hospital care. Medicare Part A then covers the cost of days 2 - 60 of an illness or hospitalization. For days of care from 61 to 180, the patient pays a coinsurance amount per day. Patients are usually not covered under Medicare Part A after 180 days per episode of illness, though they do have a one-time bank of days to cover long stays, known as the lifetime reserve. Medicare Part B is funded by a combination of premiums paid by the beneficiary and general tax revenues from the federal government. Medicare Part B covers physician services, outpatient hospital services, outpatient diagnostic laboratory and therapy services, and outpatient mental health services. There is a small annual deductible applied to this program and the patient has a 20 percent coinsurance responsibility for all payments made by Medicare Part B. This is Ted. Ted signed up for Medicare Part A. Because he also wants coverage for physician services, he signed up for Medicare Part B and authorized a deduction for his Part B premiums from his Social Security check. Three months later, he slipped and suffered a broken hip. There are two other parts of the Medicare program that have been implemented since Medicare Part A and Medicare Part B began in 1965. Part C: Medicare Part C beneficiaries can receive Medicare benefits through a private health insurance plan such as a health maintenance organization (HMO) or preferred provider organization (PPO). Medicare Part C is also referred to as the Medicare Advantage program. A private health plan provides an alternative for patients that do not wish to receive services through traditional Medicare Part A or Medicare Part B, also referred to as Original Medicare. Medicare Advantage plans market to Medicare beneficiaries by offering benefits above those provided through traditional Medicare Part A or Part B in exchange for the patient obtaining services from a selected network of providers and being subject to utilization management programs that may limit the access to certain high-cost services. The Medicare Advantage program must provide, at a minimum, the same level of services available through traditional Medicare Part A or Medicare Part B programs, but may offer additional services for an additional premium. Medicare Part D is the newest Medicare program implemented by CMS. The part D program covers outpatient prescription medicines for persons otherwise eligible for Medicare benefits. Similar to the Medicare Advantage program, Medicare Part D is administered through private health insurers that provide prescription drug benefit management through private retail pharmacies across the U.S. Medicare A - Hospital Insurance MEDICARE B - MEDICAL INSURANCE MEDICARE C - MEDICARE ADV MEDICARE D - PRESCRIPTION DRUG PLANS Medicaid and the Children's Health Insurance Program (CHIP) provide health insurance for low-income Americans, people with disabilities, pregnant mothers, and eligible children. Medicaid and CHIP are administered as joint programs between the federal government (CMS) and the individual states, with the federal government picking up about half the costs. Medicaid is the third largest domestic program in the federal budget after Social Security and Medicare and Medicaid is often the largest program in the state budget. Each state has its own Medicaid program that is financed through tax revenues and contributions from the federal government through CMS. CMS pays 50% of each state's administrative costs for administering the Medicaid program. Regarding the costs for care to Medicaid beneficiaries, CMS pays a higher share in poor states and a lower share in more affluent states (as measured by per capita income in the state). Generally speaking, Medicaid services must include: -Inpatient hospitalization -Outpatient care -Physician services -Diagnostic lab and x-ray -Family planning -Prenatal and obstetrical care -Home health -Transportation for the medically needy to obtain healthcare services -Some states administer their Medicaid program through a state government agency while other states use private managed care contractors. Again, each state Medicaid program is different from that of other states. An important element in how much an insurer will pay a provider on behalf of a patient is the patient's choice of provider. In response to the rapid escalation of healthcare costs in the U.S., health insurers have sought discounts on fees by creating provider networks with preferred or in-network providers. Under this relationship, the insurer will pay a higher proportion of the patient's costs of care in exchange for the patient going to the in-network provider. Under many insurance plans, patients may seek care from other providers outside of the insurer network, but the insurer would pay a lesser amount and leave the patient responsible for a larger amount for their care. This provision does not apply in the case of a medical emergency. In such cases, the patient may seek care at the nearest appropriate provider. Otherwise, for medically necessary, non-emergency services (referred to as elective services, but not to be confused with cosmetic surgery, an elective service generally considered not medically necessary) the patient is usually expected to seek care from an in-network provider. Hospitals now face a list of undesirable situations or conditions — known as hospital acquired conditions (HAC) which include injuries or infections incurred while the patient is hospitalized. Services to treat such conditions will not be paid by Medicare and most commercial insurers. A medical condition on the HAC list is considered to be hospital acquired if it is not shown as present on admission on the claim. Medicare's Hospital Readmission Reduction Program (HRRP) affects more than 3,000 hospitals across the country. The program reduced payment for all discharges, not just the readmissions. In recent years, patients have expressed concern about provider networks made up of low-cost (and presumably low-quality) providers, and have been seeking information through the Internet and other sources that allows them to critically evaluate providers. In some cases, patients have applied pressure to insurers to include providers with a perceived higher level of quality, while choosing not to seek care from providers with a reputation for poorer quality. So strong has been this call for quality that some patients have elected to pay higher premiums to gain access to providers with reputations for higher quality. This greater consumer awareness of provider quality has encouraged healthcare managers to identify opportunities to improve quality, both in terms of the patient's satisfaction with care as measured by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey and through improved outcomes and patient safety. Medicare's principal quality improvement program for hospitals is the Hospital Value-based Purchasing (VBP) program which requires hospitals to report on more than 30 quality measures. The program took effect in FY2013. Given the relative size of the healthcare industry in the United States economy, health care has grown to the extent that there are concerns about health care taking resources away from other parts of the U.S. economy. Recall that most people in the United States obtain health insurance as a benefit of employment. However, the cost of health insurance increases the expenses for employers, which leads to increased prices for consumer goods and services, which in turn makes U.S. employers less competitive in a world economy. The key factors that have contributed to the higher cost of health care include: A. Technology, aging population, chronic disease and litigation B. Aging population, chronic disease, performance payment and litigation C. Technology, performance payment and litigation D. All of the above A. Technology, aging population, chronic, disease and litigation What change the basis of payment for hospital outpatient services from a flat fee for individual services to fixed reimbursement for bundled services? A. Cost payment system B. Ambulatory payment classifications C. Cost compliance and litigation D. None of the above Ambulatory payment classifications when providers try to get one payor to pay for costs that have not been covered by another payor, this refers to: A. Cost Capacity B. Cost capitalization C. Cost-shifting D. Prospective cost cost-shifting The combination of age and technology has increased cost with the passage of time. A. True B. False A. True Prescription drug coverage for Medicare enrollees, which offsets some of the out-of pocket costs for medications, this covers: A.. Medicare Part A B. Medicare Part B C. Medicare Part D D. Medicare Part F C. Medicare Part D The need to abide by governmental regulations, whether they are for the provision of care, billing, privacy accounting standards, security or the like refers to: A. Compliance B. Chronic Medicare C. Health proactive standards D. None of the above A. Compliance _____________ that providers have to pay insurers to cover the cost of defending against the lawsuits and paying large jury awards. A. Ambulatory payment classifications B. Reimbursement Insurance cost plan C. Health proactive Insurance standard act D. Increased insurance premiums D. Increased insurance premiums A set of federal compliance regulations to ensure standardization of billing, privacy and reporting as institutions convert to electronic systems is called: A. Health Insurance standard Act B. Reimbursement Insurance Act C. Medicare Reporting Act D. Health Insurance portability and Accountability Ac D. Health Insurance Portability and Accountability Act ____________ is the tendency health care practitioners to do more testing and to provide more care for patients than might otherwise be necessary to protect themselves against potential litigation. Defensive In which act, federal legislation designed to tighten accounting standards in financial reporting and that holds top executives personally liable as to the accuracy and fairness of their financial statements? A. Sarbanes-Oxley Act B. Insurance accountability Act C. Financial statement Act D. Portability and Accountability Standardized Act A. Sarbanes-Oxley Act Similarly, increased cost of government insurance programs creates pressure on legislatures to reduce funding to non-healthcare programs or increase taxes. Generally, there is some concern that the rate of increase for healthcare expenditures in the U.S. is not sustainable over the long term. Therefore, there is some pressure on legislators in the U.S. to reform the healthcare system. Increased cost of govt insurance > Necessity to reduce funding or increase taxes > Becomes unsustainable > Pressure to reform the healthcare system The definition of reform in the context of health care could take many different forms. Some consider healthcare reform to be a complete change to a national healthcare system (funded and delivered by the central government) such as that currently used in Great Britain. Others consider reform to be consolidation of health insurers into a single government operated insurance plan (funded, but not delivered, by the central government) such as that seen in Canada or France. Others still consider reform to be a change in the way that health insurance is marketed to consumers, such as use of a health insurance exchange like those in Germany or Switzerland, where all consumers have access to a panel of approved commercial insurance plans. In 2019, U.S. healthcare spending totaled $3.8 trillion, or $11,582 per person. The overall share of the U.S. economy devoted to health care spending was 17.7 percent, and growing at an annual rate of 4.6%. Health insurance market reform (ACA OBAMA PROVISION) Guaranteed issue and renewability (no exclusion for pre-existing conditions) Rating variation based on age limited to 3 to 1 ratio Medical loss ratio requirements for insurers (the proportion of premium dollars spent on clinical services must be 85 percent or higher) Individual mandate and employer requirement to provide coverage with penalties for non-compliance (note: the penalty for not obtaining insurance under the individual mandate was eliminated by the Tax Cuts and Jobs Act of 2017) Creation of state and federal Health Insurance Marketplaces (11.4 million enrollees in 2019) Benefit category standardization (bronze, silver, gold, and platinum plans) Subsidies for 85 percent of enrollees with incomes between 133 and 400 percent of the federal poverty level (FPL) Elimination of individual and health insurance plans not offering standardized benefits Imposition of a "Cadillac tax" on benefit-rich plans Medicaid (ACA - OBAMA CARE PROVISION) Eligibility raised from 100 percent of FPL to 133 percent in the 37 states including the District of Columbia that elected to expand Medicaid (8.5 million newly covered lives in 2016, with the federal government picking up 100 percent of the extra cost initially, then 90% thereafter) Healthcare delivery system transformation (OBAMA CARE ACA PROVISIONS) Medicare Shared Savings Program (Accountable Care Organizations or ACOs) Hospital Value Based Purchasing (VBP) Bundled Payments Initiative (some voluntary, others mandatory) Center for Medicare and Medical Innovation (CMMI) Cost: Initially projected at $938 billion over 10 years, financed through tax increases, fees on the pharmaceutical manufacturing and health insurance sectors and through payment cuts for providers. One of the more controversial aspects of the Affordable Care Act is its requirement for individuals to carry insurance and employers to offer it. These two provisions were intended to add more persons to the rolls of health insurers nationwide to spread the costs of healthcare over a larger number of people, hopefully reducing the prices that consumers pay for health insurance. 1. INDIVIDUAL MANDATE 2. EMPLOYER MANDATE An individual mandate requires individuals without employer-provided insurance to purchase health insurance through health insurance exchanges in each state or face tax penalties. Government subsidies to assist in the payment of health insurance premiums are available for lower income citizens not eligible for Medicaid coverage. The repeal of the individual mandate was effective January 1, 2019. The employer mandate requires employers with more than 50 employees to provide health insurance benefits to employees. Other provisions of ACA MEDICAID Medicaid eligibility criteria were also expanded under the Affordable Care Act by increasing the income limits for persons to qualify for this program. The decision to expand Medicaid lies with each state. The intent of increasing the number of persons eligible for Medicaid is to reduce the number of persons seeking care for healthcare emergencies who have no ability to pay. With more of the population covered by Medicaid, providers would no longer have to shift the costs of care for the uninsured to other patients and other insurance plans. OTHER PROVISIONS OF ACA Accountable Care Organizations (ACO) are groups of providers that agree to work together to manage the care of patients and share, sometimes with payers, the savings of achieving the Triple Aim of: (1) improving the individual experience of care, (2) improving the health of populations (population health), and (3) reducing the per capita cost of care for populations The Affordable Care Act also introduced a new payment mechanism called bundled payments that pays a single amount for an episode of care. More information on the bundled payment mechanism is in course 5 - Managing Financial Resources. Another provision of the Affordable Care Act aimed at rewarding quality is Value Based Purchasing (VBP) or pay for performance (P4P). VBP pays incentives to providers for attaining predetermined quality metrics (called one-sided risk) or places a portion of the payments to the provider at risk of loss if specified quality objectives are not met or exceeded (called two-sided risk). The amount of risk has been increasing year-by-year since implementation of the Affordable Care Act and is applied to hospital and physician provider entities. The finance function in health care organizations is ultimately the responsibility of the governing body and its finance committee which delegates the authority to the chief executive officer (CEO) who delegates the authority for direction to the chief financial officer (CFO). This is true in hospitals, health plans, and larger physician clinic entities. Larger entities may have both a CFO as the senior leader in finance with a controller reporting to the CFO. The controller would be the chief accounting officer and would be typically responsible for all accounting functions. Usually the CFO reports directly to the CEO of the business or to the owner in a smaller clinic setting. The CFO may also have a close working relationship with the governing board in a large organization or the owners in a smaller physician clinic. Financial management in a healthcare provider organization usually entails oversight of: Accounting/bookkeeping Treasury Inventory (materials management or supply chain) Budgeting Managed care contracting Reimbursement Payroll Accounts payable Financial analysis and reporting Revenue cycle. Further details on inventory and the revenue cycle can be found in Course 5 - Managing Financial Resources. Health insurance plans will usually include claims processing and contract management activities under the finance function. Since it has access to much of the data needed to manage costs and can access clinical data through its financial analysis activities, the finance function plays a much more strategic role in today's healthcare business. Historically, finance was limited to the domains of accounting, payroll, accounts payable, the chargemaster, the revenue cycle, reimbursement, contracting, the treasury function, and overseeing the supply chain. However, access to and understanding of that historical data has placed finance now in a leadership role to aid in setting the future direction of the healthcare business. With that broader strategic perspective, the challenges to the healthcare CFO are both diverse and more difficult to balance. In the past, CFOs may have been challenged to maintain operating incomes and collect sufficient cash to fund operations. As value-based payment provisions of the ACA have taken effect and some providers has seen their margins decline, the impact of quality on payments has become critical. Creating value in healthcare will require bringing payment and quality - the two factors of the value equation - to the forefront and, as in other industries, defining them around the purchaser's needs. Click the words "quality" and "cost" for more information. Balance sheet accounts are permanent accounts because their balances carry forward to each new and successive accounting period, and can be broken down into 3 categories: assets, liabilities and net assets (in a not-for-profit organization) or equity (in a for-profit organization). An asset is an economic resource available for use (you do not necessarily own the asset, but your business at a minimum has rights to use the asset). A liability is an economic obligation, or debt, owed to another person or lender. Net assets or equity is the difference between assets and liabilities and is considered the owner's financial interest in the organization, or net worth. liability is what you owe assets is what you have or owed Accounting equation By making only double sided entries which are in balance to a business's accounting record system, a bookkeeper ensures that assets always equal the sum of liabilities and owner's equity (or net assets). This fundamental equivalence is known as the accounting identity, or more commonly, the accounting equation : Assets = Liabilities + Net Assets/Equity Net assets are simply the difference between assets and liabilities. They represent an entity's financial starting position plus all of the accumulated earnings less all of the accumulated losses over time. the self-balancing nature of the accounting equation is best exemplified by a trial balance. A trial balance is a complete listing of accounts in a General Ledger in a "left" and "right" arrangement, with the debits on the left and credits on the right. Notice that a trial balance contains not only an entity's balance sheet accounts (assets, liabilities and net assets/equity) but its income statement accounts as well (revenues and expenses, which are temporary because their balances are closed out to net assets/equity at the end of the accounting period). Since by convention debits are recorded as positive numbers and credits as negative ones, a trial balance is in balance if the sums of both sides net to zero. A trial balance is the unformatted "raw material" from which financial statements are prepared. The trial balance shows the balances in any general ledger account at any point in time, but usually at an accounting period end (month, quarter, or year) Another basic element of accounting is the matching principle. The matching principle requires that revenues must be recorded in the same time period as the expenses incurred to earn that revenue. Otherwise it would be impossible to accurately assess a business's performance and measure its profits or loss in a unit of time (a month, quarter or year). Accrual based accounting is used to ensure the proper matching of revenue and expense in the accounting period in which the underlying economic transactions take place. Often, the revenue for a service provided is not realized in cash until subsequent months, and the bill and payment for a supply may not be received nor paid at the current month end, but by necessity in the subsequent month. To help get revenues and expenses matched up in the same and correct accounting periods, entries are recorded to book receivables (assets) and payables (liabilities) and the related revenues and expenses, and in accounting, these entries are called accruals. If the actual amounts are known, those amounts become the basis for the end of period accrual entries made. In some cases, if the exact amount of revenue to be collected or supplies or other expenses to be paid at the end of the accounting period we are closing is not known, then it is allowable to use a reasonable estimate until the true amount is known. In accounting, this is called an accounting estimate and can be the basis for accrual entries made at the end of an accounting period. One textbook defines an accrual as "Recognition of an expense (or revenue) and the related liability (or asset) that is caused by an accounting event, frequently by the passage of time, and that is not signaled by an explicit cash transaction." In other words, the flow of cash in or out of the business does not necessarily line up with the end of a given accounting period. These accrual entries help to square that up in the time period of interest (month, quarter or year). The matching principle is the basis for what is known as the accrual basis of accounting where revenue is recognized when earned and expenses are recognized when incurred. Most corporations are required to use the accrual basis of accounting and it is specifically required by the Centers for Medicare and Medicaid Services (CMS) for financial reporting purposes (such as a Prospective Payment System (PPS) Hospital, a Critical Access Hospital (CAH), a Federal Qualified Health Center or a Skilled Nursing Facility cost repor The accrual basis of accounting is also a requirement of: Financial Accounting Standards Board (FASB) The Government Accounting Standards Board (GASB) Generally Accepted Accounting Principles (GAAP), which is defined by the American Institute of Certified Public Accountants (AICPA) FASB, GASB & GAAP are all sets of rules and guidelines similar to those set up by the Joint Commission, State Department of Health, or CMS in the areas of clinical care and life safety - only the FASB, GASB, and GAAP rules pertain to the recording of accounting transactions he basic principles of accounting described in the previous section are used to prepare the three financial statements used in the financial management of a business, including a healthcare organization. These statements are: The Statement of Financial Position (balance sheet) The Statement of Activities (income statement or statement of operations) The Statement of Cash Flows The Statement of Financial Position (balance sheet) describes the organization's assets, liabilities, and net assets at a specific point in time, usually the end of the accounting period (month, quarter, or year). This definition applies to a physician clinic, hospital, health plan, or other health care organization. This financial statement is based on the accounting equation described earlier: assets = liabilities + net assets. Neither revenues nor expenses are shown on the balance sheet, only assets, liabilities and net asset accounts. The statement of financial position (balance sheet) is based on the accounting equation Assets = Liabilities + Net Assets/Equity The statement of activities summarizes revenues, expenses and operating income for an organization in a specified period - month, quarter, or year. The statement of activities (or income statement, as it is also called), is generally organized the same way regardless of the type of entity it relates to. The basic format of this statement is: However, the similarities end with those high-level classifications. Income statements for physician clinics, hospitals and health plans appear different from each other in the broad labels of revenues and expenses. More details are on the next slide. Many consider bad debt and charity care as the same thing — a foregone payment to someone who cannot pay — although this view is not correct. See if you can match the correct explanation for each term below. charity care- the patient does not have the ability to pay bad debt- the patient has the ability to pay but does not An increase in payables represents a source of cash, whereas a decrease in payables represents a use of cash in a given accounting period. A payable is recorded when a purchase is made on credit, but not yet paid by period end. The entity has incurred an expense, but has not yet used cash to pay for it; therefore the entity has reduced operating income, but not had the corresponding decrease in cash for expense incurred. Thus, an increase in payables represents a source of cash from operating activities. When the organization pays down its current payables, that action represents a use of cash, and would be shown on the statement of cash flows as a negative number or a number in parentheses. This is true regardless of the type of health care entity for which a statement of cash flows is prepared. With respect to payables, managers should treat accounts payable as they might handle a personal credit card, where credit is used only to supplement short term swings in cash flow, without over-extending the privilege of buying on credit. Slow or late payments to vendors can alienate those vendors, potentially costing the entity its ability to use credit. Managers are therefore cautioned to not use credit as a source of cash; that short-term benefit could result in long-term harm to a valuable business relationship. A word of caution should be considered when evaluating changes in receivables or payables for healthcare organizations, as there are some practical limitations to how far an entity can gain cash from these types of transactions. When considering an increase in receivables, managers must find a reasonable balance between aggressive collections to reduce receivables and limiting the use of cash through increases in receivables. An overly aggressive collection policy may alienate patients or health plans and should be tempered with the need to fully collect the amount due from the patient or health plan in a timely fashion. Direct costs are the costs that can be traced directly to a department, product, or service. These are the costs shown in a department manager's monthly operating report and include: Salaries of nurses or patient caregivers Salaries of department managers and supervisors Employee benefits, including paid time off (PTO) Medications Supplies Purchased services (agency nurses) Equipment maintenance contracts Direct costs in a health plan would be the actual claims payments made by the plan on behalf of its members.The key item with direct costs is that they are the costs directly associated with providing services or products.Direct costs can be variable which are costs that vary proportionately to changes in the volume of products or services or fixed which are costs that remain constant in relation to changes in the volume of products or services. Indirect costs are the costs necessary to operate the business that are not incurred in the provision of products or services to patients. These costs are sometimes referred to as "overhead" or "administrative" costs.Examples of such costs are: Salaries paid to executives Support services such as laundry, cafeteria, business office, medical records, accounting or information systems Facility operating costs such as maintenance, security or utilities This definition applies in a health plan, a hospital, or a physician office. The key point with indirect costs is that they represent the costs of providing support or resources for the actual delivery of products or services but they have no direct relationship to the volume or type of services provided.Indirect costs can also be variable or fixed. DiRECT Costs that are incurred to provide the services of a healthcare entity. INDIRECT Costs that are necessary to operate the business, outside of services to patients. VARIABLE Costs that vary directly with the volume of services provided. Cost allocation is a process by which indirect costs are assigned to a part of the organization that actually provides services to a patient or client. Since a solid understanding of the direct and indirect costs is essential to setting a fair price for services, it is equally essential that managers understand all of the costs associated with providing a service. It is important in a cost allocation exercise that all indirect costs have been allocated to all service areas of the entity. We often use the distinction of revenue producing departments to describe those direct service-providing areas of the entity that incur direct costs. The term non-revenue or overhead department is used to describe those areas that incur indirect costs REVENUE PRODUCING - DIRECT SERVICE PRODUCING AREAS NON-REVENUE/OVERHEAD DEPT-AREAS THAT INCUR DIRECT COST Has multiple parts; one for each revenue producing part COST DRIVER The amount of indirect or overhead cost to be allocated cost pool COST DRIVER The cost driver should be closely related to the manner in which a revenue producing area consumes services or obtains benefit from a non-revenue area of the entity. In this sense, manager should perceive a cost driver as a fair allocation of costs (for which they have no control) to their area of responsibility any revenue producing function in the organization. This should create an incentive for the manager in a revenue producing area to limit the amount of services they use from overhead departments to reduce costs. As pressures mount on healthcare entities to become more price competitive, a keen attention to all costs of providing services — direct and indirect — is essential Examples of Cost Drivers Department Cost Driver-Reason Administration # of employee or total revenue Accounting # of employee or total revenue Housekeeping square footage cleaned Maitenance square footage maintained or work orders complet Information Systems number of users Human Resources number of employees Lakeside Clinic is planning to renovate its existing building that will decrease the amount of square footage in its pediatric exam rooms by 500 square feet and increase the space in the billing office by 500 square feet. Lakeside Clinic allocates its housekeeping costs to revenue producing departments based on square footage. How will this change affect the allocation of housekeeping costs to the pediatric area? the amount allocated to pediatrics decreases. The amount allocated for housekeeping will decrease for the pediatric department. Which of the items below are examples of cost drivers? A. Number of employees B. Square footage utilized The step down approach considers the interrelationships between overhead departments Some situations may require the cost allocation to account for the fact that some overhead departments obtain benefits from other overhead departments. The approach that takes into consideration the interrelationships between overhead departments is one used by hospitals and nursing facilities and is known as the step-down approach. While direct allocation is not permitted on Medicare cost reports for hospitals and nursing homes, the step-down approach is permitted. The step-down approach starts with one overhead function that serves the most other departments (usually administration) and spreads its cost to other functions in the organization including other overhead functions. The overhead function having the next most service to other functions has its costs (plus the costs allocated by other overhead functions) spread to other areas of the organization. This cost allocation approach is illustrated below. Is the statement below an example of the direct method of allocation or the step-down approach to allocation? Costs are distributed to only revenue producing areas of the entity. Type either D for direct or S for step-down in the box provided. Step down The direct and step-down approaches are effective in estimating costs at a high level, such as within an entire clinic, hospital, or even a department within the organization. Knowing the total costs of operation can be useful in setting prices if volumes are fairly predictable with a limited number of charge items or if the resource usage of each service is similar. A drawback with the direct and step-down approaches is that neither is particularly useful in estimating the costs of a specific service such as a clinic or emergency room visit. This is very important when a manager needs to determine the costs of a service to set a price for that service to negotiate a specific payment rate. This is known as activity-based costing or "ABC." Activity based costing is a bottom-up or micro costing approach, in contrast to an allocation driven, top-down costing method used on the Medicare Cost Report. The process of completing an ABC analysis can be broken into four steps. Gather total costs and activity statistics Determine what drives costs (healthcare costs are frequently driven by time) Measure cost drivers Convert cost drivers into costs and calculate total per-unit costs The first step — gathering total data — establishes a rate per unit of service for the activities that are used in a service, such as in a clinic visit. For example, the manager needs to understand the cost per visit for medicine and for behavioral health in a clinic that has both medicine and behavioral health services. Using either a direct or step-down method, the analysis would result in a cost per visit that is a blend of both the medicine and behavioral health services. If the actual number of resources used in a service is different, then an analysis using direct or step-down methods could be misleading. The process of assigning indirect costs to a part of the organization that provides services to a patient is: Select the best response. A. Cost allocation Your Answer Cost allocation is the process of assigning indirect costs to a part of the organization that provides direct services to patients. offering a highly specialized service or operating in a rural market where the entity may be the only provider of healthcare services greatly simplifies the pricing decision. Entities that operate with little competition can use a full-cost pricing approach, where all direct and overhead costs and a desired level of profit (profit is considered to be an economic cost and must be considered in pricing services) are included. Under a full-cost pricing approach, the price for services covers all costs of the service plus desired profits. Buyers in this situation have little leverage to entice a service provider to lower prices since they have few alternative sources for that service. However, in today's competitive healthcare marketplace few entities — hospital, health plan, or physician — are able to use a full cost approach to set prices and may have to reduce prices in order to secure customer volumes. Hospitals or physician offices in competitive markets may find it necessary to set prices below full cost — the sum of desired profit, indirect, and direct cost — to offer a price low enough to attract customers. In such a situation, the seller of a service — hospital, physician, or health plan — must offer a discounted price that does not cover full cost. In general, a seller will offer a lower price to a customer that buys more of a service — essentially trading a lower price for higher volumes of sale. In such a situation, the seller will set its prices using a marginal cost pricing approach. This requires a manager to make difficult decisions on how much cost can be included in the price charged to a customer based on a value judgment about how much customer volume will be gained for that lower price. Ultimately, healthcare entities (whether for profit or not for profit) need to recover their full costs. If entities price some of their services using a marginal cost approach, they must charge more than full cost elsewhere in order to turn a profit. more competition may call for pricing below full cost to attract or retain volume one decreases the price of an item, the effect will be an increase in volume as an offset Hillside Hospital is a 50 bed rural provider that operates at 80% capacity and is currently making a profit. There is no other competition within a 30 mile radius. The hospital has been approached about a contract with a new health plan that could bring an additional 10% in patient volumes. Which pricing approach should it use in this situation? full cost pricing Providers with little competition should use full-cost pricing. Suburban Pediatrics is a five physician practice that operates in the suburbs of a large metropolitan area. The clinic would like to contract with Doctors Health Plan, which services 50% of the population in the area and has several other pediatric groups already under contract. Which pricing approach should it use in this situation? A. Marginal cost pricing Marginal cost pricing is used in competitive markets where providers will provide services below full-cost in order to attract volume. In order to use marginal cost pricing, a manager will first reduce the amount of profit per unit of service and expect to make a total profit goal with higher volumes of service. This is true in a health plan, hospital, or physician clinic setting. If reducing profits is not sufficient to arrive at a market competitive price, then the manager may have to critically assess the indirect costs of providing a service and reduce those costs or shift those costs to other customers who will unknowingly pay a higher price per unit of service. his cost shifting strategy is frequently used in physician clinics and hospitals, where lower prices are received from government insurers (Medicare and Medicaid) and negotiated from insurers that have large numbers of members that can generate large volumes of patient referrals. The lost revenue from discounts given to those large volume buyers is made up by higher prices charged to the other customers. This can occur in a health plan where discounts are extended to customers such as large employer groups, and higher prices per member are charged to smaller groups or individuals. Health plans and healthcare providers may take on some degree of risk in their pricing when setting fixed fee prices such as: Capitation rates Per discharge prices Insurance premiums In order to generate a profit when prices are pre-established or fixed, an entity must keep costs at or below a level known as target cost. In the past, healthcare organizations could pass on costs to their customers by raising prices. In today's competitive environment, prices are frequently dictated by others or set competitively with the intent of attracting business. In this environment, cost is driven by price rather than price by cost. This pricing strategy, when applied to capitation rates or by health plans in setting premiums, should be used only with the assistance of an actuary to ensure that the cost targets are realistic and achievable. ealth plans have two different approaches to apply target cost pricing. In the early days of commercial insurance, health plans used a community rating approach to set prices based on the costs incurred to provide services to members of a local market area (i.e., everyone in the community paid the same price). An important consideration in applying community rating is that on average, younger men tend to use fewer healthcare resources than women of childbearing age and older persons. However, under community rating, all persons pay the same premium for insurance regardless of their risk or needing healthcare services. This can be viewed as inequitable to younger people who pay a higher premium than they would if the price were linked to their relative risk of needing healthcare services. The experience rating approach breaks a community down into groups and determines the premiums they pay based on the risk of that specific group needing services. Some groups that have a higher proportion of low-risk individuals would be charged lower premiums than a group having a higher risk (older or female) demographic. There is not necessarily a best way to determine health plan premiums, though some form of experience rating remains the most common method in today's market. Jim Smith is a 24 year-old programmer for a high-tech start-up company. His employer offers health insurance through a regional health plan and he learned that the health plan uses a group rating method to determine premiums it charges to clients. Because this is a start-up company with limited resources, the company offers only a limited insurance subsidy to employees. Jim is also eligible to obtain insurance through the state health insurance exchange with a small subsidy. He has researched the state health insurance exchange and found it uses a community rating method. Based on this set of facts, which option for health insurance would likely have the lowest premium cost for Jim? A. Through his employer The company health plan uses a group rating method which takes into account his risk of illness and charges a premium that reflects that risk. Because he is a young, healthy male, his cost of health insurance will be lower than with a community rated product offered through the state health insurance exchange. Regarding full cost pricing and marginal cost pricing, which statement below is true? A. Full cost pricing includes all direct and overhead costs plus a desired level of profit and is used when competition is low reak-even analysis is a simple procedure that can assist managers in understanding the relationship between variable costs, fixed costs, revenue (volume), and profit. Fairway Family Care plans to add a new asthma prevention and treatment program to its clinic. The service would generate $75 per visit in collected revenue and incur $50 in variable costs per visit. The program would also have $10,000 in fixed costs per year. What is the break-even number of visits for this new program? C. 400 visits 75-50=25 10,000/25=400 Break-even analysis can be performed equally in a hospital, clinic, or health plan context. Direct costs (variable and fixed) in a hospital or physician clinic are fairly straightforward. Examples of variable direct costs are non-exempt staff salaries, medications and supplies. Direct fixed costs include salaries of exempt staff (supervisors and managers) and equipment costs that do not vary with volume. Indirect variable and fixed costs are costs incurred at a higher level and must be allocated to a particular revenue center. In a health plan, the direct or variable cost entails those items making up the medical loss amount described in the prior unit — claims, capitation, and case management costs — while indirect or fixed costs are exemplified by claims processing, administration, or marketing. A health plan determines its contribution margin from the difference between premiums and medical expenses and applies that against its fixed costs to determine its break-even point in members. Contribution margin= premiums- medical expenses This amount is applied against fixed costs to determine the break even point A break-even analysis is prepared to: A. Understand the level of volume needed to cover the costs of doing business and generate a profit Managing cost is important at all levels of an organization, from the executive office to the individuals taking care of patients or maintaining a healthcare facility. An executive can certainly have influence on operating costs through: Decisions to hire additional staff Setting pay rates Acquiring new technology Front-line employees who provide services can also have a significant impact on costs if they are careful in the amount of resources they use for a task. Truly, managing costs can be influenced at all levels of a physician office or hospital entity — which translates into the prices paid by consumers and the government for health insurance. t is essential that managers use some degree of judgment and context in their efforts to manage costs. There is a point where a healthcare entity can reduce costs to a point where the quality of services provided is adversely affected. If a hospital reduces its salary costs through reductions of housekeeping and nursing staff, it can result in a facility that is not kept clean or where essential patient care needs are not met. In the current healthcare industry, hospitals and physicians could see payments reduced if the quality of care to a patient results in some harm to the patient. Hospitals and physicians must be aware of the costs involved in providing a level of care that meets patient needs, while addressing constraints of a competitive marketplace. dont decrease costs at the expense of quality This concept applies equally in the health plan entity, where fees negotiated with hospitals or physicians could go so low as to limit the number of providers available to meet the medical care needs of plan members. Further, if cost-cutting goes too far in the administrative areas, the customer service needs of members or contracted hospitals or physicians would not be met. This could result in loss of members or drive available hospitals or physicians to another health plan. dont allow fees to decrease so much as to limit the number of providers available In summary, healthcare managers must be attentive to cost in order to remain competitive. However, managers must resist the temptation to maximize profits by cutting costs too far, resulting in harm to patients or failure to meet the service needs of patients or customers. A critical element of working with a budget is understanding that it is a management tool, not a financial tool. A budget sets targets and objectives based on a plan developed by management. While finance and accounting staff actively participate in budget preparation and supporting managers in quantifying the targets such as revenues or expenses, it is senior management that guides the target-setting process based on the goals of the strategic plan. Budgets are useful in helping managers better control operations in their clinic, hospital, or health plan. Comparing actual results with budget targets can help managers identify areas where improvement in performance is needed. If revenues are below expectation or expenses above budget targets, identifying those differences can guide managers toward potential problem areas and help to focus corrective action where it is most needed. Values in the budget can be used as benchmarks against which actual revenue and expense results can be compared. Budgets are set up at the total organization level or for departments or service areas in smaller organizations. Budgets are control standards that are often used to evaluate managers. Budgets provide the organization with an excellent opportunity to educate the non-financial managers on financial matters. Usually the budget for a healthcare entity is based on a forecast for the coming year. However, monitoring progress toward organizational goals on a year-by-year basis is generally ineffective, as unfavorable changes in financial performance could remain uncorrected until they have had a significant negative impact. Generally, an annual budget projection is broken down into quarterly or monthly segments and those annual subdivisions are used for ongoing monitoring and control in a healthcare business. An incremental approach is one where the budget projection starts with the actual results of the prior year and then is adjusted up or down based on expected future changes. This approach can be useful for a business that believes that past results are reasonably predictive of future activity and consistent with the goals of the business. It is also effective if managers assess each area of the budget for adjustment based on the needs of the business and known changes (such as reimbursement changes, market competition, or regulatory changes). However, this approach can preserve operational inefficiencies (such as excessive staffing or supply usage) if projections are not critically assessed from time to time. A zero-based approach is one where managers start each budget projection as if there were no past experience and each line item is justified as to its reasonableness each year period this approach can result in a tightly controlled budget, which may be appropriate in a physician clinic, hospital, or health plan in financial difficulty. The process can be tedious and very labor intensive. However, this approach can result in a more realistic and affective budget target, but at a cost of a greater amount of time and effort required to produce it. You are training a new manager in your organization on the value of a budget in management. Which of the following statements best describes the utility of a budget for management? Zero-based budgets are useful by setting all non-essential costs at zero and then reviewing actual amounts in detail. Your Answer That's right! A budget should be used to see if the business is on track to meet its strategic objectives. Some health care businesses may combine the advantages of both approaches by practicing an incremental budget on an ongoing basis and producing a zero-based budget every three to five years. This method helps an organization prepare a routine budget with relative ease, while maintaining critical assessment of the assumptions making up the budget. The key point in budgeting is that it expresses a longer-term plan in monetary terms in a one-year increme It is important for managers to understand the budgets are a tool and not an absolute number that must be achieved. A budget is used by managers to see if the business is on track to meet its strategic goals and, if it is not, what needs to be changed to move the organization closer to achieving those goals. A budget is only a projection and, therefore, has areas of imperfection when compared to actual results. However, when used with a degree of judgement, the budget can be a valuable management tool. Managers start each budget projection as if there were no past experience and each item is justified to its reasonableness each year. zero based Senior managers work with finance staff to prepare a budget, and the budget is passed on to staff to implement. top down Starts with the actual results of the prior year and is adjusted up or down based on expected future changes. incremental Work on the budget starts at the lower levels of an organization. bottoms up Budgets can be used for all of the following EXCEPT: B. An absolute number that must be achieved budget is an operations management tool that presents feedback on a service or product's performance financially. This information is useful to managers in reviewing and adjusting operations. Managers often refer to the budget as if it were one document. However, the budget is actually comprised of several components that provide important details that are useful to controlling various elements of a healthcare business. These components are normally referred to as the: operating budget, capital budget and cash budget. These budget components may not be separately identified in smaller organizations such as a physician office. However, the financial planning process for a healthcare business may include elements from each of these budget components. 3 components of a budget for a healthcare business 1. cash budget 2. capital budget 3. operating budget A capital expenditure is defined as the purchase of land, buildings, or equipment for use, not resale, in providing services to patients or clients. These items should have an expected useful life of more than one year and exceed a minimum cost of threshold (usually $1,000 or more, depending on the size and nature of the business). A capital expenditure is depreciated over the expected useful life of the asset. The level of fixed asset acquisitions as well as the useful life of each asset drives depreciation expenses on the income statement higher or lower. In the overall budgeting process, the change in depreciation should be taken into account to ensure the business can continue to generate a positive margin. Capital expenditures (and the associated depreciation) typically represented 6-10% of operating expenses in a healthcare business. Since resources available to purchase capital items are usually scarce, managers must make a rational decision about what investments they can afford to make. In a health care business, capital needs are usually classified as maintenance capital and strategic capital. Maintenance Capital Capital investments made to replace existing capabilities or maintain current service levels are examples of the maintenance capital. Strategic Capital Capital investments made to expand capacity, capabilities, or enter new service lines are termed strategic capital. Capital Budget After completion of the operating budget, managers can look at any capital investments required to achieve the budget goals or the overall strategic objectives for the business. A health plan may want to invest in new computer systems, while a hospital may seek to invest in more efficient diagnostic testing equipment, or a clinic may wish to add another exam room. Determining capital investments is an important next step in the budgeting and planning process, since capital investments can be a significant use of scarce resources for a healthcare business. These decisions are detailed in a capital budget. Trinity Medical Center has just learned that it must replace its emergency generator system. How would you categorize this capital investment and why? Maintenance capital, because it helps the medical center to maintain its ability to provide care A hospital needs an emergency generator to provide electricity for patient care if electricity from a local utility is not available. Since it had a generator before and the generator did not produce any revenue, the investment represents maintenance capital. Managers must set priorities for maintenance and strategic capital based on the availability of earnings from operations, investment income, cash levels, or the ability to incur (and repay) debt for capital items. Usually, high priority is placed on replacement of revenue-producing items or items that are required for the business to operate, even if it is not a revenue-producing area. Maintenance capital decisions are often supported by increasing repair expenses and patient safety concerns. If resources are available after meeting those replacement needs, the business can consider any new revenue-producing capital items, followed by any other non-revenue producing items. In order to finalize its prioritization, healthcare businesses may need to conduct specialized analyses of a potential capital investment to determine if the expected benefit of the investment justifies the expenditure. The potential benefit should be clearly and easily measured, such as increased revenues or decreased expenses in serving patients or clients from use of the proposed investment item. Among the techniques used in capital investment analysis are net present value (NPV), internal rate of return (IRR), and payback period. Net present value analysis estimates the present value of the future cash inflows and outflows associated with the asset (i.e., expresses them in today's dollars) and subtracts from the asset's current acquisition cost. If the present value exceeds the price of the item, the investment has a positive NPV and can be beneficial to the business. The associated IRR gives a percent answer for the capital expenditure when the NPV is artificially held constant at zero. Both NPV and IRR take into account the effects of time on money. The payback period simply estimates the net cash taken in by the business by an investment (either through increase revenues or reduced expenses) over future years and determines how long it will take for the business to collect the same amount of cash it spent on the investment. All other things equal, the investment with the shortest payback period receives the highest priority for acquisition. The payback period as described in easy to understand, but does not take into account the effects of time on money. Trinity Medical Center is evaluating the purchase of a new piece of lab equipment. The financial analysis of that project yielded the following information in the table below. Using this information, estimate the payback period for the lab equipment acquisition three Years That's Right! The total investment of $750,000 ÷ $250,000 cash per year = 3 year payback period Trinity Medical Center is evaluating the purchase of a new piece of lab equipment. The financial analysis of that project yielded the following information in the table below. Using the information on net present value provided here, what would you decide to do on this proposed capital investment and why? acquire the equipment because the net present value is positive The investment will generate $508,000 more than the $750,000 investment. Completion of the operating and capital budget allows managers to determine expected cash needs for the coming year. If the business needs cash to finance operations (due to slower collection of receivables or increased inventories) or to make capital investments, plans must consider those needs. If the business does not have enough cash to meet all those needs, then financing through a line of credit, leasing of equipment, incurring long-term debt, or fundraising are needed. These decisions form the basis of the cash budget Order for heading in budget 1. Total source of cash 2. Less use of cash 3. Total use of Cash 4. Cash needed 5. Sources of cash Now, decide and select the categories as sources of cash. A. Income from operations B. Depreciation and amortization D. Sale of old equipment Now, decide and select the categories as uses of cash. A. Capital investment Lastly, select the correct number from the options given below to complete the budget for Hillside Clinic (shown in graphic). Add income, depreciation and sale of old equipment A part of the operating budget, specifying the volume of work load expected during the time period covered by a budget. Statistical budget Details of the expected sources and uses of cash by a business as a part of its annual budget. Cash Budget A subset of the operating budget of a business, focusing on the operating revenues of that business. Revenue Budget A subset of the operating budget of a business, focusing on the operating expenses of that business. Expense Budget The operating budget is comprised of all of the following EXCEPT: Cash Budget The operating budget estimates the projected activity levels and associated revenues and expenses, the operating budget, and the sources and uses of cash. (includes: everything in that sentence NOT CASH BUDGET) Capital investments made to replace existing capabilities or maintain current service levels are examples of: B. Maintenance capital Capital investments to maintain service capabilities, or levels of service are examples of maintenance capital. Net present value analysis estimates: A. The cash flows associated with the asset over its useful life expressed in today's dollars compared to its acquisition cost Net present value is a calculation that compares the amount invested today to the present value of the future cash receipts from the investments. Managers can use the budget to manage a healthcare business by comparing budgeted amounts with actual results achieved by the business. The calculated difference between the actual and budgeted amount is known as the variance. There are two common conventions used in budget variance analysis. Favorable variance: Variances that are favorable to the business (such as revenues greater than budget or expenses lower than budget) are calculated so that they result in a positive number. Negative variance: Variances that are unfavorable (such as revenues lower than budget or expenses greater than budget) are calculated in the opposite manner, to yield a negative value. Negative values are usually expressed with parentheses around them. Variance Analysis Conventions The variance convention is usually carried out by two different arithmetic approaches. 1. When calculating a revenue variance, the budget amount is subtracted from the actual amount. actual - budget = revenue variance 2. When calculating an expense variance, the actual amount is subtracted from the budget amount. budget - actual = expense It is of course also possible to calculate variances by consistently subtracting budget from actual or actual from budget, as long as one remembers if a positive or negative variance is favorable or unfavorable. When learning about variance formulas later in this course it can be helpful to adopt a convention to always start the calculation with the one or the other Simple variance analysis: The simple budget variance uses the budget as prepared before the beginning of the fiscal period and computes the variances between the budget projection and the actual results. As its name implies, this method is very simple, taking only the difference between the actual and budgeted result, but may be limited if actual volumes differ from the budget projection. flexible variance analysis: Flexible budget variance requires the manager to adjust the budget for changes in volume by applying revenue and expense-per-unit standards to the actual volume. The analysis then determines the variance between actual results and a budget projection that has been "flexed" to the actual service volume experienced. Essentially, the flexible budget is prepared after actual volumes are known. actual - budget = variance Select the variance convention used to calculate an expense variance. Budget - Actual = Expense Variance Variance is the a calculation of variance (difference) in performance from that expected in the budget. What is a flexible budget variance analysis? A. Comparison of actual results to a budget that, when prepared, recognizes that expenditures are a function of activity levels and are adjusted accordingly Working with a flexible budget means working with a budget that adjusts or flexes for changes in activity levels. Select the variance convention used to calculate a revenue variance. Select the best response. . Actual - Budget = Revenue Variance The calculation of revenue variance begins with taking actual revenue and subtracting the budgeted amount. Rate variance (also referred to as price variance) is an estimate of how much of a total budget variance is due to the rate per unit of revenue or expense being different than the budget estimate for the entity. This is only one component of the total variance and simply tells how much of the total variance is a result of price - which is something that may not be controllable by managers. The rate variance is calculated by the formula: Using data from the fixed budget analysis example in Table 4, the rate variance for variable expenses is calculated as follows: Actual rate per visit = $81.50 Budget rate per visit = $80.00 Actual volume = 15,500 visits ($81.50 - $80.00) x 15,500 = $1.50 x 15,500 = $23,250 Unfavorable This calculation indicates that the $63,250 total budget variance for salaries and supply expenses, $23,250 was due to higher rates for labor and supplies. Calculation of the volume variance will indicate that the remainder of the total variance is due to changes in patient visit volumes. The volume variance is an estimate of the extent to which the total budget variance in a budget line item is a result of actual volumes being different from those used in the budget projection. When combined with the rate variance, volume variance can be very useful to a manager needing to know more about a budget variance. The volume variance is calculated using the formula: Using this table, note that volume variable for the variable expenses is calculated as follows: Actual volume = 15,500 visits Budget volume = 15,000 visits Budget rate per visit = $80.00 (15,500 - 15,000) x $80.00 = 500 x $80.00 = $40,000 unfavorable The total rate and volume variances should equal the total budget variance for the budget line item being evaluated. In this example, the total budget variance for variable expenses in Table 4 is $63,250. The rate and volume variance calculations demonstrated here indicate that, of the total variance, $23,250 can be attributable to differences in the expense rate per visit, and $40,000 of the variance is a result of patient visit volume that is 500 visits higher than expected. This relationship is summarized below: Rate Variance = $23,250 U Volume Variance = $40,000 U Total Variance = $63,250 U U = unfavorable Select the variance convention used to calculate a rate variance. (Actual Rate - Budget Rate) x Actual Volume = Rate Variance The correct rate variance convention is (Actual Rate - Budget Rate) x Actual Volume = Rate Variance. What is a rate variance analysis? A. An estimate of how much of a total budget variance is due to the rate per unit of revenue or expense being different than the budget estimate for the entity. Rate variance analysis is an estimate of how much of a total budget variance is due to the rate per unit of revenue or expense being different from the budget estimate. Select the variance convention used to calculate a volume variance. (Actual Volume - Budget Volume) x Budget Rate = Volume Variance This is the correct calculation of volume variance. his course focused on the budget as a primary tool for management control of operations. It is the most commonly used operational tool in the industry. The budget as a management tool can have some limitations. Primary among those is that a budget relates only to the one organization for which it was compiled and reflects that organization's unique operating characteristics. However, managers may want to see how the expectations generated within the organization through its strategic planning and budgeting processes compare with other organizations. The process of benchmarking can be a valuable exercise in gaining further insight to operational performance. Benchmarking is the comparison of key performance measures relative to the competition, other organizations, or groups of organizations compiled by an industry group like the HFMA, the American Hospital Association, America's Health Insurance Plans, or the Medical Group Management Association. Organizations such as these can provide valuable benchmarks on key ratios described elsewhere in this training material. A good example of this is the HFMA Key Hospital Financial Statistics and Ratio Medians published annually by HFMA for its members. Performance against financial targets in an operating budget can certainly help a healthcare business maintain its financial solvency, but as noted earlier, the rate and volume of inputs to providing patient care can be important in driving favorable results. In particular, the volume of labor inputs for providing care in a hospital or clinic or in serving customer service needs in a health plan can be critical in controlling labor costs. Labor makes up the majority of operating expenses in a hospital or clinic and a majority of administrative costs in a health plan. Setting standards for the amount of labor per unit of service - or a productivity standard - can be a valuable control tool for managers in healthcare businesses. Benefits of the process of benchmarking include all of the following EXCEPT: Serves as a primary tool for managers to maintain the budget Benchmarking can assist managers in thinking about activities and improvements that impact the budget. However, benchmarking is not fundamentally a budgeting tool but a performance improvement tool. strategic planning is a function that all managers can play a part in. This is especially true in healthcare finance as financial managers adopt much more of a strategic role in the industry. Not only must financial managers see the bigger picture of the organization strategically from both a business and clinical care perspective, but they must also translate that strategic vision into measurable terms through the budgeting process. Further, through the use of financial management tools such as budget and variance analysis, managers can assess problems with resource use in their businesses and better manage those resources in today's challenging healthcare industry. The revenue cycle in healthcare is the flow of money between the patient, the insurer, and the provider of healthcare services, as illustrated here and diagrammed more fully in course 1, Healthcare Finance - The Big Picture. However, the term revenue cycle is more commonly used to describe a more limited set of transactions: the sequential, interrelated processes a healthcare provider performs beginning with scheduling a patient and ending with the healthcare provider getting paid. In this course, we will use the term revenue cycle in this narrower, more conventional sense. charge - the dollar amount a provider sets for services rendered before negotiating any discounts. The charge can be different from the amount paid. price - The total amount a provider expects to be paid by health plans/payers and patients for healthcare services. Health plan - An organization that negotiates or sets rates for provider services, collects revenue through premium payments or tax dollars, processes provider claims for service, and pays provider claims using collected premium or tax revenues. Provider - An entity, organization, or individual that furnishes a healthcare service. Balance Billing - Occurs when a healthcare provider bills a patient for charges (other than copayments, coinsurance or any amounts that may remain on the patient's annual deductible) that exceed the health plan's payment for a covered service. In-network providers are contractually prohibited from balance billing health plan members, but balance billing by out-of-network providers is common. Price Transparency - In healthcare, readily available information on the price of healthcare services that, together with other information, helps define the value of those services and enables patients and other care purchasers to identify, compare and choose providers that offer the desired level of value. Value - The quality of a healthcare service in relation to the total price paid for the service by care purchasers. Per the AICPA (American Institute of Certified Public Accountants) Audit and Accounting Guide, the following payment methodologies are commonly utilized by third-party payers/health plans: Fee-for-service Per diem Per case Episodic Capitation Risk-based contracts Each type of payment may have different methods of structuring the payment to the provider. Each variation in the way a provider is paid creates different business incentives and risks for both providers and health plans. Fee-for-service is a charge-based payment mechanism in which a provider is paid either list price (full charges) or a percentage of charges (full charges less a discount) for the specific services rendered. The business incentive for a physician or healthcare facility provider under fee-for-service payment is to provide more units of service in order to receive more payments. It is because of this incentive to provide more services that health plans began in the 1980s to create utilization management programs aimed at limiting the volume of services to those that were only deemed medically necessary. The definition of medical necessity differed among health plans. Medical necessity guidelines in general were supposed to be based on best practices in medicine, so that the patient received only those services needed to address the immediate illness or injury. Most Healthcare Facilities and physicians set "retail" prices significantly above rates actually paid by commercial insurers or the government. They do this for three reasons: 1. Access to contract payment rates 2. percent of charge contracts 3. outlier provisions Reason 1: Access to Contracted Payment Rates Although increasingly rare, not all insurers participate in provider networks that give them access to contracted payment rates. Some auto insurers, liability insurers or companies providing travel insurance to visitors from abroad still pay a provider's full charges. Percent-of-Charge Contracts Reason 2: Percent-of-charge Contracts In markets with little competition, percent-of-charge contracts are still common. The higher the price, the higher the percent-of-charge payment, unless the contract limits a pro reason 2: Percent-of-charge Contracts In markets with little competition, percent-of-charge contracts are still common. The higher the price, the higher the percent-of-charge payment, unless the contract limits a provider's annual price increases. Reason 3: Outlier Provision Some insurance contacts contain an outlier provision that entitles providers to an additional payment (a lump-sum payment or a percentage of actual charges above a threshold) for particularly sick and high-cost patients. Which of the following would benefit the most from a cost-based payment method? A. The healthcare provider The payment mechanism is advantageous for healthcare providers, as there is a higher likelihood that all costs will be paid, and there is no incentive to be efficient in providing care, since costs will be reimbursed by the insurer. The rapid escalation of healthcare costs in the U.S. after the start of cost-based payment in Medicare and Medicaid programs led to the implementation of the Prospective Payment System (PPS) of paying acute care healthcare providers for inpatient services in 1983 and outpatient services in 2000. Since then, CMS has introduced prospective payment systems for most other types of institutional healthcare providers. There are five main types of prospective payment commonly used in today's healthcare market: DRG healthcare provider Per Procedure Case rate - healthcare provider or physician Per diem - healthcare provider Bundled payment - healthcare provider, physicians and post-acute providers A payment based on the patient's diagnosis is known as a Diagnosis Related Group (DRG) payment. DRGs are most widely used in payments to healthcare providers. A DRG is a classification of a disease or injury into one of approximately 750 different categories. The amount paid is a flat rate per discharge and is adjusted based on: Relative severity of the patient's condition Relative weight; Each DRG is assigned a relative weight that defines the increase or decrease adjustment to the payment. Case Mix Index- The average level of severity of conditions of patients in a healthcare provider during a specified period is known as the case mix index. The DRG approach is more favorable to the health plan than charge-based payment, as it fixes rates paid to the healthcare provider at a predictable rate. Healthcare providers have an incentive to limit the costs of providing care but also to limit the care provided to only that covered by the DRG. In addition, healthcare providers have an incentive to look for any conditions that may influence a DRG assignment to a higher relative weight to increase payment. Also, a healthcare provider bears some risk for costs if a DRG payment is not sufficient to pay the costs for a patient who uses more resources than an average patient in that same DRG classification. This is a strong incentive for a healthcare provider to limit the costs of care wherever possible, while not causing harm to the patient or reducing the quality of care provided. Would it be more beneficial to the provider to have a higher or lower DRG classification? Type H for high, or L for lower in the box below. Lowr In an effort to simplify the payment structure for healthcare providers and physicians, a per-procedure payment mechanism may be preferable. In this situation, a health plan pays a specified fee for each procedure performed on a patient in a healthcare provider or ambulatory care facility, or by a physician. Two per-procedure payment approaches are used: 1. Ambuatory and 2. resource based value If a patient receives multiple procedures during one occasion of service, then the patient record is analyzed to determine the primary procedure that was performed, and that procedure is paid at the full per-procedure rate. The fee paid for any other procedures performed during the same visit is usually discounted. The common discounting approach for per-procedure rates is to pay the: rimary procedure Primary procedure at 100% of the per-procedure fee Secondary procedure Second procedure at 50% of the normal per-procedure fee Third or subsequent procedures Third and subsequent procedures at 25% of the normal per-procedure fee As with the per-procedure method, the per diem payment is administratively easy for the health plan and provides a predictable payment rate that is useful in setting competitive premium rates. However, the facility has a strong incentive to keep a patient longer, since an additional day of service increases payments. This requires the health plan to monitor patient length of stay to verify that the patient stay is only for the number of days that are medically necessary. This process is referred to as concurrent review. Which of the following activities does not occur in the financial department itself? Ordering supplies Finance provides needed fiscal resources for ordering supplies but does not directly place orders for supplies. Select the formula below that reflects the value proposition. One way that providers and payers are aligning is around an organized effort to promote the overall health of groups of patients — a concept known as population health management. Managing population health entails a group of providers and a health plan collaborating to improve performance on measures of overall health (such as hypertension, diabetes, or cancer screenings) for a specific group of patients. Also important in this effort is improving health outcomes and ultimately reducing the amount spent on services for those patients. In the past, health plans have had the overall goal of improving population health. However, those goals — which include reducing payments for diagnostic and treatment services that make up the income for physicians and hospitals — may be in conflict. A population health initiative can help better align the interests of physicians, hospitals and health plans. The ACO model is one such way that managers outside of health plans are getting involved in the management of population health. Quality in this context is defined as a "composite of clinical outcomes, safety and patient experiences with healthcare services." healthcare quality Payment in this definition of value is the "amount paid by all purchasers of healthcare, including the insurer and patient." Payment for care Finance can lead the effort to opening the lines of communication between clinical and finance areas by providing credible data from the business intelligence function that documents efficiency and outcomes. Clinicians relate to data as long as data is credible and presented objectively. It can quickly help build an understanding between finance and clinical disciplines. Solicitation of input and ideas from clinicians on data gathering, reporting and presentation will further build that cooperative relationship. It is essential that data-sharing be done in an objective and constructive manner. One way that providers and payers are aligning is around an organized effort to promote the overall health of groups of patients — a concept known as population health management. Managing population health entails a group of providers and a health plan collaborating to improve performance on measures of overall health (such as hypertension, diabetes, or cancer screenings) for a specific group of patients. Also important in this effort is improving health outcomes and ultimately reducing the amount spent on services for those patients. n the past, health plans have had the overall goal of improving population health. However, those goals — which include reducing payments for diagnostic and treatment services that make up the income for physicians and hospitals — may be in conflict. A population health initiative can help better align the interests of physicians, hospitals and health plans. The ACO model is one such way that managers outside of health plans are getting involved in the management of population health The healthcare industry is undergoing a rapid evolution in its basic business model, moving from a volume-based emphasis to one of demonstrated value. The past skills for success for a healthcare leader that included identifying ways to increase volumes of services and prices for such services are now of lesser value. Instead, success in today's healthcare industry requires skills in working cooperatively with multiple disciplines and in understanding that business success is less related to cost-cutting and more to optimizing the use of resources to provide high-quality care. This is much more of a big picture view for healthcare leaders — the focus is less on numbers alone and more on the context in which those numbers are viewed. The successful healthcare leader must think not only about numbers but also about causes and solutions. CURRENT ASSETS- CURRENT LIABILITIES= WORKING CAPITAL Working capital is the difference between current assets (cash, receivables, short-term investments and inventory) and current liabilities (salaries and benefits payable and accounts payable): As the definition shows, working capital is not the same as cash. It is, rather, the surplus of cash- near-cash items such as accounts receivable and liquid short-term investments, over current obligations. Working capital management entails not only keeping working capital levels adequate for day-to-day operations but also maximizing available cash. Managing accounts payable and salaries payable is a straightforward process, as the payment due dates for those expenses are usually explicitly known. Inventory management is not so easy. When a patient is acutely ill and needs services that require supplies, it is not practical to wait for delivery of those items. Some supplies must be kept on hand to be immediately available to meet patient care needs. When supplies are purchased and placed into inventory, they are paid for with cash, and that cash is no longer available for other uses. Therefore, it is important to maintain the minimum level of inventory needed to address patient care needs. The days in payables ratio is also an important tool. A health plan has a large amount of payables on hand in terms of claims awaiting adjudication. Health plan managers must be sure that they are paying invoices presented for payment in a timely fashion. This is equally true for a physician clinic or healthcare provider purchasing supplies on trade credit. Timely payments are essential to maintain access to trade credit, which allows the healthcare provider or clinic to finance supplies used to provide care Working capital management involves three parts: collecting receivables, making payments only on the due date and minimizing inventory. Of these three, which is the most difficult to manage? Minimizing inventory is the most difficult to manage. It is important to have enough supplies on hand for patient treatment yet avoid carrying excess inventory. hile receivables and cash are useful for day-to-day operations, some needs of a healthcare business cannot be funded through receivables and cash. The common sources of capital to fund long-term needs are debt and equity. Short-term debt is repaid in one year or less. Long-term debt is repaid over more than one year. Debt with a maturity of one year or less is called short-term debt. Short-term debt generally consists of amounts owed to banks on revolving lines of credit, similar to personal lines of credit secured by a borrower's home equity, and the current portion of long-term debt (the portion of long-term debt due within a year or less). Other forms of short-term debt such as invoices for goods and services already delivered and provided (accounts payable) and other obligations to lenders or contractual agencies, are better characterized as current liabilities than as short-term debt. short term can be act payable and lines of credit act payable Vendors typically grant customers time (usually up to 30 days) to pay for goods shipped and services performed. In the customer's double entry accounting system these amounts are recorded as an expense and until paid, also as an accounts payable. This grace period in the due date for goods and services represents a form of short-term vendor financing that allows an entity to use its cash for other immediate uses. Strictly speaking, credit balances in patient accounts receivable are a form of debt also insofar as they represent overpayments that must be refunded to payers and patients, rather than payment and adjustment processing errors that need to be corrected. For this reason external auditors often reclassify credit balances in A/R, if material, to accounts payable in an entity's audited financial statements. line of credit Some businesses acquire additional short-term debt through a line of credit with their bank. A line of credit is like a credit card, through which the organization can draw funds as needed to meet immediate cash needs. Interest rates for a line of credit can be high, since the debt is usually not secured with any assets of the business. A line of credit can be an expensive way to finance a business if it is used repeatedly over a long period of time. However, for intermittent, short-term borrowing it may be a valuable option. There is little financial incentive in the current fee-for-service system for providers to coordinate patient care with other providers and verify that services provided are helping the patient. Historically, most insurers have not paid physicians or hospitals for preventive health services or for efforts to coordinate care with other providers, instead paying for diagnosis and treatment of a medical condition. The Patient Protection and Affordable Care Act (also known as the ACA) changed this landscape, and the focus has continued to shift from volume to value. Capitation has had some success in reducing the incentives for fee-for-service reimbursement and encouraging providers to maximize efficiency and healthcare service delivery. Depending on who controls the capitated payment on the provider side, capitation may not provide incentives for providers to coordinate care decisions with other caregivers. Instead, capitation can create an incentive to limit care to only those services needed to address a current illness or injury. Neither capitation nor fee-for-service care offers much incentive for providers to devote resources to preventive healthcare services to keep patients healthy, despite the fact that preventive care is more cost-efficient for the healthcare system overall. pros of capitation -reduces incentives of fee-for-service -encourages providers to maximize efficiency Cons of capitation -creates an incentive to limit care -no extra monthly payment for coordinating care There are four models of reimbursement that provide motivation for providers to work together to generate positive patient outcomes. These models are as follows: 1. Patient centered medical homes 2. Accountable Care Organizations ACOs 3. Bundled Payments 4. Quality Payment Program under the Medicare access and CHIP Reauthorization Act (MACRA) Primary care delivery model intended to organize providers into a coordinate team meet a patients healthcare needs Medical Home The medical home includes: Primary care, NPs, PAs, Pharmacists, Nutritionists, Health Educators, and Social Workers, to provide direct care to coordinate care Some health plans have started to contract with medical homes a way to control costs and promote greater coordination and quality of care the team of providers is organized to do the following 1. treat medical conditions 2. promote health and wellness 3. manage chronic illness such as -diabetes, -asthma, and -hypertension Comprehensive Primary Care Plus in partnership with commercial insurance plans and state Medicaid agencies to redesign primary care delivery and reward practices based on performance on patient experience, clinical quality, and cost. CPC pays prospective monthly care management fees averaging 15-28+ For providers and health plans that consider an ACO arrangement to be too labor-intensive or require too much of a capital investment, a viable alternative may be the bundled payment model. A bundled payment is a model where the health plan pays a single prospective rate to all providers involved in a patient's care and the providers then divide the payment among themselves. For example, for a patient receiving a hip replacement, a bundled payment encompasses services for the hospital, surgeon, physical therapists and home health providers. The voluntary Bundled Payments for Care Improvement (BPCI) Initiative with four care models and approximately 591 participants (2018). The two most popular models are hospital plus post-acute care and post-acute care only. Bundled Payments for Care Improvement The mandatory Care for Joint Replacement (CJR) model with 465 hospital participants in 67 geographic areas (2018). Care for Joint Replacement The voluntary Oncology Care Model with more than 138 oncologist practices participating in incentives to improve care coordination for chemotherapy patients (2020). Oncology Care Model The bundled payment model has a predictable cost structure for complex and expensive services. health plan The bundled payment model provides autonomy over how finances are organized. provider As part of its strategy to become a low-cost, high-value provider that is attractive to health plans in the community, Valley Medical Center is exploring use of bundled payments in a contract with Amalgamated Health Plans. Valley Medical Center has operated in a fee-for-service relationship with Amalgamated for the past twenty years, and has been paid on DRG and case rates during that time. Physicians in the community have admitted patients to the medical center and billed Amalgamated for their services. What areas should Valley Medical Center be attentive to in accepting bundled payments? D. Identifying an equitable allocation of bundled payments among providers under the contract The Quality Payment Program (QPP) will reform Medicare payments for more than 600,000 clinicians across the country. The QPP has two tracks. Eligible clinicians need only choose which track they prefer—MIPS or Advanced APMs—based on their practice size, specialty, location, and patient population. MIPS and APMS (MIPS)-MERIT BASED INCENTIVE PAYMENT SYSTEM- Adjusts Part B physician payments as much as 4 percent up or down in 2019, rising to 9 percent in 2022 and beyond, based on four categories of performance: Quality (replacing PQRS), Improvement Activities (a new category), Advancing Care Information (replacing EHR) and cost (replacing VM). ADVANCED ALTERNATIVE PAYMENT MODELS (APMS)- Providers participating in advanced APMs such as patient-centered medical home (PCMH), the CPC+ program, an MSSP track 2 or 3 ACO or a Next Generation ACO are exempted from MIPS reporting requirement. The APMs pay a 5 percent annual incentive payment from 2019 to 2024. The 5 percent bonus is tied to the percentage of patients a provider sees through an advanced APM in a given year. Overall, the Medical Home, ACO, bundled payment, and Quality Payment Program initiatives all provide motivation for providers to work together to generate positive patient outcomes. Also, such payment mechanisms reduce the incentive for providers to increase the volume of services and increase the incentive to be accountable for care quality and value. The models continue to evolve but share one common key element - the need for all parties to have a clear and detailed understanding of financial and clinical data to deliver efficient high-quality care. In the next section of this course, we will examine the concept of analyzing and understanding this data. Which of the following describes the organization of primary care providers into a coordinated team to meet a patient's healthcare needs? MEDICAL HOME A medical home is a team-based delivery model led by a physician that is intended to provide comprehensive medical care to patients with the goal of maximizing health outcomes and reducing overall costs. The Affordable Care Act encourages providers to form entities called _________ which encourages them to work together to keep patients healthy. ACO An Accountable Care Organization (ACO) is a payment and care delivery model, included in the Affordable Care Act, that ties provider reimbursements based on quality metrics and expected cost reductions for the care of a defined population of patients. Which of the reimbursement models below establishes a single prospective rate to all providers involved in a patient's care for the providers to divide equitably among themselves? Bundled payments are payments for specific healthcare services that are intended to be shared among treatment care teams. Health Plan Strategies -Attractive provider network design that appeals to consumers at prices they are willing to pay Transparency tools that encourage the use of high-value providers Population health incentives that reward individuals for managing their health Provider Strategies Insight into how consumers want to access care and making it easy for them to choose the health system every time Price transparency tools, including cash prices for shoppable services and procedures - There are three components of implementing business intelligence. They are: 1. Data Strategy 2. Data Availability 3. Data Integrity Data Strategy (First Step) A critical first step in implementing a business intelligence function is to agree on a data strategy that specifies: What data is gathered What is measured A process to protect the accuracy of such data Once this strategy is established, management must decide what metrics will be monitored. In some cases, the metrics monitored will be dictated by government regulators or private health plans. Also, the organization may want to measure other metrics that indicate progress toward strategic objectives. Data Availability (Second Step) For business intelligence data to be useful, it must be available to decision-makers in time for them to take action on it. Clinical measures indicating the quality of patient care should be reported as frequently as possible (almost in real time if possible). Other metrics, such as performance on a capitation contract or income, do not need to be reported as often. A schedule of priorities for the business intelligence function should be established so that managers know when to expect information. Data Integrity (Third Step) A final critical element in business intelligence, particularly in health [1] care, is a process for maintaining the integrity of data. Data integrity is important not only for accurate reporting of clinical data that could influence patient care, but also for evaluating the costs of care under fixed or prospective payment methodologies. Data strategy Specifies what data is gathered and measured Data Integrity Important for accurate reporting and for evaluating costs Data Availability Data must be received on a timely basis to be useful The HFMA Value Project defines value as "quality in relation to the total payment for care." One element of the conversation about healthcare value remains constant: Finance professionals may have limited training in clinical science, and clinical professionals may have limited training and experience in financial management. Essential elements of the cooperative relationship between clinical and financial staff include: A common set of objectives Agreement on communication strategies A sense of trust and transparency between the two disciplines Because the strategic plan for a healthcare business usually has input from multiple stakeholders, finance and clinical staff generally share a common understanding of organization goals. However, the finance or clinical perspectives may differ in how the strategic objectives can be achieved. Some clinicians may view organizational success very differently than finance staff and not consider the financial implications of clinical decisions. Finance can lead the effort to opening the lines of communication between clinical and finance areas by providing credible data from the business intelligence function that documents efficiency and outcomes. Clinicians relate to data as long as data is credible and presented objectively. It can quickly help build an understanding between finance and clinical disciplines. Solicitation of input and ideas from clinicians on data gathering, reporting and presentation will further build that cooperative relationship. It is essential that data-sharing be done in an objective and constructive manner. Providers of healthcare services to beneficiaries of federal healthcare programs such as Medicare, Medicaid, CHIP (Children's Health Insurance Program) and TRICARE (the health program for active-duty and retired uniformed service members and their families) must comply with all statutes and regulations governing those programs. compliance = conformity with applicable laws and regulations Providers that bill federal programs must have a compliance program with the following features: A chief compliance officer A hotline or other anonymous method to communicate complaints Written compliance policies and procedures Ongoing training for all personnel Disciplinary guidelines and enforcement Internal monitoring and auditing The goal of compliance programs is to prevent fraud and abuse. Let's learn about some of the laws and regulations with which healthcare entities must comply. HIPPPA STARK I AND II ANTI-KICKBACK STATUE Stark I and II rules prohibits physician self-referrals for health services to entities with which the physician or their family has a financial relationship. Anti-Kickback Statute makes it a criminal offense to knowingly and willfully offer, pay, solicit or receive any remuneration for, or in order to induce, referrals. [Show More]
Last updated: 2 years ago
Preview 1 out of 105 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$13.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 28, 2023
Number of pages
105
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 28, 2023
Downloads
0
Views
170



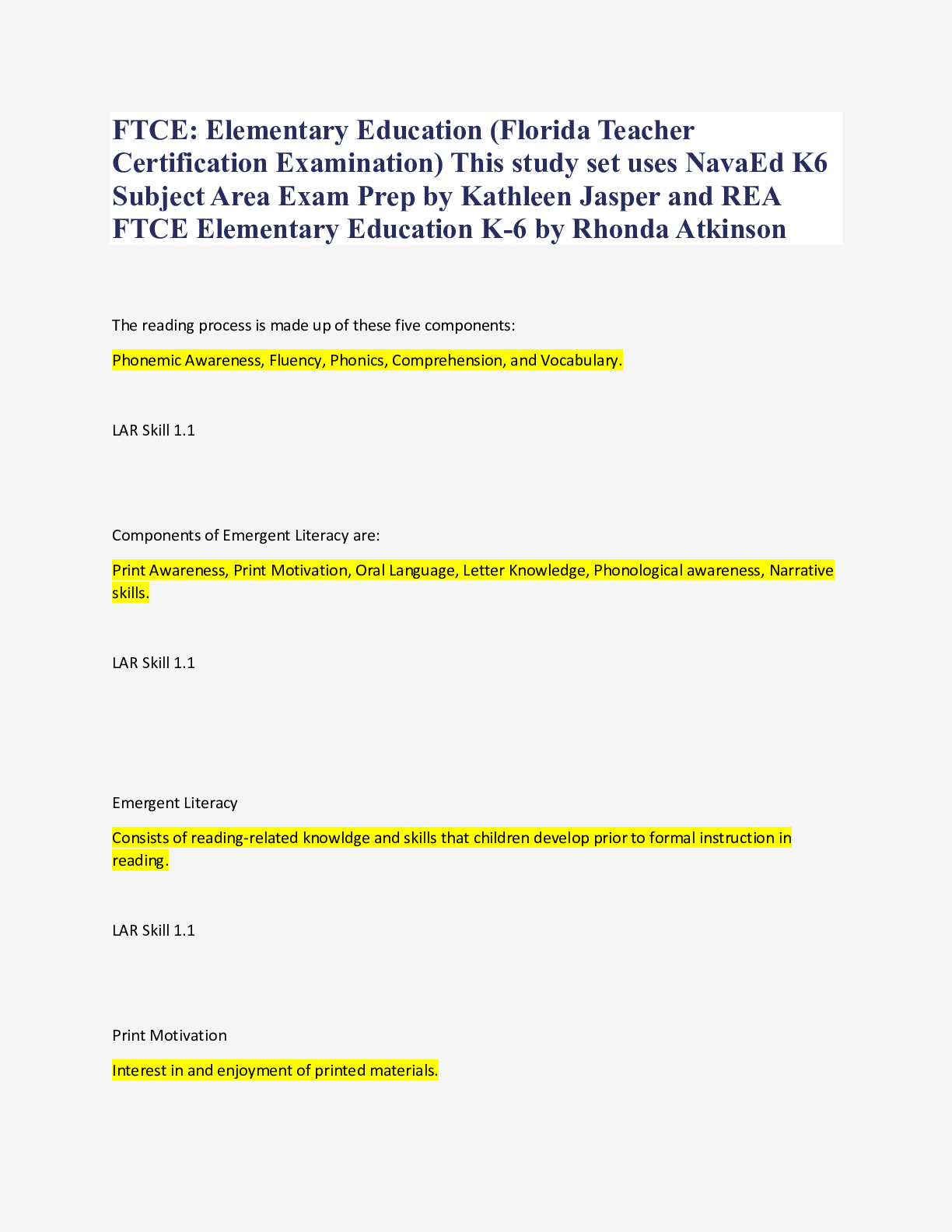

 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)