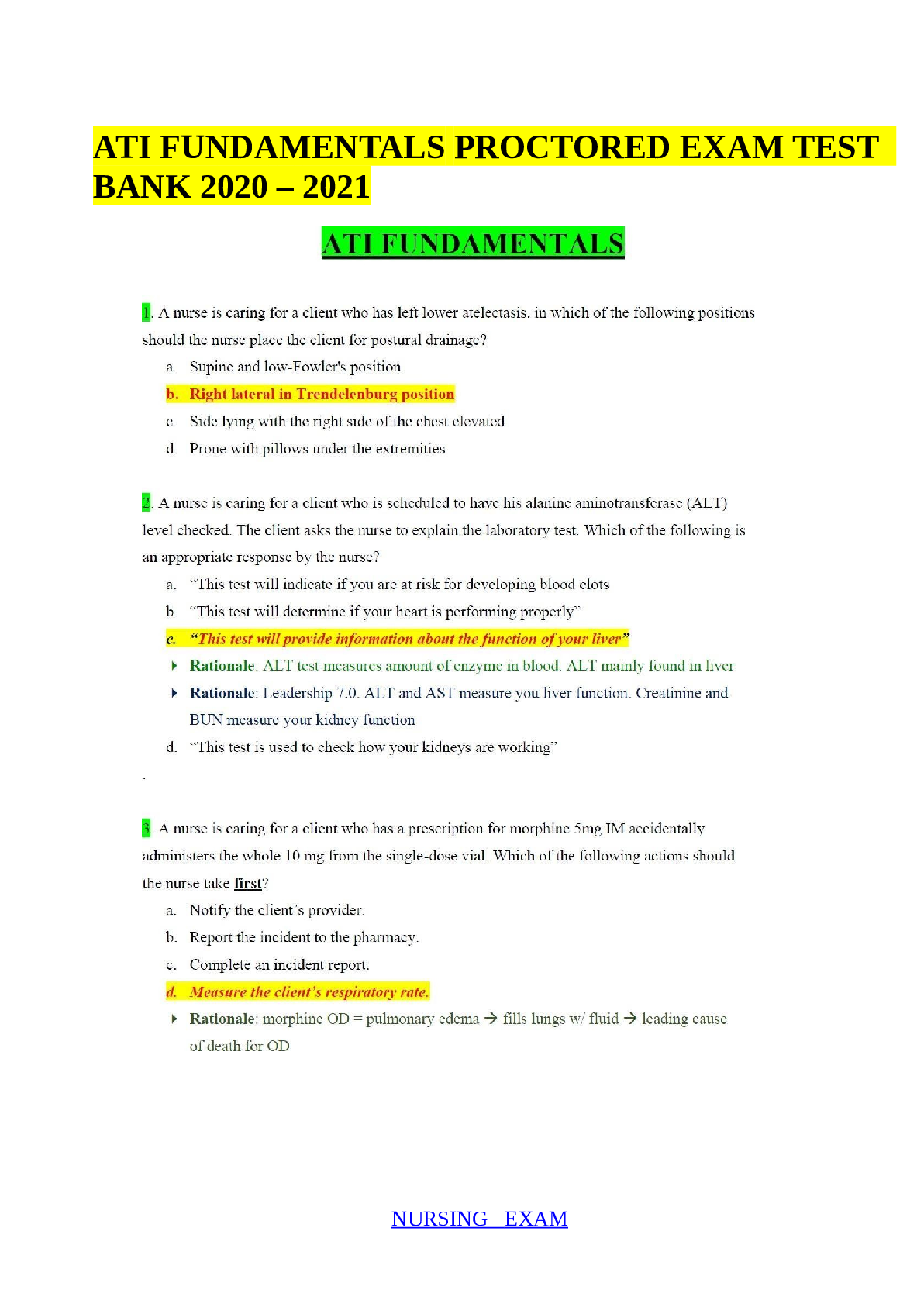
SOCRA - CCRP (high level) Questions and Answers (100% Correct Solutions)
Document Content and Description Below
Nuremberg Code (1947) A research ethics code that arose in response to the Nazis' inhumane experimentation (nuremberg trials) - holocaust, racial hygiene / eugenics / master race. The Nuremberg ... Code - 10 points 1. voluntary 2. necessary for results 3. logical design and results 4. avoid unnecessary harm 5. cannot result in death or disablement 6. risk assessment 7. protect subjects against harm 8. qualified investigators 9. right to withdrawal 10. right to end trial if needed Belmont Report (1979) Three core principles are identified: respect for persons, beneficence, and justice. Arose in response to Tuskegee Syphilis Study - studying untreated syphilis on African-American men unaware of their true condition and tx plan. Belmont Report - definitions of core 1. Respect for persons: informed consent + no deception 2. Beneficence: maximize benefits and minimize risk 3: Justice: fair procedures considering risk analysis. Belmont Report - current role Serves as a historical document and provides the moral framework for understanding regulations in the United States on the use of humans in experimental methods. Belmont Report - review of 7 items for research trials 1. IRB approved 2. Obtain informed consent 3. Ensure understanding 4. No coercion 5. Monitor adverse events 6. Maintain privacy 7. Ensure patients receive minimal care for their condition Declaration of Helsinki (1964, 1975) Set of ethical principles regarding human experimentation developed for the medical community by the World Medical Association (WMA) Good Clinical Practice (GCP) ICH-GCP and ISO-GCP (medical device) enforces guidelines on ethical aspects of a clinical trial. Covers human rights, standards on trial conduct, roles and responsibilities (IRB, PI, sponsor, monitors). GCP v Declaration of Helinski GCP lacks moral principles and guidance surrounding COI, study design, benefits, result reporting. Also restricts placebo in control group v effective alternative tx Common Rule US federal policy that specifies ethics regulations for human subjects research 1. ICF in reasonable language, reasons why they would not want to participate in research 2. Disclosure of use of de-identified data / specimens for future studies, commercial profit, clinically relevant results disclosed, genome sequencing 3. Consent waiver only if research could not be carried out without accessing / using information / specimens in an identifiable format. Pre-screening for trial permitted if able to obtain oral or written communication OR access records / stored biospecimens. 4. Exempt / Limited IRB if - record review both retrospectively AND propectively - benign behavioral interactions - collect identifiable sensitive data via adults in surveys/interviews 5. Continuing review - not required if expedited level 6. Multi-instituitional research studies required to use 1 IRB (effective 01-19-2020) Title 21 US Code of Federal Regulations (11, 50, 56, 312, 812) Title 21 is part of the code of federal regulations governing good and drugs for the FDA, DEA, and ONDCP (office of national drug control policy) 11 - e-records + e-signatures 50 - protection human subjects 56 - IRB that oversee trials 312 - drug trial requirements 812 - controlled substances Title 21 CFR Part 11 1. Controls - audits, validators, audit trails, e-sigs, documentation for software + systems processing e-data. 2. E-records cannot be illegible, inaccessible, or corrupted 3. "Hard copies" are authoritative documents for regulatory purposes Title 21 CFR Part 50 The National Research Act of 1974 Established the National Commission. Issued in 1974, 45 CFR 46 raised to regulatory status: US Public Health Service Policy Henry K. Beecher Article (1966) Detailed 22 published medical studies presenting risk to subjects without their knowledge or approval. Beecher's article clearly demonstrated that unethical research was not confined to Nazi atrocities. U.S. Public Health Service (PHS) Study of Untreated Syphilis / Tuskegee Syphilis Study (1932-1972) Examined the natural course of untreated syphilis in Black American men. All were impoverished sharecroppers from Macon County, Alabama, were unknowing subjects in the study; they were not told that they had syphilis, nor were they offered effective treatment when it became available in the late 1940s with the availability of penicillin. Willowbrook studies (1956-1970) Children with intellectual disabilities were deliberately infected with the hepatitis virus Jewish Chronic Disease Hospital study (1963) Live cancer cells were injected into 22 cognitively impaired patients. National Research Act (1974) Congress passed this act in response to the concern on prior studies (PHS Syphilis, prisoner research, willowbrook etc) - est. National Commission to identify basic ethical principles + guidelines - required IRBs at organizations receiving funding The National Commission (1975-1978) Created recommendations for regulating human subject research - vulnerable populations, psychosurgery, IRBs, etc. Final report published 1979 - Ethical Principles and Guidelines for the Protection of Human Subjects of Research -> Belmont Report The Belmont Report Based on National Commission deliberations. 1. Respect for Persons 2. Beneficence 3. Justice Analytical framework guiding the resolution of problems arising from human subject research. Belmont: Respect for Persons Subjects are autonomous agents - informed consent If diminished autonomy, need additional protection. - Condition (age, health, cognition) - Circumstances (poverty, lack of education, social status) Also respect person's right to privacy (not directly addressed in Belmont). Belmont: Beneficence Strive to do no harm while maximizing benefits + minimizing harm. Systematic Assessment - account for probability and magnitude of potential harm Benefit - to individual or advancement of scientific knowledge Minimize risk - risks in research should be the minimum to achieve the research objective. Researchers + IRBs should carefully consider alternative, less risky procedures / modifications to reduced magnitude or probability of harm. Belmont: Justice Injustice is when benefit is denied from a person without good reason, and some the burden is imposed unduly. Example: research on prisoners or institutionalized children - both will not see the benefit and must bear the burden. Subject selection - are some selected due to availability, compromised position, or manipulatability? Must be based on scientific need, not convenience. Do not exclude so they do not derive benefit (i.e. not speaking english). Undue influences from real or perceived pressures - financial, power, implied benefits. 45 CFR 46 PHS policy raised to regulatory status for "Regulations for the Protection of Human Subjects of Biomedical and Behavior Research) in anticipation of the National Research Act. First set of federal regulations detailing requirement of organizational assurances, IRB review, ICF, and ethical conduct. Revised in 1981 21 CFR 50 + 21 CFR 56 Adopted by FDA on ICF in 1980, IRBs in 1981 respectively 21 CFR 812 + 21 CFR 312 Adopted by FDA in 1980 and 1981 for investigational medical devices + drugs & biologics respectively. 45 CFR 46, Subpart A 1991 - 17 federal agencies that conduct, support, or otherwise regulate human subjects research issued uniform regulations - "The Federal Policy for the Protection of Human Subjects." = Common Rule Updated -> 2018 Requirements: strengthen human subject protections, reduce administrative burdens, add flexibility. Major changes to IRB operations, ICF, definitions, and exemptions. Declaration of Helsinki International codes + standard in response to Nuremberg Trials 1964 - World Medical Assembly meeting in Helsinki Finland adopted "Recommendations Guiding Medical Doctors in Biomedical Research Involving Human Subjects." Has been revised multiple times (1975, 1983, 1989, 1996, 2000, 2008, and 2013). CIOMS guidelines International codes + standard in response to Nuremberg Trials 1982 - Council for International Organizations of Medical Sciences adopted "International Ethical Guidelines for Biomedical Research Involving Human Subjects". Revised in 1993, 2002, and 2016. WHO guidelines International codes + standard in response to Nuremberg Trials 2001 - World Health Organization (WHO) adopted "Standards and Operational Guidance for Ethics Review of Health-Related Research with Human Participants." Designed to serve as international guidelines for the review + conduct of human subject research. ICH guidelines International codes + standard in response to Nuremberg Trials 1996 - International Conference on Harmonisation (ICH) brings together drug regulatory authorities and pharmaceutical industry of Europe, Japan, and the U.S. They adopted standards on Good Clinical Practice (ICH E6). ICH E6 details the responsibilities and expectations of all individuals - including researchers, monitors, sponsors, and IRBs. ICH E6 standards, while not part of any country's regulations, provide international standards for transnational pharmaceutical research. ICH renamed itself "International Council for Harmonisation" in 2015, added members, and in 2016 released a revised E6(R2) guideline. The FDA adopted the revised E6(R2) guideline as guidance. Presidential Commission report 1983 - Response on to further concerns regarding human subject research despite new regulations. Report raised concerns on adequacy of IRB review process. Office for the Protection from Research Risks (OPRR) (the predecessor to OHRP) at the National Institutes of Health (NIH) conducted multiple investigations of allegations of non-compliance with the regulations. Independent Reviews - General Accounting Office (GAO) & HHS Inspector General March 1996 and June 1998 respectfully GAO - IRBs overworks, competing demands, limited funds for inspections, complex research + large volumes HHS - reviewed too much too quickly with little expertise, minimal CR of approved research, little training. Are IRBs effective? Response to IRB concerns increased vigilance. OPRR began for cause and not for cause investigations. Did enact change, however then human subject Jesse Gelsinger died -> public outcry. Human Research Protections Program (HRPP) Response to issues with IRBs to further protect human subjects. Objective to assist in meeting ethical principles and regulatory requirements. Resulted in - Higher IRB standrads - Inc responsibility for researches - Inc requirements for COI - Accreditation requirements of HRPPs NBAC National Bioethics Advisory Committee (NBAC, 2001) Defines vulnerable subjects Deciding to use vulnerable populations requires: 1. To include vulnerable population? 2. Is it possible to do research without using the vulnerable population? Vulnerable population Populations at higher risk for: - Physical control, coercion, undue influence, manipulation. Federally, Due to: - children, prisoners, impaired decision-making, economically / educationally disadvantaged (45 CFR 46.111(b)) NBAC wishes to not categorize, but look at individual circumstances that may not allow them to give voluntary informed consent: - Cognitive / communicative, institutional, deferential, medical, economic, social IRB role and responsibilities - IRB's role, authority, and composition requirements are defined by federal regulations - review committee to help protect human subjects - approve, modify, disapprove, continuing review, material changes, observe, suspend / terminate approval -5+ members, varied background, 1 non-scientist, 1 scientist, 1 unaffiliated -Members must be qualified, knowledgeable and diverse HHS U.S. Department of Health and Human Services OHRP Office for Human Research Protections IRB Requirements - Risk / Benefit Analysis - ICF / Assent procedures + documentation - Subject Selection, include safeguards if research involved vulnerable populations - Privacy during recruitment and confidentiality during research - Plan for data collections, storage, and analysis (DSMB) - Design / Methods are scientifically sound - Additional - recruitment + safeguards Will also review: - PI qualifications + scientific collaborators - compliance w/ laws + regulations -IB + protocols (for FDA-regulated research) Type of IRB Review 1. Convened Committee Review - standard approach, for all new and greater than minimal risk research 2. Expedited Review - minimal changes to an approved study, no more than minimal risk & - IND / IDE not required - only collecting blood by sticks or venipuncture - noninvasive specimen collection - noninvasive procedures commonly done in clinical practice (no anesthesia or sedation, only FDA approved medical devices being used as marketed) - data collection / voice-video etc - individual group characteristic/behavior research -CR where enrollment is permanently closed with all subjected completed and is only in long-term follow-up -CR where no subjects enrolled with no additional risks -CR where study is only doing data analysis 3. Limited IRB Review of Select Exempt Categories - research education instructional strategies, techniques, curricula, or classroom management methods, which is not likely to adversely impact the student. - interactions for educational tests, surveys, interviews, or observations of public behavior & (1 or more) + privacy is kept with no identifiers + no liability to the subjects + identity can be ascertained by the investigator if needed. - Benign behavior interventions w/ data collection & (1 or more) + see above. Examples: board games, puzzles with various noises, etc. - Secondary research using private info / identifiable biospecimens & (1 or more) +knowledge is publicly available - Internal federal employee studies, contract/consulting arrangements, cooperative agreements, grants to better the public programs. - Consumer taste / food quality study - Broad consent to store / maintain identifiable private info / biospecimens for potential secondary research - Broad consent to use data/specimens for secondary research NOT Exempt: subjects prisoners, children, or observation of children with research participating in activities being observed. PI Recordkeeping PIs must keep signed consent documents, IRB correspondence, and research records for at least 3 years post trial. - sponsor/IRB may require longer. HHS Regulations 45 CFR 46 (Protection of Human Subjects 2018) applies to all human research submitted to or funded by HHS. Subpart A: Basic HHS Policy for the Protection of Human Subjects Subpart B: Additional Protections for Pregnant Women, Human Fetuses and Neonates Involved in Research Subpart C: Additional Protections Pertaining to Biomedical and Behavioral Research Involving Prisoners as Subjects Subpart D: Additional Protections for Children Involved as Subjects in Research Subpart E: Registration of Institutional Review Boards NIH Regulations sIRBs be used for multi-site trials. All Phase III randomized clinical trials are to have DSMB/DSMCs Site FWA Federalwide Assurance (FWA) = compliance assurance is a written document submitted by an organization (not an IRB) that is engaged in non-exempt human subjects research conducted or supported by HHS. Site in non-exempt research + Subject to Common Rule Each IRB that is designated by an organization under an assurance of compliance approved for federal wide use by OHRP under 45 CFR 46.103(a) and that reviews research involving human subjects conducted or supported by the HHS must be registered with HHS. sIRB Single IRBs for multi-site trials. HHS regulations further require a reliance agreement between organizations that are relying and serving as sIRBs to include the responsibilities that each will undertake. Broad Consent Broad consent may be used as an alternative to informed consent for studies involving the storage, maintenance, and secondary research uses of identifiable private information and biospecimens. ICF Parts 1. This a research study aimed to X, expected to last Y years for X visits. Every 6 months you will come in for follow-up and an injection. 2. Risks 3. Benefits 4. Alt options 5. Confidentiality, if applicable FDA inspections 6. If greater than minimal risk - explain compensation / medical tx available in the event of injury. 7. Who to contact 8. Voluntary participation statement 9. Collecting identifiable information / identifiable biospecimens must include statement about use of future studies or will not be used for future studies. Legally effective elements as applicable include: 1. Possibility of unforeseeable risks 2. Subject participation terminated by the researcher 3. Costs to the subject 4. Consequences of withdrawing consent 5. Significant new findings will be communicated if it may relate to subject's willingness to continue 6. Approximate total number of subjects 7. Biospecimens (if de-identified) may be used for commercial profit and if subject will share in that profit. 8. If results will be disclosed and under what conditions. 9. Biospecimens if it will include whole genome sequencing 42 USC 282(j)(1)(A) A description of this clinical trial will be available http://www.ClinicalTrials.gov, as required by U.S. Law. This Web site will not include information that can identify you. At most, the Web site will include a summary of the results. You can search this Web site at any time. Qualifies as a clinical trial under the HHS definition and is subject to the Common Rule, there is an additional requirement to post the consent for to a publicly available federal website from 46.116(h). Until a special website is developed, or further guidance is provided, an option is posting the consent form for the trial to ClinicalTrials.gov or a docket folder on Regulations.gov (OHRP 2019). HHS Regulations for Waivers and Alterations 1. Government projects (public service like initiatives) 2. General waivers and alterations - no more than minimal risk - cannot be carried out w/o waiver - cannot be carried out w/o private info (if applicable) - will not adversely affect rights + welfare - subjects provided with pertinent info after participation (whenever appropriate) 3. Screening, recruiting, or determining eligibility ICF Exceptions - emergency research requirements are met - life-threatening with requirements for an exception met + documentation of (a). researcher + physician agree the situation calls for test article (b). subject/LAR unable to communicate (c). insufficient time to obtain consent (d). no alternative exists providing equal or better chance of survival Waiver of Signed Consent / Oral Consent FDA - minimal risk, no procedures HHS - + only identifiable link of subject to research would be the consent and principal risk would be breach of confidentiality. Subjects will be asked if they want consent to be documented. + minimal risk, no procedures + subject part of group/community where signing forms is not the norm, minimal risk, appropriate alternative mechanism to documents ICF obtained. LAR verbal telephone consent FDA - Fax ICF to LAR, review on phone, LAR returns faxed ICF to researcher HHS - does allow the exchange of consent information to take place face-to-face or by mail, telephone, fax, or video. An electronic format for the consent signature is also allowed. Electronic informed consent (eIC) video to demonstrate a study procedure, use of a tablet instead of a paper-based consent form, and use of electronic signatures HHS regulations also require that a written copy be given to the person signing the informed consent form. The copy could be in paper or an electronic format (Protection of Human Subjects 2018). SBR Social and Behavioral Research (SBR) Refers broadly to research that deals with human attitudes, beliefs, and behaviors. Biomedical and clinical researchers sometimes incorporate SBR questions and methodologies into their physiological research. SBR Methods Questionnaires Opinion data and other oral data Direct observation Data already collected for other purposes (such as records from education, healthcare, social service programs, employment, and insurance coverage) Non-invasive physiological measurement (such as skin impedance and pupil dilation as reflection of emotional arousal or attention). SBR Risks + Benefits Psychosocial stress + discomfort Physiological harms that are less predictable, more subjective, variable, and less remediable. Socio-cultural factors (i.e. collecting demographics of undocumented immigrants v citizens) Main risk tends to be breaches of confidentiality involving sensitive data SBR Data Management Code data, secure master list, secure environment, de-linking data from identifiers SBR Debriefing Distress or deception experiment design includes debriefing about information withheld at the end of their participation. Ex: debrief subject with a description of what really happened, explain why the research could not be conducted otherwise, issue an apology. *IF deceoption is used for benign behavioral intervention, research must inform the subject that they will be deceived before participating in research. Records-Based Research Hypotheses can be posed and answered by analyzing documented information in various types of paper or electronic records (such as medical, motor vehicle, criminal justice, or school records). Must: 1. Understand risks 2. Plan to minimize those risks 3. Obtain required approvals before conducting research Privacy defined in terms of having control over the extent, timing, and circumstances of sharing oneself (physically, behaviorally, or intellectually) or information about oneself with others. *Low when patient gave IC, however much higher if records review without consent. Confidentiality pertains to the actual handling of the personal information once it is obtained. Risk Minimization Ethical and regulatory responsibility to minimize research risks to human subjects Common rule - research exclusions The Common Rule specifically excludes certain activities from the definition of research: - Scholarly or journalistic activities - Public health surveillance activities - Criminal justice activities (collection and analysis of information, biospecimens, or records) conducted for criminal justice purposes - Authorized operational activities in support of intelligence, homeland security, defense, or other national security missions Is the research eligible for exemption from the federal regulations? Records-based research may be exempt if any of the following apply: 1. identifiable private info is publicly available 2. Info recorded in a manner that the subject cannot be identified (no contact, will se identifiers but will not record) 3. Research information for purpose of "health care operation" or "research" 45 CFR 164.501 - or "public health activities and purposes" - 45 CFR 164.512[b] 4. Federal dept/agency using gov't information for non-research activities 5. Identifiable private information used for secondary research in which broad consent was obtained + documented; waiver of consent obtained; IRB does limited IRB review to determine secondary research is within scope of broad consent + does not include returning individual research results to subjects unless legally required Expedited review? If the records review activity constitutes human subjects research, and does not qualify for exemption, it will then be subject to federal regulations. - no more than minimal risk - in expedited review category 5 (prospective / retrospective research using materials) limited data set If most, but not all, mandated identifiers are removed Family Educational Rights and Privacy Act (FERPA) Includes public kindergarten through twelfth grade (K-12) schools and postsecondary institutions Genomics v Genetics Genomics - DNA sequence in cell to biological function Genetics - inherited differences in DNA sequence between individuals + the effect of the difference in biological function if any Genetic & Genomic Research Risks - reveal predispositions to future disease, making information psychologically powerful + raising concerns of stigma/discrimination - Gene sequences shared by relatives, one person's genetic info provides information on their relatives who did not necessarily consent - Reveal ancestry conflicting with family / social / religious histories & beliefs - Genetic concepts + info have historically been misused to affect social/political ends Genetic Determinism controlling influence on human health, behavior, and disease. GWAS studies with WGS or WES GWAS = genome-wide association studies WGS = whole genome sequencing WES = only parts of genome coding for proteins (1% of entire DNA sequence) Large genomic studies by NIH requirements de-identify upload to central databases Maximizes use of information generated since studies are complex, difficult, and expensive Clinical v Research Information Many organizations do not segregate clinical and research information in electronic medical records. Is DNA truly able to anonymized? Yes In order to re-identify DNA sequence information, those attempting the re-identification must have a reference sequence that includes individual identifiers. That is, the DNA sequence is not intrinsically identifiable. While the risk of re-identification currently is low, it may increase with time due to technological developments. Therefore, research subjects should be told that there is a small risk of future re-identification of de-identified information or biospecimens. As with all research involving informational risks, researchers cannot guarantee complete confidentiality. To date, there are no instances of re-identification of data or specimens for illicit motives. Researchers who obtain access to some de-identified datasets, like the NIH database of Genotypes and Phenotypes (dbGaP) resource, are required to guarantee that they will not attempt to re-identify data. Any attempt to re-identify data or specimens would be a serious breach of research ethics unless explicitly authorized by an IRB for a critical purpose. Group privacy More broadly, some genetic research can produce discoveries about entire subpopulations, some of which correspond to racial or ethnic groups. Genetic Research ICF - lay language. - specimen storage & access information - if can be contacted about individual results - if a code can be used to re-link identity to samples - plan to develop commercial products or assays, and info about financial rights - future testing of samples. - future research studies, including those that may have a different focus. - if result (general, personal results, or incidental) will be returned to subjects. - yes/no to whole genome sequencing - commercial profit - sharing y/n - disclosure if clinically relevant results Managing incidental findings If the genetic analysis is likely to yield incidental findings, the study should describe plans for management of such findings. Management plans should include a description of the responsible individual that makes the determination of what results to return and who will inform the research subjects. Genetic Information Nondiscrimination Act (GINA) in 2008 GINA prohibits discrimination in healthcare insurance and employment based on genetic information. NIH Genomic Data Sharing Policy (2014) - Genomic data without associated phenotypic characteristics are available in an unrestricted fashion to the general public - Genomic data without associated phenotypic characteristics are available in an unrestricted fashion to the general public 45 CFR 46, Subpart D 45 CFR 46, Subpart D - Additional Protections for Children as Research Subjects. 45 CFR 46.404-7 Research was to be classified according to the risk and the direct benefit to the child. 45 CFR 46.116(f) Waiver or alteration of consent or assent is also allowed for children where studies involve no more than minimal risk (defined under 45 CFR 46.404) 45 CFR 46.404 Research on children must present no more than minimal risk to the subject. (blood work, urine, CXR, psychological tests, observation) Direct benefit is not required. Requires consent from >=1 parent 45 CFR 46.405 Research that presents greater than minimal risk to the subject may be approvable under 45 CFR 46.405 if it holds the potential for direct personal benefit to the child. Requires consent from >=1 parent 45 CFR 46.406 Research involving greater than minimal risk and no prospect for direct benefit to the child subject. - Risk is no more than minor increase (catheter, biopsy, MRI, sensitive survey) - Risks must be commensurate with those risks inherent in the subject's actual medical situation, assent if possible. (additional bone marrow biopsy in) - Research must be likely to yield knowledge of vital importance about the child's disease or condition. Requires consent from >=2 parent 45 CFR 46.407 Presents an opportunity to understand, prevent, or alleviate a serious problem affecting the health and welfare of children. -Review by HHS by panel of experts Requires consent from >=2 parent 45 CFR 46.409 Ward research not permitted if not necessary to include them. Advocate needs to be appointed to act in best interest of the child. Assent The child's assent is not a necessary condition for proceeding with the research if the IRB determines that: - capability of some or all of the children is so limited that they cannot reasonably be consulted - intervention or procedure involved in the research holds out a prospect of direct benefit that is important to the health or well-being of the child (45 CFR 46.405) and is available only in the context of the research NIH Guidelines - research on children March 1998, the NIH published Guidelines on the Inclusion of Children as Participants in Research Involving Human Subject -Children must be included in all human subjects research, conducted or supported by the NIH, unless there are scientific or ethical reasons not to include them Exclusion reasons: -irrelevant to children -study results are known in children or from another study ongoing -separate age-specific study is warranted + preferable -insufficient data in adults to determine potential risks in children 21 CFR 50, Subpart D Additional Protections for Children in Clinical Investigations in response to Children's Health Act of 2000 -does not allow waiver of consent except in emergency research keeping with 21 CFR 50.23 & 50.24 -FDA will not object when IRBs approve waiver/alteration of consent in research with minimal risk if other criteria are met + documented Best Pharmaceuticals for Children Act (2002) extends marketing exclusivity for pharmaceutical companies who test new drugs in children Pediatric Research Equity Act (2004) enables FDA to require testing of drugs for pediatric use Common Rule - Exemptions with child research Research with children is eligible for exemption in categories 1, 4, 5, 6, 7, and 8 listed in 45 CFR 46.104. Research with children may also be exempt under category 2: + observation of public behavior, the researcher does not participate in the activities being observed. + administering educational tests + Information recorded that the identity of subjects could not be easily ascertained (directly or through identifiers linked to subjects). + disclosure of the subjects' responses would not place the subjects at risk of criminal or civil liability or be damaging to them. Common Rule - Expedited with child research Research subject to Subpart D may be approved via expedited IRB review. The only limitation is Category 2 with respect to the amount and frequency of blood that may be collected (OHRP 1998). 45 CFR 46, Subpart B Additional Protections for Pregnant Women, Human Fetuses and Neonates Involved in Research Came about in 1975 post 1970's Roe v. Wade when US Congress required National Commission to report on research on a human fetus. Research Involving Pregnant Women or Fetuses Minimal risk + benefit to mom/fetus = allowed Minimal risk + no benefit = allowed if important knowledge Greater than minimal + benefit = allowed if risk to fetus is least possible Greater than minimal + no benefit = NOT allowed Both fetus parents consent if benefit only to child. Research Involving Neonates (aka new borns) Uncertain viability - only if no added risk - or if it may increase survival to viability Consent = - Parent or LAR of parent Non-viable - vitals not artificially maintained - research will not terminate heartbeat / respiration - no added risk - important knowledge that is not by any other means Consent = Parent or LAR of parent Viable = Child Research Involving Dead Fetus, Fetal Material, or the Placenta In most states, the use of tissue from dead fetuses for research purposes would fall under the Uniform Anatomical Gift Act (UAGA), which requires consent of both parents. However, some states specifically ban research that involves aborted fetuses, their organs, tissues, or remains. Research involving fetal material for transplantation and utilizing embryos produced by in vitro fertilization for the generation of human embryonic stem cell lines has been subject to additional restrictions. 45 CFR 46, Subpart B - Exempt from IRB Same exemption conditions outlined in 45 CFR 46.104 FDA Review The FDA bases its approval decision upon bioresearch data generated and reported to the FDA by the sponsor to support the product's marketing approval. These data are collected by the sponsor during clinical research conducted under an IND application or an Investigational Device Exemption (IDE). Investigational New Drug (IND) Application Research involving a drug or biologic that has not yet reached the marketplace or that studies a new use of the marketed product requires an IND application per 21 CFR 312. IND Application Approval This determination is based upon: - Data from prior animal or human testing - Methods of manufacturing - Plans for testing and reporting significant toxicities - A well-developed clinical research plan that minimizes risks to the subjects Clinical investigation of a marketed drug does not require an IND if all of the following conditions are met: -Not for a new indication, new labeling, or significant change in advertising. -Does not involve change to the route of administration or dosage level, subject population usage, or other factors that significantly increases the drug product's risks of harm (or decreases the acceptability of the risks). - In compliance with IRB review in 21 CFR 56 and informed consent requirements in 21 CFR 50. - In compliance with requirements for promotion and sale at 21 CFR 312.7. Form FDA 1572 Agreement between the researcher and the sponsor assuring compliance with FDA regulations *Not used for devices Off Label" Use of Drugs, Devices, and Biologics Use of a marketed product in this manner, when the intent is the practice of medicine, does not require the submission of an IND per 21 CFR 312.2(d) or IDE per 21 CFR 812.2. Definition of a Medical Device Healthcare product that does not achieve its primary intended purpose by a chemical interaction or by being metabolized. Ex: laser, sutures, pacemakers, diagnostic aids (reagents + test kits for in vitro diagnosis) Medical Device Amendments of 1976 + Safe Medical Devices Act of 1990 Provide the regulatory framework for medical device development, testing, approval, and marketing. Premarket approval process If the device is not exempt, the FDA at 21 CFR 807.81(a)(1) determines whether the device is substantially equivalent to similar devices marketed before the 1976 amendment. These devices are often referred to as 510(k) devices and require a summary to be submitted to the FDA to determine substantial equivalence (21 CFR 807.92). If the new medical device is not substantially equivalent, the company may need to demonstrate safety and efficacy in a premarket approval application, which could include clinical trials. Investigational Device Exemption (IDE) The IDE regulations at 21 CFR 812 specify how to conduct these clinical trials. Classify as: 1. Significant risk (SR) 2. Non-significant risk (NSR) ^first by sponsor, then IRB needs to agree Risk is assessed by proposed use, not just the device. Significant Risk (SR) Devices 21 CFR 812.3 -implant -support/sustain life -substantial importance in diagnosing, curing, mitigating, tx, or prevents health impairment -Serious risk to health, safety, or welfare For use of a significant risk device in research, the sponsor must submit an IDE application to the FDA per 21 CFR 812.20 Non-Significant Risk (NSR) Devices It is considered to have an approved IDE application (that is, no application is filed with the FDA) Studied without FDA oversight as long as Sponsor: -monitors, record keeps, and proper labeling requirements IRB must agree it is NSR NSR device study does not require approval by the FDA and only must follow the abbreviated requirements at 21 CFR 812.2(b) Trial of an NSR device requires IRB approval, informed consent, and proper study monitoring and it must meet all other regulatory compliance requirements. EX: catheters, dental filings, pads/tampons, TENS (transcutaneous electric nerve stimulation) devices 21 CFR 50.25 Elements of informed consent, as required by the FDA Similar to U.S. Health and Human Services (HHS) regulation at 45 CFR 46.116. Key differences: -46.116(b)(5) "key information" be presented first., in a way a subject can understand -46.116(b)(9) requires additional statements about if identifiable private information or identifiable biospecimens will be used in future research FDA requires 2 statements 1. Subject's records may possibly be inspected by the FDA 2. Statement that the clinical trial will be listed in a registry. Per 21 CFR 50, the required language is, "A description of this clinical trial will be available on http://www.ClinicalTrials.gov...." 21 CFR 50.23 Exception from General Requirements - use of test article The IRB must be notified within a maximum of five days if a test article was used in an emergency situation for one individual. 21 CFR 50.24 Exception from Informed Consent Requirements for Emergency Research Unlike the exception noted in 21 CFR 50.23, the activities described in 21 CFR 50.24 are associated with an IRB-approved research study that involves research in emergencies. Requires -urgent intervention necessary with available tx unproven/unsatisfactory -subjects cannot consent b/c of condition -subject prospect of direct benefit -IP administered before consent can be obtained via pt or LAR -unreasonable to identify prospective individuals for eligibility in advance Waive / Alt Consent - No more than minimal risk Will not object if an IRB approves a waiver or alteration of consent for a no more than minimal risk clinical investigation if the IRB determines: 1. no more than minimal risk 2. The waiver / alteration will not adversely affect the rights and welfare of the subjects 3. research could not practicably be carried out without the waiver or alteration 4. Whenever appropriate, the subjects will be provided with additional pertinent information after participation. When FDA and HHS Regulations Differ FDA (2018) guidance says that the regulation that offers the greater protection to human subjects should be followed. For example, the revised Common Rule has a "key information" requirement for consent, and the FDA regulations do not. However, this key information requirement offers additional protections to subjects and it is not in conflict with any FDA regulations. However, research that is no longer subject to continuing review under the revised Common Rule would still require continuing review under FDA regulations pursuant to 21 CFR 56.109(f). Verbal Consent 21 CFR 56.109(c)(1), the FDA allows the IRB to waive the requirement for the subject (or the subject's LAR) to sign the consent if two conditions are met: 1. no more than minimal risk 2. no procedures requiring written documentation outside of participation in the study IRB may require the researcher to provide the subject with written materials about the research per 21 CFR 56.109. IND/IDE Requirements for Emergency Use (FDA/Sponsor) Options if patient does not fit trial needs or no active trial 1. Contact manufacturer and determine if the drug can be made available for an "emergency use" under the company's IND. 2. FDA per 21 CFR 312.36 may authorize the manufacturer to allow the drug to be used in advance of an IND submission 3. If the company agrees to provide the product, the physician can contact FDA, explain the situation, and obtain an emergency IND to permit the drug's shipment. 4. If there is no IDE, the physician may use the device and notify FDA of its use after the fact. The physician should obtain both an independent assessment from another physician and informed consent from the subject, before emergency use of the device occurs. IND/IDE Requirements for Emergency Use (IRB) In an emergency use situation, the FDA at 21 CFR 56.104(c) permits an exemption from prior review and approval by an IRB Devices - concurrence of the IRB chair is required before the use takes place. HHS regulations do not prohibit a researcher from using any investigational or approved drug or device in an emergency situation for the subject's clinical care, but they do not consider information collected to be research data. FDA does consider this to be a research use and wants the data reported to them. IRB review and approval is required in all circumstances if the researcher wishes to use the data for research purposes. Subsequent use of the investigational product at the organization should have prospective IRB review and approval. If the IRB was not notified before the investigational drug or device was used in an emergency situation, the IRB should be notified per organizational policy or within five working days (21 CFR 50). The FDA and sponsor should be notified as necessary. Inspections and Audits FDA's Bioresearch Monitoring Program conducts "not for cause" and "for cause" inspections of IRBs, clinical researchers, and sponsors. 21 CFR 11 - Electronic Records; Electronic Signatures 1. Computer system must ensure accuracy, reliability, and consistent performance. -SOPS, audits, testing, training required 2. Computer systems must use and maintain secure, computer-generated, time-stamped audit trails independently recording date+time of entries/actions that create, modify, or delete e-records. 3. Computer systems must use system checks to ensure only those authorized are accessing the system, altering records, and performing actions. 4. Procedures established to ensure records are retained for duration of time, proper format, and meet FDA requirements. *does not apply to paper printouts or paper records HIPAA protections Protected health information (PHI) created in or by covered entities HIPAA covered entities healthcare providers, healthcare provider organizations, health plans, and health information clearinghouses that engage in electronic healthcare transactions Privacy Notice The privacy notice must include the ways in which data subjects may register complaints and report problems, either locally or with federal authorities. HIPAA allows for research-related access to individuals' identifiable health data without authorization under certain circumstances: - Minimal Risk - Research solely for activities preparatory to research (i.e protocol development, potential subject & not leave the covered entity) - Deceased individual's information is used - "Grandfathered" where legal permissions were in place prior to effect of HIPPA Data that do not identify individuals can be used for research without specific authorization if: 1. Only fully de-identified data are used. 2. A "limited data set" is used, under an approved "data use agreement." HIPAA - ICF waiver/alterations Only if research is no more than minimal risk and includes privacy protections: 1. Plan to protect data identifiers from improper use/disclosure 2. Plan to destroy data identifiers at earliest opportunity dependent on research 3. Assurances that PHI will not be reused/disclosed to anyone else except as required by law for oversight or research as permitted by HIPPA 4. Could not be conducted without access and use of PHI 5. Could not be conducted without waiver / alteration of authorization Permitted access under HIPAA without consent - process Researcher must make a written or oral representation to the covered entity's designated officials that such access is necessary for the research purposes -- someone from the IRB, the Privacy Board, or a privacy officer / designee -- who would then determine the appropriateness of the request. De-identified Data No longer PHI and likely not human research if direct/indirect identifiers were removed. Limited data set (LDS) Disclosure Requires data user agreement to obtain the LDA with all direct identifiers removed Agreement must: -explain permitted uses/disclosure by the recipient consistent with the research - limit individuals who can receive the data - require recipient to agree not to re-identify the data or contact subjects Disclosure Accounting Not required for: -internal sharing / use -disclosures as described in authorization -to the subjects -LDS subject to data user agreement -de-identified data =/= PHI While HIPAA may not require it, many organizations will require that researchers maintain logs of all disclosures from research data collections as a security measure, including transfers to other individuals within the covered entity. Electronic data storage will increasingly offer this capability cheaply and automatically; older collections will require manual logging. HIPAA Authorizations - plain language - signed by subject/ LAR - specify PHI used/disclosed, to who, and for how long (end of study etc) Can be included in ICF, cannot be with privacy notice Conflicts of Interest in Human Subjects Research COIs may arise in human subjects research when researchers and/or organizations have financial or personal relationships that may compromise or appear to compromise the integrity of the research, protection of human subjects, and/or reputation of the researchers or organizations. 42 CFR 50, Subpart F 1995 PHS became the first division of the federal government to implement regulations requiring disclosure and management of individual research-related COIs Goal is to promote objectivity in research by ensuring that PHS-funded research is free from bias due to researcher COIs. Jesse Gelsinger, died as a result of the experimental therapy he received in the study - COI Both the researcher responsible for the study's oversight and the university where the research was conducted had significant financial ties to the company sponsoring the research, as well as an intellectual property interest in the therapy being evaluated in the study Association of American Medical Colleges (AAMC 2002) issued a report recommending that academic organizations develop policies to identify and manage institutional conflicts related to human subjects research. The potential bias that COIs may impart can affect multiple research activities including: - enrollment and inclusion/exclusion criteria - personnel hired to conduct the study - Recruitment and consenting - Vendor selection to buy equipment and other supplies - Data collection, analysis, and interpretation - Sharing of research results - Choice of research design and statistical methods COI Types Individual v Institutional + Financial v Non-Financial Conflict of conscience when a person has personal convictions that may jeopardize their objectivity in an area of science 42 CFR 50 (Policies of General Applicability 2011) PHS-funded research, each "investigator" named on a PHS proposal must disclose "significant financial interests" to a designated official at the applicant organization. Significant financial interest (SFI) - publicly of non-publicly traded entity in the 12 months preceding the disclosure and the value of any equity interest in the entity, which when aggregated, exceeds $5,000 - Intellectual property rights and interests upon receipt of income related to such rights and interests (royalties that flow through the applicant organization are carved out and do not have to be disclosed) - Reimbursed or sponsored travel (travel reimbursed or sponsored by a federal, state, or local government is carved out and does not have to be disclosed) financial conflict of interest (FCOI) an SFI that could "directly and significantly affect the design, conduct or reporting of PHS-funded research." If the SFI is determined to be a FCOI, then the organization must develop a management plan (if possible) and submit a FCOI report to the awarding agency FDA Regulation Governing Disclosure of COIs 1999, requires applicants submitting marketing applications for drugs, biologics, or devices to certify the absence of certain financial interests or to disclose financial interests of researchers who conducted clinical studies covered by the regulation at 21 CFR 54.4(a) Management of COIs Critical to ensuring research integrity, the public's trust in the organization, and the protection of human subjects' rights, safety, and welfare. Aimed at reducing the opportunity to bias the research May include COI committees and management plans, informed consent form disclosure language, as well as additional management controls (such as divesture and independent data review). Divestiture Strategy If an individual researcher had a significant conflict that was deemed unmanageable by other means, divesting (or selling) interests might be advised as a means of eliminating the source of the conflict. ICOI Management For example, many ICOI management plans require use of an external IRB when the organization has an equity interest in an entity related to human subjects research. 45 CFR 46 B - x C - y D - z 45 CFR 46 B - Pregnant Women C - Prisoners D - Children According to the authors, there are four common abuses that historically are described as giving rise to vulnerability. Which response below contains the correct four? There are four common abuses that historically are described as giving rise to vulnerability 1) physical control, 2) coercion, 3) undue influence, and 4) manipulation. These exist along a continuum of severity with physical control being the most severe and undue influence and manipulation being the least (Nelson and Merz 2002, V69-80). The other abuses- prejudice, neglect, and disrespect - should still be avoided in research. Which of the following was the result of the Beecher article? A. Realization that ethical abuses are not limited to the Nazi regime B. An identification of basic ethical principles C. Multiple Congressional hearings D. Additional FDA regulations Answer: A. Realization that ethical abuses are not limited to the Nazi regime When required, the information provided to the data subject in a HIPAA disclosure accounting ... must be more detailed for disclosures that involve fewer than 50 subject records. Where fewer than 50 subjects' records are involved, the listing must be more specific and detailed, commensurate with the requirements for other kinds of PHI disclosure accounting, including: specific date(s) of disclosures; names of entities to which PHI was disclosed; description of the PHI involved in the disclosure; and purpose of the disclosure. The FDA regulations governing disclosure of individual COIs require: Applicants submitting marketing applications to disclose financial COIs of researchers who conducted clinical studies The FDA's regulation governing disclosure of individual COIs requires applicants submitting marketing applications for drugs, biologics, or devices to certify the absence of certain financial interests or to disclose financial interests of researchers who conducted clinical studies covered by the regulation. The regulation specifies that the FDA may refuse to file any marketing application that does not contain a disclosure of researchers' financial interests or a certification that the applicant acted with due diligence to obtain researchers' disclosures, but was unable to do so. FDA Form 482 Notice of inspection FDA Form 483 Inspectional Observations FDA Form 1572 Statement of the Investigator FDA Form 3454 Certification - Financial Interests and Arrangements of Clinical Investigators FDA Form 3455 Disclosure - Financial Interests and Arrangements of Clinical Investigators FDA Form 3500 For Voluntary Reporting of Adverse Events and Product Problems FDA Form 3500A For Use by User-Facilities, Distributors, and Manufacturers for Mandatory Reporting ICH - E6 parts 1) glossary; 2) principles; 3) IRBs/IECs; 4) investigator; 5) sponsor; 6) protocol and amendments; 7) investigator's brochure; and 8) essential documents. Important Differences between ICH & FDA guidelines 1. IRB Regulations - ICH requires Investigator to Obtain IRB Assurance that the IRB is in Compliance with ICH 2. Medical Records - ICH E6 allows broader access to research records and to otherwise confidential medical records than is required by FDA regulations. 3. Investigator Responsibilities - US FDA requires 1572 - ICH requires qualified physician investigator / sub-investigator for medical decisions - Source data should be attributable, legible, contemporaneous, original, accurate, and complete. Changes to source data should be traceable, should not obscure the original entry, and should be explained if necessary. 4. Sponsor Responsibilities - quality management system with risk-based approach & which can be safely omitted - sponsor delegate responsibilities in writing to CROs, but must maintain oversight. FDA only requires sweeping statement of responsibility transfer. - sponsor (w/ SOP maintenance for these systems) must ensure electronic trial data systems match requirements for completeness, accuracy, reliability, and validated. (more specific than FDA, which states responsible for data handling + record keeping). - Noncompliance action required (protocol, SOP, GCP, regulatory) with root cause analysis + corrective action implementation. If continuous &/or serious to end investigator/institutions participation. 5. Sponsor Monitoring ICH E6 has more detailed sponsor monitoring requirements. -Risk Based, on site or on site + central or central only if justified. - written monitoring reports - monitoring plan tailor specific human subject population + data integrity risks. 6. Sponsor Record Retention -at least 2 years post approval marketing application and no pending / contemplated marketing applications - OR at least 2 years since formal discontinuation of clinical development - longer as required 6. ICF Signatures - subject/LAR + person on study team performing ICF discussion. - FDA only subject signature + date. 7. Subject Receipt of ICF - ICH states subject receives signed+dated copy of ICF - should state the subject will receive this in ICF to be compliant. -FDA allows signed or unsigned 8. Assent - Children or Cognitive Impairment Adults - ICH requires subject to be informed of research to extent they're capable to assent, sign and date ICF. - HHS & FDA state children assent unless appropriate not to. Incapacitated adults not specifically required to assent. 9. Impartial Witness - Illiterate Subjects - Witness to attest of explanation and understanding of subject/LAR, to sign + date in addition to subject/LAR. - FDA does not mandate witness, only to document ICF by reading it to the subject or short form consent + written summary for oral presentation. 10. Emergency Situation - ICH mandate approved protocol and LAR consent if possible. If not both should be informed, then consent obtained to contain as appropriate. Procedures per protocol. - FDA allows exception for consent w/ notice of IRB within 5 business days 11. Elements of Consent - Explain alt tx options, benefits, risks - many chose not to be compliant with this. - Probability being assigned to each study arm (not req by FDA) - Include subject responsibilities - Payment info - prorated as well. FDA info sheet includes guidance and is common practice. 12. Non-therapeutic Trials (not addressed specifically in FDA) - No direct benefit to subject, should be done on subjects who personally can give consent. - LAR if +cannot be down by other means +low risk +negative impact minimized + low +not prohibited by law +IRB approval Trial subjects should have disease/condition that the trial is investigating. 13. Primary Physician Notification - ICH states recommends notifying the PCP about subject's participation in the trial. 14. IRB Responsibilities - ICH states IRB should review: protocol/amendments, ICF, pt facing material, IB, safety, payments, CV for investigator, etc. - ICF & FDA - retain docs 3+ years after completion of trial -Review changes & deviations (FDA does not state to review deviations) - ICH does not state IRBs can waiver/alteration of consent for no more than minimal risk studies. IND Contents - Cover letter - Form FDA 1571 (Investigational New Drug Application [IND]) - Form FDA 1572 (Statement of Investigator) - Introductory statement and general investigational plan - Investigator's Brochure (or copy of the approved labeling (including the package insert) can be provided in lieu of the Investigator's Brochure (IB). if for approved drug seeking ZYX) - Protocol(s) - Chemistry, manufacturing, and controls information - Pharmacology and toxicology information - Previous human experience with drug - Additional information - Relevant information Letters of Cross-Reference Might already have an active IND for the drug being studied by a sponsor-investigator. In these instances, the manufacturer may agree to provide a letter of cross-reference that enables the sponsor-investigator to reference the following technical information from the manufacturer's IND in the sponsor-investigator IND: - Chemistry, manufacturing, and controls (CMC) information - Pharmacology and toxicology information - Previous human experience with the drug Form FDA 1571 Contractual agreement between the sponsor and FDA. Agrees to: - Not to begin clinical investigations until thirty (30) days after FDA's receipt of the IND, unless the investigator receives earlier notification from the FDA - Not to begin or continue investigations covered by the IND if those studies are placed on clinical hold - That an IRB/IEC that complies with 21 CFR 56 will be responsible for initial and continuing review and approval of each of the studies in the proposed clinical investigations - To conduct the investigation in accordance with all other applicable regulatory requirements Required Reports on active IND - Protocol Amendments - Informational Amendments (new toxicology etc) - AE & IND Safety where: + investigators immediately report any SAEs. + Sponsor-investigators must notify authorities & participating investigators in writing on unexpected & serious AE ASAP and no later than 15 calendar days. + AE unexpected, fatal, or life threatening no later than 7 calendar days -Annual reports (IND Reports) within 60 days of anniversary date that IND went into effect -Final report shortly after trial, and accurate financial information IDE Content An IDE submission includes: - Cover letter to the FDA - Cross-reference letter from device supplier* - Table of contents - Report of prior investigations* - Investigational plan - Manufacturing information* - Investigator information** - IRB information - Sales information - Device labeling - Informed consent materials - Any other relevant information that FDA requests for review of the IDE application - Information previously submitted to FDA in accordance with 21 CFR 812 may be incorporated by reference *If the device being studied is an approved device, the sponsor-investigator can cross-reference a PMA for the technical sections (manufacturing information and report of prior investigations). A letter of authorization is obtained from the device manufacturer to allow this cross-reference. ** Names and addresses of investigators that have signed an Investigator Agreement at the time of the original submission should be included + Not required for NSR devices. +When determining SR / NSR - FDA determination is final if sponsor/IRB differ. Required Reports on active IDE - Current Investigator List at 6-mo intervals - Unanticipated Adverse Device Effects (UADEs) within 10 working days of sponsor notice - Annual progress reports starting 1 year after approval - Final report within 6 months of trial completion - As applicable - withdrawal of IRB approval, recalls/dispositions, devise use without consent Financial Disclosures collected for all drugs/devices submitted to FDA. Forms not submitted until NDA is filed for marketing. Premature Termination / Suspension of Trial ICH E6 notes that if the clinical trial is prematurely terminated or suspended, regardless of reason, that the investigator or the institution should promptly notify subjects in the study. [Show More]
Last updated: 2 years ago
Preview 1 out of 68 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)

CCRP AACVPR TESTS COMPILATION PACKAGE DEAL (100% Correct Solutions)
CCRP AACVPR TESTS COMPILATION PACKAGE DEAL (100% Correct Solutions)
By Prof. Goodluck 2 years ago
$20.5
13
Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 05, 2023
Number of pages
68
Written in
All
Additional information
This document has been written for:
Uploaded
Oct 05, 2023
Downloads
0
Views
262




 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)