*NURSING > STUDY GUIDE > NSG 6420: FNP I Adult/Gero Final Review Study Guide (All)
NSG 6420: FNP I Adult/Gero Final Review Study Guide
Document Content and Description Below
NSG 6420: FNP I Adult/Gero Final Review Study Guide 1. General Concepts in Geriatrics Impact of physiological changes with aging: Kennedy Chapter 1. The major impact of all of these physiolo... gical changes can be highlighted with three primary points. First, there is a reduced physiological reserve of most body systems, particularly cardiac, respiratory, and renal. Second, there are reduced homeostatic mechanisms that fail to adjust regulatory systems such as temperature control and fluid and electrolyte balance. Third, there is impaired immunological function: infection risk is greater, and autoimmune diseases are more prevalent. Reduced renal function, particularly the glomerular filtration rate (GFR), affects the clearance of many drugs, and creatinine clearance provides an index of renal function for use in choosing doses of renally eliminated or nephrotoxic drugs (such as digoxin, H2 blockers, lithium, and water-soluble antibiotics). Normal age related changes: Changes in kidney function begin in the fourth decade of life and continue to decline with each subsequent decade. by age 70, an individual might reasonably have a 40% to 50% decrease in renal function, even in the absence of disease. With advancing age, the ability of the liver to metabolize drugs does not decline. Although liver size and blood flow do decline with age, routine liver function test results are typically normal when no disease exists. Decreased liver size and blood flow can result in decreased first-pass metabolism. Older adults often experience more sedation from central nervous system drugs than younger persons at the same concentration. Signs and symptoms of depression: Altered presentation is another common feature in older adults. The patient with depression may not present with a dysphoric mood but rather agitation and psychotic features. Questions The major impact of the physiological changes that occur with aging is: Reduced physiological reserve Reduced homeostatic mechanisms Impaired immunological response All of the above All of the following statements are true about laboratory values in older adults except Reference ranges are preferable Abnormal findings are often due to physiological aging Normal ranges may not be applicable for older adults Reference values are not necessarily acceptable values Mini Mental Status: Buttaro Chapter 13 Geriatric specialists have multiple assessment tools, such as the Folstein Mini-Mental State Examination, the Mini-Cog screen for dementia, the Short Portable Mental Status Questionnaire, the AD8 Dementia Screening Interview, and the Montreal Cognitive Assessment (MoCa), to differentiate short-term memory loss from dementia and to observe the progression of cognitive impairment. Questions When prescribing medications to an 80-year-old patient, the provider will a. begin with higher doses and decrease according to the patient’s response. b. consult the Beers list to help identify potentially problematic drugs. c. ensure that the patient does not take more than five concurrent medications. d. review all patient medications at the annual health maintenance visit. The Beers list provides a list of potentially inappropriate medications in all patients age 65 and older and helps minimize drug-related problems in this age group. Older patients should be started on lower doses with gradual increase of doses depending on response and side effects. Patients who take five or more drugs are at increased risk for problems of polypharmacy, but many will need to take more than five drugs; providers must monitor their response more closely. Medications should be reviewed at all visits, not just annually. REF: Polypharmacy/Consequences of Polypharmacy/Management An 80-year-old woman who lives alone is noted to have a recent weight loss of 5 pounds. She appears somewhat confused, according to her daughter, who is concerned that she is developing dementia. The provider learns that the woman still drives, volunteers at the local hospital, and attends a book club with several friends once a month. What is the initial step in evaluating this patient? a. Obtain a CBC, serum electrolytes, BUN, and glucose b. Ordering a CBC, serum ferritin, and TIBC c. Referring the patient to a dietician for nutritional evaluation d. Referring the patient to a neurologist for evaluation for AD Patients with weight loss, confusion, and lethargy are often dehydrated and this should be evaluated by looking at Hgb and Hct, electrolytes, and BUN. This patient is currently leading an active life, so the likelihood that recent symptoms are related to AD, although this may be evaluated if dehydration is ruled out. Anemia would be a consideration when dehydration is ruled out. Referrals are not necessary unless initial evaluations suggest that malnutrition or AD is present. REF: Dehydration/Pathophysiology/Clinical Presentation/Physical Examination The practitioner is establishing a plan for routine health maintenance for a new female client who is 80 years old. The client has never smoked and has been in good health. What will the practitioner include in routine care for this patient? Select all that apply. a. Annual hypertension screening b. Baseline abdominal aorta ultrasound c. Colonoscopy every 10 years d. One-time hepatitis B vaccine e. Pneumovax vaccine if not previously given f. Yearly influenza vaccine For older clients a one-time pneumovax is given after age 65. Influenza vaccine should be given every year. Hypertension screening should be performed at each office visit, not just annually. An abdominal aorta US is performed once for every smoking male. Colonoscopy is performed every 10 years after age 50, but not after age 74. REF: Table 13-1: Recommended Screening and Immunizations 2. HEENT Pharyngitis Buttaro Chapter 101 In noninfectious pharyngitis the patient reports a sore throat and dryness; if environmental allergens are the cause, symptoms often include rhinorrhea, watery eyes, and postnasal drip. Viral causes are more common (rhinorivus) In viral pharyngitis, findings include fever, cough, nasal symptoms, and mild erythema with little or no pharyngeal exudate. Treatment of viral pharyngitis includes rest, fluids, humidification, voice rest, and warm saline gargles to ease discomfort. 7 Acetaminophen or ibuprofen should be used for fever and general discomfort. Bacterial pharyngitis is more common in children younger than 15. Streptococcus pyogenes is the etiologic agent for acute pharyngitis. Group A β-hemolytic Streptococcus (GAS) is the most important to identify because it is responsible for acute rheumatic fever (ARF) and poststreptococcal glomerulonephritis. Patients may report a sudden onset of sore throat, painful swallowing, fever (temperature higher than 38.5° C [101.3° F]), chills, headache, nausea, vomiting, and abdominal pain. With bacterial pharyngitis, rhinitis, cough, conjunctivitis, and myalgias are not typically present. Diagnostic studies used to detect GAS infection include a throat culture, a rapid antigen detection test (RADT). Penicillin V, 500 mg 2-3 times daily for 10 days) is indicated in GAS pharyngitis primarily to prevent complications, such as suppurative tonsillitis, glomerulonephritis, and rheumatic fever. Clarithromycin, 250 mg twice daily for 10 days, is indicated for patients with penicillin allergy. questions A patient has sore throat, a temperature of 38.5° C, tonsillar exudates, and cervical lymphadenopathy. What will the provider do next to manage this patient’s symptoms? a. Order an antistreptolysin O titer b. Perform a rapid antigen detection test c. Prescribe empiric penicillin d. Refer to an otolaryngologist The RADT is performed initially to determine whether GAS is present. The ASO titer is not used during initial diagnostic screening. Penicillin should not be given empirically. A referral to a specialist is not required for GAS infection. A patient reports a sudden onset of sore throat, fever, malaise, and cough. The provider notes mild erythema of the pharynx and clear rhinorrhea without cervical lymphadenopathy. What is the most likely cause of these symptoms? a. Allergic pharyngitis b. Group A streptococcus c. Infectious mononucleosis d. Viral pharyngitis Viral pharyngitis will cause sore throat, fever, and malaise and is often accompanied by URI symptoms of cough and runny nose. Allergic pharyngitis usually also causes dryness. GAS causes high fever, cervical adenopathy, and marked erythema with exudate. Infectious mononucleosis will cause an exudate along with cervical adenopathy A school-age child has had 5 episodes of tonsillitis in the past year and 2 episodes the previous year. The child’s parent asks the provider if the child needs a tonsillectomy. What will the provider tell this parent? a. Current recommendations do not support tonsillectomy for this child. b. If there is one more episode in the next 6 months, a tonsillectomy is necessary. c. The child should have radiographic studies to evaluate the need for tonsillectomy. d. Tonsillectomy is recommended based on this child’s history. Recommendations suggest 6 to 7 documented episodes of GAS within 1 year, 5/year for 2 consecutive years, or 3/year for 3 years. Radiographic studies are not indicated Mononucleosis (Buttaro Chapter 233) EBV-IM (Epstein-Bar Virus infectious mononucleosis) occurs most often in adolescents and young adults, with the highest incident at ages 15 to 19. Transmission of EBV-IM occurs through exposure to oropharyngeal secretions. The classic triad of symptoms of acute IM includes fever, pharyngitis, and lymphadenopathy. The typical adolescent with EBV-IM is seen with sore throat, fever, and lymph node and tonsillar enlargement. Additional common presenting symptoms include pharyngeal inflammation and transient palatal petechiae. Reports indicate that splenic enlargement occurs in 40% to 100% of cases and can be confirmed with ultrasound. An abdominal examination identifies splenomegaly and hepatomegaly. Rash and jaundice should be noted because they are associated with EBV-IM. he most useful laboratory test is the serologic test for heterophil antibodies. Treatment of uncomplicated EBV-IM is primarily supportive, including adequate hydration, nonsteroidal anti-inflammatory drugs or acetaminophen for fever reduction and myalgias. Individuals with splenomegaly should be encouraged to refrain from strenuous physical activity for 3 to 4 weeks to avoid the risk of splenic rupture Questions A patient with EBV-IM also has group A beta-hemolytic streptococcal pharyngitis and is being treated with amoxicillin. On the third day of treatment, the patient develops a rash. A urinalysis is normal. What does this indicate? a. A reaction to the amoxicillin b. A streptococcal rash c. Hematologic complications d. Hemolytic-uremic syndrome 80% to 100% of patients with IM who are taking amoxicillin will develop a rash. A streptococcal rash appears at the onset of symptoms, not 3 days after initiation of antibiotics. This rash does not indicate hematologic complications or hemolytic-uremic syndrome. An adolescent patient who plays football in high school is diagnosed with EBV infectious mononucleosis and is noted to have splenomegaly. What will the provider recommend to this patient about returning to sports? a. Abdominal ultrasounds are recommended to determine safety. b. Corticosteroid therapy may help shorten the course of the disease. c. He may return to minimal contact practice in 2 to 3 weeks. d. It will be safe to play football in 3 to 4 weeks. Patients with splenomegaly should be encouraged to refrain from strenuous activity for 3 to 4 weeks to avoid the risk of splenic rupture. Serial US studies beginning at week 2 to 3 may be helpful in determining the risk of rupture. Corticosteroids have not been shown to reduce the severity or duration of symptoms. Strenuous activity is not recommended until 3 to 4 weeks; without an US, it is not possible to ensure absolute safety for sports. An adolescent patient has fever, pharyngitis, and cervical lymphadenopathy and has a negative group A beta-hemolytic throat culture. A complete blood count shows absolute lymphocytosis, but a heterophil antibody test is negative for Epstein-Barr virus (EBV). What will the provider tell the patient about the likelihood of infectious mononucleosis (IM)? a. It will be necessary to repeat the heterophil antibody test in a few weeks. b. Liver function tests will help to confirm a diagnosis of EBV-IM. c. The likelihood of EBV infectious mononucleosis is still high. d. This IM is most likely caused by a virus other than Epstein-Barr virus. Because heterophil antibodies may not reach detectable levels early in the disease, it is possible to have a negative result. This patient has symptoms and the suspicion for disease remains high. Repeat testing in 7 to 10 days will help confirm the diagnosis. A positive heterophil antibody test with absolute lymphocytosis is diagnostic of acute IM. Epstein-Barr nuclear antigen is measured 6 to 8 weeks after onset of symptoms to distinguish between acute and previous infection. LFTs may be elevated in patients with IM, but this is not diagnostic. Symptoms associated with allergies (buttaro chapter 73) allergic conjunctivitis, a condition seen most frequently in the spring and summer. Unlike conjunctivitis from infectious causes, allergic conjunctivitis typically occurs simultaneously in both eyes. Its predominant feature is itching. If discharge is present, it will be clear or stringy and white. The conjunctiva has a boggy appearance. Because allergic conjunctivitis is typically associated with systemic allergies, an oral antihistamine can be helpful in controlling ocular symptoms. Agents to consider include fexofenadine and loratadine. Conjunctivitis Bacterial conjunctivitis is typically accompanied by thick, purulent discharge. Patients will report that both eyes are sticky or glued shut. Gonococcal conjunctivitis is typically seen in sexually active adults but can also occur in neonates via maternal-neonate transmission. trimethoprim–polymyxin B or fluoroquinolone drops, four times a day for 1 week. The following types of bacterial conjunctivitis require systemic treatment: • H. influenzae: treat with oral amoxicillin-clavulanate • Gonococcal: ceftriaxone, 1 g intramuscularly, one dose or ciprofloxacin, 500 mg orally if the patient has a penicillin allergy and one dose of azithromycin, 1g orally—requires same-day referral to an ophthalmologist. • Chlamydial: azithromycin, 1 g orally, one dose or doxycycline, 100 mg twice daily for 7 days Viral conjunctivitis is self-limited and typically lasts 5 to 14 days. A recent upper respiratory infection or exposure to sick individuals can point to a diagnosis of adenoviral conjunctivitis. Treatment is supportive with artificial tears and cool compresses. In addition, topical corticosteroids should be avoided because they can prolong viral shedding and increase infectivity. Adenoviral conjunctivitis can occur in three different forms. Adenoviral conjunctivitis pharyngoconjunctival fever: systemic symptoms Epidemic keratoconjunctivitis: bilateral conjunctival hyperemia and chemosis, petechial and larger subconjunctival hemorrhages. have corneal involvement, and it is appropriate to refer these patients to an ophthalmologist. questions A patient who has a cold develops conjunctivitis. The provider notes erythema of one eye with profuse, watery discharge and enlarged anterior cervical lymph nodes, along with a fever. Which treatment is indicated? a. Antihistamine-vasoconstrictor drops b. Artificial tears and cool compresses c. Topical antibiotic eye drops d. Topical corticosteroid drops Viral conjunctivitis accompanies URI and is generally self-limited, lasting 5 to 14 days. Symptomatic treatment is recommended. Antihistamine-vasoconstrictor drops are used for allergic conjunctivitis. Topical antibiotic drops are sometimes used for bacterial conjunctivitis. Topical corticosteroid drops are used for severe inflammation. A patient reports bilateral reports burning and itching eyes for several days. The provider notes a boggy appearance to the conjunctivae, along with clear, watery discharge. The patient’s eyelids are thickened and discolored. There are no other symptoms. Which type of conjunctivitis is most likely? a. Allergic b. Bacterial c. Chemical d. Viral Allergic conjunctivitis generally presents simultaneously in both eyes with itching as a predominant feature. Discharge is generally clear or stringy and white and the patient will have lid discoloration, thickening, and erythema. Bacterial conjunctivitis is characterized by acute inflammation of the conjunctivae along with purulent discharge. Chemical conjunctivitis will not have purulent discharge. Viral conjunctivitis is usually in association with a URI. A patient with allergic conjunctivitis who has been using a topical antihistamine-vasoconstrictor medication reports worsening symptoms. What is the provider’s next step in managing this patient’s symptoms? a. Consider prescribing a topical mast cell stabilizer b. Determine the duration of treatment with this medication c. Prescribe a non-sedating oral antihistamine d. Refer the patient to an ophthalmologist for further care Antibiotic-vasoconstrictor agents can have a rebound effect with worsening symptoms if used longer than 3 to 7 days, so the provider should determine whether this is the cause. Topical mast cell stabilizers are useful as prophylaxis for recurrent or persistent allergic conjunctivitis and results do not occur for several weeks. Oral antihistamines may be the next step if it is determined that the cause of worsening symptoms is related to the allergy. It is not necessary to refer to ophthalmology at this time. REF: Management Corneal abrasion (Buttaro chapter 74) The most common symptom of a corneal abrasion or foreign body is sudden onset of severe eye pain in the affected eye. This pain typically resolves after application of a topical anesthetic eye drop. Other symptoms include blurred vision, redness, tearing, light sensitivity, eyelid swelling, and blepharospasm. Use of topical fluorescein dye can assist in the diagnosis. One drop of fluorescein can be applied and viewed under a cobalt blue light or Wood lamp. A corneal abrasion should appear as a bright green area. Topical anesthetics such as proparacaine should never be used or prescribed for pain control; their prolonged use may lead to corneal melting. A healthy corneal epithelium will repopulate rapidly, from just a few hours for a small, uncomplicated defect to 3 to 5 days with larger defects. Questions A patient who works in a furniture manufacturing shop reports a sudden onset of severe eye pain while sanding a piece of wood and now has copious tearing, redness, and light sensitivity in the affected eye. On examination, the conjunctiva appears injected, but no foreign body is visualized. What is the practitioner’s next step? a. Administration of antibiotic eye drops b. Application of topical fluorescein dye c. Instillation of cyclopegic eye drops d. Irrigation of the eye with normal saline The practitioner must determine if there is a corneal abrasion and will instill fluorescein dye in order to examine the cornea under a Wood’s lamp. Antibiotic eye drops are not indicated as initial treatment. Cyclopegic drops are used occasionally for pain control, but should be used with caution. Irrigation of the eye is indicated for chemical burns. Glaucoma (Kennedy Chapter 7) Acute glaucoma, also known as angle-closure or narrow-angle glaucoma, is an obstruction to the outflow of aqueous humor from the posterior to the anterior chamber. The predominant age range is 60 to 70 years old. The history reveals severe, unilateral eye pain, blurred vision, lacrimation, reports of seeing colored halos around lights, and a red eye. Headache, nausea, and vomiting frequently accompany eye pain, causing eye pain to be overlooked. Immediately refer patients for a complete ophthalmic examination. permanent visual loss occurs within 2 to 5 days if this condition is untreated. Surgical treatment includes peripheral iridectomy or laser iridotomy Chronic Glaucoma: initially; tunnel vision, night blindness, halos around lights. gradual visual field loss, chronic glaucoma is called the silent blinder. Medical treatment with eye drops is usually first-line therapy Prostaglandin analogs are the most effective drugs at lowering IOP and can be considered as initial medical therapy. Ttimolol is frequently prescribed for glaucoma and can exacerbate bradycardia and asthma in susceptible patients. Questions During an eye examination, the provider notes a red light reflex in one eye but not the other. What is the significance of this finding? a. Normal physiologic variant b. Ocular disease requiring referral c. Potential infection in the “red” eye d. Potential vision loss in one eye The red reflex should be elicited in normal eyes. Any asymmetry or opacity suggests ocular disease, potentially retinoblastoma, and should be evaluated immediately Sinusitis (Buttaro Chapter 92) The most common cause of acute sinusitis is a bacterial infection caused by Streptococcus pneumoniae. The presenting signs and symptoms include nasal congestion, purulent nasal discharge, and a headache that becomes more intense when the patient bends forward. Fever, fatigue, and other constitutional symptoms are common. The onset is abrupt, with infection in one or more paranasal sinuses. There is an association between sinusitis and asthma. Chronic sinusitis occurs with episodes of prolonged sinus infection (more than 12 weeks). Nasal congestion, discharge, and a cough that lasts for more than 30 days are common. Severe pain and headache are not usually present in chronic sinusitis CT scanning without contrast enhancement may be indicated for patient with recalcitrant symptoms that have not responded to two or more courses of antibiotic therapy. Questions A patient is concerned about frequent nasal stuffiness and congestion that begins shortly after getting out of bed in the morning. The patient denies itching and sneezing. A physical examination reveals erythematous nasal mucosa with scant watery discharge. What treatment will the provider recommend for this patient? a. Consultation for immunotherapy b. Daily intranasal steroids c. Oral antihistamines each morning d. Oral decongestants as needed Intranasal steroids should be considered for symptomatic relief for patients with sinusitis, especially those with allergic rhinitis. Oral mucolytics have little support in efficacy. Saline solution rinses may provide some relief, but there is no evidence to support their usefulness. Topical decongestants do decrease nasal congestion and edema, but the potential harm of rebound congestion requires recommendation with caution. Which are potential complications of chronic or recurrent sinusitis? Select all that apply. a. Allergic rhinitis b. Asthma c. Meningitis d. Orbital infection e. Osteomyelitis Complications of chronic or recurrent sinusitis include spread of infection to other tissues and may cause meningitis, orbital cellulitis, and osteomyelitis. Allergic rhinitis and asthma are associated with chronic sinusitis, but not complications of this condition. A patient has nasal congestion, fever, purulent nasal discharge, headache, and facial pain and begins treatment with amoxicillin-clavulanate. At a follow-up visit 10 days after initiation of treatment, the patient continues to have purulent discharge, congestion, and facial pain without fever. What is the next course of action for this patient? a. A CT scan of the paranasal sinuses b. A referral to an otolaryngologist c. A second course of amoxicillin-clavulanate d. A trial of azithromycin This patient may have subacute sinusitis and may benefit from a second course of the antibiotic. The lack of fever shows improvement, so this antibiotic may be used. CT scan is usually not performed in adults unless other complications are present or suspected. Referral to an otolaryngologist is necessary if no improvement after the second course of antibiotics. Azithromycin is not used in adults unless pregnant, due to resistance patterns. REF: Clinical Presentation/Diagnostics/Management Acute otitis media in adults (Buttaro chapter 86) Otitis media, characterized by fluid in the middle ear. most often associated with upper respiratory tract infections or allergies. The most common bacterial causative agents are Streptococcus pneumoniae and Haemophilus influenzae. otoscopic examination is key to accurate diagnosis of otitis. Cerumen removal may be necessary to obtain a clear view of the TM. AOM usually is characterized by a throbbing, painful earache with impaired hearing. In OME, fluid is present in the middle ear without signs or symptoms of acute infection. The TM often is dull gray, although it may appear injected. Amoxicillin is the recommended first-line antibiotic for children who are not allergic and have not received it in the last 30 days Questions Which symptoms in children are evaluated using a parent-reported scoring system to determine the severity of pain in children with otitis media? Select all that apply. a. Appetite b. Difficulty sleeping c. Level of cooperation d. Poor hearing e. Tugging on ears Decreased appetite, difficulty sleeping, and tugging on ears are part of the Acute Otitis Media Severity of Symptom Scale used to evaluate pediatric pain. Children may refuse to cooperate for reasons other than pain. Poor hearing is not part of the pain assessment. Which patient may be given symptomatic treatment with 24 hours follow-up assessment without initial antibiotic therapy? a. A 36 month old with fever of 38.5° C, mild otalgia, and red, non-bulging TM b. A 4 year old, afebrile child with bilateral otorrhea c. A 5 year old with fever of 38.0° C, severe otalgia, and red, bulging TM d. A 6 month old with fever of 39.2° C, poor sleep and appetite and bulging TM Children older than 24 months with fever less than 39° C and non-severe symptoms may be watched for 24 hours with symptomatic treatment. Children with otorrhea, those with severe AOM, and any children with fever greater than 39° C should be given antibiotics. A pediatric patient has otalgia, fever of 38.8° C, and a recent history of upper respiratory examination. The examiner is unable to visualize the tympanic membranes in the right ear because of the presence of cerumen in the ear canal. The left tympanic membrane is dull gray with fluid levels present. What is the correct action? a. Perform a tympanogram on the right ear b. Recommend symptomatic treatment for fever and pain c. Remove the cerumen and visualize the tympanic membrane d. Treat empirically with amoxicillin 80 to 90 mg/kg/day The AAP 2013 guidelines strongly recommend visualization of the tympanic membrane to accurately diagnose otitis media and not to treat based on symptoms alone. The practitioner should attempt to remove the cerumen in order to visualize the tympanic membrane. A tympanogram cannot be performed when cerumen is blocking the canal. Because the child may have an acute ear infection, antibiotics may be necessary. 3. Skin Herpes Zoster Buttaro Chapter 55, Kennedy chapter 6 Herpes zoster is an acute vesicular eruption caused by a virus histologically identical to the varicella (chickenpox) virus. the virus spreads across the sensory ganglion to other neurons, which causes a cutaneous eruption of a dermatome distribution. If herpes zoster affects bilateral dermatomes, it is considered to be disseminated herpes zoster. atients usually experience hyperesthesia with a burning or tingling pain at the site 4 to 5 days before the eruption appears. Pain in a dermatomal pattern may precede the appearance of the vesicles. The direct immunofluorescence with fluorescein-tagged antibody (DFA) or polymerase chain reaction (PCR) (if available) is preferred over the old standard Tzanck smear. A Tzanck test is a rapid way to confirm the diagnosis of zoster in the provider's office but does not distinguish between VZV and herpes simplex virus. Postherpetic neuralgia is not reduced by antiviral therapy, but these agents may help with healing in the acute phase. Give acyclovir, 800 mg 5 times a day for 7 to 10 days; famciclovir, 500 mg orally every 8 hours for 7 days; or valacyclovir, 1000 mg orally every 8 hours for 7 days/ he vaccine for herpes zoster (Zostavax) is available and is recommended for patients age 60 and older. Questions Which of the following dermatological conditions results from reactivation of the dormant varicella virus? A. Tinea versicolor B. Seborrheic keratosis C. Verruca D. Herpes zoster An older adult male presents with pain in his right chest wall for the past 48 hours. Upon examination, the nurse practitioner notices a vesicular eruption along the dermatome and identifies this as herpes zoster. The NP informs the gentleman that: A. All symptoms should disappear within three days B. Oral medications can dramatically reduce the duration and intensity of his symptoms C. He has chickenpox and can be contagious to his grandchildren D. He has a sexually transmitted disease The immunofluorescent antibody (IFA) is a laboratory test used to diagnose which of the following disorders? A. Tinea versicolor B. Herpes zoster C. Squamous cell carcinoma D. Human papilloma virus `Which of the following is generally not a first-line treatment for post herpetic neuralgia? A. Intrathecal methylprednisolone B. Gabapentin C. 5% lidocaine patch D. Topical capsaicin A patient who has had a previous herpes zoster outbreak experiences a second outbreak and asks the provider about treatment to reduce the duration and severity of symptoms. What will the provider recommend? a. Acyclovir b. Lidocaine patch c. Oral corticosteroids d. Topical corticosteroids Acyclovir, given within 72 hours of onset of rash, has been shown to reduce the duration and severity of the rash and pain and to reduce the risk for PHN and disseminated disease. Lidocaine patches help with pain, but do not reduce the duration of the symptoms. Corticosteroids have not been shown to prevent development of PHN, but have shown modest reduction in duration and severity. An older patient experiences a herpes zoster outbreak and asks the provider if she is contagious because she is going to be around her grandchild who is too young to be immunized for varicella. What will the provider tell her? a. An antiviral medication will prevent transmission to others. b. As long as her lesions are covered, there is no risk of transmission. c. Contagion is possible until all of her lesions are crusted. d. Varicella zoster and herpes zoster are different infections. Herpes zoster lesions contain high concentrations of virus that can be spread by contact and by air; although they are less contagious than primary infections, contagion is possible until all lesions are crusted. Antiviral medications shorten the course, but do not reduce transmission. Covering the lesions does not prevent transmission. Herpes zoster and varicella zoster are the same. A patient has a unilateral vesicular eruption which is described as burning and stabbing in intensity. To differentiate between herpes simplex and herpes zoster, which test will the provider order? a. Polymerase chain reaction analysis b. Serum immunoglobulins c. Tzanck test d. Viral culture The PCR is a rapid and sensitive test that can differentiate between the two. Serum Ig levels are not diagnostic. The Tzanck test identifies the presence of a herpes virus, but does not differentiate between the two types. Viral culture will differentiate, but is not rapid. 60-year-old patient with a previous history of shingles asks about the herpes zoster vaccine. What will the provider recommend? a. A series of two herpes zoster vaccinations b. A single dose of herpes zoster vaccine c. No herpes zoster vaccine is necessary d. Prophylactic vaccination if exposed to chicken pox All patients 50 years and older should have a single dose of herpes zoster vaccine regardless of previous herpes zoster infection. Dermatitis Buttaro chapter 48 Contact dermatitis is further classified as irritant or allergic type. A well-demarcated area of erythema, scaling, or crusting will occur at the site of the exposure. The hands are the most common area affected. A potassium hydroxide (KOH) slide can rule out dermatophyte infection; bacterial. The mainstay of treatment is topical application of medium- to high-potency corticosteroids. Questions A child has irritant contact dermatitis with lesions on the extremities and face. Which treatment is recommended for this patient? a. Antihistamines b. Medium- to high-potency topical corticosteroids c. Oral corticosteroids d. Topical calcineurin inhibitors When periorbital regions or more than 20% of the body surface area is involved, the use of an oral steroid is appropriate. Antihistamines produce relaxation and improve sleep, but do not reduce the pruritus associated with contact dermatitis. Topical calcineurin inhibitors may be used in place of topical steroids, but oral steroids are indicated in this instance. A patient who has been exposed to poison ivy presents with inflammation and a vesicular rash on one arm. The provider recommends a topical steroid, but the next day the patient calls to report similar lesions appearing on the face. What will the provider tell this patient? a. The rash is spreading through self-inoculation. b. The vesicles may continue to develop for up to 2 weeks. c. The rash may spread over the next 8 weeks. d. The patient must have been re-exposed to the irritant. Exposure to poison ivy resin results in vesicles and bullae that develop for up to 2 weeks. Once the resin is washed off, no further spread occurs. With insufficient treatment, the rash may persist, but not spread, for up to 8 weeks. Impetigo (buttaro chapter 47 The common initial presentation of impetigo is vesiculopustular or even bullous lesions. When the lesions rupture and exude their contents, they create the classic honey-colored crusts. Questions A child has vesiculopustular lesions around the nose and mouth with areas of honey-colored crusts. The provider notes a few similar lesions on the child’s hands and legs. Which treatment is appropriate for this child? a. Amoxicillin-clavulanate b. Culture and sensitivity of the lesions c. Sulfamethoxazole-trimethoprim d. Topical antiseptic ointment This child has symptoms of impetigo which has spread to the hands and legs. A systemic penicillinase-resistant penicillin is recommended. It is not necessary to obtain a culture since this can be treated empirically in most cases. MRSA is unlikely, so sulfamethoxazole-trimethoprim is not indicated. Oral antibiotics, not topical antiseptics, are the treatment of choice. Psoriasis Buttaro Chapter 62 Psoriasis is an inflammatory, autoimmune disease, papulosquamous eruption characterized by well-circumscribed erythematous macular and papular lesions with loosely adherent silvery white scale. The dermis is highly vascular, and tiny bleeding points are revealed if the scales are removed (Auspitz sign). High-potency topical glucocorticosteroids applied BID produce maximum benefit in 2 to 3 weeks. Ointments are the preferred vehicle because of better medicine penetration and support of the skin moisture barrier; however, ointments are not easily tolerated by the patient. Methotrexate, a folic acid antagonist, is highly effective in treating severe, recalcitrant psoriasis involving a large body area, acute pustular psoriasis, and psoriatic arthritis Questions A child has plaques on the extensor surfaces of both elbows and on the face with minimal scaling and pruritis. What is the likely cause of these lesions? a. Atopic dermatitis b. Guttate psoriasis c. Psoriasis d. Seborrhea Children with psoriasis often have lesions on the face and have less scaling than adults. Psoriasis tends to present on extensor surfaces, while atopic dermatitis occurs on flexor surfaces. Guttate psoriasis appears as teardrop-shaped lesions that appear on the trunk and spread to the extremities and are occasionally seen after streptococcal infections in adolescents. Seborrhea usually occurs on the scalp. A patient with psoriasis develops lesions on the intertriginous areas of the skin. Which treatment is recommended? a. High-potency topical steroids b. Oral corticosteroid injections c. Topical steroids with vitamin D d. Topical, low-potency steroids Patients with intertriginous psoriasis should be treated with low-potency topical steroids. High-potency steroids usually produce maximum benefit in 2 to 3 weeks and research suggests combining high-potency steroids with vitamin D analog is best. Oral corticosteroids are used for recalcitrant symptoms. A patient with severe, recalcitrant psoriasis has tried topical medications, intralesional steroid injections, and phototherapy with ultraviolet B light without consistent improvement in symptoms. What is the next step in treating this patient? a. Cyclosporine b. Etanercept c. Methotrexate d. Oral retinoids Methotrexate has shown good efficacy in treating recalcitrant psoriasis. Cyclosporine and oral retinoids are effective, but have serious side effects. Etanercept and other biologic agents are effective but expensive and should be tried after all other treatments have failed. REF: Management/Systemic Medications/Biologic Agents Tinea Capitis Questions Patients who have an underlying tinea infection to the cellulitis should also be treated with which one of the following? A. An anti-fungal medication B. Topical steroids C. Oral steroids D. Zinc oxide Which of the following descriptions best illustrates assessment findings consistent with tinea capitis? A. Circular erythematous patches with papular, scaly annular borders and clear centers B. Inflamed scaly dry patches with broken hairs C. Web lesions with erythema and scaling borders D. Scaly pruritic erythematous lesions on inguinal creases Skin cancer: Basal Cell Carcinoma Questions A 70-year-old white male comes to the clinic with a slightly raised, scaly, pink, and irregular lesion on his scalp. He is a farmer and works outside all day. You suspect actinic keratosis, but cannot rule out other lesions. What recommendation would you give him? A. Ignore the lesion, as it is associated with aging. B. Instruct him to use a nonprescription hydrocortisone cream to dry up the lesion. C. Perform a biopsy or refer to a dermatologist. D. Advise him to use a dandruff shampoo and return in one month if the lesion has not gone away. A smooth round nodule with a pearly gray border and central induration best describes which skin lesion? A. Seborrheic keratosis B. Malignant melanoma C. Herpes zoster D. Basal cell carcinoma An 82-yeAnan 82 years old female has a “pimple” on his nose that occasionally bleeds and may have increased in size in the past year. The lesion is a 0.7-cm, dome-shaped, umbilicated papule with pearly translucence. There is also a hemorrhagic crust covering the central portion. Which of the following is the most likely diagnosis? A. Squamous cell carcinoma B. Basal cell carcinoma C. Keratocanthoma D. Sebaceous hyperplasia AsymmetA Asymmetrical bi-color lesion with irregular border measuring 8 mm is found on the right lower arm of an adult patient. This assessment finding is consistent with: A. Melanoma B. Basal cell carcinoma C. Leukoplakia D. Senile lentigines 4. Cardiovascular Hypertension (Buttaro Chapter 114, Kennedy chapter 8) Hypertension is diagnosed on the basis of a persistently high BP identified on 3 measurements at least 1 week apart Questions A patient who has had mild pulmonary hypertension with a previous symptom of a loud second heart sound on exam now has edema and jugular vein distension. This indicates which complication? a. Left ventricular dysfunction b. Right ventricular dysfunction c. Tricuspid valve involvement d. Mitral valve involvement Right ventricular dysfunction occurs as the disease worsens with manifestations that include jugular vein distension, edema, and increased liver size. These symptoms do not indicate left ventricular dysfunction or valvular involvement.REF: Physical Examination In mitral stenosis, p waves may suggest: Left atrial enlargement Aortic regurgitation requires medical treatment for early signs of CHF with: ACE inhibitors A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: Women with ischemic heart disease many times do not present with chest pain Some patients may have no symptoms or atypical symptoms. Diagnosis may only be made at the time of an actual myocardial infarction A & B only The best evidence rating drugs to consider in a post myocardial infarction patient include: ASA, ACE/ARB, beta-blocker, aldosterone blockade A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan may include: Exercise stress test Preceding a stress test, the following lab work might include: CBC and differential to differentiate ischemic heart disease from anemia Which test is the clinical standard for the assessment of aortic stenosis: Echocardiography What is the most common valvular heart disease in the older adult? Aortic stenosis Ischemic heart disease is: Defined as imbalance between oxygen supply and demand. Frequently is manifested as angina Leading cause of death in the elderly. All of the above. The aging process causes what normal physiological changes in the heart? The heart valve thickens and becomes rigid, secondary to fibrosis and sclerosis An older adult may present with atypical clinical signs of pneumonia. The nurse practitioner needs to be aware that the clustering of all of the following signs and symptoms may be indicative of pneumonia in an older person except: Bradycardia Which of the following statements is true concerning anti-arrhythmic drugs? Most anti-arrhythmics have a low toxic/therapeutic ratio and some are exceedingly toxic. Susan P., a 60-year-old woman with a 30 pack year history, presents to your primary care practice for evaluation of a persistent, daily cough with increased sputum production, worse in the morning, occurring over the past three months. She tells you, “I have the same thing, year after year.” Which of the following choices would you consider strongly in your critical thinking process? Chronic bronchitis The best way to diagnose structural heart disease/dysfunction non-invasively is: Echocardiogram A common auscultatory finding in advanced CHF is: S3 gallop rhythm The organism most commonly responsible for community-acquired pneumonia in older adults is: Streptococcus pneumonia A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is most likely? Pulmonary embolism Hyperlipidemia (kennedy chapter 14 Reductions in lipid levels have been shown to be effective in primary and secondary prevention of cardiovascular disease. The primary target of therapy, in general, is lowering low-density lipoprotein (LDL) cholesterol. econdary causes of hyperlipidemia include hypothyroidism, poorly controlled diabetes mellitus, nephrotic syndrome, certain drug therapy such as glucocorticoids, and liver disease Total cholesterol ≥240 mg/dL is considered high. HDL level of ≤40 mg/dL is considered low TG levels of 200 to 499 mg/dL are considered high, Diet therapy with exercise and stress reduction should be initiated first for a 3- to 6-month trial before starting medications. Questions During a routine physical examination of a 62-year-old female patient, the nurse practitioner identifies xanthelasma around both his eyes. What is the significance of this finding? A. High potential for future blindness and requires immediate referral B. None, normal variant of aging process C. Abnormal lipid metabolism requiring medical management D. Hereditary variant that is of no consequence but requires watchful waiting Mr. White is 62 years old and has chronic kidney disease that has been relatively stable. He also has a history of hyperlipidemia, osteoarthritis, and hypertension. He is compliant with his medications, and his BP has been well controlled on a calcium channel blocker. His last lipid panel showed: TC = 201, HDL = 40, TG = 180, LDL = 98. He currently takes Crestor 20 mg daily. In the office today, his BP is 188/90, and his urine dip now shows significant proteinuria. He denies any changes in his dietary habits or medication regimen. What would be the best medication change for Mr. White at this point? A. No change—have him return in 4 weeks for a re-check of his blood pressure and urine B. Increase the dose of the calcium channel blocker for his hypertension C. Change the calcium channel blocker to an ACE-I D. Increase the dose of his Crestor and have him return in 3 months for a re-check of his BP Acute myocardial infarction Typical symptom is prolonged chest pain (more than 20 minutes’ duration); atypical symptoms include shortness of breath, neurological symptoms (confusion, weakness), and worsening of heart failure. Elderly persons may not recognize that throat, shoulder, arm, jaw, or abdominal pain may be referred cardiac pain or angina equivalent. Dyspnea is the second most common symptom of MI in both younger and older populations. Chest pain should be treated with sublingual nitroglycerin, repeated 3 times, 5 minutes apart, unless the patient is hypotensive, has right ventricular infarction, or has aortic stenosis. Thrombolytic agents include tissue-type plasminogen (tPA) and streptokinase (SK). Indications for thrombolysis are based on the existence of chest pain and specific ECG changes. Aspirin therapy should be initiated at 162 to 325 mg daily fro 1 motnh to 1 year ACE inhibitors reduce mortality in post-MI patients Questions 1. An asymptomatic 63-year-old female has a low-density lipoprotein level of 135 mg/dL. Which test is beneficial to assess this patient’s coronary artery disease risk? a. Coronary artery calcium score b. C-reactive protein c. Exercise echocardiography d. Myocardial perfusion imaging The CRP is useful in asymptomatic women >60 years who have LDL <160 mg/dL to predict CAD risk. Although the CACS has shown some benefit in patients with moderate risk, the role for this diagnostic test is unclear. Exercise echocardiography and myocardial perfusion imaging are not performed initially.REF: Overview of Cardiac Diagnostic Testing Which risk assessment for coronary artery disease is recommended for all female patients? a. Coronary artery calcium score b. Electrocardiogram c. Exercise stress test d. Framingham risk score The Framingham risk score is a quick method for identifying potential risk for CAD and can guide providers in choosing subsequent tests based on risk level. The ECG is performed on women with risk factors. The exercise stress test is useful in symptomatic women who have a normal ECG. The CACS may be used if moderate risk is present. A key symptom of ischemic heart disease is chest pain. However, angina equivalents may include exertional dyspnea. Angina equivalents are important because: A. + B. Some patients may have no symptoms or atypical symptoms. Diagnosis may only be made at the time of an actual myocardial infarction C. Elderly patients have the most severe symptoms D. A & B only The best evidence rating drugs to consider in a post myocardial infarction patient include: A. ASA, ACE/ARB, beta-blocker, aldosterone blockade B. Ace, ARB, Calcium channel blocker, ASA C. Long-acting nitrates, warfarin, ACE, and ARB D. ASA, clopidogrel, nitrates A 55-year-old post-menopausal woman with a history of hypertension complains of jaw pain on heavy exertion. There were no complaints of chest pain. Her ECG indicates normal sinus rhythm without ST segment abnormalities. Your plan may include: A. Echocardiogram B. Exercise stress test C. Cardiac catheterization D. Myocardial perfusion imaging Syncope (Buttaro chapter 36, kennedy chapter 5) sudden and transient loss of consciousness and postural tone resulting from a reduction in oxygen to the brain. The most common cause of syncope is vasovagal. Orthostatic hypotension is rare in patients younger than 40 years, yet is one of the most common causes of syncope in patients older than 70 years. he ECG is the most important diagnostic test with a focus on the rate and rhythm. Questions A form of syncope that is more common in the elderly than younger adults is: A. Vasovagal B. Carotid sinus sensitivity C. Orthostatic hypotension D. Arrhythmias Which tests are indicated as part of the initial evaluation for women of childbearing age who report syncope? Select all that apply. a. 12-lead electrocardiogram b. Cardiac enzyme levels c. Complete blood count d. Electroencephalogram e. Serum glucose testing Initial evaluation for all patients reporting syncope should include a standard 12-lead ECG. Women of childbearing age should have a CBC, serum pregnancy test, and serum glucose testing. Cardiac enzyme levels are obtained if the patient has cardiac risk factors. EEG is performed only if there is a concern for seizure disorder. REF: Syncope/Diagnostics A healthy 20-year-old patient reports having had 1 or 2 episodes of syncope without loss of consciousness. Which is the most likely type of syncope in this patient? a. Cardiac b. Neurogenic c. Orthostatic hypotensive d. Reflex syncope Neurally mediated or reflex syncope is the most common cause of syncope and is primarily seen in young adults. Cardiac, neurogenic, and orthostatic syncope are generally seen in older adults. REF: Syncope/Pathophysiology An elderly patient reports experiencing syncope each morning when getting out of bed. Which assessment will the health care provider perform first to evaluate this patient’s symptoms? a. Cardiac enzyme levels b. Electroencephalogram c. Fasting blood glucose d. Orthostatic blood pressures Orthostatic blood pressures should be measured first since this patient reports problems associated with rising from a supine position. The other tests are performed as part of the diagnostic workup only if indicated by associated symptoms or suspected causes. REF: Syncope/Physical Examination 5. Pulmonary Community acquired pneumonia (Buttaro chapter 111, kennedy chapter 8) A patient has a cough and fever and the provider auscultates rales in both lungs that do not clear with cough. The patient reports having a headache and sore throat prior to the onset of coughing. A chest radiograph shows patchy, nonhomogeneous infiltrates. Based on these findings, which organism is the most likely cause of this patient’s pneumonia? a. A virus b. Mycoplasma c. S. pneumoniae d. Tuberculosis Atypical pneumonias, such as those caused by mycoplasma often present with headache and sore throat and will have larger areas of infiltrate on chest radiograph. Viral pneumonias show more diffuse radiographic findings. S. pneumonia will have high fever and cough and distinct areas of infiltration.REF: Pathophysiology/Clinical Presentation A young adult, previously healthy clinic patient has symptoms of pneumonia including high fever and cough. Auscultation reveals rales in the left lower lobe. A chest radiograph is normal. The patient is unable to expectorate sputum. Which treatment is recommended for this patient? a. A B-lactam antibiotic plus a fluoroquinolone b. A respiratory fluoroquinolone antibiotic c. Empiric treatment with a macrolide antibiotic d. Hospitalization for intravenous antibiotics This patient likely has community-acquired pneumonia. The patient has typical symptoms and, even though the chest radiograph is normal, will require outpatient treatment. For community-acquired pneumonia in a previously healthy individual, treatment with a macrolide antibiotic is the recommended first-line therapy. B-lactam plus fluoroquinolone therapy is used for patients in the ICU. Respiratory fluoroquinolones are used for patients with underlying disorders who develop pneumonia. Hospitalization is not necessary.REF: Management A patient who was initially treated as an outpatient for pneumonia and then hospitalized for two weeks after no improvement continues to show no improvement after several antibiotic regimens have been attempted. What is the next step in managing this patient? a. Administration of the pneumonia vaccine b. Increasing the dose of the antibiotics c. Open lung biopsy d. Performing diagnostic bronchoscopy Patients who do not respond to antibiotic therapy may have opportunistic fungal or other infections, bronchogenic carcinoma, or other diseases. Bronchoscopy can exclude or confirm these. The pneumonia vaccine is preventative for pneumococcal causes and will not help this patient. Increasing the dose of the antibiotics is not recommended. Open lung biopsy may be performed if a bronchoscopy is inconclusive.REF: Complications An older adult may present with atypical clinical signs of pneumonia. The nurse practitioner needs to be aware that the clustering of all of the following signs and symptoms may be indicative of pneumonia in an older person except: A. Bradycardia B. Malaise C. Anorexia D. Confusion The organism most commonly responsible for community-acquired pneumonia in older adults is: A. Pseudomonas aeruginosa B. Staphylococcus aureus C. Proteus mirabilis D. Streptococcus pneumonia Asthma (kennedy chapter 8, buttaro 103) A patient who has asthma calls the provider to report having a peak flow measure of 75%, shortness of breath, wheezing, and cough, and tells the provider that the symptoms have not improved significantly after a dose of albuterol. The patient uses an inhaled corticosteroid medication twice daily. What will the provider recommend? a. Administering two more doses of albuterol b. Coming to the clinic for evaluation c. Going to the emergency department d. Taking an oral corticosteroid ANS: A The patient is experiencing an asthma exacerbation and should follow the asthma action plan (AAP) which recommends three doses of albuterol before reassessing. The peak flow is above 70%, so ED admission is not indicated. The patient may be instructed to come to the clinic for oxygen saturation and spirometry evaluation after administering the albuterol. An oral corticosteroid may be prescribed if the patient will be treated as an outpatient after following the AAP. REF: Management An adult develops chronic cough with episodes of wheezing and shortness of breath. The provider performs chest radiography and other tests and rules out infection, upper respiratory, and gastroesophageal causes. Which test will the provider order initially to evaluate the possibility of asthma as the cause of these symptoms? a. Allergy testing b. Methacholine challenge test c. Peak expiratory flow rate d. Spirometry Spirometry is recommended at the time of initial assessment to confirm the diagnosis of asthma. Allergy testing is performed only if allergies are a possible trigger. The methacholine challenge test is performed if spirometry is inconclusive. PEFR is generally used to monitor asthma symptoms. REF: Diagnostics A patient is seen in clinic for an asthma exacerbation. The provider administers three nebulizer treatments with little improvement, noting a pulse oximetry reading of 90% with 2 L of oxygen. A peak flow assessment is 70%. What is the next step in treating this patient? a. Administer three more nebulizer treatments and reassess b. Admit to the hospital with specialist consultation c. Give epinephrine injections and monitor response d. Prescribe an oral corticosteroid medication Patients having an asthma exacerbation should be referred if they fail to improve after three nebulizer treatments or three epinephrine injections, have a peak flow less than 70% and a pulse oximetry reading less than 90% on room air. Giving more nebulizer treatments or administering epinephrine are not indicated. The patient will most likely be given IV corticosteroids; oral corticosteroids would be given if the patient is managed as an outpatient. REF: Definition and Epidemiology T.B. (immunization) (kennedy chapter 8 / Buttarp chapter 235) A 25-year-old patient has a tuberculosis skin test which reveals an area of induration of 12 mm. The patient is a recent immigrant from Mexico and lives in a homeless shelter. What is the recommended treatment for this patient? a. Administer the BCG vaccine b. Begin INH preventive therapy c. Order INH and Rifampin d. Perform regular TB skin testing every few months Patients younger than 35 who have any risk factors for TB and with an area of induration ≥10 mm should be considered for INH preventive therapy. This patient is an immigrant from Mexico and lives in a homeless shelter, so TB preventive therapy is acceptable. BCG vaccine is not helpful. INH and Rifampin are used if patients develop symptoms or if there is antibiotic resistance.REF: Management A provider is concerned that a young child may have latent tuberculosis infection (LTBI). Which test will be performed initially to screen for this infection? a. Chest radiograph b. Interferon gamma release assay c. Mantoux test d. Two-step TST The Mantoux test is the most cost-effective test to administer as an initial screen. Chest radiograph is not used to detect LTBI because there is no radiographic evidence with latent infection. The IGRA may be used, but is more costly and the sensitivity in young children has not been established. The two-step TST is not indicated.REF: Latent Tuberculosis Infection/Diagnostics A patient who has HIV infection has a negative tuberculosis skin test with induration less than 10 mm. The provider learns that the patient lives with a person who has active tuberculosis. What is the next step in managing this patient? a. Begin empiric antibiotic therapy b. Order a chest radiograph c. Perform an interferon gamma release assay d. Refer to an infectious disease specialist Patients who are immunocompromised who have had contact with a person with infectious TB should have a chest radiograph. Until infection is established, empiric antibiotic therapy is not indicated in order to reduce the risk of antibiotic resistance. IGRA is not indicated. If radiograph results are positive, or if the diagnosis remains unclear, referral is indicated.REF: Management Ali is a 72-year-old man who recently came to the U.S. from Nigeria. He reports having BCG (bacille Calmette-Guerin) vaccination as a child. Which of the following is correct regarding a tuberculin skin test? A. It should not be done at all. B. It should be read as smaller than it really is. C. Vaccination history is irrelevant; read as usual. D. It should be read as larger than it really is. The routine testing of tuberculosis should occur in all of the following vulnerable populations except: A. Nursing home residents B. Prison inmates C. Hospitalized elderly D. Immune-compromised patients Bronchitis (Buttaro chapter 102 An adult patient who had pertussis immunizations as a child is exposed to pertussis and develops a runny nose, low-grade fever, and upper respiratory illness symptoms without a paroxysmal cough. What is recommended for this patient? a. Azithromycin daily for 5 days b. Isolation if paroxysmal cough develops c. Pertussis vaccine booster d. Symptomatic care only Adults previously immunized against pertussis may still get the disease without the classic whooping cough sign seen in children and are contagious from the beginning of the catarrhal stage of runny nose and common cold symptoms. Azithromycin or other macrolide antibiotics are useful for reducing symptoms and for decreasing shedding of bacteria to limit spread of the disease. Patients should be isolated for 5 days from the start of treatment. Pertussis vaccine booster will not alter the course of the disease once exposed. Symptomatic care only will not reduce symptoms or decrease disease spread. REF: ManagementQuestion 2 of 3 A patient develops a dry, non-productive cough and is diagnosed with bronchitis. Several days later, the cough becomes productive with mucoid sputum. What may be prescribed to help with symptoms? a. Antibiotic therapy b. Antitussive medication c. Bronchodilator treatment d. Mucokinetic agents Antitussive medications are occasionally useful for short-term relief of coughing. Antibiotic therapy is generally not needed and should be avoided unless a bacterial cause is likely. Bronchodilator medications show no demonstrated reduction in symptoms and are not recommended. Mucokinetic agents have no evidence to support their use. REF: Communication and Language Development A patient develops acute bronchitis and is diagnosed as having influenza. Which medication will help reduce the duration of symptoms in this patient? a. Azithromycin b. Clindamycin c. Oseltamivir d. Trimethoprim-sulfamethoxazole Oseltamivir is an antiviral medication used to reduce the severity and duration of symptoms of influenza. The other medications are antibacterial medications and not effective to treat influenza. Susan P., a 60-year-old woman with a 30 pack year history, presents to your primary care practice for evaluation of a persistent, daily cough with increased sputum production, worse in the morning, occurring over the past three months. She tells you, “I have the same thing, year after year.” Which of the following choices would you consider strongly in your critical thinking process? A. Seasonal allergies B. Acute bronchitis C. Bronchial asthma D. Chronic bronchitis COPD (Buttaro Chapter 106 / kennedy chapter 8) Which is characteristic of chronic bronchitis and not emphysema? a. Damage to the alveolar wall b. Destruction of alveolar architecture c. Mild alteration in lung tissue compliance d. Mismatch of ventilation and perfusion Chronic bronchitis causes much less parenchymal damage than emphysema does, so there is milder alteration in lung tissue compliance. The other symptoms are characteristic of emphysema. A patient with chronic obstructive pulmonary disease and reports daily symptoms of dyspnea and cough. Which medication will the prescriber order? a. Ipratropium bromide b. Pirbuterol acetate c. Salmeterol xinafoate d. Theophylline Ipratropium bromide is an anticholinergic medication and is used as first-line therapy in patients with daily symptoms. Pirbuterol acetate and salmeterol xinafoate are both beta2-adrenergics and are used to relieve bronchospasm; pirbuterol is a short-term medication used for symptomatic relief and salmeterol is a long-term medication useful for reducing nocturnal symptoms. Theophylline is a third-line agent. Which test is most diagnostic for chronic obstructive pulmonary disease? a. COPD Assessment Test b. Forced expiratory time maneuver c. Lung radiograph d. Spirometry for FVC and FEV1 Spirometry testing is the gold standard for diagnosis and assessment of COPD because it is reproducible and objective. The forced expiratory time maneuver is easy to perform in a clinic setting and is a good screening to indicate a need for confirmatory spirometry. Lung radiographs are non-specific, but may indicate hyperexpansion of lungs. The COPD assessment test helps measure health status impairment in persons already diagnosed with COPD. PE (kennedy chapter 8 / Buttaro chapter 113) Which clinical sign is especially worrisome in a patient with a pulmonary embolism? a. Abnormal lung sounds b. Dyspnea c. Hypotension d. Tachycardia Hypotension in a patient with PE has a high correlation with acute right ventricular failure and subsequent death. The other signs are common with PE.REF: Diagnosis A patient who has undergone surgical immobilization for a femur fracture reports dyspnea and chest pain associated with inspiration. The patient has a heart rate of 120 beats per minute. Which diagnostic test will confirm the presence of a pulmonary embolism? a. Arterial blood gases b. CT angiography c. D-dimer d. Electrocardiogram Ct angiography is used to diagnose PE. D-dimer assays have good negative predictive value but have poor positive predictive value, making it useful for excluding but not confirming the presence of PE. An ECG does not confirm PE but is used to demonstrate comorbid conditions. Arterial blood gases do not confirm PE and are used to identify the degree of respiratory compromise.REF: Diagnostics A patient develops a pulmonary embolism after surgery and shows signs of right-sided heart failure. Which drug will be administered to this patient? a. Low molecular heparin b. Tissue plasminogen activator c. Unfractionated heparin d. Warfarin Fibrinolytic therapy with recombinant tissue plasminogen activator is given to patients with hypotension and right-sided heart failure. Heparin is used for its anticoagulant properties in all patients with PE. Warfarin is not indicated. A 72-year-old woman and her husband are on a cross-country driving vacation. After a long day of driving, they stop for dinner. Midway through the meal, the woman becomes very short of breath, with chest pain and a feeling of panic. Which of the following problems is most likely? A. Pulmonary edema B. Heart failure C. Pulmonary embolism D. Pneumonia 6. Endocrine Type 2 diabetes (Buttaro chapter 206 / kennedy chapter 14) A patient who has diabetes has a blood pressure of 140/90 mm Hg and albuminuria. Which initial action by the primary care provider is indicated for management of this patient? a. Consulting with a nephrologist b. Limiting protein intake c. Prescribing an antihypertensive medication d. Referring to an ophthalmologist Patients with diabetes who have elevated blood pressure and reduced renal function should be referred to a nephrologist. Limiting protein intake and giving an antihypertensive medication may be recommended, but evaluation by a nephrologist is essential. Ophthalmology referral will be made as well to assess concurrent ocular damage. A patient who is obese has recurrent urinary tract infections and reports feeling tired most of the time. What initial diagnostic test will the provider order in the clinic at this visit? a. C-peptide level b. Hemoglobin A1C c. Random serum glucose d. Thyroid studies HbA1C, along with fasting plasma glucose or a 2-hour plasma glucose during an OGTT are diagnostic of diabetes. This patient is probably not fasting, so a glucose level will not be helpful. C-peptide levels help to distinguish type 1 from type 2 diabetes and may be performed after a diagnosis of diabetes is made and if there is uncertainty about the cause. Thyroid studies are helpful in evaluating comorbidity. A patient recently diagnosed with type 1 diabetes mellitus is in clinic for a follow-up evaluation. The provider notes that the patient appears confused and irritable and is sweating and shaking. What intervention will the provider expect to perform once the point of care blood glucose level is known? a. Dipstick urinalysis for ketones b. Giving a rapid-acting carbohydrate c. Injection of rapid-acting insulin d. Performing a hemoglobin A1C This patient has signs of hypoglycemia, so a rapid-acting carbohydrate should be given once this is confirmed. Assessing for ketones is done if the patient is hyperglycemic, as is insulin administration. Hemoglobin A1C gives information about long-term and not immediate glucose control. A patient with type 2 diabetes mellitus becomes insulin dependent after a year of therapy with oral diabetes medications. When explaining this change in therapy, the provider will tell the patient: a. it is necessary because the patient cannot comply with the previous regimen. b. that strict diet and exercise measures may be relaxed with insulin therapy. c. the use of insulin therapy may be temporary. d. this is because of the natural progression of the disease. Even after several years of therapy for type 2 DM well controlled with oral diabetic medications, diet, and exercise, the natural progression of the disease may require patients to become insulin dependent. Patients must understand that this does not represent failure on their part. Adding insulin may cause weight gain, so continuing lifestyle measures is essential. The addition of insulin is not temporary. A patient has been prescribed metformin (Glucophage). One week later he returns with lowered blood sugars but complains of some loose stools during the week. How should the nurse practitioner respond? A. Discontinue the medication immediately B. Reassure the patient that this is an anticipated side effect C. Double the dosage of medication and have patient return in 1 week D. Order a chem. 7 to check for lactic acidosis A 60-year-old obese male client has type 2 diabetes mellitus and a lipid panel of TC = 250, HDL = 32, LDL = 165. The nurse practitioner teaches the patient about his modifiable cardiac risk factors, which include: A. Advancing age, diabetes, hyperlipidemia, and male gender B. Diabetes, obesity, and hyperlipidemia C. Hyperlipidemia, smoking, and family history of heart disease D. Male with age > 45, diabetes mellitus, and hyperlipidemia ____ 13. A diabetic patient presents with the complaint of right foot pain but denies any recent known injury. He states it has gotten progressively worse over the past few months. On exam, vibratory sense, as well as sensation tested with a monofilament, was abnormal. The patient’s foot is warm, edematous, and misshapen. The nurse practitioner suspects Charcot foot. What intervention is indicated? A. Warm soaks and return for follow-up in 1 week B. Referral to a pain management clinic C. Referral to an orthopedist D. Referral to a cardiologist for evaluation of peripheral vascular disease ____ 14. What is a sign of insulin resistance that can present in African American patients? A. Acanthosis Nigricans B. Psoriasis Nigricans C. Seborrheic Nigricans D. Bullemic Nigricans Thyroid disease (hypo/hyper)( Kennedy chapter 14 / Buttaro chapter 214 Which thyroid stimulating hormone (TSH) level indicates hyperthyroidism? a. 0.2 uIU/L b. 0.4 uIU/L c. 2.4 uIU/L d. 4.2 uIU/L A TSH less than 0.3 uIU/L indicates hyperthyroid; greater than 4.0 uIU/L indicates hypothyroid, and between 0.3 to 4.0 uIU/L indicates euthyroid.REF: Thyroid Function Tests A 20-year-old female patient with tachycardia and weight loss but no optic symptoms has the following laboratory values: decreased TSH, increased T3, and increased T4 and free T4. A pregnancy test is negative. What is the initial treatment for this patient? a. Beta blocker medications b. Radioiodine therapy c. Surgical resection of the thyroid gland d. Thionamide therapy Beta blockers should be initiated for patients with Graves’ disease to alleviate the alpha-adrenergic symptoms of the hyperthyroidism. Radioiodine therapy is used for patients with Graves’ ophthalmopathy. Surgical resection is performed for pregnant women who cannot be managed with thioamides or for patients who refuse radioiodine therapy. Thioamide therapy is recommended for patients younger than 20 years old, pregnant women, those with a high likelihood of remission, and those with active Graves’ Orbitopathy.REF: Management/Graves’ Disease A postpartum woman develops fatigue, weight gain, and constipation. Laboratory values reveal elevated TSH and decreased T3 and T4 levels. What will the provider tell this patient? a. A thyroidectomy will be necessary. b. She should be referred to an endocrinologist. c. She will need lifelong medication. d. This condition may be transient. Postpartum hypothyroidism may be a transient condition and does not require surgical intervention, referral to a specialist, or lifelong medication unless it proves to be long-standing or refractory to treatment.REF: Hypothyroidism/Management A patient has thyroid nodules and the provider suspects thyroid cancer. To evaluate thyroid nodules for potential malignancy, which test is performed? a. Radionucleotide imaging b. Serum calcitonin c. Serum TSH level d. Thyroid ultrasound Thyroid ultrasound evaluation should be performed for all patients with known thyroid nodules; high-resolution sonography can clearly distinguish between solid and cystic components. Radionucleotide imaging is not specific; many cold nodules are benign. The routine measurement of serum calcitonin levels is not useful or cost-effective. TSH levels are not specific to malignancy. An elderly client presents with a new onset of feeling her heart race and fatigue. An EKG reveals atrial fibrillation with rate >110. The patient also has a new fine tremor of both hands. Which of the following would the nurse practitioner suspect? A. Hypothyroidism B. Hyperthyroidism C. Congestive heart failure D. Type 2 diabetes mellitus A 62-year-old female complains of fatigue and lack of energy. Constipation has increased and the patient has gained ten pounds in the past 3 months. Depression is denied although the patient reports a lack of interest in usual hobbies. Vital signs are within normal limits and the patient’s skin is dry and cool. Which of the following must be included in the differential? A. Hyperthyroidism B. Hypothyroidism C. Hyperparathyroidism D. Grave’s disease Mrs. Black, an 87-year-old patient, has been taking 100 mcg of Synthroid for 10 years. She comes to your office for a routine follow-up, feeling well. Her heart rate is 90. Your first response is to: A. Increase the Synthroid B. Order TSH C. Start a beta-blocker D. Order thyroid scan When evaluating the expected outcome for a hypothyroid elderly patient placed on levothyroxine, the nurse practitioner will: A. Assess a weekly TSH B. Assess the TSH in 4-6 weeks C. Ask the patient if the symptoms have subsided and adjust dosage accordingly D. Decrease the dosage should a cardiac event occur The primary reason levothyroxine sodium is initiated at a low dose in an elderly patient with hypothyroidism is to prevent which of the following untoward effects? A. Angina and arrhythmia B. Nausea and diarrhea C. Confusion and delirium D. Osteoporosis and muscle weakness Six months ago an elderly patient was diagnosed with subclinical hypothyroidism. Today the patient returns and has a TSH of 11.0 and complains of fatigue. He has taken Synthroid 25 mcg daily as prescribed. What is the best course of action for the nurse practitioner? A. Assess further for a cause of fatigue B. Double the dose of Synthroid C. Discontinue the Synthroid D. Prescribe Liotrix (T3 & T4 combination) Which of thwhich of the following signs of hyperthyroidism commonly manifest in younger populations, but is notably lacking in the elderly? A. Weight gain B. Constipation C. Bradycardia D. Exophthalmos 7. GI Gastric/duodenal ulcer 144 Contributing factors • H. pylori infection • Use of NSAIDs • Certain infectious conditions and comorbidities Diagnostic tests: Endoscopic gastroduodenoscopy with a biopsy Questions A patient has persistent epigastric pain occurring 2 to 3 hours after a meal. Which test is definitive for diagnosis peptic ulcer in this patient? a. Barium swallow with radiography b. Breath test or stool antigen testing for H. pylori c. Endoscopy with biopsy of gastric mucosa d. Physical exam with percussion of the upper abdomen Endoscopy provides the most accurate diagnosis of PUD and allows biopsy of multiple areas to exclude malignancy. Barium swallow may still be performed in patients unwilling to undergo endoscopy. Breath tests and stool antigen testing for H. pylori can confirm a bacterial cause. Physical exam generally yields negative findings.REF: Physical Examination/Diagnostics What is the best treatment for H. pylori-related peptic ulcer disease? a. H2RA and clarithromycin for 14 days b. H2RA, bismuth, metronidazole, and tetracycline for 10 to 14 days c. PPI and clarithromycin for 14 days d. PPI, amoxicillin, and clarithromycin for 10 days A PPI and clarithromycin for 14 days has documented improved effectiveness over other regimens. Use of an H2RA is cheaper.REF: Management/Table 144-1: Treatment of H. pylori infection A patient who has been taking an NSAID for osteoarthritis pain has peptic ulcer disease. What is the initial step in treating this patient? a. Discontinue the NSAID b. Order prostaglandin therapy c. Prescribe a proton pump inhibitor d. Recommend an H2 receptor antagonist The first step in treating medication-induced peptic ulcer is to discontinue the medication. H2 receptor antagonists are the first anti-secretory medications prescribed. Proton pump inhibitors are more expensive and are used as second-line treatment. Prostaglandin therapy helps protect the gastric and duodenal mucosa and is used if NSAIDS cannot be discontinued.REF: Management Diverticulitis: Buttaro Chapter 133 Diverticulitis, or complicated diverticular disease, is the most common complication of diverticulosis. Often there is tenderness in the left lower quadrant. A CT scan is the test of choice. In general, treatment consists of taking clear liquids for 2 or 3 days, limiting physical activity, and taking oral antibiotics such as trimethoprim-sulfamethoxazole (Bactrim DS, 160 mg/800 mg twice daily) plus metronidazole (500 mg three times daily), amoxicillin–clavulanate potassium (Augmentin, 875 mg/125 mg), or ciprofloxacin (500 mg twice daily) plus metronidazole (500 mg three times daily) for 7 to 14 days Questions A patient has intermittent left-sided lower abdominal pain and fever associated with bloating and constipation alternating with diarrhea. The provider suspects acute diverticulitis. Which tests will the provider order? a. Barium enema examination b. CT scan of abdomen and pelvis c. Plain abdominal radiographs d. Rigid sigmoidoscopy e. Stool for occult blood A CT scan of the abdomen and pelvis is the preferred imaging study if acute diverticulitis is suspected with diverticular abscess. Occult blood tests are necessary because uncomplicated diverticulosis is not known to cause occult rectal bleeding. Barium enema should be avoided in acute diverticulitis because of the risk of extravasation of barium into the peritoneal cavity, causing chemical peritonitis. Plain radiographs are not useful because they will appear normal. Rigid sigmoidoscopy usually cannot be performed beyond the recto-sigmoid junction, so is not useful. A patient has a history of diverticular disease and asks what can be done to minimize acute symptoms. What will the practitioner recommend to this patient? a. Avoiding saturated fats and red meat b. Consuming a diet high in fiber c. Taking an anticholinergic medication d. Using bran to replace high-fiber foods Increasing dietary fiber reduces constipation and reduces the incidence of acute symptoms. Avoiding saturated fats and red meats does not reduce the risk of diverticulitis, but does decrease the risk of colon cancer. Anticholinergics and antispasmodics do not prevent attacks, but may help with symptoms. Bran may be used as an adjunct to high-fiber foods, but should not replace other high-fiber sources. REF: Management A patient who has a history of diverticular disease has left-sided pain and reports seeing blood in the stool. What is an important intervention for these symptoms? a. Ordering a CBC and stool for occult blood b. Prescribing an antispasmodic medication c. Referring the patient for a lower endoscopy d. Reminding the patient to eat a high-fiber diet Patients with suspected diverticular abscess of rectal bleeding need further evaluation and a referral for lower endoscopy is warranted. Hemorrhage is more common from the right colon. The other actions do not have priority over the need to evaluate the cause of the bleeding. REF: Complications/Indications for Referral or Hospitalization Colonoscopy : Colonoscopy: every 10 years after age 50, stopping at age 74 ALT levels The first sign of hepatitis may be the elevation of the serum aminotransferases aspartate aminotransferase (AST) and alanine transaminase (ALT). These enzymes increase proportionately during the prodromal phase of hepatitis and can reach 20 times normal (in acute hepatitis). An AST level that is more than twice the ALT level is typical with alcoholic liver injury. Elevated alkaline phosphatase levels suggest cholestasis, primary biliary cirrhosis, or infiltrative liver disease 8. Neurological Brain tumors: Growth of abnormal cells – tumors – in the tissue of the brain Questions A patient develops a gait disorder and the patient’s spouse reports noticing recent personality changes. The provider suspects a brain lesion. Which evaluation is especially important in the initial physical examination? a. Assessment of peripheral reflexes b. Evaluation of speech c. Examination of the optic fundi d. Testing for memory loss Gait disorders and personality changes are more typical presentations with non-focal lesions. Examination of the optic fundi for papilledema may be the only finding to indicate increased intracranial pressure. The other assessments help determine focal involvement. Which is the preferred treatment for primary brain tumors? a. Chemotherapy b. Palliative care c. Radiation therapy d. Surgical resection Surgical resection is the most effective treatment for brain tumors. Chemotherapy is limited in effectiveness because of difficulty crossing the blood-brain barrier. Radiation therapy is used as a primary, adjuvant, or palliative therapy. Palliative care is not the preferred treatment; many patients with brain tumors live for many years. Headache Migraine: Migraine without aura is the more common. The patient complains of an ipsilateral headache. The pain is described as pounding or throbbing, aggravated by physical activity. The pain lasts 4 to 72 hours and may be associated with nausea, vomiting, photophobia, and phonophobia. These patients usually retreat to a dark, quiet room until the attack is over. They often can identify a trigger that will precipitate the attacks. Common triggers include medication overuse, obesity, depression, stressful life events, sleep problems including snoring, weather changes, foods (cheese, chocolate), alcohol, change in altitude, delay or skipping of a meal, and hormonal changes. In migraine with aura, the aura usually occurs before the onset of head pain. Visual auras can be characterized by spots, shimmering bright lights, or areas of visual loss (scotomas). Somatosensory-type auras can also occur, with tingling or numbness of the fingers, motor disturbances such as hemiparesis or monoparesis, and cognitive disorders. Tension-Type Headache: described as feeling like there is a tight band around the head. Nausea and vomiting are not present Cluster Headache: severe unilateral, retro-orbital pain. Years can pass between attacks, and the event often occurs at the same time each year. alcohol will often precipitate an attack in patients with acute or chronic cluster headache Preventive Therapy. Propranolol, Inderal, diltiazem, amlodipide, amitriptyline Abortive Therapy. Simple analgesics, such as acetaminophen and aspirin, can represent first-line treatment in the management of mild to moderate headaches. When simple analgesics are ineffective, combining them with a short-acting barbiturate, such as butalbital (Fioricet, Fiorinal, Esgic), may be effective. Ergot derivatives are effective in the treatment of moderate to severe attacks Questions A patient has recurrent cluster headaches and asks about abortive therapy. Which therapy is effective for a majority of patients with cluster headaches? a. Lithium b. NSAIDs c. Oxygen d. Verapamil Oxygen works as abortive therapy for cluster headaches in 75% of patients and should be inhaled at the start of an attack. Lithium and verapamil work well as preventive medications for cluster headaches, but are not given for abortive treatment. NSAIDs are not useful.REF: Management A patient reports recurrent headaches occurring 1 or 2 times per month that generally occur with weather changes or when sleep patterns are disrupted and describes them as severe, with throbbing on one side of the head and sometimes accompanied by nausea. What is the recommended treatment for this type of headache? a. Gabapentin b. Propranolol c. Rizatriptan d. Topiramate This patient describes migraine headache without aura and has fewer than 4 per month. An abortive medication, such as rizatriptan is recommended. The other medications are preventive medications and are used for patients having more than 4 per month.REF: Clinical Presentation/Management Which medications may be useful in treating tension-type headache? Select all that apply. a. Antiemetics b. Lithium c. Muscle relaxants d. NSAIDs e. Oxygen Antiemetics, muscle relaxants, and NSAIDs may all be used to treat tension-type headaches. Lithium and oxygen are not used Which form of headache is bilateral? A. Cluster B. Tension C. Migraine D. Acute angle closure glaucoma CVA • A CVA (“stroke”) is an interruption of blood circulation to the brain causing a neurologic deficit that reflects the area of the brain affected. CT – non-contrast scan of head Types: • Ischemic (most prevalent) Lacunar (predominantly older adults and pts with DM) Transient Ischemic Attack (TIA is an acute cerebrovascular syndrome (ACVS) • Hemorrhagic (most lethal, younger, healthy adults) Clinical Presentation: • Hemiparesis, hemisensory loss, visual field defects, ataxia (difficulty with balance and coordination), dysarthria (difficulty speaking), reflex asymmetry, and Babinski’s sign • Headache is common in hemorrhagic stroke • ACVS (TIA) more commonly precedes ischemic stroke than hemorrhagic stroke Questions A previously healthy 30-year-old patient is brought to the emergency department with signs of stroke. Diagnostic testing determines an ongoing ischemic cause. The patient’s spouse reports that symptoms began approximately 2 hours prior to transport. What is the recommended treatment? a. Administration of low-molecular-weight heparin b. Neurosurgical consultation for possible surgery c. Observation for complications prior to initiating tPA d. Tissue plasminogen activator (tPA) administration This patient meets the criteria for tPA administration and it should be begun within 3 hours after onset of symptoms. This patient has had symptoms for over 2 hours, so tPA should begin immediately. LMW heparin is not indicated. Neurosurgical intervention is recommended for patients with hemorrhagic stroke.REF: Thrombolytic Therapy An elderly patient is brought to the emergency department after being found on the floor after a fall. The patient has unilateral sagging of the face, marked slurring of the speech, and paralysis on one side of the body. The patient’s blood pressure is 220/190 mm Hg. What is the likely treatment for this patient? a. Carotid endarterectomy b. Close observation until symptoms resolve c. Neurosurgical consultation d. Thrombolytic therapy This patient has signs consistent with hemorrhagic stroke and will need consultation with a neurosurgeon to determine whether surgical intervention will be beneficial. Carotid endarterectomy is performed in patients with carotid stenosis and is used in patients with hemispheric ACVS (TIA). Patients with TIA may be observed to monitor symptoms. Thrombolytic therapy is given to patients with ischemic stroke.REF: Management/Surgery A patient exhibits visual field defect, ataxia, and dysarthria and complains of a mild headache. A family member reports that the symptoms began several hours prior. An examination reveals normal range of motion of the neck. What type of cerebrovascular event is most likely? a. Hemorrhagic stroke b. Hypertensive intracerebral hemorrhage c. Ischemic stroke d. Transient ischemic attack Patients with ischemic stroke typically do not have headache; if they do, it is milder than with hemorrhagic stroke. A TIA resolves within minutes.REF: Clinical Presentation Anxiety butaro 247 A patient is diagnosed with panic disorder and begins taking a selective serotonin reuptake inhibitor medication. Six weeks later, the patient reports little relief from symptoms. What will the provider do next to manage this patient? a. Change the medication to buspirone b. Discontinue the medication c. Increase the medication dose d. Refer to a mental health provider Patients taking SSRIs for anxiety disorders should see effects within 2 to 4 weeks. If patients have not had good results in 4 to 6 weeks, the provider should change the medication or refer to a mental health provider. Discontinuing an SSRI abruptly can cause withdrawal symptoms. Increasing the medication dose will not improve the effects. Buspirone is somewhat useful only for GAD.REF: Management Which medication are useful in treating both obsessive-compulsive disorder and PTSD? Select all that apply. a. Benzodiazepines b. Buspirone c. Selective serotonin reuptake inhibitors d. Serotonin-norepinephrine reuptake inhibitors e. Tricyclic antidepressants SSRIs, SNRIs, and TCAs are useful in treating both OCD and PTSD. Benzodiazepines and buspirone are not indicated for either disorder.REF: Table 247-1: Pharmacologic Management of Anxiety Disorders: Indications and Considerations A patient reports symptoms of restlessness, fatigue, and difficulty concentrating. The provider determines that these symptoms occur in relation to many events and concerns. What other things will the provider question this patient about? a. Ability to manage social situations b. Body image and eating habits c. Headaches and bowel habits d. Occupational performance This patient has symptoms consistent with generalized anxiety disorder (GAD) in which feelings occur in relation to many events. Patients with GAD often have headaches and irritable bowel syndrome. Phobias are linked to particular events and often include social situations. Patients with OCD tend to have eating disorders and difficulty with occupational and academic performance. Cranial nerves A gross screening for hearing is the whisper tests. Which cranial nerve is being tested when the nurse practitioner conducts this test? Cranial nerve V Cranial nerve VII Cranial nerve VIII Cranial nerve IV Alzheimer buttaro 193 A patient with dementia experiences agitation and visual hallucinations and is given haloperidol with a subsequent worsening of symptoms. Based on this response, what is the likely cause of this patient’s symptoms? a. Alzheimer’s disease b. Lewy body dementia c. Pseudodementia d. Vascular neurocognitive disorder Patients with Lewy body dementia may present with these symptoms and will have an increased sensitivity to neuroleptics; when given haloperidol for agitation, will actually get worse. The other causes do not have these characteristic symptoms and are not sensitive to neuroleptics in this manner. A patient with Alzheimer’s disease (AD) is taking donepezil to treat cognitive symptoms. The patient’s son reports noting increased social withdrawal and sleep impairment. What is the initial step to manage these symptoms? a. Encourage activity and exercise b. Prescribe a selective serotonin reuptake inhibitor c. Recommend risperidone d. Referral to a neurologist for evaluation Patients with AD may have improvement in depression with nonpharmacologic management, including exercise and increased activity. If this is not effective, an SSRI may be prescribed. Risperidone, and other antipsychotics should not be prescribed.REF: Management An elderly patient has symptoms of depression and the patient’s daughter asks about possible Alzheimer’s disease since there is a family history of this disease. A screening evaluation shows no memory loss. What is the initial step in managing this patient? a. Order brain imaging studies such as CT or MRI b. Perform genetic testing to identify true risk c. Prescribe a trial of an antidepressant medication d. Recommend a trial of a cholinesterase inhibitor drug Elderly patients with depression who do not have other signs of AD may be given a trial of antidepressant medications initially in order to evaluate these symptoms. Brain imaging studies are not indicated initially. Genetic testing is not indicated. Once the degree of depression is determined and if other symptoms appear, an anticholinesterase inhibitor may be ordered.REF: Clinical Presentation/Diagnostics Suicide buttaro chapter 8 9. Musculoskeletal Osteoarthritis buttaro 184 Morning stiffness, Bouchard’s nodes (PIP joints), Heberden’s nodes (DIP joints), and crepitus Morning stiffness lasting <30 minutes or stiffness that improves with activity common Most commonly affects the hips, knees, and cervical and lumbar spine Most commonly affects the hips, knees, and cervical and lumbar spine Questions A 45-year-old patient has mild osteoarthritis in both knees and asks about non-pharmacologic therapies. What will the provider recommend? a. Aerobic exercise b. Glucosamine with chondroitin c. Therapeutic magnets or copper bracelets d. Using a cane or walker Aerobic exercise helps with cardiovascular conditioning and weight reduction as well as improved range of motion, decreased pain, and strengthening of supporting structures. Randomized controlled studies have failed to demonstrate significant pain relief with glucosamine. Therapeutic magnets and copper have not been proven to be effective. A young patient with mild symptoms will not need assistive devices and should focus on conditioning. A patient who has osteoarthritis in the carpometacarpal joints of both thumbs asks about corticosteroid injections to treat symptoms. What will the provider tell this patient about this therapy? a. Corticosteroid therapy reduces inflammation and improves joint mobility b. Injections may be administered as needed up to 6 times per year c. Intra-articular injections provide significant pain relief for 3 to 4 months d. This treatment may cause a temporary increase in pain, warmth, and redness Intra-articular injections of corticosteroids are helpful in decreasing pain, but may cause a transient increase in pain, warmth, and redness. This therapy does not improve inflammation and joint mobility. Injections are not recommended more than 3 to 4 times per year. The duration of pain relief is variable. A 50-year-old woman reports pain in one knee upon awakening each morning that goes away later in the morning. A knee radiograph is negative for pathology and serum inflammatory markers are normal. What will the provider tell this patient? a. A magnetic resonance imaging study is necessary for diagnosis b. That the lack of findings indicates no disease process c. To take acetaminophen 1 gram three times daily for pain d. To use a cyclooxygenase 2-selective NSAIDs to reduce inflammation Acetaminophen is the mainstay for initial treatment of osteoarthritis. Radiologic findings are often negative in the early stages of the disease. There are no serologic markers for OA. A COX2-selective inhibitor has cardiovascular side effects and should not be used unless necessary. These agents are used more for pain than for inflammation.REF: Diagnostics/Management Rheumatoid arthritis buttaro 218 Which are symptoms of rheumatoid arthritis that distinguish it from osteoarthritis? Select all that apply. a. Extra-articular inflammatory signs b. History of injury to affected joints c. Morning stiffness of at least one hour d. Symmetric tender, swollen joints e. Unilateral joint involvement The clinical presentation of RA includes extra-articular symptoms, morning stiffness lasting at least one hour, and symmetric, bilateral joint involvement. OA often has a history of previous injury and is usually asymmetric and may be unilateral. A patient is diagnosed with rheumatoid arthritis after a review of systems, confirmatory lab tests, and synovial fluid analysis. What will the provide order initially to treat this patient? a. Disease-modifying anti-rheumatic drugs b. Long-term glucocorticoid therapy c. Non-pharmacological treatments d. Nonsteroidal anti-inflammatory drugs Treatment with DMARDs should be initiated as soon as the diagnosis of RA is established in order to achieve disease modification. Long-term glucocorticoid therapy is not recommended because of adverse effects. NSAIDs are not first-line drugs and increase the risk of cardiac and renal complications. Non-pharmacological treatments are used as adjunctive and not first-line therapy. A patient has swelling and tenderness in the small joints of both hands and reports several weeks of malaise and fatigue. A RF test is negative. What will the primary care provider do next? a. Begin treatment with a biologic disease-modifying anti-rheumatic drug b. Order radiographic tests, a CBC, and acute-phase reactant levels c. Reassure the patient that the likelihood of rheumatoid arthritis is low d. Refer the patient to an orthopedic specialist for evaluation and treatment The patient has signs of RA; the RF test may be negative initially, but will become positive in 70% to 80% of patients. The provider’s next step is to order tests to confirm the diagnosis and to provide a baseline to monitor disease progress and response to treatment. DMARDs may be ordered when the disease is confirmed. The PCP may treat in consultation with a rheumatologist who will order medications and will refer the patient for physical therapy, occupational therapy and psychotherapy. Low back pain buttaro 181 A patient has recurrent lumbar pain which is sometimes severe. The patient reports that prescription NSAIDs are no longer effective for pain relief. What will the provider recommend? a. Adjunctive treatment with physical therapy b. Beginning treatment with opioid analgesics c. Complementary and alternative therapies d. Referral to an interventional spine physician Patients with recurrent or chronic lower back pain may benefit from lumbar epidural corticosteroid injection performed by an interventional spine physician. Physical therapy is often used for acute injury if no improvement in 4 to 6 weeks. Opioid analgesics are not usually effective.REF: Spinal Interventional Procedures A patient reports severe back pain located in the lumbar spine. To evaluate whether the patient has axial pain or radicular pain, which assessment is necessary? a. Asking the patient to perform the Valsalva maneuver b. Assessing reflexes and asking about tingling or numbness c. Determining whether the pain is present with prolonged sitting d. Noting whether pain is mitigated with frequent position shifts Associated neurological signs are present with radicular pain and include numbness, tingling, weakness, and reflex changes. The other symptoms occur with both axial and radicular pain. A patient has an acute onset of lower back pain associated with lifting heavy objects at work. A physical examination reveals no loss of lower extremity function or neurological symptoms. What is the initial intervention for this patient? a. MRI to evaluate soft tissue involvement b. Plain radiographs to evaluate the extent of the injury c. Traction therapy to minimize complications d. Treatment with a nonsteroidal anti-inflammatory drug NSAIDs are appropriate as first-line treatment in patients without potential complications. Radiologic studies are performed if improvement does not occur in 4 to 6 weeks. Traction may be used for patients with radicular symptoms to help resolve neurological deficits, although systematic review of research has not clearly identified a benefit to this therapy.REF: Management 10. Hematology Iron deficiency anemia buttaro/ Anemia of chronic disease/ CBC indices A 20 kg child has iron-deficiency anemia and will begin taking an oral iron preparation. What will the provider teach the child’s parents about administration of this medication? a. Iron supplements should be given with food. b. The child must take the iron for 3 months. c. The correct dose is 30 mg twice daily. d. The iron is stopped when the hemoglobin increases. The dose for children is 3 mg/kg/day in divided doses. This child should get 60 mg/day, which is 30 mg/dose twice daily. Iron supplements are best absorbed on an empty stomach. Iron is given for at least 4 to 6 months. Hemoglobin levels will begin to increase in 1 to 2 weeks, but the iron is given until the serum ferritin increases sufficiently in 4 to 6 months. A 60-year-old female patient has recently lost weight and a physical examination reveals a beefy-red, sore tongue, with no neurological findings. Based on these clinical findings, what will the provider anticipate finding in the laboratory data? a. Decreased homocysteine levels b. Leukopenia and thrombocytopenia c. Low hemoglobin and elevated MCV d. Normal methylmalonic acid level Macrocytic anemia caused by vitamin B12 deficiency will have symptoms described above. Although folate acid deficiency causes macrocytic anemia, there are rarely any symptoms. Hemoglobin will be decreased and MCV will increase. Homocysteine levels will be increased. The patient with B12 deficiency will have leukopenia and thrombocytopenia with severe deficiency, characterized by neurologic findings, which this patient does not have. Methylmalonic acid level will decrease. A patient reports recent mild fatigue and palpitations. A complete blood count reveals a decreased hemoglobin level and a normal ferritin level. What other findings are likely to be present? a. Decreased hematocrit b. Decreased MCV, MCH, and MCHC c. Elevated total iron-binding capacity d. Paresthesias, koilonychia, and pica This patient has signs of milder iron-deficiency anemia and will also have a low hematocrit level. The RBC indexes are the last to change as the anemia becomes more severe. When the ferritin level drops, the TIBC will become elevated. Paresthesias, koilonychia, and pica occur with more severe anemia. 11. Genito-urinary Prostate disease kennedy chapter 11 , buttaro 147 Which ethnic group has the highest incidence of prostate cancer? A. Asians B. Hispanics C. African Americans D. American Indians Men with an initial PSA level below 2.5 ng/ml can reduce their screening frequency to what intervals? A. Every 6 months B. Yearly C. Every 2 years D. Every 2 to 4 years . All of the following may be reasons associated with an elevated PSA besides prostate cancer except: A. Prostatitis B. Urinary tract infection C. Perineal trauma D. Digital rectal exam In the diagnosis of acute bacterial prostatitis, a midstream urine culture is of benefit. To be diagnostic, the specimen should reveal how many white blood cells per high-power field? A. Five B. Ten C. Fifteen D. Twenty In chronic bacterial prostatitis, what is the organism most commonly associated with the disease? A. Klebsiella B. Proteus C. Pseudomonas D. Escherichia coli In acute prostatitis, an exam of the prostate may find the gland to be: A. Nodular B. Cool and pliable C. Swollen and tender D. Asymmetrical _All of the following antimicrobials may be indicated in chronic bacterial prostatitis except: A. Ciprofloxacin B. Levofloxacin C. Trimethoprim D. Azithromycin Mr. Jones is a 68-year-old retired Air Force pilot that has been diagnosed with prostate cancer in the past week. He has never had a surgical procedure in his life and seeks clarification on the availability of treatments for prostate cancer. He asks the nurse practitioner to tell him the side effects of a radical prostatectomy. Which of the following is NOT a potential side effect of this procedure? A. Urinary incontinence B. Impotence C. Dribbling urine D. Selected low back pain A 79-year-old man is being evaluated for frequent urinary dribbling without burning. Physical examination reveals a smooth but slightly enlarged prostate gland. His PSA level is 3.3 ng/mL. The patient undergoes formal urodynamic studies, and findings are as follows: a decreased bladder capacity of 370 mL; a few involuntary detrusor contractions at a low bladder volume of 246 mL; an increased postvoid residual urine volume of 225 mL; and a slightly decreased urinary flow rate. Which of the following is not consistent with a normal age-associated change? A. PSA level of 3.3 ng/mL B. Decreased bladder capacity C. Involuntary detrusor contradictions D. Increased postvoid residual urine volume A male patient reports nocturia and daytime urinary frequency and urgency without changes in the force of the urine stream. What is the likely cause of this? a. Bladder outlet obstruction b. Lower urinary tract symptoms c. Prostate cancer d. Urinary tract infection Lower urinary tract symptoms (LUTS) result from irritative changes in the lower tract. Bladder outlet obstruction causes hesitancy, decreased caliber and force of the urine stream, and post-void dribbling. Diagnosis of prostate cancer and UTI require further testing and are less likely causes. A 70-year-old male reports urinary hesitancy, post-void dribbling, and a diminished urine stream. A digital rectal exam reveals an enlarged prostate gland that feels rubbery and smooth. Which tests will the primary care provider order based on these findings? a. Bladder scan for post-void residual b. PSA and bladder imaging c. Urinalysis and serum creatinine d. Urine culture and CBC with differential The DRE reveals a prostate gland consistent with BPH. The primary provider should order a urinalysis and creatinine to evaluate possible infection and renal function. A bladder scan is ordered at the discretion of the urologist. The prostate exam isn’t consistent with prostate cancer, so PSA and bladder imaging are not necessary. Symptoms of prostatitis would indicate a need for evaluation of possible infection.REF: Diagnostics/Box 147-1: Diagnostics A patient has been taking terazosin daily at bedtime to treat BPH and reports persistent daytime dizziness. What will the provider do? a. Prescribe finasteride instead of terazosin b. Recommend taking the medication in the morning c. Suggest using herbal preparations d. Switch the prescription to doxazosin Patients who cannot tolerate the side effect of alpha-adrenergic antagonists, the provider may initiate therapy with a 5a-reductase inhibitor such as finasteride. Terazosin should be given at bedtime to minimize these adverse effects. Herbal preparations have not been proven to be safe or effective. Doxazosin is in the same drug class as terazosin. Urinary tract infection UTIs have six categories of classification: uncomplicated, complicated, isolated, unresolved, reinfection, and relapse. 2 UTIs are considered complicated if they include the presence of pyuria, positive urine culture, fever, or structural or functional abnormality of the urinary tract or if they occur in the presence of urinary catheterization. All UTIs in males are considered complicated. Common reasons for UTIs in men include prostatitis, epididymitis, orchitis, pyelonephritis, cystitis, and urethritis. A 30-year-old male patient has a positive leukocyte esterase and nitrites on a random urine dipstick during a well patient exam. What type of urinary tract infection does this represent? a. Complicated b. Isolation c. Uncomplicated d. Unresolved All UTIs in males are considered complicated, because the infection source is not secondary to ascending infection.REF: Definition and Epidemiology An asymptomatic pregnant woman has a positive leukocyte esterase and positive nitrites on a urine dipstick screening. What will the provider do next? a. Admit to the hospital b. Obtain a urine culture c. Order a renal ultrasound d. Prescribe trimethoprim-sulfamethoxazole Urine culture is the definitive test and should be obtained in all pregnant women. Admission to the hospital is usually not necessary. Renal ultrasound is used to identify abnormalities or obstructions that may be causing recurrent symptoms. TMP-SMZ is contraindicated in pregnant women.REF: Diagnostics/Management A fluoroquinolone (Ciprofloxin) is prescribed for a male patient with a UTI. What should the nurse practitioner teach the patient regarding taking this medication? A. It must be taken on an empty stomach B. Its effectiveness is decreased by antacids, iron, or caffeine ingestion C. It may cause a metallic aftertaste D. Its effectiveness is not a concern and it can be taken with any medications 12. Primary, Secondary and Tertiary Prevention Kennedy Chapter 2 An example of secondary prevention you could recommend/order for older adults would be to: A. Check for fecal occult blood B. Wear seat belts in the car C. Provide foot care for a diabetic patient D. Administer a tetanus shot Leo L. is a 62-year-old African American male who comes for an initial visit to your practice. Personal health history includes smoking 1 pack/day since age 11, consuming a case of beer (24 bottles) every weekend, and working as an assembler (sedentary job) for the past 10 years. Family history in first-degree relatives includes hypertension, high cholesterol, heart attack, and type 2 diabetes mellitus. Leo’s BMI is 32; BP today is 130/86. You order a fasting glucose, lipid profile, and return visit for BP check. This is an example of: A. Primary prevention B. Secondary prevention C. Tertiary prevention D. Health profiling Performing range of motion exercises on a client who has had a stroke is an example of which level of prevention? A. Primary prevention B. Tertiary prevention C. Secondary prevention D. Rehabilitation prevention The nurse practitioner demonstrates an understanding of primary prevention of falling among the elderly through which management plan? A. Evaluate a need for assistive devices for ambulation after the client has been injured from a fall. B. Provide resources to correct hazards contributing to falls in the home environment. C. Reinforce the need to use prescribed eyeglasses to prevent further injury from falls. D. Provide information about medications, side effects, and interactions. 13. Content from each Grand Round presentation- Recommended Screening and Immunizations MMUNIZATIONS Pneumovax: one time after age 65 Influenza: annually Hepatitis B: annually Herpes zoster: one time after ago 60 NR Tetanus: every 10 years CARDIOVASCULAR SCREENING Abdominal aorta ultrasound: once in every smoking man Hypertension: at each office visit, no age restriction CANCER SCREENING Colonoscopy: every 10 years after age 50, stopping at age 74 Fecal occult blood slides: annually until age 74 Breast: every 2 years until age 74 Prostate: insufficient evidence for age >75 Ivan W. is a 65-year-old man who is new to your practice. He has a history of COPD, CAD, hypertension, and type 2 diabetes mellitus. He has had no immunizations since his discharge from the military at age 25. Childhood diseases included chickenpox, measles, mumps, and “German measles.” He presents for a disease management visit. Which of the following immunizations would you recommend for Ivan? A. MMR, influenza, pneumococcal, Zostavax B. Influenza, pneumococcal, PPD, Hepatitis B C. Tdap, pneumococcal, influenza, Zostavax D. Hepatitis B, influenza, pneumococcal, Hepatitis A 2. A 50-year-old female patient has a blood pressure of 118/72 mm Hg, a negative family history for breast and ovarian cancer, a normal Pap smear 2 years prior, and a Framingham risk screening within normal limits. Which should be part of this patient’s routine annual well-patient exams? a. Bone mineral density screening b. Breast cancer screening and mammogram c. Cervical cancer screening with a Pap test d. Lipid screening and cholesterol tests ANS: B The American Cancer Society recommends yearly mammogram at age 40. Bone mineral density screening begins at age 50 to 64, based on risk. Cervical cancer screening should be performed every 3 years unless there is increased risk. Lipid screening and cholesterol is performed annually if there is increased risk according to the Framingham guidelines. REF: Table 17-1: Screening Tests for Women/Table 17-4: Comparison of American Cancer Society and USPSTF Screening Guidelines for the Early Detection of Cancer in Asymptomatic Individuals 3. A 55-year-old patient who had influenza in the previous influenza season asks about the flu vaccine. What will the provider tell the patient? a. Having influenza vaccine confers lifetime immunity b. The FluMist vaccine may be used each year c. The Fluzone High-Dose vaccine is recommended d. The trivalent influenza vaccine is indicated annually ANS: D Because the strains of influenza vary from year to year, annual immunization with TIV is indicated for all persons. Lifetime immunity is not conferred with infection. The Flu Mist is used in persons 50 years of age and younger. The Fluzone High-Dose vaccine is used in patients older than 65 year. REF: Influenza Vaccine [Show More]
Last updated: 2 years ago
Preview 1 out of 60 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 02, 2021
Number of pages
60
Written in
Additional information
This document has been written for:
Uploaded
Mar 02, 2021
Downloads
0
Views
93



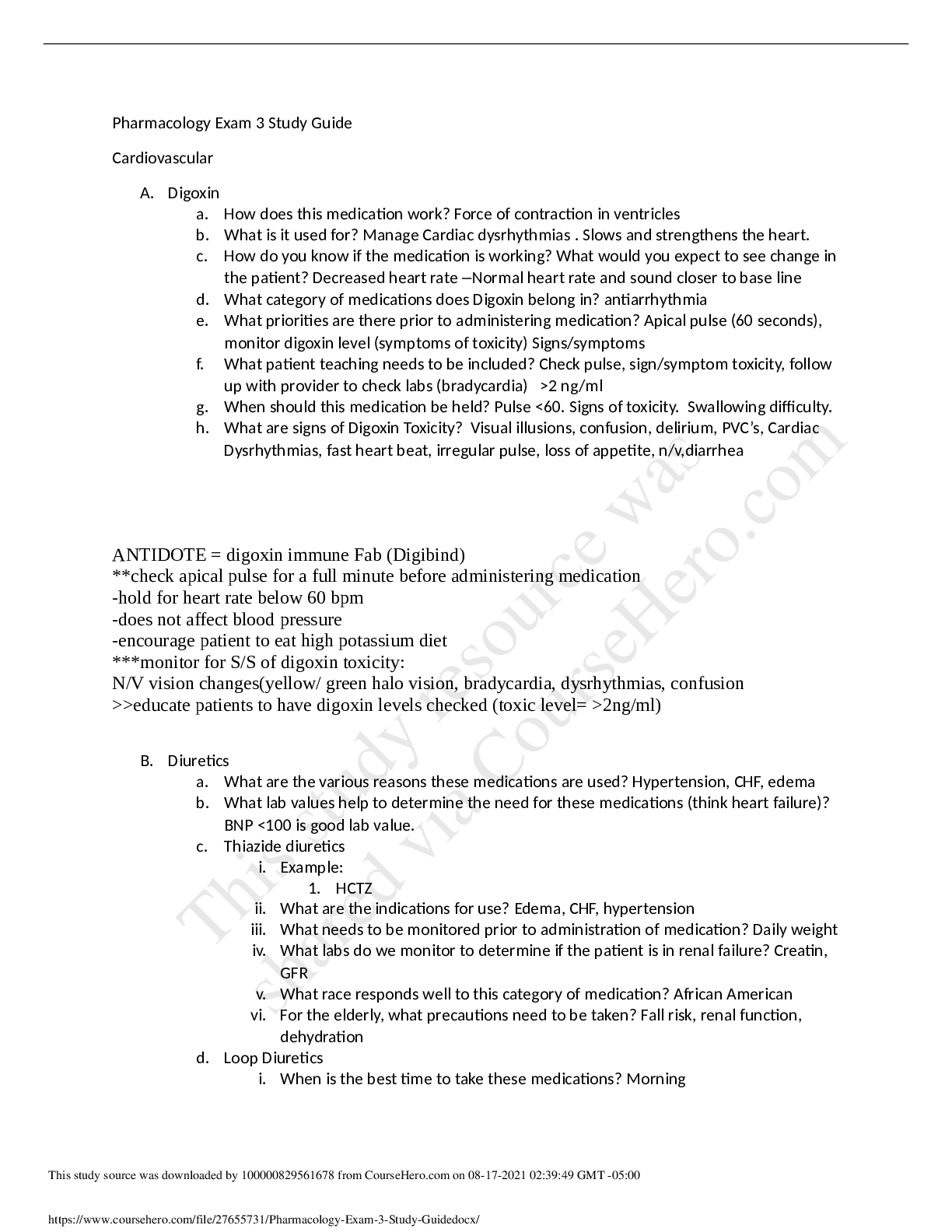


.png)