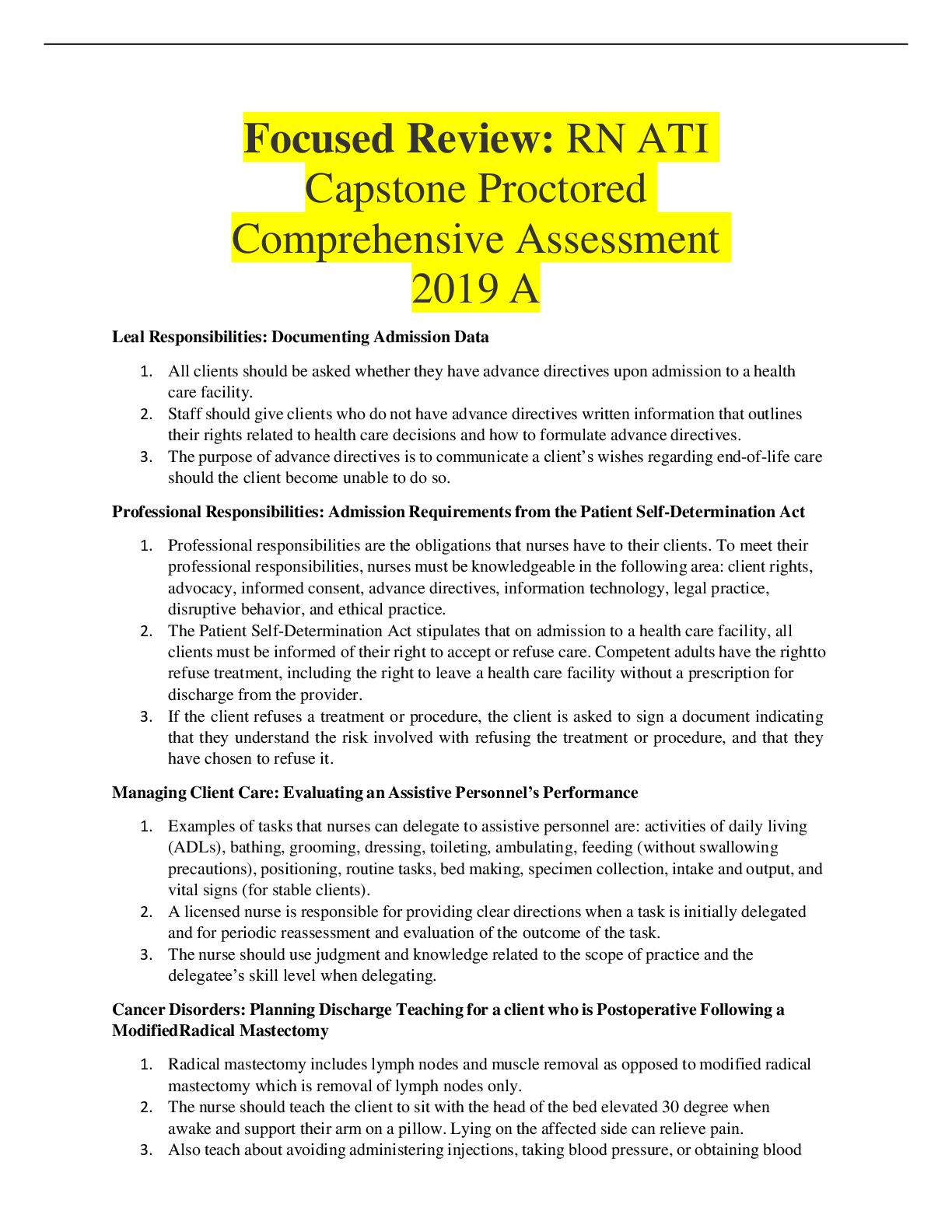
ATI MENTAL HEALTH STUDY GUIDE. Chapters 2-22. Best quick read guide towards exam.
Document Content and Description Below
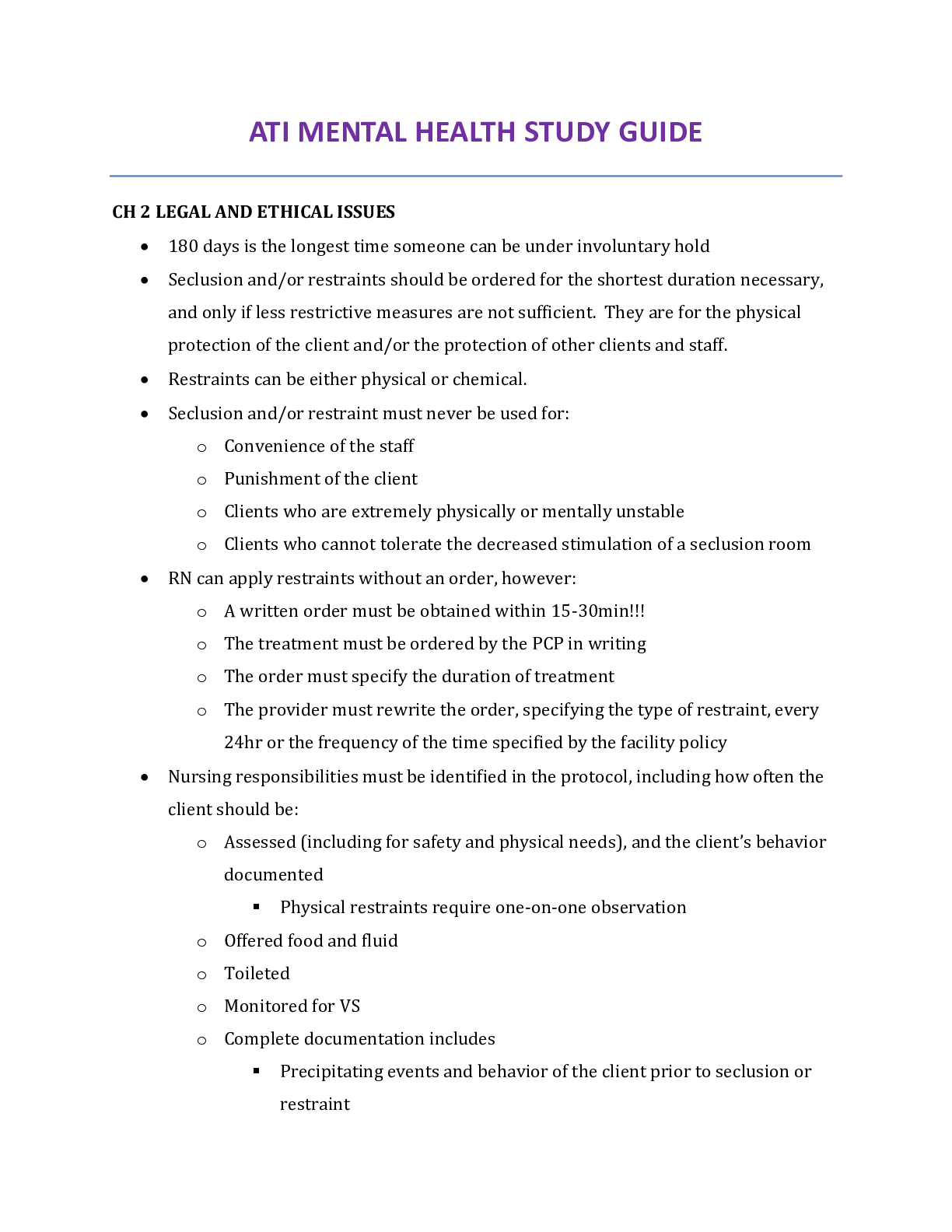
ATI MENTAL HEALTH STUDY GUIDE
CH 2 LEGAL AND ETHICAL ISSUES
• 180 days is the longest time someone can be under involuntary hold
• Seclusion and/or restraints should be ordered for the shortest
...
duration necessary, and only if less restrictive measures are not sufficient. They are for the physical protection of the client and/or the protection of other clients and staff.
• Restraints can be either physical or chemical.
• Seclusion and/or restraint must never be used for:
o Convenience of the staff
o Punishment of the client
o Clients who are extremely physically or mentally unstable
o Clients who cannot tolerate the decreased stimulation of a seclusion room
• RN can apply restraints without an order, however:
o A written order must be obtained within 15-30min!!!
o The treatment must be ordered by the PCP in writing
o The order must specify the duration of treatment
o The provider must rewrite the order, specifying the type of restraint, every 24hr or the frequency of the time specified by the facility policy
• Nursing responsibilities must be identified in the protocol, including how often the client should be:
o Assessed (including for safety and physical needs), and the client’s behavior documented
Physical restraints require one-on-one observation
o Offered food and fluid
o Toileted
o Monitored for VS
o Complete documentation includes
Precipitating events and behavior of the client prior to seclusion or restraint
Alternative actions taken to avoid seclusion or restraint
The time treatment began
The clients current behavior, what foods or fluids were offered and taken, needs provided for, and VS
Medication administration
• Tort
o False imprisonment confining a client to a specific area, sch as a seclusion room, is false imprisonment if the reason for such confinement is for the convenience of the staff.
o Assault making a THREAT to a client’s person, such as approaching the client in a threatening manner with a syringe in hand, is considered assault.
o Battery touching a client in a harmful or offensive way is considered battery. This would occur if the nurse threatening the client with a syringe actually grabbed the client and gave an injection.
CH 3 EFFECTIVE COMMUNICATION
• Nonverbal communication
o Nurses should be aware of how they communicate nonverbally. The nurse should assess the client’s nonverbal communications for the meaning being conveyed, remembering that culture impacts interpretation. Attention to the following behaviors is important, as it is compared to the verbal message being conveyed
Appearance
Posture
Gait
Facial expressions
Eye contact
Gestures
Sounds
Territoriality
Personal space
Silence
• Therapeutic communication is the PURPOSEFUL use of communication to build and maintain helping relationships with clients, families, and significant others.
• Characteristics of therapeutic communication include:
o Client centered – not social or reciprocal
o Purposeful, planned, and goal-directed
• Barriers to effective communication
o Asking irrelevant personal questions
o Offering personal opinions
o Giving advice
o Giving false reassurance
o Minimizing feelings
o Changing the topic
o Asking “why” questions
o Offering value judgments
o Excessive questioning
o Responding approvingly or disapprovingly
CH 4 STRESS AND DEFENSE MECHANISIMS
Adaptive use of defense mechanism helps people to achieve their goals in acceptable ways.
Defense mechanisms become maladaptive when they interfere with functioning, relationships, and orientation to realtity
Defense mechanisims
o Altruism dealing with anxiety by reaching out to others
A nurse who lost a family member in a fire is a volunteer firefighter
o Sublimation dealing with unacceptable feelings or impulses by unconsciously substituting acceptable forms of expression
A person who has feelings of anger and hostility toward his work supervisor sublimates those feelings by working out vigorously at the gym during his lunch period.
o Suppression voluntarily denying unpleasant thoughts and feelings
A person who has lost his job states he will worry about paying his bills next week.
o Repression putting unacceptable ideas, thoughts, and emotions out of conscious awareness
A person who has a fear of the dentist’s drill continually “forgets” his dental appointments.
o Displacement shifting feelings r/t an object, person, or situation to another less threatening object, person, or situation
A person who is angry about losing his job destroys his child’s fave toy
o Reaction formation overcompensating or demonstrating the opposite behavior of what is felt
A person who dislikes her sister’s daughter offers to babysit so that her sister can go out of town.
o Undoing performing an act to make up for prior behavior
An adolescent completes his chores without being prompted after having an argument with his parent.
o Rationalization creating reasonable and acceptable explanations for unacceptable behavior
A young adult explains he had to drive home from a party after drinking alcohol because he had to feed his dog.
o Dissociation temporarily blocking memories and perceptions from consciousness
An adolescent witnesses a shooting and is unable to recall any details of the event.
o Splitting demonstrating an inability to reconcile negative and positive attributes of self or others
A client tells a nurse that she is the only one who cares about her, yet the following day, the same client refuses to talk to the nurse.
o Projection blaming others for unacceptable thoughts and feelings
A young adult blames his substance use disorder on his parent’s refusal to buy him a new car
o Denial pretending the truth is not reality to manage the anxiety of acknowledging what is real
A parent who is informed that his son was killed in combat tells everyone he is coming home fro the holidays.
o Regression demonstrating behavior from an earlier developmental level; often exhibited as childlike or immature behavior
A school-age child begins wetting the bed and sucking his thumb after learning his parents are separating.
Anxiety
o Levels of anxiety
Mild
• Occurs in the normal experience of everyday living
• It increases one’s ability to perceive reality
• There is an identifiable cause of the anxiety
• Other characteristics include:
o Vague feeling of discomfort
o Restlessness
o Irritability
o Impatience
o Apprehension
• The client may exhibit behaviors such as finger- or foot-tapping, fidgeting, or lip-chewing as mild tension-relieving behaviors.
Moderate
• Occurs when mild anxiety escalates
• Slightly reduced perception and processing of information occurs, and selective inattention may occur
• Ability to think clearly is hampered, but learning and problem solving may still occur
• Other characteristics include:
o Concentration difficulties
o Tiredness
o Pacing
o Change in voice pitch
o Voice tremors
o Shakiness
o Increased HR and RR
• The client may report somatic complaints including headaches, backache, urinary urgency and frequency, and insomnia
• The client with this type of anxiety usually benefits from the direction of others
Severe
• Perceptual field is greatly reduced with distorted perceptions
• Learning and problem solving do not occur
• Functioning is ineffective
• Other characteristics include:
o Confusion
o Feelings of impending doom
o Hyperventilation
o Tachycardia
o Withdrawal
o Loud and rapid speech
o Aimless activity
• The client with severe anxiety usually is not able to take direction from others
Panic-level
• Characterized by markedly disturbed behavior
• The client is not able to process what is occurring in the environment and may lose touch with reality The client experiences extreme fright and horror
• The client experiences severe hyperactivity or flight
• Immobility can occur
• Other characteristics may include:
o Dysfunction in speech
o Dilated pupils
o Severe shakiness
o Severe withdrawal
o Inability to sleep
o Delusions
o Hallucinations
CH 5 CREATING AND MAINTAINING A THERAPEUTIC AND SAFE ENVIRONMENT
Transference occurs when the client views a member of the health car team as having characteristics of another person who has been significant to the client’s personal life.
o Example: A client may see a nurse as being like his mother, and thus may demonstrate some of the same behaviors with the nurse as he demonstrated with his mother.
o Nursing implication: A nurse should be aware that transference by a client is more likely to occur with a person in authority
Countertransference occurs when a health care team member displaces characteristics of people in her past onto a client.
o Example: A nurse may feel defensive and angry with a client for no apparent reason if the client reminds her of a friend who often elicited those feelings.
o Nursing implication: A nurse should be aware that clients who induce very strong personal feelings may become objects of countertransference.
CH 7 PSYCHOANALYSIS, PSYCHOTHERAPY, AND BEHAVIORAL THERAPIES
Psychoanalysis a therapeutic process of assessing unconscious thoughts and feelings, and resolving conflict by talking to a psychoanalyst.
o Past relationships are a common focus for therapy
Psychotherapy involves more verbal therapist-to-client interaction than classic psychoanalysis
o Client and therapist develop a trusting relationship
o Psychodynamic psychotherapy employs the same tools as psychoanalysis; but focuses more on the client’s present state rather than his early life.
o Interpersonal psychotherapy (IPT) assists clients in addressing specific problems. It can improve interpersonal relationships, communication, role-relationship, and bereavement.
o Cognitive therapy is based on the cognitive model, which focuses on individual thoughts and behaviors to solve current problems. It treats depression, anxiety, eating disorders, and other issues that can improve by changing a client’s attitude toward life experiences.
o Behavioral therapy is based on the theory that behavior is learned and has consequences. Abnormal behavior results from an attempt to avoid painful feelings. Changing abnormal or maladaptive behavior can occur without the need for insight into the underlying cause of the behavior.
Has been successful in treating clients who have phobias, substance use or addictive disorders, and other issues.
CH 9 STRESS MGMT
Stress is the body’s nonspecific response to any demand made upon it.
Anxiety and anger are damaging stressors that cause distress
General Adaptation Syndrome (GAS) is the body’s response to an increased demand
o 1st stage “fight or flight”
o if stress is prolonged maladaptive responses can occur
Acute Stress
o Apprehension
o Unhappiness or sorrow
o Decreased appetite
o Increased RR, HR, CO, and BP
o Increased metabolism and glucose use
o Depressed immune system
Prolonged stress (Maladaptive response)
o Chronic anxiety or panic attacks
o Depression, chronic pain, sleep disturbances
o Weight gain or loss
o Increased risk for MI, stroke
o Poor diabetes control, htn, fatigue, irritability, decreased ability to concentrate
o Increased risk for infection
CH 10 BRAIN STIMULATION THERAPIES
ECT
o Uses electrical current to induce brief seizure activity while the client is anesthetized
o Indications:
MDD
• Clients whose manifestations are not responsive to pharmacological treatment
• Clients who are actively suicidal or homicidal and for whom there is a need for rapid therapeutic reponse
• Clients who are experiencing psychotic manifestations
Schizophrenia
• Spectrum disorders that are less responsive to neuroleptic medications, such as schizoaffective d/o
Acute Manic Episodes (Bipolar)
• ECT is used for clients who have bipolar d/o with rapid cycling (4 or more episodes of acute mania within 1 yr) and very destructive behavior
• Both of these features tend to respond poorly to lithium therapy.
• These clients receive ECT and then a regimen of lithium therapy.
o Contraindications:
No absolute contraindications for this therapy if it is deemed necessary to save a client’s life
Conditions that place client’s at a higher risk if ECT is used:
• Recent MI
• Hx of CVA
• Cerebrovascular malformation
• Intracranial mass lesion
• Increased intracranial pressure
o Mental health conditions for which ECT has not been found useful include:
Substance abuse
Personality d/o
Dysthymic d/o
Cyclothymia
Anxiety
o Nursing actions
Prepare the client
• Typical course of ECT is 3 x a week for a total of 6-12 tx
• Provider obtains informed consent
• Medication mgmt.
o Any medications that affect the client’s seizure threshold must be decreased or discontinued several days prior to ECT procedure
o MAOIs and Lithium should be d/c 2 weeks prior to ECT
• Severe HTN should be controlled b/c a short period of HTN occurs immediately after the ECT procedure
• Any cardiac conditions, such as dysrhythmias, should be monitored and treated before the procedure
• The RN monitors VS and mental status before and after
• RN assesses the client’s and family’s understanding and knowledge of the procedure and provides teaching as necessary
• 30 min prior to the beginning of the procedure, an IM injection of atropine sulfate or glycopyrrolate (Robinul) is given to decrease secretions and counteract any vagal stimulation
• An IV line is inserted and maintained until full recovery
Ongoing care
• ECT is administered early in theAM after the client has fasted for a prescribed period of time
• A bite guard should be used to prevent trauma
• Electrodes are applied for EEG monitoring
• Client is mechanically ventilated and receives 100% O2
• Ongoing cardiac monitoring is provided, including BP, ECG, and oxygen saturation
• An anesthesia provider administers a short-acting anesthetic, such as methohexital (Brevital), via IV bolus
• A muscle relaxant is administered, succinylcholine (Anectine)
• A cuff is placed on one leg or arm to block the muscle relaxant so that seizure activity can be monitored in the lib distal to the cuff
• An electrical stimulus is typically applied for 0.2-0.8 sec; enough to cause a 25-60 sec seizure
• After seizure activity has ceased, anesthetic is d/c and the client is extubated and assisted to breathe voluntarily
Postprocedure Care
• Client is transferred to recovery where LOC, cardiac status, VS, and oxygenation continue to be monitored
• Client is positioned on his side to facilitate drainage and prevent aspiration
• Client is monitored for ability to swallow and return of the gag reflex
• The client is usually awake and ready for transfer back to the mental health unit or other facility within 30-60 min after the procedure.
o Complications
Memory loss and confusion
• Short-term memory loss, confusion, and disorientation may occur immediately following the procedure.
Transcranial Magnetic Stimulation
o TMS is a noninvasive therapy that uses magnetic pulsations to stimulate specific areas of the brain. “wakes the brain up”
o Indications:
MDD clients who are nonresponsive to pharmacologic tx
o Nursing Actions
Educate the client
• Daily for 4-6 wks
• can be performed as an outpatient
• lasts 30-40 min
• A noninvasive electromagnet is place on the client’s scalp, allowing the magnetic pulsations to pass through
• Client is alert during the procedure
o Complications
Common adverse effects include mild discomfort or a tingling sensation at the site of the electromagnet
Seizures are a rare but potential complication
Vagus Nerve Stimulation
o VNS provides electrical stimulation through the vagus nerve to the brain through a device that is surgically implanted under the skin on the client’s chest.
o VNS is believed to result in an increased level of NT
o Indications:
Depression that is resistant to pharmacological treatment and/or ECT
o Nursing Action:
Educate the client about VNS
• Performed as an outpatient surgical procedure
• Delivers around-the-clock programmed pulsations
• Client can turn off the VNS device at any time by placing a special external magnet over the site of the implant
Assist provider in obtaining informed consent
o Complications
Voice changes due to the proximity of the implanted lead on the vagus nerve to the larynx and pharynx
Other potential adverse effects include hoarseness, throat or neck pain, dysphagia; usually improve with time
Dyspnea with exertion is possible; therefore, the client may want to turn off the VNS during exercise.
CH 11 ANXIETY DISORDERS
Elevated or persistent anxiety can result in anxiety disorders causing behavior changes and impairment in functioning.
Anxiety levels can be:
o Mild restlessness, increased motivation, irritability
o Moderate agitation, muscle tightness
o Severe inability to fxn, ritualistic behavior, unresponsive
o Panic distorted perception, loss of rational thought, immobility
Recognized anxiety d/o include:
o Separation anxiety d/o the client experiences excessive fear or anxiety when separated from an individual to which the client is emotionally attached
o Panic d/o the client experiences recurrent panic attacks
o Phobias the client fears a specific object or situation to an unreasonable level
o Generalized anxiety d/o the client exhibits uncontrollable, excessive worry for more than 3 months.
o Not recognized as anxiety d/o by DSM-5
Obsessive-compulsive and related d/o
• OCD the client has intrusive thoughts of unrealistic obsessions and tries to control these thoughts with compulsive behaviors
• Hoarding d/o the client has difficulty parting with possessions, resulting in extreme stress and functional impairments
Trauma- and stressor-related d/o
[Show More]
Last updated: 3 years ago
Preview 1 out of 40 pages

.png)


.png)