NURSING 3SS3 Care Scenario 3 Readings
Chapter 16 Nursing management during post partum period (25 pages) 474-498
Sara - 479.5-485
Emotional status: assess how she interacts with family, her level of independence, ener
...
NURSING 3SS3 Care Scenario 3 Readings
Chapter 16 Nursing management during post partum period (25 pages) 474-498
Sara - 479.5-485
Emotional status: assess how she interacts with family, her level of independence, energy levels, eye contact with infant, posture and comfort level while holding the newborn, sleep and rest patterns
Bonding and attachment:
- Identify family discord that might interfere with the attachment process
- Mothers from different cultures may behave differently from what is expected in your own culture
- Engaging in conversation with the woman regarding different practices can be helpful
- Bonding: close emotional attraction to a newborn by the parents that optimally develops during the first 30-60minutes after birth – unidirectional, from parent to infant
o Optimal bonding of the parents to a newborn requires a period of close con within the first few minutes to a few hours after birth
o Mother initiates bonding when she caresses her infant and exhibits certain behaviours typical of mother tending to her child – skin to skin contact is encouraged as soon after the birth as possible
o Infant responds with body and eye movements – looks at the mother
o Length and time of bonding depends on health of infant and mother
- Attachment: development of strong affection between an infant and a significant other (mother, father, sibling, caretaker)
o Follows a progressive or developmental course that changes over time
o Individualized and multifactorial process
o Occurs thru mutually satisfying experiences
o Maternal attachment begins during pregnancy and continues thru birth and postpartum periods
o Attachment behaviours: seeking, staying close to, and exchanging gratifying experiences with the infant
o Can be complicated by premature birth
- Bonding is important in attachment
- Mothers “explore” their infants by touching their face, extremities and stroking the infant with their fingers and then followed by palm contact on the trunk and then mother draws their infant toward them and holds the infant
- En face position: mothers interact with their infants thru eye to eye contact in this position
- Process for fathers is similar to that of mothers
- Attachment for the father increase as the baby responds to him
- Include the father in teaching and care for the infant
- Attachment is a process and doesn’t occur instantly
- Midwives teach fathers to massage their partners which has been proven to have positive effect on pregnancy, labour, bonding and attachment
- The developmental task for the infant is learning to differ between trust and mistrust
- If the caretaker is responsive to care and meets the baby’s needs, the infant will trust the caretaker and view the world as a safe place and grow up to be secure, self reliant, trusting, cooperative and helpful
- Transition to parenthood: affected by environment, fam dynamics, and partners
o Commitment, attachment and preparation for infant during pregnancy (includes choice of care provider, prenatal instruction)
o Acquaintance with and increasing attachment ot infant, learning how to care for infant and physical restoration during the first weeks after birth
o Moving toward a new normal routine in the first 4 months after birth
o Achievement of parenthood role around 4 months where mothers have integrated the role of parent into their lives
Factors affecting attachment:
- Parents background – care they received, culture, relationship in family, previous pregnancies, postpartum depression
- Infant: health at birth
- Care practices: behavioursof doctors, midwives, nurses, hospital personnel; care and support during labour
- Attachment occurs more readily with the infant whose temperament, health, appearance and gender fits the parent’s expectations
- If the infant doesn’t meet the expectations, they may grieve the loss of the fantacy that they had about the infant during pregnancy
- Factors associated with the health care facility: separation of infant and parents after birth, policies that discourage unwrapping and exploring the infant, intensive care environment, staff indifference or lack of support for caretaking attempts and abilities
Critical attributes of attachment:
- Bonding: the initial connection
- Attachment: reciprocal process that continues to develop as mutually satisfying interactions occur between parents and child
- Parents who are responsive to their infant’s cues will promote the infants development and growth
- Maternal behaviours that facilitate attachment:
o Fingertipping: explore face, fingers and toes with fingertips
o Stroking baby’s chest with her palm
o Beginning to identify specific features of infant including resemblance to family members
o Speaking to the infant in a high pitched and soothing voice and referring to it as its gender rather than as “it”
- Parents place infant at centre of their lives
Positive behaviours: close physical contact, eye to eye contact, speaking in soft high pitched tones, touching and exploring the infant
- Infant smiles, alert, strong grasp reflex, sucks well, feeds easily, enjoys being held close, eye to eye contact, follows parents face
Negative behaviours: disappointment in the infant, fails to explore infant, fails to claim infant as part of family, avoids caring for infant, finds excuses not to hold infant close, uninterested in having infant in the room
- Infant feeds poorly, regurgitates often, cries for long periods, colicky and inconsolable, flat affect, rarely smiles, resists holding and closeness, sleeps with eyes closed most of the time, stiffens body when held, unresponsive to parents
Nursing interventions: less is more
- Vaginal may be discharged in 24 hours or less depending on condition and preferences
- Caesarean birth may remain hospitalized for 72 hours
- Use this time to address pain, immunizations, nutrition, activity and exercise, lactation, discharge teaching, sexuality and contraception, follow up
See page 158 and 159 for nursing care plan
Providing optimal cultural care:
- Aboriginal women from remote areas are encouraged to relocate to major centres to await the birth of their child since their home communities are not seen as having appropriate resorurces to delivery babies – the women may experience cultural isolation
- There are now new model of care so they stay in their homes and are attended to by midwives or physicians locally – develop resources in these communities
- Childbearing practices and beliefs vary across cultures – dietary restrictions, clothes, taboos, activities for maintaining mental health, silence, prayer, meditation
Cultural influences during postpartum period:
- French Canadian: European and aboriginal; speaking French may help if possible
o La culbute: parent holds baby above crib and rotates him or her in hopes the infant will sleep during the night and be awake in the day
- First nations: communicate with them to find out their cultural practices
o Extended family is important so consider accommodations
o Attempt to accommodate traditional native healing practices when possible to foster harmony
- Asian: korea, china, japan, Philippines, southeast asia
o Family is a core value and honour and harmony
o More protective behaviour of their children
o Japanese: cleanliness and protection from cold, daily bating, infants kept in quiet clean warm place for first month of life; breastfeeding is primary feeidng method; many women stay in parents home for 1-2 months; bathing can be family activity at home
o Filipino: grandparents often assist in care of their grandchildren; breastfeeding is encouraged, and some breastfeed for up to 2 years; women have difficulty discussing birth control and sexual matters; strong religious beliefs prevail and bedside prayer is common; families are close knit and numerous visitors can be expected at hospital
- Hispanic: Latin America, central America, south America
o Woman makes decisions as it is her role to care for women and children
o Extended fam members are consulted before the medical community in case of illness; home remedies and fold remedies may be valued
- Mexican: newborn’s grandmother lives with mother for several weeks to help; more women breastfeed more than 1 years; infant is carried in a shawl so there is easy access to breastfeeding; women may avoid eye contact and may not feel comfortable being touched by a stranger; some women may bring religious things into the room and display them
- Muslim: they are patriarchal but within the marriage, the woman may have considerable influence over decision making
o Birth of the child is welcomed and it promotes family status
o Muslim women are concerned with modesty so they may prefer female birth attendants only
o Not permitted to eat pork so check food items
o Male-female touching is prohibited except in an emergency situation
o Woman stays in house for 40 days after birth being cared for by female family members
o Most will breastfeed but some religious events call for fasting which can increase risk of dehydration or malnutrition
o Woman are exempt from 5x daily prayers as long as lochia is present
o Extended family is present thru much of the hospital stay
Promoting comfort:
- Many women will have pain from episiotomy, lacerations, edematous perineum, inflamed hemorrhoids, engorged breasts, afterbirth pains bc of uterine contractions in breastfeeding, sore nipples
- Apply cold and heat:
o Ice pack after vaginal birth during fouth stage of labour and for the first 24 hours; 20 minutes on, 10 minutes off
o Peri bottle: warm tap water in a bottle sprayed over perineal area after each voiding and before applying a new pad- direct the water flow from front to back
o After the first 24 hours, a sitz bath with warm water may be prescribed and substituted for the ice pack to reduce swelling and promote comfort – this enhances circulation and healing
Basin that fits on the commode; a bag with warm water is hung on a hook and connected via a tube onto the front of the basin
Use several times daily for hygiene and comfort
- Topical preparations: anesthetic spray to numb the area after the peri bottle or sitz bath
- Analgesics: Tylenol, NSAIDs like ibuprofen to relieve mild postpartum discomfort
o Moderate to severe pain: narcotic like codeine or oxycodone with aspirin or acetaminophen – instruct about adverse effects like dizziness, lightheadedness, nausea, vomiting, constipation, urinary retention, myoclonus, sedation
o Inform that drugs are secreted into breastmilk and most meds that mother takes are passed into the milk but acetaminophen and ibuprofen and other mild analgesics are considered relatively safe for breastfeeding mothers
Assisting with elimination:
- The bladder is edematous, hypotonic and congested postpartum so bladder distention, incomplete emptying and inability to void are common
- A full bladder interferes with uterine contractions and may lead to hemorrhage so encourage mom to void often – if this is difficult, use warm water over the area, listen to running water, take a warm shower, drink fluids, place hand in basin of warm water
- Catheterization may be needed if they don’t pee in 4-6 hours
- Decreased bowel motility during labour, high iron content in prenatal vitamins, postpartum fluid loss and pain meds may make a woman constipated and the mom may fear that bowel movements will cause pain or injury
- Use a stool softener like docusate with or without a laxative
- Ambulate frequently, increase fluid and fibre intake
- Eat fruits and veggies, drink 8-12 cups of fluids daily
Promoting activity rest and exercise:
- Promote importance of physical fitness
- The lifestyle changes that occur postpartum may affect health for decades
- Early ambulation is encouraged to reduce risk of thromboembolism and improve strength
- Fatigue should be assessed as a symptom for post partum depression or a thyroid condition but fatigue is normal postpartum
- Suggestions for adequate rest:
o Nap when baby naps; reduce participation in outside activities and limit vititors; determine infants sleep wake cycles and attempt to increase wakefulness during the day so baby sleeps longer at night; eat a balanced diet; share household tasks; ask father or other family to provide care during the night sometimes so you can sleep
- Demands of parenthood may reduce or prevent exercise but walking at a fast pace or pushing baby in stroller are great ways to maintain healthy exercise
- Emphasize benefits to a regular exercise program: lose pregnancy weight, increase energy levels, speed return to pre-pregnant size and shape; provides an outlet for stress
- Breastfeeding and exercise can control weight in long term
- Challenges to exercising: ligament laxity, competing demands (newborn care), lack of information about weight retention (lack of activity equates to weight gain) and stress incontinence (leaking of urine during activity)
- Uncomplicated vaginal birth: resume exercise in the immediate postpartum period
- Caesarean: follow advice of physician; start slowly
- Suggest jogging strollers, exercise videos, home exercise equipment
- Exercising after birth promotes feelings of wellbeing and restore muscle tone lost during pregnancy
- Walking is great exercise as long as woman avoids jarring and bouncing movements bc joints don’t stabilize until 6-8 weeks postpartum
- Exercising too much too soon can cause more bleeding and bright red lochia
- Recommended exercises for first few weeks: abdominal breathing, head lifts, modified sit ups, double knee roll, pelvic tilt
Abdominal breathing:
- Lie on flat surface and take a deep breath thru nose and expand abdo muscles
- Slowly exhale and tighten abdo muscles for 3-5 seconds
Head lift:
- Lie flat with knees flexed and feet flat
- Lift head off flat surface, tuck it onto your chest and hold for 3-5 seconds
- Relax head and return to starting position
Modified sit ups:
- Life flat and raise head and shoulders 14-18cm so your outstretched hands reach your knees
- Keep waist on flat surface
- Slowly return to starting position
Double knee roll:
- Lie flat with knees bent
- Keep shoulders flat and slowly roll your knees to your right side to touch the flat surface
- Rolls knees back over body to the left side until they reach the flat surface
- Go back to starting position
Pelvic tilt:
- Lie on back on flat surface with knees bent and arms at side
- Slowly contract abdo muscles while lifting pelvis up towards celiing
- Hold for 3-5 seconds and slowly return to starting position
Preventing stress incontinence: (urine loss associated with coughing, sneezing, laughing or lifting)
- Due to weak pelvic floor muscles and supportive tissue
- More vaginal deliveries, more likely to have this
- Walk, bike, swim, low impact aerobics
- Start kegel exercises
- Lose weight if necessary bc obesity is associated with stress incontinence
- Avoid smoking and limit alcohol and caffeine intake
- Kegel exercises: strengthen pelvic floor muscles bc they facilitate structural support and maintain the bladder neck in position so as not to leak during increases in intraabdominal pressure
o Women can do this, doing 10 5-second contractions whenever they change diapers, talk on the phone or watch TV
o Identify the correct pelvic floor muscles by contracting them to stop the flow of urine while sitting on toilet
o Repeat this several times to get familiar with it
o Start by emptying bladder
o Tighten pelvic floor muscles and holdfor 10 seconds
o Relax muscle completely for 10 seconds
o Perform 10 exercises at least 3 times daily and progressively increase
o Perform the exercises in different positions like standing, lying and sitting
o Keep breathing during the exercises
o Don’t contract your abdo, thigh, leg or butt muscles during these
o Relax while doing kegels and concentrate on isolating the right muscles
o Attempt to tighten your pelvic muscles before sneezing, jumping or laughing
Assisting with self care measures:
- Talk about how to prevent infection by frequently changing peri pads and applying and removing them front to back, avoid using tampons, shower once or twice daily using milk soap, use sitz bath after every bowel movement , use peri bottle with warm water after urination, wash hands before changing peri pads
- For hemorrhoids, have the client apply a witch hazel-soaked pad, ice packs or hemorrhoidal cream
Ensuring safety:
- Orthostatic hypotension: check BP before ambulating client, elevate head of bed for a few minutes before ambulating, have client sit on side of bed for a few moments before getting up, help client stand up, ambulate alongside client and provide support if needed, frequently as how her head feels
- Instruct woman to put newborn back into the crib if she is feeling sleepy – don’t fall asleep holding the baby
Counselling about sexuality and contraception:
- Most couples wait 4-6 weeks after delivery before having sex
- Fatigue, physical demands by infant and the stress of new roles and responsibilities may stress the emotional reserves of couples
- Body needs time to recover
- Body image issues may be a factor
- New parents don’t get as much pricacy
- Sexual intercourse can be resumed once bright-red bleeding has stopped and perineum has healed after an episiotomy or laceration (3-6 weeks postpartum)
- Determine what knowledge and concerns the couple has – inform them that fluctuations in sexual interest are normal
- Educate on how to prevent discomfort – vaginal lubrication may be impaired so use a water based gel lubricant
- Pelvic floor exercises help enhance sensation
- Contraceptive options should be included in the discussion – advice them to use a barrier method (condom with spermicidal gel or foam) until they choose another form of contraceptive
- Emphasize that there is still a chance to become pregnant when women are breastfeeding and experiencing amenorrhea
Promoting nutrition:
- Encourage mom to take good care of herself and eat a healthy diet so that the nutrients lost during pregnancy can be replaced and she can return to a healthy weight
- Eat a variety of foods with high nutrient density
- Eat meals with little or no prep
- Avoid high fat fast foods
- Drink about 2500 mL per day
- Avoid fad weight reduction diets
- Avoid excessive intake of fat, sugar and caffeine
- Follow Canada’s food guide (7-8 services of fruits and veggies; 6-7 grain products; 2 servings milk; two servings of meat; 30-45mL of unsaturated oils and fats
- Breastfeeding nutritional needs are higher than during pregnancy – it influences the quality of breast milk
- Some women require an extra 2 servings daily of certain food groups
- Breastfeeding mothers should take a daily multivitamin that contains -.4mg of folic acid
Supporting woman’s choice of feeding method:
- Many mothers choose formula
- Nurses must be able to deliver sound, evidenced based info to help the new mother choose the best way to feed her infant and must support her in her decision
- Factors that affect choice of feeding method: culture, employment demands, support from significant others and family, knowledge base
- Make sure couples have the info they need to make an informed decision
- Women who should not bresatfeed: antithyroid drugs, antineoplastic drugs, alcohol, street drugs – enter breastmilk and harm infant
- Many meds are considered safe in the context of breastfeeding but not all
- HIV positive women should not breastfeed
- Babies who should not breastfeed: inborn error of metabolism like galactosemia or PKU
- Other contraindications: a current pregnancy, serious mental health disorder that would prevent mother from remembering to feed infant consistently
Recommendations for breastfeeding
- Breastfeed all full term newborns
- Exclusive breastfeeding for first 6 months
- Breastfeeding up to 2 years is optimal
- After birth all new borns should be quickly dried assessed and placed skin to skin with mother – provides physiologic stability, warmth and opportunities for the first feed
- Policies that should be in place: have a breastfeeding policy, inform all women about benefits of breastfeeding, show mothers how to initiate breastfeeding within 30 mins of birth, give no food or drink other than breastmilk to all newborns, encourage breastfeeding on demand, allow now pacifiers to be given to breastfeeding infants, practice rooming in 24 hours daily
- Encourage mothers to believe in themselves and their ability to accomplish successful breastfeeding – make sure they know it takes time and practice
- Instruct mother to wash hands before starting
- Afterpains will increase during breastfeeding
- Make sure mother is comfy and pain free and not hungry
- Start feeding with an awake and alert infant who is showing hunger signs
- Urge mother to relax and encourage letdown reflex
- Have mother lightly tickle infants upper lip with nipple to stimulate infant to open mouth wide
- Bring baby rapidly only breast with wide open mouth
- Tell her to listen for sucking noise
- Use a finger to break the suction
- Show how to burp infant between breasts
- Show diff positions
- Reinforce and praise mother for her efforts
Providing assistance with bottle-feeding:
- Some women experience guilt and stigmatization as a result of the decision to feed infant with formula
- Discuss types of formula with parents
- Caution regarding soy formula in cases in which there is no cultural reasons to avoid cows milk or no allergy to cows milk – there can be long term consequences for infant like hormonal disturbances or thyroid malfunction due to exposure to soy products
- Educate on how to maintain asepsis, sterility and concentration of formula
- Commercial formula can be powdered (must be mixed with water0, condensed liquid (must be diluted with water0 and prepackaged (ready to be used in disposable bottles)
- Infant will need 150-200mL per day of formula milk per kg of body weight each day
- Newborn only needs 30-60mL per feed for first week of life but will increase to 90-120mL per feed by 1 month of age and 120-180mL per feed from 2-6 months; after this, 180-220mL at each feeding
- Babies cues to feed: rooting, crying
- After 6 months, the number of feeding declines to accommodate other foods in the baby’s diet like fruits, cereals, veggies
- Guidelines:
o Make feeding relaxing time and promote bonding
o Always hold newborn when feeding and hold the baby close
o Tilt bottle so nipple and neck are always filled with formula – prevents taking in too much air
o Stimulate sucking reflex by touching nipple to infants lips
o Look for expiry dates
o Refrigerate any powdered formula that has been combined with tap water after constitution
o Discard any formula not taken and don’t save it for future feedings
o Follow hunger cues
o Burp infant frequently
o Don’t let baby hold bottle until after 1 year of age
o Use only iron fortified infant formula for the first year
Breast care:
- Wear a supportive bra – fit snugly while still allowing mother to breast without restriction
- Assessing breasts: instruct mother to examine daily to look at milk supply, condition of nipples, success of breastfeeding, palpating them to see if they are soft, filling or engorged
- Alleviating engorgement: temporarily happens during first week postpartum – usually resolves within 72 hours of it happening
o In breastfeeding woman: encourage feeding every 2-3 hours, using manual expression just before feedingto soften breast so newborn can latch better; let newborn feed on first breast until it softens before switching to other side
o For bottle feeding woman: breast engorgement is self limiting that disappears as increasing estrogen levels suppress milk formulation; encourage woman to use ice packs, wear a snug supportive bra 24 hours a day and to take mild analgesics; avoid stimulation to breasts that might foster milk production like warm showers or massaging them
Suppressing lactation:
- Supportive snug bra approx. 6 hours post delivery and don’t take it off – only for showers
- Milk suppression may take 5-7 days
- Take mild analgesics to reduce discomfort
- Let shower water flow on back rather than breasts so it doesn’t stimulate milk
- Avoid massage or sucking breasts
- Ice packs
- Meds to suppress are no longer recommended
Nurses play major role in assisting families to adapt to changes and transitioning to parenthood
- Provide guidance about what sibliings responses to the new baby could be, more tension, child development and meeting needs of various members of the family
- Don’t assume that just bc a woman has other children that her knowledge is up to date and good
Promoting parental roles:
- Repeated continued contact with newborn helps parents learn cues and understand behaviour
- Provide opportunity for parents to interact with baby – exploration, holding, providing care
- Model behaviour by holding newborn close and speaking positively
- Refer to newborn by name in front of parents
- Speak directly to newborn in calm voice
- Encourage parents to pick up and hold newborn
- Point out newborn responses and physical features
- Involve parents and praise them for efforts
- Evaluate strengths and weaknesses
- Look for risk factors for lack of support
- Consider culture
- Monitor coping behaviours
- Identify support systems and ask direct questions
- Provide guidance on newborn sleep-wake cycles, variations in appearance, developmental milestones (growth spurts), interpreting cues, how to quiet a crying infant, signs and symptosm of illness, integrating siblings into care
Explaining sibling roles:
- Can be overwhelming for a young child to have another family member introduced
- Siblings need extra attention and reassurance that they are loved and important
- Expect and tolerate thumb sucking, bedwetting (some regression)
- Encourage discussion about the new infant during family times
- Encourage siblings to participate in decisions like toys to buy
- Take sibling on tour of maternity ward
- Spend special time with the child
- Read books to the child and play games
- Role play safe handling of baby with a doll
- Purchase a gift that the child can give to the newborn
- Purchase a gift that can be given to the child by the newborn
- Arrange for child to come to hospital to see newborn
- Encourage grandparents to pay attention to the older child when visiting
Grandparents role: support and comfort
- Depends on how close they live, willingness, culture
- Grandparents take charge approach may not be welcomed
- Assess communication skills, role expectations, support skills
Teaching about postpartum blues:
- Asses sleep deprivation and exhaustion
- Postpartum is happy yet stressful
- May have emotional fluctuations – crying ne minute and laughing the next
- Postpartum blues: transient emotional disturbances beginning in the first week after childbirth – wide range of labile emotions like uneven energy, insomnia, difficulty decision making, emotional insecurity, grieving for a former sense of self and body image – begin 3-4 days after and resolve by day 10
- Affect up to 70%
- If they last longer than 2 weeks, possible that PPD is developing – feeling hopeless, isolated, despair, harming oneself or baby
- Blues require no formal treatment other than support and reassurance
- Encourage mom to vent her feelings
Preparing for discharge:
- Shortened stay if mother is afebrile and VS normal, lochia is appropriate, Hg and Hct are normal, uterus is firm; urninary output is adequate; ABO and RhD status known and taken care of; surgical wounds healing and no signs of infection; mother can ambulate without difficulty; food and fluids taken well; self care and infant care are understood; family or other support is available to care for mother and baby; mother is aware of complications
Safe sleeping:
- Smoke free
- Baby on back
- Baby in crib next to adults bed for first 6 months
- Safe crib – no toys or loose bedding
- Bed sharing is not recommended – more SIDS and suffocation
Immunizations:
- Check rubella status and give SC injection of rubella if not immune
- Consent form for vaccine
- Nursing mothers can receive the vaccine
- Inform of adverse effects – rash, joint symptoms, low grade fever 5-21 days later
- Avoid pregnancy at least 3 months after being vaccinated bc of risk of teratogenic effects
- Rh status of baby to be checked if mom is Rh negative – injection of Rh immunoglobulin within 72 hours if baby is positive
Ensure follow up care:
- Women who are discharged too early have risk of uterine subinvolution, discomfort at an episiotomy or caesarean site, infection, fatigue, maladjustment to new role
- Nursing care: family focused, phone calls, out patient clinics, home visits – public health nurses usually do this
- Phone call: during first week to see how things are going
- Out patient follow up: visits to office arranged soon after discharge;
o Office visit 4-6 weeks later if woman had an uncomplicated vaginal birth
o Caesarean: 2 weeks after discharge
o Hospitals specify when to make visits
- Home visit follow up: usually made within first week
o Assess for and manages physical and psychological problems
o Maternal assessment – general wellbeing, vitals, breast care, abdo status, voiding status, fundus and lochia status, psychological and coping, family relationships, feeding, environmental safety check
o Infant assessment: physical exam, vitals, home safety check, developmental status
o Feeding techniques
o Emotional needs of new family
o Warning signs of problems and how ot prevent and eliminate them
o Sexuality issues
o Immunizations
o Smooth transitions
o Links to community resources
See page 176-178 for maternal assessment and newborn assessment forms
Chapter 18 Early newborn period (14 pages) 532-545
Maintaining thermoregulation:
- Potential for heat loss
- Thoroughly dry the infant
- Put a cap on the head
- Ensure skin to skin with mom and cover baby with warm blanket
- Make sure the newborn isn’t exposed to cold surfaces or cool drafts
- Axiliarry temp should be maintained between 36.3-37
- Use a warmed cover on the weight scale
- Warm stethoscopes and hands
- Delay initial bath until temp has stabilized
- Avoid placing cribs near cold outer walls
- Place newborn in incubator if other interventions aren’t good enough
Assessment of the newborn:
Perinatal history:
- Review maternal history for certain risk factors
- Mothers name, medical record number, blood type, serology result, rubella and helpatitis status
- HIV and GBS status
- Intrapartum maternal antibiotic therapy (type, dose, duration)
- Maternal illnesses that could have affected the pregnancy
- Gestational diabetes
- Prenatal care visits
- Risk for blood group incompatibility like Rh status and blood type
- Fetal distress and any nonreassuring FHR patterns during labour
- Known inherited conditions like sickle cell anemia and PKU
- Birth weights of previous live born children and identification of any newborn problems
- SDOH that may impact
- History of substance use
- History of mental health conditions
- Cultural factors
- Pregnancy complications associated with abnormal fetal growth
- Info on progresso f labour, birth, labour complications, duration of ruptured membranes, presence of meconium in the amniotic fluid
- Meds given to mother during labour, at birth and immediately after
- Time and method of delivery including presentation and use of focepts or vacuum extractor
- Status of newborn at birth – APGAR
- Meds administered to the newborn
- Postbirth maternal info like placental findings, positive cultures, fever
Newborn physical exam:
- Within the first 24 hours after birth
- Delay the exam until the newborn has adjusted from inside to the outside world
- Share info with parents
- In a quiet newborn, begin with the least invasive and noxious elements of the exam and then progress to areas most likely to irritate the newborn (like moro reflex)
- Typical physical exam: skin colour, posture, state of alertness, head size, overall behavioural state, resp status, sex, any obvious congenital anomalies
Anthropometric measures:
- Most parents want to know length and weight right away
- Also measure head and chest circumference
- These measurements will be ompared with future serial measurements to determine growth patterns
- Weight is affected by race, maternal age, size of parents, maternal nutrition, placental perfusion
- Weight should be correlated with gestational age
- LGA infants may have ahd a diabetic mother
- SGA infants or preterm may have a genetic syndrome
- Head circumference: 32-38cm – measure the occipitofrontal circumference
o Should be about ¼ of length
o Small head may indicate microcephaly bc of rubella, toxoplasmosis, prenatal cocaine, or alcohol exposure, SGA
o Enlarged head may indicate hydrocephalus or increase intracranial pressure
- Chest circumference: 30-36cm (about 2-3 cm less than head circumference)
Vitals:
- TPR are monitored frequently
- Assess at 1 and 2 hours following the first vitals, at hour 6, then once per shift until discharge
- If infant was cool and is being warmed, check the temp every 15-30 mins until within normal range
- BP not routinely assessed
- Get apical pulse – one minute (usually 120-160)
o Sinus arrhythmia is normal finding
o Murmurs don’t necessarily indicate congenital heart disease but assess frequently
- Palpate apical, femoral and brachial pulses for presence and equality
- Respirations for a minute – slightly irregular, shallow, unlaboured – 30-60/minute
o Abdo movements with breathing is normal
o Not grunting, gasping, apnea longer than 20 seconds, asymmetry, decreased chest expansion, abnormal breath sounds or sternal retractions
Skin: colour, texture, turgor, integrity
- Smooth and flexible
- Colour consistent with genetics
- Skin turgor: pinch a small area of skin over chest or abdomen and note how quit it returns to original position – immediately is normal
- Warm skin and intact
- May be blotchy or mottled especially in extremities
- Acrocyanosis: persistent cyanosis of fingers, hands, toes, feet with mottled blue or red discolouration and coldness – may be seen in first few weeks in response to exposure to cold
- Note rashes, ecchymoses or petechiae, nevi or dark pigmentation
- Petechiae may be result of pressure on the skin during the birth process
- Forceps marks may be observed over cheeks and ears
- Vernix caseosa: thick white substance protecting the skin of fetus – formed by secretions from oil glands and is found in first 2-3 days after birth in body creases and the hair – doesn’t need to be removed
- Stork bites: superficial vascular areas found on nape of neck, eyelids and between eyes and upper lip – where the stork may have picked up the baby in the myth – bc of immature BVs and are most visible when newborn is crying – this is normal and most fade and disappear within first year
- Milia: unopened sebaceous glands frequently found on newborn’s nose – could also be on chin and forehead
o They form from oil glands and disappear within 2-4 weeks
o Epsteinspearsl: when they are found in mouth and gums
- Mongolian spots: blue or purple splotches that appear and lower back and bum – usually in Asian, black and indan newborns but can occur in dark skinned newborns of all races
- Erythema toxicum: newborn rash: benign, idiopathic, generalied transient rash in up to 70% of newborns during first week of life
o Small white or yellow papules or vesicles on skin
o Common on face, chest, back, extremities
o Lack of pattern
o Caused by eosinophils reacting to the environment as the immune system matures
- Harlequin sign: dilation of BVs on only one side of the body, giving the newborn the appearance of wearing a clown suit - distinct midline demarcation which is describes as pale on the nondependent side and red on the opposite, dependent side
o Due to autonomic imbalance of cutaneous vasculature and commonly seen in low birth weight newborns when there is a positional change
o Transiet – lasts as long as 30 mins but no intervention needed
- Nevus flammeus: port wine stain: face or neck; capillary angioma located directly below the dermis – flat with sharp demarcations and pink to purple- red
o Made of mature capillaries that are congested and dilated
o Ranges in size from a few mm to half the body surface
o Permanent and will not fade
o Can be associated with syndromes, structural malformations, bony or muscular overgrowth, certain cancers
o Monitor with periodic eye exams, neuro imagine and extremity measurements
- Nevus vasculosus: strawberry mark – benign capillary hemangioma in the dermal and subdermal layers – raised, rough, dark red, sharply demarcated – commonly found in head region and grows rapidly for 6 months and then regresses over a period of several years without treatment
Head: varies with sex, age, ethnicity; correlated with body size
- Head should be symmetric and round
- As many as 90% of the congenital malformations present at birth are visible on the head
- Two fontanels:
o Anterior – diamond shaped and closes at 18-24 months and is 4-6cm
o Posterior – triangular, smaller (0.5-1cm) and closes by 6-12 weeks
o Palpate both – should be soft, flat and open
- Skull should be smooth and fused except at the fontanels
- Molding: elongated shaping of fetal head to accommodate passage thru birth canal
o Occurs with vaginal birth from vertex position where elongation of the fetal head occurs with prominence of the occiput and overriding sagittal suture line
o Resolves within a week without intervention
- Caput succedaneum: localized edema on the scalp that occurs from the pressure of the birth process
o After prolongel labour
o Poorly demarcated soft tissue swelling that crosses suture lines
o Pitting edema and overlying petechiae and ecchymosis are noted
o Swelling gradually goes away in 3 days without treatment
o Vacuum extraction usually have this where cup was used
- Cephalhematoma: localized effusion of blood beneath the periosteum of the skull
o Due to disruption of vessels during birth
o Occurs after prolonged labour and things like forceps and vacuum extraction
o Well-demarcated, often fluctuant swelling with no overlying skin discolouration
o Swelling doesn’t cross suture lines and firmer to the touch than an edematous area
o Usually appears on 2nd or 3rd day of life and dispears in a few weeks or months
- Abnormalities in head or fontanel size:
o Microcephaly: head circumference more than 2 standard deviations below avg or less than 10% of normal parameters for gestational age, caused by failure of brain development (familial, infections, syndroms, FASD)
o Macrocephaly: head circumference more than 90% of normal usually related to hydrocephalus – usually familial and could also be a manifestation of other anomalies like hydrocephalus and skeletal disorders
o Large fontanels: more than 6cm in the anterior diameter bone to bone or more than a 1cm diameter in the posterior fontanel
Possibly associated with malnutrition, hydrocephaly, congenital hypothyroidism, trisomies 13, 18 and 21, and various bone disorders like osteogenesis imperfecta
o Small or closed fontanels: smaller than normal anterior and posterior diameters or fontanels that are closed at birth; associated with microcephaly or premature synostosis (union of two bones by osseous material)
Face: observe for fullness and symmetry
- If forceps were used, they may have bruising and reddened areas over both cheeks and parietal bones secondary to the pressure of the forceps blades
o Reassure parents that this resolves without treatment
- Problems with the face: facial nerve paralysis caused by trauma from the use of forceps – paralysis usually on first or second day of life
o They will usually demonstrate asymmetry of the face with the inability to close the eye and move the lips on the affected side
o Newborns with facial nerve paralysis have difficulty making a seal around the nipple and consequently milk or formula drools from the paralyzed side of the mouth
- Most facial nerve palsies resole spontaneously within days but full recovery may take weeks to months
Nose: symmetry, position, lesions
- Midline, patent nares, intact septum
- Nostrils equal size and patent
- Slight mucus discharge may be present but there should be no actual drainage
- Preferential nose breathing and will use sneezing to clear the nose if needed
- Can smell after the nasal passages are cleared of amniotic fluid and mucus
Mouth:
- Lipds should be intact with symmetric movement and positioned in the midline
- No lesions
- Lips for pink colour, moisture and cracking
- The lips should encircle the nurses finger to form a vacuum
- Variations in lips: cleft upper lip (separation extending up to the nose) or thin upper lip associated with FASD
- Assess inside of mouth for alignment of the mandible, intact soft and hard palate, sucking pads inside the cheeks, a midline uvula, a free moving tongue, and working gag, swallow, and sucking reflexes
- The mucus membranes lining the oral cavity should be pink and moist with minimal saliva present
- Normal variations:
o Epstein’s pearls: small, white epidermal cysts on the gums and hard palpate that disappear in weeks
o Erupted precocious teeth that may need to be removed to prevent aspiration
o Thrush: white plaque inside mouth caused by exposure to candida albicans during birth – cannot be wiped away with qtip
o Combo of small jaw, recessive chin (micrognathia) and a tongue that tends to fall backwards (glossoptosis) accompanied by resp distress may indicate the presence of Pierre Robin sequence
Eyes:
- Colour, eyelids, lashes, conjunctiva, sclera, iris, pupils
- Position, colour, size, movement
- Could be edema of the eyelids and subconjunctival hemorrhages due to pressure during childbirth
- Eyes should be clear and symmetrically placed
- Blink reflex: bring something close to eye and they should quickly blnk
- Pupillary reflex: pupil equal, round, reactive to light
- Assess gaze – track objects to the midline
- Movement can be uncoordinated in first few weeks
- Transient strabismus: deviation or wandering of eyes independently
- Searching nystagmus: involuntary repetitive eye movement
- The two above are normal for 3-6 months
- Examine internal eye structures
o Red reflex; luminous red appearance seen on retina – seen bilaterally on retinoscopy
shows no dullness or irregularities
- Chemical conjunctivitis: commonly occurs within 24 hours of instillation of eye prophylaxis after birth
o Lid edema with sterile discharge from both eyes
o Usually resolves in 48 hours without treatment
Ears: size, shape, skin condition, placement, amount of cartilage, patency of auditory canal
- Soft and pliable and recoil quickly when folded and released
- Alighted with eyes
- Low-set ears are characteristic of syndromes and genetic abnormalities
- Otoscopic exam isn’t usually don’t bc the ears are filled with amniotic fluid and vernix caseosa so its hard to see the tympanic membrane
- Most places have universal newborn hearing screening programs
- Delays in identification and intervention can affect cognitive, verbal, behavioural and emotional development
- Causing of hearing loss: conductive, sensorineural, central
- Risk factors for congenital hearing loss: cytomegalovirus infection and preterm birth necessitating a stay in the NICU
- Newborns typically turn towards noises and startles with loud ones
Neck: movement and ability to support head
- Will appear almost nonexistent bc its so short
- Creases are noted
- Lateral folds of skin: webbing: indicates turner’s syndrome: genetic condition seen in a girl that is caused by the absence of an x chromosome
- Neck should move freely in all directions and should be capable of holding the head in midline position
- Enough head control to hold head up briefly without support
- Inspect and palpate clavicles, which should be straight and intact
- Clavicle is most frequently injured bone during labour and delivery
- Primary cause of fracture is mechanical compression seen during difficult deliverieis such as shoulder dystocia
- Usually a fractured calvicle is asymptomatic but could show decreased movement, crepitus (grating that can be felt or heard with movement), pain or tenderness
- Treatment: immobilize and minimize pain
Chest: size, shape, symmetry
- Round and symmetrical with circumference 2-3cm smaller than head
- Xiphoid process may be prominent at birth but becomes less apparent when adipose tissue accumulates
- Nipples can be engorged and may secrete white discharge – bc of high levels of maternal estrogen while in utero
- Some have extra (supernumerary) nipples – small, raised pigmented areas vertical to the main nipple line, 5-6cm below the normal nipple – tend to be familial; reassure parents that this is harmless
- Usually barrel shaped with equal anteroposterior and lateral diameters
- Auscultate lungs for equal sounds – little diff between inspiration and expiration
- Fine crackles can be heard on inspiration soon after birth as result of clearing amniotic fluid from lungs
- Diminished breath sounds may indicate atelectasis, effusion, poor resp effort
- Resp issues most common cause of nICU
- Listen to heart when baby is quiet or sleeping – S1 and S2 are accentuated at birth
- If murmurs present after 12 hours of life, evaluate to rule out cardiac disorder
Abdomen: shape and movement
- Protuberant but not distended
- Abdominal movements usually synchronized with respirations
- Listen to bowel sounds and palpate for consistency, masses and tenderness
- Listen and palpate in clockwise way
- Palpate gently to feel liver, kidneys and masses
- Normal findings: bowel sounds in all 4 quadrants, no masses or tenderness on palpateion
- Distention may indicate air swallowing, ascites, obstruction or perforation of the GI tract, infection, masses or enlarged abdo organ
- Sunken abdo: diaphragmatic hernia
- Inspect umbilical cord area for two arteries and one vein
o Umbilical vein larger than the arteries
o If only a single artery is present, associations with CV, renal, and GI anomalies
o Look for bleeding, infection, granuloma
Genitalia:
- Inspect penis and scrotum
- In uncircumcised male, foreskin should cover the glans
- In the circumcised male newborn, the glans should be smooth with the meatus centred at the tip of the penis – it will be red until it heals
- Urinary meatus should be midline at the glans tip – if its on the ventral surface of the penis, hypospadias is present; if its on the dorsal surface, its epispadias
- Inspect scrotum for size, symmetry, colour, rugae, location of testes
- Scrotum usually is relatively large and should be pink in white neonates and dark brown in neonates of colour
- Rugae should be well formed and should cover the scrotal sac
- There should be no bulging excessive edema or discolouration
- Some edema is common due to hydrocele (collection of fluid in scrotum) that disappears in 3-6 months
- Palpate scrotum for testes which should be in the sac and should feel firm and smooth and be equal size
- Undescended testes might be palpated in the inguinal canal in preterm infants; they can be unilateral or bilateral
- In female, inspect genitalia
- Urethral meatus is below the clitoris in the midline
- It will be engorged and the labia majora and minora may both be edematous
- Labia majora are large and cover the labia minora
- Clitoris is large and hymen is thick – these findings are bc of estrogen and progesterone from mom
- Vaginal discharge with mucus and blood may be present – pseudomenstruation
- Variations in female newborns: labial bulge that indicates inguinal hernia; ambiguous genitalia; rectovaginal fistula with feces present in vagina; imperforate hymen
- Inspect anus for position and patency
Extremities and back:
- Upper extremities for appearance and movement
- Hands for shape, number of fingers, palmar creases
- Observe spontaneous movement of extremities
- Polydactyly: extra digits
- Syndactyly: fusing of two or more digits
- A single palmar crease (simian line) is associated with down syndrome
- Brachial plexus injury can occur in macrosomic infants during a difficult birth involving shoulder dystocia
- Erb’s palsy: injury resulting from damage to the upper plexus during labour and birth – the affected arm hangs limp alongside the body and the affected shoulder and arm are adducted, extended and internally rotated with a pronated wrist
o Moro reflex is absent on the affected side in brachial palsy
o Complete recovery usually occurs but may take a few months
- Asses lower extremities in the same manner – equal length with symmetric skin folds
- Inspect for clubfoot: turning inward position which is secondary to intrauterine positioning
- Inspect the back – spine should be straight and flat and should be easily flexed when baby is held in prone position
- Look for a skin disruption, tuft of hair, pilonidal dimple in the back or a cyst, sinus tract or mass – can be signs of congenital spinal or neurological anomaly and should be documented and reported to primary HCP
See page 91 for a newborn assessment summary
Ortolani manoeuvre:
- Baby lays down
- Flex hips and knees to 90 degrees at the hip
- Grasp inner aspect of thighs and abduct the hips to about 180 degrees while applying upward pressure
- Listen for sounds – there should be no clicks heard – this would indicate that the femoral head hits the acetabulum as the head re-enters the area and suggests developmental hip dysplasia
Barlow manoeuvre:
- Baby lays down and you grasp the inner aspect of thighs, adduct the thighs while applying outward and downward pressure to the thighs
- Feel for the femoral head slipping out of the acetabulum and listen for a click
Neurological status: alertness, posture, muscle tone, reflexes
- Newborn should be alert and not persistently lethargic
- Normal posture: hips abducted and partially flexed with knees flexed, arms adducted and flexed at elbow, fists clenched with fingers covering thumb
- Assess for muscle tone: support newborn with one hand under the chest and observe how neck muscles hold the head; neck extensors should be able to hold the head in line briefly and only a slight head lag when pulling newborn from supine position to sitting one
Newborn reflexes:
- Absent or abnormal reflexes or persistence of the reflex past the age where it should be lost or return of a reflex in older child or adult may indicate neurologic pathology
- Sucking, moro, stepping, tonic neck, rooting, Babinski, palmar grasp
- Spinal reflexes: truncal incurvation (galant reflex) and anocutaneous reflex (anal wink)
- Moro: startled newborn
- Stepping reflex: hold newborn upright and inclined worward with the soles of the feet touching a flat surface and baby should make stepping or walking motion, alternating flexion and extension with the soles of their feet
- Tonic neck reflex: resembles the stance of a fencer – also called fencing reflex – have newborn lie on the back and turn the baby’s head to one side; the arm toward which the baby is facing should extend straight away from the body with the hand partially open, whereas the arm on the side away from the face is flexed and the fist is clenched tightly
- Rooting reflex: stroke the cheek and newborn turns to side it was stroked
- Babinski: stroke lateral sole of foot and toes splay out – diminished response indicates neuro dysfunction; disappears at approx. 1 year of age
- Grasp reflexes: palmar and plantar – hand and foot
- Blinking, sneezing, gagging, coughing are all protective reflexes elicited when an object or light is brought close to the eye (blinking), something irritating is swallowed or bulb used for suctioning (gagging and coughing) or irritatnt is brought close to nose (sneezing)
- Truncal incurvation reflex: galant reflex: present at birth and disappears in a few days to 4 weeks
o Newborn in prone position or held in ventral suspension, apply firm pressure and run a finger down either side of the spine and this stroking causes the pelvis to flex toward the stimulated side – lack of response indicates a neurologic or spinal cord problem
o Indicates T2-S1 innervation
- Anocutaneous reflex: anal wink: elicited by stimulating the perianal skin close to the anus
o The external sphincter will constrict (wink) immediately with stimulation
o Indicates S4-5 innervation
o Absence indicates abnormality of CNS
Chapter 22 second half starting at post partum infection (8 ish pages)
Post partum infection: common cause of morbidity and mortality
- About 8%
- High in c section than vaginal
- Incidence is expected to increase bc of earlier discharge of postpartum women from the hospital
- Defined as fever of 38 or higher after the first 24 hours after childbirth, occurring on at least 2 of the first 10 days after birth, excluding first 24 hours
- Infections easily enter female genital tract and ascend thru the internal genital structures
- Decreasing vaginal acidity bc of amniotic fluid blood and lochia (which are alkaline) – this encourages growth of bacteria
- Now since women are discharged sooner, nurses must assess new mothers for risk factors and identify early subtle signs and symptoms of an infectious process
- Common etiology involves organisms that are in the normal vaginal flora – aerobic and anaerobic (staphylococcus aureus, E. coli, klebsiella, Gardnerella vaginalis, gonococci, group A or B hemolytic strep, chlamydia trachomatis)
- Common infections are metritis, wound infections, UTIs, mastitis
- Metritis: lower abdo tenderness, foul smelling lochia, anorexia, nausea, fatigue and lethargy, leukocytosis
o Clinical endometritis
o Post partum uterine infections usually involving more than just the endometrial lining
o Involves endometrium, decidua, adjacent myometrium
o Uterine cavity is sterile until rupture of amniotic sac
o Risk increases with C section – 10-20% of c sections
o Primary prevention is key and focuses on reducing risk factors
o Broad spectrum antibiotics
- Wound infection: weeping serosanguineous or purulent drainage, separation of wound edges, edema, erythema, tenderness, maternal fever, elevated WBCs
o Cesarean surgical incisions, episotomy site, genital tract from laceration
o Usually not identified till after discharge bcsymptosm may not manifest till 24-48 hours after birth
o Teach about signs and symptoms to look for
o Manage it by recognizing the infection and open the wound to allow drainage
o Good handwashing, pad changes, hydration, ambulation
o Parenteral antibiotics
- UTI: urgency, frequency, dysuria, flank pain, low grade fever, urinary retention, hematuria, urine positive for nitrates, cloudy urine with strong odour
o E coli, klebsiella, proteus, Enterobacter
o Catheterization and frequent vaginal exams can increase risk
- Mastitis; flu like symptoms, tender hot red painful on one breast, inflammation of breast area, breast tenderness, cracking of skin around nipple or areola, breast distention with milk
o Inflammation of breast tissue caused by milk stasis and bacterial invasion
o Usually unilateral
o Risk factors: stress, fatigue, cracked nipples, plugged or blocked ducts, ample milk supply and decrease in number of feeding, engorgement, stasis
o Can be caused by a missed feeding, bra too tight, breast trauma, poor drainage of duct and alveoli, poor maternal nutrition, vigours exercise, infection
o Most common organism is staph aureus which comes from the infants mouth or throat
o Diagnosis usually made without a culture
o If its not treated, can progress to breast abscess
o Treatment: empty the breasts and control the infection - infant sucking, manual expressing; increased frequency of nursing, control infection with antibiotics
Nursing assessment:
- Assess for risk factors:
o Prolonges (over 6 hours) premature rupture of membranes
o Insertion of fetal scalp electrode or intrauterine pressure cathether
o C section
o Instrument assisted birth like forceps or vacuum
o Catheter
o Regional anesthesia that decreases perception to void
o Unwell staff
o Anemia, obesity, smoking, rug abuse
o Pre-existing colonization with the organisms
o Retained placental fragments
o Manual removal of retained placenta
o Trauma to genital tract like episiotomy or laceration
o Prolonged labour with frequent vaginal checks
o Gestational diabetes
o Break in aseptic technique
- Pay attention to abdomen, fundus, breasts, urinary tract, episiotomy, lacerations, incisions
- Episiotomy site:
o REEDA (redness, erythema or ecchymosis, edema, drainage, approximation
- Monitor vitals – temp
Nursing management: preventing infection
- Maintain aseptic technique
- Use good handwashing
- Reinforce measures for good peri care
- Adequate lighting to look at episiotomy site
- Screen visitors for infections
- Review history for preexistin infections
- Monitor finals
- Monitor frequency of vaginal exams
- Assess frequency of vaginal exams and length of labour
- Assess for early infection signs
- Insepct wounds for inflammation and drainage
- Encourage rest hydration and healthy eating
- Client teaching is big – tell about infection signs and symptoms, stress handwashing and peri care
Teaching to woman with infection:
- Continue antibiotics and keep taking them tilltheyre done
- Check temp every day
- Watch for other signs and symptoms of infection
- Wash hands, wipe from front to back, remove peri pad using front to back and fold pad in half and wrap in toilet paper, wash hands before applying new pad, handle a new pad by the edges and avoid touching the part that touches your body, use a peri bottle, drink fluids, adequate rest
See page 193 for care plan
Postpartum emotional disorders: new mothers may feel weepy, overwhelmed, unsure whats happening
- Lower incidence of postpartum emotional disorders in cultures that promote open expression of emotions and women centered care
- Plummeting levels of estrogen and progesterone can contribute to post partum mood disorders
Baby blues: most ppl (50-85%) get this
- Mild depressive symptoms of anxiety, irritability, tearfulness, mood swings, increased sensitivity, fatigue
- Peak at day 4-5 and usually resolve by day 10
- 20% go on to post partum depression
Post partum depression:
- If symptoms of baby blues last beyond 6 weeks and seem to get worse, may have PPD
- 8-23% may get it
- Can happen within the first year
- Feel worse over time
- Risk factors; history of depression, history of PPD, fam history of depression, life stress, childcare stress, prenatal anxiety, lack of social support, relationship stress, difficult or complicated pregnancy, traumatic birth experience, birth of high risk or special needs infant
- Gradual onset and becomes evident within first 6 weeks postpartum
- Common manifestations: loss of pleasure, low mood, exhaustion not relieved by sleep, guilty feelings, irritability, can’t concentrate, anxiety, despaire, compulsive thoughts, loss of libido, loss of confidence, sleep difficulties, loss of appetite, failure feelings
- Prophylaxis starts with prenatal risk assessment and education
- Based on history of prior depression, prophylactic antidepressant therapy may be needed in 3rd trimester
- Antidepressants, anti-anxiety meds, psycho-therapy
Post partum psychosis:
- 1 in 1000 births
- Within 3 weeks of birth
- Sleep disturbances, fatigue, depression, hypomania
- Tearful, confused, preoccupied with feelings of guilt and worthlessness
- Early symptoms resemble depression but may escalate to delirium, hallucinations, anger towards herself and infant, biaarre behaviour, manifestations of mania, thoughts of hurting herself or infant
- Looses touch with reality
- Most women with this are hospitalized for up to several months and psychotropic drugs are treatment with psychotherapy and support group therapy
- Greatest hazard is suicide
- Risk for infanticide and child abuse
Nursing assessment:
- Teach that they may be emotional after birth – don’t feel bad for not being happy even tho they think they “should” be happy
- Assess for risk factors: poor coping, low self esteem, stressors, mood swings and emotional stress, fam history or personal history, substance abuse, limited supports
- Physical findings: activity and fatigue, sleeping habits
- Verbal and nonverbal indicators of anxiety
- Difficulty concentrating
- Nutritional intake; weight loss
Nursing management:
- Encourage client to verbalize feelings
- Recommend that they seek help for chores and child care
- Stress importance of good nutrition and adequate exercise and sleep
- Encourage her to make a support system
- Assist woman to structure her day to get control of it
- Keep expectations realistic
- Postpone major life changes like moving or changing jobs
- Give info about bodily changes
- Review signs and symptoms of the emotional disorders
- Stress that many women need help and help is available
See page 197 for key concepts of the chapter
RNAO breastfeeding (3 pages)https://rnao.ca/sites/rnao-ca/files/bpg/breast_feeding_BPG_WEB_updated_Oct_2_1.pdf
Page 18-19
Recommendations:
- Assess breastfeeding using validated and reliable tools within the first 24 hours, between 2-8 days postpartum, and from day 9 postpartum and onwards
- Facilitate skin to skin contact with breastfeeding immediately following childbirth or once clinically stable
- Support early initiation of breastfeeding within one hour of birth or once they are stable – prental education and bedside assistance
- Support the breastfeeding dyad to achieve effective positioning, latch and milk transfer
- Support responsive cue based breastfeeding by educating and recognizing the needs of the breastfeeding person
- Teach hand expression to all breastfeeding ppl prior to discharge
- Implement individualized breastfeeding self efficacy interventions thru the perinatal period to enhance breastfeeding confidence
- Provide individualized assistance to support or enhance breast milk production
- Provide proactive breastfeeding support
- Facilitate informed decision making regarding pacifier use
- Provide education thru the perinatal period as long as breastfeeding continues
- Include family in education and support
Page 143
Breastfeedign populations that may need extra support:
- Adolescents
- Deaf
- History of breast surgery
- History of sexual trauma
- Incarcerated ppl
- Indigenous
- Obese
- Depression and anxiety
- GDM
- Low health literacy
- Low income
- Visual impairment
- Transgender
Situations that may require extra help:
- Mastitis and reduing nipple pain
- Induced lactation and relactation
- Substance use – alcohol, cannabis, tobacco
Government of Ontario (2 pages)
https://resources.beststart.org/wp-content/uploads/2018/12/B03-E.pdf
How often to breastfeed (per 24 hours):
- At least 8 feeds per day
- Baby sucking strongly, slowly steadily and swallowing often
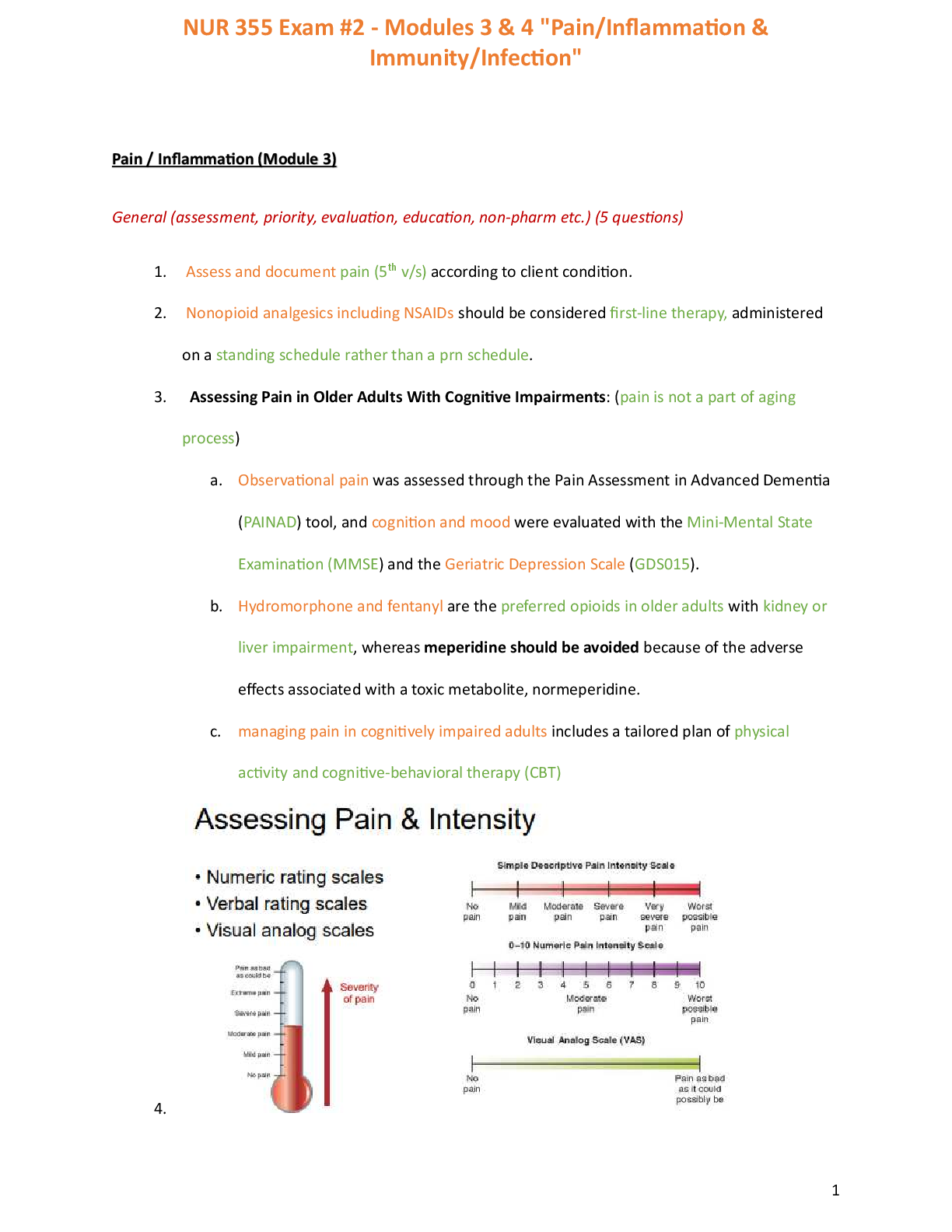
Stomach size:
- 1-2 days; size of cherry
- 3-4 days: size of walnut
- 5-6 days; size of apricot
- 7+ days size of egg
Wet diapers per 24 hours:
- Day 1: at least 1 wet
- Day 2: at least 2 wet
- Day 3: at least 3
- Day 4: at least 4
- Day 5 and beyond at least 6 with pale yellow or clear urine
Soiled diapers:
- Day 1-2: 1-2 black or dark green
- Day 3-4: at least 3 brow, green or yellow
- Day 5 and beyond: at least 3 large soft and seedy yellow
Weight; most babies lose a bit in the first 3 days then from day 4 onward, they gain weight regularly
- Return to birth weight by 10-14 days of age
Growth spurts: babies often vary the length of time between feedings and some feedings will be closer together
Babies should have a strong cry, more actively and wake easily and mothers breasts should feel softer and less full after breastfeeding
Breastfeeding guidelines for consultants;
- Observe mother
- Assess positioning and proper alignment of mother and baby – ensure maternal comfort
- Assess latch: babies mouth wide open, lips flanged and chin pressed into breast
- Assess baby for wet and soiled diapers, gaining weight, moist mouth and bright eyes and alert
- If problems happen, reassess and try strategies
Increasing mothers milk supply and baby’s intake:
- Correct position and latch
- Increase number of feets
- Use breast compressions during feedings
- Switch breasts several times in the same feeding
- Express milk after feeds
Acceptable breastfeeding supplements;
- First choice – milk from breast
- Second choice – previously expressed breast milk from mother
- Third choice – pasteurized donor breast milk
- Fourth choice – commercial cow milk based infant formula
When supplementation is required, this can be used: cup, spoon, dropper, finger feeding; supplemental nursing device at breast; bottle feeding
[Show More]




.png)