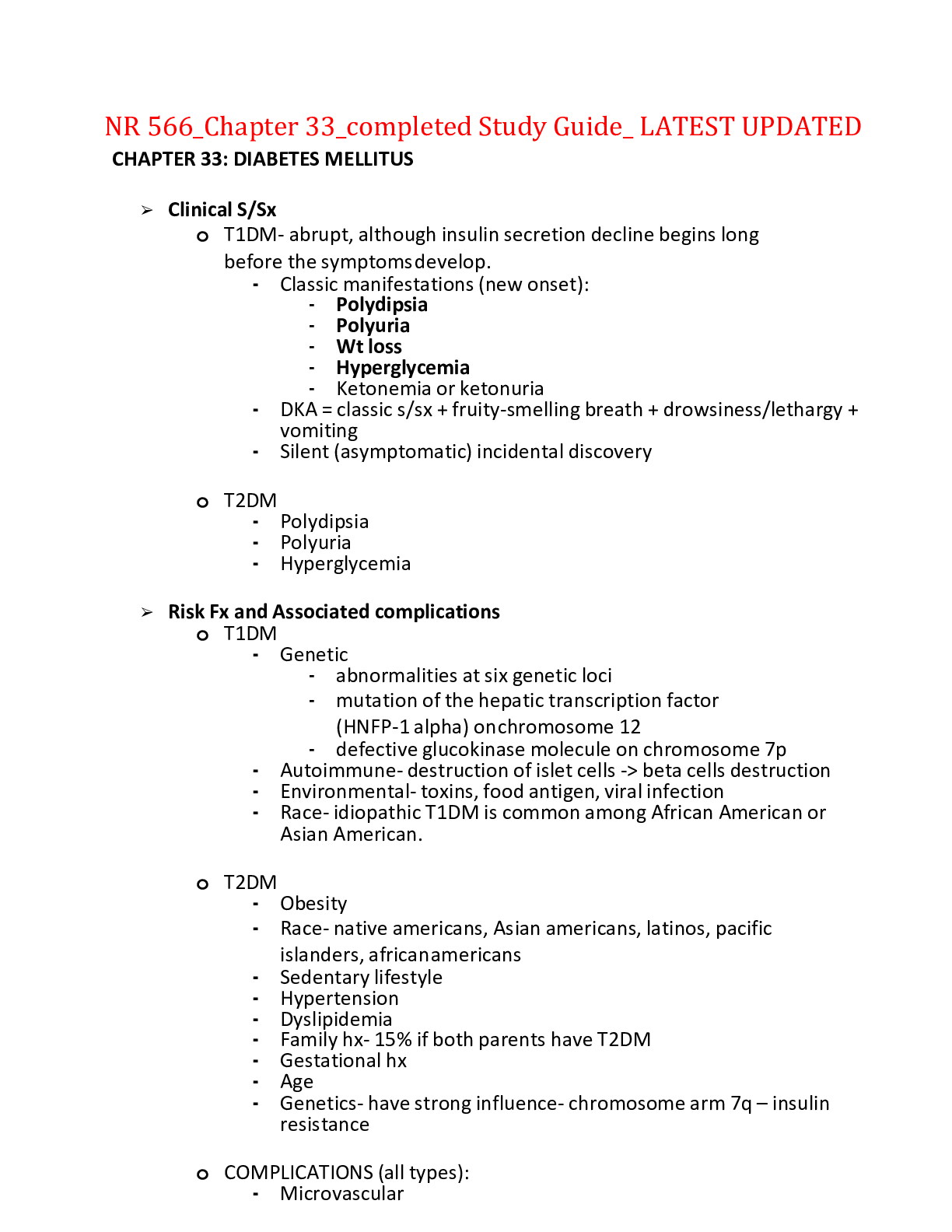
NR 566_Chapter 33_completed Study Guide_ LATEST UPDATED
CHAPTER 33: DIABETES MELLITUS
➢ Clinical S/Sx
o T1DM- abrupt, although insulin secretion decline begins long before the symptoms develop.
▪ Classic manifestat
...
NR 566_Chapter 33_completed Study Guide_ LATEST UPDATED
CHAPTER 33: DIABETES MELLITUS
➢ Clinical S/Sx
o T1DM- abrupt, although insulin secretion decline begins long before the symptoms develop.
▪ Classic manifestations (new onset):
• Polydipsia
• Polyuria
• Wt loss
• Hyperglycemia
• Ketonemia or ketonuria
▪ DKA = classic s/sx + fruity-smelling breath + drowsiness/lethargy + vomiting
▪ Silent (asymptomatic) incidental discovery
o T2DM
▪ Polydipsia
▪ Polyuria
▪ Hyperglycemia
➢ Risk Fx and Associated complications
o T1DM
▪ Genetic
• abnormalities at six genetic loci
• mutation of the hepatic transcription factor (HNFP-1 alpha) on chromosome 12
• defective glucokinase molecule on chromosome 7p
▪ Autoimmune- destruction of islet cells -> beta cells destruction
▪ Environmental- toxins, food antigen, viral infection
▪ Race- idiopathic T1DM is common among African American or Asian American.
o T2DM
▪ Obesity
▪ Race- native americans, Asian americans, latinos, pacific islanders, african americans
▪ Sedentary lifestyle
▪ Hypertension
▪ Dyslipidemia
▪ Family hx- 15% if both parents have T2DM
▪ Gestational hx
▪ Age
▪ Genetics- have strong influence- chromosome arm 7q – insulin resistance
o COMPLICATIONS (all types):
▪ Microvascular
• Eyes, heart, kidneys, nervous system
• Retinopathy with potential loss of vision
• Nephropathy leading to renal failure
• Peripheral neuropathy with risk of:
o Foot ulcers
o Amputation
o Charcot’s joint
• Autonomic neuropathy with:
o GI, GU, CV s/sx
o sexual dysfunction may occur.
▪ Macrovascular
• Atherosclerotic conditions which increases the risk of HTN, abnormalities in lipid metabolism, abnormalities of platelet function, and periodontal disease:
o Cardiovascular
o Peripheral vascular
o Cerebrovascular
➢ Diagnostic Criteria
o Pre-diabetes
▪ BG too high to be considered normal BUT does not meet criteria for DM
• Impaired glucose tolerance (IGT) or Impaired fasting glucose (IFG)
• IFG 100-125 mg/dL
• IGT 140-199 mg/dL
• HbA1c 5.7% - 6.4%
▪ At risk for diabetes and CVDs and may have insulin-resistance syndrome
o T1DM and T2DM
▪ 4 tests used:
• Acute symptoms of DM + casual plasma glucose ≥ 200mg/dL
• Fasting plasma glucose (FPG) >126 mg/dL- most reliable
• 2-h post-load plasma glucose in an oral glucose tolerance test ≥ 200mg/dL
• HbA1c ≥ 6.5%
▪ Tests should be:
• confirmed on a subsequent day, unless (+) overt clinical s/sx
• preferrable to confirm with the same test OR one that is considered more predictive
• If a repeated test is below the diagnostic criteria -> REPEAT TEST in 3- 6months.
➢ Criteria for screening asymptomatic adults
o Individuals with BMI ≥25 and:
▪ ≥45y/o- should be tested, if normal- repeat test at 3yr intervals.
▪ ≤45y/o + risk factors:
• Physically inactive
• First-degree relative with DM
• High-risk ethnic group (African American, Hispanic, Native American, Asian American, Pacific Islander)
• Delivered a baby weighing >9lbs or previously dx of GDM
• Hypertension (BP ≥140/90)
• HDL cholesterol ≤35 mg/dL and Triglycerides ≥250 mg/dL
• (+) PCOS
• IGT or IFG on previous testing
• Conditions associated with insulin resistance (PCOS, acanthosis nigricans)
• Hx of CVD
➢ Insulin and OHG
o Insulin- exogenous insulin produces the same effect as the naturally occurring hormone.
▪ Lowers BG levels by:
• Promoting protein synthesis by increasing amino acids transport into cells
• Stimulates glucose entry into cells as energy source
• Increases storage of glucose as glycogen (glycogenesis) in muscle and liver cells
• Inhibits glucose production in liver and muscle cells (glycogenolyis)
• Enhances fat storage (lipogenesis) and precent mobilization of fat for energy (lipolysis and ketogenesis)
• Inhibits glucose formation form non-CHO sources, such as amino acids (gluconeogenesis)
▪ Basal insulin once or twice daily
▪ Subcutaneous injection (IV in hospital settings for rapid acting like regular insulin)
▪ 2 long-acting insulin analogs (important breakthroughs in DM management and tx.
• Insulin glargine-
o can be given at HS or at any time of day (but should be given consistently at the same time each day.
o CANNOT BE MIXED with other insulin
• Insulin detemir-
o Prolonged absorption
o Provides a more consistent 24-hr basal effect d/t to its protein binding effect in the plasma and near injection site
o Cannot be diluted or mixed with other insulin preparations
• BOTH glargine and detemir-
o may have less nocturnal hypoglycemia effects
o expensive than NPH
▪ T2DM will usually require insulin d/t progressive beta cell dysfunction after a period of time.
• Preferred: basal insulin once or twice daily (IAI or LAI)
• NPH- nocturnal hypoglycemia
o Oral Agents
▪ Only effective in T2DM
▪ Monotherapy (reduction of A1c by 0.5%-2.0%), combination therapy (further decrease in A1c)
▪ PRIMARY CARE PROVIDER SHOULD COORDINATE THE START OF MEDICATIONS WITH AN OB OR ENDOCRINE SPECIALIST!
▪ Beguanides
• Are not considered hypoglycemic drugs
• INITIAL DRUG OF CHOICE for monotherapy
• Metformin
o Decreasing hepatic glucose production by decreasing gluconeogenesis
o Increases peripheral glucose uptake and utilization
o Improves response to blood glucose levels so that the liver produces appropriate amount of glucose
o Decreases intestinal glucose absorption
• Initial dose: Metformin 500mg once or twice daily (max dose 2,550mg daily)
• Titrate dose to decrease GI adverse reactions
• Helps with weight loss and reduction in LDL-C, reduction in total cholesterol, reduction in triglycerides, and increase HDL-C.
▪ Sulfonylureas
• Increase endogenous insulin secretion by the beta cells and may improve the binding between insulin and insulin receptors or increase the number of receptors
• (+) hypoglycemic effects – d/t increased endogenous insulin and improved beta cells sensitivity to BG levels or suppression of glucose release by the liver.
o Risk for hypoglycemia when taken with abx (clarithromycin, levofloxacin, TMP/SMZ, metronidazole, ciprofloxacin)
• Used to be the first class to treat T2DM, but now considered
SECONDARY AGENTS partially d/t hypoglycemic risk.
• PREGNANCY CATEGORY C (except for glyburide)
• Common S/E: hypoglycemia, wt gain
• 1st GENERATION- chlorpropamide, tolazamide, tolbutamide
• 2nd GENERATION- glipizide, glyburide, glimepiride
▪ Alpha-Glucosidase inhibitors
• Do not act directly on any of the defects in metabolism seen in T2DM
• Competitively inhibit and delay absorption of complex CHO from small bowel and lower BG levels after meals.
• No weight gain, does not promote wt loss
• Limited role as adjunct therapy to individuals who can not take metformin (except those patients on NGT)
• Can reduce A1c by 0.5%-1%
▪ Thiazolidinediones (TZD)
• Oral antihyperglycemic agents best classified as “insulin sensitizers”
• Activate a nuclear receptor that regulate gene transcription -> increased utilization of available insulin by the liver and muscle cells, and adipose tissue.
• Reduce hepatic glucose production -> appropriate glucagon production by the liver
• pioglitazone (Actos) and rosiglitazone (Avandia)
• Precautions: RISK FOR CARDIOVASCULAR PROBLEMS.
o Rosiglitazone- close monitoring of heart failure s/sx
• Fluid retention is also a notable s/e of the drug class
• Bladder Cancer- high risk for north American and European diabetics.
• Reduce A1c by 1.5%-2%.
▪ Meglitinides
• Short acting insulin secretagogues
• Close the ATP-dependent potassium channels in the beta cell membrane
-> depolarizes beta cells – opening of calcium channels -> influx of calcium -> increases secretion of insulin
• repeglanide (Prandin), nateglinide (Starlix)
• plasma insulin levels falls to baseline 4hrs after dosing.
o Dosed TID no more than 20mins ac.
• Lowering of postprandial (after meal) BG levels (beneficia to patients with postprandial hyperglycemia)
• Administration:
o 0-30 mins prior to each meal
o Should be omitted if meals are not eaten
o If extra meals are eaten, extra doses should also be taken
• Lowers A1c by 0.5%-1%
▪ Selective Sodium Glucose Co-transporter 2 (SGLT-2) inhibitors
• Inhibit renal SGLT-2 action > blocking about 90% of the glucose reabsorption in the kidneys and promoting excretion of glucose in the urine
• The higher the glucose = the higher is more excreted in the urine
• canagliflozin (Invokana), dapglifoxin (Farxiga), empagliflozin (Jardiance)
• combined with other agents to reduce glycemic levels
• Major S/E:
o GENITAL YEAST INFECTIONS
o Continuous presence of glucose in the urine
➢ Tx Algorithm
o Appropriate tx:
▪ Initial assessment is complex and includes an extensive hx about s/sx and:
• the chronic complications associated with diabetes
• current drugs being taken including OTCs
• alternative therapies that might affect BG levels
• family hx of DM, CVD, cerebrovascular disease, or dyslipidemia
• gestational hx
• ETOH of drug abuse
▪ Thorough PE including feet inspection
▪ Laboratory data – after PE
▪ THE RESULT OF THE ASSESSMENT WILL DETERMINE WHETHER AN INTENSIVE OR CONVENTIONAL THERAPY OR REFERRAL FOR COMPLICATIONS BE STARTED EARLY.
o T1DM
o T2DM
➢ Insulin therapy- daily dose on initiation
o Correction Factor (CF) and insulin:CHO ratio (I:C) for both T1DM and T2DM
o 1,500 rule:
▪ Enables the provider to find the CF, or
▪ how much 1unit of insulin will drop blood sugar for high BG levels (usually >140- 150)
▪ STEPS IN CALCULATION:
1. Calculate the total daily dose (TDD) of insulin = basal + bolus (50% each)
2. Divide 1,500 by TDD
o 500 rule:
▪ Enables the provider to find the I:C ratio.
▪ STEPS IN CALCULATION:
1. Calculate the total daily dose (TDD) of insulin = basal + bolus (50% each)
2. Divide 500 by TDD
➢ A1c tx goal
o Tx regimens that reduce average A1c (<7%) are associated with fewer long-term microvascular and neuropathic complications.
o Target of 6.5% - can be suggested to patients with low risk of hypoglycemia or adverse effects of tx.
➢ Mean plasma glucose level according to A1c
➢ Insulin tx algorithm for Type 1 DM
o T1DM requires insulin.
o Insulin tx pattern/type: intensive, split-mixed, continuous
o Total daily insulin requirement = 0.3 to 0.4 units/kg/d with titration to glycemic targets.
o Intensive insulin therapy:
▪ Not appropriate for patients who are less capable, risk for hypoglycemia
▪ Appropriate for patients who are intelligent, motivated, and reliable
➢ Clinical manifestations of diabetic autonomic neuropathy
o Diabetic Autonomic Neuropathy (DAN) is often insidious and screening for it may require several tests.
▪ Detailed hx
▪ Detailed PE
o Clinical S/Sx:
▪ Resting tachycardia
▪ Exercise intolerance
▪ Orthostatic hypotension
▪ Constipation
▪ Gastroparesis
▪ Erectile dysfunction
▪ Sweat gland dysfunction
▪ Impaired neurovascular function
o Cardiovascular Autonomic Dysfunction (CAN) is a CVD risk factor and is the most clinically important form of DAN.
➢ Hypoglycemia tx (e.g. amt of CHO)
o Hypoglycemia – BG < 70mg/dL
o Treatment – “The Rule of 15”
▪ When symptoms occur:
• Consume 15g of fast-acting CHO
o 4oz juice
o 8oz milk
o One-half can of regular soft drink
o 1tbsp honey
o 4-5 hard or soft candies
• Wait 15mins then Check BG
o Commercial use of glucose tablets or gel may be used.
o Chocolate candy IS NOT EFFECTIVE
o A small snack or small meal should be eaten within few hours of the hypoglycemic episode.
➢ Storage of insulin
o According to ADA (2020), the following are tips for storing insulin:
▪ Do not store insulin near extreme heat or extreme cold
▪ Never store insulin in the freezer, direct sunlight, or in the glove compartment of a car
▪ Check the expiration date before using, and don’t use any insulin beyond its expiration date
▪ Examine the bottle closely to make sure the insulin looks normal before you draw the insulin into the syringe.
➢ Drug monitoring with metformin
o Renal function- before initiating therapy, and at least annually thereafter
▪ Creatine Clearance (CCr)- initially
▪ Serum creatinine- annually
▪ more frequent for patients with risk for developing altered renal function.
➢ Antidiabetic meds and Photosensitivity
o Sulfonylureas can cause photosensitivity
➢ Antidiabetics to avoid in elderly and why
o Metformin- at risk for hypoglycemia and lactic acidosis (careful screening is a must)
▪ Often contraindicated to elderly due to renal insufficiency or presence of heart failure.
o Amylin agonists (pramlintide)- at risk for hypoglycemia
o Meglitinides- at risk for hypoglycemia
o Sulfonylureas- may cause severe hypoglycemia
▪ Chlorpropamide- long half-life and risk for prolonged hypoglycemia
▪ Glyburide- most likely to cause hypoglycemia and is not recommended for elderly
o TZDs:
▪ should be avoided in patients with symptomatic heart failure
▪ recent evidence shows that TZDs are associated with an increased risk of fractures in female patients.
▪ Since osteoporosis and heart failure are common comorbidities in older patients with diabetes, this may limit the use of TZDs somewhat.
▪ TZDs should be reserved for second- or third-line therapy in elderly patients with diabetes.
➢ Improving pt compliance with diabetes tx
o Lifestyle changes:
▪ place an emphasis on altered eating patterns, not “dieting”
▪ “exercise first” rather than “diet and exercise” mantra
▪ Educate patient about information regarding low- or no-cost diabetes meal planning and self-educational materials (websites like ADA, NIDDK)
o discuss the importance of adherence at each follow-up visit
o assist patients in removing barriers to adherence such as lack of social support and cost of tx regimen
o maximize team approach, make the patient as an active partner
➢ Diabetic meds to avoid when taking digoxin
o Acarbose (alpha glucosidase inhibitor) - may decrease digoxin levels
o Sitagliptin (DDP-4 or “gliptins”)- may increase serum concentration of digoxin
o Canagliflozin (SGLT-2 inhibitor)- increased AUC of digoxin
➢ Classes of diabetic meds
o Oral agents
▪ Biguanides, sulfonylureas, thiazolidinediones (TZD), Alpha glucosidase inhibitors, meglitinides, dipeptidyl peptidase-4 inhibitors (DPP-4), selective sodium glucose cotransporter 2 (SGLT-2) inihibitors
o Injectables
▪ Amylin agonists
▪ Glucagon-like peptide (GLP-1) agonists
▪ Insulin
➢ Diabetic meds with need of renal dose adjustment
o Alpha-Glucosidase inhibitors (acarbose, miglitol)
o Meglitinides (repaglinide, nateglinide)
o DPP-4 (gliptins)
➢ Diabetic meds associated with increased risk of genital mycotic infections
o Selective Sodium Glucose Co-Transporter 2 (SGLT-2) inhibitors
▪ canagliflozin (Invokana)
▪ dapglifoxin (Farxiga)
▪ empagliflozin (Jardiance)
[Show More]


.png)