*NURSING > STUDY GUIDE > Rasmussen College: PN3 Final Study Guide LATEST UPDATED,100% CORRECT (All)
Rasmussen College: PN3 Final Study Guide LATEST UPDATED,100% CORRECT
Document Content and Description Below
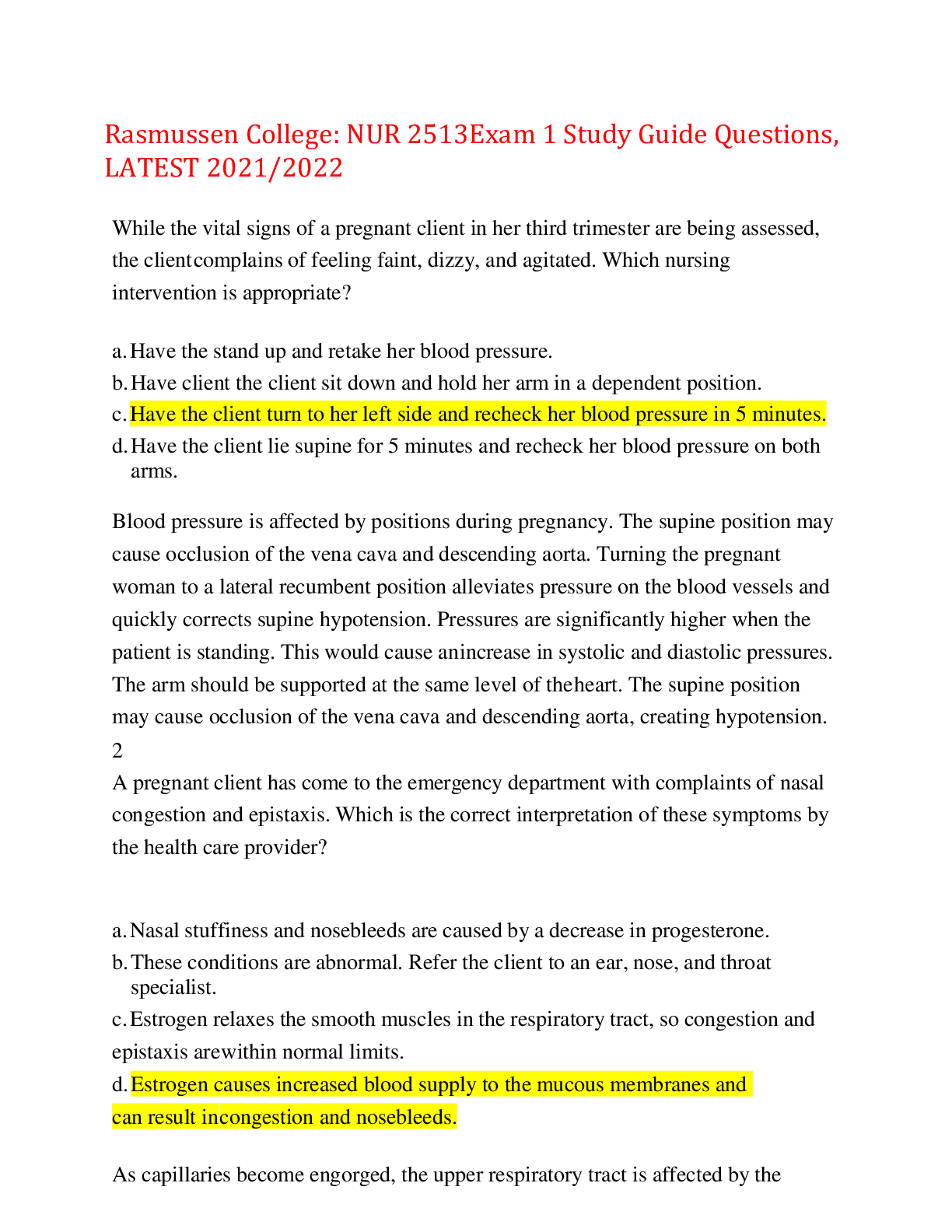
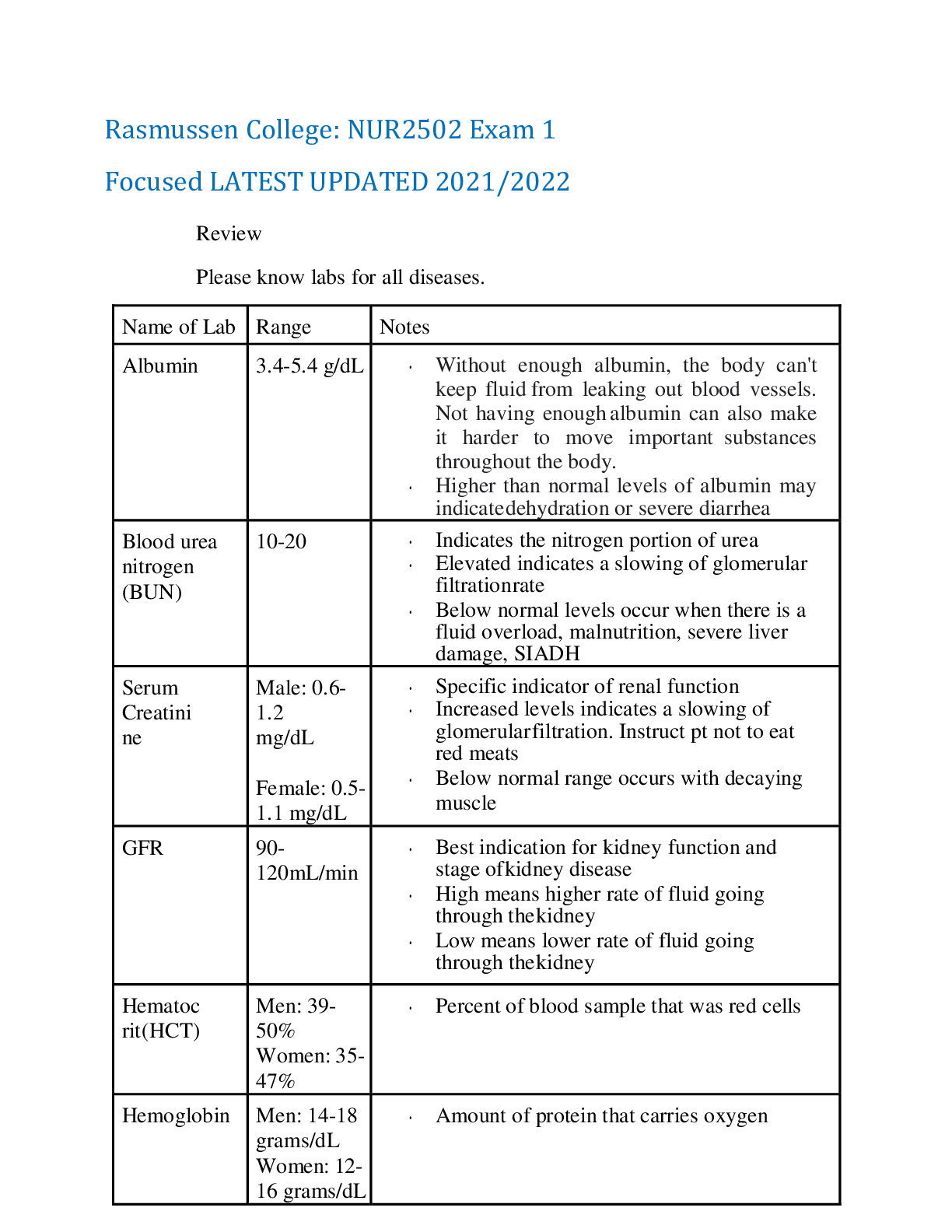
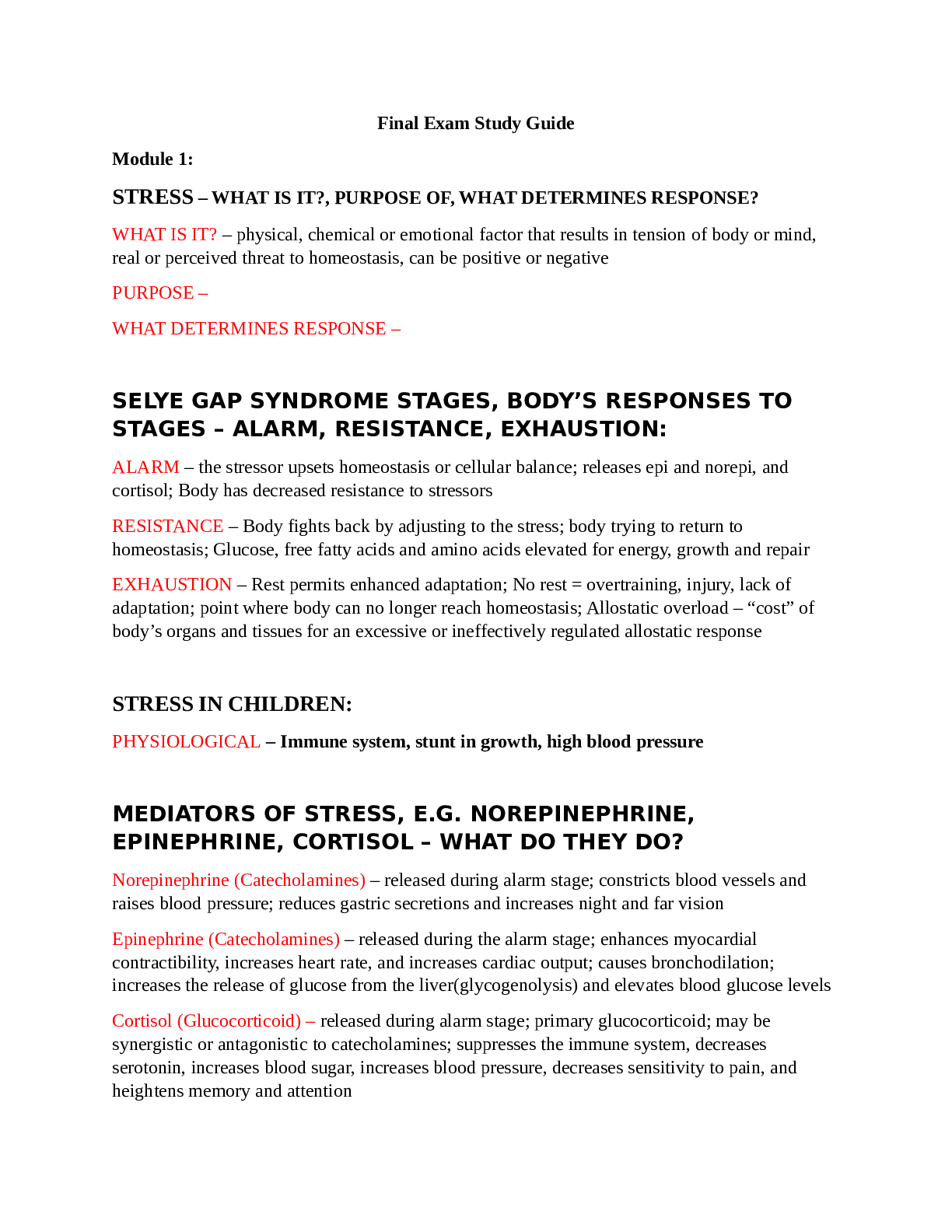
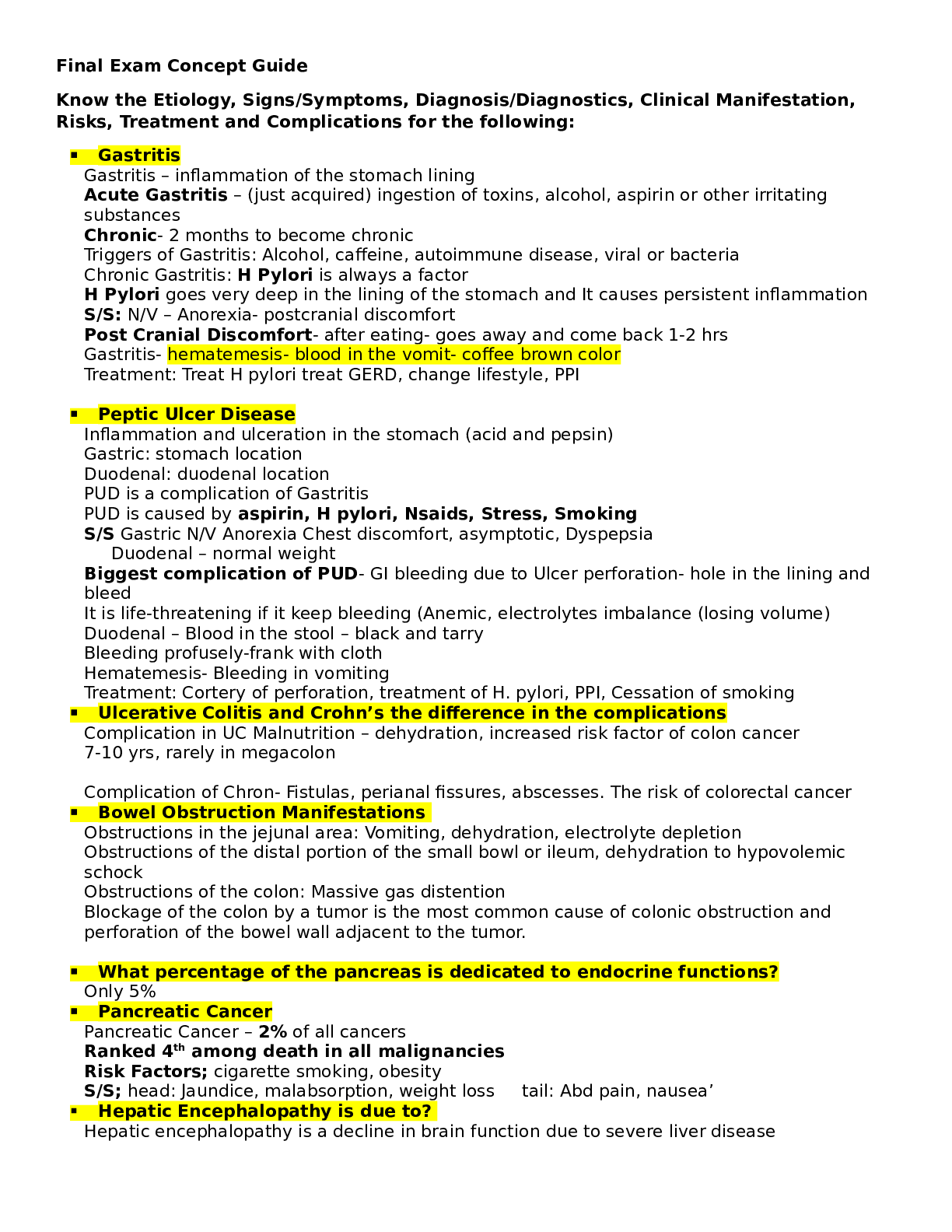
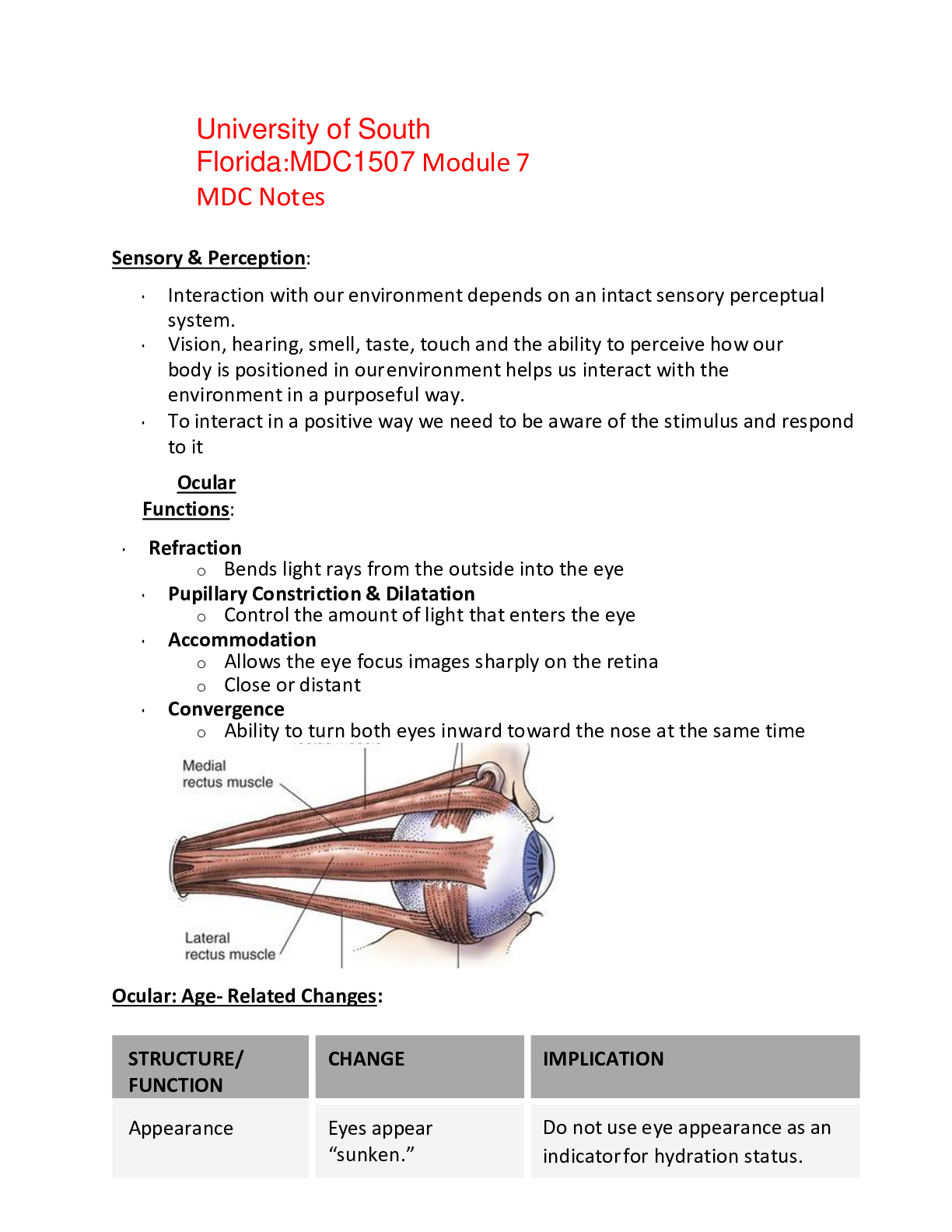
Rasmussen College: PN3 Final Study Guide LATEST UPDATED Professional Nursing III Final Exam Concept Guide Know and understand about the complications of chemotherapy • Cognitive funct ... ion=support and provide resources for cognitive training. Let them know other patients report it too. Warn against: excessive alcohol or drug use, head injury risks • Mucositis=oral cryotherapy (rest of interventions listed below) • Fatigue=space out and prioritize care • Alopecia=teach how to avoid scalp injury; coordinate wig purchases for patient based on income and lifestyle • N/v=give antiemetic’s BEFORE hand, during, and after. Keep on a schedule and educate patient to take them even when they feel okay. o Peppermint or ginger for relief Know thrombocytopenia and what precautions are necessary • Impaired clotting/bleeding; may require transfusion therapy o Precautions: ensure a safe environment for the patient and have bleeding precautions in place -electric razor, soft bristled toothbrush, don’t blow nose, no IM injections if possible, etc.… Know about internal /external radiation / brachytherapy Precautions for each • Internal/brachytherapy o The patient is a hazard ▪ Unsealed: enter body fluids and eliminated in waste products, making the waste radioactive ▪ Solid implants are in one place, the patient emits radiation but excreta is not radioactive. • Precautions: wear dosimeter badge, keep front of lead apron facing patient, no pregnant women or children under 16, visitors must stay 6 ft. away and limit visits to 30 min/day, never touch radioactive source with bare hands (use forceps), and save all dressings, bed linens until the radioactive source is removed; then dispose as usual. • External/teletherapy o Radiation delivered from a source outside of the patient. The source is external; therefore, the patient is not radioactive, and there is no hazard to others. Know basic labs such as CBC & Electrolytes, Pt, INR, and PTT • CBC o Hemoglobin: 13-17 o Hematocrit: 35%-48% • Electrolytes o K+: 3.5-5 o Na: 135-145 o Mag: 1.5-2.5 o Cal: 9-11 o Phosphorus: 2.5-4.5 • Clotting o Pt: 11-13.5 seconds o INR: 0.8-1.1 o PTT: 25-35 seconds Know how to treat low hemoglobin • Blood transfusion Know the drugs to treat low hemoglobin and platelets when getting chemo • Hgb: Epoetin alfa—can prevent or improve anemia and reduce the need for transfusions • Platelets: Oprelvekin (neumega)—increases platelet production by stimulating bone marrow (biologic response modifier) Know what mucositis is and how to treat during chemo and after chemo • Mouth sores caused by chemo o Tx—oral cryotherapy using ice chips before, during, or after rapid infusions of agents (vasoconstriction) ▪ Sodium bi-carb rinses, frequent oral assessments and hygiene • Soft bristled toothbrush, gentle flossing, saline rinse • IV injections of Palifermin—stimulates growth of mucous membranes in the mouth Know your burns • Phases o Resuscitation—onset24/48 hours o Acute—36/48 hours after—wound closure o Rehabilitation—wound closurehighest functioning BSA % ------Rule of 9’s How to differentiate each thickness • Superficial=leaves a good blood supply, pink and moist; blanches; painful • Partial thickness=blisters occur • Full thickness=eschar; not as painful How to treat burns • Monitor airway—assess by looking for drooling, trouble handling secretions, brassy cough, wheezing, or diminished breath sounds • Assess fluid resuscitation—urine output 30 mL/hr. • Assess for hypovolemic shock—monitor degree of edema and cardiac status • Assess for fluid shift hyponatremia and hyperkalemia • Give fluids—LR • Monitor electrolytes • Prevent infection (hand hygiene and standard precautions) • Drug management—morphine • Prevent gastric ulcers (curling’s)—H2 blockers, PPI’s (pantoprazole) Complications • Infection • Immobility contractures • Hypertrophic scarring Interventions • Rapid fluid therapy, oxygen therapy, pain management, antibiotic administration, CAM therapy, quiet environment, wound care management Know the Parkland Formula • 4 mL LR X BSA% X body weight (kg) o First half of solution over 8 hours o Second half over 16 hours Different types of triaging (Disaster & In hospital) What’s your priorities? The ranking system for each TRIAGE UNDER USUAL CONDITIONS TRIAGE UNDER MASS CASUALTY Emergent (immediate threat to life) Emergent—red tag Urgent (major injuries that require immediate treatment) Urgent—yellow tag Non-urgent (minor injuries that do not require immediate treatment) Non-urgent—green tag Does not apply Expected to die—black tag Understand stress debriefing after a mass casualty The different types • Two general types of debriefing occur after a mass casualty incident or disaster. o The first type entails bringing in critical incident stress debriefing (CISD) teams to provide sessions for small groups of staff to promote effective coping strategies. o The second type of debriefing involves an administrative review of staff and system performance during the event to determine whether opportunities for improvement in the emergency management plan exist. Know types of ventilators How to wean off Know high pressure and low-pressure alarms o Pressure cycled: pushes air into the lungs until a preset airway pressure is reached; used for short periods (bi-PAP) o Time-cycled: pushes air into the lungs until a preset time has elapsed o Volume-cycled: pushes air into the lungs until a preset volume is delivered; constant tidal volume is delivered • Weaning—mechanical breaths decrease from 12 to 2 HIGH pressure alarm LOW pressure alarm Secretions or mucus plugs Leak in ventilator Patient coughs, gags or bites ET tube Patient stops breathing with SIMV or Wheezing/bronchospasm CPAP Tube displacement Cuff leak of the ET Pneumothorax Increased PIP Obstruction of tubing Know and understand ARDS What it is • Persistent hypoxia even with oxygenation What are the signs & symptoms? o Refractory hypoxemia o Decreased pulmonary compliance o Dyspnea o Noncardiac-associated bilateral pulmonary edema o Dense pulmonary infiltrates on x-ray (ground-glass appearance) Who’s at risk? ▪ Often ARDS occurs after an acute lung injury (ALI) in people who have no pulmonary disease as a result of other conditions such as sepsis, burns, pancreatitis, trauma, and transfusion. Know your labs associated with heparin & Coumadin • HIT or heparin induced thrombocytopenia is a complication of this medication • Labs associated are platelets and aPTT o Therapeutic 1.5-2.5; control value (25-30 seconds 40-70 seconds) How to prevent venous thromboembolism • Anticoagulation therapy, mobilizing, pneumatic compression devices, SCD’s, ted hose, keep feet flat Know and understand Flail chest and how to treat it • Flail chest—fractures of at least 2 neighboring ribs in two or more places causing paradoxical chest wall movements o Tx—oxygen therapy, pain management, deep breathing and positioning, fluid secretion clearance by coughing and tracheal suctioning; possible mechanical ventilation Know what tension pneumothorax is and how to treat it • Life-threatening complication of pneumothorax in which air continues to enter the pleural space during inspiration and does not exit during expiration. As a result, air collects under pressure, completely collapsing the lung and compressing blood vessels, which limits blood return. o Tx— Initial management is an immediate needle thoracostomy, with a large-bore needle inserted into the second intercostal space in the midclavicular line of the affected side. A chest tube then is placed into the fourth intercostal space, and the other end is attached to a water- seal drainage system until the lung re-inflates. Know your rhythm strips and how to treat each rhythm Know what’s stable or unstable Rhythm EKG Treatment Sinus bradycar dia If stable, treat underlying cause If not, ATROPINE 0.5 mg IV Sinus tachycar dia Bedrest if hypotension or weakness is occurring. Avoid substances that increase the heart rate, such as caffeine Stress management strategies V-tach Cardioversion SVT *chest pain, SOB, palpitations, BP Adenosine Cardioversion V-fib After ensuring that v-fib is real… Cardioversion! A-fib *lightheaded Anticoagulants and calcium channel blockers (diltiazem/Cardize m) A-flutter *saw tooth Antidysrhythmic, anticoagulants, cardioversion, catheter ablation Asystole CPR! Know and understand pacemakers and complication with insertion • Consequences of a pacemaker: ▪ Stimulate an arrhythmia ▪ Pericardial effusion ▪ Infection ▪ Hematoma o Prolonged hiccups need immediate attention o Patient education and instruction for pacemakers • Don’t lift more than 10 pounds • Ensure microwave is working properly • No MRI • Let airport security know Know and understand about coronary artery disease • Broad term that includes chronic stable angina & acute coronary syndromes • It affects the arteries that provide blood, oxygen, and nutrients to the myocardium • When blood flow from the coronary arteries is partially of completely occluded it causes ischemia and infarction Treatment Type Typical s/s Treatment Chronic stable angina chest discomfort that occurs with moderate to prolonged exertion in a pattern that is familiar to the patient Nitro and/or rest Unstable: (new onset, variant (after rest), and pre-infarction) Chest pain or discomfort that occurs at rest or with exertion causing severe activity limitation Nitro, aspirin, beta blockers, EKG, PCI Myocardial Infarction (STEMI & NonSTEMI) chest pain, SOB, nausea EKG, MONA, PCI, CABG CABG and complications, patient education • CABG is indicated when patients do not respond to medical management of CAD or when disease progression is evident. o Complications: Fluid and electrolyte imbalance, Hypotension, Hypothermia, Hypertension, Bleeding, Cardiac tamponade, Decreased level of consciousness, Angina pain ▪ Patient education: Develop a teaching plan, which usually includes education about the normal anatomy and physiology of the heart, the pathophysiology of angina and MI, risk factor modification, activity and exercise protocols, cardiac drugs, and when to seek medical assistance. Teach patients that myocardial healing after an MI begins early and is usually complete in 6 to 8 weeks. Remind those who have undergone traditional CABG that the sternotomy should heal in about 6 to 8 weeks, but upper body exercise needs to be limited for several months. Know and understand Ventricular Remodeling after a MI Complications that can arise • Obvious physical changes do not occur until 6 hours after the infarction when the infarcted region appears blue and swollen • After 48 hours turns grey with yellow streaks as neutrophils invade tissue and begin to remove necrotic cells • 8 to 10 days granulation tissue forms at the edges of the necrotic tissue • 2 to 3 months the necrotic area develops into a shrunken, thin, firm scar permanently changing the size and shape of the left ventricle Know Cushing’s disease Signs & symptoms • Buffalo hump, protruding abdomen, moon face • Hypernatremia, hypokalemia Surgical treatment o Removal of pituitary tumor (Transsphenoidal hypophysectomy) Know SIADH Signs & symptoms • weakness, muscle spasms, diplopia, lethargy, confusion, speech and swallowing difficulties, and changes in pupil size and eye movement Treatment o Fluid restriction o Drug therapy (diuretics, vasopressin receptor antagonists) o Monitor for fluid overload Know what Pheochromocytoma is • A rare tumor of adrenal gland tissue. It results in the release of too much epinephrine and norepinephrine What is the cardinal sign? o HYPERTENSION ▪ Palpitations, severe headache, profuse sweating Know Addison’s disease Signs & symptoms • GI issues, salt craving, weight loss, weakness, bronze pigmentation of the skin Treatment o Hydrocortisone, fludrocortisone o Avoid fasting, increase salt intake Know Diabetes Insipidus Signs & symptoms • THIRSTY (dehydration s/s), considered if urine output is >4L in 24 hours and is greater than the amount ingested • Urine specific gravity to between 1.001 & 1.005 • Hypernatremia • Hypercalcemia • Hypokalemia Treatment o Desmopressin Know the different types of shock Type Signs/symptoms Caused by? Treatment/interventions Hypovolemic— Total body fluid decreased (in all fluid compartments). o BP o Flat veins o ↑ Resp. rate o Cyanosis o ↑Thirst o Urine output o lightheaded -dehydration -hemorrhaging IV, fluids, oxygen, elevate feet, keep head flat, examine and maintain pressure over bleeding, vasopressors Cardiogenic—heart muscle is unhealthy and there is a pumping problem o rapid breathing o SOB o tachycardia -MI -Pericarditis -dysrhythmias Fluids, vasopresssors Distributive— blood volume is not lost from the body but is distributed to the interstitial tissues where it cannot perfuse organs (anaphylaxis, sepsis, capillary leak syndrome) o septic: fever o anaphylactic: uticaria, wheezing o capillary leaking: bounding pulses Blood vessel dilation, pooling of blood in venous and capillary beds, and increased capillary leak. Fluids, epi, abx, steroids (depending on which type it is) Obstructive— problems that impair the ability of the normal heart to pump effectively. The heart itself remains normal. o Chest pain o Lightheaded o ↑HR o Shallow breath -cardiac tamponade Fluids and treating underlying cause Know what Disseminating Intravascular Coagulation • When SIRS becomes amplified, all tissues are involved and are hypoxic to some degree. Some organs are experiencing cell death and dysfunction at this time. Microthrombi formation is widespread, with clots forming where they are not needed. Who is at risk? o older adults, immunocompromised, or those with a central line How is it treated? ▪ correct cause, platelet replacement, bleeding control Know the different stages of shock What happens in each stage? Know MAP ⟶ INITIAL—MAP decreased by less than 10mmHg ▪ Difficult to detect at this stage r/t compensatory mechanisms are effective ▪ Increased HR, RR, slight INCREASE in systolic BP may be only signs ⟶ NONPROGRESSIVE—MAP decreases by 10-15mmHg ▪ Kidneys/hormones activated r/t cardiovascular mechanisms not able to maintain MAP ▪ renin, antidiuretic hormone (ADH), aldosterone, epinephrine, and norepinephrine ▪ urine output decreases, tissue hypoxia (not great enough to cause permanent damage), hyperkalemia, acidosis ▪ thirst, increased HR, RR, decreased BP ⟶ PROGRESSIVE—Sustained decrease in MAP of more than 20mmHg ▪ No longer oxygenation to vital organs (ischemic) ▪ Patient senses “something bad” “impending doom” ▪ Confused, thirsty, rapid/weak pulse, decreased BP, increased lactic/potassium, cyanosis, cool/moist skin, anuria ⟶ REFRACTORY/MODS ▪ Too much cell death/tissue damage have occurred despite interventions ▪ Trigger small clots—liver, heart, brain, kidneys lost first ▪ Loss of consciousness, nonpalpable pulse, cold/dusky extremities, slow/shallow RR Know acute kidney injury Causes o Blood loss, sepsis, septic shock, severe dehydration, burns, anaphylaxis, renal artery stenosis, nephrotoxic drugs, thrombi in kidneys, ingested toxins, certain cancers, kidney stones, Lupus Signs & symptoms ▪ Increased creatinine (normal: 0.5-1.2) ▪ Decreased urine output (oliguria) ▪ Edema ▪ Imbalance of electrolytes Treatment • Maintain fluid balance, kidney replacement therapy (dialysis) Know renal disease / renal failure Causes o Many different things; two common- diabetes and hypertension Signs & symptoms ▪ Metallic taste in the mouth, Anorexia, N/V, Muscle cramps, Uremic “frost” on skin, Itching, Fatigue and lethargy, Hiccups, Edema, Dyspnea, Paresthesia Treatment • Manage fluid volume, prevent pulmonary edema, prevent infection or injury, kidney replacement therapy (dialysis), controlling the disease that lead to its development, drug therapy, nutrition therapy, fluid restriction Know about dialysis What is does • removes excess fluids & waste products, restores fluid and electrolyte balance and acid-base balance Complications o Peritoneal— ▪ Peritonitis, Pain, Tunnel infections, Poor dialysate flow, Fibrin clot formation, Dialysate leakage Hemodialysis— ▪ Thrombosis or stenosis, Infection, Aneurysm formation, Ischemia, Heart failure, Clotting at AV site Know what Disequilibrium syndrome is with dialysis • Characterized by mental status changes and can include seizures or coma, although this severity of disequilibrium syndrome is rare with today's HD practice. A mild form of disequilibrium syndrome includes symptoms of nausea, vomiting, headaches, fatigue, and restlessness. It is thought to be the result of a rapid reduction in electrolytes and other particles. Reducing blood flow at the onset of symptoms can prevent this syndrome. Know what an AV fistula is How to assess it o Positive bruit o Palpable thrill What are the complications? ▪ Infection or clotting Know your different types of fractures Who is at risk for which fracture • Fragility/pathologic/spontaneous— occurs after minimal trauma to a bone that has been weakened by disease o At risk? Those with bone cancer or osteoporosis • Stress/fatigue— results from excessive strain and stress on the bone o At risk? Athletes and overuse • Compression— produced by a loading force applied to the long axis of cancellous bone o At risk? Older adults with osteoporosis • Open: bone exposed to air through break in skin (risk for infection) • Closed: skin intact Know the assessments and treatments for fractures • Determine type of injury, ask how it happened, obtain drug/alcohol use hx, and ask about recreational activities o Tx: after assessing airway, manage acute pain, immobilize, keep patient supine ▪ split, cast, immobilization devices, or traction Know how to treat pain with fractures • analgesics, nerve block, and immobilization Know what R.I.C.E. is and what the therapeutic benefit of each of it is Know how to educate for your patient for this • REST the injured part, immobilize the joint above and below the injury with a splint if needed • ICE intermittently several times a day for the first 24 to 48 hours (heat maybe used after that if it helps) • COMPRESSION for the first 24 to 48 hours with an elastic wrap • ELEVATE the affected limb higher than the heart for long periods as often as possible Know how to prevent Stress Fractures o You can help prevent stress fractures by wearing the appropriate athletic shoes for your activity. Make sure to not overdo training or exercise. Rest, especially when your muscles are tired. Condition your body for “spring training” before participating fully in any sport. Stop smoking, and eat a healthy well-balanced diet. Know about compression fractures Nonsurgical management • Analgesics • Bed rest • Nerve blocks • Physical therapy to maintain muscle strength Surgical management. • Vertebroplasty – bone cement injected through the skin directly into the fracture site to provide stability • Kyphoplasty – cavity-creating device such a balloon to partially re-expand a compressed vertebral body Know what traction is for fractures • Application of a pulling force to the body to provide reduction, alignment, and rest at that site The different types • Skin— applied by using elastic bandages or adhesive, foam boot, or sling • Skeletal— applied with pins, wires, or tongs; weight 25- 40 lbs. • Balanced suspension traction— system of pulleys, ropes and weights used to immobilize femur fractures • Dunlop’s traction— Used to align fx of the humerus (horizontal); vertical traction maintains the forearm in proper alignment • Buck’s (extension) traction—Used to immobilize a lower limb, alleviated muscle spasms; boot appliance is applied What is the purpose? ▪ Provides proper bone alignment and reduces muscle spasms How to assess for complications ▪ Asses for color, motion, and sensation; assess insertion sites for signs of infection Know the different types of embolisms • Fat embolism and venous thromboembolism What are the signs & symptoms? o Fat embolism: altered mental status, hypoxemia, dyspnea, and tachypnea; also petechiae o Venous thromboembolism: ^ same as fat except no petechiae Which conditions are risk factors for each type? ▪ Fat fractured pelvis or long bone ▪ Venous lower extremity surgery or trauma Understand the complications of fractures for ex: osteomyelitis, fat embolism & compartment syndrome How these complications are treated Know the different types of amputations • Elective: chooses to d/t issues such as: diabetes, peripheral vascular disease (PVD), arteriosclerosis, or numerous attempts to repair complex injuries • Traumatic: car crash, war, industrial accident What are the possible complications and how to prevent them? • Hemorrhage leading to hypovolemic shock ⟶ Control bleeding and fluid/electrolyte balance • Infection ⟶ Keep the site clean; use aseptic technique when handling • Phantom limb pain ⟶ Beta blockers, antiepileptic drugs, antispasmodics, and IV infusion of calcitonin. Opioids not as effective as they are for residual limb pain • Neuroma ⟶ Surgery to remove: although it often regrows and is more painful than before ⟶ Peripheral nerve blocks, steroid injections, and cognitive therapies such as hypnosis. • Flexion contractures ⟶ Proper positioning such as prone position every 3 to 4 hours for 20 to 30 minutes to prevent hip flexion contractures ⟶ Active range of motion exercises in the early post- operative period help to prevent this complication Know the different types of stroke including TIA (ischemic/hemorrhagic) ((Tx, risk factors, dx, s/s, complications and how to treat complications)) o TIA— Temporary neurologic dysfunction resulting from brief interruption in cerebral blood flow is easy to ignore or miss particularly if the symptoms resolve by the time the patient reaches the ED; typically symptoms of a TIA resolve in 30 to 60 minutes (up to 24 hours) ▪ Symptoms: Visual deficits Blurred vision Diplopia (double vision) Blindness in one eye Tunnel vision Mobility (motor) deficits Weakness (facial droop, arm or leg lift, hand grasp) Ataxia (gait disturbance) Sensory perception deficits Numbness (face, hand, arm, leg) Vertigo Speech deficits Aphasia (loss of ability to understand or express speech) Dysarthria (slurred speech) ▪ Prevention • Reducing high blood pressure (highest risk factor for stroke) • Antiplatelet drugs: aspirin, clopidrogrel [Plavix] • Controlling Diabetes: blood sugar within 100 mg/dl to 180 mg/dl • Lifestyle changes: quit smoking, increasing activity, healthy eating o Ischemic strokes: ▪ The two major interventions for ischemic stroke are: fibrinolytic therapy and endovascular interventions Alteplase (tPA), activase Endovascular – embolectomy Carotid artery angioplasty with stenting o Hemorrhagic: Vessel integrity is interrupted and bleeding occurs into the brain tissue or into the subarachnoid space ▪ *Often reports “worst headache of my life” • Nausea & vomiting • Photophobia • Cranial nerve deficits • Change in mental status or LOC ***risk factors for strokes include: hypertension, smoking/drinking, substance abuse, obesity, sedentary lifestyle, oral contraceptive use Know what the NIH scale is ▪ National Institute of Health Stroke scale o Evaluates severity of stroke; 11 assessment areas Know the drugs that are used to treat stroke & increased cranial pressure o Thrombolytics o Anticoagulants – particularly for Afib o Lorazepam, other antiepileptics for seizures o Calcium channel blockers – nimodipine (Nimotop) to prevent vasospasms o Most common after subarachnoid bleed o Stool softeners o Analgesics (for pain) o Antianxiety drugs Know the normal range of intracranial pressure - Normal ICP 10 to 15 mm/hg – treatment when 20 mm/hg usually as this is when neurons die What are the signs & symptoms of ICP ▪ H/A, deteriorating LOC, restlessness. Late sign - pinpoint or dilated pupils that are sluggish Know the cognitive, motor, & sensory deficits of stroke. Cognitive: ⟶ Changes in LOC ⟶ Decreased proprioception – sense of body position ⟶ Difficulty with language o Aphasia – difficulty speaking o Alexi or dyslexia – difficulty reading o Agraphia – difficulty with writing o Acaluclia – difficulty with math calculation Motor: Sensory: o Hemiplegia – paralysis on one side of the body o Hemiparesis – weaken on one side o Ataxia – gait disturbance o Hypotonia or flaccid paralysis – extremities fall when lifted o Hypertonia or spastic paralysis – increased muscle activity causing fixed position o Agnosia – inability to use an object correctly o Apraxia – inability to perform previously learned motor skills o Unilateral inattention (body neglect) syndrome – being unaware of paralyzed side o Ptosis – eyelid drooping o Hemianopsia – blindness in half of the visual field o Homonymous hemianopsia – blindness in the same side of both eyes o Nystagmus – involuntary movement of eyes o Parasthesias – numbness, tingling or unusual sensations. Know the different levels of the brain such as pia mater, arachnoid space, etc. Understand about aneurysms and arteriovenous malformations • An aneurysm is an abnormal ballooning or blister along a normal artery commonly developing in a weak spot on the artery wall. Larger aneurysms are more likely to rupture than smaller ones. • An arteriovenous malformation (AVM) is an angled collection of malformed, thin-walled, dilated vessels without a capillary network. This uncommon abnormality occurs during embryonic development. Vasospasm may occur as a result of a sudden and periodic constriction of a cerebral artery, often following an SAH or bleeding from an aneurysm or AVM rupture. This constriction interrupts blood flow to distal areas of the brain. Reduced perfusion from vasospasm contributes to secondary cerebral ischemia and further neurologic dysfunction. Know about brain tumors and signs & symptoms • Location o Primary tumors originate within central nervous system (CNS) o Secondary tumors from metastasis in other parts of body • Classification- benign, malignant or metastatic o Signs/symptoms o Headache – more severe on waking in the morning o Nausea and vomiting o Seizures o Impaired sensory perception o Dizziness, loss of balance o Weakness or paralysis o Changes in cognition, personality or mentation o Papilledema (swelling of the optic disc) indicates ICP Know hepatitis A, B, C & D Signs & symptoms How they are spread Which ones have vaccines? How are they treated? Hepatitis A Hepatitis B Hepatitis C Hepatitis D It is a hardy virus Has a core antigen, surface antigen Transmission is HDV (delta and survives on Spread by: blood to blood hepatitis) is human hands -Unprotected sex IV drug needle caused by a It is resistant to -Sharing razors or toothbrushes sharing (highest defective RNA detergents and acids -Needle sticks in health care incidence) virus that needs but can be workers Blood products or the helper function destroyed by bleach -Blood transfusions not screened organ transplants of HBV and high before 1992 Health care workers Usually develops temperatures -Hemodialysis (needle stick injury) into a chronic Usually a mild -Direct contact with open sores Unsanitary tattoo disease course similar to flu -Mother infecting infant during birth equipment Incubation period like symptoms The clinical course may be varied Unlike hepatitis B, is 14 to 56 days Spread by oral-fecal with symptoms of anorexia, most people with Spread same as route from person to vomiting, fever, fatigue, RUQ pain, hepatitis C do not hepatitis B person or dark urine with light stool, joint pain clear the virus and especially IV drug contaminated food and jaundice chronic infection users or water Usually occur with 25 to 180 days develops Sexual contact is Incubation period is after exposure Most people are also a high risk 15 to 50 days with Most recover, clear the virus from unaware they are peak at 25 to 30 their body and develop immunity infected and is days Small percentage do not develop detected in routine Usually not severe immunity and become carriers and blood work or when illness unless elderly can infect others liver problems or existing liver disease *vaccine available High risk for cirrhosis and liver cancer *vaccine available occurs Incubation period is 7 weeks Know and understand about liver disease Risk factors o Hepatitis and alcoholism, drugs/toxins, bile duct dz, and genetic disorders Signs & symptoms ▪ Jaundice, n/v, abdominal pain/swelling, edema, fatigue, easy bruising, dry skin, petechiae Treatment ⟶ Nutrition therapy—low sodium; Vitamin supplements such as thiamine, folate, and multivitamin preparations are typically added to the IV fluids because the liver cannot store vitamins. ⟶ Drug therapy—diuretics, beta-blocker (prevent bleeding), lactulose, metronidazole ⟶ Paracentesis ⟶ Respiratory support. How to diagnose ✓ MRI, CT, ultrasound Complications - Portal hypertension - Ascites and esophageal varices - Coagulation defects - Jaundice - PSE with hepatic coma - Hepatorenal syndrome - Spontaneous bacterial peritonitis Know and understand about liver cancer Risk factors o cirrhosis, HBV & HCV, alcoholism Signs & Symptoms ▪ Early stages without symptoms ▪ Late stages with weight loss, anorexia, RUQ discomfort Treatment - Surgical resection and liver transplant only long term tx How to diagnose ⟶ Alpha-fetoprotein (AFP) a tumor marker for cancers of the liver, testis, and ovaries are elevated; alkaline phosphatase also elevated ⟶ CT, Ultra Sound and Biopsy Complications - bile duct obstruction, anemia, or bleeding Know and understand about Lactulose and Liver disease o One of the drugs used to decrease ammonia levels is lactulose; a liquid that is given orally or in NG tube o Promotes the excretion of ammonia in the stool with a laxative effect o Prevent absorption of ammonia in the colon ▪ The desire effect is two to three soft stools per day and decrease in patient confusion Know about liver transplant and what disqualifies a patient • Advanced cardiac disease • Severe respiratory disease • Metastic tumors • Inability for compliance Understand about a liver biopsy and possible complications ▪ If coagulation is abnormal patient is high risk for bleeding o Prothrombin time and hemoglobin before procedure Know and understand about fatty liver • Caused by the accumulation of fats in and around the hepatic cells. It may be caused by alcohol use or other factors such as: diabetes, obesity, elevated lipid profile Know your labs associated with liver disease and pancreatitis o Liver: Serum levels of alanine aminotransferase (ALT)—most specific to the liver, aspartate aminotransferase (AST), and lactate dehydrogenase (LDH) typically are elevated because these enzymes are released into the blood during hepatic inflammation. o Serum Ammonia levels (normal 15 to 45 µ/dL (11 to 32 µmol/L) o PT / INR is usually prolonged o Albumin levels low (normal=3.4-5.4) o Pancreatitis: Blood amylase or lipase levels are typically elevated 3 times the normal level Know and understand about Pancreatitis / pancreatic cancer Risk factors o Pancreatitis: trauma, obstruction, alcoholism, viral infections, smoking, drug toxicity, cystic fibrosis, gallstones, abdominal surgery o Cancer: diabetes, cirrhosis, high intake of red meat, obesity, male gender, smoker Treatment ▪ Acute: NPO, hydration with IV fluids, pain control, drug therapy, NG tube ▪ Chronic: drug/nutrition therapy or surgical removal How to diagnose - Usually s/s are vague - Ultrasound and CT’s must be used to dx Complications ▪ Jaundice, anorexia, pain, glucose intolerance, splenomegaly, ascites Know the signs & symptoms associated with complications and conditions associated with liver dysfunctions - Jaundice (yellowing of the skin and mucous membranes) and Icterus (yellowing of the sclera) - Dry skin - Rashes - Purpuric lesions such as petechiae or ecchymosis - Palmar erythema - Spider angiomas - Ascites - Peripheral edema of the extremities and sacrum - Vitamin deficiency, especially fat soluble Vitamin A, D, E and K Know what cholecystitis / choleliathasis is • Inflammation of the gallbladder Signs & symptoms o Varying degrees of abdominal discomfort such as indigestion, constant pain in RUQ that may radiate to right shoulder or scapula o The severe pain of biliary colic is produced by the obstruction or movement of one or more stones o Indigestion, nausea, vomiting o Belching and flatulence o Feeling of abdominal fullness, rebound tenderness (Blumberg’s sign) o Jaundice, clay-colored stools, dark urine How it’s treated ▪ Non-surgical treatment: extracorporeal shock wave lithotripsy (ESWLL) to break up the stones ▪ Surgical management: Cholecystectomy laparoscopically is the gold standard (lap chole) Who’s at risk? - The four F’s – Female, Forty, Fat & Fertile - Women - Aging - Obesity - Rapid weight loss - Increased cholesterol levels - Hormone replacement therapy - Gastric bypass surgery - Diabetes - Pregnancy Know what Ascites is • Collection of fluid within the peritoneal cavity caused by hydrostatic pressure from portal hypertension • Massive ascites can cause renal vasoconstriction, triggering the renin-angiotensin system resulting in sodium and water retention o Risk of developing spontaneous bacterial peritonitis How to treat it ▪ Low sodium diet (early stage) ▪ IV replacement of thiamine, folate and multivitamin (liver cannot store vitamins) ▪ Diuretic and possibly potassium supplement depending on choice of diuretic. Sometimes Lasix and spironolactone in combination ▪ Paracentesis with a trocar catheter to remove fluid from the peritoneal cavity In class review: 1) Compound fracture—open 2) Closed-skin intact 3) Pathologic—d/t osteoporosis or cancer 4) Stress fx—lighten up on intensity; d/t overuse 5) Patient got cast and in pain=acute compartment syndrome 6) Capillary refill= less than 3 seconds 7) Compartment syndrome a. How many p’s?=6 o Pain o Pallor o Paresthesia’s o Paralysis o Pulselessness o Pressure 8) What impedes healing for a fx? Disease that caused it 9) Which fx has fat embolism=long bone, pelvis, and hip; starts with a fat globule which causes it; hypoxemia, petechiae, neuro issues (also pulmonary embolism) a. Restlessness, confused, altered LOC, low 02 saturation, ABG’s off, dyspnea, tachypnea 10) Fat embolism come from contrast dye; although rare 11) Which fx is when an older adult has a fx before they fall? Pathological fx a. d/t osteoporosis 12) before they cast someone, they will often splint them for a few days to allow the swelling to go down, so the cast fits properly 13) priority questions 14) compartment syndrome; fasciotomy; look for pulses, increased pain, and color 15) ibuprofen a. bleeding precaution; take with food 16) Concerned about circulation in an arm? Check what? a. Distal pulses (radial) or pedal pulses if concerned with leg circulation 17) What if someone has wound drainage? a. Wound culture to ensure they’re receiving right abx 18)What is ischemic stroke? Blocked vessel; thrombosis or clot causes occlusion a. Carotid artery is involved too 19) NIH to assess stroke 20) Ischemic stroke? Alteplase (tPa) 21)Hemorrhagic stroke—caused by aneurysm or arteriovenous malformation (cluster of arteries and veins) a. Worst headache of life; sudden b. Visual…photophobia, mental status change, n/v 22) Patient has increased ICP? a. Elevate HOB 30 degrees i. Any injury to brain increases risk for ICP (anoxia, stroke) at risk for cerebral edema ii. Doesn’t happen instantly; usually over time before s/s show 23) Aphasia—unable to speak or comprehend language 24) Ataxia—gait disturbance 25) Leading cause of death after head injury? ICP 26) s/s of brain tumor a. severe headache in morning 27) TIA a. Symptoms resolves within 24 hours (this is how you define it) 28) Know ischemic (facial drooping, arm drop, right sided numbness) vs hemorrhagic (sudden headache, photophobia) 29) How do you know ICP? Restless, change in mental status, headache, agitation 30) Know rules of ischemic stroke a. They can’t have fibrinolytic? Know perimeters!!! i. the blood pressure must be below 185/110 1. if not, the patient must be given rapid acting antihypertensive meds such as labetalol or nicardipine ii. Age older than 80 years iii. Anticoagulation regardless of international normalized ratio (INR) iv. Imaging evidence of ischemic injury involving more than one third of the brain tissue supplied by the middle cerebral artery v. Baseline National Institutes of Health Stroke Scale score greater than 25 vi. History of both stroke and diabetes 31) What typically causes brain bleeds? Aneurism and AVM 32) Hep A—fecal oral; dirty water/food a. Protection? VACCINE 33) Hep B—sex, IV drugs, a. Protection? VACCINE 34) What causes liver disease? a. The most common causes for cirrhosis in the United States are chronic alcoholism, chronic viral hepatitis, nonalcoholic steatohepatitis (NASH) or fatty liver, bile duct disease, and genetic diseases 35) Encephalopathy? Elevated Ammonia—reverse with lactulose 36) Paracentesis? Drains fluid a. At risk for infection and bleeding; check HgB, platelets and INR beforehand 37) Mannitol for ICP 38) Pancreatitis—NPO, rest pancreas a. Elevated amylase and lipase b. IV fluid administration 39) Cirrhosis—liver transplant for cure 40) Advanced directive 41) Sign of liver disease a. Icterus, jaundice, palmar rash, spider angiomas, esophageal varices i. #1 cause=alcoholism 42) Know the 5 f’s—cholecystitis a. Fat, female, fertile, fair skin, forty 43) Cheyne-stokes=rapid shallow breathing followed by apnea a. An abnormal pattern of breathing characterized by progressively deeper, and sometimes faster, breathing followed by a gradual decrease that results in a temporary stop in breathing called an apnea. The pattern repeats, with each cycle usually taking 30 seconds to 2 minutes. 44) Pain with gall stones? Right upper quadrant 45) Pancreatic cancer? Hard to dx 46) Worried about cancer pt? prevent infection; neutropenic precautions 47) Chemo after radiation? a. To finish killing cancer cells 48) Epoetin— RBC stimulant; anemia tx 49) Precautions for brachytherapy patients 50) Platelet count, CBC 51) How do we triage in disaster? 52) Rule of nines 53) Burn pt—airway, fluid resuscitation, pain 54) When do we start parkland? At time of injury 55) Properly hydrated? Urine output; 30 mL per hour 56) Experienced nurse for triage 57)Mechanically ventilated? Curling’s ulcer; PPI (pantoprazole) a. Vent alarms; high or low 58) Flail chest—2 or more fractured/broken ribs in an area a. Paradoxical chest movements; causes breathing disturbances; could possibly intubate 59) Shock types; obstructive and cardiogenic (MI) 60) MI—EKG 61) Atropine—symptomatic bradycardia 62) What are we worried about with clot buster? Bleeding a. MI patients can have tPA 63) s/s Cushing’s 64) know SIADH 65) Addison’s 66) diabetes insipidus—dehydration & electrolyte imbalance 67) small cell lung cancer—SIADH 68) DIC—coagulation problem 69) What causes distributive? Anaphylaxis, sepsis, neurogenic (spinal/head) 70) Chronic kidney disease? Low protein 71) Kidney injury? Creatinine and decreased urine output 72) Differences between hemodialysis and peritoneal dialysis 73) Dosage calculations 74) EKG strips • Brain tumor s/s to report: o New onset of seizures o one-sided weakness o loss of balance o problem with vision o inability to talk • Recovering TBI instructions: o Acquire medical clearance before returning to work that uses heavy equipment o Limit alcohol o Eat well balanced diet o Avoid all illicit street drugs • Nurse assessing adequacy of ventilation o O2 98% o Nail beds pink with good capillary refill o Quiet, effortless breath sounds at bases of lungs bilaterally • Client recovering from pelvic fx, becomes restless with dyspnea; concerned with fat emboli when which s/s assessed? o Upper body petechiae o Seizures o Temperature 102 degrees • Patient hyperventilating; s/s respiratory alkalosis o Tingling fingertips o Numbing around mouth o Cramping of feet • Liver d/o o Low vitamin A o Increased bleeding o Poor digestion of fats o Insulin resistance o Nerve damage • Septic shock; do what first? o Obtain 2 blood cultures • Reasons a patient might refuse pain meds o Fear that pain means disease is worse o Fear of addiction o Fear of side effects o Concerns of being a bad patient • Cancer cell characteristics o Aneuploidy o Migratory o Poorly differentiated o Abnormal chromosomes • Pyelonephritis interventions o Ensure adequate hydration o Monitor vitals and fluid balance o Provide urinary aseptic o Monitor electrolytes and creatinine clearance • Chronic renal failure manifestations o Anemia o Constipation o Restless legs o Left ventricular dysfunction o Prickle or burning sensation of extremities • 1) A client with a new burn injury asks the nurse why he is receiving intravenous cimetidine (Tagamet). What is the nurse’s best response? “This will help prevent stomach ulcers, which are common after burns.” • 2) The nurse is assigned a group of patients. Which patient would the nurse identify as being at increased risk for impaired gas exchange? A patient with a hemoglobin of 8.5 g/dL • 3) The nurse is assessing a patient for the adequacy of ventilation. What assessment findings would indicate the patient has good ventilation? (Select all that apply.) ---- 1. Oxygen saturation level is 98%. 2. Nail beds are pink with good capillary refill. 3. There is presence of quiet, effortless breath sounds at lung base bilaterally. • 4) The nurse is assessing a patient's differential white blood cell count. What implications would this test have on evaluating the adequacy of a patient's gas exchange? Elevation of WC = generalized inflammation • 5) The nurse would identify which patient as having a problem of impaired gas exchange secondary to a perfusion problem? A patient with Peripheral artery disease of LE • 6) A client is in the emergency department after being rescued from a house fire. After the initial assessment, the client develops a loud, brassy cough. What intervention by the nurse takes priority? Apply oxygen and continuous pulse oximetry. • 7) The nurse would identify which body systems as directly involved in the process of normal gas exchange? (Select all that apply.) Cardiovascular system, pulmonary system, Neurologic. • 8) The RN has assigned a client who has an open burn wound to the LPN. Which instruction is most important for the RN to provide the LPN? Wash hands on entering the client’s room. • 9) The acid-base status of a patient is dependent on normal gas exchange. Which patient would the nurse identify as having an increased risk for the development of respiratory acidosis? A patient with ---- Chronic lung disease with ↑CO2 retention • 10) A client who weighs 90 kg and had a 50% burn injury at 10 AM arrives at the hospital at noon. Using the Parkland formula, calculate the rate that the nurse should use to deliver fluid when the IV is started at noon. • ---- 4ml/Kg/%TBSA per 24 hours 4 X 90 = 360 X 50 = 18,000 ---- Give half in first 8 hours 9,000/8 and second half in 16 hours 9,000/16. • HOWEVER!!!! (Burn at 10am and its noon, so 6 hour infusion needed) 9,000 / 6 = 1,500mL/hr • SVT med= adenosine • Unstable SVT=cardioversion • Which med decreases heart contractility and decreases the demand for myocardial oxygen demand? [Show More]
Last updated: 3 years ago
Preview 1 out of 32 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 28, 2022
Number of pages
32
Written in
All
Additional information
This document has been written for:
Uploaded
Feb 28, 2022
Downloads
0
Views
131