NUR 2063 Final REVISED Final Exam Study Guide Patho Spring 2020
Final Exam Concept Guide
Know the Etiology, Signs/Symptoms, Diagnosis/Diagnostics, Clinical Manifestation, Risks, Treatment and Complications for the foll
...
NUR 2063 Final REVISED Final Exam Study Guide Patho Spring 2020
Final Exam Concept Guide
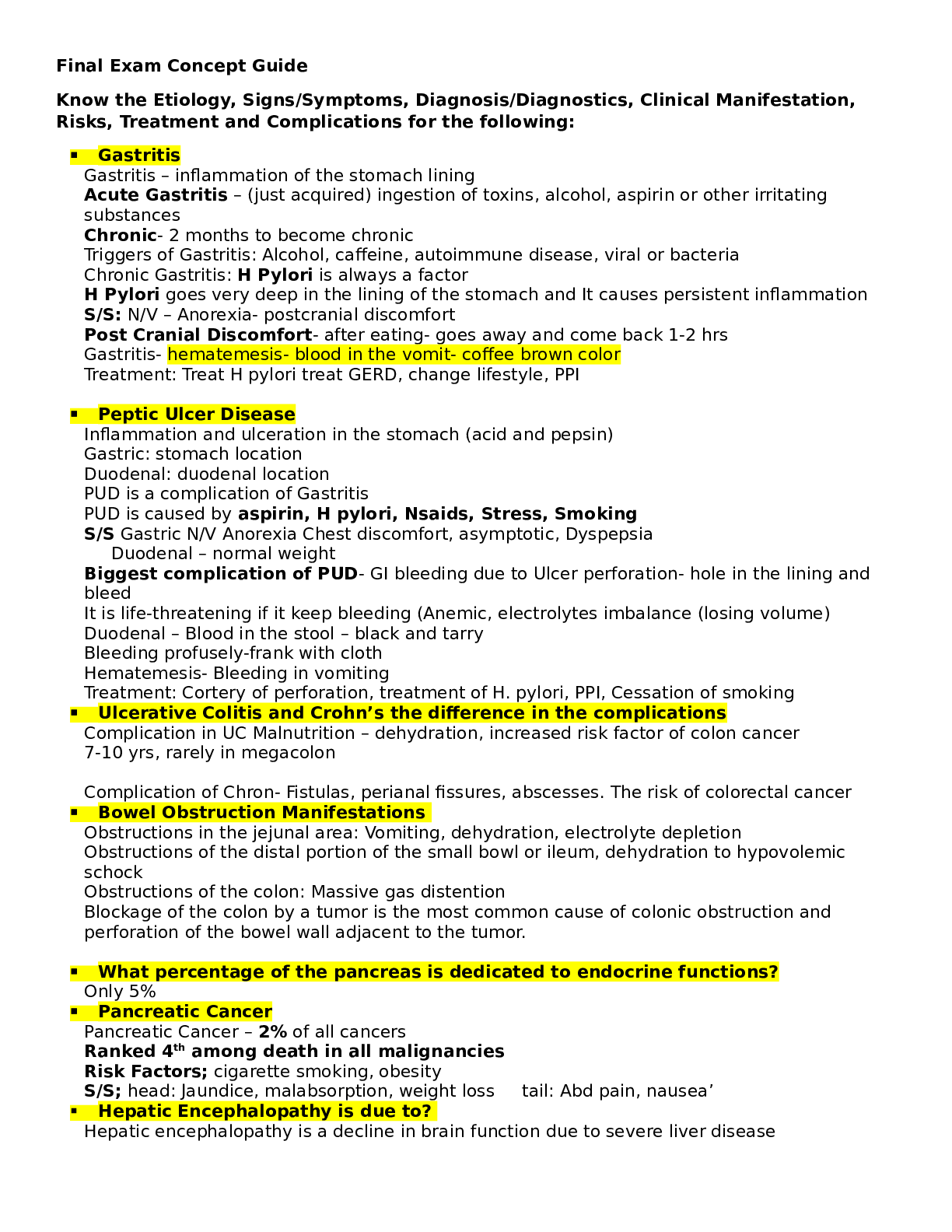
Know the Etiology, Signs/Symptoms, Diagnosis/Diagnostics, Clinical Manifestation, Risks, Treatment and Complications for the following:
▪ Gastritis
Gastritis – inflammation of the stomach lining
Acute Gastritis – (just acquired) ingestion of toxins, alcohol, aspirin or other irritating substances
Chronic- 2 months to become chronic
Triggers of Gastritis: Alcohol, caffeine, autoimmune disease, viral or bacteria Chronic Gastritis: H Pylori is always a factor
H Pylori goes very deep in the lining of the stomach and It causes persistent inflammation
S/S: N/V – Anorexia- postcranial discomfort
Post Cranial Discomfort- after eating- goes away and come back 1-2 hrs Gastritis- hematemesis- blood in the vomit- coffee brown color
Treatment: Treat H pylori treat GERD, change lifestyle, PPI
▪ Peptic Ulcer Disease
Inflammation and ulceration in the stomach (acid and pepsin) Gastric: stomach location
Duodenal: duodenal location PUD is a complication of Gastritis
PUD is caused by aspirin, H pylori, Nsaids, Stress, Smoking S/S Gastric N/V Anorexia Chest discomfort, asymptotic, Dyspepsia
Duodenal – normal weight
Biggest complication of PUD- GI bleeding due to Ulcer perforation- hole in the lining and bleed
It is life-threatening if it keep bleeding (Anemic, electrolytes imbalance (losing volume) Duodenal – Blood in the stool – black and tarry
Bleeding profusely-frank with cloth Hematemesis- Bleeding in vomiting
Treatment: Cortery of perforation, treatment of H. pylori, PPI, Cessation of smoking
▪ Ulcerative Colitis and Crohn’s the difference in the complications Complication in UC Malnutrition – dehydration, increased risk factor of colon cancer 7-10 yrs, rarely in megacolon
Complication of Chron- Fistulas, perianal fissures, abscesses. The risk of colorectal cancer
▪ Bowel Obstruction Manifestations
Obstructions in the jejunal area: Vomiting, dehydration, electrolyte depletion Obstructions of the distal portion of the small bowl or ileum, dehydration to hypovolemic schock
Obstructions of the colon: Massive gas distention
Blockage of the colon by a tumor is the most common cause of colonic obstruction and perforation of the bowel wall adjacent to the tumor.
▪ What percentage of the pancreas is dedicated to endocrine functions?
Only 5%
▪ Pancreatic Cancer
Pancreatic Cancer – 2% of all cancers
Ranked 4th among death in all malignancies Risk Factors; cigarette smoking, obesity
S/S; head: Jaundice, malabsorption, weight loss tail: Abd pain, nausea’
▪ Hepatic Encephalopathy is due to?
Hepatic encephalopathy is a decline in brain function due to severe liver disease
Hepatic encephalopathy is usually precipitated by certain well-defined clinical developments, including hypokalemia, hyponatremia, alkalosis, hypoxia, hypercarbia, infection, use of sedatives, GI hemorrhage, protein meal gorging, renal failure, and constipation. In some patients, progressive liver failure leads to chronic encephalopathy without other exacerbating factors.
Hepatic encephalopathy is graded 1 to 4:
• Grade 1: Confusion, subtle behavioral changes, no flap
• Grade 2: Drowsy, clear behavioral changes, flap present
• Grade 3: Stuporous but can follow commands, marked confusion, slurred speech, flap present
• Grade 4: Coma, no flap
▪ Gastroesophageal Varices Management
Initial treatment: Fluid resuscitation to stop bleeding Large bore intravenous lines are placed
Admin of parenteral vitamin K and plasma, platelet infusion if thrombocytopenia is present
Octreotide acetate (synthetic analog) no more vasopressin 3-5 days Metoclopramide and B blockers
Esophagogastroduodenoscopy EGD to determine site of bleeding
▪ Difference between Diverticulosis and Diverticulitis
Diverticulosis (diverticular disease) presence of diverticula in the colon.
Diverticula are acquired herniations of the mucosa and submucosa through the muscular coat of the colon
Diverticulosis The presence of one or more diverticula vs diverticulitis inflammation of one or more diverticula
▪ Kidney Disease- Assessment-CVA
Pain associated with intrarenal disorders are assessed by palpating or light percussion over the costovertebral angle (CVA) posteriorly and is recorded as CVA tenderness. Pain is transmitted to the spinal cord between T10 and L1
▪ Kidney Cancer signs and symptoms
Benign renal neoplasm: S/S Hematuria and flank pain Some may be asymptomatic until large
Renal cell carcinoma: Metastatic disease
Risk factors: smoking, obesity and hypertension S/S CVA tenderness, hematuria, palpable mass
▪ Dialysis- Benefits and Risks
▪ Filter blood and rid the waist
Dialysis is the only therapeutic option for those with ESRD unable to obtain transplant Each treatment of dialysis remove about 2/3 of the total body urea content
Dialysis maintain volume status
Prevent and treat acid-base and electrolyte disturbances Prevent and treat uremia
Support nutritional needs. Prevent and treat infection Orevent and treat anemia Improve quality of life
Lower mortalty and morbidity rates Control pains
VS
RISKS
Electrolytes imbalance (potassium and sodium) -need to check hyper or hypo
Low blood pressure (have to check vitals before and after) Risk for infection
Long-term mobidity Life threatening
Cardiovascular disease remained the most common cause of death in ESRD patient
▪ Acute Kidney Injury- Three phases- Prodromal- Oliguric- Postoliguric
Prodomal Phase
- Normal or declining urine output
- Serum blood urea nitrogen (BUN) and creatine levels rise Oliguric phase (10-14 days) range from 1 day to 8 weeks
- Oliguria – Small abnormal amount of urine
- Edema, Hypertension, Hypervolemia
- Distended neck veins, weight gain
- Crackles, possibly heart faily
- WBC and RBC in urine
- Protein in urine
- Hyperkalemka
- Volume overload
- Azotemia and uremia
- Metabolic acidosis Postoliguric phase (5% recover)
- Fluid volume deficit
- Labs begin to normalize
- Polyuria – sodium waste
▪
▪ Acute Tubular Necrosis and the causes of Acute Tubular Necrosis
ATN is the result of tubular cell injury
- Ischemia: Exposure to nephrotoxic substances
- ½ of all cases of AKI
Nephrotoxins leading cause of ATN (aminoaglycosides, NSAIDS, amphotericin B, cisplatin, tetracycline.
CI- AKI or Contrast-induced nephropathy
▪ Cystitis- signs and symptoms
(inflammation of the bladder) no fever or flank pain If fever is present – Might be infection (UTI)
Confusion Cloudy urine Frequency Urgency Dysuria
Intrarenal Kidney Injury- Toxic causes of
Box 28.1
Types of Acute Kidney Inj ury Prerenal
• • Absolute decrease in circulating volume
o • Hemorrhage
o • Dehydration
o • Burns
• • Relative decrease in circulating volume
o • Distributive shock (neurogenic, anaphylactic, septic)
o • Third-spacing and edema
o • Decreased cardiac output
▪ • Cardiogenic shock
▪ • Dysrhythmias
▪ • Cardiac tamponade
▪ • Heart failure
▪ • Myocardial infarction
• • Primary renal hemodynamic abnormalities
o • Occlusion or stenosis of renal artery*
o • Drug-induced impairment of renal autoregulation in susceptible persons†
Postrenal
• • Benign prostatic hyperplasia
• • Kinked or obstructed catheters
• • Intraabdominal tumors
• • Strictures
• • Calculi
Intrarenal/Intrinsic
• • Tubular (acute tubular necrosis)
o • Ischemic
▪ • Prolonged prerenal failure
▪ • Transfusion reactions
▪ • Rhabdomyolysis
o • Nephrotoxic
▪ • Prolonged postrenal failure
▪ • Certain antimicrobials (antibiotics; antifungal and antiviral drugs)
▪ • Radiographic contrast media
▪ • Certain cytotoxic chemotherapy agents
▪ • Recreational drugs (amphetamines, heroin)
▪ • Environmental agents (heavy metals, carbon tetrachloride, insecticides)
▪ • Snake and insect venom
• • Glomerular
o • Acute glomerulonephritis
• • Interstitial
o • Acute allergic interstitial nephritis
o • Acute pyelonephritis
• • Vascular
o • Vasculitis
o • Emboli
o • Nephrosclerosis (due to primary hypertension, hypertensive emergencies, and urgency)
▪
▪ Two electrolytes that are affected by the kidney’s inability to regulate.
Potassium and Sodium Hypokalemia and Hyponatremia
▪ Renin-Angiotensin-Aldosterone System and the relationship between the autoregulation of the kidneys
Renin-Angiotensin-Aldosterone System (RAAS) act to increase the total circulating volume in the kidney attempt to autoregulate perfusion and maintain GFR.
▪ What is the Glomerelus?
▪ It is a segment of nephron that filters fluid from blood into Bowman capsule, prevents passage of blood cells and proteins.
▪ What is Glomerulonephritis?
▪ An assortment of immune-mediated conditions that produce inflammation of the glomeruli.
▪ Diabetes Type I and Type II
Type 1: Destruction of the B cells of the pancreas results in absolute insulin deficiency 5-20 yrs
Chromosone 6
Type 2: Most common form of DM – Insulin resistance and B cells dysfunction lead to a resistance lack of insulin
Risk factor: Female sex, obesity, and sedentary lifestyle
Risk factor: non Caucasian, elderly
▪ Poly’s of Diabetes
▪ 3 P : Polyuria, Polyphagia, Polydipsia
▪ Cushing’s Syndrome characterized by
Cushing Adrenocortical Syndrome Insufficiency
Truncal
obesity Moon face Dorsocervical
fat pad Hirsutism Muscle
wasting Striae Petechiae Glucose
intoleranc e
Hypertension Hypokalemia Weakness Hypotension Hypoglycemia Hyperpigmentatio
n (Addison disease)
Hyperkalemia Weight loss
▪ Traumatic Brain Injury
➢ Traumatic brain injury (TBI) refers to injuries of brain tissues sustained as a consequence of trauma
➢ Traumatic brain injury == head injury
➢ Injuries to the cranials ≠ not always brain injury
➢ TBI is the leading cause of death and disability in the U.S. 50,000 + yr
➢ Causes TBI (falls, sports injuries, firearms, and transportation-related trauma)
➢ Fall majority for 0-4 or 65+, motor vehicle TBI – 14-24 yr. Men are more likely to die than women
➢ Types of TBI:
▪ Severity
▪ Location
▪ Mechanisms of injury
➢ Severity of TBI is classified by Glasgow coma scale (CGS) (standardized tool developed for the purpose assessing the LOC in acutely brain-injured patients. To evaluate patient with an altered LO
➢ Glasgow coma scale: Mild score (13-15), Moderate (9-12), severe (8 – below)
➢ Primary injury- initial trauma injury on brain cells
- Focal injuries (coup)
- Polar injuries (coup contrecoup)
- Diffuse injury
In addition, as location, Primary Injury can also differentiated by Mechanism of injury
- Concussion
- Contusion
- Intracranial hematoma.
Concussion also known as Mild traumatic brain injury (MTBI) most common for military and athletes. Alterations or LOC≤30 mn but no evidence of brain damage on CT.
Symptoms: Headache, n/v, dizziness, fatigue, blurred vision, cognitive, emotional disturbances
Contusion CT or MRI reveals area of Brain Tissue damage (necrosis, laceration, bruising)
Intracranial hematoma: Localized collection of blood within the cranium. Three types; Epidural, subdural, subachnoid.
Secondary Injury : Body’s response to initial injury may cause more harm than the initial injury.
Can cause: Ischemia, hypoxic events, vasogenic/neurogenic edema, and other processes that leads to brain swelling and increased ICP.
Treatment: Cardiopulmonary stabilization. Radiologic screening, maintenance of normal body temperature or mild hypothermia, normal PaCO2, normal glucose level and noema intravascular volume recommended. Acutely elevated ICP, mannitol(osmotic diuretic) sedation, hypothermia and mild hyperventilation.
▪ Reperfusion Injury- Definition
Reperfusion injury is the secondary injury that occurs after reestablishing blood flow
▪ Increased Cranial Pressure- ICP
▪ ICP is the pressure exerted by the contents of the cranium and normal ranges from 0-15 mmhg
The volume of the cranium nerve is made up 3 parts: brain tissue, cerebrospinal, blood Monroe-kellie hypothesis – the relationship between the 3 components of cranium Compliance – the ability to accommodate changes in volume w/o sign. Increase in pressure The most common causes of ICP: stroke, trauma and tumors
▪ Most sensitive indicator of altered brain function?
A change in Level of consciousness LOC is one of the most sensitive indicators of altered brain function
▪ Assessment of the brainstem function- How do you assess it?
Pupil light reflex Oculovestibular reflex Corneal reflex
▪ CVA- Types and causes
Transient ischemic attack (TIA) – Episodes of stroke s/s with a duration of less than 24 hr and less
than1hr (30% pt with stroke have prior TIA) Ischemic stroke- Sudden occlusion of cerebral artery secondary to thrombus formation/embolization
- Thrombotic strokes: atherosclerosis and hypercoagulable states
- Embolic strokes: cardiac sources
Hemorrhagic stroke = Hemorrage within the brain parenchyma and after a severe and long- standing
Hypertension. (30 % mortality rate)
▪ Test used to diagnosed CVA
Non-contrast CT scan /diffusion weighted brain MRI
▪ Meningitis what is it?
Meningitis is the pyogenic infection that invades the leptomeninges and the subarachnoid space.
the most comment sequela to microbial invasion of the CNS. (most bacterial but can be viral/fungal)
Bacteria: Streptoccocus pneumoniae
▪ Encephalitis What is it?
Encephalitis is the inflammation of the brain caused by viruses, bacteria, fungi and parasites
▪ Seizures- how they are classified?
1. Generalized seizures: Entire brain Surface
• Absence (petit mal)
• Atypical absence
• Myoclonic
• Atonic (drop attack)
• Clonic
• Tonic
• Generalized tonic-clonic (grand mal)
2. Partial Seizure: Part of the brain surface
• Simple partial: There is no impairment of consciousness during the seizure.
• Complex partial: There is impairment of consciousness during the seizure.
• With secondary generalization: Onset begins as simple partial and then progresses to impairment of consciousness.
▪ Status Epilepticus what is it?
Status Epilepticus is a continuing series of seizures without a period of recovery between episodes
▪ Dementia
Progressice deterioration and continuing decline of memory and other cognitive changes 60 % to 80 % of Alzheimer are dementia- Vascular dementia is the most common cause
No cure
Cause is unknown
Dementia-causing illness: - Alcoholism
- Alcoholism
- Intracranial tumor
- Normal-pressure hydrocephalus
- Parkinson disease
- Lewy body disease
- Huntington disease
- Multiple sclerosis MS
- Bocine Spongiform encephalopathy (Mad Cow) Delerium and depression in elederly different than dementia
Delirium in global mental dysfunction – Acute Confusional state Primary risk factor: age and family
Others: Head trauma, diabetes, depression, stroke, hypertension diabetes
Signs and Symptoms memory lost, anxiety and agitation, diffulty in judgement, problem solving and communication. Assistance needed for ADL . Difficulty eating and swallowing. Weight loss
▪ Parkinson disease
Disorder of mobility - 1 million americans affected. 60,000 cases each year
4 % are younger than 50 Y/O idiopatic or acquired
Common causes: Infection, intoxication, and trauma
Drug Toxicity: Phenotiazine class: (Chlorpromazine, prochlorperazine, Thioridazine) and Butyrophenone(haloperidol)
Parkinson disease results from degeneration of the pigmented dopaminergic neurons found in the subtantia nigra and to a lesser extent neurons elsewhere in the brain.
Lewy bodies are cytoplasmic inclusions are found in the surviving neurons.
▪ GERD signs and symptoms
Heartburn Chest pain Regurgitation Epigastric pain Dry cough
Hoarseness in the morning Esapheogeal strictures with Gerd
▪ Multiple Sclerosis- Structures effected by the demyelination?
Chronic demyelinating disease of the CNS – sign disability in young adults
Autoimmune disorder that results in inflammation and scarring of the myelin sheaths covering nerves.
Age onset (20-50 yr)
2 -3x more common in women vs men
In MS, the demyelination of nerves can happen anwhere in the CNS. Structures most frequently affected are the optic nerves, the oculomotor nerves, the corticospinal, cerebellar, and posterior column system.
Myelin facilitates nerve conduction. So the inflammation with MS slow or interrupt the conduction of nerve impulses.
▪ Spinal Cord Injuries- major mechanisms of injury?
A problem of the young
Male 3-4x risk – weekends/summer months
Motor vehicle crashes- highest number of sci 2) violent gun shot wounds, falls, recreational accident
The major Mechanisms of injury are hyperflexion, hyperextension and compression
Flexion injury with tearing of the posterior ligaments and dislocation is the most unstable injury and is aften associated with severe neurologic deficits
Hyperextension injury is the most common
S/S complete loss of function below the level of injury , Spinal shock (a few hrs) Flaccid paralysis of all skeletal muscles. Loss of all spinal reflexes, loss of pain, proprioception and other sensations, bowel and bladder dysfunction with paralytic ileus, loss of thermoregulation. Bradycardia, hypotension
▪ How to treat Spinal Cord Injuries
Stabilization of the spinal vertebra (to prevent further trauma to spinal cord) Sugery – internal fixation or external fixation and bracing
Surgery within 24 hrs if cord compression
Use od high-dose methylprednisolone (1st 8 hrs) (controversial method) Removing or alleviating the painful stimuli
Use od adrenergic receptor-blocking medication to manage hypertensive crisis Prevent respiratory and urinary tract infections
Skin pressure sores
Septicemia and fecal impaction
▪ Hypoventilation build up what?
Hypoventilation causes build up of acid (acidosis) and too little oxygen in the blood. Hypoventilation occurs when delivery of air to the alveoli is insufficient to meet the need to provide O2 and remove CO2.
- Decrease rate and depth of respiration
- Results in increased PaCO2 ≥45 mm Hg
- Hypoxemia – increased alveolar CO2
▪ Causes: drugs (morphines, barbiturates) , obesity (Pickwickian syndrome, myasthenia gravis, obstructive sleep apnea, chest wall damage.
▪ Normal ABG’s- Only must know normal values
pH 7.35-7.45
PaCO2 35-45 mm Hg
PaO2 80-100%
HCO3 22-26 mEq/L
SaO2 95-100%
▪ Acute Respiratory Failure- the goal of treatment
Maintaining ventilatory support by maintaining airway patency and ensuring adequate alveolar is the primary goal of therapy.
Mechanical ventilation
Management of the underlying cause.
▪ Virchow’s Triad of PE
Virchow (1800 Pathologist) 3 Factors that predisposed patient to thrombus formation an increase of PE (Pulmonary Embolism)
- Venous Stasis (sluggish blood flow
- Hypercoagulability
- Damage to the venous wall (intimal injury)
Box 21.4
Fa c t o r s P r e d i s p o s i n g t o P u l m o n a r y E m b o l i s m o f Vi r c h o w ' s Tr i a d Venous Stasis
• Extended bed rest (delayed venous removal of activated clotting factors)
• Postoperative state
• Immobility (activated clotting factors)
• Vascular disorders (thrombophlebitis of lower extremities and pelvic area)
• Congestive heart failure (venous backflow/stasis)
• Cardiac dysrhythmias (atrial fibrillation)
• Dehydration
• Prolonged air travel
• Obesity
Hypercoagulability
• Oral contraceptives (estrogen therapy), hormone replacement therapy
• Pregnancy, early puerperium
• Polycythemia (chronic high altitude; chronic pulmonary disease with decreased PaO2 and increased PaCO2)
• Malignant pathologic processes, visceral cancer
• Cigarette smoking
• Inherited resistance to activated protein C
• Deficiency of protein S
• Deficiency of antithrombin III
• Prothrombin gene mutation
• Presence of antiphospholipid antibodies (lupus), anticoagulant and anticardiolipin antibodies
Damage to Vessel Wall (Intimal Injury)
• Blunt trauma
• Penetrating wounds
• Bone fractures with soft tissue injury
• Surgical procedures (hip, pelvic, abdominal, cardiovascular)
• Obstetric manipulations during labor and delivery
• Burns
• Central venous catheter
-
▪ Embolisms the different types
▪ 7 Types of embolisms:
▪ -Thrombotic
▪ -Fat
▪ -Amniotic Fluid
▪ -Air
▪ -Tumor
▪ Foreign material
▪ Septic
▪ Parasite
▪
▪ Asthma- definition
Asthma is complex lung disease and associated with the release of inflammatory chemicals from mast cells in the airways.
Asthma is a lung disease characterized by:
- airway obstruction that is reversible (to some patients)
- airway inflammation
- increased airway reactivity to a variety of stimuli
Mast cell release are IgE (immunoglobin E) mediated for both extrinsic and intrinsic asthma.
Extrinsic Asthma: Allergies, family hx of the disease. Positive reaction to environmental triggers.
Intrinsic Asthma: Respiratory Tract infections and psychological factors(harder to treat)
▪ Exercise-Induced Asthma is due to?
Exercise-induced asthma is due to Running, jogging, bicycling.
Bronchospasm occurs within 3 min after exercise and usually resolve in 60 minute.
▪ Acute and Chronic Bronchitis
Acute Bronchitis is an acute inflammation of the trachea and bronchi . 80% of the 12 mil cases per yr in UD.
o Influenza Virus A or B
o Parainfluenza Virus
o respiratory syncytial virus
o Coronavirus
o Rhinovirus
o Coxsackie virus
o Adenovirus
o Streptococcus pneumoniae
o Hemophilus influenza
o Mycoplasma
o Moraxella
o Chlamydia pneumoniae
(heat, smoke inhalation, inhalation of irritant chemicals)
Risk factors: smokers, young children, elderly -winter months)
Pathogenesis: The airways become inflamed and narrowed from capillary dilation, swelling from exudation of fluid, infiltration with inflammatory cells.
S/S mild and self-limiting: - low-grade fever
- substernal chest discomfort
- sore throat
- postnasal drip
- fatigue
Associated inflammation of the larynx and trachea produces croup syndrome
Diagnosis: Clinical presentation- onset of the cough.
Treatment: Antibiotic therapy for bacterial infection
Viral infection resolved spontaneously in most normal healthy person Primary goal is symptom management with antitussive agents – beta-2 agonists and bronchodilatoes
Codeine-containing medication are helpful
Non-pharmacologic: increase fluid intake, avoid smoke, use vaporizer in bedroom
Chronic Bronchitis:
Major causes of chronic bronchitis are:
- Cigarette smoking (90 %)
- Repeated airway infections
- Genetic predisposition
- Inhalation of physical or chemical irritants
Chronic Bronchitis: Type B COPD
Diagnosed: Symptomatically by hypersecretion of bronchial mucus and a chronic or recurrent productive cough of more than 3 months duration and occurring each year for 2 or more successice yes in patient.
Airway obstruction is persistent and irreversible in patients with chronic brochitis and emphysema.
3:1 ratio of annual cases of chronic bronchitis to emphysema.
Pathogenesis: Chronic inflammation and swelling of the bronchial mucosa resulting in scarring, increased fibrosis of the mucous membrane, hyperplasia of bronchial mucous glands and globet cells, hypertrophy of bronchial wall thickness which cause (potentiates) obstruction to airways.
Neutrophil activity cause inflammation.
Interleukin-8 levels are elevated. CD8 T-lymphocyte levels are elevated.
Two bacteria is involved with chronic bronchitis: H. influenza and S.Pneumoniae
The chronic bronchitis patient appear as the blue bloater: Oxygen desaturation (cyanosis) and edmea associated with right-sided heart failure.
S/S of Chronic Bronchitis:
- Overweight (1:2 male to female ratio)
- 30s and 40s
- SOB (shortness of breath) on exertion
- Excessive amounts of sputum (mixture of saliva and mucus) most severe in the am
- Chronic cough
- Excess of body fluids( edema, pypervolemia)
- Hx of smoking
- Complaints of chills
- Malaise
- Muscle aches
- Fatigue
- Loss of libido
- Insomnia
End-stage of Chronic Bronchitis, Patient has
- Right-side heart failure
- Distended neck veins
- Right ventricular heave
- Right ventricular gallop
- Peripheral edema
- Hypoxia- pulmonary hypertension
- Cyanosis
Diagnosis: Chest radiography, pulmonary functions tests, Elevated PaCO2 and decreased PaO2 (below 65 mmhg)
Severe Chronic Bronchitis: Physical Exam: Scattered crackles, rhonchi, wheezes, jugular vein distension, clubbing, pedal and ankle edema
Treatment: Because Bronchitis and Emphysema has similar therapy 1- Block the progression of the disease
2- Return the patient to optimal respiratory function 3- Return the patient to usual activities of daily living
Inhaled B-2 agonists
Inhaled anticholinergic brichodilatoes Cough suppressants
Antimicrobial agents for infection
Inhaled or oral cortisosteroids for acute exacerbations
Low-dose of Oxygen therapy for patient with Pao2 less than 55 mmhg Mechanical ventilation
Home oxygen therapy Smoking cessation
Emphysema 1
Type A COPD – destructive changes of the alveolar walls and abnormal enlargement of the distal air sacs.
Causes: smoking, air pollution, occupations (Welding, mining, working with asbestos),
∞-1 antitrypsin deficiency (1%). Develop over a long period Person over 50
Cigarette smoking in excess of 70 pack -years
Pathogenesis: Pathologic changes leading to alveolar destruction are associated with the released of proteolytic enxymes from inflammatory cells such as neutrophils and macrophages.
How does smoking causes alveolar damages? 2 ways:
- Leads to inflammation in the lung tissue (parenchyma)
- It inactivates ∞-1 antitrypsin which would usually protect the lunc parenchyma.
S/S of patients with emphysema
- Exertional dyspnea
- Thin person over 55 years
- Increased SOB for past 3+4 yrs
- Increase with women who smoke
- Use of accessory muscles to breathe
- Progressive dyspnea
- Pursed-lip breathing
- Minimal Cough
- Barrel chest -Overinflation – increase lung volume
- Digital clubbing
-
At RISK: Pneumothorax, chest pain on the affected side, dyspnea Late: Major symptom is dyspnea on exertion. Pink puffers
Treatment the same as chronic Bronchitis Cessation of smokins
▪ Chronic Obstructive Pulmonary Disease
▪ Acute Respiratory Distress Syndrome (ARDS)
ARDS is characterized by damage to the alveolar-capillary membrane Mortality rates ranges from 30% To 50 %
Decline in the PaO2 (does not respond to O2 therapy)
The common denominator appears to be increased permeability of the pulmonary vasculature
Flooding of the alveoli with proteinaceous fluid
S/S - increase in pulse rate
- Dyspnea
- Low PaO2
- Shallow, rapid breathing Progression - - - Tachycardia
- Tachypnea
- Hypotension
- Marked restlessness
- Decreased mental status
- Production of frothy secretions
- Phys Assessment: crackles and rhonchi
- Using accessory muscles to breath
Late - Cyanosis
Diagnosis- Hallmark is hypoxemia
- Hypotension
- Decreased UO (urine output)
- Respiratory and metabolic acidosis
- Cardiopulmonary arrest
- Arterial blood gas hypercapnia
- Chest radiography
- Pulmonary function test Treatment: Addressing the underlying cause (sepsis)
Maintaining fluid and electrolyte balance Volume ventilator
PEEP (positive end-expiratory pressure)
▪ Tension Pneumothorax- treatment
Tension pneumothorax is medical emergency
Results from the buildup of air under pressure in the pleural space Severe tachycardia
Hypotension
Tracheal shift to the contralateral disease Neck vein distension
Hyperresonance Subcutaneous emphysema
Treatment;
15-25 % : treated symptomatically, monitor closely, resolution within several weeks.
Over 15 – 25% Chest tube placed with water seal and suction 100 % oxygen
Chemical pleurodesis Thoracotomy
▪ Pneumonia
Pneumonia (breath)
An inflammatory reaction in the alveoli and interstitium of the lung usually caused by an infectious agent
Pneumonia can result from 3 sources
- Aspiration of oropharyngeal secretions of bacterial flora and or gastric contents (20-35 % of all pneumonia)
- Inhalation of contaminants (virus, mycoplasma)
- Contamination from the systemic circulation Classifications of Pneumonia : Community acquired/hospital acquired 15-20 % with pneumonia requires hospitalization
Pneumonia classified: bacterial
Atypical Viral
Pneumonia : Gram positive
Gram negative
Gram positive: Staphylococcus and streptococcus Gram negative: E coli, Hearmophilus influenza, kleb,
Risk: Elderly , diminisged gag reflex, seriously ill., hospiralized, hypoxix immunocompromised
▪ TB- transmission
Transmission: It is a airbone disease
- inhalation of small droplets containing bacteria
TB baccillus
- Droplets expelled with cough, sneeze, or talking
-
▪ Bacteria Mycobacterium tuberculosis – acid fast aerobic bacillus
▪ Most common sites are the lungs and the lymph nodes
▪
▪ Sources of Electrolyte Stores
Every fluid compartment contains electrolytes- Electrolytes compositions differs in each compartments.
The concentration of K, Mg, Ca is higher inside cells than fluids outsise of cells.
Total calcim ions content concentration is higher inside cells, intracellular calcium is bound to other molecules.
The concentration of active ionized Ca ions is higher in the extracellular fluids.
The cells and bones are called electrolyte pools as they serve as important reservoir of Ca, K, Mg.
Distribution of electrolytes between the extracellular fluid / the electrolyte polls is influenced by hormones (epinephrine – K ions) (Isulin – K and Ph ions) and PTH (calcium ions)
PG 531 Electrolyte Distribution
▪ Anemia
Anemia is a deficit of red cell
➢ _- Low oxygen-carrying capacity leads to hypoxia.
● Opposite of anemia: polycythemia
➢ Excess of red cells
➢ Increases blood viscosity and volume
● Relative anemia—normal total red cell mass with disturbances in regulation of plasma volume
● Absolute anemia—actual decrease in numbers of red cells
➢ Decreased production
➢ Increased destruction
▪ Hormone that Kidney’s secrete
▪ • The kidney secretes two important endocrine hormones: erythropoietin, a growth factor for red blood cells (RBCs), and active vitamin D, a necessary cofactor for calcium absorption from the intestine.
▪ • In chronic kidney disease, impaired production of these hormones results in anemia and osteodystrophy.
▪ Definition of Polycythemia
Red cells are present in excess increasing blood viscosity which turns cause hypertension. 3 Types of polycythemia: - Polycythemia vera- neoplastic transform bones marrow
- Secondary Polycythemia – chrnic hypoxemia (over production of erythropoietin)
- Relative polycythemia
▪ Thrombocytopenia is caused by
- Decreased platelet production
o Folate/b12 deficiency
o Radiation therapy
o Chemotherapy
o Drugs (ETOH, Thiazides, phenytoin)
o Aplastic anemia
o Cancer in bone narrow
- Decreased platelet survival
o Drugs (Thiazides, digoxin, heparin, furosemide, certain antibiotics
o Mechanical prosthetic heart valves
o Viral and bacterial infections
o Circulating immune complexes
o Increased destruction in the spleen
o Disseminated intravascular coagulation
- Splenic Sequestration (pooling)
o Splenomegaly
o Hypothermia
- Platelet dilution
o Massive transfusion with blood stored more than 24 hrs
Thronmocytopenia is caused by Generalized bleeding
▪ Disseminated Intravascular Coagulation (DIC)- What is it? And How to treat it? Disseminated intravascular coagulation (DIC) is a acquired hemorrhagic syndrome in which both clotting and bleeding occur simultaneously.
Treatment: removal or correction of the underlying cause and support of major organ.
- Replacement of depleted clotting factors with fresh frozen plasma
- Packed red blood cells, platelets
- Cryoprecipitate
- Antifibrinolytics (aminocaproic acid) may be used if life-theating hemorrhage
- Heparin therapy to stop thrombin formation
-
▪ Chronic Myeloid Leukemia (CML) - diagnosis is by identifying which chromosome abnormality?
Chronic Myeloid Leukemia represents 15 % of all cases od leukemia in US Onset 40-50 y
Malignat granulocyrs that carry a unique chromosomal abnormality (The Philadelphia chromosome Ph-)
The Philadelphia chromosome is fomed because of the balanced translocation between chromosome 9 and 22.
The overall survival is poor.. 2 years
S/S fatigue, weight loss, diaphoresis, bleeding, abdomral discomfort from enlarged spleen.
▪ Chronic Myeloid Leukemia (CML)- Treatment prognosis CML does not respond well to chemotherapy
Temporary remission Poor survival
2 years survival time if untreated
Anti bcr/abl therapy m(imatinib) to reduce the number of leukemic cells ‘ Patient might develop resistance to drugs
- ONLY CURATIVE TREATMENT is allogenic bone marrow transplantation with a suitable donor
- 25 % mortality with transplant (related donor)with 50 %-60 % disease- free survival
- 50 % mortality with transplant-unrelated
- Once CML which the blast phase – survival is 3-4 months
▪ GERD
See other study guide
▪ Initial symptoms of Malignancies
▪ Hodgkin Disease
30% of malignant lymphoma Onset 20-40 yrs.. across life span Males and worst prognosis
Overall 5 yrs survival rate for all stage treated : 85 % It is a malignant disorder of the lymph nodes
Characterized by Reed-stemberg cells, Eipstein-barr virus
Malignant but grow/spread in predictable way; sets HD apart from other lymphomas Usually metastasizes along contiguous lymphatic pathways
Usually present in single node or localized node chaint. There are 2 typed
- Rare lymphocyte Type (5%)
- Classical type cHD (95%) S/S Early signs are often asymptomatic
Painless lymphadenopathy Fever
Night sweats Pruritus
Weight loss Malaise
-Cerical nodes
-lymp nodes enlargements above diaphragm Iguinal nodes
-Disease spread from site of origin to other lymph nodes (spleen and bone narrow)
Prognosis and treatment
Ann Arbor staging also used for NHL
Stages of HD
A: Absence of clinical symptoms
B: Symptoms present at time of staging
(Loss of 10 % or more body weight, Unexplained fever, night sweats)
CS: Hx. PA, noninvasive procedures (computed tomography (CT scan)
PS: Invasive procedure such as laparotomy and tissue biopsy (Non-Hodgkin) B-call, T-call and NK-Cell lymphoma
▪ Hypertension- Modifiable and Non-Modifiable Factors
Most common primary diagnosis in the US>
Heart disease, kidney disease, peripheral vascular disease and stroke. Responsible for 7.6 mil (worlwide)
Prehypertension – range between normal blood pressure (120/80) to stage 1 hyper
- Stage that we initiate efforts to prevent or deter progression of disease Primary hypertension- essential hypertension – Silent killer - Sys BP
≥140 mmhg Dias BP ∈90 mmHg
Most common form of hypertension Rare prior to age 10-
Major risk for cardiovascular disease
Complication: End-organ damage, renal failure, stroke, heart disease, increase myocardial work in HF,
Treatment: Lifestyle modifications, wgt loss, exercise, DASH diet, alcohol moderation. Decrease sodium intake. Drug therapy for heart rare, SVR and stroke
Modifiable: - dietary factors, sedentary lifestyle, obesity/weight gain, metabolic syndrome.
Elevated blood glucose levels/Diabetes, elevated cholesterol, alcohol and smoking
Non-modifiable: Family hx, age, ethinicity/genetics
(maternal smoking, pregnancy induced hypertension, low birth rate)
▪ Hypertension- Organs effected
o Renal (Parenchymal and vascular)
o Cardiovascular
o Tumor
o Endocrine (Hyperthyroidism, cushing disease, congenital adrenal hyperplasia, primary hyperaldosteronism)
o Neurologic (Guillain-Barre Syndrome, Increased intracranial pressure)
o Other (Systemic arteritis. Sleep apnea)
▪ Hypertension is the most common primary diagnosis in U.S
▪ 32 % of 80 mil adults in U.S has High Blood Pressure
▪ Higher in Non-hispanic black adults (44.9 %)
▪ Hypertension is the most common Risk factor for cardiovascular worldwide
▪ Normal Range fore blood pressure is 120 mmHg systolic – 80 mmHg diastolic – 18 and older
▪ Prehypertension : range between normal BP to Stage 1 Hypertension
▪ Stage 1 Hypertension : Sys 140 mmHg or dias 90 mmHg
▪ Primary Hypertension (essential hypertension)
▪ No clear cause so idiopathic disorder
▪ Different than secondary hypertension where blood pressure elevation is cause
▪ Primary hypertension most common 90-95 %
▪ Systolic blood pressure is the major risk for subsequent cardiovascular disease
▪ Hypertension- Management
- Lifestyles modifications
- Drug therapy (heart rate, stroke, Systemic vascular resistance)
▪ Coronary Artery Disease
CHD (Ischemic Heart disease) CA. Insufficient delivery of oxygenated blood to the myocardium (Ischmea) because of the atherosclerotic coronary arteries.
CHD cause 1 in 6 death in UD.
_ (dysrhythmias, sudden cardiac arrest, heart failure)
Ethiology: Atherosclerosis of coronary arteries is the source od nearly all SHD
Risk factors: Family Hx, Abd lipid levels, smoking, hypertension, diabetes, obesity)
▪ Definition of Atherosclerotic Plaques
They are plaques that are from injury to the coronary artery endothelium and they are filled with large lipid core, fragiles and prone to ruptures.
▪ Myocardial Ischemia- What is it
It is when blood flow to the heart muscle (myocardium) is obstructed by a partial or complete blockage of a coronary artery by a buildup of plaques (artherosclerosis) If plaques ruptured, you can have a heart attack (myocardial infarction)
▪ Acute Coronary Syndrome
Risk : Smoking, Fam Hx, Obesity, Lifestyle sedentaty, diabetes, poor diets, lipids Up
S/S ; MI Chest pain (more severe than typical angina) (patient might say elephant sitting on chest)
Chest pain that may radiate to the arm shoulder , jaw and back N/V
Diaphoresis (sweating) SOB (dyspnea)
Etiology: Plaqu rupture with thrombus development Unstable Angina – Occlusion is partial
With MI- Occlusion is complete
Treatment: Decrease myocardial oxygen demand – increase myocardial oxygen
supply
Monitor and manage complications
Diagnosis : EKG and Biomakers
▪ Definition of Unstable Angina Pectoris
▪ Chest pain associated with intermittent myocardial ischmia (Burning, crushing, squeezing, choking, or referred pain)
- Result from inefficient cardiac pumpin (resultant pulmonary congestion and SOB)
▪ Condition in which your heart doens;t get enough blood flow and oxygen. May lead to an heart attack. Angina is a type of chest discomfoer caused by a poor blood flow through the blood
vessels (coronary of the heart muscle (Myocardium)
▪
▪
▪
▪
▪
▪
▪ What is reperfusion therapy
▪ Left sided heart failure
▪ Right sided heart failure
▪ Medication management for Systolic Heart Failure
▪ Effects of Right Sided Heart Failure
▪ MI- Signs and symptoms
▪ Shock
• Shock represents a diverse group of life-threatening circulatory conditions. The common factor among all types of shock is hypoperfusion and impaired cellular oxygen utilization. Inadequate cellular oxygenation may result from decreased cardiac output, maldistribution of blood flow, or reduced blood oxygen content.
• • During the compensatory stage of shock, homeostatic mechanisms are sufficient to maintain adequate
tissue perfusion despite a reduction in cardiac output. Manifestations of sympathetic nervous system (SNS) activation are an elevated heart rate, increased myocardial stimulation, bronchodilation, vasoconstriction, cool clammy skin, dilated pupils, and decreased urine output. Blood pressure is maintained even though cardiac output has fallen.
• • During the progressive stage of shock, compensatory mechanisms begin to fail, and hypotension and progressive tissue hypoxia result. Shift of cells to anaerobic metabolism results in lactate production
and metabolic acidosis. A lack of cellular adenosine triphosphate (ATP) production leads to cellular swelling, dysfunction, and death. Generation of oxygen free radicals, release of inflammatory cytokines, and activation of the clotting cascade lead to further cellular and organ dysfunction.
▪ Cardiogenic Shock
▪ Cardiogenic shock is usually a result of severe ventricular dysfunction associated with myocardial infarction. Other causes include cardiomyopathy, ventricular rupture, and congenital heart defects.
▪ • Diagnostic features of cardiogenic shock include decreased cardiac output as a result of left ventricular dysfunction, along with elevated left ventricular end-diastolic pressure, S3 heart sounds, and pulmonary edema. Sympathetic activation leads to an increased heart rate, vasoconstriction, and a narrow pulse pressure.
▪ • Low cardiac output leads to reduced oxygen delivery to tissues. Tissues extract a greater percentage of oxygen from the delivered blood, which leads to reduced Svo2.
▪ • Therapy is aimed at improving cardiac output and myocardial oxygen delivery while reducing cardiac
workload. Pharmacologic treatment often includes the use of inotropic agents, afterload-reducing agents (e.g., vasodilators), and preload-reducing agents such as nitrates and diuretics. Intraaortic balloon counterpulsation may be used to reduce afterload and improve coronary artery perfusion. Ventricular assist devices (VADs) may be used for longer-term circulatory support, whereas heart transplantation provides definitive treatment.
▪
▪ Obstructive Shock
▪ Obstructive shock results from mechanical obstructions that prevent effective cardiac filling and stroke volume.
▪ • Pulmonary embolism, cardiac tamponade, and tension pneumothorax are common causes of obstructive shock.
▪ • Prompt management of the underlying obstruction is necessary to prevent cardiovascular collapse.
▪ Hypovolemic Shock
• Hypovolemic shock results from inadequate circulating blood volume precipitated by hemorrhage, burns, dehydration, or leakage of fluid into interstitial spaces.
• • The classic features of hypovolemic shock are the result of low cardiac output and low intracardiac pressures. Manifestations are due primarily to sympathetic nervous system (SNS) activation: elevated heart rate, vasoconstriction, and increased myocardial contractility.
• • The severity of symptoms of hemorrhagic shock correlates with the amount of blood loss; however,
there is significant variation in the clinical presentation of hypovolemic and hemorrhagic shock, and careful assessment is required to diagnose it in the early stages.
• • Therapy for hypovolemic shock is aimed at fluid replacement and control of the source of volume loss. Colloids, isotonic crystalloids, and blood products may be used as replacement fluids.
▪ Anaphylactic Shock
Anaphylactic shock is a result of excessive mast cell degranulation in response to antigen. Mast cell degranulation usually is mediated by IgE antibodies. Release of vasodilatory mediators, such as histamine, into the circulation by mast cells results in severe hypotension. Urticaria, bronchoconstriction, stridor, wheezing, and itching are usually present. Treatment includes maintenance of airway patency and the use of epinephrine, antihistamines, vasopressors, and fluids to restore blood pressure.
▪ Septic Shock
▪ Septic shock results from a severe systemic inflammatory response to infection. Gram-negative bacteria, gram-positive bacteria, and fungal infections are common causes of septic shock. In gram-negative shock,
endotoxins in bacterial cell walls stimulate massive immune system activation. Septic shock from any organism is characterized by release of large numbers of immune mediators (e.g., cytokines) resulting in widespread inflammation. The clotting cascade, complement system, and kinin system are activated as part of the immune response.
▪ • Widespread inflammation leads to profound peripheral vasodilation with hypotension, maldistribution of blood flow with cellular hypoxia, and increased capillary permeability with edema formation.
▪ • Initially, septic shock is characterized by abnormally high cardiac output resulting from immune- mediated vasodilation and sympathetic activation of the heart. The patient is usually febrile, pink, and warm. Even though cardiac output is high, cellular hypoxia is present because of maldistribution of blood flow. Reduced cellular oxygen utilization is manifested as a high Svo2.
▪
▪ Goal of treating sepsis is
Treatment for sepsis is aimed to improve the distribution of blood flow and managing infection with antibiotics. Administration of fluid and drugs to increase cardiac and vascular perfomance to improve blood flow
▪ Cancer and its ability to metastasize unpredictable- does not follow cellular functions rules
Malignant cells produced specialized enzymes and receptors to enable them to escape their tissue of origin and metastize. The spread generally occurs by way of bloodstream or lyphatics.
Tumor cells lodge in the capillary beds of the organs that drain them Some cancer are prone to metastize: Breast, lung, bone, colon.
▪ CVA
▪ Osteoporosis
The most common metabolic bone disease (10 mil 50+ in Us)
Happens when rate of bone resorption is greater thatn rate of bone formation and oastoblastic and osteoclastic balance is disrupted
Bone mineral density is greater or equal to 2.5 standard
Risk factor: age, corticosteroid use, Hx of Rheumatoid arthritis, Fam Hx, estrogen level. Family Hx is a major risk factor
After menopause. The rapid of normal bone loss develop rapidly so estrogen deficiency increase the risk of osteoporosis
Other risk: Small frame, Caucasian or Asian, high dose of thyroid, diet low on calcium and vitamin D, physical inactivity. Smoking or increase alcohol intake/ Patient with chronic renal function who have abnormal parathyroid function. Cushing syndrome,. Hyperthyroidisms.
Anorexia nervosa. COPD, Type 1 diabetes. Celiac disease, lupus. Cancer Rheumatoid Arthritis.
S/S: often asymptomatic until bone fracture
Shortened stature
muscle wasting or spasms of back muscles/difficulty bending Stooped posture
Bone that breaks more easily than expected
C/O of impaired breathing
Complication: Fall risk (spine or hip fractures), disability and increased risk of death
Treatment:
Good nutrition (Protein)
Moderate to regular exercise (walking, riding stationary bicycle) Calcium (1000-1500 mg daily)
Vitamin D to maintain bone mass (30 mg/mL dihydroxyvitamin D) Biphosphonates
▪ Passive Immunity
▪ Passive immunity involves the transfer of plasma containing preformed antibodies agains a specific antigen from a protected or immunized person to an unprotected or nonummunized person.
▪ Provide immediate but temporary protection
Needs: 1) when B-cell immunodefiency 2) highly susceptive person are exposed to disease without active immunization 3) antibody injection
- Mom to fetus (IgG crass the placental barrier)
- Newborn receive IgA through Breast milk
- Serotherapy ) Immunization of anibodies to unprotected person
▪ Immunoglobulin involved allergic hypersensitivity reactions
In the majority of cases the antibody typically responsible is IgE isotype (IgE
-Asthma)
▪ Clinical indicator of Acute Blood Loss- Orthostatic hypotension
Acute Blood Loss Anemia – present after trauma or secondary to disease. It rapidly decrease the overall blood volume and impairs O2 delivery
Hemoocrit level is less than 40 % in men and 37 % in women .. Hemoglobin conc is less than 14 in men and 12 in womwn ..
Tachycardia is seen with exercise Slight drop in BP
(10 % Loss -500 ml) no clinical signs expect vasovagal syncop
(30 % Loss-1500 ml) Flat neck vein with supine postural hypotension
(40% loss-2000 ml) Central venous pressure. Cardiac output, arterial PB below normal
Patient is supine / at rest/ air hunger/ tachycardia/ cold/ clammy skin
(50 % loss -2500 ml) SCHOCK AND DEATH
Treatment_ Blood Volume replacement therapy with crystalloid solutions _ good prognosis if underlying cause is managed
▪ Asthma
[Show More]