*NURSING > STUDY GUIDE > Rasmussen College:NUR 2502 MDC 3 Final Exam Study Guide _LATEST 2021/2022,100% CORRECT (All)
Rasmussen College:NUR 2502 MDC 3 Final Exam Study Guide _LATEST 2021/2022,100% CORRECT
Document Content and Description Below
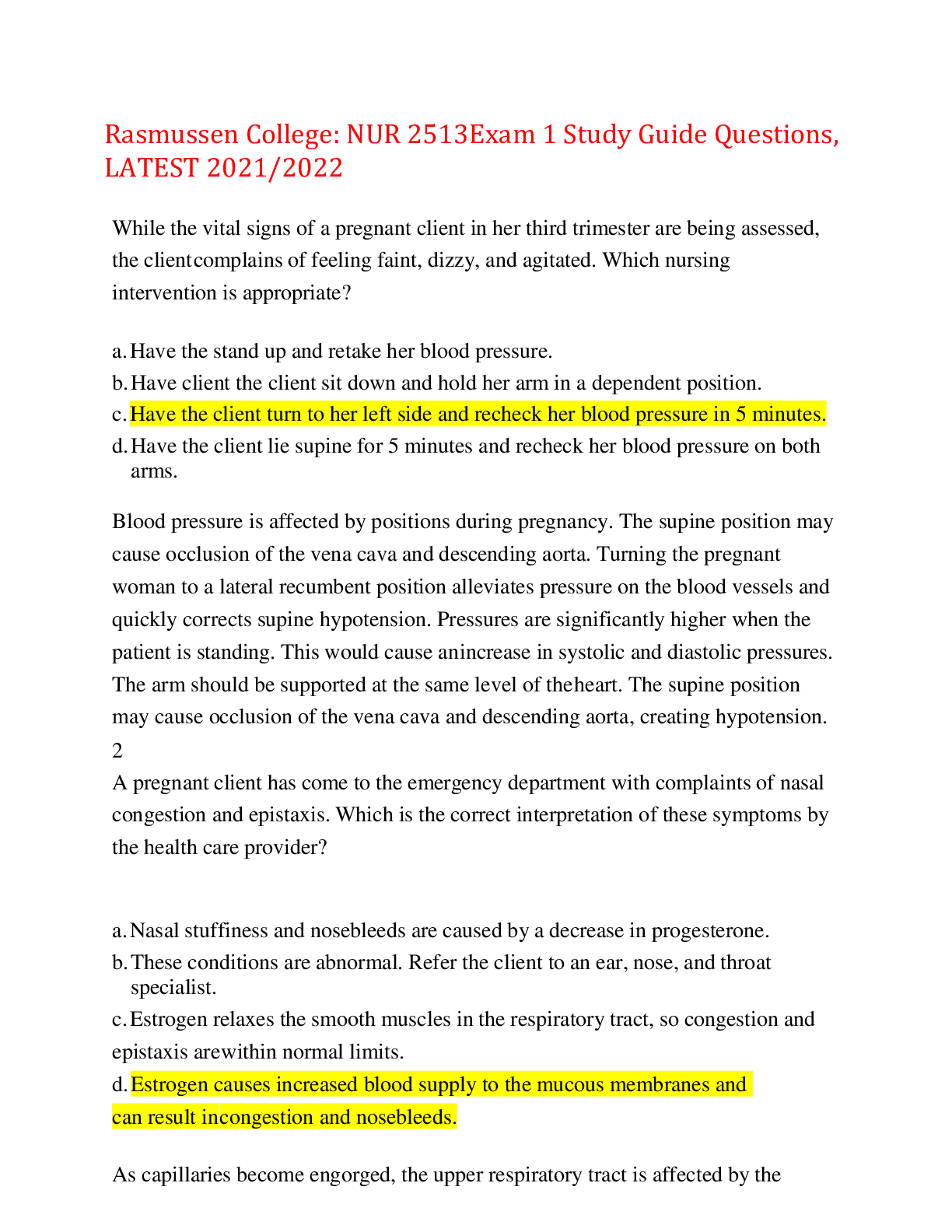
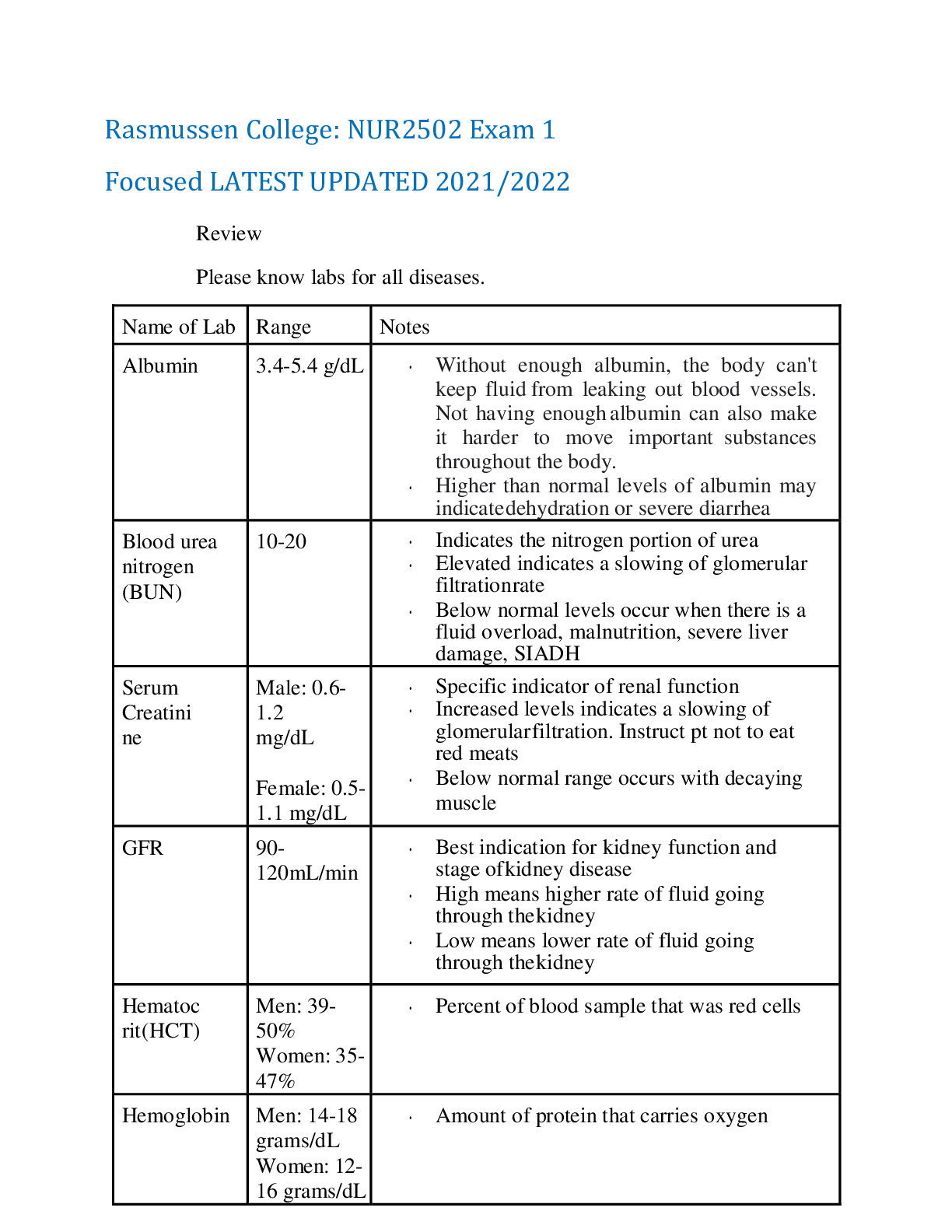
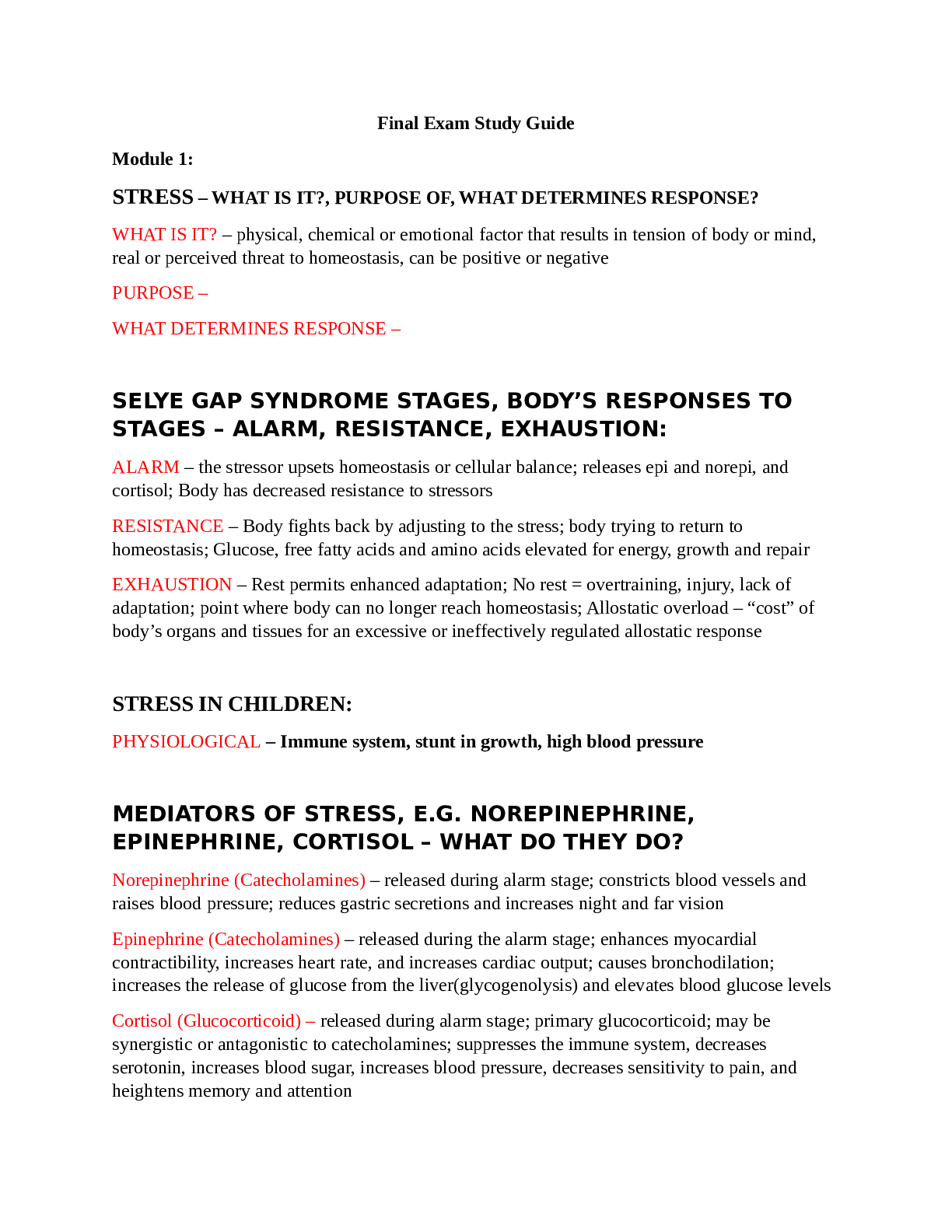
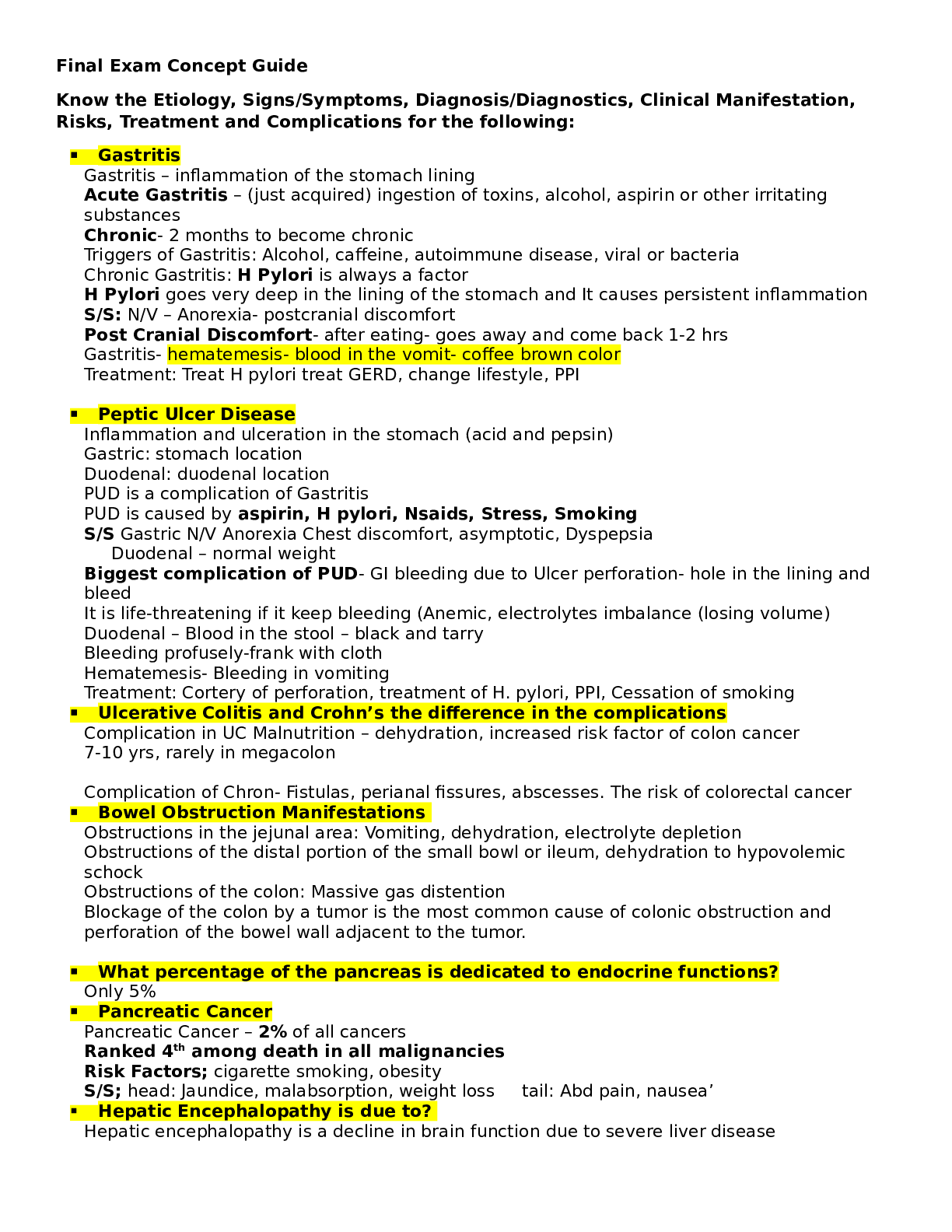
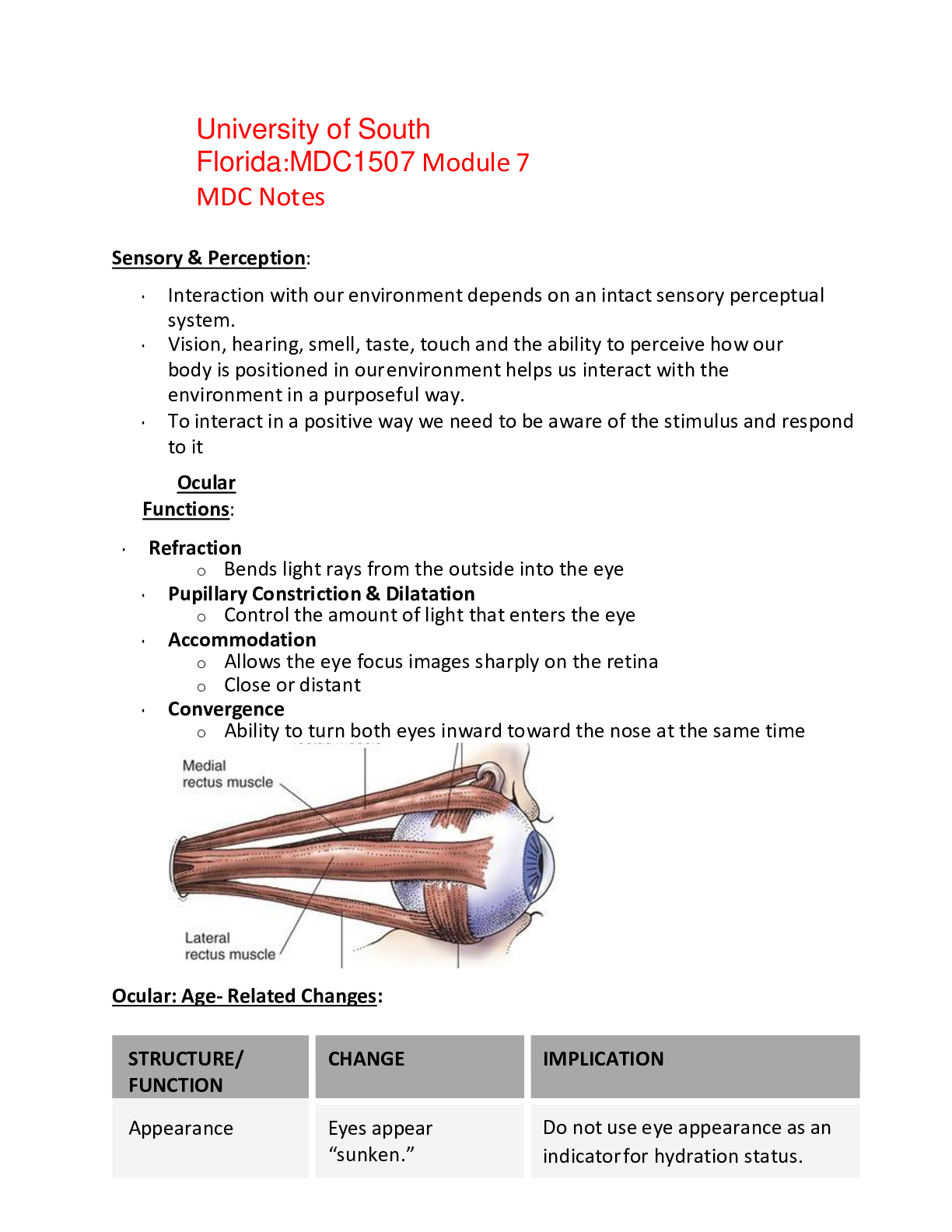
Rasmussen College:NUR 2502 MDC 3 Final Exam Study Guide _LATEST 2021/2022 Cardiac Disorders Heart failure – 3 types • Left-sided heart failure – results from ineffective left ventricular c... ontraction causing a backup of fluid into the lungs, which results in pulmonary congestion. o Symptoms ▪ Chest discomfort ▪ Dyspnea ▪ Palpitations ▪ Skipped heartbeats ▪ Tachycardia ▪ Weakness ▪ Dizziness ▪ Fatigue ▪ Oliguria (Kidney failure) • Right-sided heart failure – results from the inability of the right ventricle to effectively contract to pump blood, causing a backup of fluid into the periphery. o Symptoms ▪ Nausea ▪ Anorexia ▪ Leg edema ▪ Ascites ▪ Nocturia ▪ Hepatomegaly • High-output failure – results from an increased metabolic state in which cardiac output remains normal or above normal. High-output failure is caused by increased metabolic needs or hyperkinetic conditions, such as septicemia, high fever, anemia, and hyperthyroidism. • Patient Education o Take medication as prescribed. Avoid NSAIDS o Stay active as tolerated o Weigh daily o Limit sodium to 2-3g per day. Limit fluid to 2 L per day • Diagnostics o ABG o Chest x-ray o EKG o Echocardiogram – best tool in diagnosing HF. Mitral stenosis Is the stiffening/narrowing of the valves preventing normal blood flow from the left atrium into the left ventricle. This can lead to left atrial dilation and pulmonary congestion. • Causes o Rheumatic fever o Congenital abnormalities • Symptoms o Dyspnea o Orthopnea (SOB lying down) o Nocturnal dyspnea o Hemoptysis o Dry cough o Pulmonary HTN o Hepatomegaly Mitral Regurgitation The mitral valve does not close completely causing a backflow of blood into the Left Atrium. • Can lead to hypertrophy of the left atrium and ventricle due to increased pressure. • Causes o Rheumatic fever o Infective Endocarditis o Papillary muscle dysfunction Mitral Prolapse The enlargement of the mitral valve leaflets which then prolapse into the left atrium. • Causes o Marfan syndrome o Congenital heart disease o Genetics • What sound would you anticipate auscultating? – A midsystolic click heard at the apex of the heart. Aortic stenosis Narrowing of the aortic valve, obstructing ventricular outflow Can lead to ventricular hypertrophy resulting in effective perfusion of oxygenated blood If left untreated, can progress to right-sided heart failure. • What sound would you expect to hear if auscultating? - A diamond-shaped, systolic crescendo-decrescendo murmur Aortic regurgitation The valve does not close appropriately allowing blood to backflow into the ventricles. • Assessment Findings o Palpitations o Dyspnea o Orthopnea o Paroxysmal nocturnal dyspnea o Fatigue o Angina o Sinus tachycardia o Blowing, decrescendo diastolic murmur • Treatment o Rest o ACE inhibitors (-pril) o O2 o Beta blockers (-lol) o Digoxin o Diuretics o Calcium channel blockers (-dipine) • Multidimensional Care o Monitor patient signs and symptoms of heart failure (edema, tachypnea, tachycardia, fatigue, cough, dyspnea) o Implementation of transvenous pacing to maintain heart rate o Administer anti-coagulants as prescribed to prevent thrombus formation o Manage post-operative pain o Monitor post-operative bleeding o Daily weight o Fluid & Sodium Restriction • What sounds might you auscultate? – “bounding” apical pulse. Infective endocarditis • Causes o IV drug use o Valve replacement o Streptococcus viridans o Staphylococcus aureus • Treatment o Antibiotics o Surgery to remove/repair infected valve and shunts o Maintain proper oral hygiene – soft toothbrush twice a day • Symptoms o Fever w/ chills, night sweats, malaise, fatigue o Anorexia & weight loss o Cardiac murmur o Development of HF o Systemic embolism o Petechiae o Osler’s nodes on palms of hands and sole of feet o Janeway’s lesions – flat, reddened maculae on hands o Positive blood cultures Pericarditis This is an inflammation of the Pericardium-the sac around the heart. • Causes o Tissue damage from surgery o Trauma, o Cancer and cancer treatments o TB Rheumatic carditis Develops after an infection with Group A beta-hemolytic streptococci or Rhematic Fever. Involves layers of the heart and impacts contractility and cardiac output. Cardiomyopathy • Diagnosis o Chest x ray o Echocardiogram – evaluate valvular damage o Cardiac catheterization • Assessment Findings o Assess and monitor patient heart rate and rhythm for transplant patients o Administer immunosuppressant post-transplant to prevent organ rejection o Monitor for signs of organ rejection to include: o Shortness of breath o Fatigue o Fluid gain o New bradycardia o Atrial dysrhythmias o Monitor for signs and symptoms of infection such as fever, chills, and redness or drainage at the operative site • Treatment o Medications ▪ Beta blockers (metoprolol, carvedilol) ▪ Antidysrhythmic drugs ▪ Calcium channel blocker (verapamil) ▪ Diuretics ▪ Digoxin (Lanoxin) ▪ Ivabradine (Corlanor) ▪ Anticoagulants o Implantable cardiac defibrillator o Myomectomy o Heart transplant o Percutaneous alcohol septal ablation • Multidimensional Care o Implementation of medication regimen (both restrictive and obstructive) o Prepare the patient for an implantable cardioverter-defibrillator (obstructive) to prevent sudden cardiac death o Prepare the patient for surgical intervention o Preoperative teaching o Post-operative monitoring to include: o Monitor for bleeding o Assess patient for signs and symptoms of cardiac tamponade Hypertension • Causes o Modifiable risk factors: Obesity, diet, lifestyle, substance abuse, o Non-modifiable risk factors: Genetics, Age, Ethnicity o Illnesses: Kidney disease, Diabetes, Metabolic disorders • Nursing Interventions o Monitoring of blood pressure o Administration of prescribed medications to maintain blood pressure, teach compliance after discharge • Patient education o Diet modification – sodium restriction o Weight loss o Limit alcohol use o Regular exercise o Utilization of relaxation techniques o Monitor BP Arteriosclerosis and atherosclerosis • Nursing care o Perform a neurovascular assessment to identify deficits o Consult a dietician for diet modification o Implement scheduled activities daily • Patient Education o Importance of physical activity 3 – 4 times per week o Importance of diet modification to reduce LDL-C Peripheral artery disease Disorder that of the vascular system in which the extremities do not receive adequate blood supply resulting in leg pain while walking. The cause of the disorder is due to the buildup of fatty deposits in the arteries or atherosclerosis. PAD is classified as inflow or outflow. Inflow obstructions involve the distal end of the aorta and the internal and external iliac arteries. Outflow obstructions involve the femoral, popliteal, and tibial arteries and are below the superficial femoral artery. Outflow obstructions can cause significant tissue damage. A complication of PAD is ulcer formation. An acute peripheral arterial occlusion is a sudden interruption of blood to the extremity. Occlusions may affect the upper and lower extremities. Embolic occlusions are common in patients who have recently suffered from an acute myocardial infarction and/or have a dysrhythmia called atrial fibrillation. • Causes o Increased age o Obesity o Smoking o Diabetes o Hypertension o Embolus • Symptoms o Pale/Bluish in color o Weak or absent pulses in the legs and feet o Skinny & dry skin o No hair on legs o Sores and wounds can develop • Nursing Interventions o Perform a neurovascular assessment to identify deficits o Consult a dietician for diet modification o Implement an exercise plan to build up collateral circulation o Maintain a warm environment to reduce the risk of vasodilatation o Prepare the patient for surgery o Provide pre-operative teaching o Provide post-operative monitoring to include: o Assess for pain and provide pain management o Monitor for bleeding o Monitor peripheral pulses o Monitor surgical site for signs of infection o Provide patient teaching to include: o Importance of assessing affected extremity o Importance of lifestyle modification to include: o Diet modification o Smoking cessation o Adherence to medication regimen o Instruction on wound care o Identification of safety hazards in the home Peripheral venous disease Results from thrombus formation, defective valves, and skeletal muscle weakness. These conditions interrupt the blood flow throughout the venous system. • Causes o Defective valves o Skeletal muscle weakness o Thrombus formation • Symptoms • Nursing Interventions o Monitor intake and output to assure adequate hydration o Apply graduated compression stockings or intermittent pneumatic compression devices to prevent deep vein thrombosis o Encourage patient ambulation o Prepare the patient for surgical intervention if indicated o Provide post-operative monitoring to include: o Inspect the groin site status post angiogram for bleeding and infection o Perform a neurovascular check o Administer anticoagulation therapy as prescribed o Provide patient and family education on: o Importance of adherence to prescribed medications o Instruct the patient on dietary requirements and foods to avoid if on Coumadin o Instruct the patient regarding the importance of follow-up labs for monitoring of anticoagulation therapy o Instruct the patient to avoid medications or activities that can increase the chance of bleeding Aneurysms • Causes o Atherosclerosis o Hypertension o Hyperlipidemia o Smoking o Age o Gender o Family history • Diagnosis o CT Scan o Ultrasonography o Thoracic MRI o Transesophageal echocardiogram • Treatment o Medications ▪ Beta blockers (propranolol) ▪ Antihypertensives ▪ Analgesics ▪ Blood products o Aneurysmectomy o Endovascular stent grafts o Abdominal aortic repair • Nursing Interventions o Frequent blood pressure monitoring to avoid periods of hypertension in order to avoid rupture o Adherence to medication regimen to maintain blood pressure o Prepare the patient for emergency surgery if the patient is exhibiting signs and symptoms of rupture, such as sudden intense chest or back pain, trouble swallowing, trouble breathing, or hypotension o Provide post-operative monitoring to include: o Hemodynamic status o Monitor incision for bleeding or infection o Assess pain and provide management o Administer blood and blood products Coronary artery disease Narrowing of the coronary arteries due to the presence of atherosclerosis • Causes o Hypertension o Smoking o High cholesterol • Patient Education o Limit cholesterol (<200mg/day) o Limit sodium (<1500mg/day) o Avoid trans fats o At least 40 minutes of moderate exercise o Don’t/quit smoking • Management o Check lipids daily o Manage diabetes o Check BP regularly Angina Pectoris • Medication – Nitroglycerine • What are the medication parameters for Nitro?? o No phosphodiesterase inhibitors for erectile dysfunction such as sildenafil (Viagra, Revatio), tadalafil (Cialis), or vardenafil (Levitra) within the past 24 to 48 hours o Three doses 5-minutes apart • What diagnostic test should be performed? o EKG o Cardiac catheterization • Assessment Findings o Aching o Burning o Discomfort o Dizziness o Fatigue o Feeling of fullness in your chest o Feeling of heaviness or pressure Females can experience atypical angina Acute coronary syndrome ACS is the continuum of Angina to Myocardial Infarction. There is an imbalance between cardiac O2 supply and demand. • Diagnosis o 12 lead ECG o Troponin T & I – test to assess cardiac tissue necrosis o Thallium scans – assess for ischemic or necrotic tissue o CT o Cardiac catheterization • Assessment Findings o Chest pain or discomfort, which may involve pressure, tightness or fullness. o Pain or discomfort in one or both arms, the jaw, neck, back or stomach. o Shortness of breath. o Feeling dizzy or lightheaded. o Nausea. o Sweating. • Treatment o Manage pain o Medications ▪ Nitroglycerine ▪ Beta blockers ▪ Calcium channel blockers ▪ ACE inhibitors o O2 o Thrombolytic therapy o Percutaneous coronary intervention o Coronary artery bypass graft surgery • Multidimensional Care o Administer oxygen as prescribed o Administer nitroglycerin as prescribed o Administer Morphine as prescribed o Administer aspirin as prescribed o Assess the patient’s appropriateness of thrombolytic therapy by reviewing the contraindications o Prepare the patient for nonsurgical intervention Cardiac Dysrhythmias Normal Sinus rhythm o There is one P wave for each QRS complex. Sinus bradycardia - <60 bpm • Symptoms o Syncope (“blackouts” or fainting) o Dizziness and weakness o Confusion o Hypotension o Diaphoresis (excessive sweating) o Shortness of breath o Chest pain • Treatment o Temporary pacing o Permanent pacemaker Sinus Tachycardia A Fib Atrial Flutter V Tach V Fib Supraventricular Tachycardia (SVT) Premature Ventricular Contraction (PVC) Hematological Disorders Sickle cell disease • Symptoms o Pulmonary HTN o High risk output failure o JVD o Extremities distal to blood occlusion are cold with slow capillary refill o Priapism o Pallor or cyanosis • Priority o Hydration o O2 o Pain management • Best treatment o Blood transfusion o Warm compresses on pain areas Anemia o Symptoms o Pallor of the ears, nail beds, the conjunctiva, and around the mouth o Cold to the touch o Cold intolerance o Brittle nails o Tachycardia o Murmurs o Orthostatic hypotension o Dyspnea on exertion o Decreased O2 saturation o Increased somnolence and fatigue o Causes o Headache o Sickle cell disease ▪ Autosomal-recessive inheritance of two defective gene alleles for hemoglobin synthesis o Glucose-6-phosphate dehydrogenase (G6PD) deficiency anemia ▪ X-linked recessive deficiency of the enzyme G6PD o Autoimmune hemolytic anemia ▪ Abnormal immune function in which a person's immune reactive cells fail to recognize his or her own red blood cells as self-cells o Iron deficiency anemia ▪ Inadequate iron intake caused by: ▪ Iron-deficient diet ▪ Chronic alcoholism ▪ Malabsorption syndromes ▪ Partial gastrectomy ▪ Pregnancy ▪ Adolescence o Infection ▪ Vitamin B12 deficiency anemia ▪ Dietary deficiency ▪ Partial gastrectomy ▪ Pernicious anemia ▪ Malabsorption syndromes o Folic acid deficiency anemia ▪ Dietary deficiency ▪ Malabsorption syndromes ▪ Oral contraceptives ▪ Anticonvulsants ▪ Methotrexate o Aplastic anemia ▪ Radiation ▪ Benzene ▪ Chloramphenicol ▪ Alkylating agents ▪ Antimetabolites ▪ Sulfonamides ▪ Insecticides ▪ Epstein-Barr virus ▪ Hepatitis B ▪ Cytomegalovirus o Patient Education o Drink 3-4 L of fluid a day o Avoid smoking and alcohol o Contact HCP at the first sign of infection o Get flu shots yearly o Inquire about pneumonia vaccine o Avoid extreme hot or cold temperatures o Consider genetic counseling Polycythemia vera Slow-growing blood cancer disorder in which there is an increase in red blood cell production leading to leukocytosis, thrombocytosis, and elevated hemoglobin levels above normal. These abnormal clonal stem cells interfere with normal cell growth. This uncontrollable growth results in abnormally viscous blood that impedes circulation and increases the risk of intravascular thrombosis formation. • Nursing Care o Apheresis - withdrawal of whole blood and removal of some of the patient's blood components, in this case RBCs. The plasma is then reinfused back into the patient (Blood donation to reduce blood volume) o IV fluids o Pain Medication Hereditary hemochromatosis Hereditary hemochromatosis is a hereditary disorder that causes the body to absorb too much iron. Excess iron is stored in the liver, spleen, heart, joints, skin, and pancreas. These iron deposits can result in organ failure. • Symptoms o Abdominal pain o Liver enlargement o Hyperglycemia o A gradual darkening of the skin o Diabetes o Liver cirrhosis o Endocrine gland failure o Heart disease o Death Myelodysplastic syndromes Myelodysplastic syndromes are a group of disorders caused by the formation of abnormal cells in the bone marrow. The abnormal cell production is due to a loss of normal cellular regulation. These abnormal cells are destroyed once they are released into the blood resulting in a reduction of white blood cells and platelets. • Diagnosis o CBC o Bone marrow biopsy • Assessment Findings o Anemia – Low RBC o Neutropenia – Low WBC (risk for infection) o Thrombocytopenia – Low platelets (bleeding risk) • Treatment o Antitumor medications o Erythrocyte stimulating drugs o Stem cell transplant • Multidimensional Care o Monitor for signs of bleeding o Administer blood and blood products for anemia o Administer platelets for thrombocytopenia o Educate the patient and family on stem cell transplant Leukemia • Assessment Findings o Ecchymoses o Petechiae o Infected lesions o Pallor o Bleeding gums o Anorexia/ weight loss o Bone and joint pain o Tachycardia o Orthostatic hypotension o Dyspnea on exertion o Fatigue o Headache o Fever • Nursing Interventions o Monitor for bleeding o Administer blood and blood products as needed o Provide adequate nutrition based on patent preference o Perform a skin assessment to identify potential break down. Turn the patient every two hours. o Implement neutropenic precautions o Monitor patient for adverse effects of treatment o Administer antiemetics if the patient experiences nausea and vomiting with chemotherapy treatment o Educate the patient and family on stem cell transplant o Educate the patient and family for post-discharge care to include management of a central venous catheter o Educate the patient and family on palliative and hospice care if unresponsive to treatment Lymphomas • Assessment Findings o Fevers o Night sweats o Unplanned weight loss • Diagnostics o CBC o Bone marrow biopsy o Liver function test o CT o PET scan • Treatment o Chemo o Antiemetics o Antidiarrheals o Blood transfusions o External beam radiation o Stem cell transplant Myeloma • Symptoms o Fatigue o Easy bruising o Bone pain & fractures o Frequent urination o Infection o Hypercalcemia o Fluid imbalance • Nursing Interventions o Maintain proper body alignment to promote comfort o Implement fall risk strategies in order to prevent injury o Prepare the patient for radiation treatment o Administer antiemetics if the patient experiences nausea and vomiting with chemotherapy treatment o Inspect skin to assure no breakdown, implement pressure reduction intervention (turning and position q2 hours, off load boney prominences) o Educate the patient on dialysis if needed o Educate the patient on surgical intervention if needed o Administer medications as prescribed Thrombocytopenia • Treatment o Implement bleeding precautions o Implement fall risk strategies in order to prevent injury o Provide emotional support o Platelet transfusion for decreased platelet count o Maintain a safe environment to prevent injury o Post-operative management if indicated Hemophilia • Diagnosis o aTTP – measures clotting ability • Assessment Findings o Bleeding o Blood in stool and urine o Bruising o Heavy or prolonged periods o Internal bleeding, nosebleed o Swollen joint o Tachycardia o Tachypnea • Treatment o Injections of clotting factors VIII or IX • Multidimensional Care o Implement bleeding precautions o Implement fall risk strategies in order to prevent injury o Provide emotional support o Maintain a safe environment to prevent injury o Prepare patient for regularly scheduled infusions of synthetic factor VIII or the infusion of this substance only when injury or bleeding occurs [Show More]
Last updated: 2 years ago
Preview 1 out of 26 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Feb 25, 2022
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Feb 25, 2022
Downloads
0
Views
86