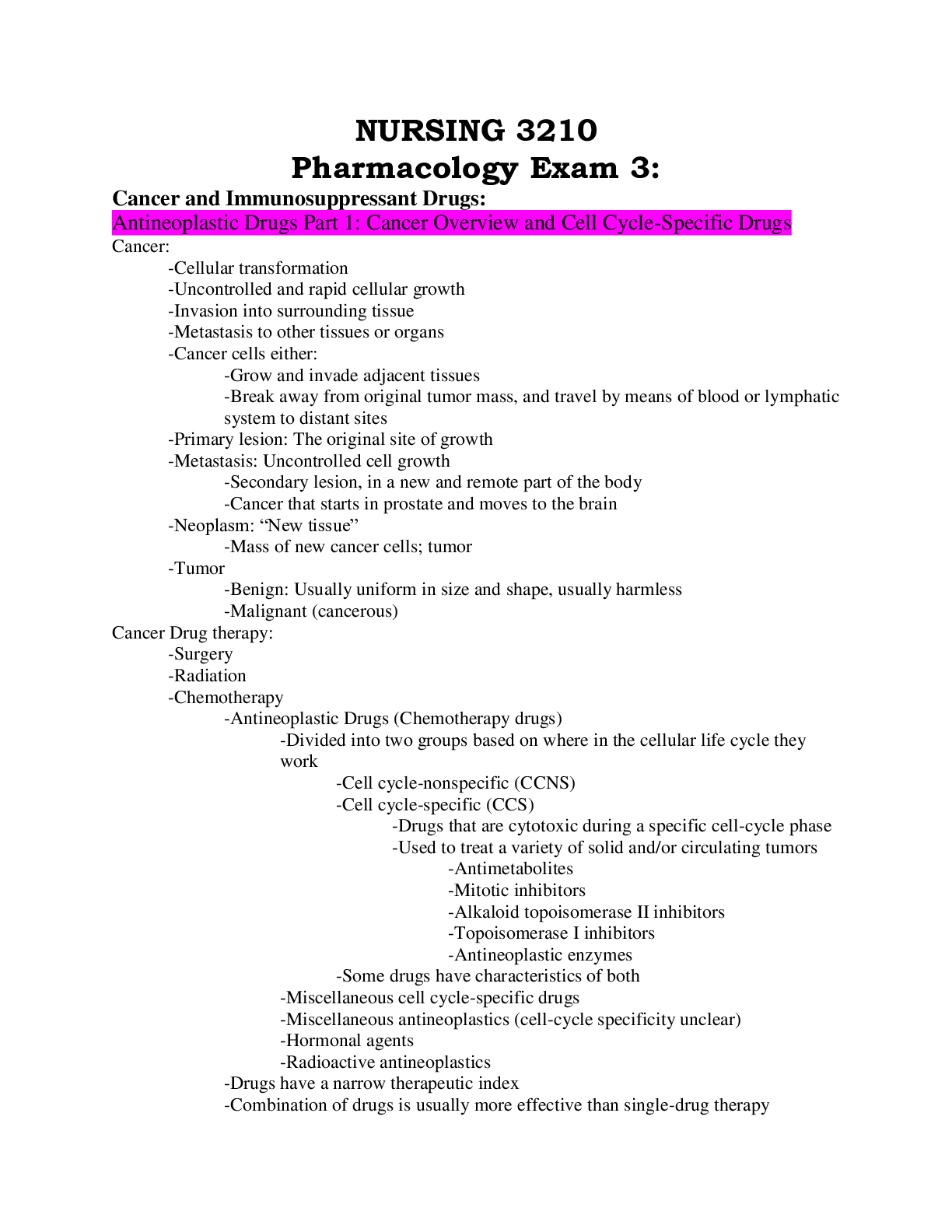
NURSING 3210
Pharmacology Exam 3:
Cancer and Immunosuppressant Drugs:
Antineoplastic Drugs Part 1: Cancer Overview and Cell Cycle-Specific Drugs
Cancer:
-Cellular transformation
-Uncontrolled and rapid cellular gro
...
NURSING 3210
Pharmacology Exam 3:
Cancer and Immunosuppressant Drugs:
Antineoplastic Drugs Part 1: Cancer Overview and Cell Cycle-Specific Drugs
Cancer:
-Cellular transformation
-Uncontrolled and rapid cellular growth
-Invasion into surrounding tissue
-Metastasis to other tissues or organs
-Cancer cells either:
-Grow and invade adjacent tissues
-Break away from original tumor mass, and travel by means of blood or lymphatic
system to distant sites
-Primary lesion: The original site of growth
-Metastasis: Uncontrolled cell growth
-Secondary lesion, in a new and remote part of the body
-Cancer that starts in prostate and moves to the brain
-Neoplasm: “New tissue”
-Mass of new cancer cells; tumor
-Tumor
-Benign: Usually uniform in size and shape, usually harmless
-Malignant (cancerous)
Cancer Drug therapy:
-Surgery
-Radiation
-Chemotherapy
-Antineoplastic Drugs (Chemotherapy drugs)
-Divided into two groups based on where in the cellular life cycle they
work
-Cell cycle-nonspecific (CCNS)
-Cell cycle-specific (CCS)
-Drugs that are cytotoxic during a specific cell-cycle phase
-Used to treat a variety of solid and/or circulating tumors
-Antimetabolites
-Mitotic inhibitors
-Alkaloid topoisomerase II inhibitors
-Topoisomerase I inhibitors
-Antineoplastic enzymes
-Some drugs have characteristics of both
-Miscellaneous cell cycle-specific drugs
-Miscellaneous antineoplastics (cell-cycle specificity unclear)
-Hormonal agents
-Radioactive antineoplastics
-Drugs have a narrow therapeutic index
-Combination of drugs is usually more effective than single-drug therapy-Nearly all drugs cause adverse effects
-Dose-limiting adverse effects
-Patient can no longer tolerate therapy
-Harmful to all rapidly growing cells
-Harmful cancer cells
-Healthy, normal human cells
-Hair follicles
-GI Tract cells (N/V/D)
-Diarrhea- lose a lot of electrolytes
-Bone Marrow cells
-Anemia, platelets destroyed, WBC destroyed
Cell Cycle Specific Drugs: Antimetabolites
-Folate (folic acid) antagonist
-Methotrexate (MTX), pemetrexed, palatrexate
-Interferes with the use of folic acid
-As a result, DNA is not produced, and the cell dies
-Give leukoforin rescue to protect healthy cells and to keep the patient from
having so much bone marrow suppression
-Pyramidine antagonists
-Fluorouracil (5-FU), floxuridine (FUDR)
-Interrupts metabolic pathways of pyramidine bases
-Results in interruption of DNA and RNA synthesis
-So they are not able to produce
-Treats a variety of cancers
-Purine antagonists
-Cladribine (Leustatin), fludarabine (F-AMP)
-Treats leukemia and lymphoma patients
-Interrupts metabolic pathways of purine nucleotides
-Results in interruption of DNA and RNA synthesis
-Tumor lysis syndrome: Causes patient to have elevated phosphate and potassium
levels and decreased calcium levels
-Some patients need to be placed on dialysis
-pg. 733-734
-Antimetabolites: Indications:
-Used in combination with other drugs to treat various types of cancer, such as
solid tumors and some hematologic cancers
-Acute and chronic lymphocytic leukemias
-Leukemias (several types)
-Colon, rectal, breast, stomach, lung, pancreatic cancers
-Oral and topical forms may be used for low-dose maintenance and palliative
cancer therapy
-Often used in combination chemotherapy regimens
-Methotrexate is also used to treat severe cases of psoriasis and rheumatoid
arthritis
-Antimetabolites: Adverse Effects
-Hair loss, nausea, vomiting, myelosuppression-Neurologic, cardiovascular, pulmonary, hepatobiliary, GI genitourinary,
dermatologic, ocular, otic, and metabolic toxicity
-Tumor lysis syndrome
-Palmar-plantar dysesthesia (also called hand-foot syndrome), Stevens-Johnson
syndrome, toxic epidermal necrolysis
-Risk for bleeding (bleeding gums, sores, bruising)
-Patients will feel very tired, will lose a lot of weight
Cell Cycle Specific Drugs: Mitotic Inhibitors
-Vinca alkaloids (periwinkle plant)
-Vinblastine, vincristine, vinorelbine
-Taxanes
-Docetaxel (European yew tree: needles)
-Paclitaxel (Western yew tree: bark)
-Dosage on page 736
-Indications:
-Often used in combination therapies
-Used to treat a variety of solid tumors and some hematologic malignancies
-Testicular, small cell lung, breast, ovarian, non-small cell lung cancers
-Kaposi’s sarcoma: AIDS related, very weak immune system
-Acute leukemia
-Adverse Effects:
-Hair loss, nausea, vomiting, myelosuppression
-Liver, kidney, lung toxicities
-Convulsions
-Extravasation
-Several specific antidotes can be used
Cell cycle Specific Drugs: Alkaloid Topoisomerase II Inhibitors
-Derived from mandrake plants
-Used to treat small cell lung cancer and testicular cancer
-Not used as much now because of significant toxicities without therapeutic benefit
-Etoposide (VP-16)
-Paclitaxel (Taxol)
Cell Cycle Specific Drugs: Topoisomerase 1 Inhibitors (Camptothecins)
-Derived from camptothecin, a substance taken from a Chinese shrub
-Topotecan (Hycamtin)
-Irinotecan (CPT-11, Camptosar)
-Prevent DNA regulation
-Indications:
-Ovarian and colorectal cancer
-Small cell lung cancer
-Other tumors (Cervical cancer, evolved cancer)
-Adverse effects:
-Bone marrow suppression (predictable, reversible, noncumulative, manageable)
-GI Effects (Nausea, vomiting, diarrhea)
-Irinotecan causes cholinergic diarrhea (delayed, 2-10 days after dosage)
-Used to use immodiumCell Cycle Specific Drugs: Antineoplastic Enzymes
-Synthesized using cultures of bacteria and recombinant DNA technology
-As a result, an enzyme is produced
-This enzyme is isolated nad purified for clinical use
-Asparaginase (Elspar): Used to treat acute lymphocytic leukemia
-Pegaspargase (Oncaspar)
Cell Cycle Specific Drugs: Nursing Implications:
-Assess baseline blood counts before administering antineoplastic medications
-Follow specific administration guidelines for each antineoplastic drug
-Remember that all rapidly dividing cells (both normal and cancer cells) are affected
-Mucous membranes
-Hair follicles
-Bone marrow component
-Monitor for effects on these tissues or complications
-Monitor for complications
-GI mucous membranes, stomatitis, altered bowel function with high risk for poor
appetite, nausea, vomiting, diarrhea, and inflammation and possible ulcerations of
GI mucosa
-Monitor for complications:
-Alopecia
-Bone marrow components: dangerously low (life-threatening) blood cell counts
-Monitor for adverse effects specific to the type of antineoplastic drug given
-Implement measures to monitor for and prevent infection in patients with neutropenia or
leukopenia
-Reverse isolation
-Implement measures to monitor for and prevent bleeding in patients with
thrombocytopenia and anemia
-Keep in mind that anemia may result in severe fatigue
-Monitor for stomatitis (oral inflammation and ulcerations), and implement measures to
reduce the effects if it occurs
-Anticipate nausea and vomiting, and implement measures to reduce these effects
-Antiemetics often work better if given 30-60 min before chemotherapy is started
-Women of childbearing age will need to use a nondrug form of contraception during
therapy
-In addition to physical measures, keep in mind the need for emotional support during
this time for both the patient and family
-Monitor for therapeutic responses to antineoplastic therapies and the many possible
adverse effects
Antineoplastic Drugs Part 2: Nonspecific Drugs and Miscellaneous Drugs
Alkylating Drugs:
-Classic alkylators (nitrogen mustards)
-Nitrosoureas
-Miscellaneous akylators
-Mechanism of Action:-Work by preventing cancer cells from reproducing
-Alter the chemical structure of the cells’ DNA
-Bifunctional or polyfunctional
-Indications: Used in combination with other drugs to treat various types of cancer
-Recurrent ovarian cancer
-Brain tumor
-Lymphomas
-Leukemias
-Breast cancer
-Bladder cancer
-Others
-Adverse Effects:
-Dose-limiting adverse effects
-Nausea and vomiting, myelosuppression
-Alopecia
-Nephrotoxicity, peripheral neuropathy, ototoxicity
-Hydration can prevent nephrotoxicity (keeps fluid flowing)
-Extravasation causes tissue damage and necrosis
-Discontinue medication immediately
-Examples:
-Cisplatin (Platinol)
-Cyclophosphamide (Cytoxan)
-Mechlorethamine (Nitrogen mustard)
-Nursing Implicaitons:
-Monitor for expected effects of bone marrow suppression
-Expect nausea, vomiting, diarrhea, stomatitis
-Hydration is important to prevent nephrotoxicity
-Report ringing/ roaring in the ears- possible ototoxicity
-Report tingling, numbness, or pain in extremities- peripheral neuropathies may
occur
Cytotoxic Antibiotics:
-Natural substances produced by the mold Streptomyces
-Synthetic substances also used
-Used only for cancer; too toxic to treat infections
-Anthracycline antibiotics
-Daunorubicin, doxorubicin, epirubicin, idarubicin, valrubicin
-Other cytotoxic antibodies
-Bleomycin, dactinomycin, mitomycin, mitoxantrone, plicamycin
-Indications:
-Used in combination chemotherapy regiments
-Used to treat a variety of solid tumors and some hematologic malignancies
-Leukemia, ovarian, breast, bone, others
-Squamous cell carcinomas
-AIDS-related Kaposi’s sarcoma (when intolerant to other therapies
-Adverse Effects:
-All can produce bone marrow suppression, except bleomycin-Hair loss, nausea, vomiting, myelosuppression
-Heart failure (daunorubicin)
-Acute left ventricular failure (doxorubicin)
-Pulmonary fibrosis and pneumonitis (bleomycin)
-Liver, kidney, and cardiovascular toxicities
-Many others
-Cardiomyopathy is associated with large amounts of doxorubicin (Adriamycin)
-Routine monitoring of cardiac ejection fraction with multiple-gated
acquisition (MUGA) scans
-Need a baseline
-Cumulative dose limitations
-Cytoprotective drugs such as dexrazoxane (Zinecard) can decrease the
incidence of this devastating toxicity
-Nursing Implications:
-Expect bone marrow suppression, nausea, vomiting, diarrhea, stomatitis
-Monitor heart, lungs, pulmonary fibrosis may occur
-Monitor for nephrotoxicity, liver toxicity
-Monitor cardiovascular status
-Daunorubicin may turn the urine a reddish color
Miscellaneous Antineoplastics:
-Bavacizumab (Avastin)
-Angiogenesis inhibitor
-Blocks blood supply to the growing tumor
-Used to treat metastatic colon cancer, rectal cancer in combination with 5-
fluorouracil, non-small cell lung cancer, and malignant glioblastoma
-Many adverse effects, including nephrotoxicity
-Hydroxyurea (Hydrea, Droxia)
-Action similar to antimetabolites
-Used to treat squamous cell carcinoma and some leukemias
-Imatinib (Gleevec)
-Used to treat chronic myeloid leukemia (CML)
-Mitotane (Lysodren)
-Not as common
-Adrenal cytotoxic drug
-Used specifically for inoperable adrenal corticoid carcinoma
-Oral form only
Hormonal Drugs:
-Used to treat a variety of neoplasms in men and women
-Hormonal therapy used to:
-Oppose effects of hormones
-Block the body’s sex hormone receptors (antagonize the body so cells don’t grow
as rapidly)
-Used most commonly as adjuvant and palliative therapy
-But may be used a drug of first choice for some cancers
-pg 755
-Female-Specific Neoplasms:-Aromatase inhibitors
-Anastrozole, aminoglutethiamide
-Selective estrogen receptor modulators
-Tamoxifen, toremifene
-Progestins
-Megestrol (Megace), medroxyprogesterone
-Megace also stimulates appetite
-Androgens
-Fluoxymesterone, testolactone
-Estrogen receptor antagonist
-Fulvestrant
-Male-Specific Neoplasms
-Antiandrogens
-Bicalutamide, flutamide, nilutamide
-Gonadrotropin-releasing hormone antagonists
-Leuprolide, goserelin
-Antineoplastic hormone
-Estramustine
Extravasation:
-Leaking of an antineoplastic drug into surrounding tissues during IV administration
-Can result in permanent damage to nerves, tendons, muscles; loss of limb
-Skin grafting or amputation of that limb may be necessary
-Prevention is essential
-Continuous monitoring of IV site is essential
-If you suspect extravasation, stop infusion immediately. With IV site in place, aspirate to
pull back out any medication until you get blood. Call doctor to tell him what happened,
consult pharmacy to find antidote to that drug. Elevate affected limb. May need dressing,
hot/cold packs. DOCUMENT WHAT HAPPENED, WHAT IT LOOKED LIKE.
Handling Antineoplastic Drugs:
-Those preparing and administering these drugs may be exposed to negative
consequences
-Most facilities have these drugs mixed under special environments in the pharmacy
-All nurses must be certified to handle these drugs!!!!!!
-During care of a patient receiving these drugs, special precautions may be implemented,
depending on facility policies
-Double flushing of bodily fluids in the commode
-Special hampers for disposal of all objects
-Personal Protective equipment
-Special concerns if chemotherapy liquid spills
Nursing Implications:
-Assess baseline blood counts before administering antineoplastic drugs
-Follow administration guidelines for each antineoplastic drug
-Monitor closely for anaphylactic reactions
-Keep epinephrine, antihistamines, and anti-inflammatory drugs on hand
-Monitor closely for complications associated with bone marrow suppression
-Anemia, thrombocytopenia, neutropenia-Fever, anemia, fatigue
-Monitor for oncologic emergencies
-Infections, pulmonary toxicity, allergic reactions, stomatitis with severe
ulcerations, bleeding, metabolic aberrations, bowel irritability with diarrhea,
renal, liver, cardiac toxicity
-Cytoprotective drugs may be used to reduce toxicities
-IV Amifostine to reduce renal toxicity associated with Cisplatin
-IV or PO Allopurinol to reduce hyperuricemia
Biologic Response- Modifying and Antirheumatic Drugs:
BRM’s:
-Alter the body’s response to diseases such as cancer and autoimmune, inflammatory, and
infectious diseases
-Hematopoietic drugs
-Immunomodulating drugs
-Interferons
-Monoclonal antibodies
-Interleukin receptor agonists and antagonists
-Miscellaneous drugs
-Fourth part of cancer therapy in addition to surgery, chemo, radiation
-Also used for other diseases
-Autoimmune: MS, Lupis
-Inflammatory
-Infectious
-Mechanism of action:
-Enhancement or restoration of the host’s immune system defenses against the
tumor
-Direct toxic effect on the tumor cells, which causes them to lyse, or rupture
-Adverse modification of the tumor’s biology, which makes it harder for the
tumor cells to survive and reproduce
-Therapeutic Effects of BRMs
-Regulation or enhancement of the immune response
-Cytotoxic or cytostatic activities against cancer cells
-Inhibition of metastases, prevention of cell division, or inhibition of cell
maturation
Hematopoietic Drugs (HD’s):
-HD’s promote the synthesis of various types of major blood components by promoting
growth, or differentiation, and function of their precursor cells in the bone marrow
-Produced by rDNA technology
-HDs are used to:
-Decrease duration of chemotherapy-induced anemia, neutropenia, and
thrombocytopenia
-Enable higher doses of chemotherapy to be given
-Build up WBC, platelets, not losing all of these cells
-Erythropoietic Drugs:
-Epoetin alfa (Epogen, Procrit)-Synthetic derivative of the hormone erythropoietin (produced in kidneys)
-Promotes synthesis of RBCs by stimulating RBC precursor
-Darbepoetin alfa (Aranesp)
-Colony-Stimulating factors (CSFs)
-Filgrastim (Neupogen)
-Granulocyte colony-stimulating factor (G-CSF)
-Stimulates precursor cells for the type of WBCs known as granulocytes
-Administered before patient develops infection
-Do not given within 24 hours of a patient recieving myosuppressant
antineoplastic drugs
-Pegfilgrastim (Neulasta)
-Longer-acting form of filgrastim
-Sargramostin (Leukine)
-Indicated for promoting bone marrow recovery after autologous (own
marrow) or allogenic (donor marrow) bone marrow transplantation in
patients with leukemia and lymphoma
-Platelet-promoting drugs:
-Oprelevekin (Neumega)
-Enhances synthesis of platelets
-Indicated for the prevention of chemotherapy-induced severe
thrombocytopenia and avoidance of the need for platelet transfusions
-Mechanism of Action:
-Decrease the duration of chemotherapy induced anemia, neutropenia, and
thrombocytopenia
-Allow for higher dosages of chemotherapy
-Decrease bone marrow recovery time after bone marrow transplantation or
irradiation
-Stimulate other cells in the immune system to destroy or inhibit the growth of
cancer cells, as well as virus- or fungus-infected cells
-Indications
-Used in patients who have experienced destruction of bone marrow cells as a
result of cytotoxic chemotherapy
-Decrease the duration of low neutrophil counts, thus reducing the incidence and
duration of infections
-Enhance the functioning of mature cells of the immune system, resulting in
greater ability to kill cancer cells as well as viral- and fungal-infected cells
-Also enhance RBC and platelet counts in patients with bone marrow suppression
resulting from chemotherapy
-Allow for higher doses of chemotherapy, resulting in the destruction of a greater
number of cancer cells
-Adverse Effects:
-Usually mild
-Most common: Fever, muscle aches, bone pain, flushing
Immunomodulating Drugs:
-Medications that therapeutically alter a patient’s immune response to malignant tumor
cells-Drugs that modify the body’s own immune response so that it can destroy various
viruses and cancerous cells
Interferons (IFNs)
-Proteins with three basic properties:
1. Antiviral
2. Antitumor
3. Immunomodulating
-Used to treat certain viral infections and cancer (pg 769 complete list of drugs)
-Effects on Immune System:
-Restore the immune system’s function if it is impaired
-Augment the immune system’s ability to function as the body’s defense
-Inhibit the immune system from working
-Helpful in autoimmune disorders
-Indications:
-Viral Infections: Genital warts, hepatitis
-Cancer:
-Chronic myelogenous leukemia, follicular lymphoma, hairy-cell
leukemia, Kaposi’s sarcoma, malignant melanoma
-Autoimmune disorders: Multiple Sclerosis
-Adverse Effects:
-Flulike effects: Fever, chills, headaches, myalgia
-Dose-limiting adverse effect is fatigue
-Other adverse effects: Anorexia, Dizziness, Nausea, Vomiting, Diarrhea
Cancer and Immunosuppressant Drugs: Biologic Response-Modifying and
Antirheumatic Drugs:
Monoclonal Antibodies (MABs):
-Treatment of cancer, rheumatoid arthritis, multiple sclerosis, and organ transplantation
-Specifically target cancer cells and have minimal effect on healthy cells
-Fewer adverse effects than traditional antineoplastic medications
-Cancer treatment:
-Alemtuzaumab (Campath)
-Bevacizumab (Avastin)
-Cetuximab (Erbitux)
-Other disease processes, including rheumatoid arthritis
-Adalimumab (Humira)
-Infliximab (Remicade)
Interleukins:
-Beneficial antitumor action
-Interleukin receptor agonists
-Aldesleukin (Proleukin)
-Treatment of metastatic renal cell carcinoma and metastatic melanoma
-Off-label uses include HIV infection and AIDS, and non-Hodgkin’s
lymphoma
-Denileukin diftitox (Ontak)-Tocilizumab (Actemra)
-Anakinra (Kineret)
-IL-1 receptor antagonist
-Used to control symptoms of rheumatoid arthritis
-Autoimmune disorder causing inflammation and tissue damage in
joints
-Diagnosis primarily symptomatic
-Treatment consists of NSAIDs and disease-modifying
antirheumatic drugs
-Capillary Leak Syndrome:
-Severe toxicity of aldesleukin therapy
-Capillaries lose ability to retain vital colloids in the blood; these substances are
“leaked” into the surrounding tissues
-Result: Massive fluid retention
-Respiratory distress
-Heart failure
-MI
-Dysrhythmias
-Reversible after interleukin therapy is discontinued
Disease-Modifying Antirheumatic Drugs (DMARDs)
-Modify the disease of rheumatoid arthritis
-Exhibit anti-inflammatory, antiarthritic, and immunomodulating effects
-Slow onset of action of several weeks, versus minutes to hours for NSAIDs
-Also referred to as slow-acting Antirheumatic drug (SAARDs)
-Arthritis Drugs:
-Methotrexate
-Etanercept (Enbrel)
-Used to treat rheumatoid arthritis (including juvenile RA) and psoriasis
-Patients must be screened for latex allergy (some dosage forms may
contain latex)
-Onset of action: 1 to 2 weeks
-Contraindicated in presence of active infections
-Reactivation of hepatitis and TB have been reported
-Subcutaneous injection given weekly usually
-Abatacept (Orencia)
-Used to treat rheumatoid arthritis
-Caution if history of recurrent infections or COPD
-Patients must be up to date on immunizations before starting therapy
-May increase risk of infections associated with live vaccines
-May decrease response to vaccines
-Given IV every 4 weeks and must obtain height and weight
-Leflunomide (Arava)
Nursing Implications:
-Assess for allergies, specifically allergies to egg proteins, IgG, or neomycin
-Assess for conditions that may be contraindications
-Assess baseline blood counts; perform cardiac, renal, and liver studies-Assess for presence of infection
-Follow specific guidelines for preparation and administration of drugs
-Monitor the patient’s response during therapy
-Teach patients to report signs of infection immediately
-Sore throat
-Diarrhea
-Vomiting
-Fever over 100.5 (38.1 C) or higher
Cancer and Immunosuppressant Drugs: Immunosuppressant Drug
-Drugs that decrease or prevent an immune response, thus suppressing the immune system
-Used to prevent or treat rejection of transplanted organs
-All suppress certain T-lymphocyte cell lines, thus preventing their involvement in the immune
response
-Results in a pharmacologically immunocompromised state
-Mechanisms of action vary according to drug
-Major classes used to prevent organ rejection:
-Glucocorticoids
-Calcineurin inhibitors
-Antimetabolites
-Biologics
-Indications vary from drug to drug
-Primarily indicated for the prevention of organ rejection
-Drugs:
-Muromonab-CD3 (Orthoclone OKT3), Mycophenolate (CellCept), and tacrolimus
(Prograf) are indicated for both prevention of rejection and treatment of organ rejection
-Muromonab-CD3 is the only drug indicated for reversal of organ rejection
once rejection of a transplanted organ has started
-Azathioprine (Imuran)
-Prophylaxis of organ rejection concurrently with other immunosuppressant
drugs, such as cyclosporine and corticosteroids
-Also used in the treatment of rheumatoid arthritis
-Cyclosporine (Sandimmune)
-Prevention of organ rejection
-May be used for other autoimmune disorders
-Use a styrofoam container to administer to increase potency
-Tacrolimus (Prograf)
-Used for the prevention of liver transplant rejection
-Other uses are unlabeled uses
-Glatiramer acetate (Copaxone)
-Works by blocking T-cell autoimmune activity against myelin protein, which
reduces the frequency of the neuromuscular exacerbations associated with
multiple sclerosis
-Muromonab-CD3 (Orthoclone OKT3)
-Reversal and prevention of graft rejection-The only immunosuppressant drug used for the treatment of MS
-Used to reduce the frequency of MS relapses (exacerbations) in relapsingremitting multiple sclerosis (RRMS)
-Mycophenolate (CellCept)
-Indicated for the prevention of organ rejection as well as the treatment of organ
rejection
-FDA blackbox warning for increased risk of congenital malformations and
spontaneous absorptions when used during pregnancy
-Common side effects include hypertension, hypotension, peripheral edema,
tachycardia, pain, headache, hyperglycemia, hyperlipidemia, electrolyte
disturbances, and others
Adverse effects:
-Vary according to drugs and may be devastating
-All immunosuppressed patients have a heightened susceptibility to opportunistic
infections
Nursing Implications:
-Perform a thorough assessment before administering these drugs
-Renal, liver, and cardiovascular function studies
-CNS baseline function
-Respiratory assessment
-Baseline vital signs
-Baseline laboratory studies, including hemoglobin, hematocrit, WBC, and
platelet counts.
-Assess for contraindications, drug allergies, and drug interactions
-Monitor WBC counts throughout therapy; if the count drops below normal range,
contact the prescriber
-Oral immunosuppressant should be taken with food to minimize GI upset
-Oral forms are used when possible to decrease the risk of infection that may occur with
parenteral injections
-Grapefruit juice also interacts with some of these drugs (i.e. cyclosporine)
-Oral antifungal drugs are usually given with these drugs to treat oral candidiasis that
may occur
-Assess the oral cavity often for white patches on the tongue, mucous membranes, and
oral pharynx
-Mix oral cyclosporine solution in a glass container
-Do not use Styrofoam containers, because the drug adhere to the inside wall of the
container
-Monitor for therapeutic responses
-Monitor for adverse effects and signs of drug toxicity
-Follow guidelines for parenteral administration carefully
-Inform patients that lifelong therapy with immunosuppressants is indicated with organ
transplantation
-Patients taking immunosuppressants should be encouraged to take measures to reduce
the risk of infections
-Avoiding crowds
-Avoiding people with colds or other infections-Inform patients to immediately report fever, sore throat, chills, joint pain, fatigue, or
other signs of a severe infection
Cancer and Immunosuppressant Drugs: Immunizing Drugs and Biochemical
Terrorism
Immunity:
-Immune response
-Antigens
-Antibodies
-Active immunization
-Artificial:
-The body is exposed to a relatively harmless form of an antigen
-The immune system is stimulated and “remembers” this antigen if
subsequent exposures occur
-Does not cause a full-blown infection
-Natural:
-Person acquires by surviving the disease itself and producing antibodies
to the disease-causing organism
-Passive immunization
Biological Antimicrobial Drugs:
-Also called biologicals
-Antitoxins
-Antisera
-Toxoids and vaccines (immunizing biological)
-Used to prevent, treat, or cure infectious diseases
Toxoids:
-Stimulate one’s immune system to produce a specific antibody
-Artificial active immune response
-These antibodies protect against future exposures
Vaccines:
-Suspensions of live, attenuated (weakened) or killed (inactivated) microorganisms
-These slight alterations in the bacteria and viruses prevent the person injection from
contracting the disease
-Also stimulate the production of antigens against a specific antibody
-Vaccinations with live bacteria or virus provide lifelong immunity
-Vaccinations with killed bacteria or virus provide partial immunity, and booster shots
are needed periodically
Active Immunizing Drugs: Examples:
-BCG vaccine (tuberculosis)
-Diphtheria, tetanus, and pertussis toxoids, several forms (Tdap)
-Haemophilus influenza Type B conjunate vaccine (Hib)
-Influenza Virus Vaccine (Fluzone, FluMist)
-Hepatitis B virus vaccines
-Measles, mumps, rubella virus vaccine, live- several forms
-Pneumococcal bacterial vaccines-Human papilloma virus vaccine (Gardasil, carvarix)
-Poliovirus vaccine; several forms
-Rabies virus vaccine
-Smallpox virus vaccine
-Tetanus toxoid
-Varicella virus vaccine (chickenpox)
-Herpes Zoster Vaccine
Indications:
-Active Immunization
-Prevents infection caused by bacterial toxins or viruses
-Provides long-lasting or permanent immunity
-“Herd immunity”
Passive Immunization
-Serum or concentrated immunoglobulins from humans or animals are injected
into a person
-The substances needed to fight off invading microorganisms are given directly to
a person
-The immune system is bypassed
-Short-lived compared with active immunization, but works faster
-Artificial Passive Immunization
-Administration of serum or concentrated immunoglobulins
-Provides the inoculated person the substance needed to fight off the invading
microorganism.
-Bypasses the host’s immune system
-Natural Passive Immunization
-Antibodies are transferred
-From mother to fetus through the placenta
-From mother to infant through breast milk for breastfed infants
Passive Immunizing Drugs:
-Antitoxins
-Immunoglobulins
-Snake and spider antivenins (antivenom)
-Antivenins
-Pit viper, coral snake
-Black widow spider
-Hepatitis B immune globulin
-Rabies immunoglobulin (human) following animal bite
-RhO(D) immune globulin (RhoGAM)
-Tetanus immunoglobulin
-Varicella-zoster immunoglobulin
Indications:
-Passive Immunization:
-Antitoxins, antivenins, immunoglobulins
-Minimizes effects of poisoning by the venoms of spiders and certain snakes
-Provides quick immunity before a person’s own immune system has a chance to
make antibodies (such as in cases of exposure to hepatitis B or rabies viruses)-CDC/Department of Health and Human Services recommendations for adult and
pediatric immunizations (US)
-Provide specific dosages and intervals for immunizations
-Refer to the CDC website for current recommendations
Adverse Effects:
-Range from mild and transient to very serious or life threatening
-Minor effects
-Fever, minor rash, soreness at injection site, itching, adenopathy
-Severe effects
-Fever higher than 103, encephalitis, convulsions, anaphylactic reaction, dyspnea,
others
-Minor reactions
-Treated with acetaminophen and rest
-Serious or unusual reactions
-Serum sickness
-Report serious or unusual reactions to the Vaccine Adverse Event Reporting
System (VAERS)
-Serum sickness can occur after repeated injections of equine made immunizing
drugs
Nursing Implications
-Assess patient’s health history, medication history, allergies, pregnancy status
-Assess previous reactions and responses to immunizations
-Assess for contraindications, including immunosuppression
-Before giving any drug, recheck the specific protocols for administration and schedules
for administration
-Follow manufacturer’s guidelines for drug storage, administration, routes, and site of
administration
-Encourage parents of young children to keep a journal of the child’s immunization status
with dates of immunizations and reactions, if any
-If discomfort occurs at the injection site, apply warm compresses and give
acetaminophen
-Do not give aspirin to children
-Monitor for therapeutic responses and adverse reactions
Illnesses Caused by Possible Bioterrorism Agents:
-Anthrax: Anthrax is a serious illness caused by a spore-forming bacterium. Most often,
anthrax bacteria enter your body through a wound in your skin. You can also become
infected by eating contaminated meat or inhaling the spores.
-Smallpox: Virus.
-Botulism : Botulism is a rare but serious paralytic illness caused by a nerve toxin that is
produced by the bacterium Clostridium botulinum.
-Tularemia : Tularemia is a disease of animals and humans caused by the bacterium
Francisella tularensis. Tick and deer fly bites, skin contact with infected animals, and
ingestion of contaminated water.
-Viral Hemorrhagic Fever : Caused by several viruses.(listed on page 716)-Plague : Plague is an infectious disease caused by Yersinia pestis, a naturally occurring
bacterium found primarily in wild rodents. (Pneumonic plague, Bubonic plague, &
Septicemic plague)
-Bubonic plague is most common and results of an infected flea.
Possible Bioterrorism Agents: Page 809 Table 49-5
-Sarin (nerve gas)
-Mustard (blistering agents)
-Cyanide (blood agent)
-Chlorine (choking agent)
-Radioactive elements
-Ricin
Drugs Affecting the Endocrine System:
Pituitary Drugs:
Neuroendocrine System: Pituitary Hormones
-Hypothalamus (controls the pituitary gland)
-Pituitary gland:
-Two lobes: Anterior and posterior
-Each lobe is individually linked to and communicates with the
hypothalamus to control secretion of hormones
Pituitary Drugs:
-Drug therapy is used primarily to make up for hormone deficiency
-Anterior drugs: Somatotropin, Somatrem
-Growth Hormone
-Stimulate skeletal growth in patient with deficient GH, such as deficient
GH, such as dwarfism
-Posterior: Vasopressin and Desmopressin
-Used in the treatment of diabetes insipidus
-Patient loses a lot of water- they have excessive thirst and diarrhea
-MOA of pituitary drugs:
-Either augments or antagonizes the natural effects of the pituitary
hormones
-Adverse Effects of pituitary drugs
-Affects cardiovascular system, respiratory system, and central nervous
system
-Page 496 Tables 30-2, 30-3, and 30-4
Nursing Implications
-Obtain thorough nursing assessment and medication history
-Assess for contraindications specific to each drug
-No alcohol
-Assess medication history for possible interactions
-Ensure patients understand these drugs DO NOT CURE THE DISEASE
-Provide specific instructions for nasal spray forms of vasopressin
-Do not discontinue drugs abruptly-Do not take over-the-counter products without checking with healthcare provider
-Avoid alcohol when taking these drugs
-Take medication at the same time every single day
-Keep levels normal
-Parents of children who are receiving growth hormones should keep a journal
reflecting the child’s growth.
-Monitor for therapeutic responses
-Monitor for adverse effects
-Patients with Desmopressin:
-Obtain orthostatic vital signs for those patients
-Cardiac enzymes and an EKG
-Desmopressin causes prolonged QT intervals
-You want a baseline EKG
-Monitor patient’s leukocyte levels
Thyroid Gland:
-Secretes hormones essential for proper regulation of metabolism
-Hormones secreted:
-Thyroxine (T4)
-Calcitonin
-
-Hypothyroidism
-Deiciency in thyroid hormones
-Primary hypothyroidism: Abnormal thyroid gland
-Secondary hypothyroidism: Problem with TSH (thyroid stimulating hormone)
-Regulates T3 and T4 hormones
-Thyroid Replacement Drugs:
-Levothyroxine (Synthroid, Levothyroid)
-Synthetic thyroid hormone T4
-Liothyronine (Cytomel)
-Synthetic thyroid hormone T3
-MOA:
-Thyroid preparations are given to replace what the thyroid gland cannot
produce to achieve normal thyroid levels
-Thyroid drugs work the same way as thyroid hormones
-Pregnancy:
-Monitor levels every 3-4 weeks and need to be on the lowest possible
dose
-Thyroid Replacement Drugs: Indications
-To treat all forms of hypothyroidism
-Also used for thyroid replacement therapy
-Adverse Effects:
-Cardiac dysrhythmias are the most significant adverse effects
-Contraindications: Recent MI, hyperthyroidism
-Drug interactions:
-Increases effects of anticoagulants
-Decreases serum levels of dignoxin-Take before meals 30 min-1 hour before eat
-Hyperthyroidism: Excessive thyroid hormone
-Caused by several diseases
-Graves’ disease
-Goiters and eyes protrude
-Heart starts racing (patient will feel it)
-Thyroid storm
-Take with meals (while you eat)
-Affects multiple body systems, resulting in an overall increase in metabolism
-Thyroid storm: Critical care patient
-Leads to death
-Treatment:
-Surgery to remove all or part of the thyroid gland
-Antithyroid drugs: thioamide derivatives
-Methimazole (Tapazole)
-Propylthiouracil (PTU)
-Antithyroid Drugs:
-Mode of Action: Impedes the formation of the thyroid hormone
-Indications:
-Hyperthyroidism
-Adverse Effects: Liver toxicity is the most devastating effect
-Not recommended for use in pregnancy
-Drug interactions: Increases affects of anticoagulants
-Nursing Implications: Thyroid replacement Drugs:
-Teach patient to take thyroid drugs once daily in the morning
-Do not switch brands without physician approval
-Fight insurance company
-Teach patient that lifelong therapy is normally required
-Teach patients therapeutic effects take several weeks to occur
-Better tolerated with food
-Avoid eating foods high in iodine (seafood, soy sauce, tofu, and iodized
salt)
-Monitor for therapeutic response
-Monitor for adverse effects
Type 1 Diabetes Mellitus: Juvenile Diabetes
-Lack of insulin production or production of defective insulin
-Affected patients need insulin injections
-Only about 10% of diabetic patients
-Treatment: Insulin therapy learn peak times
-Function as a substitute for the endogenous hormone
-Effects are the same as normal endogenous insulin
-Restores the diabetic patient’s ability to:
-Metabolize carbohydrates, fats, and proteins
-Store glucose in the liver
-Rapid-Acting: Most rapid onset of action (5-15 minutes)- shorter duration
-Shorter duration-Insulin lispro (Humalog)
-Insulin aspart (NovoLog)
-Insulin glulisine (Apidra): Newest
-May be given SC or continuous SC infusion
-Short-Acting:
-Regular insulin (Humulin R)
-Onset 30-60 minutes
-The only insulin product that can be given by IV bolus or IV
infusion
-CAN ONLY BE GIVEN WITH NORMAL SALINE
-Check glucose every single hour for insulin drip
-Intermediate-Acting: cloudy insulin
-Isophane insulin suspension (also called NPH)
-Cloudy appearance: clear before cloudy
-Slower in onset
-More prolonged in duration than regular insulin
-Not as long as the longer acting insulin types
-Never shake cloudy insulin, always roll (causes clots)
-Long-Acting:
-Glargine (Lantus), Detemir (Levemir)
-Clear, colorless solution
-Lantus is only approved for once or twice daily dosage
-Never mix Lantus and Levemir
-Combination insulin products
-NPH 70% and regular 30%
-Humulin 70/30, Novolin 70/30, Novolog 70/30
-NPH 50% and regular insulin 50%
-Humulin 50/50
-Developed to simplify the dosing process
-Sliding scale insulin
-Short-acting or regular insulin doses adjusted according to blood glucose
test results
-Subcutaneous insulin is ordered in an amount that increases as the blood
glucose increases
-Disadvantage:
-Delays insulin administration until hyperglycemia occurs
-Results in large swings in glucose control
-Every 6 hours monitor glucose for TPN and PPN
Type 2 Diabetes Mellitus
-Most common type
-Caused by insulin resistance
-Associated with:
-Obesity
-Coronary heart disease
-Dyslipidemia (high blood cholesterol levels)
-Hypertension-Increased risk for thrombotic
-Treatment:
-Lifestyle changes: Exercise, change diet
-Oral drug therapy
-Insulin when the above no longer provide glycemic control
-Oral Antidiabetic Drugs:
-Used for type 2 diabetes
-Biguanides: Metformin (Glucophage)
-Only drug in this class
-Frist line drug that’s most commonly used for the treatment of Type II
DM
-MOA:
-Increases uptake of glucose by tissues leaving less in the
bloodstream
-Do not increase insulin secretion from the pancrease (does not
cause hypoglycemia)
-Adverse Effects:
-GI: Abdominal bloating, feeling of fullness
-May also cause metallic taste
-Lactic acidosis is rare, but can be fatal
-Contraindications:
-Renal dysfunction or failure
-Alcoholism, heart failure: increased risk of lactic acidosis
-Drug Interactions:
-Contrast media can be associated with renal problems and lactic
acidosis
-Should not be given with other drugs that cause hyperglycemia
because of risk of loss of glucose control
-Sulfonylureas: Second line treatment
-Glyburide (DiaBeta, Micronase)
-Glipizide (Glucotrol)
-May be allergic to sulfa drugs
-MOA:
-Stimulate insulin secretion from the pancrease, thus increasing
insulin levels
-Result in lower blood glucose levels
-Adverse effects;
-Contraindications:
-Hypoglycemia
-Sulfa drugs (antibiotic) allergy
-Drug interactions:
-Effects can be enhanced when taken with alcohol and some over
the counter drugs
-Thiazolidinediones
-Also known as glitazones
-End in –zone-MOA:
-Decrease insulin resistance
-Increase glucose uptake and use in muscle
-Adverse Effects:
-Moderate weight gain, edema
-Contraindications:
-Heart failure, kidney and liver disease
-Also used for patients that have a spike in their blood sugar after they eat
-Glinides:
-Increase insulin secretion from the pancreas
-Not on exam
-Injectable Antidiabetic Drugs:
-Amylin Agonists
-Suppresses glucagon secretion
-SC injection
-Can be given to type I or type II diabetics who have failed to
achieve optimal glucose control with insulin
-Simlin
-Incretin Mimetics:
-Stimulates insulin secretion
-Only available as a SC injection
-Indicated for type II DM patients unable to maintain glucose
control with other oral antidiabetics
-Should not be given in combination with insulin
-Byetta, Genuvia
Gestational Diabetes:
-Hyperglycemia that develops during pregnancy
-Insulin may or may not be required
-Usually subsides after delivery
Hypoglycemia:
-Mild cases can be treated with diet
-Higher intake of protein and lower intake of carbs to prevent rebound
postprandial hypoglycemia
-Symptoms:
-Early: Confusion, irritability, tremor, sweating
-Late: Seizures, coma and death will occur if not treated
-Sugar is less than 50
-Eat to fix
-Glucose elevating drugs
-Oral forms of concentrated glucose
-50% dextrose in water
-Glucagon:
-Natural hormone secreted by the pancreas
-SC as a quick response to severe hypoglycemia
-May induce vomiting
-Turn patient on side (they will probably vomit)-Also used for patients that have a food bolus stuck in esophagus (presses
on trachea)
Nursing Implications:
-Before giving drugs that alter glucose levels, obtain and document levels
-Assess patient’s ability to consume food
-Assess for nausea or vomiting
-Hypoglycemia may be a problem if antidiabetic drugs are given and the patient
does not eat
-Keep in mind that overall concerns for any diabetic patient increase when the patient:
-Is under stress
-Has an infection
-Has an illness or trauma
-Is pregnant or lactating
-Hemoglobin A1C will determine if patient is truly diabetic
-Thorough patient education is essential regarding:
-Diet and exercise recommendations
-Self-administration of insulin or oral drugs
-Insulin:
-Check blood glucose level before giving insulin
-Roll vials between hands instead of shaking them to mix suspensions
-Ensure correct storage of insulin vials
-ONLY USE INSULIN SYRINGES- THEY ARE ORANGE
-Draw up clear before cloudy
-Oral Antidiabetic Drugs:
-Always check blood glucose levels before giving
-Usually given 30 minutes before meals
-Alpha-glucosidase inhibitors are given with the first bite of each main meal
-Metformin is taken with meals to reduce GI effects
-Metformin will need to be discontinued if the patient is to undergo studies with
contrast dye because of the risk of developing lactic acidosis
-Check with the prescriber before administering
-Assess for signs of hypoglycemia
-If present, give oral glucose
-If unconscious, give D50W IV or glucagon SC
-Monitor blood glucose levels
-After giving glucose, give them something to eat and recheck their sugar
-Monitor for therapeutic response:
-Decrease in blood glucose levels to the level prescribed by physician
-Monitor for hypoglycemia and hyperglycemia
-Hgb A1C-lab test to best reflect the patietn’s adherence to therapy for several months
previously
Adrenal Drugs:
-Adrenal Gland:
-Portions of the adrenal gland include:
-Adrenal Medulla
-Adrenal Cortex-Each has different functions and secretes different hormones
-Adrenocortical Hormones
-Over-secretion of glucocorticoids leads to Cushing’s syndrome
-Cushing’s syndrome can result in exaggerated facial roundness, weight
gain around the midsection and upper back, thinning of your arms and
legs, and stretch marks.
-Under-secretion of glucocorticoids leads to Addison’s disease
-Addison’s syndrome leads to decreased blood sodium and glucose levels,
increased potassium levels, dehydration and weight loss.
-Drugs:
-Can be either synthetic or natural
-Many different drugs and forms
-Two types of corticosteroids
-Glucocorticoids
-Examples: (end in –sone)
-Hydrocortisone
-Cortisone
-Methylprednisolone (Solu-Medrol)
-Prednisone (Deltasone)
-Betamethasone
-MOA: Inhibit or help control inflammatory and immune
responses
-Some have mineralcorticoid activity as well
-Wide variety of indications:
-Adrenocortical deficiency
-Cerebral edema
-Collagen diseases
-Dermatologic diseases
-GI diseases
-Exacerbations of chronic respiratory illnesses, such as
asthma and COPD
-Organ transplants
-Cosontyn: Helps make a diagnosis then treated with
glucocorticosteroid
-Administration:
-Inhalation
-Nasally
-Topically
-Oral- not if you have adrenal problems
-Contraindications:
-Serious infections, including sepsis, systemic fungal
infections, and varicella
-Known diagnosis of cataracts, glaucoma, mental health
problems
-Mineralocorticoids
-Examples:-Fludrocortisone Acetate (Florinef)
-Most commonly prescribed mineralocorticoid
-Causes fluid and water retention by preventing
sodium and water from being excreted
-Treats Addison’s syndrome
-Indications:
-Treatment of adrenocortical insufficiency caused by
Addison’s disease
-Contraindications:
-Fungal infections
-Corticosteroids: Adverse Effects
-Potent effects on all body systems
-Cardiovascular
-Heart failure, cardiac edema, hypertension- all
caused by electrolyte imbalances that can occur
(hypokalemia, hypernatremia)
-CNS:
-Convulsions, mood swings, nervousness, insomnia,
“steroid psychosis”
-Integumentary:
-Fragile skin, poor wound healing
-Musculoskeletal:
-Muscle weakness, loss of muscle mass,
osteoporosis
-Other:
-Weight gain, glaucoma, cataracts
-Endocrine:
-Growth suppression, Cushing’s syndrome,
menstrual irregularities, hyperglycemia
-GI
-Peptic ulcers with possible perforation,
pancreatitis, abdominal distention
-Corticosteroids: Drug Interactions
-Loop diuretics
-Aspirin and other NSAIDs
-Antidiabetic drugs
-OTC and herbals
-Adrenal steroid inhibitors
-Examples: Aminoglutethimide (Cytadren)
-Indications:
-Treatment of Cushing’s syndrome
-Some types of cancers
-Metastatic breast cancer and Adrenal cancer. Only in oral
forms.
-Only oral form
-Nursing Implications:-Perform a physical assessment to determine baseline weight, height, intake and
output status, vital signs (especially BP), hydration status, immune status
-Obtain baseline laboratory studies
-Assess for edema and electrolyte imbalances
-Be aware that these drugs may alter serum glucose and electrolyte levels
-Systemic forms may be given by oral, IM, or IV
-Oral forms should be given with food or milk to minimize GI upset
-For topical applications, follow instructions about use and type of dressing, if
any, to apply
-Clear nasal passages before giving a nasal corticosteroid
-After using an orally inhaled corticosteroid, instruct patients to rinse their mouths
to prevent possible oral fungal infections
-Teach patients on corticosteroids to avoid contact with people with infections
-Patients should be taught to take all adrenal medications at the same time every
day
-These medications should NEVER be abruptly discontinued
Women’s Health Drugs:
-Female Reproductive System:
-Estrogens:
-Responsible for:
-Development and maintenance of the female reproductive system
-Development of female secondary sex characteristics
-Indications:
-Treatment or prevention of disorders that result from estrogen
deficiency
-Oral contraception (given with a progestin)
-Dysmenorrhea
-“Hot flashes” of menopause
-Uterine bleeding
-Osteoporosis treatment and prophylaxis
-Currently there is controversy about whetehr or not hormone
replacement therapy (HRT) is safe- Ongoing studies
-Adverse Effects:
-Thrombolytic events- most serious
-Nausea- most common
-May cause chloasma (brown spots)
-Contraindications:
-Undiagnosed abnormal vaginal bleeding
-Pregnancy
-Active thromboembolic disorder or history
-Progestins:
-Synthetic derivatives of progesterone
-Examples:
-Medroxyprogesterone (Provera, Depo-Provera)
-Etonogestrel implant (Implanon)
-Indications:-Treatment of functional uterine bleeding
-Prevention of conception
-Maybe used in combination with estrogen
-Treatment of amenorrhea
-Treatment of some cancers and endometriosis
-Alleviation of PMS syndromes
-Adverse Effects:
-Liver dysfunction
-Thrombolytic Events
-Implications: Estrogens and Progestins
-Take smallest dose needed
-Rotate sites with IM doses
-Give oral doses with meals to reduce GI problems
-DO NOT SMOKE- adds to thrombolytic events
-Increased susceptibility to sunburn may occur- advise patients to wear
sunscreen or avoid sunlight
-Instruct patients to report weight gain of 5 or more pounds in 1 week
-Advice patients to complete annual follow up exams.
-Contraceptive Drugs:
-Medications used to prevent pregnancy
-Oral medications
-Most contain estrogen-progestin combinations
-Long-acting injectable form of Medroxyprogesterone (Depo-Provera)
-Given intramuscularly
-Transdermal contraceptive patch
-Intravaginal ring
-MOA: Prevent ovulation by inhibiting the release of gonadotropins and
increasing uterine mucous viscosity
-Drug Effects:
-Improve menstrual cycle regularity
-Decrease blood loss during menstruation
-Decrease incidence of ovarian cysts and ectopic pregnancies
-Indications:
-To prevent pregnancies
-Treats endometriosis and hypermenorrhea
-Postcoital emergency contraception (72 hours after unprotected
sex, useless after egg has implanted)
-Adverse Effects:
-Drug Interactions:
-Antibiotics
-Drugs that may have reduced effectiveness if given with
oral contraceptive drugs
-Oral anticoagulants, vitamins
-Contraindications:
-Pregnancy
-Risk for or history of thromboembolic effect-Osteoporosis:
-Risk factors: age, post menopausal, Asian and Caucasian more likely
-Drug therapy:
-Calcium supplements and vitamin D
-Biphosphonates:
-Alendronate (Fosamax)
-Must sit up for 30 minutes after taking
-MOA: Work by inhibiting bone resorption, thus preventing bone
loss
-Indications:
-Adverse effects: GI upset, joint pain, esophageal burns, risk of
osteonecrosis of the jaw
-Contraindicatoins: Esophageal dysfunction
-Drug Interactions: Calcium supplements and antacids, NSAIDS
and Aspirin
-Selective estrogen receptor modifier (SERM)
-Raloxifene (Evista)
-MOA: Stimulate estrogen receptors on bone receptor
-Prevent bone loss after menopause
-Estrogen- thrombolytic effects
-SERMS:
-Calcitonin: Inhibits bone resportion to treat osteoporosis
-Miacilin: nasal spray
-No salmon allergies
-Fertility Drugs:
-Various medical techniques used to treat infertility
-Clomiphene (Clomid)
-Nonsteroidal ovulation stimulant
-Increases chance of ovulation and conception
-Also used for men with low sperm count and slow moving sperm
-Used for envitro fertilization as well
-Indications:
-Induce ovulation and spermatogenesis
-Adverse Effects:
-Tachycardia, DVT
-Nursing Implications:
-Take as ordered
-Keep a journal while on fertility drugs
-Contraindications:
-Known allergy
-Abnormal uterine bleeding
-Enlarged ovaries
-Pregnancy
-Uncontrolled thyroid function
-Liver disease
-Uterine Altering Medications:-Alter uterine contractions
-Promote labor
-Prevent start or progression of labor
-Used to reduce risk of post partum hemorrhage
-Uterine Stimulants:
-Oxytocics:
-Oxytocin (Pitocin)- Synthetic form:
-Used to induce labor at or near full-term gestation
-Enhances labor when contractions are weak and
ineffective
-IV pump, heart monitor, monitor uterine contractions
-Prevent or control postpartum uterine bleeding
-Induce labor after miscarriage
-Promote milk ejection during lactation
-Prostaglandins:
-Cause potent contraction of smooth muscle of the uterus
-Used to induce labor by softening the cervix (cervical ripening)
and enhancing uterine muscle tone
-Dinoprostone (Prostin E2)
-Cervidil: More common name of Dinoprostone
-Ergot alkaloids: Methylergonovine (Methergine)
-Increase force and frequency of uterine contractions
-Used after delivery of the infant and placenta to prevent
postpartum uterine atony and hemorrhage
-Not to hypertensive patients because it causes stroke or seizures in
patient
-Progesterone antagonist: Mifepristone (Mifeprex)
-Stimulates uterine contractions to induce abortion
-Uterine Relaxants:
-Tocolytics: Used to stop labor that beings before term to prevent
premature birth. (after 20th week of gestation)
-Terbutaline (Brethine)
-Cause relaxation of the smooth muscle of the uterus, thus stopping
premature contractions
-“Off-label” use, usually used in respiratory
-Magnesium sulfate IV also used to stop labor
-Indomethacin (NSAID)
-Calcium Gluconate MUST be available in case of magnesium
toxicity
-Adverse Effects:
-Palpitations, tachycardia, hypertension, tremors, anxiety
-Contraindications:
-Cardiac dysrhythmias, maternal cardiac disease, pregnancy before
20 weeks
-Nursing Implications:-Before giving any uterine stimulants, assess the mother’s vital signs and
fetal heart rate
-Uterine relaxants are used when premature labor occurs beteween the 20th
and 37th weeks of gestation
-Follow specific administration guidelines carefully for IV administration
of uterine relaxants or stimulants
-Monitor patient’s vital signs and fetal condition during therapy
Men’s Health Drugs:
-Androgens:
-Testosterone: A type of androgen
-Several synthetic derivatives of testosterone
-Transdermal forms available (best topically as a patch)
-Anabolic steroids: Derivative of testosterone
-Sometimes used for treatment of anemia and breast cancer
-Great potential for misuse by athletes (esp. weight lifters and body
builders)
-Primary use: Replacement therapy (other uses vary with specific drug)
-Mechanism of Action: Similar to body’s endogenous androgens
-Stimulation of normal growth and development of male sex organs
-Development and maintenance of male secondary sex characteristics
-Includes the growth and maintenance of the prostate
-Adverse Effects:
-Fluid retention
-Most devastating: Peliosis of liver, hepatic effects
-Drug Interactions:
-Anticoagulants, oral hypoglycemic
-Androgen Inhibitors
-5-Alpha-reductase inhibitors:
-Block effects of endogenous androgens
-Used to treat benign prostatic hyperplasia (BPH)
-Results in alleviation of symptoms of BPH
-May be used for treatment of male-pattern baldness. May cause
PSA concentractions to decrease, loss of libido, loss of erection,
ejaculatory dysfunction
-Pregnant women: WEAR GLOVES
-Example:
-Finasteride (Proscar)
-Alpha 1- adrenergic blockers
-Used for symptomatic relief of obstruction caused by BPH
-Adverse Effects
-Androgen receptor blockers
-GnRH analogs:
-Used to treat prostate cancer
Drugs that block the effects of natural occurring endogenous
androgens in the body
-Drugs for Erectile Dysfunction:-Sildenafil (Viagra)
-First oral drug for ED
-Adverse Effects:
-Headache, flushing, chest pain, hypotension
-Priapism
-Unexplained visual loss
-Others:
-Tadalafil (Cialis)
-Vardenafil (Levitra)
-Alprostadil (Carverject): Injected directly into erectile tissue or
suppository form into the urethra
-Nursing Implications:
-Assessment should include complete history, including medication history,
urinary elimination problems, potential contraindications
-Obtain baseline vital signs
-Assess renal and liver function
-Assess PSA level and perform digital rectal exam (DRE) before beginning any
drugs for treatment of prostate disease
-IM testosterone should be given deeply
-Pregnant women should not handle crushed or broken tablets of 5 alpha
reductase inhibitors
-Educate patients on proper administration techniques for each drug
-Monitor for therapeutic responses
-Monitor for adverse effects
[Show More]