PCCN Exam Prep Questions with Correct Answers, Graded A+, All Rated 100%
Document Content and Description Below
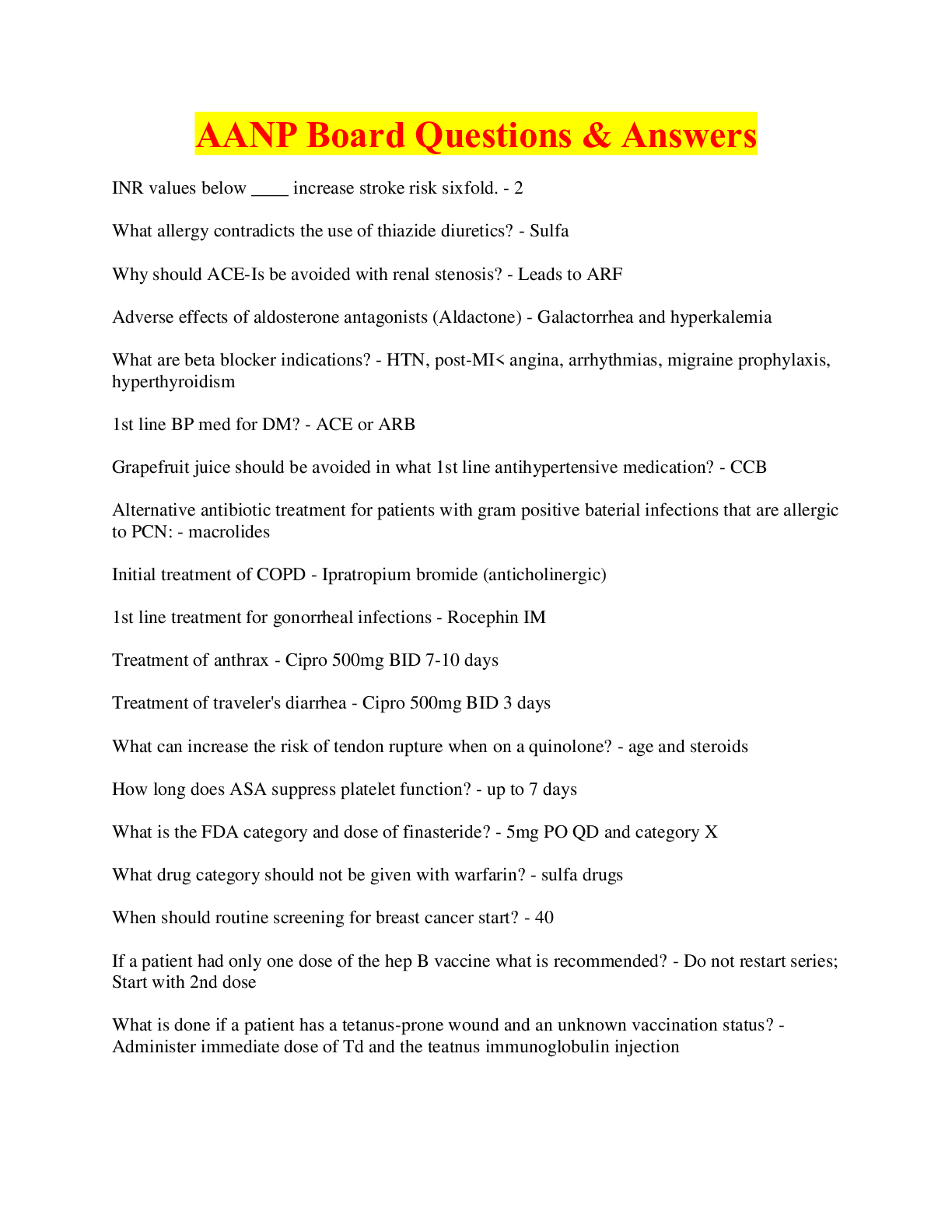
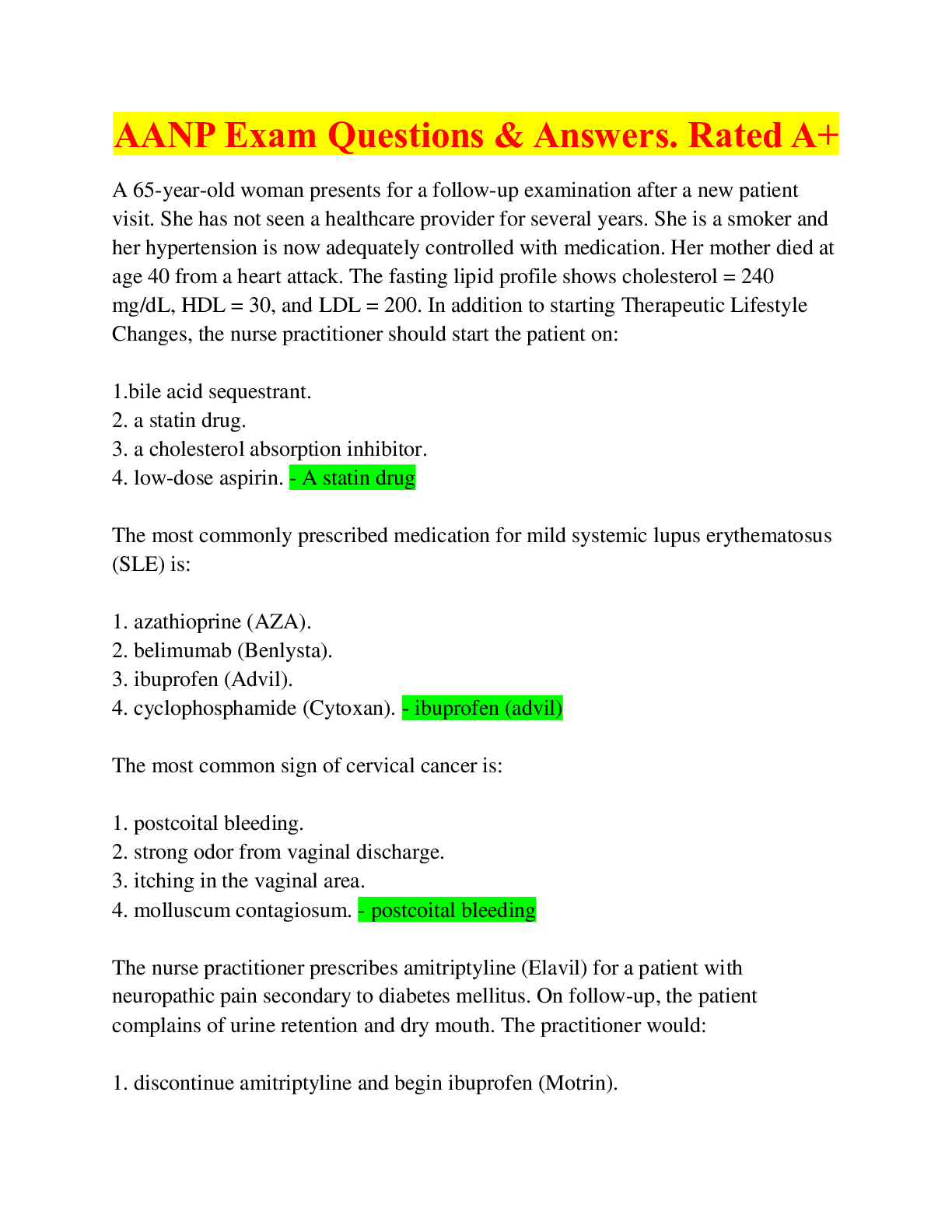
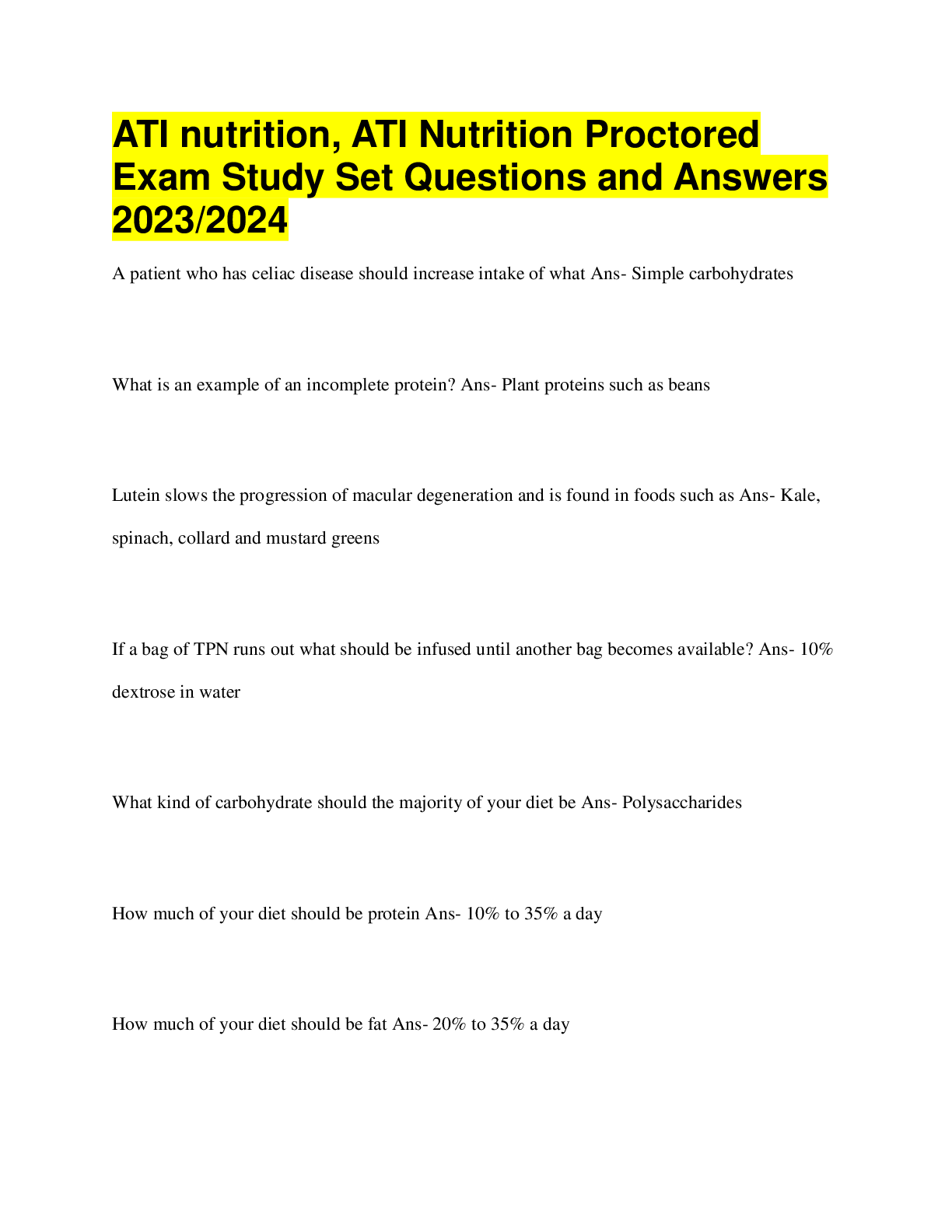
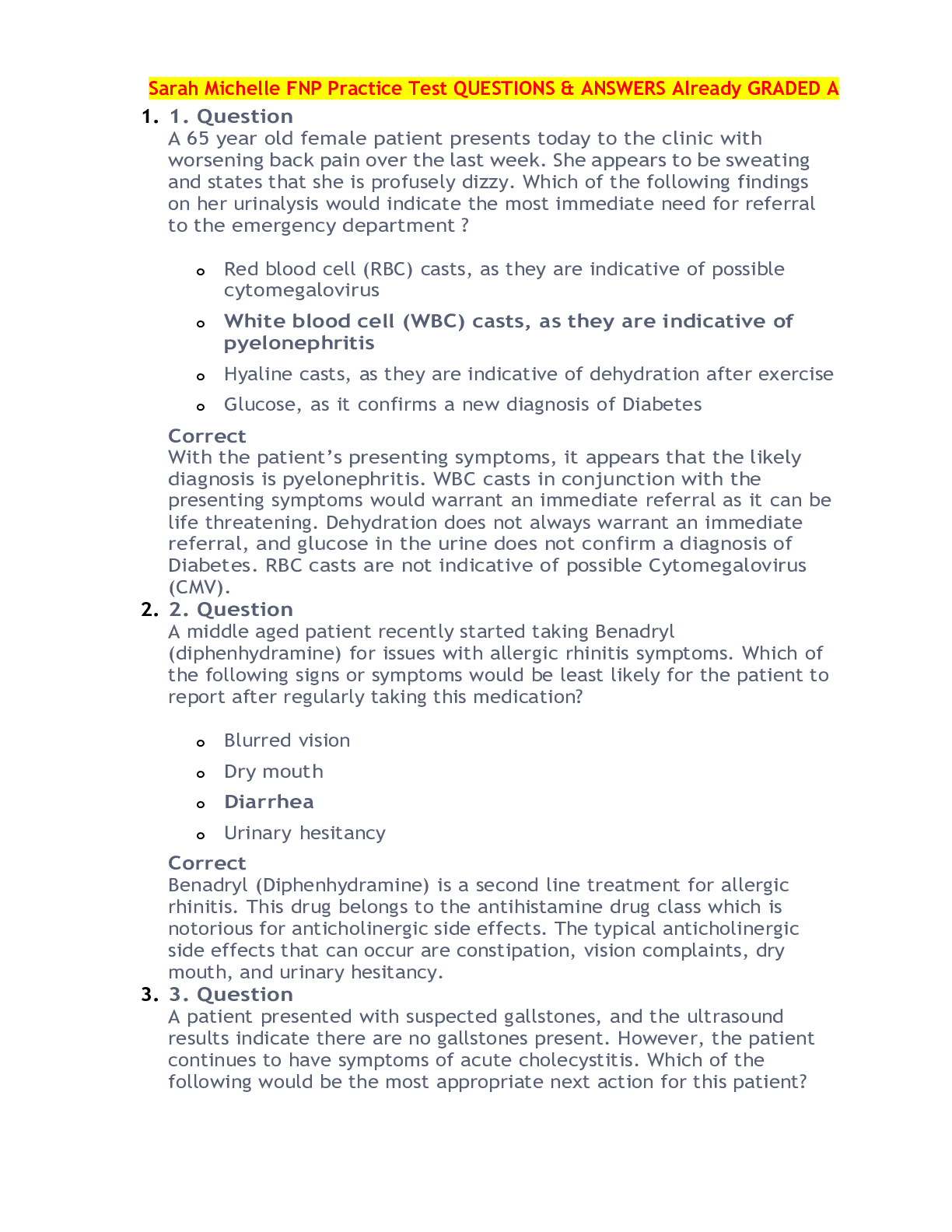
PCCN Exam Prep Questions with Correct Answers, Graded A+, All Rated 100%-Discharge education for a patient after a percutaneous coronary intervention (PCI) with transradial access should include: a. ... "Do not play tennis for 1 week." b. "Do not take a tub bath for 1 week." c. "It is normal to feel some numbness and tingling in the hand." d. "It is normal to feel some intermittent chest pain for about a week." - a Which of the following findings would occur in dilated cardiomyopathy? A. Murmur of mitral regurgitation B. Hypertension C. Elevated sedimentation rate D. Syncope - a (Mitral regurgitation is often present in dilated cardiomyopathy as a result of ventricular dilation and stretching of the mitral valve ring. Syncope is seen in hypertrophic cardiomyopathy. Elevated sedimentation rate is associated with inflammatory response and may be seen in restrictive cardiomyopathy because it frequently is associated with connective tissue disorders. Hypotension rather than hypertension may be seen in dilated cardiomyopathy.) (Remember that dilated cardiomyopathy is like heart failure except that heart failure results from some other condition (e.g., hypertension) and cardiomyopathy is a primary muscle disease. Mitral regurgitation also occurs in left ventricular failure as a result of stretching of the mitral valve ring. Choose option a.) A patient has just returned from aortofemoral bypass grafting. He has bilateral audible pulses. How is the ankle-brachial index (ABI) calculated? A. Divide the brachial pressure by the ankle pressure on the opposite side. B. Divide the ankle pressure by the brachial pressure on the opposite side. C. Divide the brachial pressure by the ankle pressure on the same side. D. Divide the ankle pressure by the brachial pressure on the same side. - D (ABI is ankle-brachial index, or ankle artery pressure divided by brachial artery pressure. The pressure at the ankle normally is higher than the pressure at the brachial artery, and the normal ABI is 1 or greater. This measurement is more quantitative than the presence or absence of audible Doppler pulses. If an occlusion is developing, the ankle artery pressure (measured with a blood pressure cuff and a Doppler stethoscope) will decrease and the calculated ABI will decrease long before the pulses are no longer audible.) (Consider that you are looking for obstruction downstream, so compare the same leg and divide the ankle artery pressure (normally higher) by the brachial artery pressure.) A patient with a recent history of an inferior myocardial infarction starts to complain of severe dyspnea. Physical assessment reveals a loud, blowing holosystolic murmur that is loudest at the apex and radiates to the axilla. Crackles are audible throughout the lung fields, and pulse oximetry reveals hypoxemia. What is the most likely cause of the patient's deterioration? A. Ruptured ventricular septum B. Acute left ventricular failure C. Reinfarction D. Ruptured papillary muscle - d (This question describes a mitral regurgitation murmur. In a patient with acute myocardial infarction, this is the result of ischemia or rupture of the papillary muscle. This occurs most often with inferior myocardial infarction (MI) affecting the posterior leaflet of the mitral valve and during the healing process. Rupture of the ventricular septum occurs more in anteroseptal MI, the murmur is at the lower left sternal border, and the clinical presentation is a shock state. The mitral regurgitation murmur that occurs in left ventricular failure because of stretching of the mitral valve is not typically this loud, and the symptoms of left ventricular failure are usually early post-MI. There is no new pain, so reinfarction or extension is unlikely.) (Ruptured papillary muscle and left ventricular failure are likely to have this clinical presentation of pulmonary edema, but only ruptured papillary muscle would cause a loud murmur. Time frame is also helpful in the differentiation because ruptured papillary muscle would be later than acute left ventricular failure as a result of MI.) A patient with heart failure caused by diastolic dysfunction is prescribed carvedilol (Coreg). What type of drug is carvedilol? A. Calcium channel blocker B. Angiotensin-converting enzyme inhibitor C. Alpha- and noncardioselective beta-blocker D. Cardioselective beta-blocker - c (Carvedilol (Coreg) is an alpha- and noncardioselective beta-blocker. Carvedilol is like phentolamine (Regitine) plus propranolol (Inderal). The drug is used for Class II or III heart failure.) A patient becomes apneic and pulseless. Cardiopulmonary resuscitation (CPR) has been initiated, and the monitor shows asystole in two leads. Which of the following drugs would be used initially? A. Calcium gluconate B. Atropine C. Epinephrine D. Amiodarone (Cordarone) - c (After CPR is initiated and an intravenous access is established, epinephrine should be given. Calcium was used in the past in asystole but is used today only for hypocalcemia, calcium channel blocker toxicity, hyperkalemia, and hypermagnesemia. Atropine is no longer recommended for asystole. Amiodarone is not indicated in asystole because asystole is the absolute absence of irritability.) (Remember that in any pulseless situation, epinephrine is the number 1 drug.) A patient continues to have severe chest pain after 25 mg of IV morphine over the past hour. The blood pressure in the one arm is significantly lower than in the other arm. The femoral pulses are faint with mottling of the feet bilaterally. Based on these findings, what test should be expedited for completion? A. Cardiac isoenzyme profile B. Ventilation/perfusion scan C. Magnetic resonance imaging D. Chest x-ray film - d (The first diagnostic test should be a chest x-ray film for the probable diagnosis of dissecting aortic aneurysm. The chest x-ray film would reveal a widening mediastinum. An additional, more indicative finding would be calcified aortic knob with extension of the aortic wall.) Which of the following laboratory profiles would be expected in a patient with a history of alcoholism and cirrhosis of the liver? A. Prolonged activated partial thromboplastin time (aPTT), decreased albumin, hypokalemia B. Decreased alanine transaminase (ALT), decreased transferrin, hyperkalemia C. Elevated carcinoembryonic antigen (CEA), decreased aspartate transaminase (AST), hyponatremia D. Decreased bilirubin, decreased lactate dehydrogenase (LDH), hypernatremia - a (In liver disease, the prothrombin time and aPTT are prolonged, albumin and transferrin levels are low (liver cannot convert amino acids to plasma proteins), liver enzymes (ALT, AST, LDH) are elevated, bilirubin levels are elevated, and potassium levels are low. CEA is a cancer marker and would not be abnormal is this patient.) (Always start with what you know. If you remember that patients with liver disease have coagulopathies, choose option a.) A patient with renal failure has hemoglobin of 7 g/dL. He asks why the renal failure has caused "low blood." Which of the following responses would best explain the occurrence of anemia in this patient? A. "Renal failure causes platelets in your blood not to work well, and you are bleeding internally." B. "Ammonia that builds up in your blood suppresses your bone marrow." C. "Your kidney cannot make erythropoietin, a hormone that stimulates production of red blood cells." D. "Toxins that build up in your blood destroy red blood cells." - c (Erythropoietin is a hormone that the kidney in failure no longer produces. Erythropoietin normally stimulates production and release of red blood cells from the bone marrow. The explanation should be as accurate and as simple as possible.) When caring for a patient with a chest tube, which of the following is appropriate? A. Place the drainage unit at the level of the chest. B. Coil the tubing loosely on the bed. C. Ensure continuous bubbling in the water-seal chamber. D. Milk or strip the chest tubes every hour. - b (The chest tube drainage system should be placed below the level of the chest. Continuous bubbling in the water-seal chamber indicates air leak. Milking and stripping of the tube should never be done routinely because they are associated with negative pressures of 100 to 400 cm H2O on the pleural space. Excess tubing should be coiled on the bed because dependent loops are associated with increased lung pressures and decreased drainage.) [Show More]
Last updated: 11 months ago
Preview 5 out of 67 pages

Loading document previews ...
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
BUNDLE: Progressive Care Certified Nurse (PCCN) Exam TESTBANK, PCCN Actual Exam, Exam Prep, PCCN Exam 1, PCCN Final Exam, Final Exam Review, PCCN Practice Exam Notes 2025 Answered & Adult CCRN/PCCN Certification Practice Test Exam Questions & Answers, ALL RATED 100%
BUNDLE: Progressive Care Certified Nurse (PCCN) Exam TESTBANK, PCCN Actual Exam, Exam Prep, PCCN Exam 1, PCCN Final Exam, Final Exam Review, PCCN Practice Exam Notes 2025 Answered & Adult CCRN/PCCN Ce...
By PROF 11 months ago
$53.5
8
Reviews( 0 )
$18.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 02, 2025
Number of pages
67
Written in
All
Additional information
This document has been written for:
Uploaded
Jan 02, 2025
Downloads
0
Views
42