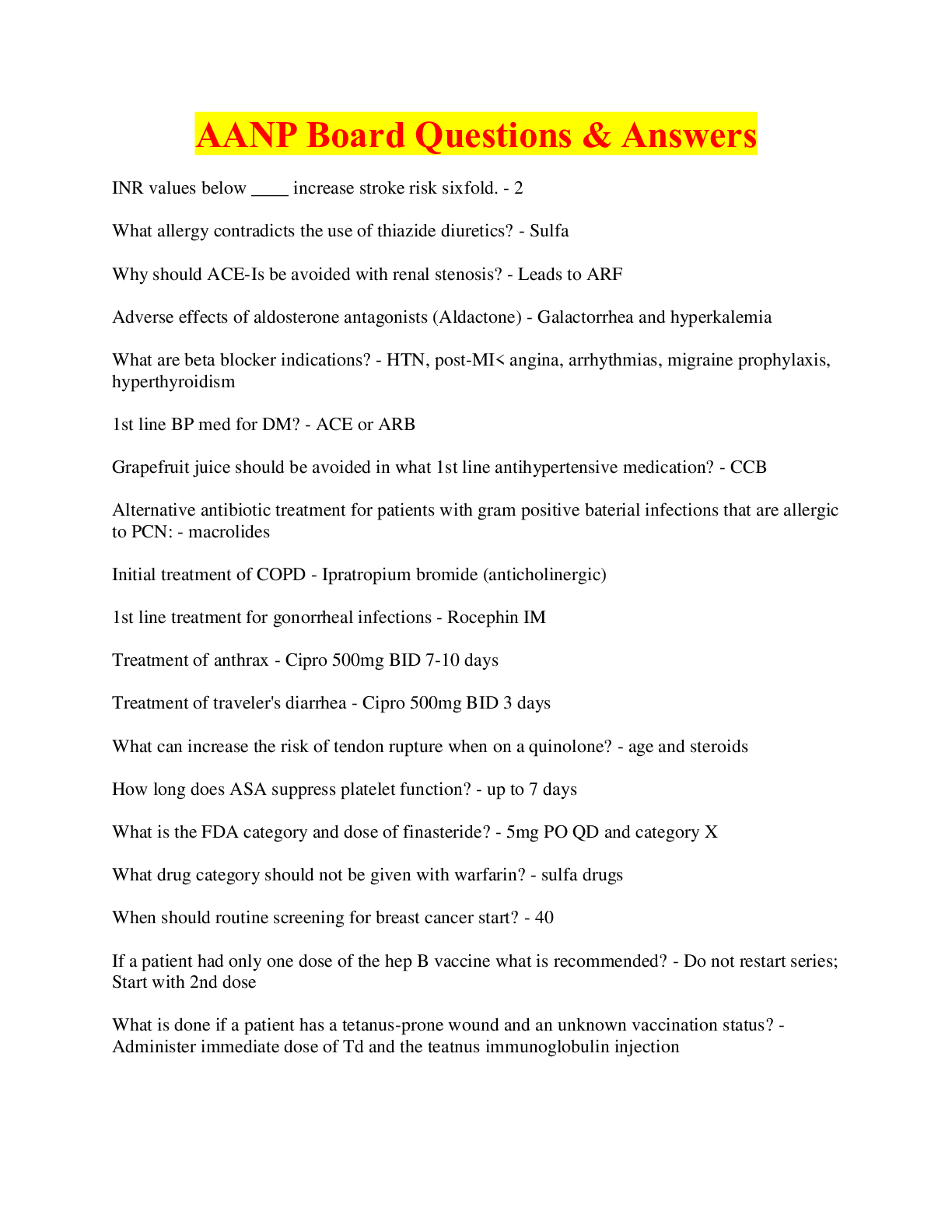
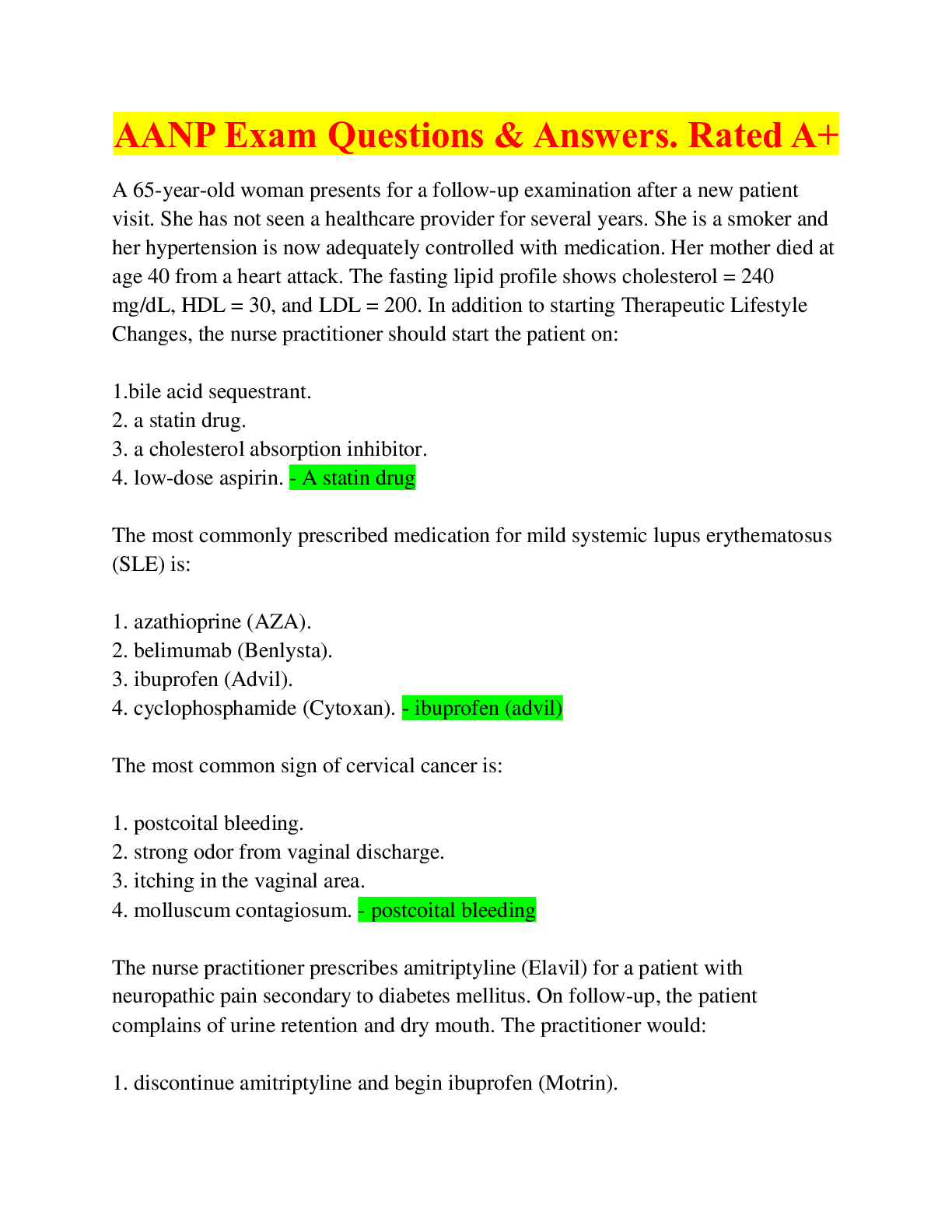
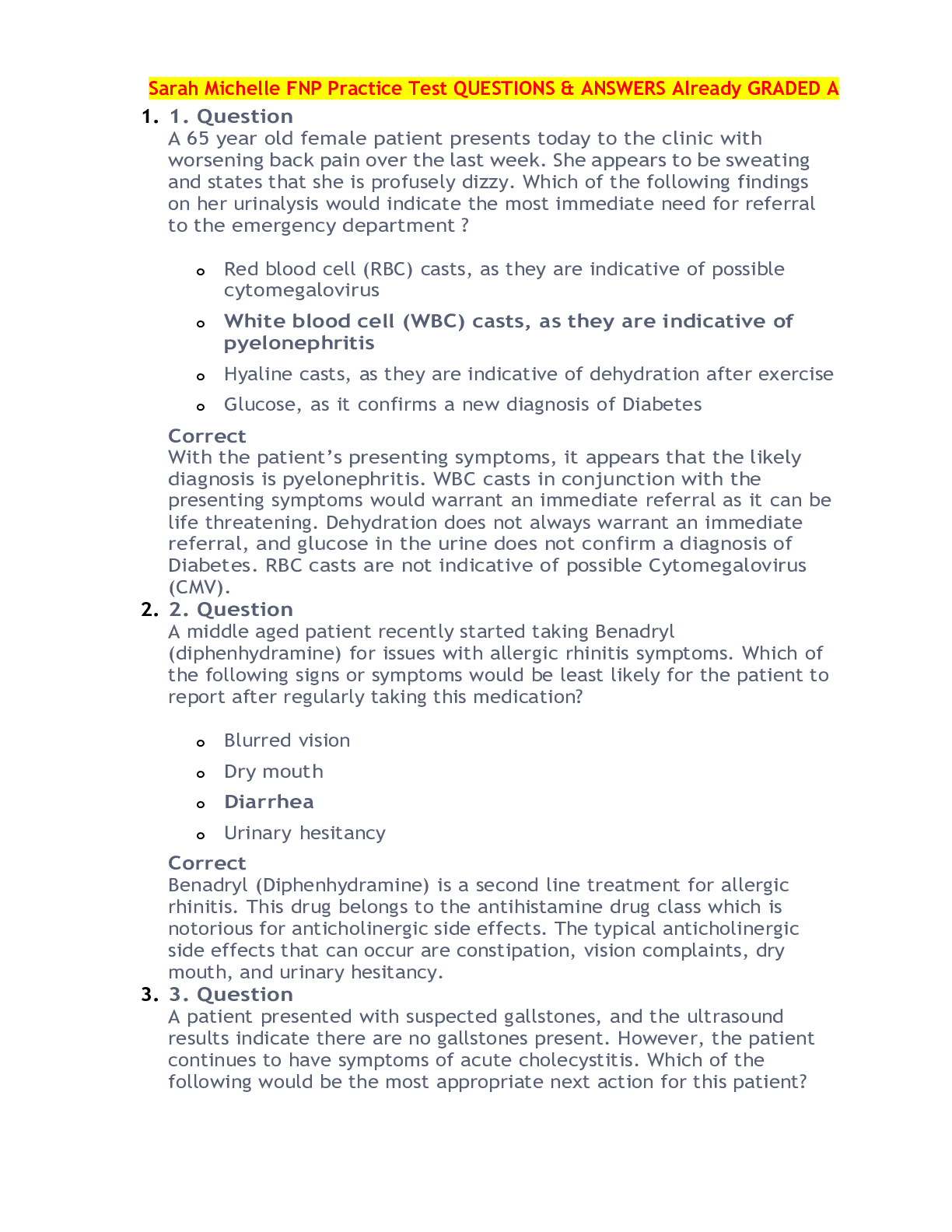
*NURSING > EXAM > PCCN Actual Final Exam Questions & Answers, All Answers Explained, Rated 100% (All)
PCCN Actual Final Exam Questions & Answers, All Answers Explained, Rated 100%
Document Content and Description Below
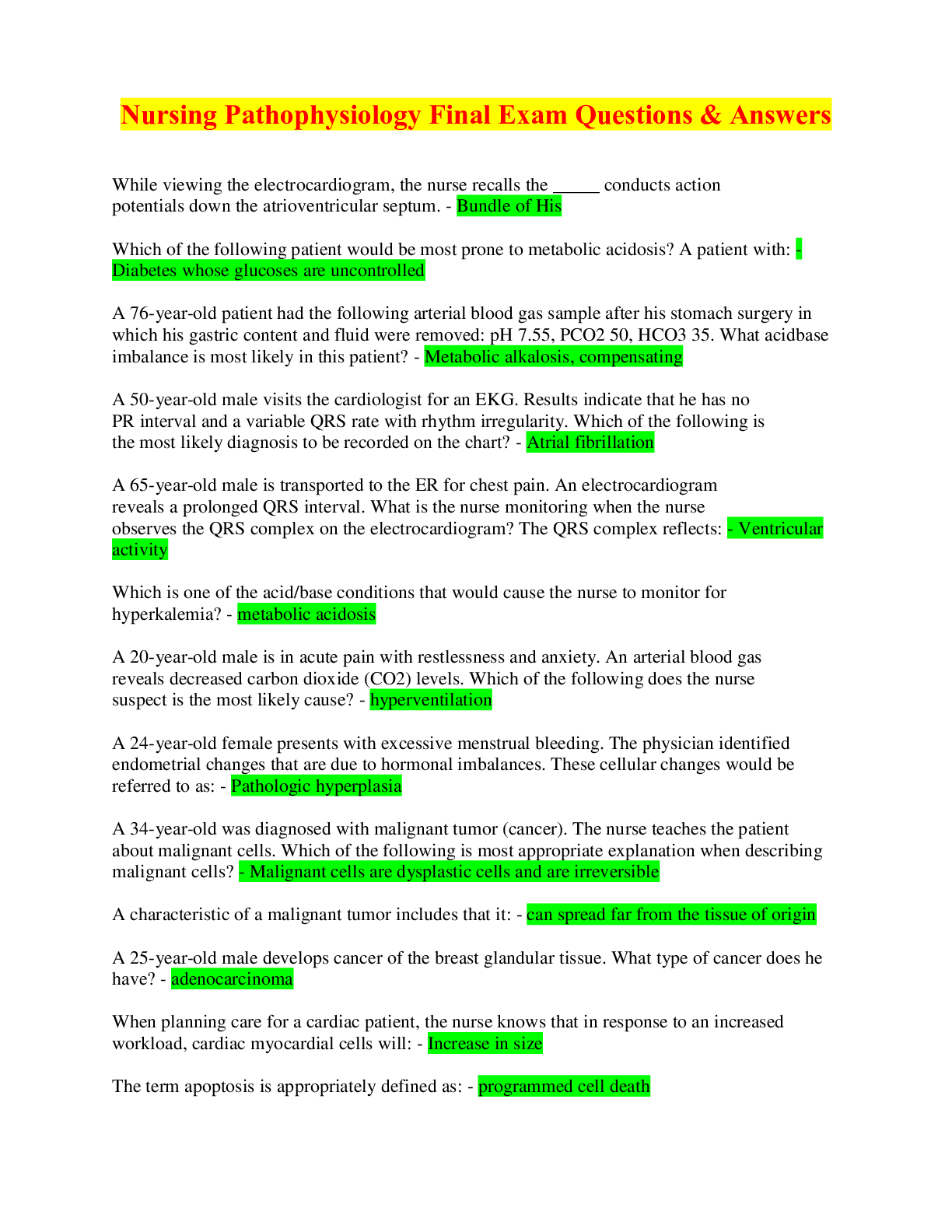
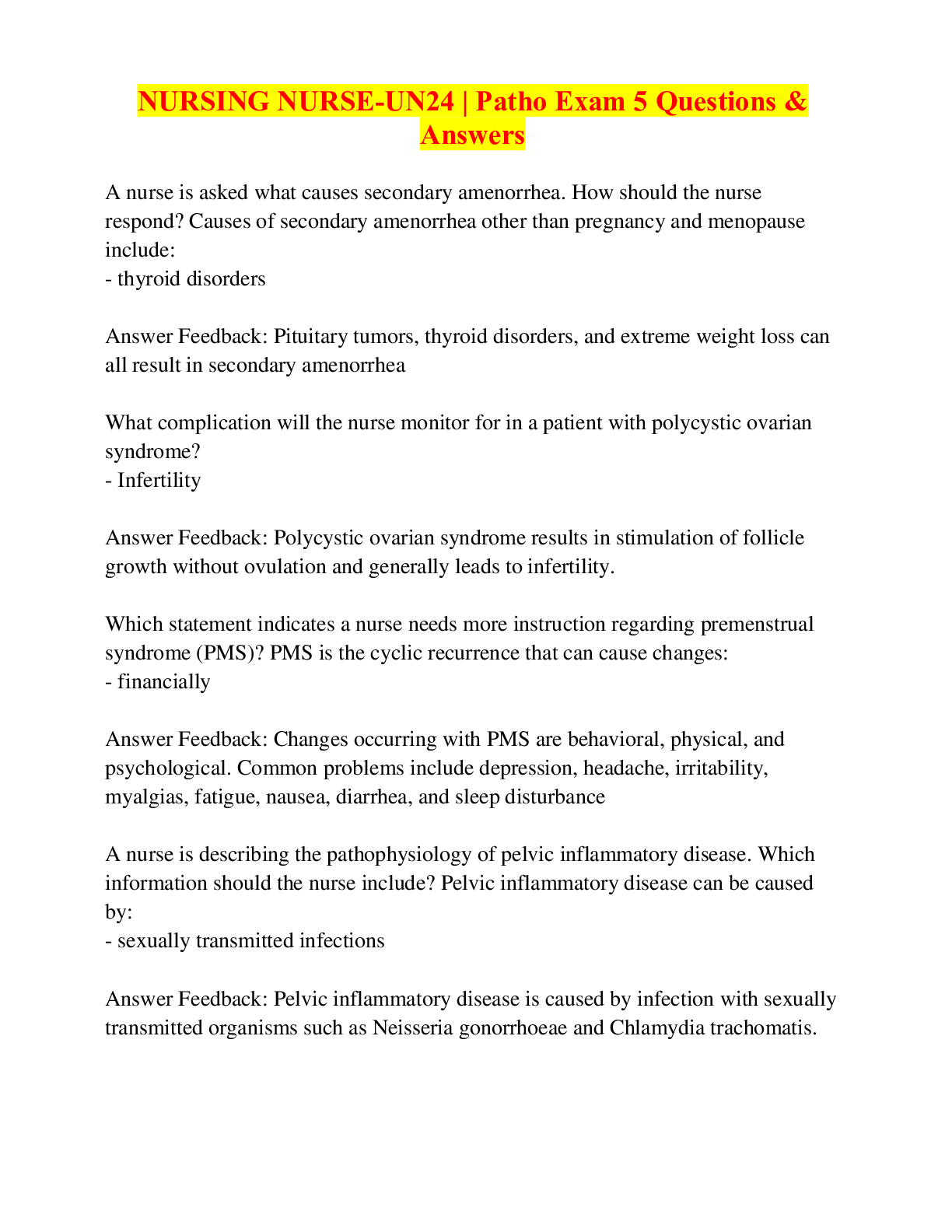
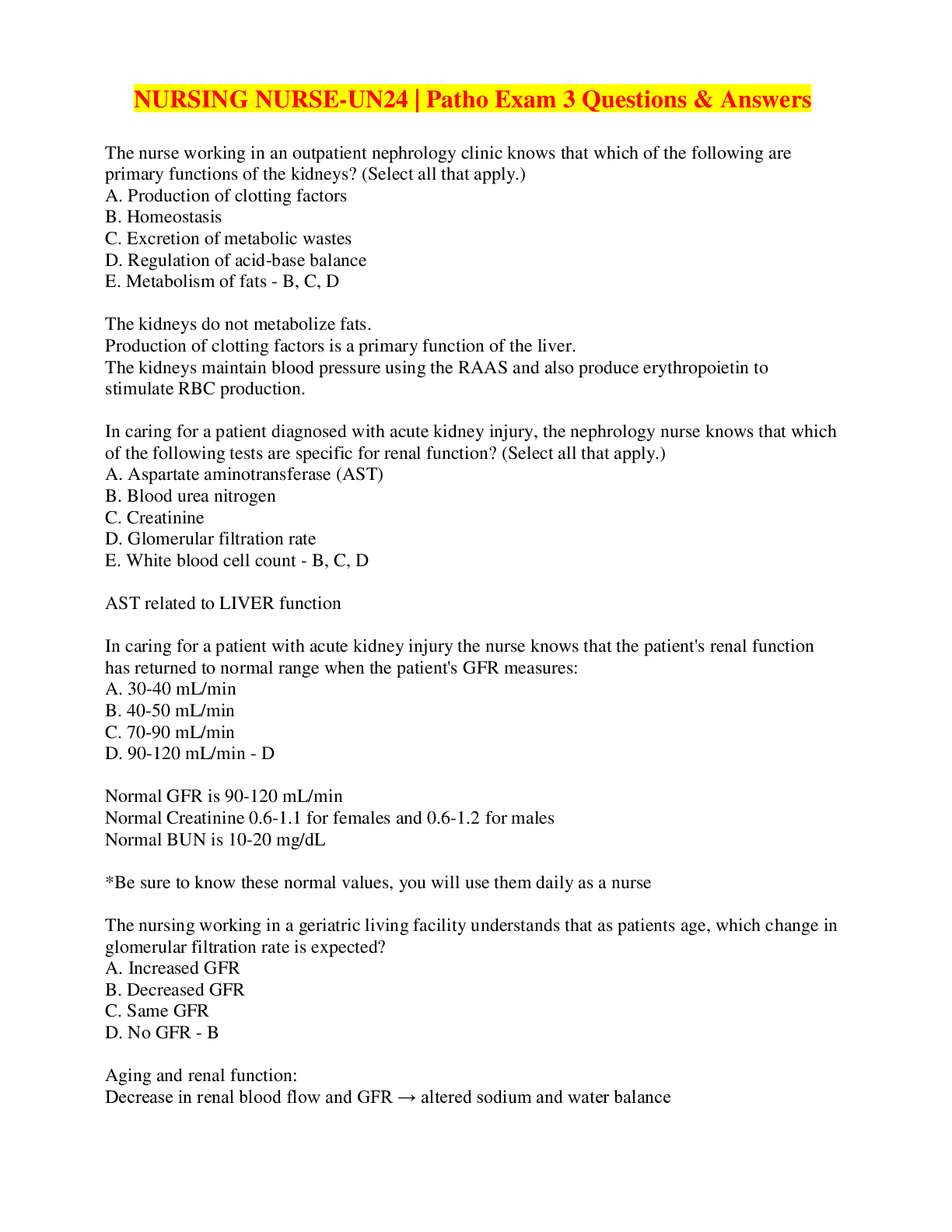
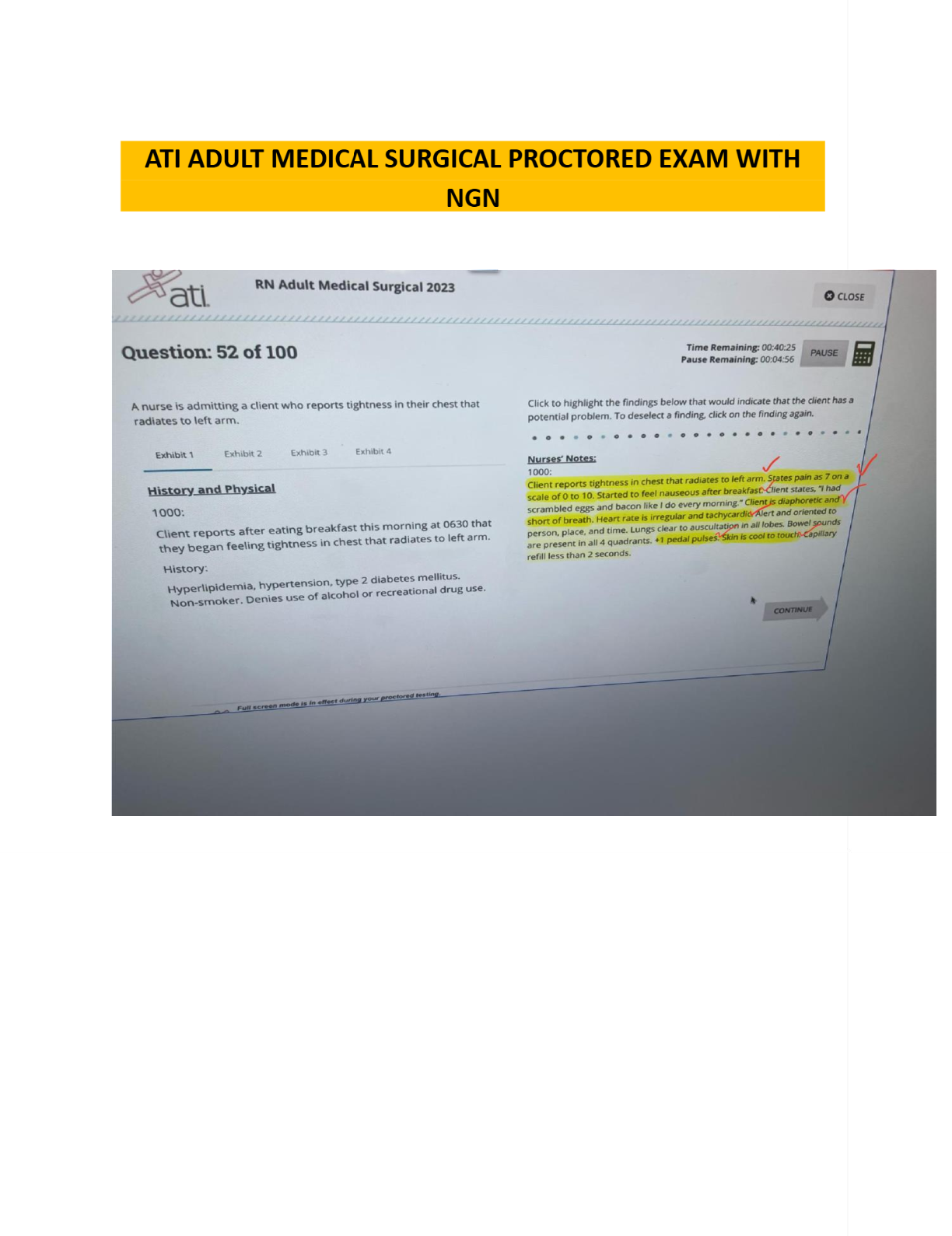
PCCN Actual Final Exam Questions & Answers, All Answers Explained, Rated 100%-A 45-year old woman is admitted with type 1 diabetic mellitus. She is hyperventilating, has signs of dehydration (increase ... d urine output and increased thirst), and is tachycardic. Initial treatment would include: A. Diazoxide (Hyperstat) to inhibit the release of insulin B. glucose for hypoglycemia C. insulin therapy for ketoacidosis, fluid and electrolyte replacement D. intravenous fluids for dehydration and glucose for hypoglycemia - C. insulin therapy for ketoacidosis, fluid and electrolyte replacement The patient is exhibiting the signs and symptoms of diabetic ketoacidosis (DKA). Signs of dehydration, such as polydipsia and polyphagia, are due to large urine output, increased thirst is secondary to dehydration and tachycardia is due to sympathetic nervous system stimulation from an increased glucose level and ketosis. Initial treatment would include insulin therapy, re-hydration with fluids and electrolyte replacement. Diazoxide would not be used since it inhibits insulin release (this patient requires insulin to lower glucose). The patient is not hypoglycemia. Signs and symptoms of hypoglycemia are similar; tachycardia, change in behavior (irritability) or level of consciousness, sweating and shaking. A 45-year-old female with history of bipolar disorder is one-day postoperative following abdominal surgery. The patient slept only one or two hours during the night and is speaking rapidly, throwing her belongings at the nurses and insists she is going to leave the hospital. The nurse should: A. Notify the mental health crisis team B. Notify social services C. Notify the nursing supervisor D. Notify the patient's husband - A. Notify the mental health crisis team In many hospitals, this can be the rapid response team. Not all hospitals have access to mental health professionals so the rapid response team answers these calls. The mental health crisis team is comprised of mental health professionals who can assess the mental status of the patients as well as the medical-surgical assessment. After the complete assessment is made, the decision of how to treat this possible exacerbation of her bipolar disorder may be made. The patient is at risk for hurting herself and others and may need continuing assessment of mental and surgical status beyond the rapid response team. Decisions will be made with the attending physician. Social services may help with placement, but not during an acute situation. The nursing supervisor may be notified as the rapid response team is notified; this is a great strategy; however, the supervisor may not have the ability to assess this complex patient. The supervisor is more able to delegate care and request more help to the area if needed. The patient's husband will need to be called after the immediate assessment is made. A 55 year old male postoperative patient is demonstrating signs of pain; tachycardia, hypertension, abdominal guarding and increased respiratory rate. The patient refuses pain medication because he believes he will become addicted to the narcotics. What is the nurse's best response? A. Acknowledge that the patient is entitled to refuse pain medications B. Tell the patient that opioids have a low addiction rate when used for postoperative pain while in the hospital C. Admire the patient's stoicism D. Acknowledge opioid addiction potential, and offer a back rub - B. Tell the patient that opioids have a low addiction rate when used for postoperative pain while in the hospital Many people are concerned about addiction rates of narcotics; however, the use of narcotics for postoperative pain while in the hospital has a very low addiction rate. The risk for abuse increases when patients go home with narcotics. Explaining to the patient that limited use in the hospital will increase his recovery and reduce inflammation is the correct response. Any patient may refuse medications after an explanation of the facts are given. A back rub or alternative care is a way to treat the patient if they absolutely refuse medications; however, the best answer is to correct the patient's misinformation about the use of narcotics during the immediate postoperative period. A 55-year old male is admitted from the ICU after an acute Type III aortic dissection. Treatment plan includes blood pressure control. What medications would the nurse anticipate in this patient? A. digoxin (Lanoxin) and furosemide (Lasix) B. metoprolol (Lopressor) and lisinopril (Prinivil) C. furosemide and spironolactone (Aldactone) D. bumetanide (Bumex) and amlodipine (Norvasc) - B. metoprolol (Lopressor) and lisinopril (Prinivil) The blood pressure control of this patient is the most important treatment in his care. The two most common drugs for the treatment of an aortic dissection are a beta blocker and ACE inhibitor. Diuretics may be added for more control of blood pressure, but are not first-line drugs. Digoxin is not required for this patient. A 68 year old male is 4 hours postoperative after percutaneous transluminal coronary angioplasty and stent placement and complains of flank pain. He is restless, tachycardic, hypotensive, and his hemoglobin and hematocrit levels (H+H) have dropped. Which of the following nursing actions is correct? A. Keep the head of the bed flat and apply pressure at the sheath site to stop bleeding. B. Notify a physician immediately and anticipate ultrasound-guided compression and possible surgery to stop the bleeding. C. Notify a physician immediately, and anticipate anticoagulation or thrombolytic therapy. D. Notify a physician immediately, stop anticoagulation therapy, and anticipate the need for intravenous fluid and/or blood - D. Notify a physician immediately, stop anticoagulation therapy, and anticipate the need for intravenous fluid and/or blood This angioplasty and stent patient is probably experiencing a retroperitoneal arterial bleed into the flank area, requiring cessation of anticoagulants and preparation for fluid administration and/or blood. Lying the patient flat and applying pressure to the sheath site treats the bleeding or hematoma at the sheath site. Ultrasound-guided compression and surgery is indicated if a pulsatile mass or bruit occurs near the insertion site, indicating pseudoaneurysm or arteriovenous fistula formation. Anticoagulation therapy is indicated for decreased circulation in extrremity related to thrombus or embolus. [Show More]
Last updated: 11 months ago
Preview 5 out of 71 pages

Loading document previews ...
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Also available in bundle (1)
Click Below to Access Bundle(s)
BUNDLE: Progressive Care Certified Nurse (PCCN) Exam TESTBANK, PCCN Actual Exam, Exam Prep, PCCN Exam 1, PCCN Final Exam, Final Exam Review, PCCN Practice Exam Notes 2025 Answered & Adult CCRN/PCCN Certification Practice Test Exam Questions & Answers, ALL RATED 100%
BUNDLE: Progressive Care Certified Nurse (PCCN) Exam TESTBANK, PCCN Actual Exam, Exam Prep, PCCN Exam 1, PCCN Final Exam, Final Exam Review, PCCN Practice Exam Notes 2025 Answered & Adult CCRN/PCCN Ce...
By PROF 11 months ago
$53.5
8
Reviews( 0 )
$17.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 02, 2025
Number of pages
71
Written in
All
Additional information
This document has been written for:
Uploaded
Jan 02, 2025
Downloads
0
Views
41