*NURSING > SOAP NOTE > NR 509 SOAP Note week 3.docx[CONTAINS SUBJECTIVE INFORMATIONS:HISTORY OF PRESENT ILL NESS[HPI] CURR (All)
NR 509 SOAP Note week 3.docx[CONTAINS SUBJECTIVE INFORMATIONS:HISTORY OF PRESENT ILL NESS[HPI] CURRENT MEDICATION ] GRADED A+]
Document Content and Description Below
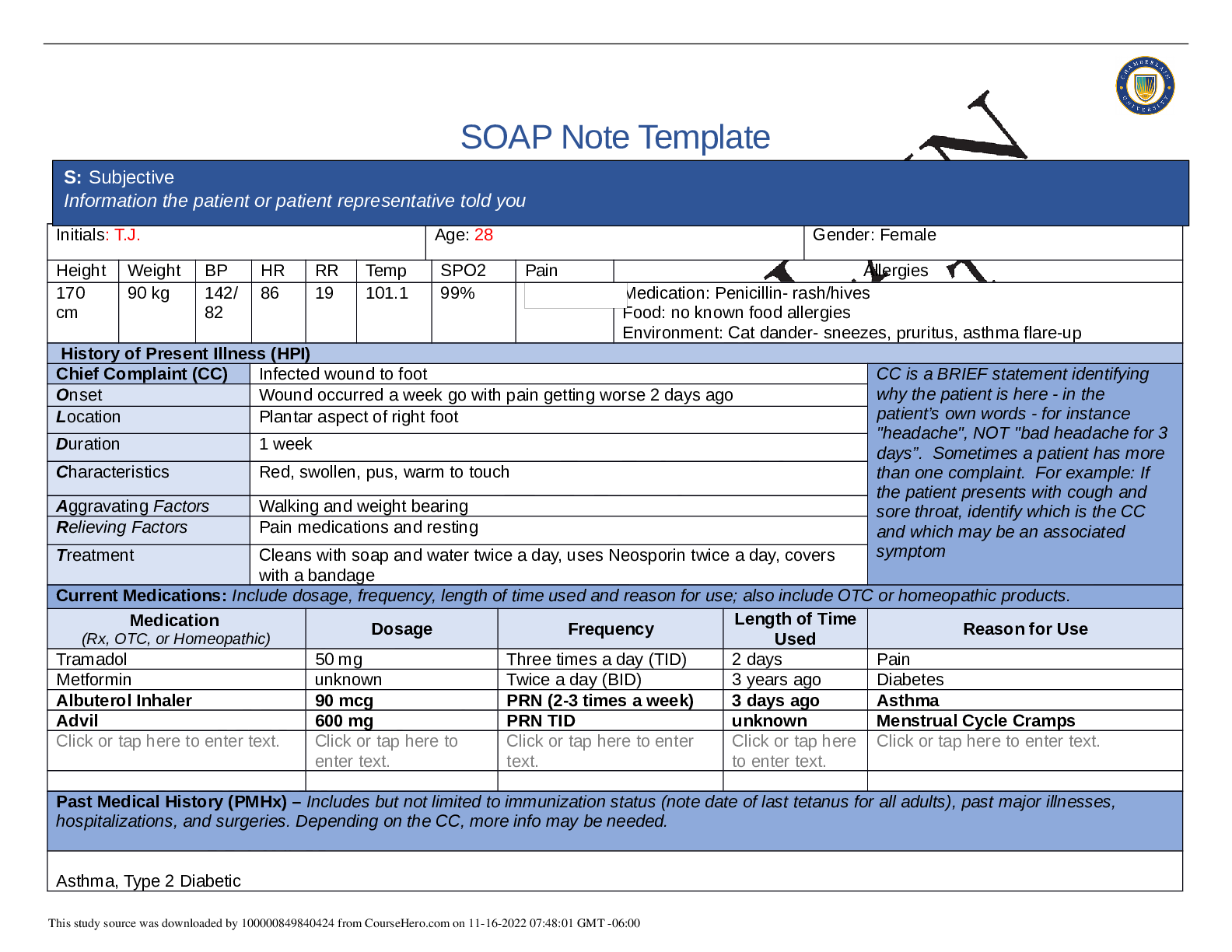
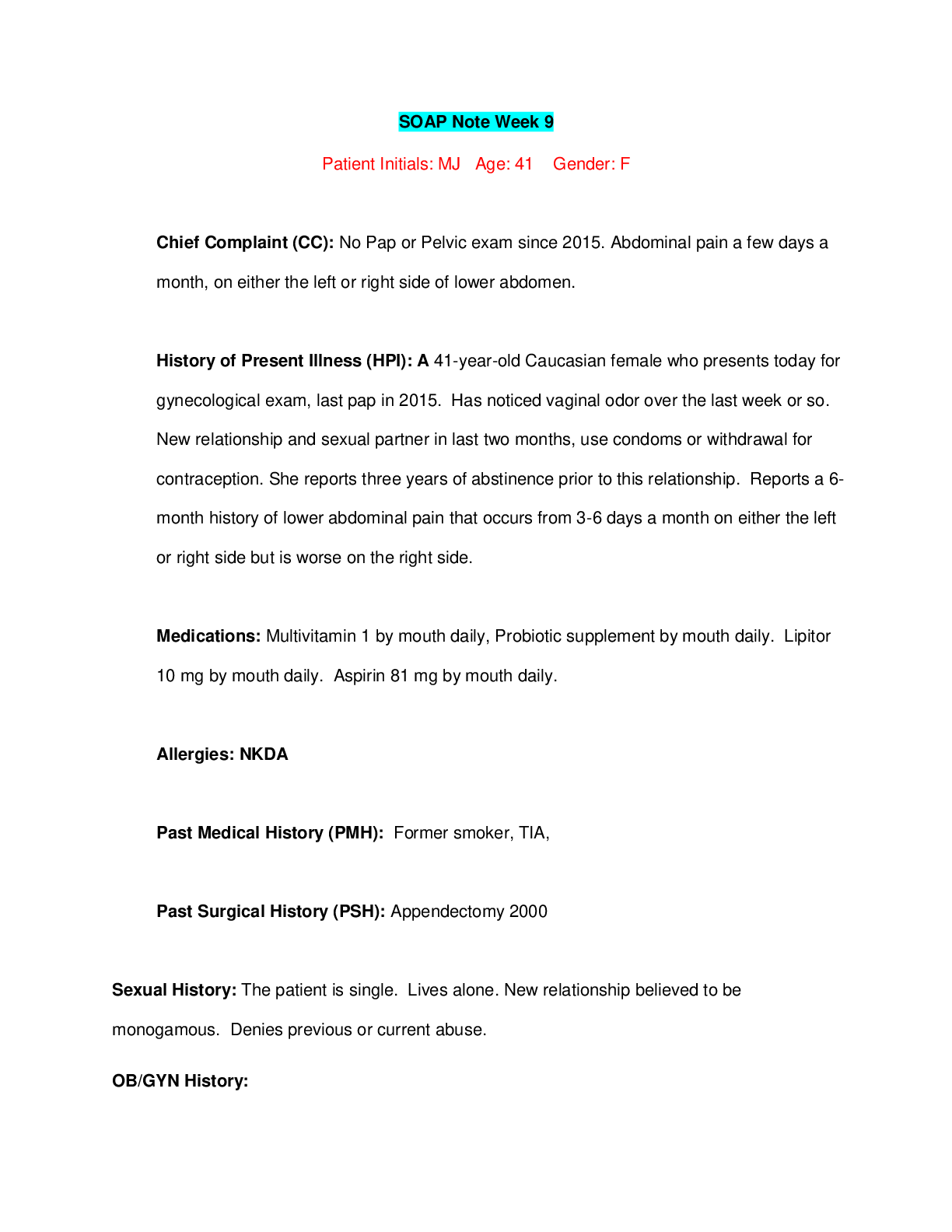
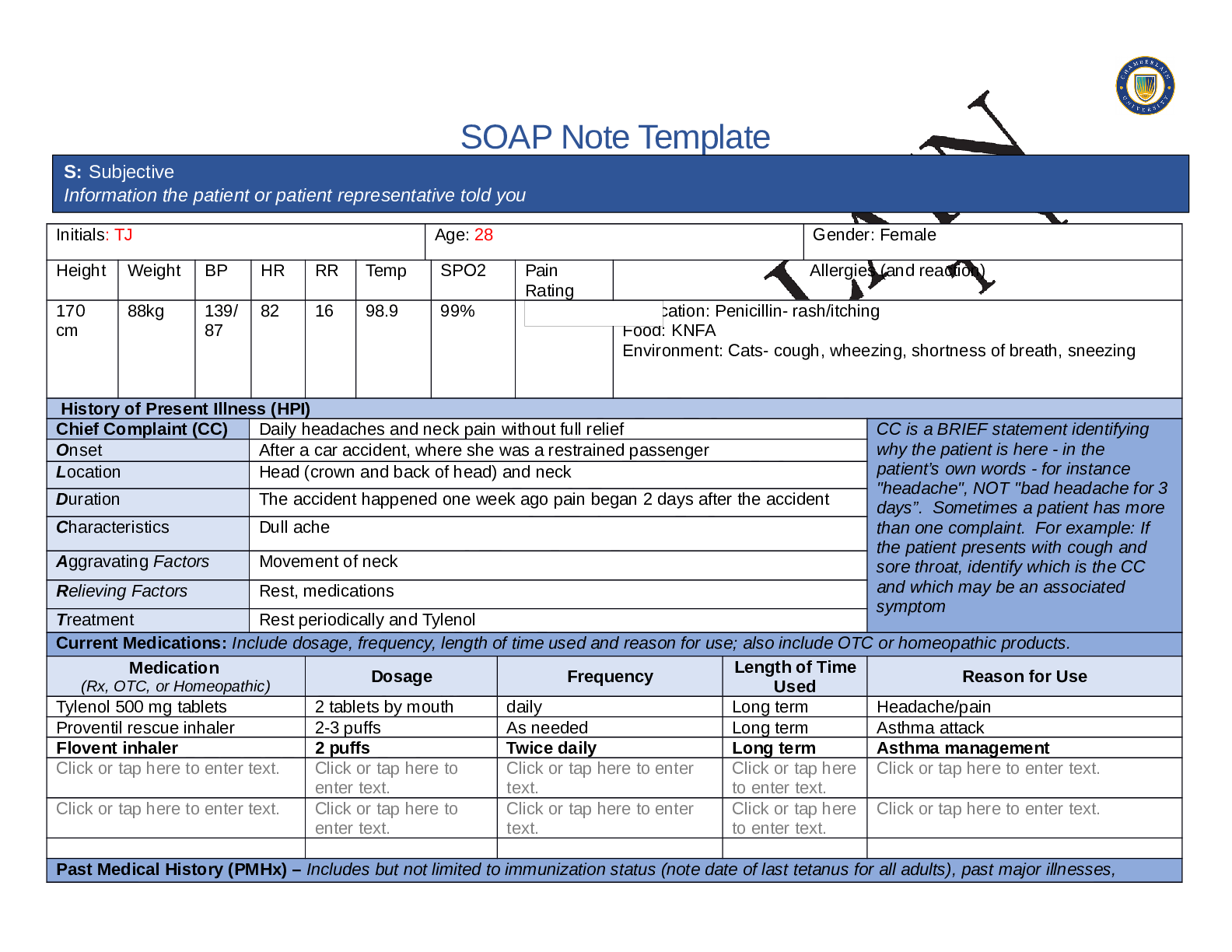
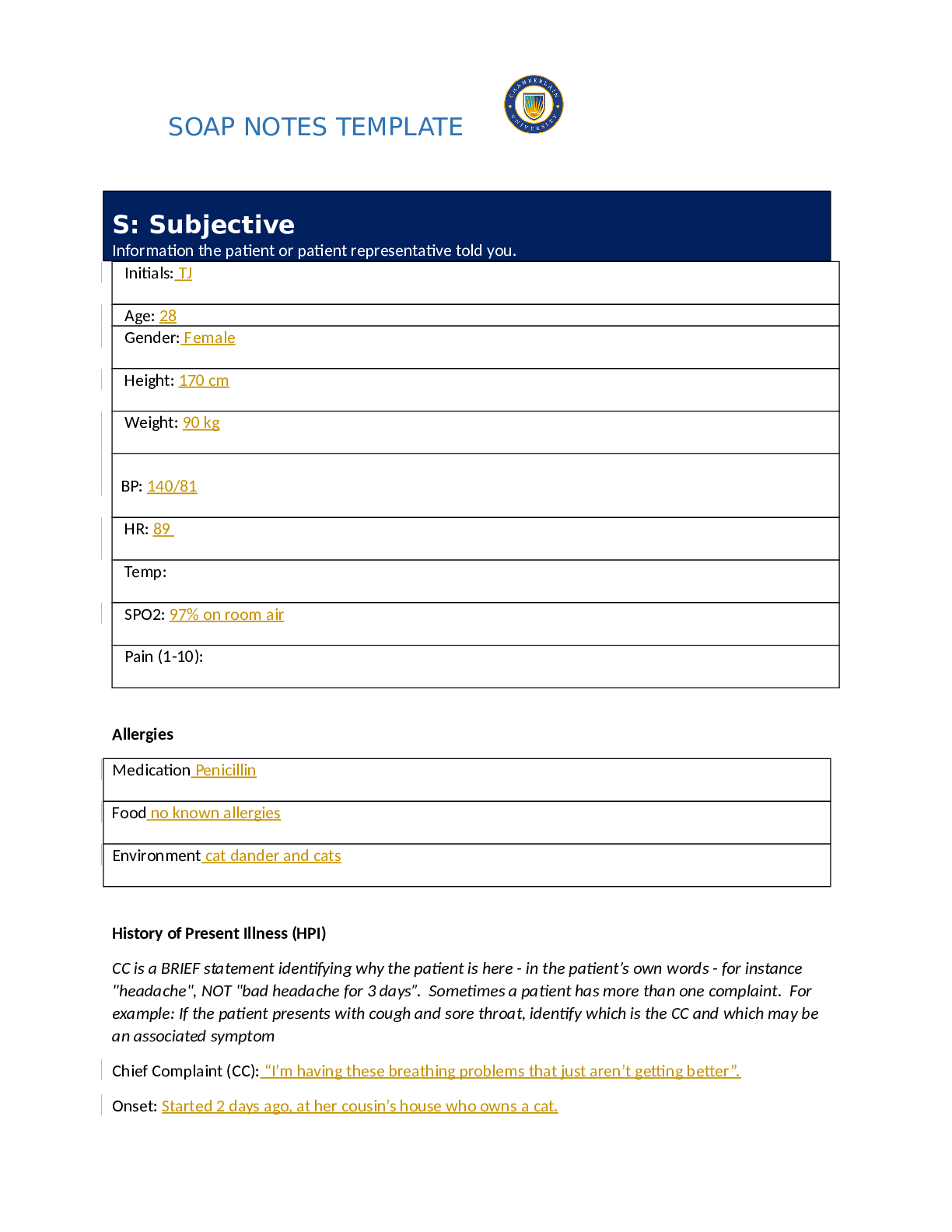
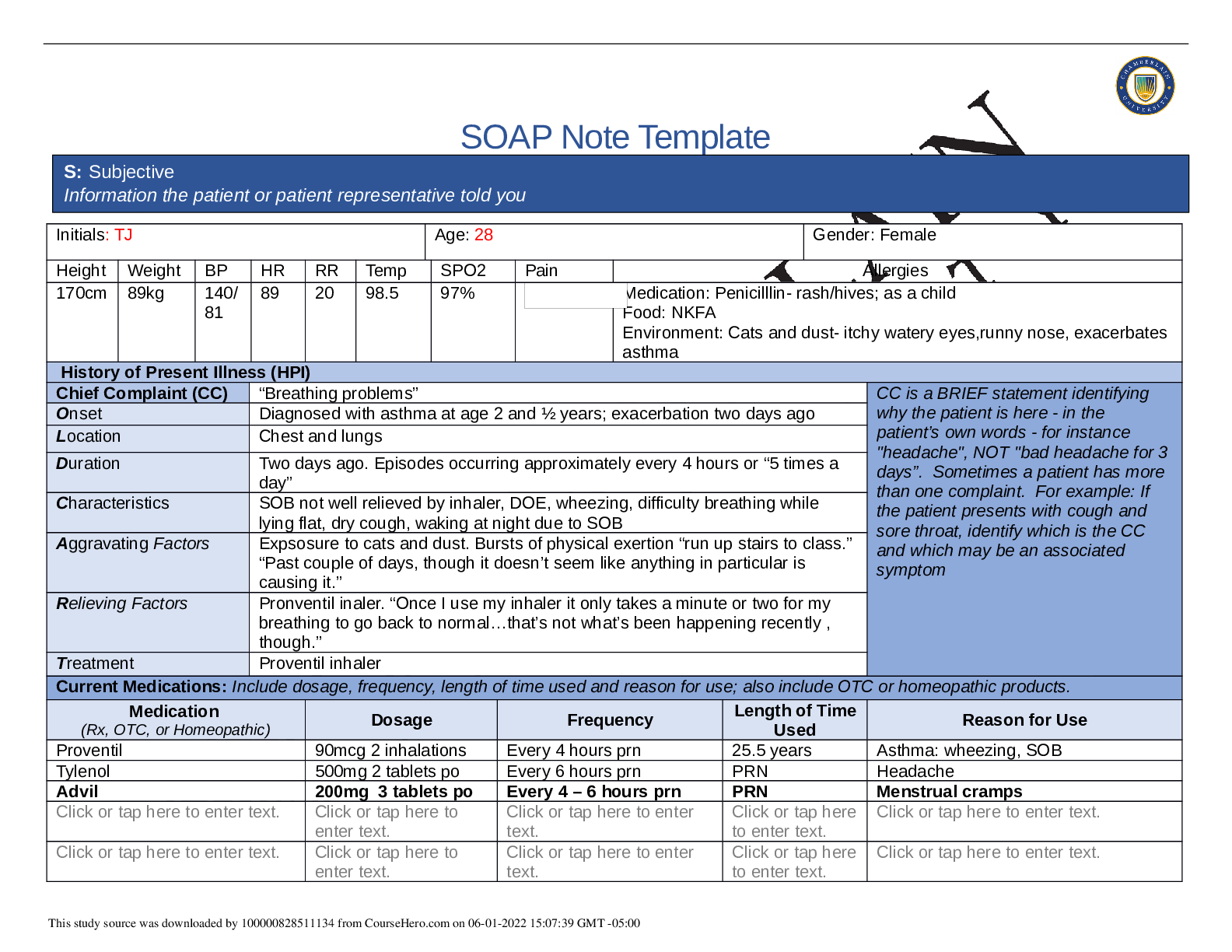
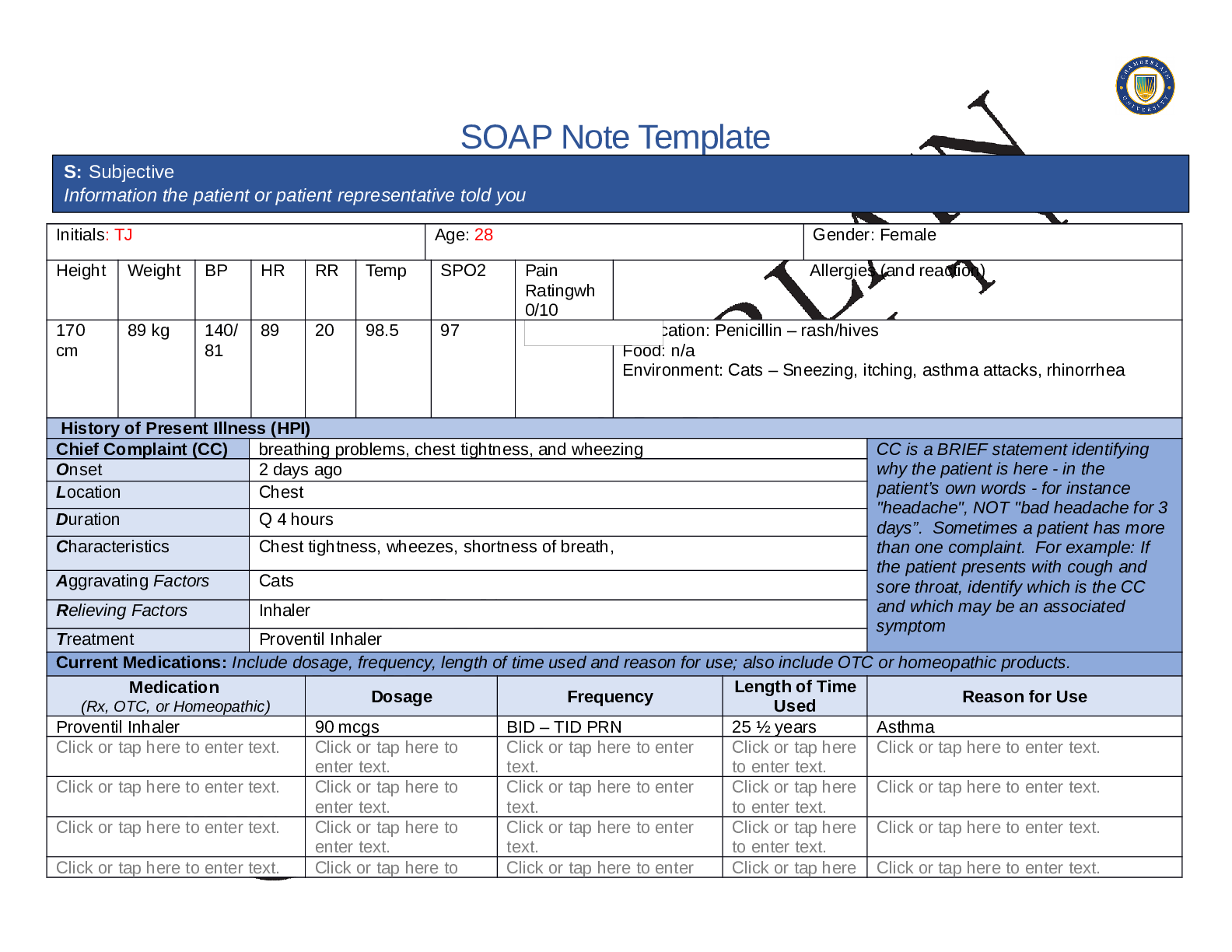
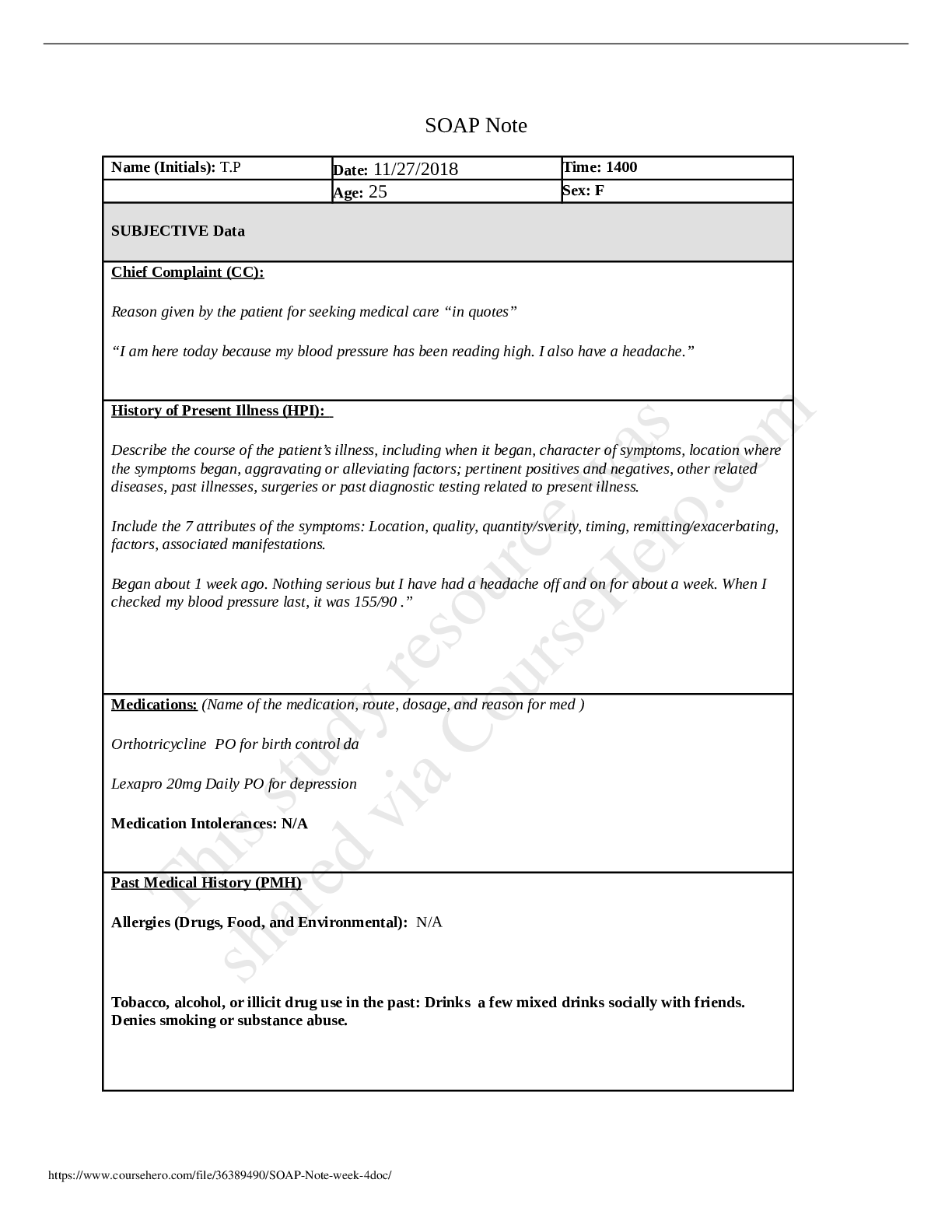
SOAP Note Template Initials: TJ Age: 28 Gender: Female Height Weight BP HR RR Temp SPO2 Pain Rating Allergies (and reaction) 170 cm 88kg 139/ 87 82 16 98.9 99% Medication: Penicillin- rash/it... ching Food: KNFA Environment: Cats- cough, wheezing, shortness of breath, sneezing History of Present Illness (HPI) Chief Complaint (CC) Daily headaches and neck pain without full relief CC is a BRIEF statement identifying why the patient is here - in the patient’s own words - for instance "headache", NOT "bad headache for 3 days”. Sometimes a patient has more than one complaint. For example: If the patient presents with cough and sore throat, identify which is the CC and which may be an associated symptom Onset After a car accident, where she was a restrained passenger Location Head (crown and back of head) and neck Duration The accident happened one week ago pain began 2 days after the accident Characteristics Dull ache Aggravating Factors Movement of neck Relieving Factors Rest, medications Treatment Rest periodically and Tylenol Current Medications: Include dosage, frequency, length of time used and reason for use; also include OTC or homeopathic products. Medication (Rx, OTC, or Homeopathic) Dosage Frequency Length of Time Used Reason for Use Tylenol 500 mg tablets 2 tablets by mouth daily Long term Headache/pain Proventil rescue inhaler 2-3 puffs As needed Long term Asthma attack Flovent inhaler 2 puffs Twice daily Long term Asthma management Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Click or tap here to enter text. Past Medical History (PMHx) – Includes but not limited to immunization status (note date of last tetanus for all adults), past major illnesses, S: Subjective Information the patient or patient representative told you hospitalizations, and surgeries. Depending on the CC, more info may be needed. Ms. Jones is a pleasant, obese 28-year-old African American woman in no acute distress, she does appear uncomfortable. She is alert and oriented, dressed appropriately and maintains eye contact. She is allergic to penicillin and cats and denies food allergies. She is positive for a history of diabetes, which she states she does not take medication for and asthma that is well controlled, which she takes a daily inhaler for and has a rescue inhaler that has not been used in approximately eight months. She is up to date on immunizations, only reports prior hospitalizations for asthma as a child, no previous surgeries. Ms. Jones arrived at the clinic today and presents with complaints of a headache and neck stiffness that started 2 days after she was in a minor car accident which was a rear end collision. The accident occurred one week ago, and she states that she was a restrained passenger in the vehicle and denies loss of consciousness afterwards. She did not seek medical treatment after the accident. Social History (Soc Hx) - Includes but not limited to occupation and major hobbies, family status, tobacco and alcohol use, and any other pertinent data. Include health promotion such as use seat belts all the time or working smoke detectors in the house. Ms. Jones reports near finishing of her college schooling and will become an accountant. She reports occasional alcohol use with her friends once or twice a week but states she never drinks more than two to three drinks at a time. She denies any history or present use of tobacco and denies vaping. She denies any current drug use and reports marijuana use as a teenager. She reports she does wear her seatbelt. Family History (Fam Hx) - Includes but not limited to illnesses with possible genetic predisposition, contagious or chronic illnesses. Reason for death of any deceased first degree relatives should be included. Include parents, grandparents, siblings, and children. Include grandchildren if pertinent. She denies any familial history of neurological disorders and reports the recent death of her father. Review of Systems (ROS): Address all body systems that may help rule in or out a differential diagnosis Check the box next to each positive symptom and provide additional details. Constitutional If patient denies all symptoms for this system, check here: ☒ Skin If patient denies all symptoms for this system, check here: ☒ HEENT If patient denies all symptoms for this system, check here: ☐ ☐Fatigue Click or tap here to enter text. ☐Weakness Click or tap here to enter text. ☐Fever/Chills Click or tap here to enter text. ☐Weight Gain Click or tap here to enter text. ☐Weight Loss Click or tap here to enter text. ☐Trouble Sleeping Click or tap here to enter text. ☐Night Sweats Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Itching Click or tap here to enter text. ☐Rashes Click or tap here to enter text. ☐Nail Changes Click or tap here to enter text. ☐Skin Color Changes Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Diplopia Click or tap here to enter text. ☐Eye Pain Click or tap here to enter text. ☐Eye redness Click or tap here to enter text. ☒Vision changes not new onset since accident ☐Photophobia Click or tap here to enter text. ☐Eye discharge Click or tap here to enter text. ☐Earache Click or tap here to enter text. ☐Tinnitus Click or tap here to enter text. ☐Epistaxis Click or tap here to enter text. ☐Vertigo Click or tap here to enter text. ☐Hearing Changes Click or tap here to enter text. ☐Hoarseness Click or tap here to enter text. ☐Oral Ulcers Click or tap here to enter text. ☐Sore Throat Click or tap here to enter text. ☐Congestion Click or tap here to enter text. ☐Rhinorrhea Click or tap here to enter text. ☐Other: Click or tap here to enter text. Respiratory If patient denies all symptoms for this system, check here: ☒ Neuro If patient denies all symptoms for this system, check here: ☐ Cardiac and Peripheral Vascular If patient denies all symptoms for this system, check here: ☒ ☐Cough Click or tap here to enter text. ☐Hemoptysis Click or tap here to enter text. ☐Dyspnea Click or tap here to enter text. ☐Wheezing Click or tap here to enter text. ☐Pain on Inspiration Click or tap here to enter text. ☐Sputum Production ☐Syncope or Lightheadedness Click or tap here to enter text. ☒Headache daily without full relief ☐Numbness Click or tap here to enter text. ☐Tingling Click or tap here to enter text. ☐Sensation Changes ☐Speech Deficits Click or tap ☐Chest pain Click or tap here to enter text. ☐SOB Click or tap here to enter text. ☐Exercise Intolerance Click or tap here to enter text. ☐Orthopnea Click or tap here to enter text. ☐Edema Click or tap here to enter text. ☐Murmurs Click or tap here to enter text. ☐Palpitations Click or tap here to enter text. ☐Faintness Click or tap here to enter text. ☐Claudications Click or tap here to enter text. ☐PND Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Other: Click or tap here to enter text. here to enter text. ☐Other: Click or tap here to enter text. MSK If patient denies all symptoms for this system, check here: ☐ GI If patient denies all symptoms for this system, check here: ☒ GU If patient denies all symptoms for this system, check here: ☒ PSYCH If patient denies all symptoms for this system, check here: ☒ ☒Pain neck ☐Stiffness Click or tap here to enter text. ☐Crepitus Click or tap here to enter text. ☐Swelling Click or tap here to enter text. ☐Limited ROM ☐Redness Click or tap here to enter text. ☐Misalignment Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Nausea/Vomiting Click or tap here to enter text. ☐Dysphasia Click or tap here to enter text. ☐Diarrhea Click or tap here to enter text. ☐Appetite Change Click or tap here to enter text. ☐Heartburn Click or tap here to enter text. ☐Blood in Stool Click or tap here to enter text. ☐Abdominal Pain Click or tap here to enter text. ☐Excessive Flatus Click or tap here to enter text. ☐Food Intolerance Click or tap here to enter text. ☐Rectal Bleeding Click or tap here to enter text. ☐Other: ☐Urgency Click or tap here to enter text. ☐Dysuria Click or tap here to enter text. ☐Burning Click or tap here to enter text. ☐Hematuria Click or tap here to enter text. ☐Polyuria Click or tap here to enter text. ☐Nocturia Click or tap here to enter text. ☐Incontinence Click or tap here to enter text. ☐Other: Click or tap here to enter text. ☐Stress Click or tap here to enter text. ☐Anxiety Click or tap here to enter text. ☐Depression Click or tap here to enter text. ☐Suicidal/Homicidal Ideation Click or tap here to enter text. ☐Memory Deficits Click or tap here to enter text. ☐Mood Changes Click or tap here to enter text. ☐Trouble Concentrating Click or tap here to enter text. ☐Other: Click or tap here to enter text. GYN If patient denies all symptoms for this Hematology/Lymphatics If patient denies all symptoms for this system, Endocrine If patient denies all symptoms for this system, system, check here: ☒ check here: ☒ check here: ☐ ☐Rash Click or tap here to enter text. ☐Discharge Click or tap here to enter text. ☐Itching Click or tap here to enter text. ☐Irregular Menses Click or tap here to enter text. ☐Dysmenorrhea Click or tap here to enter text. ☐Foul Odor Click or tap here to enter text. ☐Amenorrhea Click or tap here to enter text. ☐LMP: Click or tap here to enter text. ☐Contraception Click or tap here to enter text. ☐Other:Click or tap here to enter text. ☐Anemia Click or tap here to enter text. ☐ Easy bruising/bleeding Click or tap here to enter text. ☐ Past Transfusions Click or tap here to enter text. ☐ Enlarged/Tender lymph node(s) Click or tap here to enter text. ☐ Blood or lymph disorder Click or tap here to enter text. ☐ Other Click or tap here to enter text. ☐ Abnormal growth Click or tap here to enter text. ☐ Increased appetite Click or tap here to enter text. ☐ Increased thirst Click or tap here to enter text. ☐ Thyroid disorder Click or tap here to enter text. ☐ Heat/cold intolerance Click or tap here to enter text. ☐ Excessive sweating Click or tap here to enter text. ☒ Diabetes no medications taken ☐ Other Click or tap here to enter text. [Show More]
Last updated: 2 years ago
Preview 1 out of 11 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$10.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Mar 21, 2021
Number of pages
11
Written in
Additional information
This document has been written for:
Uploaded
Mar 21, 2021
Downloads
0
Views
177




.png)