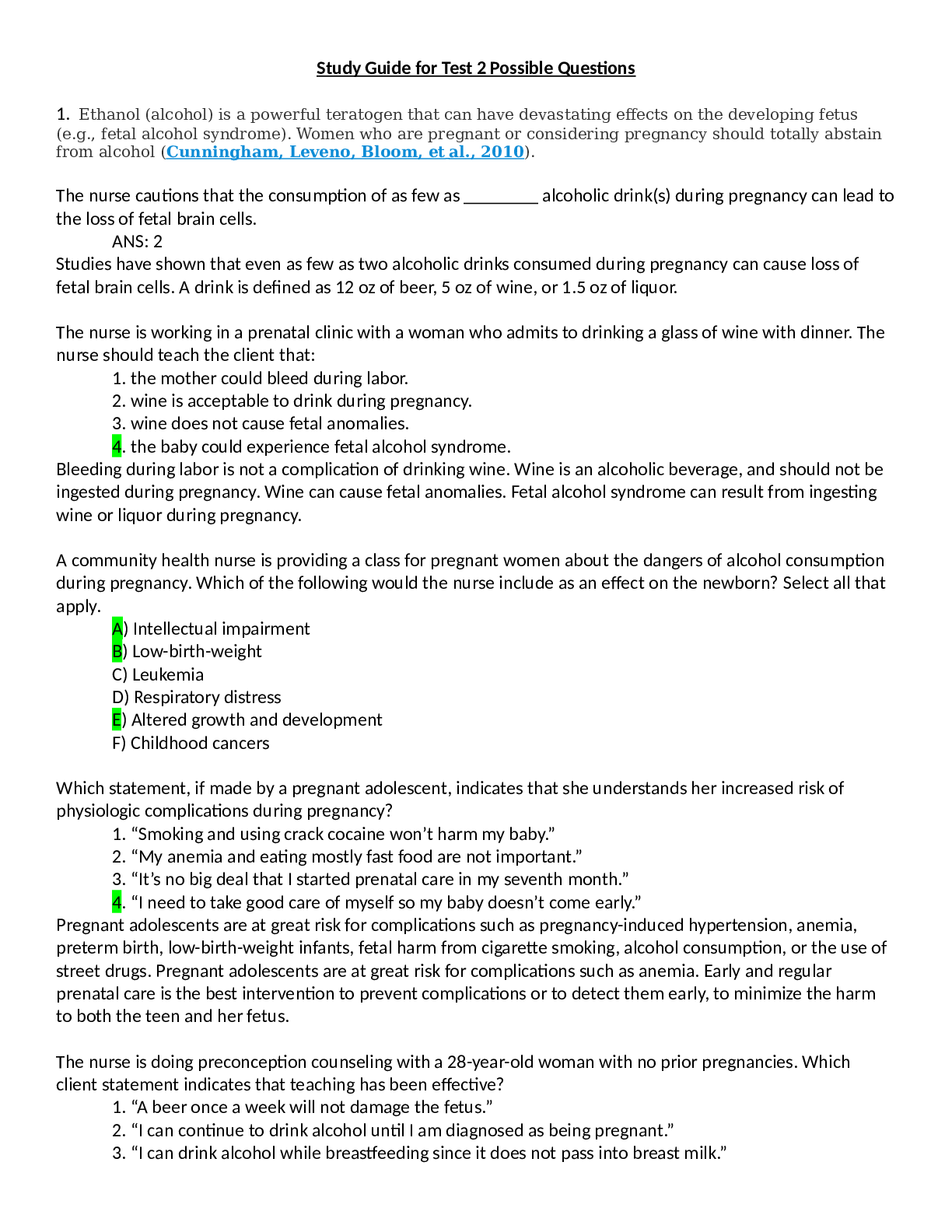
1. Ethanol (alcohol) is a powerful teratogen that can have devastating effects on the developing fetus
(e.g., fetal alcohol syndrome). Women who are pregnant or considering pregnancy should totally abstain
from alcohol
...
1. Ethanol (alcohol) is a powerful teratogen that can have devastating effects on the developing fetus
(e.g., fetal alcohol syndrome). Women who are pregnant or considering pregnancy should totally abstain
from alcohol ( Cunningham, Leveno, Bloom, et al., 2010).
The nurse cautions that the consumption of as few as ________ alcoholic drink(s) during pregnancy can lead to
the loss of fetal brain cells.
ANS: 2
Studies have shown that even as few as two alcoholic drinks consumed during pregnancy can cause loss of
fetal brain cells. A drink is defined as 12 oz of beer, 5 oz of wine, or 1.5 oz of liquor.
The nurse is working in a prenatal clinic with a woman who admits to drinking a glass of wine with dinner. The
nurse should teach the client that:
1. the mother could bleed during labor.
2. wine is acceptable to drink during pregnancy.
3. wine does not cause fetal anomalies.
4. the baby could experience fetal alcohol syndrome.
Bleeding during labor is not a complication of drinking wine. Wine is an alcoholic beverage, and should not be
ingested during pregnancy. Wine can cause fetal anomalies. Fetal alcohol syndrome can result from ingesting
wine or liquor during pregnancy.
A community health nurse is providing a class for pregnant women about the dangers of alcohol consumption
during pregnancy. Which of the following would the nurse include as an effect on the newborn? Select all that
apply.
A) Intellectual impairment
B) Low-birth-weight
C) Leukemia
D) Respiratory distress
E) Altered growth and development
F) Childhood cancers
Which statement, if made by a pregnant adolescent, indicates that she understands her increased risk of
physiologic complications during pregnancy?
1. “Smoking and using crack cocaine won’t harm my baby.”
2. “My anemia and eating mostly fast food are not important.”
3. “It’s no big deal that I started prenatal care in my seventh month.”
4. “I need to take good care of myself so my baby doesn’t come early.”
Pregnant adolescents are at great risk for complications such as pregnancy-induced hypertension, anemia,
preterm birth, low-birth-weight infants, fetal harm from cigarette smoking, alcohol consumption, or the use of
street drugs. Pregnant adolescents are at great risk for complications such as anemia. Early and regular
prenatal care is the best intervention to prevent complications or to detect them early, to minimize the harm
to both the teen and her fetus.
The nurse is doing preconception counseling with a 28-year-old woman with no prior pregnancies. Which
client statement indicates that teaching has been effective?
1. “A beer once a week will not damage the fetus.”
2. “I can continue to drink alcohol until I am diagnosed as being pregnant.”
3. “I can drink alcohol while breastfeeding since it does not pass into breast milk.”
4. “I need to stop drinking alcohol completely when I start trying to get pregnant.”
1. It is not known how much alcohol will cause fetal damage; therefore, alcohol during pregnancy is
contraindicated. 2. Women should discontinue drinking alcohol when they start to attempt pregnancy.
3. Breastfeeding generally is not contraindicated, although alcohol is excreted in breast milk. Excessive alcohol
consumption may intoxicate the infant and inhibit the maternal letdown reflex. 4. Because birth defects that
are related to fetal alcohol exposure can occur in the first 3 to 8 weeks’ gestation, often before the woman
even knows she is pregnant, women should discontinue drinking alcohol when they start to attempt
pregnancy.
The nurse is caring for a patient that is actively trying to conceive a child but continues to drink alcohol. The
patient states that she'll stop drinking once she is pregnant. What is the most appropriate response by the
nurse?
a. "Abstaining is best since most fetal development occurs before you realize you are pregnant."
b. "Small amounts of alcohol are safe at any time during pregnancy."
c. "Things will be okay if you quit drinking alcohol once you know you are pregnant."
d. "Alcohol use should be avoided early in pregnancy but is acceptable past week 20."
Rapid development occurs before many women know that they are pregnant, making alcohol consumption
unsafe at any time during pregnancy.
2. One problem that can interfere with milk consumption is lactose intolerance, the inability to digest
milk sugar (lactose) caused by the lack of the lactase enzyme in the small intestine. It is relatively
common in adults, particularly African-Americans, Asians, Native Americans, and Inuits (Alaska Natives).
Milk consumption can cause abdominal cramping, bloating, and diarrhea in such people, although many
lactose-intolerant individuals can tolerate small amounts of milk without symptoms.
The nurse is discussing food allergies with a group of mothers whose children are allergy prone. Which of the
following statements made by a mother best describes lactose intolerance?
1. “My child is allergic to milk; it makes her very gassy.”
2. “Dairy products require a special enzyme to be digested properly.”
3. “Being lactose intolerant means my child can’t tolerate dairy products.”
4. “My child gets diarrhea from dairy products because she can’t digest lactose.”
Food intolerance is not an allergy, but a particular food that causes the body distress within a few hours of
ingestion. The result is diarrhea, cramps, or flatulence. For example, people who drink cow’s milk who have
these symptoms are not allergic to milk but lack the enzyme needed to digest the milk sugar lactose; they are
lactose intolerant. To be lactose intolerant (exhibiting the signs after ingesting dairy products) does not
constitute a dairy allergy. The remaining options are not as specific as the answer.
The nurse is discussing food allergies with a group of mothers whose children are allergy prone. Which of the
following statements made by the nurse best describes lactose intolerance?
1. “If milk causes diarrhea, cramps, or gas, it might be an intolerance of lactose.”
2. “You don’t have to be allergic to dairy for it to cause you problems.”
3. “Allergies to milk can be very dangerous, even life threatening.”
4. “Many children outgrow their intolerance of dairy lactose.”
The traditional diet of Asian women includes little meat and few dairy products and may be low in calcium and
iron. The nurse can help a client increase her intake of these foods by which action?
a. Suggest that she eat more tofu, bok choy, and broccoli.
b. Suggest that she eat more hot foods during pregnancy.
c. Emphasize the need for increased milk intake during pregnancy.
d. Tell her husband that she must increase her intake of fruits and vegetables for the baby’s sake.
The diet should be improved by increasing foods acceptable to the woman. These foods are common in the
Asian diet and are good sources of calcium and iron. Pregnancy is considered hot; therefore, the woman would
eat cold foods. Because milk products are not part of this woman’s diet, it should be respected and other
alternatives offered. Also, lactose intolerance is common. Fruits and vegetables are cold foods and should be
included in the diet. In regard to the family dynamics, however, the husband does not dictate to the wife in this
culture.
3. Patient Teaching: Iron Supplementation
A diet rich in vitamin C (in citrus fruits, tomatoes, melons, and strawberries) and heme iron (in meats) increases the
absorption of iron supplement; therefore include these in the diet often.
Bran, tea, coffee, milk, oxalates (in spinach and Swiss chard), and egg yolk decrease iron absorption. Avoid consuming them
at the same time as the supplement.
Iron is absorbed best if it is taken when the stomach is empty; that is, take it between meals with a beverage other than tea,
coffee, or milk.
Iron can be taken at bedtime if abdominal discomfort occurs when it is taken between meals.
If an iron dose is missed, take it as soon as it is remembered if that is within 13 hours of the scheduled dose. Do not double
up on the dose.
Keep the supplement in a childproof container and out of the reach of any children in the household.
The iron may cause stools to be black or dark green.
Constipation is common with iron supplementation. A diet high in fiber with adequate fluid intake is recommended.
A patient will be taking oral iron supplements at home. The nurse will include which statements in the teaching
plan for this patient? (Select all that apply.)
a. Take the iron tablets with meals.
b. Take the iron tablets on an empty stomach 1 hour before meals.
c. Take the iron tablets with an antacid to prevent heartburn.
d. Drink 8 ounces of milk with each iron dose.
e. Taking iron supplements with orange juice enhances iron absorption.
f. Stools may become loose and light in color.
g. Stools may become black and tarry.
h. Tablets may be crushed to enhance iron absorption.
The pregnant client with significant iron deficiency anemia is prescribed iron supplements. The client confides
to the nurse that she can’t take iron because it makes her nauseous. What is the best response by the nurse?
a. “Iron will be absorbed more readily if taken with orange juice.”
b. “It is important to take this drug regardless of this side effect.”
c. “Taking the drug with milk may decrease your symptoms.”
d. “Try taking the iron at bedtime on an empty stomach.”
Iron taken at bedtime may be easier to tolerate. All the answers are true statements; however, only the option
that states that iron taken at bedtime may be easier to tolerate addresses both optimal absorption of iron and
alleviation of nausea, which will not be noticeable during sleep. It is true that taking iron with milk will
decrease the symptoms, but it will also decrease absorption.
A patient in her first trimester of pregnancy who is taking iron supplements for anemia is experiencing
constipation. What is the best advice the nurse can give her?
A) Stop taking iron supplements for a few days, exercise more, drink more fluids, eat high-fiber, lowiron foods until the constipation is relieved, then resume her iron supplement
B) Continue taking iron supplements but increase fluids and high-fiber foods; exercise more
C) Increase her iron supplements, fluid intake, and consumption of high-fiber foods; exercise more
D) Take her iron supplement every other day, increase fluid intake and consumption of high-fiber foods;
exercise more
4. In general, the nutrient needs of pregnant women, with perhaps the exception of folate and iron, can
be met through dietary sources. Counseling about the need for a varied diet rich in vitamins and minerals
should be a part of early prenatal care of every pregnant woman and should be reinforced throughout
pregnancy (see Community Focus box). It has been suggested that taking a micronutrient supplement
(including vitamins and trace minerals) before and during pregnancy reduces the risk for congenital
defects, LBW, and preterm birth, as well as preeclampsia. So the healthcare provider would want to
encourage a supplementation of folate to help with neural tube and the iron to encourage decreased
anemia.
A pregnant client arrives for her first prenatal visit at the clinic. She tells you that she has been taking an
additional 400 mcg of folic acid prior to her pregnancy. Based on information obtained, she is at 8 weeks’
gestation. What recommendation would you give regarding folic acid supplementation?
a. Have the client continue to take 400 mcg folic acid throughout her pregnancy.
b. Tell the client that she no longer has to take additional folic acid because it will be included in her
prenatal vitamins.
c. Have the client increase her folic acid intake to 1000 mcg throughout the rest of her pregnancy.
d. Schedule the client to go for an AFP (alpha-fetoprotein) test.
Prenatal vitamins include adequate folic acid supplementation, so clients should not take additional
supplementation as long they continue their prenatal vitamins. During pregnancy, the recommendation is to
increase the folic acid intake to 600 mcg. 1000 mcg of folic acid would be an excessive dose. The AFP test
should be done at 15 to 18 weeks’ gestation. This is not clinically indicated because the client is at 8 weeks’
gestation.
A nurse is preparing a presentation for an expectant parent group about neural tube defects and prevention.
Which would the nurse emphasize?
A) Smoking cessation
B) Aerobic exercise
C) Increased calcium intake
D) Folic acid supplementation
The cause of neural tube defects is unknown, but there is strong evidence to support the use of folic acid
supplementation for prevention. Smoking cessation and aerobic exercise are general health recommendations
unrelated to neural tube defects. Increased calcium intake is important for fetal growth and development, but
it is not linked to preventing neural tube defects.
The community nurse is planning prevention measures designed to avoid conditions that can cause cognitive
impairment. Taking folic acid supplements during pregnancy to prevent neural tube defects is which type of
prevention strategy?
a. Primary
b. Secondary
c. Tertiary
d. Rehabilitative
Primary prevention strategies are those designed to avoid conditions that cause cognitive impairment. Use of
folic acid supplements during pregnancy to prevent neural tube defects is a primary prevention strategy.
Secondary prevention activities are those designed to identify the condition early and initiate treatment to
avert cerebral damage. Tertiary prevention strategies are those concerned with treatment to minimize longterm consequences. Rehabilitation services is an example of tertiary prevention.
Which action by the parents demonstrates an understanding of the nurse’s teaching with regard to prevention
of iron-deficient anemia?
1. Feeding their infant with a formula that is not iron fortified
2. Starting iron-fortified infant cereal at 4 to 6 months of age
3. Introducing cow’s milk at 6 months of age
4. Limiting vitamin C consumption after 1 year of age
Starting iron-fortified infant cereal at 4 to 6 months of age is recommended for prevention of iron deficiency in
children. Infants who are not breast-fed should get iron-fortified formula. Cow’s milk should not be introduced
until 12 months of age. Vitamin C should be started at 6 to 9 months of age and continued, because foods rich
in vitamin C improve iron absorption.
The nurse is preparing a community outreach program about the prevention of iron-deficiency anemia in
infants. What statement should the nurse include in the program?
a. Whole milk can be introduced into the infant’s diet in small amounts at 6 months.
b. Iron supplements cannot be given until the infant is older than 1 year of age.
c. Iron-fortified cereal should be introduced to the infant at 2 months of age.
d. Breast milk or iron-fortified formula should be used for the first 12 months.
Prevention, the primary goal in iron-deficiency anemia, is achieved through optimal nutrition and appropriate
iron supplements. The American Academy of Pediatrics recommends feeding an infant only breast milk or ironfortified formula for the first 12 months of life. Whole cow’s milk should not be introduced until after 12
months, iron supplements can be given during the first year of life, and iron-fortified cereals should not be
introduced until the infant is 4 to 6 months old.
5. During the first trimester of pregnancy the pregnant woman's metabolic status is significantly
influenced by the rising levels of estrogen and progesterone. These hormones stimulate the beta cells in
the pancreas to increase insulin production, which promotes increased peripheral use of glucose and
decreased blood glucose, with fasting levels being reduced by approximately 10% ( Fig. 11-1, A). At the
same time an increase in tissue glycogen stores and a decrease in hepatic glucose production occur,
which further encourage lower fasting glucose levels. As a result of these normal metabolic changes of
pregnancy, women with insulin-dependent diabetes are prone to hypoglycemia during the first trimester.
During the second and third trimesters pregnancy exerts a “diabetogenic” effect on the maternal
metabolic status. Because of the major hormonal changes, decreased tolerance to glucose, increased
insulin resistance, decreased hepatic glycogen stores, and increased hepatic production of glucose occur.
Rising levels of human chorionic somatomammotropin, estrogen, progesterone, prolactin, cortisol, and
insulinase increase insulin resistance through their actions as insulin antagonists. Insulin resistance is a
glucose-sparing mechanism that ensures an abundant supply of glucose for the fetus. Maternal insulin
requirements gradually increase from approximately 18 to 24 weeks of gestation to approximately 36
weeks
FIG 11-1 Changing insulin needs during pregnancy. A, First trimester: Insulin need is reduced because of
increased insulin production by pancreas and increased peripheral sensitivity to insulin; nausea, vomiting, and
decreased food intake by mother and glucose transfer to embryo or fetus contribute to hypoglycemia.
The client with insulin-dependent type 2 diabetes and an HbA1c of 5% is planning to become pregnant soon.
What anticipatory guidance should the nurse provide this client?
1. Vascular disease that accompanies diabetes slows progression.
2. The risk of ketoacidosis decreases during the length of the pregnancy.
3. The baby is likely to have a congenital abnormality because of the diabetes.
4. Insulin needs decrease in the first trimester and increase during the third trimester.
Vascular disease progresses more rapidly during pregnancy, especially if blood sugar control is not good.
Problems such as nephropathy and retinopathy can result. The risk of ketoacidosis increases during pregnancy.
Infants of diabetic mothers have a 5% to 10% greater risk of having a congenital abnormality. This risk
increases to 20% to 25% if the HbA1c is over 10%. In addition, insulin requirements drop suddenly after
delivery of the placenta.
Why does the woman taking oral hypoglycemic agents to control diabetes mellitus need to take insulin during
pregnancy?
a. Insulin can cross the placental barrier to the fetus.
b. Insulin does not cross the placental barrier to the fetus.
c. Oral agents do not cross the placenta.
d. Oral agents are not sufficient to meet maternal insulin needs.
Oral hypoglycemic agents are not used during pregnancy because they can cross the placenta, possibly
resulting in fetal birth defects or hypoglycemia.
A pregnant woman has been diagnosed with gestational diabetes. She asks the nurse whether that means she
will have to take insulin. The nurse’s best response is:
a. “Women who develop diabetes during pregnancy usually need to take insulin for the rest of their
lives.”
b. “Oral diabetes medications are usually ordered during pregnancy.”
c. “Some women need insulin, but you may be able to control your diabetes with diet.”
d. “You will probably have to switch to oral medications after the baby is born.”
Only 10% to 15% of women with gestational diabetes require insulin during pregnancy. Oral diabetes
medications cannot be used because they can harm the fetus. Most women with gestational diabetes who
require insulin will be able to discontinue the insulin after the birth of the baby.
Nursing intervention for pregnant clients with diabetes is based on the knowledge that the need for insulin is:
a. varied depending on the stage of gestation.
b. increased throughout pregnancy and the postpartum period.
c. decreased throughout pregnancy and the postpartum period.
d. should not change because the fetus produces its own insulin.
Insulin needs decrease during the first trimester, when nausea, vomiting, and anorexia are a factor. Insulin
needs increase during the second and third trimesters, when the hormones of pregnancy create insulin
resistance in maternal cells. Insulin needs change during pregnancy.
During the first trimester of pregnancy, the patient with pregestational diabetes usually requires:
a. More insulin than before her pregnancy
b. Less insulin than before her pregnancy
c. The same amount of insulin as before her pregnancy
d. Varying amounts of insulin, based on the results of her urine glucose tests
Patients who have diabetes before they become pregnant may actually require less insulin than usual in the
first trimester because serum glucose is reduced by high fetal demands, nausea and vomiting, and anorexia.
6. Poor glycemic control later in pregnancy, particularly in women without vascular disease, increases the
rate of fetal macrosomia. Macrosomia has been defined as a birth weight more than 4000 to 4500 g or
greater than the 90th percentile. It occurs in approximately 40% of pregestational diabetic pregnancies
and up to 50% of pregnancies complicated by GDM (Landon, Catalano, and Gabbe, 2012). Infants
born to women with diabetes tend to have a disproportionate increase in shoulder, trunk, and chest size.
Because of this tendency the risk of shoulder dystocia is greater in these babies than in other macrosomic
infants. Therefore women with diabetes face an increased likelihood of cesarean birth because of failure
of fetal descent or labor progress or of operative vaginal birth (birth involving the use of episiotomy,
forceps, or vacuum extractor) (Moore and Catalano, 2009).
Gestational diabetes mellitus is a condition characterized by carbohydrate intolerance that is first identified or
develops during pregnancy. What are the risks associated with gestational diabetes that a community health
nurse would address with a pregnant woman?
1. Blood glucose must be kept in a normal range to prevent early labor.
2. Women with gestational diabetes will require early delivery.
3. Women with gestational diabetes have a higher risk for preeclampsia.
4. Gestational diabetes can be prevented with a glucose tolerance test.
Women with gestational diabetes have a greater risk for preeclampsia, caesarean section, and infection.
A nurse in the perinatal clinic explains to a student nurse that which of the following patients are at highest risk
of developing gestational diabetes? (Select all that apply.)
A. A17-year-old in her second pregnancy
B. A 24-year-old pregnant woman with placenta previa
C. A 32-year-old woman with a BMI of 40
D. A woman whose first baby weighed 10.5 lb (4.7 kg)
E. A woman whose mother and sister had gestational diabetes
The risk factors for developing gestational diabetes include age older than 25; obesity; insulin resistance;
polycystic ovary syndrome; history of pregnancy-related diabetes mellitus; history of a large-for-gestational age
infant; hydramnios, stillbirth, miscarriage, or an infant with congenital anomalies during a previous pregnancy;
family history of type 2 diabetes (first-degree relative); and ethnicity. Being young does not confer additional
risk, nor does placenta previa. The 32-year-old is obese, the 10.5-lb baby is large for gestational age, and the
mother and sister are first-degree relatives.
7. Methadone maintenance treatment (MMT) is currently considered the standard of care for pregnant
women who are dependent on heroin or other narcotics. Buprenorphine (Subutex or Suboxone) is
another medication approved for opioid addiction treatment that is being used increasingly during
pregnancy. Opioid replacement therapy has been shown to decrease opioid and other drug abuse; reduce
criminal activity; improve individual functioning; and decrease rates of infections such as hepatitis B and
C, HIV, other sexually transmitted infections, and tuberculosis. In addition, opioid replacement therapy is
associated with reduced fetal exposure to illicit drug use and improved neonatal outcomes. However, 30%
to 80% of infants exposed to opioids, including methadone or buprenorphine, in utero require treatment
for neonatal abstinence syndrome (NAS). Neither the incidence nor the severity of NAS correlates
directly with the maternal medication dose at birth ( Wisner, Sit, Altemus, et al., 2012).
A preterm infant is jittery and has an oxygen saturation of 88%. After stabilizing the newborn, what action by
the nurse is most important?
A. Assess the mother for caffeine use during pregnancy.
B. Assess the mother for opioid use during pregnancy.
C. Call Child Protective Services (CPS) to take the child away.
D. Question the father about maternal drug abuse.
Maternal opioid use can lead to neonatal withdrawal syndrome, characterized by hyperirritability,
gastrointestinal dysfunction, respiratory distress, and autonomic disturbances. After stabilizing the baby, the
nurse should first assess the mother for opioid abuse during pregnancy. Caffeine use would not cause these
effects. Calling CPS is premature at this point. Questioning the father is not the best way to determine if the
mother has abused drugs.
Which key point should you teach a pregnant woman who is prescribed opioids drugs during pregnancy?
a. Your child may become addicted to opioids and go through withdrawal after birth.
b. These drugs do not cross the placenta so are safe to use during pregnancy.
c. Some opioids have been found to cause birth defects in animal studies.
d. Opioids are not present in breast milk so it is safe to breastfeed.
A patient has just acknowledged that she is 20 weeks pregnant and confides to the nurse that she has a daily
heroin habit. The nurse discusses treatment options for the patient. Which patient statement requires followup?
a. “My plan is to visit the outpatient clinic daily for treatment.”
b. “I will see my health care provider at least every 2 weeks.”
c. “My baby will not have to go through withdrawal when I take methadone.”
d. “With oral methadone, my baby and I are at decreased risk of infection.”
Pregnant women who use heroin are often prescribed an alternative drug such as methadone, a synthetic
opiate. Methadone can be taken orally once daily and is long- acting, providing consistent blood levels to
decrease the adverse fetal effects of wide swings in blood levels found with heroin use. Methadone also
reduces the risk of infections from contaminated needles and drug-seeking behavior, such
[Show More]
.png)