HESI EXIT EXAM RN 2020 Pediatrics U-world tables
Document Content and Description Below
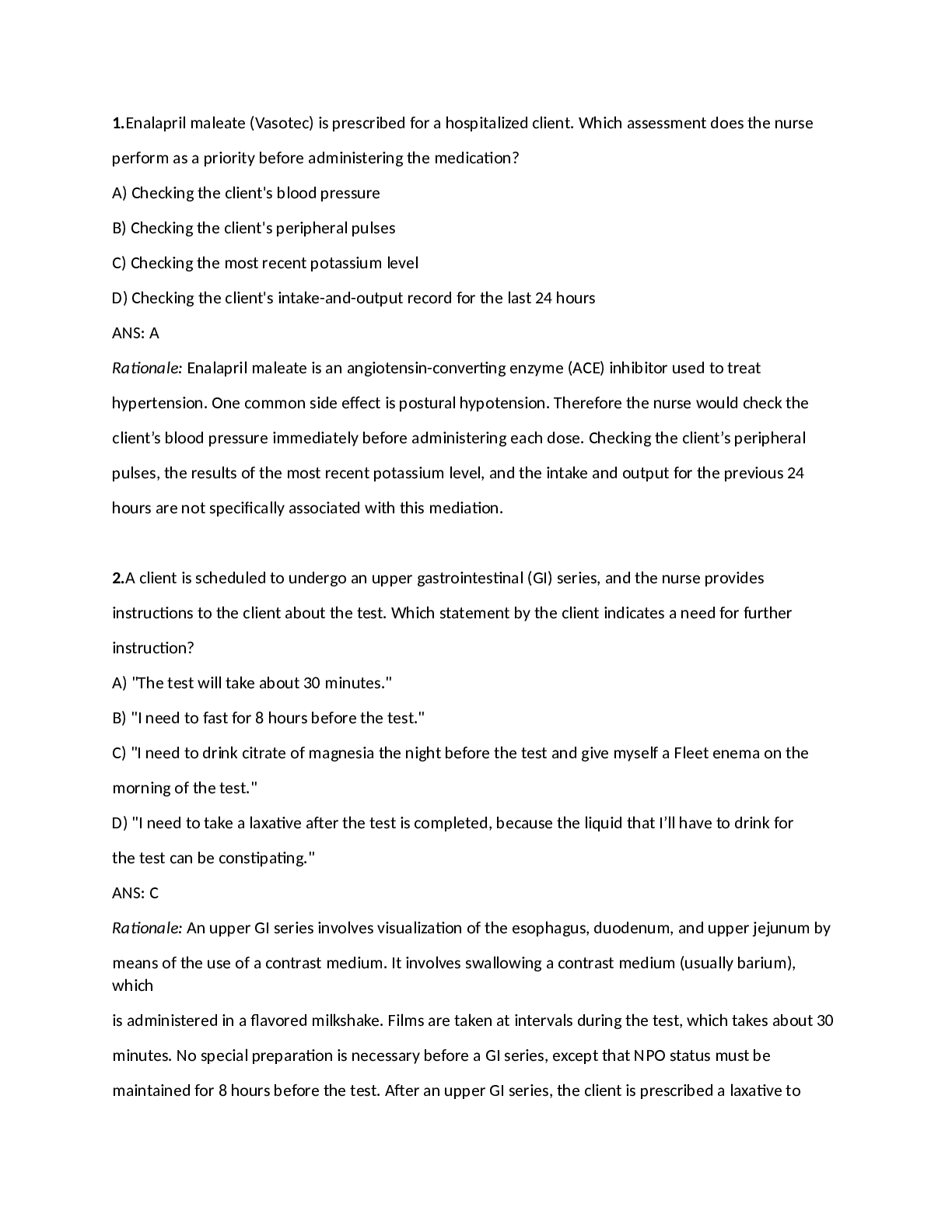
Differential diagnosis of stridor in infants & children Diagnosis Distinguishing Features Croup (Laryngotracheobronchitis) - Most common from age 6 months to 6 years - Associated with “barky”... cough, fever, rhinorrhea & congestion Laryngomalacia - Stridor most severe at age 4-8 months - Persistent stridor that worsens in supine position & improves in prone position Foreign body aspiration - Stridor caused by laryngotracheal foreign bodies has acute onset - Associated with moderate-to-severe respiratory distress Vascular Ring - Presents before age 1 year - Persistent stridor that improves with neck extension - Associated with cardiac abnormalities (50%) Croup (laryngotracheitis) Pathogenesis - Parainfluenza viral infection – inflammation of larynx & trachea Epidemiology - Age 6 months to 3 years - Fall, early winter Clinical Features - Inspiratory stridor - “Barky” seal-like cough - Hoarse voice Treatment - Mild (no stridor at rest: corticosteroids) - Moderate/severe (stridor at rest): corticosteroids + nebulized epinephrine Key respiratory tract infection in children Diagnosis Classic pathogen Presentation Laryngotracheitis (croup) - Parainfluenza virus - Age 6 months to 3 years - “Barky” coughing, stridor, hoarse voice Epiglottitis - Haemophilus influenza - Unvaccinated children - Sore throat, dysphagia, drooling, “tripod position” Bronchiolitis - Respiratory Syncytial Virus - Age <2 years - Wheezing, coughing Pertussis in Infants and Children Clinical Phases Catarrhal 1-2 weeks Paroxysmal 2-6 weeks Convalescent weeks to months - Mild cough, Rhinitis - Coughing paroxysms with inspiratory “whoops” - Symptoms resolve gradually Diagnosis - Pertussis Culture or PCR - Lymphocyte predominant leukocytosis Treatment - Macrolides (azithromycin, erythromycin, clarithromycin) Prevention - Acellular Pertussis Vaccine Complications - Pneumonia, weight loss, subconjunctival hemorrhages, pneumothorax, respiratory failure, death (infants) 2 Measles (Rubeola) – Paramyxovirus SS -RNA Clinical Presentation Prodromal: - Fever, malaise, & anorexia - Conjunctivitis, coryza, cough, Koplik spots Exanthema - Blanching, reddish-brown maculopapular rash - Cephalocaudal & centrifugal spread - Usually spares palms/soles Diagnosis - Polymerase chain reaction - Acute & convalescent serology for Antimeasles IgM & IgG Prevention - Live attenuated measles vaccine Treatment - Supportive care - Vitamin A for hospitalized children Complication - Otitis media - Pneumonia Neurologic - Encephalitis (within days) - Acute disseminated encephalomyelitis (within weeks) - Subacute sclerosing panencephalitis (within years) - Gastroenteritis Rubella (German measles) – Togavirus SS +RNA Clinical Presentation Congenital disease: - Sensorineural hearing loss - Intellectual disability - Cardiac anomalies - Cataracts, glaucoma Children: - Low-grade fever - Conjunctivitis, coryza, cervical lymphadenopathy, Forschemier spots - Cephalocaudal spread of blanching, erythematous maculopapular rash Adolescents/Adults: Same as children _ arthralgia/arthritis Diagnosis - Polymerase Chain Reaction - Acute & Convalescent serology for anti-rubella IgM & IgG Prevention - Live attenuate rubella vaccine Treatment - Supportive care Beckwith-Weidman syndrome Pathogenesis - Deregulation of imprinted gene expression in chromosome 11p15**** à IGF-2 Physical Examination - Fetal macrosomia, rapid growth until late childhood - Omphalocele or umbilical hernia - Macroglossia - Hemihyperplasia Complications - Monitor closely for hypoglycemia - Wilms tumor** - Hepatoblastoma Surveillance - Serum alpha fetoprotein - Abdominal/renal ultrasound 3 Differential Diagnosis of Regurgitation & vomiting in infants Diagnosis Clinical features Management Gastroesophageal reflux - Physiologic - Asymptomatic - “Happy spitter” - Reassurance - Positioning therapy - Pathologic (GERD) - Failure to thrive - Significant irritability - Sandifer Syndrome - Thickened feed - Antacid therapy - If severe, esophageal pH probe monitoring & upper endoscopy Milk-Protein Allergy - Regurgitation/vomiting - Eczema - Bloody stools - Elimination of dairy & soy protein from diet Pyloric Stenosis - Projectile vomiting - Olive-shaped abdominal mass - Dehydration, weight loss - Abdominal ultrasound - Pylormyotomy Prader-Willi Syndrome Clinical Features - Hypotonia - Weak suck/feeding problems in infancy - Hyperphagia/obesity - Short stature - Hypogonadism - Intellectual disability - Dysmorphic facies: Narrow forehead, Almond-shaped eyes, Downturned mouth Diagnosis - Deletion on paternal 15q11-q13 Complications - Sleep apnea - Type 2 DM - Gastric distension/rupture - Death by choking Differential Diagnosis of Otalgia Diagnosis Clinical Features Acute Otitis Media - Middle ear effusion plus acute eardrum inflammation (eg, bulging ear drum, fever) Otitis Media w/effusion - Middle ear effusion without acute inflammation Bullous Myringitis - Serous liquid filled blisters on the tympanic membrane Cerumen Impaction - Liquid or hard wax in auditory canal obstructing eardrum visualization Hemotympanum - Purple or red eardrum +/- bulging Otitis externa - Pain with tragal traction, erythematous & swollen external auditory canal +/- otorrhea 4 Acute Otitis Media Microbiology - Streptococcus pneumonia - Nontypable Haemophilus influenza - Moraxella catarrhalis Clinical Features - Middle ear effusion - PLUS - Bulging tympanic membrane Treatment - Initial: Amoxicillin - 2nd Line: Amoxicillin-clavulanic acid Complication - Conductive hearing loss - Mastoiditis - Meningitis Otitis Externa Risk Factors - Trauma/foreign material (eg, cotton swab, hearing aid) - Exposure to outdoor water sources (eg, swimming) - Skin disruption (eg, psoriasis, eczema, contact dermatitis) Clinical Manifestations - Pruritus, pain & discharge, hearing loss - Tenderness with tragal pressure/auricle manipulation - Ear canal with erythema edema & cerumen/purulent debris Management - Remove debris from canal (eg, wire loop) - Ototopical corticosteroid (inflammation) plus antibiotic (infection) - Culture of exudate in recalcitrant cases Gaucher Disease Etiology - AR, ↑prevalence in Ashkenazi Jews - Glucocerebrosidase deficiency à gluocerebroside accumulation in macrophages Typical Features - Sever splenomegaly - Anemia, thrombocytopenia - Bony pain - FTT, delayed puberty Management - Enzyme Replacement 5 Cyanotic heart disease in newborns Diagnosis Examination X-ray FIndings Transposition of the Great Vessels - Single S2 - +/- VSD - “Egg on a String Heart” (narrow mediastinum) Tetralogy of Fallot - Harsh pulmonic stenosis murmur - VSD murmur - “Bootshaped” heart (RV hypertrophy) Tricuspid atresia - Single S2 - VSD murmur - Minimal pulmonary blood flow Truncus Arteriosus - Single S2 - Systolic ejection murmur (decreased flow through truncal valve) - Increased pulmonary blood flow, edema Total Anomalous venous return with obstruction - Severe cyanosis - Respiratory Distress - Pulmonary edema, “snowma” sign (enlarged supracardiac veins & SVC) Pediatric Viral Myocarditis Etiology - Coxsackie B Virus - Adenovirus Clinical Presentation - Viral prodrome - Heart failure: Dyspnea, syncope, tachycardia, nausea, vomiting, hepatosplenomegaly Diagnostic Studies - Chest x-ray: - Cardiomegaly - Pulmonary edema - ECG Sinus Tachycardia - Echocardiogram - Decreased ejection fraction - Diffuse hypokinesis - Endomyocardial biopsy: (Gold standard) Inflammatory infiltrate of the myocardium with myocyte necrosis Prognosis - Mortality - Newborns: ~75% - Older infants/children: ~25% - Outcome of survivors - Full recovery within 203 months ~60% - Dilated cardiomyopathy/CHF ~33% Neonatal Conjunctivitis Type Age of Onset Findings Treatment Chemical - < 24 hr - Frequently occurs after application of silver nitrate prophylaxis - Mild conjunctiva irritation/injection & tearing after silver nitrate ophthalmic prophylactics - Eye lubricant Gonococci - 2-5 days - Marked eyelid swelling, profuse purulent discharge, corneal edema/ulceration - IV or IM ceftriaxone or cefoxaime Chlamydial - 5-14 days - Eyelid swelling, chemosis; watery, bloody, or mucopurulent eye discharge - Oral erythromycin 6 Risk factors for brain abscess Predisposing Problem Pathogenesis Affected Area Otitis media, mastoiditis - Direct Spread - Temporal lobe, cerebellum Frontal/Ethmoid Sinusitis - Direct Spread - Frontal Lobe Dental infection - Direct Spread - Frontal Lobe Bacteremia from other sites of infection, cyanotic heart disease - Hematogenous Spread - Multiple abscesses along distribution of middle cerebral artery (gray white junction) [Show More]
Last updated: 2 years ago
Preview 1 out of 53 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 03, 2021
Number of pages
53
Written in
Additional information
This document has been written for:
Uploaded
Apr 03, 2021
Downloads
0
Views
89


 Graded A.png)
.png)