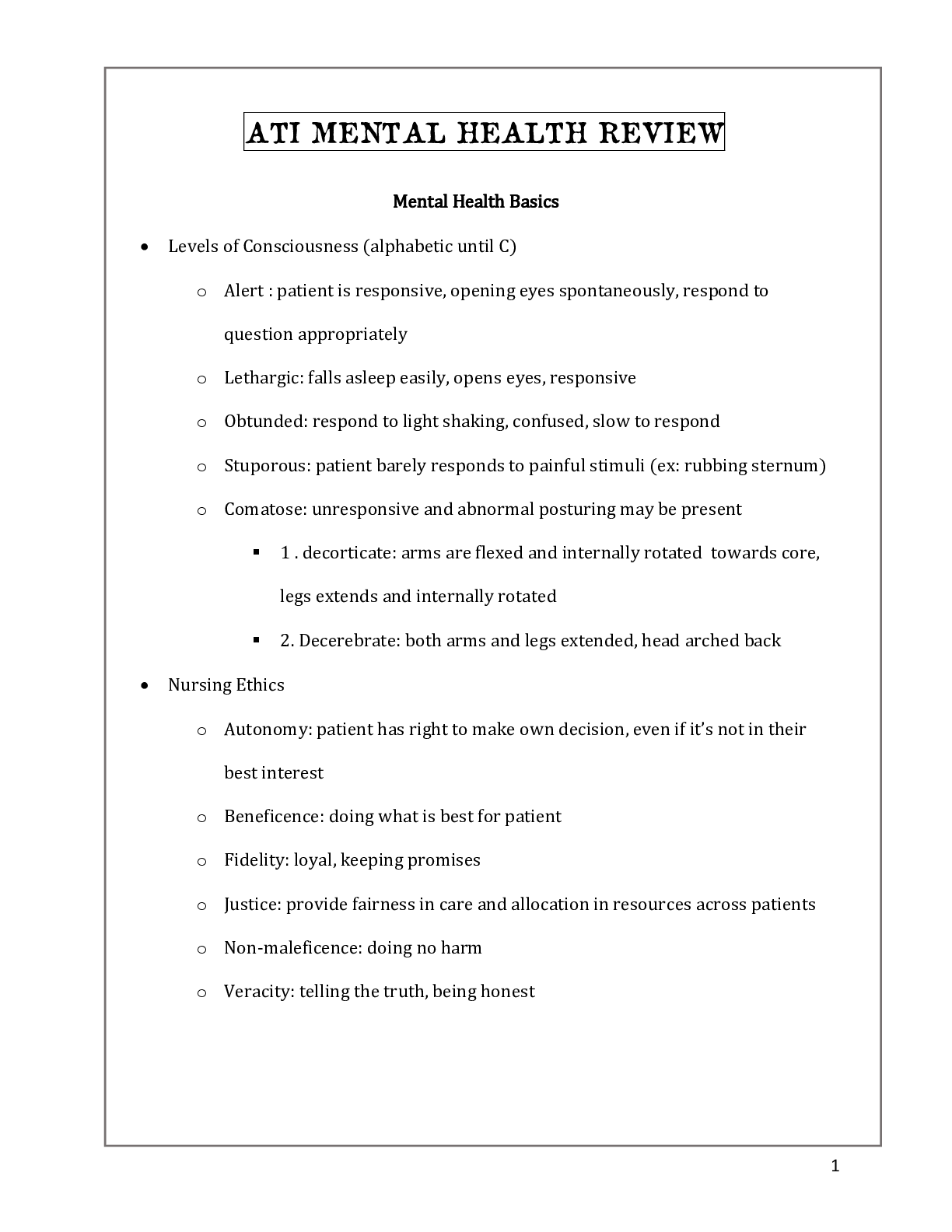
Mental Health Basics
Levels of Consciousness (alphabetic until C)
o Alert : patient is responsive, opening eyes spontaneously, respond to question
appropriately
o Lethargic: falls asleep easily, opens eyes, respons
...
Mental Health Basics
Levels of Consciousness (alphabetic until C)
o Alert : patient is responsive, opening eyes spontaneously, respond to question
appropriately
o Lethargic: falls asleep easily, opens eyes, responsive
o Obtunded: respond to light shaking, confused, slow to respond
o Stuporous: patient barely responds to painful stimuli (ex: rubbing sternum)
o Comatose: unresponsive and abnormal posturing may be present
1 . decorticate: arms are flexed and internally rotated towards core, legs
extends and internally rotated
2. Decerebrate: both arms and legs extended, head arched back
Nursing Ethics
o Autonomy: patient has right to make own decision, even if it’s not in their best
interest
o Beneficence: doing what is best for patient
o Fidelity: loyal, keeping promises
o Justice: provide fairness in care and allocation in resources across patients
o Non-maleficence: doing no harm
o Veracity: telling the truth, being honest
Patient rights
o Right to refuse treatment – applies to patients who are involuntary admitted
o Confidentiality: patients medical information is protected by HIPPA and cannot
be released unless permission given
o Mandatory reporting: nurses are required to report suspicion of abuse, and to
warn/protect third parties who are at risk for harm.
Informed Consent:
o Provider Responsibilities:
Communicates purpose of procedure, and complete description of
procedure in the patient’s primary language
Explain risks vs. benefits
Describe other options to treat condition
o RN
Make sure provider gave the patient the above information
Ensure the patient is competent to give informed consent (i.e. patient is
an adult or emancipated minor, not impaired)
Have patient sign consent document
Notify provider if patient has more questions or doesn’t understand any
information
Restraints:
o Always have alternatives before restraints.
o Can do restraint in emergency BUT need written prescription from provider
quickly after (1hr)
1
ATI
MENTAL
o Provider will need to re-write prescription every 24 hours, no PRN prescription
o Best Practice:
Wrist – two fingers
Quick release knot (slip knot, NOT SQURE)
Use a movable part of the bed frame so if you move the bed the
restraints move with them
o Types of restraints: physical (vest, belt, mitten) or chemical (sedative or
antipsychotic medication)
o Alternatives: provide verbal interventions, diversions, calm/quiet environment
o Prescription:
Prescription must be in writing
If need for constraints continue, provider must re-write prescription every
24 hours
In an emergency situation, a nurse can use restraints but must obtain a
written prescription per facility policy (15-30 minutes)
o Time limits:
Adults: 4 hours
9-17: 2 hours
<8: 1 hour
o Documentation:
Complete every 15 -30 minutes
Include: precipitating event, alternative interventions attempted,
time treatment began, medication administered, patient
assessment (current behavior, VS<, pain), patient are provided
(food, toileting)
o DC: restraints can be discontinued when patient can follow the nurses’ direction
Torts
o Unintentional Torts
Negligence: forgetting to set bed alarm for a patient at risk for falls
Malpractice: medication error that harms patient
o Intentional torts:
Assault: nurse threatens patient
Battery: nurse hits patients or administer medication against patients will
False imprisonment: nurse inappropriately restrains a patient or
administers a chemical restraint such as a sedative
Communication
o Intrapersonal communication: “self-talk”, thinking thoughts, but not verbalizing
them
o Interpersonal communication: one-on-one communication with another person
o Open-ended questions: promotes interactive discussions
o Closed-ended questions: used to obtain, specific data. Use sparingly as it can
block further communication.
Communication techniques
2
ATI
MENTAL
o Restating: repeat the patients exact words
o Reflecting: return focus back to patient
o Paraphrasing: restate patient’s feelings to confirm understanding of what patient
is saying
o Exploring: gathering more information about something patient has mentioned
o General leads: allows patient to guide discussion
o Presenting reality: communicate what is actually happening; dispel
hallucinations, delusions, false beliefs.
o Offering self: limited self-disclosure by nurse. Return focus to patient as soon as
possible.
Therapeutic communication
o WRONG
Asking why
Offering your opinion
Giving false reassurance
Giving advice
Changing the subject
Minimizing the patients feelings
o RIGHT
Asking open-ended questions
Maintaining eye contact
Sitting/standing at eye level
Therapeutic tough to convey caring and provide comfort
o Older adults:
Minimize distractions, discuss health in private settings
Face the patient when speaking
Use a lower pitch voice
Begin the interview by asking the patient to identify his/her needs and
concerns
Limit the number of items on a questionnaire when gathering data
Allow plenty of time for the patient to respond to questions.
Defense Mechanisms
o Altruism: dealing w/ stress/anxiety by helping others
o Sublimation: substitute negative impulses into acceptable forms of expression
(ex: working out hard at the gm)
o Suppression: voluntary denial of unpleasant thoughts or feelings
o Repression: unconscious denial of unpleasant thoughts or feelings
o Regression: reverting back to childlike behaviors that are inappropriate for the
patient’s current development level
o Displacement: redirecting feelings about a person or situation towards a less
threatening object/person (ex: dad loses his job, destroys his childs toy)
o Reaction formation: demonstrating the opposite behavior vs what is actually felt
(I love nursing exams)
3
ATI
MENTAL
o Undoing: performing an act to make up for a previous behavior
o Rationalization: creating an acceptable excuse for unacceptable behavior
o Dissociation: temporary compartmentalization of feelings/thoughts (forgettin
who you are during sexual assault)
o Denial: pretending truth is not reality
o Compensation: emphasizing strengths to make up for weaknesses
Anxiety
o Levels of anxiety
Mild: enhances an individuals perception. Normal experience.
Symptoms: restlessness, irritability, fidgeting, foot-tapping
Moderate: slightly reduced perception and ability to think
Symptoms: pacing, difficulty concentrating; increased RR, HR,
Severe: perception greatly reduced; no ability to problem-solve
Symptoms: feelings of “doom”, tachycardia, hyperventilation,
rapid speech
Panic level: individual loses touch with reality disturbed behaviors
Symptoms: dilated pupils, hallucinations, severe withdrawal,
severe shakiness
o Nursing interventions
Mild/moderate anxiety: active listening, evaluate patients past coping
mechanisms, assist patient w/ problem solving, teach relaxation
techniques (ex: abdominal breathing exercises), encourage exercise to
reduce anxiety
Severe/panic-level anxiety: provide a quiet environment w/ minimal
stimulation, remain with patient, set limits with short/simple statements,
help patient to focus on reality. Problem solving is NOT realistic at this
level of anxiety.
Therapeutic Relationship
o Orientation: introduce self, discuss confidentiality, establish expectations and
boundaries/parameters, identify patients needs and set goals.
o Working: perform on-going assessments, assist patient with problem solving and
behavior changes, evaluate coping strategies used by patient in the past,
introduce patient to others on the unit, revise goals and plans as needed,
support patients use of new coping skills.
o Termination: summarize goals and achievements, allow patient to share feelings
about termination of relationship, discuss ways for patient to incorporate new
healthy behaviors into his/her life.
Transference and Countertransference
o Transference: occurs when a patient views the nurse as being similar to an
important person in his/her life (often a person of authority). Can result in
patient treating nurse like this individual.
4
ATI
MENTAL
o Countertransference: occurs when the patient reminds the nurse of someone in
his/her life, which induces strong personal feelings and may cause the nurse to
treat the patient differently.
Prevention
o Primary: focus on prevention of MH problems (community education, programs)
o Secondary: focus on early detection and screening for mental illness (screening
for depression in older adults)
o Tertiary: focus on rehabilitation and prevention of complications in patients who
have already been diagnosed w/ mental illness (support group for those w/
substance abuse disorder)
Non-pharmacological Therapies
Psychoanalysis: assesses unconscious thoughts and feelings. Based on belief that
internal conflicts stem from early childhood experiences. Focuses on past relationships.
Cognitive reframing: identifies negative thoughts, examines the cause, and replaces
negative self-talk with healthier and more constructive thinking (i.e. positive self
statements)
o Includes: priority restructuring, journal keeping, assertiveness training,
monitoring thoughts
Behavioral therapies
o Modeling: therapist serves as a role model for patient. Demonstrates appropriate
behavior.
o Operant conditioning: provides positive rewards for desired behavior.
o Systemic desensitization: progressive exposure to anxiety causing stimuli while
using relaxation therapies.
o Aversion therapy: punishment for maladaptive behavior (ex: bitter taste, mild
shock) to promote behavior change.
o Others: guided imagery, biofeedback, thought stopping, muscle relaxation.
Group therapy:
o Goals: allows members to share common feelings and experiences, learn
alternative ways to solve problems.
Silent member: divide group into pairs to discuss topic, then summarizes
discussion to group
Member constantly talking: ask group to discuss their feelings regarding
the member’s monopolizing behavior
Angry/agitated member: move group members away from member to
prevent injury.
Electroconvulsive therapy (ECT)
o ECT: use of electrical activity to induce a seizure, which may enhance the effects
of NT in the brain
o Performed 2-3 times a week for a total of 6-12 treatments.
o Indications: major depressive disorder (used in conjunction with antidepressants,
does not replace medication therapy). Schizophrenia, acute manic episodes
o Medications:
[Show More]