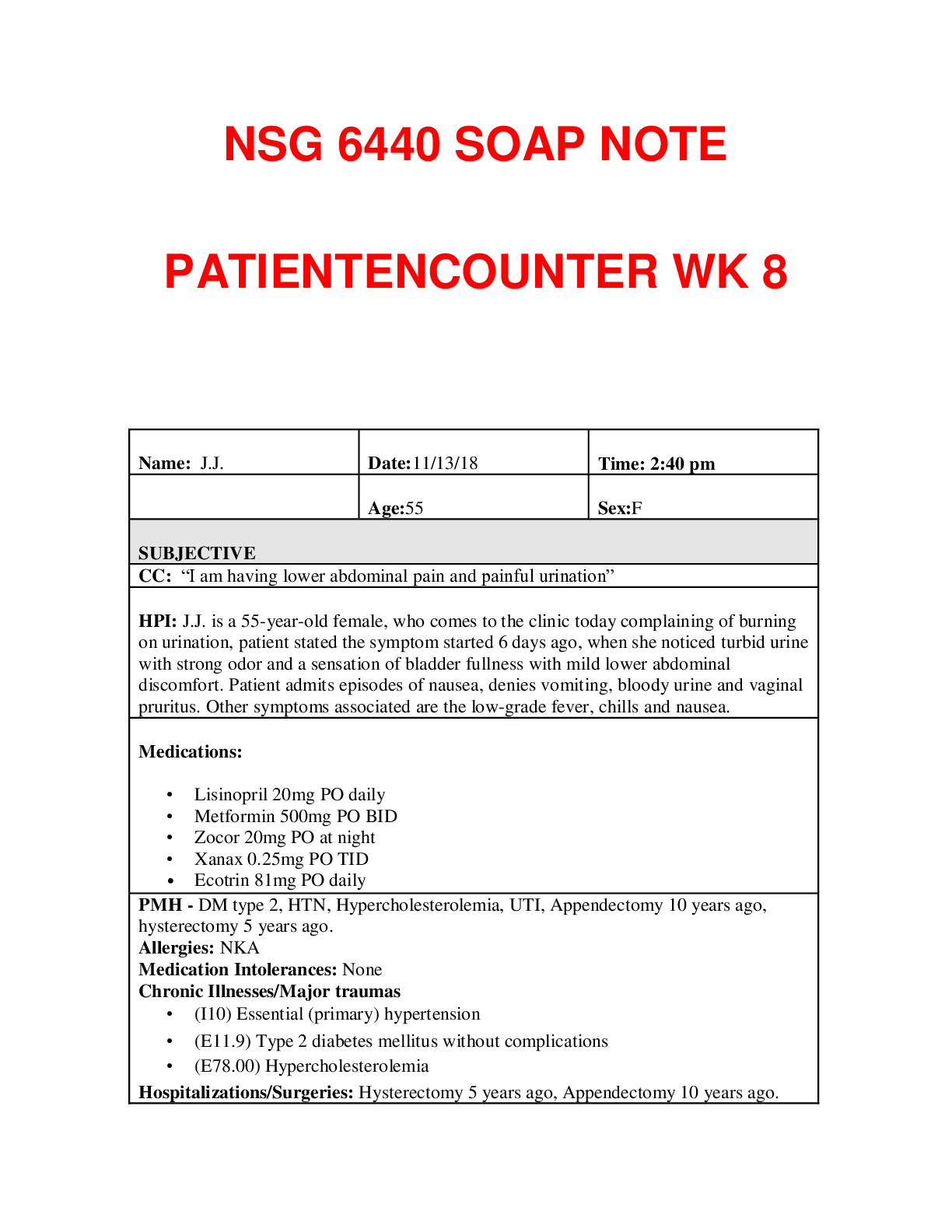
Family History.: Father (dead) Stroke; Mother (Alive) DM, MI; Son (Alive) HTN; Daughter (Alive) healthy. Social History. Patient has a high school education, and now is working for a home health agency. She also reports
...
Family History.: Father (dead) Stroke; Mother (Alive) DM, MI; Son (Alive) HTN; Daughter (Alive) healthy. Social History. Patient has a high school education, and now is working for a home health agency. She also reports she is not getting a good benefits from working. She is widow, and lives with her daughter and her son in law. Denies alcohol, tobacco use, or illegal drugs. They live in a safe neighborhood. She normally makes a regular checkup for her chronic health conditions.
Diet: She sttes try to eat healthy stuff when I have te She drinks 3 cups of coffee every day. She does not have restrictions on sodium intake, carbohydrates and fats. Exercise and Leisure: She does not do any exercises.
Sleep: The patient stated that she sleeps well
Immunization: Received flu vaccine in October 2018
Environmental hazard: Patient denies
ROS
General. Patient is complaining of low- grade fever and chills. Reports gaining 5 lbs. over the last two months.
Cardiovascular.Denies chest pain, palpitations, PND, orthopnea, edema
Skin.Denies delayed healing, rashes, bruising, bleeding or skin discolorations, any changes in lesions or moles
Respiratory.Denies cough, wheezing, hemoptysis, dyspnea, pneumonia hx, TB
Eyes. She admits to wear corrective lenses. Denies double vision.
Gastrointestinal. Patient is complaining of nausea and suprapubic pain. Denies constipation, hepatitis, hemorrhoids, eating disorders, ulcers, or black tarry or bloody stools.
Ears.Denies ear pain, hearing loss, ringing in ears, or discharge.
Genitourinary/Gynecological.Patient admits to have burning during urination, urine with strong odor, she also feels a sensation of bladder fullness with mild lower abdominal discomfort. Denies any bloody urine and fever or chills. Denies
[Show More]




_removed.png)

.png)













