*NURSING > EXAM > Peds_Maternity HESI & Obstetrics Q & A Latest 2021 / 2022 | (GUARANTEED PASS). (All)
Peds_Maternity HESI & Obstetrics Q & A Latest 2021 / 2022 | (GUARANTEED PASS).
Document Content and Description Below
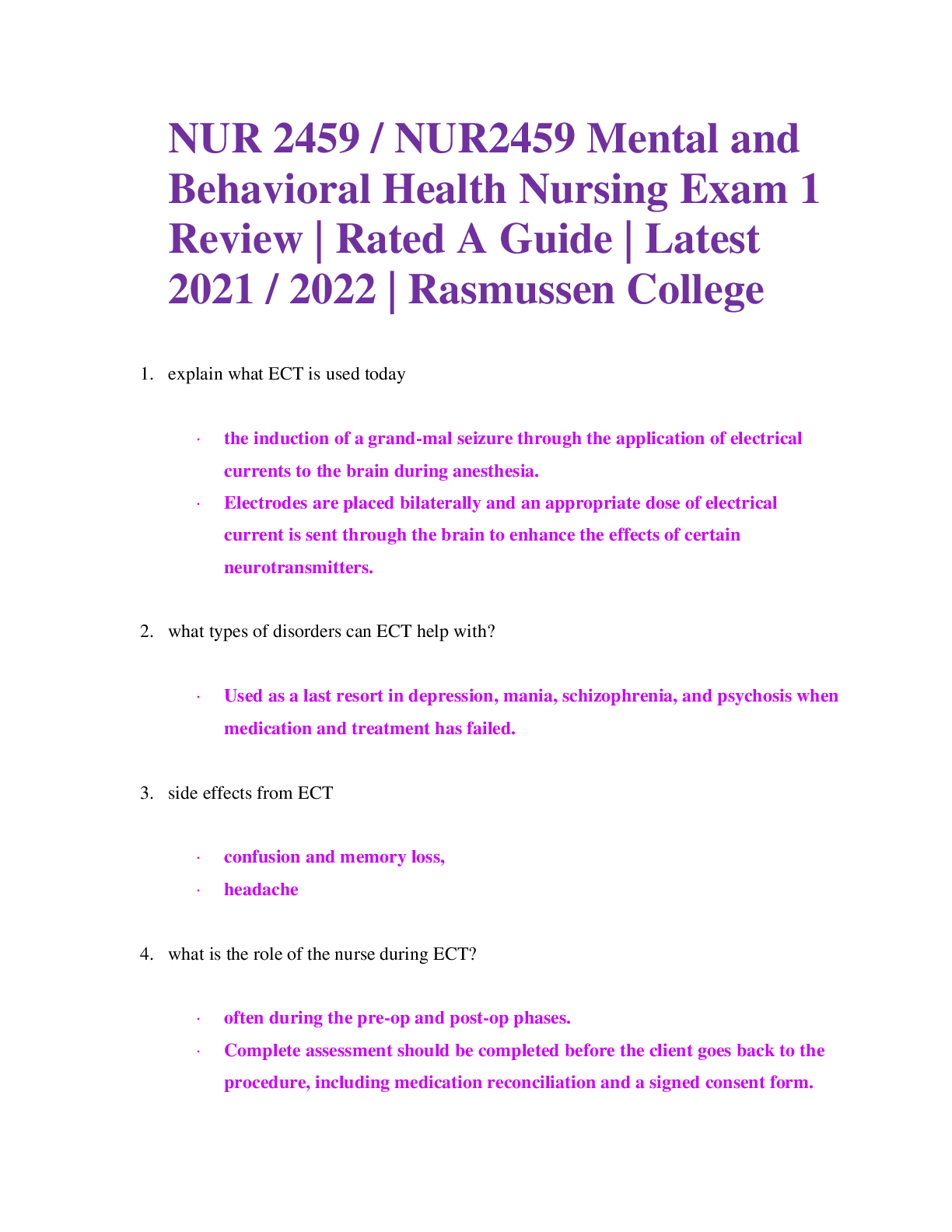
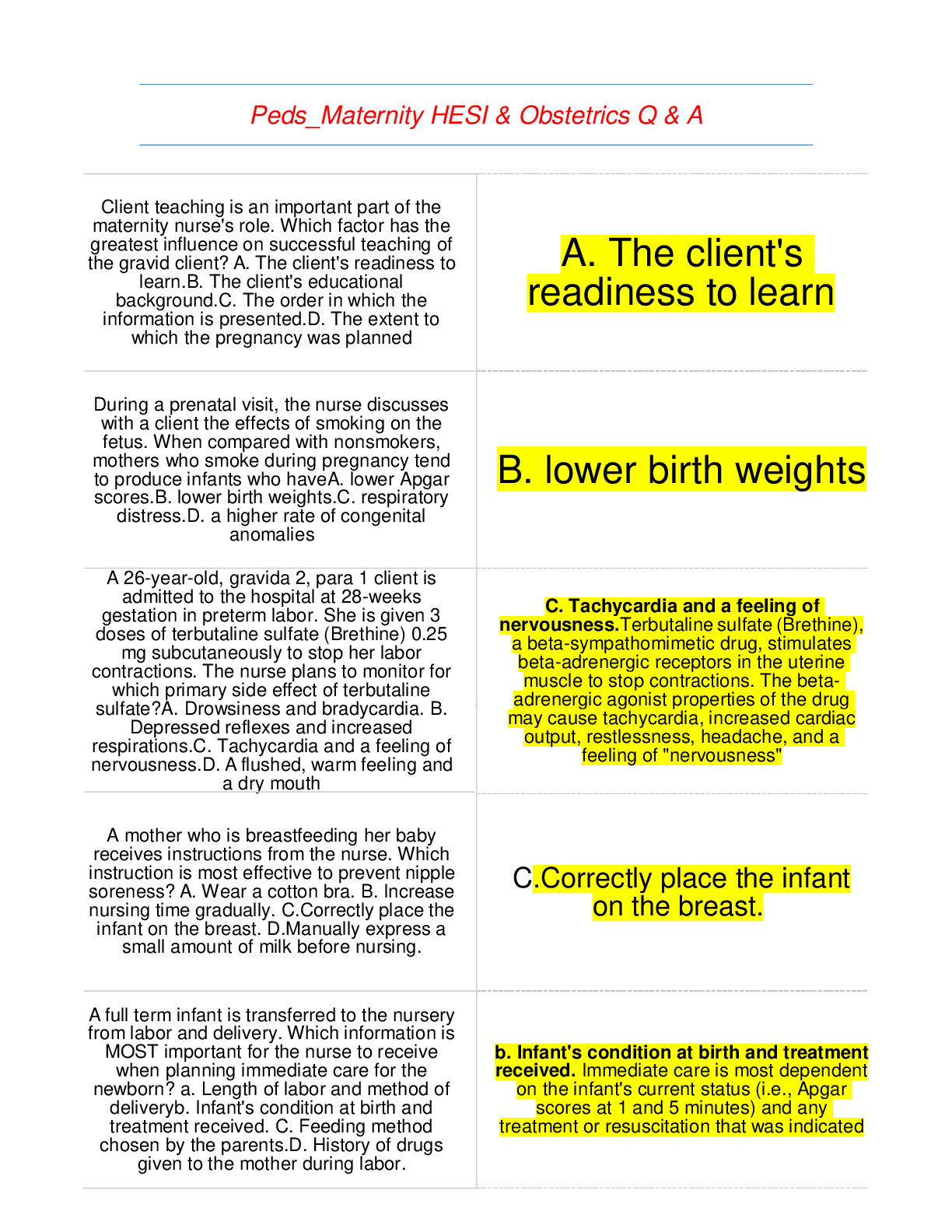
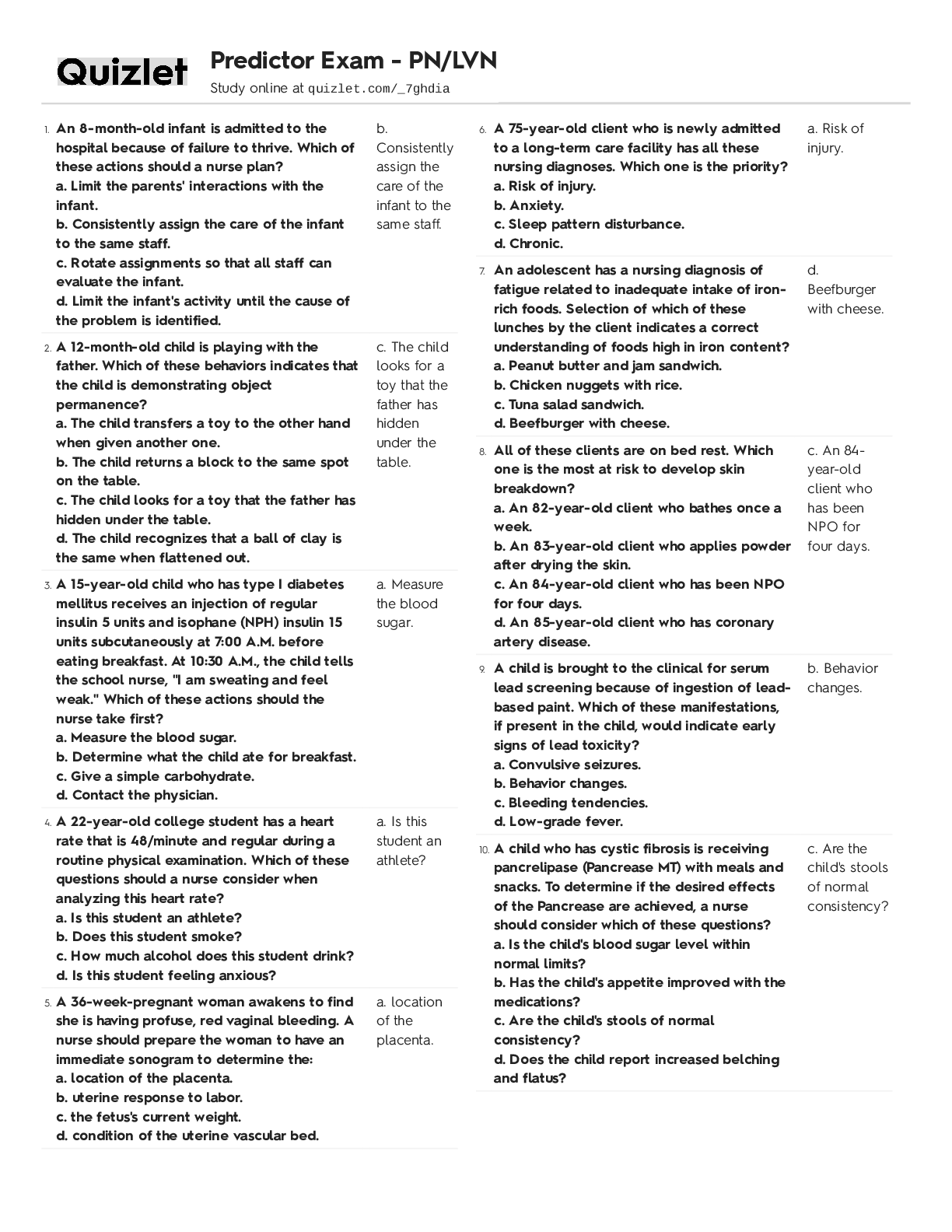
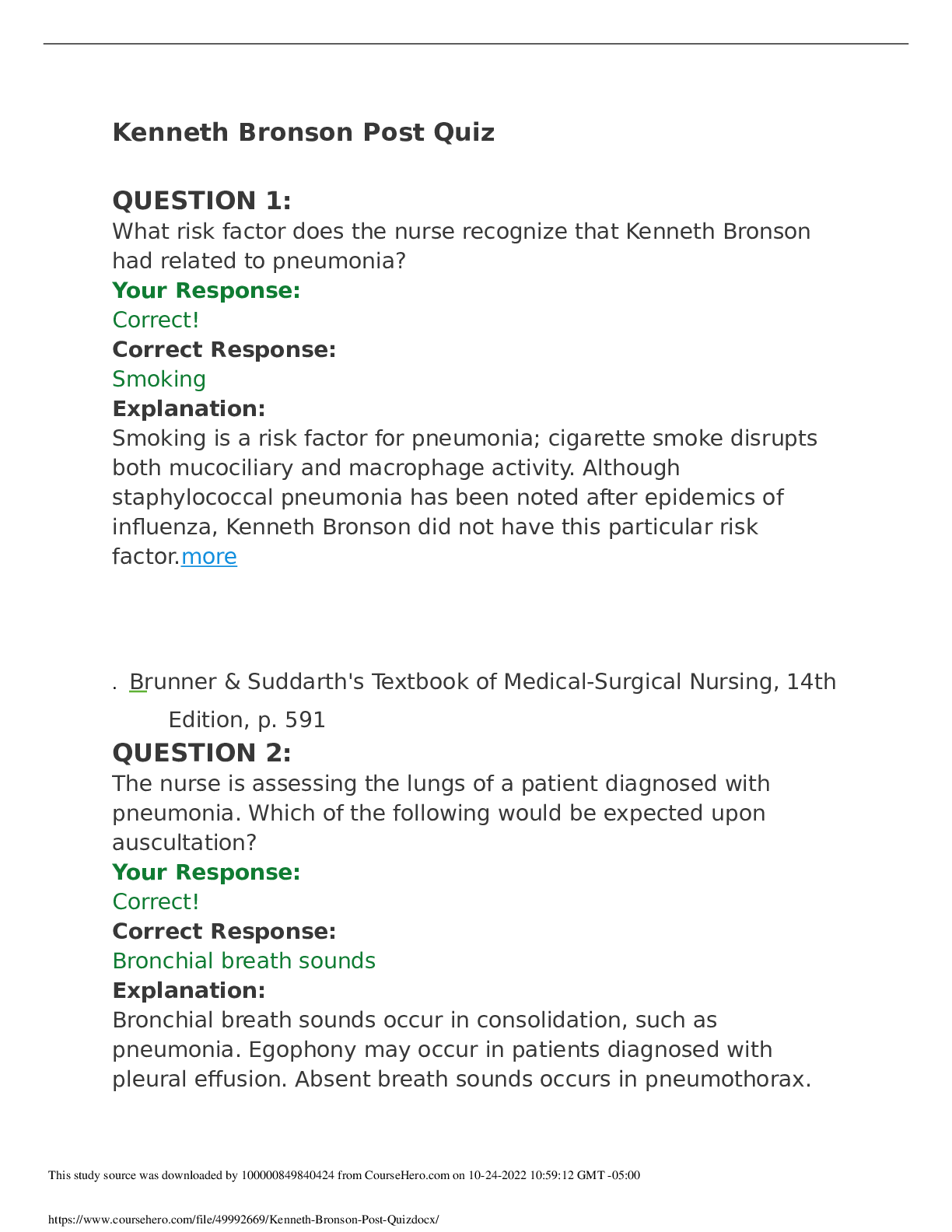
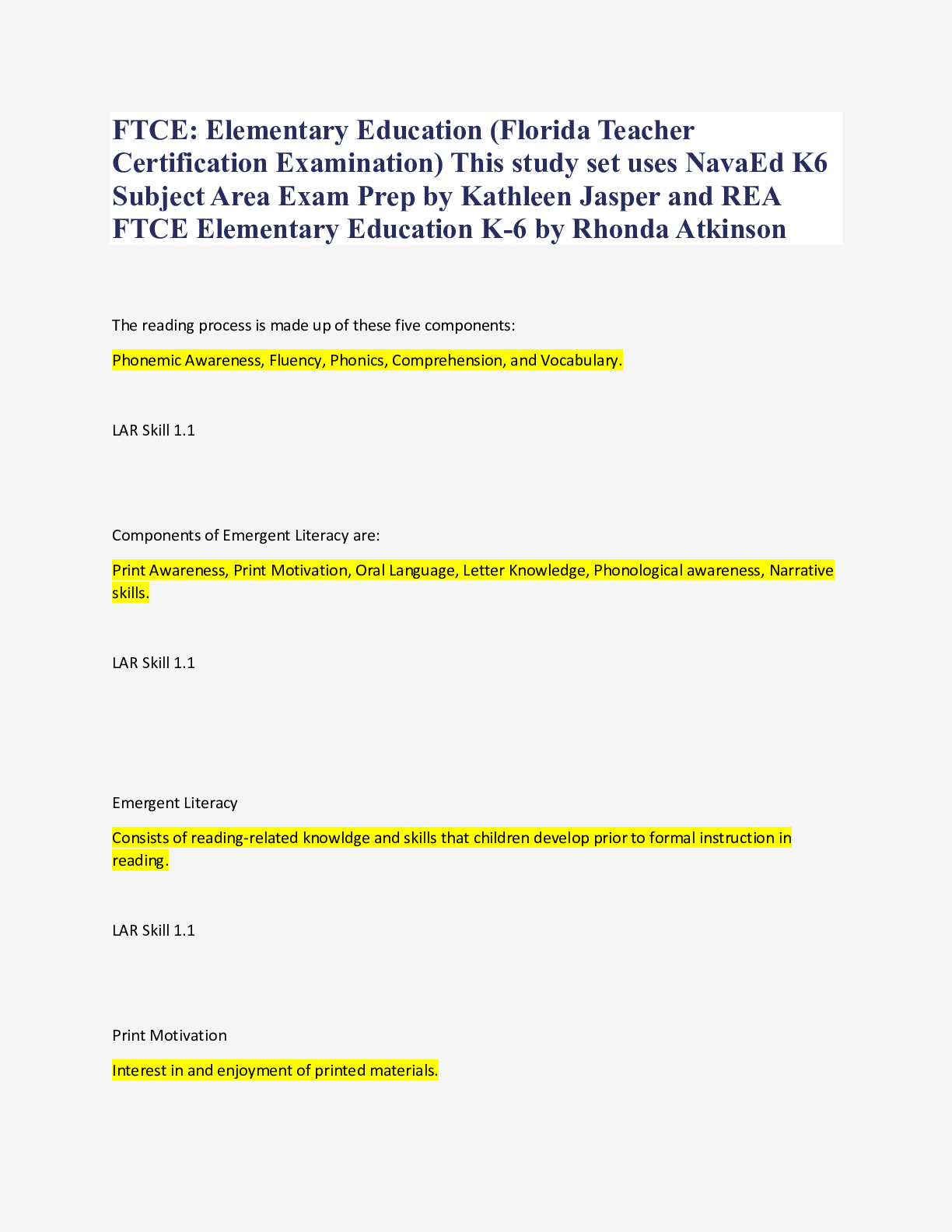
Client teaching is an important part of the maternity nurse's role. Which factor has the greatest influence on successful teaching of the gravid client? A. The client's readiness to learn.B. The clien... t's educational background.C. The order in which the information is presented.D. The extent to which the pregnancy was planned A. The client's readiness to learn During a prenatal visit, the nurse discusses with a client the effects of smoking on the fetus. When compared with nonsmokers, mothers who smoke during pregnancy tend to produce infants who haveA. lower Apgar scores.B. lower birth weights.C. respiratory distress.D. a higher rate of congenital anomalies B. lower birth weights A 26-year-old, gravida 2, para 1 client is admitted to the hospital at 28-weeks gestation in preterm labor. She is given 3 doses of terbutaline sulfate (Brethine) 0.25 mg subcutaneously to stop her labor contractions. The nurse plans to monitor for which primary side effect of terbutaline sulfate?A. Drowsiness and bradycardia. B. Depressed reflexes and increased respirations.C. Tachycardia and a feeling of nervousness.D. A flushed, warm feeling and a dry mouth A mother who is breastfeeding her baby receives instructions from the nurse. Which instruction is most effective to prevent nipple soreness? A. Wear a cotton bra. B. Increase nursing time gradually. C.Correctly place the infant on the breast. D.Manually express a small amount of milk before nursing. C. Tachycardia and a feeling of nervousness.Terbutaline sulfate (Brethine), a beta-sympathomimetic drug, stimulates beta-adrenergic receptors in the uterine muscle to stop contractions. The beta- adrenergic agonist properties of the drug may cause tachycardia, increased cardiac output, restlessness, headache, and a feeling of "nervousness" C.Correctly place the infant on the breast. A full term infant is transferred to the nursery from labor and delivery. Which information is MOST important for the nurse to receive when planning immediate care for the newborn? a. Length of labor and method of deliveryb. Infant's condition at birth and treatment received. C. Feeding method chosen by the parents.D. History of drugs given to the mother during labor. b. Infant's condition at birth and treatment received. Immediate care is most dependent on the infant's current status (i.e., Apgar scores at 1 and 5 minutes) and any treatment or resuscitation that was indicated In developing a teaching plan for expectant parents the nurse plans to include formation about when the parents can expect the infants fontanels to close. The nurse bases the explanation on knowledge that for the normal newborn, the A. anterior fontanel closes at 2 to 4 months and the posterior by the end of the first week. B. anterior fontanel closes at 5 to 7 months and the posterior by the end of the second week. C. anterior fontanel closes at 8 to 11 months and the posterior by the end of the first month. D. anterior fontanel closes at 12 to 18 months and the posterior by the end of the second month When assessing a client who is at 12 week gestation, the nurse recommends that she and her husband consider attending childbirth preparation classes. When is the best time for the couple to attend these classes?A. at 16 weeks gestationB.at 20 weeks gestation C. at 24 weeks gestation D. at 30 weeks gestation D. anterior fontanel closes at 12 to 18 months and the posterior by the end of the second month D. at 30 weeks gestationclosest (of the options) to the time parents would be ready for such classes. Learning is facilitated by an interested pupil! The couple is most interested in childbirth toward the end of the pregnancy when they are psychologically ready for the termination of the pregnancy, and the birth of their child is an immediate concern. The nurse should encourage the laboring client to begin pushing when A.there is only an anterior or posterior lip of cervix left. B.the client describes the need to have a bowel movement. C.the cervix is completely dilated.D.the cervix is completely effaced C.the cervix is completely dilated.Pushing begins with the second stage of labor, i.e., when the cervix is completely dilated at 10 cm (C). If pushing begins before the cervix is completely dilated the cervix can become edematous and may never completely dilate, necessitating an operative delivery. Many primigravidas begin active labor 100% effaced and then proceed to dilate The nurse is counseling a couple who has sought information about conceiving. For teaching purposes, the nurse should know that ovulation usually occurs A.two weeks before menstruation.B.immediately after menstruation. immediately before menstruation.C. immediately before menstruation.D. three weeks before menstruation. A.two weeks before menstruationOvulation occurs 14 days before the first day of the menstrual period. While ovulation can occur in the middle of the cycle, or 2 weeks after menstruation, this is only true for a woman who has a perfect 28-day cycle. For many women, the length of their menstrual cycle varies. The nurse instructs a laboring client to use accelerated blow breathing. The client begins to complain of tingling finger and dizziness. What action should the nurse take?a. administer o2 by face maskb. notify the HCP for the client's syndrome c. have the client breathe into her cupped hands d. check the client's BP and fetal HR/ c. have the client breathe into her cupped hands Tingling fingers and dizziness are signs of hyperventilation (blowing off too much carbon dioxide). Hyperventilation is treated by retaining carbon dioxide. This can be facilitated by breathing into a paper bag or cupped hands. When preparing a class on newborn care for expectant parents, what content should the nurse teach concerning the newborn infant born at term gestation? A.Milia are red marks made by forceps and will disappear within 7 to 10 days. B.Meconium is the first stool and is usually yellow gold in color. C.Vernix is a white, cheesy substance, predominantly located in the skin folds. D.Pseudostrabismus found in newborns is treated by minor surgery. Twenty-four hours after admission to the newborn nursery, a full-term male infant develops localized edema on the right side of his head. The nurse knows that, in the newborn, an accumulation of blood between the periosteum and skull which does not cross the suture line is a newborn variation known as: C.Vernix is a white, cheesy substance, predominantly located in the skin folds. a cephalhematoma, caused by forceps trauma and may last up to 8 weeks.Cephalhematoma, a slight abnormal variation of the newborn, usually arises within the first 24 hours after delivery. Trauma from delivery causes capillary bleeding between the periosteum and the skull. An expectant father tells the nurse he fears that his wife "is losing her mind." He states she is constantly rubbing her abdomen and talking to the baby, and that she actually reprimands the baby when it moves too much. What recommendation should the nurse make to this expectant father? A. Reassure him that these are normal reactions to pregnancy and suggest that he discuss his concerns with the childbirth education nurse. B.Help him to understand that his wife is experiencing normal symptoms of ambivalence about the pregnancy and no action is needed. C. Ask him to observe his wife's behavior carefully for the next few weeks and report any similar behavior to the nurse at the next prenatal visit. D.Let him know that these behaviors are part of normal maternal/fetal bonding which occur once the mother feels fetal movement. A new mother who has just had her first baby says to the nurse, "I saw the baby in the recovery room. She sure has a funny looking head." Which response by the nurse is best? A.This is not an unusual shaped head, especially for a first baby. B.It may look funny to you, but newborn babies are often born with heads like your baby's. C. That is normal; the head will return to a round shape within 7 to 10 days. D.Your pelvis was too small, so the baby's head had to adjust to the birth canal. A new mother asks the nurse, "How do I know that my daughter is getting enough D.Let him know that these behaviors are part of normal maternal/fetal bonding which occur once the mother feels fetal movement.These behaviors are positive signs of maternal/fetal bonding. C. That is normal; the head will return to a round shape within 7 to 10 days. breast milk?" Which explanation should the nurse provide? A.Weigh the baby daily, and if she is gaining weight, she is eating enough. B.Your milk is sufficient if the baby is voiding pale straw-colored urine 6 to 10 times a day.C.Offer the baby extra bottle milk after her feeding, and see if she is still hungry. D.If you're concerned, you might consider bottle feeding so that you can monitor her intake. A client who gave birth to a healthy 8 pound infant 3 hours ago is admitted to the postpartum unit. Which nursing plan is best in assisting this mother to bond with her newborn infant? A. Encourage the mother to provide total care for her infant. B. Provide privacy so the mother can develop a relationship with the infant. C. Encourage the father to provide most of the infant's care during hospitalization.D.Meet the mother's physical needs and demonstrate warmth toward the infant. A couple, concerned because the woman has not been able to conceive, is referred to a healthcare provider for a fertility workup and a hysterosalpingography is scheduled. Which postprocedure complaint indicates that the fallopian tubes are patent? A.Back pain B.Abdominal pain.C.Shoulder pain.D. Leg cramps. D.Meet the mother's physical needs and demonstrate warmth toward the infant.It is most important to meet the mother's requirement for attention to her needs so that she can begin infant care-taking. Nurse theorist Reva Rubin describes the initial postpartal period as the "taking-in phase," which is characterized by maternal reliance on others to satisfy the needs for comfort, rest, nourishment, and closeness to families and the newborn C.Shoulder pain.If the tubes are patent (open), pain is referred to the shoulder from a subdiaphragmatic collection of peritoneal dye/gas. Which nursing intervention is most helpful in relieving postpartum uterine contractions or "afterpains?" a. lying prone with a pillow on the abdomenb. using a breast pumpc. massaging the abdomend. giving oxytocic medications a. lying prone with a pillow on the abdomen Which maternal behavior is the nurse most likely to see when a new mother receives her infant for the first time?a. She eagerly reaches for the infant, undresses the infant, and examines the infant completely. b. Her arms and hands receive the infant and she then traces the infant's profile with her fingertips.c. Her arms and hands receive the infant and she then cuddles the infant to her own body. She eagerly reaches for the infant and then holds the infant close to her own body. On admission to the prenatal clinic, a 23- year-old woman tells the nurse that her last menstrual period began on February 15, and that previously her periods were regular. Her pregnancy test is positive. This client's expected date of delivery (EDD) is a.November 22. b.November 8. c.December 22.d.October 22. b. Her arms and hands receive the infant and she then traces the infant's profile with her fingertips.Attachment/bonding theory indicates that most mothers will demonstrate behaviors described in during the first visit with the newborn, which may be at delivery or later a.November 22. correctly applies Nägele's rule for estimating the due date by counting back 3 months from the first day of the last menstrual period (January, December, November) and adding 7 days (15+7=22) A client at 32-weeks gestation is hospitalized with severe pregnancy-induced hypertension (PIH), and magnesium sulfate is prescribed to control the symptoms. Which assessment finding indicates the therapeutic drug level has been achieved? A. 4+ reflexes. B. Urinary output of 50 ml per hour. C.A decrease in respiratory rate from 24 to 16.D. A decreased body temperature. C.A decrease in respiratory rate from 24 to 16. • Magnesium sulfate, a CNS depressant, helps prevent seizures. • A decreased respiratory rate indicates that the drug is effective. (Respiratory rate below 12 indicates toxic effects.) • Urinary output must be monitored when administering magnesium sulfate and should be at least 30 ml per hour. • (The therapeutic level of magnesium sulfate for a PIH client is 4.8 to 9.6 mg/dl.) Twenty minutes after a continuous epidural anesthetic is administered, a laboring client's blood pressure drops from 120/80 to 90/60. What action should the nurse take? A. Notify the healthcare provider or anesthesiologist immediately. B.Continue to assess the blood pressure q5 minutes.C.Place the woman in a lateral position. D.Turn off the continuous epidural. C.Place the woman in a lateral position. The nurse should immediately turn the woman to a lateral position, place a pillow or wedge under the right hip to deflect the uterus, increase the rate of the main line IV infusion, and administer oxygen by face mask at 10-12 L/min. If the blood pressure remains low, especially if it further decreases, the anesthesiologist/healthcare provider should be notified immediately A client at 28-weeks gestation calls the antepartal clinic and states that she is experiencing a small amount of vaginal bleeding which she describes as bright red. She further states that she is not experiencing any uterine contractions or abdominal pain. What instruction should the nurse provide? A.Come to the clinic today for an ultrasound. B.Go immediately to the emergency room. C.Lie on your left side for about one hour and see if the bleeding stops. D.Bring a urine specimen to the lab tomorrow to determine if you have a urinary tract infection. A.Come to the clinic today for an ultrasound. • Third trimester painless bleeding is characteristic of a placenta prevue. • Bright red bleeding may be intermittent, occur in gushes, or be continuous. • Rarely is the first incidence life- threatening, nor cause for hypovolemic shock. • Diagnosis is confirmed by transabdominal ultrasound. An off-duty nurse finds a woman in a supermarket parking lot delivering an infant while her husband is screaming for someone to help his wife. Which intervention has the highest priority? A.Use a thread to tie off the umbilical cord. B.Provide as much privacy as possible for the woman. C.Reassure the husband and try to keep him calm. D.Put the newborn to breast D.Put the newborn to breastPutting the newborn to breast will help contract the uterus and prevent a postpartum hemorrhage--this intervention has the highest priority. A pregnant client with mitral stenosis Class III is prescribed complete bedrest. The client asks the nurse, "Why must I stay in bed all the time?" Which response is best for the nurse to provide this client? A.Complete bedrest decreases oxygen needs and demands on the heart muscle tissue. B.We want your baby to be healthy, and this is the only way we can make sure that will happen. C.I know you're upset. Would you like to talk about some things you could do while in bed? D.Labor is difficult and you need to use this time to rest before you have to assume all child-caring duties The nurse is teaching breastfeeding to prospective parents in a childbirth education class. Which instruction should the nurse include as content in the class? A.Begin as soon as your baby is born to establish a four- hour feeding schedule.B.Resting helps with milk production. Ask that your baby be fed at night in the nursery. C.Feed your baby every 2 to 3 hours or on demand, whichever comes first. D. Do not allow your baby to nurse any longer than the prescribed number of minutes. The nurse is teaching care of the newborn to a group of prospective parents and describes the need for administering antibiotic ointment into the eyes of the newborn. Which infectious organism will this treatment prevent from harming the infant? a.Herpes. b.Staphylococcusc.Gonorrhea.d. Syphilis. C.Feed your baby every 2 to 3 hours or on demand, whichever comes first. c.Gonorrhea.Erythromycin ointment is instilled into the lower conjunctiva of each eye within 2 hours after birth to prevent ophthalmica neonatorum, an infection caused by gonorrhea, and inclusion conjunctivitis, an infection caused by chlamydia. The infant may be exposed to these bacteria when passing through the birth canal. A newborn infant is brought to the nursery from the birthing suite. The nurse notices that the infant is breathing satisfactorily but appears dusky. What action should the nurse take first? A.Notify the pediatrician immediately. B.Suction the infant's nares, then the oral cavity. C.Check the infant's oxygen saturation rate. D.Position the infant on the right side. C.Check the infant's oxygen saturation rate. The pediatrician should be notified if the oxygen saturation rate is below 90% Just after delivery, a new mother tells the nurse, "I was unsuccessful breastfeeding my first child, but I would like to try with this baby." Which intervention is best for the nurse to implement first? A.Assess the husband's feelings about his wife's decision to breastfeed their baby. B.Ask the client to describe why she was unsuccessful with breastfeeding her last child. C.Encourage the client to develop a positive attitude about breastfeeding to help ensure success.D.Provide assistance to the mother to begin breastfeeding as soon as possible after delivery The nurse is teaching a woman how to use her basal body temperature (BBT) pattern as a tool to assist her in conceiving a child. Which temperature pattern indicates the occurrence of ovulation, and therefore, the best time for intercourse to ensure conception? A. Between the time the temperature falls and rises.B. Between 36 and 48 hours after the temperature rises. C. D.Provide assistance to the mother to begin breastfeeding as soon as possible after delivery.Infants respond to breastfeeding best when feeding is initiated in the active phase soon after delivery. A Between the time the temperature falls and rises.In most women, the BBT drops slightly 24 to 36 hours before ovulation and rises 24 to 72 hours after ovulation, when the corpus luteum of the ruptured ovary produces progesterone. Therefore, intercourse between the time of the temperature fall and rise is the best time for When the temperature falls and remains low for 36 hours. D. Within 72 hours before the temperature falls. A woman who had a miscarriage 6 months ago becomes pregnant. Which instruction is most important for the nurse to provide this client? A.Elevate lower legs while resting. b.Increase caloric intake by 200 to 300 calories per day.c.Increase water intake to 8 full glasses per day. d.Take prescribed multivitamin and mineral supplements. d.Take prescribed multivitamin and mineral supplements.A client who has had a spontaneous abortion or still birth in the last 1½ years should take multivitamin and mineral supplements and maintain a balanced diet because the previous pregnancy may have left her nutritionally depleted A vaginally delivered infant of an HIV positive mother is admitted to the newborn nursery. What intervention should the nurse perform first?A.Bathe the infant with an antimicrobial soap. B.Measure the head and chest circumference. C. Obtain the infant's footprints. D. Administer vitamin K (AquaMEPHYTON). A.Bathe the infant with an antimicrobial soap. To reduce direct contact with the human immuno-virus in blood and body fluids on the newborn's skin, a bath with an antimicrobial soap should be administered first. A newborn, whose mother is HIV positive, is scheduled for follow-up assessments. The nurse knows that the most likely presentation for a pediatric client with AIDS is:A. shortness of breathB. Joint painC. a persistent coldD. Organomegaly C. a persistent coldRespiratory tract infections commonly occur in the pediatric population. However, the child with AIDS has a decreased ability to defend the body against these infections and often the presenting symptom of a child with AIDS is a persistent cold The nurse is caring for a woman with a previously diagnosed heart disease who is in the second stage of labor. Which assessment findings are of greatest concern? A.Edema, basilar rales, and an irregular pulse. B. Increased urinary output and tachycardia. C.Shortness of breath, bradycardia, and hypertension. D.Regular heart rate and hypertension A.Edema, basilar rales, and an irregular pulse. indicates cardiac decompensation and requires immediate intervention. A woman with Type 2 diabetes mellitus becomes pregnant, and her oral hypoglycemic agents are discontinued. Which intervention is most important for the nurse to implement? a. Describe diet changes that can improve the management of her diabetes.b.Inform the client that oral hypoglycemic agents are teratogenic during pregnancy. c. Demonstrate self- administration of insulin. d. Evaluate the client's ability to do glucose monitoring. a. Describe diet changes that can improve the management of her diabetes. A client receiving epidural anesthesia begins to experience nausea & becomes pale & clammy. What intervention should the nurse implement first?A. Rise the foot of the bedB. Assess for vaginal bleedingC. Evaluate the fetal heart rateD. Take the client's blood pressure A. Rise the foot of the bedThese symptoms are suggestive of hypotension which is a side effect of epidural anesthesia. Raising the foot of the bed will increase venous return and provide blood to the vital areas. Increasing the IV fluid rate using a balanced non-dextrose solution and ensuring that the client is in a lateral position are also appropriate interventions, and then checking the patients blood pressure. The total bilirubin level of a 36-hour, breastfeeding newborn is 14 mg/dl. Based on this finding, which intervention should the nurse implement? A.Provide phototherapy for 30 minutes q8h. B. Feed the newborn sterile water hourly.C.Encourage the mother to breastfeed frequently. D.Assess the newborn's blood glucose level. C.Encourage the mother to breastfeed frequently. Encourage the mother to breastfeed frequently.The normal total bilirubin level is 6 to 12 mg/dl after Day 1 of life. This infant's bilirubin is beginning to climb and the infant should be monitored to prevent further complications. Breast milk provides calories and enhances GI motility, which will assist the bowel in eliminating bilirubin. A 35-year-old primigravida client with severe preeclampsia is receiving magnesium sulfate via continuous IV infusion. Which assessment data indicates to the nurse that the client is experiencing magnesium sulfate toxicity? A.Deep tendon reflexes 2+. B.Blood pressure 140/90. C.Respiratory rate 18/minute. D.Urine output 90 ml/4 hours. D. Urine output 90 ml/4 hours. • Urine outputs of less than 100 ml/ 4 hours, • absent DTRs, • & RR less than 12 breaths/minute are cardinal signs of magnesium sulfate toxicity. 30-year-old gravida 2, para 1 client is admitted to the hospital at 26-weeks' gestation in preterm labor. She is given a dose of terbutaline sulfate (Brethine) 0.25 mg subcutaneous. Which assessment is the highest priority for the nurse to monitor during the administration of this drug? A. Maternal blood pressure and respirations. B.Maternal and fetal heart rates. C.Hourly urinary output. D.Deep tendon reflexes. B.Maternal and fetal heart rates. Terbutaline acts as a sympathomimetic agent that stimulates both beta 1 receptors (causing tachycardia, a side effect of the drug) and stimulation of beta 2 receptors (causing uterine relaxation, a desired effect of the drug). A full-term infant is admitted to the newborn nursery and, after careful assessment, the nurse suspects that the infant may have an esophageal atresia. Which symptoms is this newborn likely to have exhibited? a. Choking, coughing, and cyanosis.b. Projectile vomiting and cyanosis. c. Apneic spells and grunting. d. organomegaly. a. Choking, coughing, and cyanosis.the "3 Cs" of esophageal atresia caused by the overflow of secretions into the trachea. The nurse attempts to help an unmarried teenager deal with her feelings following a spontaneous abortion at 8-weeks gestation. What type of emotional response should the nurse anticipate? A.Grief related to her perceptions about the loss of this child.B.Relief of ambivalent feelings experienced with this pregnancy. C.Shock because she may not have realized that she was pregnant. D. Guilt because she had not followed her healthcare provider's instructions. The nurse is assessing the umbilical cord of a newborn. Which finding constitutes a normal finding? A.Two vessels: one artery and one vein.B.Two vessels: two arteries and no veins. C.Three vessels: two arteries and one vein. D.Three vessels: two veins and one artery A.Grief related to her perceptions about the loss of this child. C.Three vessels: two arteries and one vein. A new mother is afraid to touch her baby's head for fear of hurting the "large soft spot." Which explanation should the nurse give to this anxious client? A.Some care is required when touching the large soft area on top of your baby's head until the bones fuse together. B.That's just an 'old wives' tale' so don't worry, you can't harm your baby's head by touching the soft spot. C.The soft spot will disappear within 6 weeks and is very unlikely to cause any problems for your baby. D.There's a strong, tough membrane there to protect the baby so you need not be afraid to wash or comb his/her hair. D.There's a strong, tough membrane there to protect the baby so you need not be afraid to wash or comb his/her hair. • The anterior fontanel or "large soft spot" has a strong epidermal membrane present, which can be touched. • The anterior fontanel normally closes at 12 to 18 months of age. • The posterior fontanel closes at 8 to 12 weeks of age The nurse caring for a laboring client encourages her to void at least q2h, and records each time the client empties her bladder. What is the primary reason for implementing this nursing intervention?A. Emptying the bladder during delivery is difficult because of the position of the presenting fetal part. B. An over-distended bladder could be traumatized during labor as well as prolong the progress of labor. C.Urine specimens for glucose and protein must be obtained at certain intervals throughout labor. D. Frequent voiding minimizes the need for catheterization which increases the chance of bladder infection. client who is attending antepartum classes asks the nurse why her healthcare provider has prescribed iron tablets. The nurse's response is based on what knowledge? A. B. An over-distended bladder could be traumatized during labor as well as prolong the progress of labor. • full bladder can impair the efficiency of the uterine contractions • impede descent of the fetus during labor. • Also, b/c of close proximity of the bladder to the uterus, the bladder can be traumatized by the descent of the fetus. B. It is difficult to consume 18 mg of additional iron by diet alone.Consuming enough iron-containing foods to facilitate adequate fetal storage of iron and to meet Supplementary iron is more efficiently utilized during pregnancy.B. It is difficult to consume 18 mg of additional iron by diet alone.C. Iron absorption is decreased in the GI tract during pregnancy. D. Iron is needed to prevent megaloblastic anemia in the last trimester. A woman who thinks she could be pregnant calls her neighbor, a nurse, to ask when she could use a home pregnancy test to diagnose pregnancy. Which response is best? A. home pregnancy test can be used right after your first missed period. B.These tests are most accurate after you have missed your second period. C. Home pregnancy tests often give false positives and should not be trusted.D . The test can provide accurate information when used right after ovulation. A. home pregnancy test can be used right after your first missed period. • Home urine tests are based on the chemical detection of human chorionic gonadotrophin, • which begins to increase 6 to 8 days after conception • is best detected at 2 weeks gestation or immediately after the first missed period. 28 year old client in active labor complains of cramps in her leg.What intervention should the nurse implement. A. massage the calf and footB. extend the leg and dorsiflex the foot C. lower the leg off the side of the bedD. elevate the leg above the heart. B. extend the leg and dorsiflex the foot Dorsiflexing the foot by pushing the sole of the foot forward or by standing (if the client is capable) (B), and putting the heel of the foot on the floor is the best means of relieving leg cramps. A client at 30-weeks gestation, complaining of pressure over the pubic area, is admitted for observation. She is contracting irregularly and demonstrates underlying uterine irritability. Vaginal examination reveals that her cervix is closed, thick, and high. Based on these data, which intervention should the nurse implement first? A.Provide oral hydration. B.Have a complete blood count (CBC) drawn. C.Obtain a specimen for urine analysis. D.Place the client on strict bedrest. A client in active labor is admitted with preeclampsia. Which assessment finding is most significant in planning this client's care? A. Patellar reflex 4+B. BP 158/80C. Four- hour urine output 240 mLD. Resp 12/ min C.Obtain a specimen for urine analysis. Obtaining a urine analysis should be done first because preterm clients with uterine irritability and contractions are often suffering from a urinary tract infection, and this should be ruled out first. A. Patellar reflex 4+with pregnancy-induced hypertension indicates hyperreflexia, which is an indication of an impending seizure. A 4 week old premature infant has been receiving epoetin alfa for the last 3 weeks. Which assessment finding indicates to the nurse that the drug is effective. A.slowly increasing urinary output over the last week B.rr changes from 40s to the 60sC. changes in apical HR from the 180 to the 140D.Change in indirect bilirubin from 12mg/dl to 8mg/dl. C. changes in apical HR from the 180 to the 140 • Epogen, given to prevent or treat anemia, • stimulates erythropoietin production, resulting in an increase in RBCs. • Since the body has not had to compensate for anemia with an increased heart rate, changes in The healthcare provider prescribes terbutaline (Brethine) for a client in preterm labor. Before initiating this prescription, it is most important for the nurse to assess the client for which condition?A. Gestational DiabetesB. Elevated BPC. UTID. Swelling in lower extremities A. Gestational diabetes.The nurse should evaluate the client for gestational diabetes because terbutaline (Brethine) increases blood glucose levels. A client with NO prenatal care arrives at the labor unit screaming, "The baby is coming!" The nurse performs a vaginal examination that reveals the cervix is 3 centimeters dilated and 75% effaced. What additional information is most important for the nurse to obtain?A. Gravidty and parityB. Time and amount of last oral intakeC. Date of last normal menstrual periodD. Frequency and intensity of contractions C. Date of last normal menstrual periodEvaluating the gestation of the pregnancy takes priority. If the fetus is preterm and the fetal heart pattern is reassuring, the healthcare provider may attempt to prolong the pregnancy and administer corticosteroids to mature the lungs of the fetus. The nurse assesses a client admitted to the labor and delivery unit and obtains the following data: dark red vaginal bleeding, uterus slightly tense between contractions, BP 110/68, FHR 110 beats/minute, cervix 1 cm dilated and uneffaced. Based on these assessment findings, what intervention should the nurse implement?A. insert an internal fetal monitor B. Assess for cervical changes q1hC. Monitor bleeding from IV sitesD. Perform Leopold's maneuvers C. Monitor bleeding from IV sites • Monitoring bleeding from peripheral sites is the priority intervention. This client is presenting with signs of placental abruption. • Disseminated intravascular coagulation (DIC) is a complication of placental abruptio, characterized by abnormal bleeding Immediately after birth a newborn infant is suctioned, dried and placed under a radiant warmer. The infant has spontaneous respirations and the nurse assesses an apical HR of 80 beats/minute and respirations of 20 breaths/min. What action should be performed next?A. Initiate positive pressure ventilation B . Intervene after one min Apgar is assessed.C. Initiate CPR on the infant D. Assess the infant's blood glucose level The nurse is preparing to give an enema to a laboring client. Which client requires the most caution when carrying out this procedure?A. A gravida 6, para 5 who is 38 years of age and is early laborB. 37-week primigravida who presents at 100% effacement, 3 cm dilated, & -1 stationC. Gravida 2, para 1 who is at 1 cm cervical dilation and 0 station admitted for induction of labor due to post datesD. A 40 week- A. Initiate positive pressure ventilation this infant's vital signs are not within the normal range, and oxygen deprivation leads to cardiac depression in infants. (The normal newborn pulse is 100 to 160 beats/minute and respirations are 40 to 60 breaths/minute.) D. A 40-week primigravida who is at 6 cm cervical dilatation and the presenting part is not engaged. When the presenting part is ballottable, it is floating out of the pelvis. In such a situation, the cord can descend before the fetus causing a prolapsed cord, which is an emergency situation. primigravida who is 6 cm dilated and the presenting part is not engaged The nurse is providing discharge teaching for a client who is 24 hours postpartum. The nurse explains to the client that her vaginal discharge will change from red to pink and then to white. The client asks, "What if I start having red bleeding AFTER it changes?" What should the nurse instruct the client to do?A. Reduce activity level and notify the HCPB. Go to bed and assume a knee-chest positionC. Massage the uterus and go to the ERD. Do not worry as this is a normal occurence B. Go to bed and assume a knee-chest positio • Lochia should progress in stages from rubra (red) to serosa (pinkish) to alba (whitish), and not return to red. • The return to rubra usually indicates subinvolution or infection. • If such a sign occurs, the mother should notify the clinic/healthcare provider and reduce her activity to conserve energy One hour after giving birth to an 8-pound infant, a client's lochia rubra has increased from small to large and her fundus is boggy despite massage. The client's pulse is 84 beats/minute and blood pressure is 156/96. The healthcare provider prescribes Methergine 0.2 mg IM × 1. What action should the nurse take immediately? A client at 32-weeks gestation is diagnosed with preeclampsia. Which assessment finding is most indicative of an impending convulsion?A. Three plus deep tendon reflexesB. Periorbital edemaC. Epigastric painD. Decreased urine output A. Three plus deep tendon reflexes and hyperclonus are indicative of an impending convulsion and requires immediate attention. A client at 32-weeks gestation comes to the prenatal clinic with complaints of pedal edema, dyspnea, fatigue, and a moist cough. Which question is most important for the nurse to ask this client?A. "Which symptom did you experience first?"B. "Are you eating large amounts of salty foods?"C. "Have you visited a foreign country recently?"D. "Do you have a hx of rheumatic fever?" A couple has been trying to conceive for nine months without success. Which information obtained from the clients is most likely to have an impact on the couple's ability to conceive a child?A. Exercise regimen of both partners includes running 4 miles every morningB. Hx of having sexual intercourse 2 to 3 times per weekC. The woman's menstrual period occurs every 35 daysD. The use of lubricants has the potential to affect fertility because some lubricants interfere with sperm motility. They use lubricants w/ each sexual encounter to decrease friction After each feeding, a 3-day-old newborn is spitting up large amounts of Enfamil® Newborn Formula, a nonfat cow's milk formula. The pediatric healthcare provider changes the neonate's formula to Similac® Soy Isomil® Formula, a soy protein isolate based infant formula. What information should the nurse provide to the mother about the newly prescribed formula?A. The new formula is a coconut milk formula used with babies B. Enfamil Formula is a demineralized whey formula that is needed with diarrhea C. The new formula is a casein protein source that is low in phenylalanineD. Similac Soy isomer formula is a soy-based formula that contains sucrose The nurse is performing a gestational age assessment on a full-term newborn during the first hour of transition using the Ballard (Dubowitz) scale. Based on this assessment, the nurse determines that the neonate has a maturity rating of 40-weeks. What findings should the nurse identify to determine if the neonate is small for gestational age (SGA)? (Select all that apply.)A. Admission weight of 4 pounds, 15 ounces (2244 grams)B..Head to heel length of 17 inches (42.5 cm)C. Frontal occipital circumference of 12.5 inches (31.25 cm)D. Skin smooth with visible veins and abundant vernixE. Anterior plantar crease and smooth health surfacesF. Full flexion of all extremities is resting supine position The nurse is assessing a client who is having a non-stress test (NST) at 41-weeks gestation. The nurse determines that the client is not having contractions, the fetal heart rate (FHR) baseline is 144 bpm, and no FHR accelerations are occurring. What action should the nurse take?A. Check the client for urinary bladder distentionB. Notify the healthcare provider of the nonreactive resultsC. Have the mother stimulate the fetus to moveD. Ask the client if she has felt any fetal movement D.Similac Soy isomer formula is a soy- based formula that contains sucrose The nurse should explain that the newborn's feeding intolerance may be related to the lactose found in cow's milk formula and is being replaced with the soy-based formula that contains sucrose, which is well-tolerated in infants with milk allergies and lactose intolerance. C. Frontal occipital circumference of 12.5 inches (31.25 cm) B. Head to heel length of 17 inches (42.5 cm) A. Admission weight of 4 pounds, 15 ounces (2244 grams)full-term, appropriate for gestational age (AGA) newborn • 6-9 pounds (2700-4000 grams); • length, 19-21 inches (48-53 cm); • FOC, 13-14 inches (33-35 cm). • This neonate's parameters plot below the 10% percentile, which indicate that the infant is SGA. D. Ask the client if she has felt any fetal movement • An NST is used to determine fetal well-being, and is often implemented when postmaturity is suspected. • A "reactive" NST occurs if the FHR accelerates 15 bpm for 15 seconds in response to the fetus' own movement, • "nonreactive" if no FHR acceleration occurs in response to fetal movement. [Show More]
Last updated: 2 years ago
Preview 1 out of 31 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Apr 21, 2021
Number of pages
31
Written in
Additional information
This document has been written for:
Uploaded
Apr 21, 2021
Downloads
0
Views
123



 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)