*NURSING > Study Notes > ATI Topic Descriptors Basic Care and Comfort (13) Plan A. Advance Directives: Recognize Purpose (All)
ATI Topic Descriptors Basic Care and Comfort (13) Plan A. Advance Directives: Recognize Purpose
Document Content and Description Below
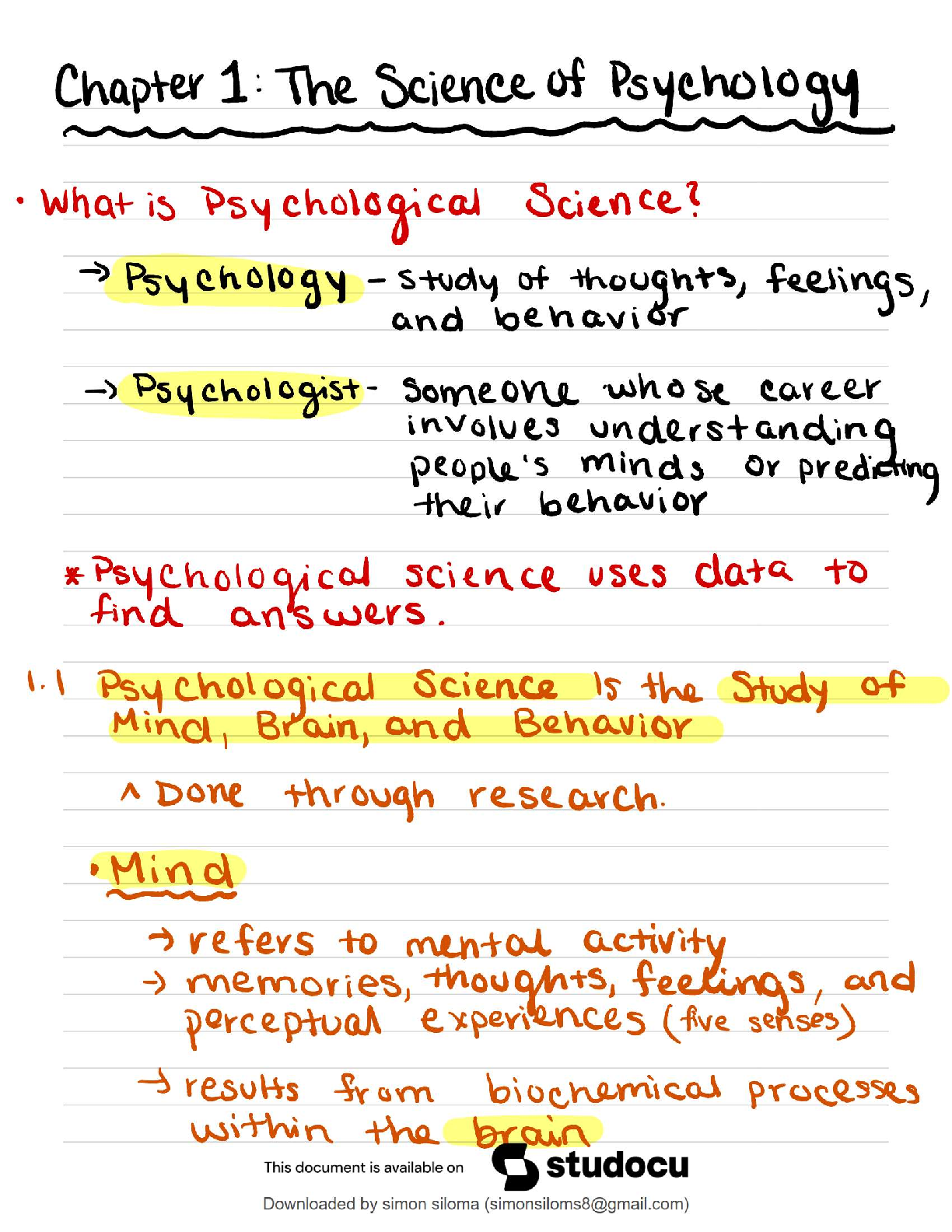
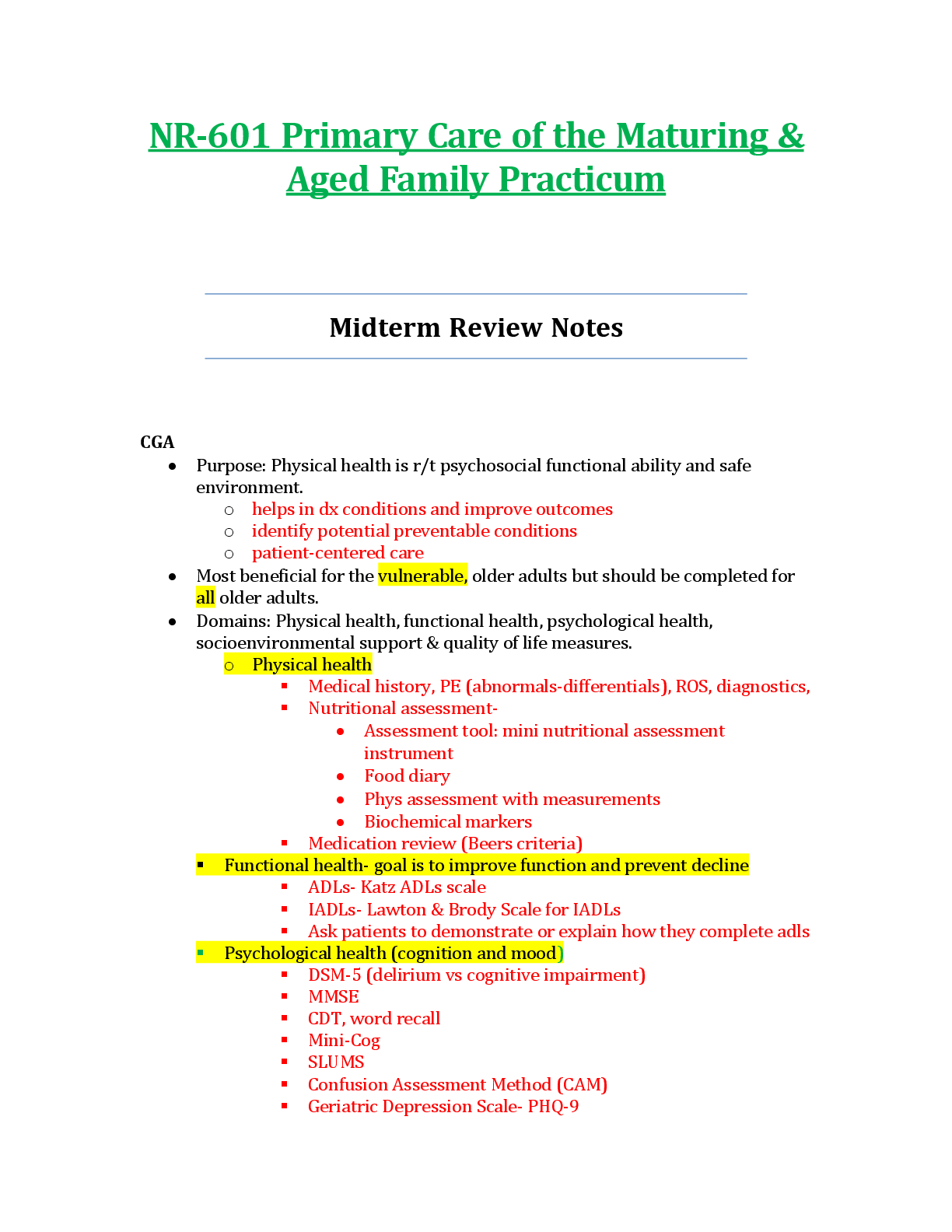
ATI Topic Descriptors Basic Care and Comfort (13) Plan A Hygiene Care: Evaluating Appropriate Use of Assistive Devices Place dentures in a denture cup or emesis basin Complimentary an ... d Alternative Therapies: Appropriate Use of Music Therapy for Pain Management Prostate Surgeries: Calculating a Clientʼs Output When Receiving Continuous Bladder Irrigations (To obtain urine output, subtract amount of fluid instilled into bladder from total output.) Urinary Elimination: Kegel Exercises for Urinary Incontinence sits on toilet with knees far apart and tightens muscle to stop the flow of urine ( to learn the muscle) Bowel Elimination Needs: Client Education Regarding Colostomy Care Stoma s/b pink. skin should be washed with mild soap, warm water and dried thoroughly before barrier applied Burns: Non-pharmacologic Comfort Interventions for Dressing Changes Distractions Application of Heat and Cold: Assess Need for Heat/Cold Applications Application of Cold: Ensure Safe Use of Cold Applications Crohnʼs Disease: Selecting a Low-Fiber, Low-Residue Diet Dumping Syndrome: Client Education Regarding Dietary Interventions Cholecystitis: Dietary Restrictions Palliative Care: Client/ Family Teaching Cognitive Disorders: Promoting Independence in Hygiene for A Client with Alzheimerʼs Disease Rest and Sleep: Recognizing and Reporting Sleep Disorders (P/P 1203) Basic Care and Comfort (13) Plan B Mobility and Immobility: Recognizing Proper Use of Crutches 4-point gait requires wt bearing on both legs 3 point gait 2-point gait Pain Management: Nonpharmacological Pain Management Urinary Elimination Needs: Preventing Incontinence Urinary Elimination: Providing Catheter Care Mobility and Immobility: Evaluating for Complications of Immobility Complications of Immobility Gastroenteral Feedings: Monitoring Tube Feedings Acute Glomerulonephritis: Dietary Choice Rest and Sleep: Interventions to Promote Sleep for Hospitalized Clients ATI Topic Descriptors Plan A Health Promotion and Maintenance (13) Uterine Atony: Performing Appropriate Assessment (Murray/Mckinney p. 734-736) Assessments for uterine atony include: Normal Physiological Changes of Pregnancy: Calculating the clientʼs delivery date ATI p. 34 Cesarean Birth: Appropriate Client Positioning ATI p. 218 Antepartum Diagnostic Interventions: Monitoring during a Nonstress Test ATI p. 85 NST Reactive : FHR accelerates to 15 beats/min for at least 15 sec and occurs 2 or more times during a 20 min period Newborn Hypoglycemia: Identify Appropriate Interventions ATI p. 424 Nursing interventions Labor and Birth Processes: Assess for True Labor vs. False Labor ATI p. 136 True Labor Contractions Cervix Fetus presenting part engages in pelvis False Labor Contractions Cervix (assessed by vaginal exam) Fetus Bonding: Promoting Maternal Psychosocial Adaptation During the Taking-In Phase ATI p. 290 Toddler: Recognizing Expected Body-Image Changes ATI Adolescent (12-20 years): Planning Age-Appropriate Health Promotion Education Contraception: Recognizing Correct Use of Condoms ATI p. 6 Immunizations: Recognizing Complications to Report ATI p. 279 Older Adult (0ver 65 years): Assessing Risk for Social Isolation Spinal Cord Injury: Promoting Independence In Self-Care Health Promotion and Maintenance Plan B Antepartum Diagnostic Interventions: Prenatal Fetal Heart Rate Monitoring Complications of Pregnancy: Recognizing Abnormal Findings Bleeding during Pregnancy Discharge Teaching: Evaluating Clientʼs Understanding of Bulb Syringe Use Postpartum Physiological Changes and Nursing Care: Performing Fundal Assessment Toddler: Provide Education on Age-Specific Growth and Development Infant (Birth to 1 yr): Identifying Normal Physical Assessment Findings ATI Topic Descriptors Management of Care (24) Plan A Advance Directives: Recognize Purpose Client Advocacy: Intervening on behalf of the Client Discharge Planning: Interventions to Promote Timely Client Discharges Clients Rights: Recognizing Client Rights Regarding Review of Records Collaboration with Interdisciplinary Team: Methods for Collaboration COPD: Planning Strategies for Fatigue ATI---determine the clientʼs physical limitations and structure activity to include periods of rest Conflict Resolution: Identify Strategies Genitalia and Rectum: Providing Privacy Consultation: Referral in Response to a Client Concern Complete referral forms to ensure proper reimbursement for services ordered. Client Education: Document Client Teaching Delegation: Use of the Five Rights of Delegation Delegation: Monitoring Outcomes of Delegated Tasks Delegation: Assigning Tasks To AP Based On Role parameters and Skill Required Disaster Planning and Emergency Management: Prioritizing Delivery of Client Care Ethics and Values: Appropriate Response to Experiencing Negative Feelings about a Client Client Education: Assisting Clients to Access current Health Information Using Information Technology Client Education: Selecting Appropriate Information Technology for Adolescent Client Education Informed Consent: Ensure Informed Consent Legal Responsibilities: Reporting Client Abuse the Performance Improvement: Utilize References to Improve Performance and Maintain Safe Practice Referrals: Assessing Need to Refer Clients for Assistance Complete referral forms to ensure proper reimbursement for services offered. Staff Development: Selecting Staff Education Activities Based on Staff Learning Styles Domains of Learning Cognitive learning, which includes all intellectual activities. Ex: person is taught and then can list what is learned. Affective learning, which includes feelings, opinions, and values. Ex: person is attentive and willing to listen to instructor Psychomotor learning, which is learning to complete a physical activity. Ex: client practices a skill. Auditory learners---learn by listening Visual learners---learn by seeing Kinesthetic learners---learn by doing Staff Development and Performance Improvement: Selecting Educational Activities to Ensure Staff Competencies Competence the ability to meet the requirement of a particular role Strategies to maintain competence include use of checklists to provide a record of opportunities and the level of proficiency in relation to skills peer observation/evaluation, planned or incidental, to assess competence complete of electronic learning modules attendance at in-services to update skills attendance at training sessions to learn specialized skills (ACLS, PLS Supervising Client Care: Information Sources for Making Client Assignments Assignment Factors Client Factors complexity of care needed specific care needs (eg cardiac monitoring, mechanical ventilation) need for special precautions (eg private room with negative air pressure and anteroom, fall precautions, seizure precautions) Health care team factors Skills Experience Nurse to client ratio Management of Care (24) Plan B Culturally Competent Care: Recognize Need for Use of Translator for Non-English Speaking Client Communication Improve the nurse/client relationship when the communication barrier is great enough to impact the exchange of info between the nurse and client use interpreters when the communication barrier is great enough to impact the exchange of info between the nurse and the client cautiously use nonverbal communication as it may have very different meanings for the client and the nurse Peripheral Venous Disease: Modification of Care Plan in Response to DVT Development Interventions Deep Vein Thrombosis and Thrombophlebitis Encourage REST facilitate bedrest and elevation of extremity above the level of the heart (avoid using a knee gatch or pillow under knees) admin intermittent or continuous warm moist compresses (to prevent thrombus from dislodging and becoming an embolus, DO NOT massage the affected limb) provide thigh-high compression or antiembolism stockings to reduce venous stasis and to assist in venous return of blood to the heart. such as abciximab (REoPRo), tirofiban (Aggrastat) and sptifibatide (Integrilin) may be effective in dissolving a clot or preventing new clots during the first 24 hr. primary complication of therapy is serious bleeding Delegation: Making Appropriate Client Assignment for a Float Nurse Assignment Factors: Complexity of care needed Specific care needs (eg cardiac monitoring, mechanical ventilation) Need for special precautions (eg private room with negative air pressure and anteroom, fall precautions, seizure precautions) Health care team factors: Skills Experience Nurse-to-Client ratio Floating is an acceptable, legal practice used by hospitals to solve their understaffing problems Legally a nurse cannot refuse to float unless a union contract guarantess that nurses can work only in a specified area or the nurse can prove lack of knowledge for the performance of assigned tasks. Nurses in a floating situation must not assume responsibility beyond their level of experience or qualification Nurses who float should inform the supervisor of any lack of experience in caring for the type of clients on the new nursing unit The nurse should request and be given orientation to the new unit Delegation: Identification of Client Concerns to be Reported to Nurse by AP for Delegated Tasks Question: Toward the end of the shift, an LPN reports to an RN that a recently hired AP has not totaled clientʼs I&O for the past 8 hr. Which of the following should the RN take? A. Confront the AP and instruct him to complete the I&O measurements B. Delegate this task to the LPN since the AP may not have been educated on this task C. Ask the AP if he needs assistance completing the I&O records. D. Notify the nurse manager to include this on the APʼs evaluation. I&O measurements are routine AP tasks; however the AP is new and my need some assistance. Making assumptions and negative evaluation without direct evidence should be avoided. Prioritizing Client Care: Recognizing Assessment Priorities Among Multiple Clients Prioritizing is deciding which needs or problems require immediate action and which ones could be delayed until a later time bec they are not urgent. before potential health-threatening concerns When prioritizing care, the nurse must consider time constraints and availbalbe resources and objectives in a health care facility Resource management includes budgeting and resource allocation Budgeting is usually the responsibility of the unit manager, but the staff nurse may be asked to provide input. Resource allocation is responsibility of the the unit manager as well as every practicing nurse. Providing cost-effective client care should be balanced with quality of care. Cost-effective resource allocation includes: providing necessary equipment and properly charging client. Returning uncontaminated unused equipment to the appropriate dept for credit. Using equipment properly to prevent wastage. Providing training to staff unfamiliar with equipment. Returning equipment (eg., IV, kangaroo pumps) to the proper dept (eg central service, central distribution) as soon as it is no longer needed. This action will prevent further cost to the client. Performance Improvement: Recognizing Priority Data Needed to Plan Staffing Referrals: Recognizing Client Need for Rehabilitation Services Resource Management: Safe Cost-Effectiveness Nursing Interventions Staff Development: Evaluate Outcomes of Staff Education Activities Staff Development: Orientation to the Workplace Orientation helps new graduates translate knowledge, principles, skills, and theories learned in nursing school into practice is necessary for nurses new to health care facility or unit to learn the procedures and protocols Topic Descriptors PHARMACOLOGICAL AND PARENTERAL THERAPIES (24) Form A Medications to Treat Depression: Recognizing Side Effects of Tricyclic Antidepressants indication: need for vascular access is long term (1 year or more) commonly for chemo care: to access: apply local anesthetic, palpate to locate the port clean with alcohol for 3 sec access with noncoring needle flush after q use and at least once a month Basic Pharmacological Principles: Expected Dosage Adjustments Based on Age of Client Pediatric dosages are based on body wt, body surface area and maturation of body organs. meds are based on age bec of greater risk for decreased skeletal growth, acute CV failure or hepatic toxicity. Intravenous Therapy: Documenting Discontinuation of IV Following Signs of Phlebitis Signs of Phlebitis Edema Throbbing, burning or pain at the site Warmth Erythema May be a red line up the arm with a palpable band at the vein site Slowed infusion Prevention: include: mechanical complication from insertion of the CVC infection metabolic alterations pneumothorax results from a puncture insult to the pulmonary system and results in the accumulation of air in the pleural cavity with subsequent collapse of the lung and impaired breathing. sudden sharp chest pain dyspnea coughing soln is suddenly d/cʼd. catheter occlusion temporarily stop infusion and flush with NS or heparin. if effort to flush is unsuccessful, attempt to aspirate a clot, is still unsuccessful, follow protocol for use of thrombolytic agent (urokinase) hypoglycemia to prevent: do not abruptly discontinue TPN but taper rate down to within 10% of infusion rate 1-2 hours before stopping. hyperglycemia monitor BG level daily until stable then as ordered or prn. TPN is initiated slowly and tapered up to maximal infusion rate. additional insulin may be required during therapy if problem persists. Form B Aminoglycosides: Assessing for Nephrotoxicity Nephrotoxicity r/t high total cumulative dose resulting in acute tubular necrosis (proteinuria, casts in the urine, dilute urine, elevated BUN, creatinine levels Monitor I/O, BUN, creatinine levels Normal values: BUN 5-20 mg/dL Creatinine 0.5-1.3 mg/dL Instruct pt to report a significant decrease in UOP Glucocorticoids: Recognizing SE of Long Term Therapy of UOP, document on clientʼs MR, record start and completion times of transfusion, total volume of transfusion and clientʼs response to transfusion, Assess infusion site for infection or infiltration assess patency of IV line do not admin blood along with any IV solution other than NS. IV solutions containing dextrose cause hemolysis of RBC the PcP do not turn on IV fluids that are connected to the Y tubing bec the remaining blood in the Y tubing will be infused and aggravate the clientʼs reaction. Admin a new IV soln of NS Stay with the client and monitor VS and UOP Notify the blood bank, recheck ID tag and numbers on the blood tag and send blood bag and IV tubing to blood bank for analysis Obtain urine specimen and send to lab to determine for RBC hemolysis Complete transfusion log sheet, which includes complete record of baseline VS, ongoing monitoring, and clientʼs response to transfusion. Basic Dosage Calculation: Monitoring IV Heparin Infusion Monitor VS. In the case of heparin overdose, stop heparin, admin protamine sulfate and avoid ASA Monitor activated partial thromboplastin time (aPTT). Keep value at , 2 times the baseline. Dosages must be checked by another nurse before admin. For continuous IV admin, use an infusion pump. Rate of infusion must be monitored q 30-60 min. Monitor aPPT q 4-6 hr until appropriate dose is determined and then monitor daily Medication effectiveness: aPTT levels of 60-80 sec No development or no further development of venous thrombi Glucocorticoids for Rheumatoid Arthritis: Evaluating Client Education Regarding Long Term Effects Client Teaching for Corticosteroid Therapy E. Plan a diet high in protein, calcium (at least 1500 mg per day) and potassium but low in fat and concentrated simple carbs such as sugar, honey, syrups and candy. F. Identify measures to ensure adequate rest and sleep such as daily naps and avoidance of caffeine lat in the day G. develop and maintain an exercise program to help maintain bone integrity H. recognize edema and ways to restrict sodium intake to less than 2000mg per day if edema occurs I. monitor glucose levels and recognize sx and signs of hyperglycemia (eg polydipsia, polyuria, blurred vision) and glycosuria (glucose in the urine). The pt should be instructed to report hyperglycemic sx or capillary glucose levels greater than 180 mg/ dL or urine positive for glucose J. notify HCP if experiencing postprandial heartburn or epigastric pain that is not relieved by antacids. K. See an eye specialist yearly to assess development of possible cataracts L. use safety measures such as getting up slowly from bed or a chair and use good lighting to avoid accidental injury M. maintain good hygiene practices and avoid contact with persons with colds or other contagious illnesses to avoid infection. Osteoporosis Advise the client to take Ca supplements, vit D, and/or biphosphonate Adrenal suppression advise client to observe for sx Insulin: Monitoring Adequate Blood Glucose Control Medication effectiveness: Glucose levels of 90-130 mg/dL preprandial and < 180 mg/dL postprandial HgA1c < 7 % Normotensive (< 130/80 mmHg) Cholesterol levels within normal range Cardiac Glycosides: Client Education to Reduce Risk Therapeutic Nursing Interventions and Client Education Advise clients to take med as prescribed and not to double the dose when a dose is not taken at the prescribed time Check pulse rate and rhythm before admin of digoxin and record, notify the PcP if HR is < 60 beats/min in an adult, <70 beats/min in children and < 90 beats/min in infants. Admin dig at same time daily. Monitor dig levels periodically while on tx and maintain therapeutic levels between 0.5-2.0 ng/mL to prevent dig toxicity Avoid taking OTC meds to prevent adverse SE and med interactions Instruct clients to observe symptoms of hypokalemia such as muscle weakness, and to notify the PCP if sx occur. Instruct clients to observe sx of dig toxicity (eg anorexia, fatigue, weakness) and to notify PcP if sx occur Management of dig toxicity Dig and potassium sparing med should be stopped immediately Monitor K levels. For levels, < 3.5 mEq/L, potassium should be administered IV or by mouth. Do not give any further K+ level > 5.0 mEq/L Treat dysrhythmias with phenytoin or lidocaine treat bradycardia with atropine ACE Inhibitors: Intervening for Client Response ACE inhibitors produce their effects by blocking the production of angiotensin II This results in: vasodilation (mostly arteriole) excretion of Na and H20, and retention of K+ (through effects on kidney) possible prevention of angiotensin II and aldosterone-induced pathological changes in blood vessels and heart. Side/Adverse Effects Interventions/Client Education First dose orthostatic hypotension if pt taking diuretic, stop med temporarily for 2-3 days prior to the start of an ACE inhibitor Start tx with a low dosage monitor the BP for 2 hr after initiation of tx instruct the client to change positions slowly and to lie down if feeling dizzy, lightheaded, or faint Cough inform client of dry cough notify PCP as med will most likely be d/cʼd HYPERKALEMIA monitor K+ levels to maintain normal range of 3.0-5.0 mEq/L Only take K+ substitutes if instructed by PCP Rash and dysgeusia (altered taste) client should inform PCP Angioedema (manifested as swelling of the tongue and oral pharynx treat severe effects with subcutaneous injection of epinephrine Neutropenia--rare complication of Captopril monitor the clientʼs WBC counts every 2 wks for 3 months, then periodically. inform the client to notify PCP at first signs of infection Furosemide: Recognizing Interactions with Other Medications Furosemide (Lasix), a high ceiling loop diuretics work in the ascending limb of Loop of Henle to Block reabsorption of Na+ and Cl-, and prevent the reabsorption of H20 Cause extensive diuresis SE: dehydration hypotension ototoxicity hypokalemia Interactions with other Meds Medication Nursing Intervention Digoxin toxicity (can occur in the presence of hypokalemia monitor ptʼs cardiac status and K+ and dig levels K+ sparing diuretics are often used in conjunction with loop diuretics to reduce the risk of hypokalemia Antihypertensives--concurrent use can have additive hypotensive effect monitor BP Lithium--levels can rise due to diuresis monitor Lithium levels NSAIDS blunt diuretic effect Watch for a decrease in effectiveness of diuretic such as a decrease in UOP Medications to Treat Pain: Identifying Need for Additional Analgesia decreased attention span Physiological measures of BP, pulse, RR will be temporarily increased by acute pain. Follow a clinical approach ABCDE to pain assessment and management A---ask about pain regularly, ASSESS pain systematically B---believe the client and family C---choose appropriate pain control options D---deliver interventions in a timely fashion Fractures: Discharge Teaching Regarding Cast Care Electrolyte Imbalances: Evaluating Effectiveness of Hypokalemia Interventions Potassium normal levels (3.5-5.0 mEq/L) Fluid Imbalances: Appropriate Intervention in Response to Signs of Fluid Volume Excess Electrolyte Imbalances: Recognizing Priority Interventions in Response to Hyponatremia Congenital Heart Disease: Interventions for Decreased Cardiac Output Shock: Recognizing S/S of Hypovolemia Acute GI Disorders: Recognizing S/S to report Herpes Zoster: Evaluating Client Teaching Cystic Fibrosis: Managing Illness at Home HIV/AIDS: Interventions to Prevent Spread of HIV Glomerular Disease: Recognizing Risk factors Burns: Priority Interventions Mechanical Ventilation: Response to Ventilator Alarms and Respiratory Distress Pulmonary Embolism: Evaluation of Tx Effectiveness COPD: Evaluating ABGs Cancer: Preventing Complications of Radiation Treatments Pain Management: Recognizing and Responding to Complications of Opioid Use Blood Transfusions: Interventions for Complications Oxygen Therapy: Assessing for S/S of Toxicity Monitoring Intracranial Pressure: Preventing Complications Electrolyte Imbalances: Priority Interventions for Hyperkalemia Tonsillitis/Tonsillectomy: Assessing for Postoperative Complications Cleft Lip and Palate: Client Eduction Regarding Feeding Techniques Glaucoma: Planning Appropriate Postoperative Interventions GERD: Recognizing Signs and Symptoms Infection Control: Preventing Transmission Communicable Diseases: Interventions to Prevent Transmission Emergency Nursing Principles: Establish Patent Airway Esophageal Varices: Response to Hemorrhage HIV/AIDS: Evaluating Antiretroviral Treatment Oncological Emergencies: Recognizing Sx of Radiation Therapy Complications Pneumonia: Recognizing and Responding to Hypoxia Topic Descriptors Psychosocial Integrity (14) Form A Family and Community Violence: Evaluating Client Outcomes for the Client Who Has been Abused Non-substance Related Dependencies: Providing Care and Support for Client with Gambling Dependency Crisis Management: Identifying Interventions Care of Those Who Are Dying: Providing Support to the Family Regarding Decision making Mood disorders: Recognizing S/S of Relapse for Bipolar Disorder Cognitive Disorders: Recognizing S/S of Impaired Cognition Psychopharmacological Therapies: Evaluating Client Teaching Regarding Lithium, Methlyphenidate, Disulfiram, and Fluoxetine Spiritual Care: Evaluating If Needs Have Been Met ask if the clientʼs needs are being met Sensoriperceptual Alterations: Planning Interventions for the Hearing Impaired Client Stress Management: Evaluate Effectiveness of Teaching Regarding Stress Management Techniques Family Dynamics: Interventions Involving Client Support Systems Effective Communication in Mental Health Nursing: Giving Broad Openings Body Image: Interventions to Assist Client Adaptation Form B Cognitive Disorders: Identifying Appropriate Interventions Group Therapy: Appropriate Group Leader Communication Techniques Coping: Assessing Support Systems ulturally Competent Care: Incorporate Religious Beliefs End of Life: Assessing Client Coping Family Dynamics: Interventions to promote Integration of Older Adults into family Structure Death and Dying: Recognizing Preschool Responses to Death Schizophrenia: Identifying Signs and Symptoms Developing and Maintaining a Therapeutic Nurse-Client Relationship: Intervene to Promote Trust Topic Descriptors Reduction of Risk Potential (24) Form A Seizures: Client Education Regarding EEG Rheumatic Fever: Recognizing Expected Lab Findings Diabetes Mellitus: Client Teaching Regarding Purpose of Self-Blood Glucose Monitoring Acid-Base Imbalances: Identify Expected lab Data Uncompensated: The pH will be abnormal and either the HCO3 or the PaCO2 will be abnormal Partially compensated: The pH, HCO3, and PaCO2 will be abnormal Fully Compensated: The pH will be normal, but the PaCO2 and HCO3 will both be abnormal Diabetic Ketoacidosis: Recognize Clinical Manifestations Fluid Imbalances: Interpret Lab Values for Dehydration Diabetes Insipidus: Recognizing Expected Lab Findings Heart Failure: Recognizing Expected Lab Findings Conscious Sedation: Monitoring Client Physiologic Response Following Conscious Sedation Peripheral Venous Disease: Prevent Complications Complications Ulcer Formation: typically over malleolus, more often medially than laterally . May lead to amputation and/or death Pulmonary Embolism: occurs when thrombus is dislodge, becomes emboli and lodges in the pulmonary vessels unfractionated heparin IV based on body wt is given to prevent formation of other clots and to prevent enlargement of existing clot, followed by oral anticoag with warfarin. Low molecular wt Heparin (LMWH) is given subq. Sickle Cell Anemia: Preventing Sickle Cell Crisis Thyroidectomy: Assess for Complications Complications Hemorrhage Thyroid Storm Airway Obstruction Hypocalcemia and Tetany (due to damage to the parathyroid glands) Nerve damage CVA: Interventions to Prevent Aspiration Postoperative Nursing: Preventing Circulatory Complications Gastroenteral Feedings: Measures to prevent Aspiration Head Injury: Assessing Neurological Status Urinary Tract Infection: Recognizing Risk Factors Joint Replacement: Client Teaching Regarding Postop Activity Limits Preoperative Nursing: Recognizing Client Finding Indicative of Readiness for Surgical Intervention Postoperative Nursing: Maintain Function of Jackson-Pratt Drain Pain Management: Management of an Epidural Catheter Intraoperative Nursing: Circulating Nurse Role Priorities Blood Pressure: Recognizing and Responding to Factors Affecting Blood Pressure Form B Angina: Recognize Appropriate Diagnostic Test Based on Client Findings Myocardial Infarction: Recognizing Diagnostic findings and Planning Care in Response Cervical CA: Recognizing Indications for Colposcopy and Biopsies Iron Deficiency Anemia: Identifying Expected lab Findings Conscious Sedation: Intervene for Complications Osteoporosis: Measures to Prevent Injury Leukemia: Interventions to Reduce Infection Risks of Chemotherapy Immobilizing Interventions: Assessing for Altered Tissue Perfusion Angina: Assessing Risk Factors Postoperative Nursing: Evaluating Postop Interventions to Prevent Complications Retinal Detachment: Evaluating Client Education Regarding Postop Care DM: S/S of Hypoglycemia Suctioning: Evaluation of Endotrach Suctioning Effectiveness COPD: Interventions for Abnormal 02 Saturation Findings Topic Descriptors Safety and Infection Control (17) Form A Newborn Discharge Teaching: Infant Safety Priorities Disaster Planning: Identify Disaster Preparedness Activities Emergency Management: Decontamination Following Exposure to Bioterrorism Ergonomic Principles: Prevention of Carpal Tunnel Syndrome Safe Medication Administration and Error Prevention: Selecting Appropriate Resources for Checking Prescription Accuracy Error Prevention: Ensuring Client Safety When Transcribing Orders Handling Infectious Materials: Appropriate Disposal Client Safety: Removing Fire Hazards Seizures: Appropriate Use of Seizure Precautions to Maintain Client Safety Surgical Asepsis: Performing Aseptic Technique Infection Control: Identifying and Reporting Errors in Surgical Skin Preparation Artificial Airway: Instructing Family on Safe Use of Equipment Emergency Management: Order of Client Evacuation in Response to a Fire HIV/AIDS: Appropriate Environmental Precautions Decreasing risks r/t sexual intercourse Decreasing risks r/t drug use Decreasing risks at work Meningitis: Client Education Regarding Prophylactic Precautions Client Safety: Evaluating Appropriate Selection of Restraints Based on Client Situation Client Safety: Appropriate Use of Restraints Client Safety: Maintain Prescribed Restraints Form B Emergency Management: Appropriate Response to Fire Ergonomic Principles: using Body Mechanics to Prevent Injuries to the Nurse Error prevention: Questioning Prescriptions Hazardous Materials: Appropriate Handling of Chemotherapy Incidents: Priority Responses Security Plans: Appropriate Interventions to Maintain Security on Obstetrical Unit [Show More]
Last updated: 3 years ago
Preview 1 out of 205 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 19, 2020
Number of pages
205
Written in
All
Additional information
This document has been written for:
Uploaded
Jun 19, 2020
Downloads
0
Views
124