*NURSING > HESI > MED SURG 209 | Med Surg II - MASTER HESI Review ; (Kidney stone, Calcium metabolism). Fortis College (All)
MED SURG 209 | Med Surg II - MASTER HESI Review ; (Kidney stone, Calcium metabolism). Fortis College Of Nursing.
Document Content and Description Below
Review Topics Part 1 1) Diabetes Insipidus – page 1161-1162 • Caused by a deficiency of production of ADH or a decreased renal response to ADH. • Clinical Manifestations: Polydipsia and P... olyuria. • Diagnostic Studies: Water deprivation test (pt deprived of water for 8-12 hrs and then given desmopressin acetate subcut or nasally), Measure level of ADH after an analog of ADH is given. • Types of Diabetic Insipidus: Central DI (results from an interference of ADH synthesis, transport, and release. Ex: brain tumor, head injury, brain surgery, CNS infection), Nephrogenic DI (results from inadequate renal response to ADH despite presence of adequate ADH. Ex: Drug therapy, renal damage, hereditary renal disease), Primary DI (Results from excessive water intake. Ex: Structural lesion in thirst center, psychological disorder). • Nursing Management: Early detection, Maintaining adequate hydration, and patient teaching for long-term management. 2) Healthcare associated pneumonia • Also known as nosocomial pneumonia, pneumonia in a non-intubated patient that begins 48 hours or longer after admission to hospital and was not present at the time of admission. Ventilator- associated pneumonia, also a type of HAP, refers to pneumonia that occurs more than 48 hours after endotracheal intubation. • Treatment: Antibiotics that can be started as soon as sputum cultures identify the exact pathogen. • Risks: In treatment of pneumonia, risk of developing multidrug-resistant organisms. Limits the available antibiotics that can be used as treatment. 3) Diabetes Mellitus long term complications • Stroke • Hypertension • Dermopathy • Atherosclerosis • Nephropathy • Peripheral neuropathy • Neurogenic bladder • Retinopathy, Cataracts, Glaucoma, Blindness • Coronary Artery Disease • Gastroparesis • Islet Cell Loss • Erectile Dysfunction • Peripheral Vascular Atherosclerosis • Gangrene • Infections • Examinations performed Daily, Annually, or when you visit HCP: Funduscopic, Fundus photography, Urinalysis, Feet Examination, and Stress Tests. 4) Renal dosing/ issues with drugs – page 1020 Box 44-3 ANTIBIOTICS OTHER DRUGS OTHER AGENTS Amikacin Captopril Gold Amphotericin B Cimetidine Heavy Metals Bacitracin Cisplatin Cephalosporins Cocaine Gentamicin Cyclosporine Neomycin Ethylene Glycol Polymyxin B Heroin Streptomycin Lithium Sulfamidies Methotrexate Tobramycin Nitrosoureas Vancomycin NSAIDS Phenacetin Quinine Rifampin Salicylates 5) Spinal cord injury – page 1419-1437 • Classification: (1) Mechanism of Injury, (2) Level of Injury, (3) Degree of Injury. • Clinical Manifestations: Motor and Sensory effects, Respiratory System (decrease in vital capacity volume), Cardiovascular System (bradycardia, peripheral vasodilation, hypotension), Urinary System (urinary dysfunction), Gastrointestinal System (incontinence, impaction, ileus, megacolon, decreased GI secretion) , Integumentary System (skin breakdown, pressure ulcers), Thermoregulation (Adjustment from body temp to room temp), Peripheral Vascular Problems (Pain, VTE, PE) • Emergency Management: Table 60-3 Ph. 1425 • NURSING ASSESSMENT o Subjective Date: Health History o Objective Data: Poikilothermism (unable to regulate body heat) o Integumentary System: Warm dry skin below level of injury o Respiratory: Injury at C1-3-Apnea, Inability to cough. Injury at C4-Poor Cough, diaphragmatic breathing, hypoventilation. Injury at C5-T6- Decreased respiratory reserve. o Cardiovascular: Injury above T6-Bradycardia, hypertension, absence of vasomotor tone. o Gastrointestinal: Decreased or absent bowel sounds, abdominal distension, constipation, fecal incontinence, fecal impaction. o Urinary: Retention, flaccid bladder, Spasticity with reflex bladder emptying. o Reproductive: Priapism, altered sexual function o Neurologic: Complete-Areflexic, flaccid paralysis, hyperactive deep tendon reflexes, bilaterally positive Babinski test. Incomplete- Mixed loss of voluntary motor activity and sensation. o Musculoskeletal: Muscle atony, Contractures. o Pain: Neuropathic, musculoskeletal, and/or visceral. 6) Blood in stool • Melena = black, tarry stools (often foul smelling) caused by digestion of blood in the GI tract. Black appearance is from the presence of iron. • Occult bleeding = small amounts of blood in gastric secretions, vomitus, or stools not apparent by appearance. Detectable by guaiac test. • Could be indication of an upper GI bleed • Hemorrhoids are the most common reason for bleeding with defecation o Focus on pain control and promote wound healing o Sitz bath 1 to 2 days after surgery and continue for 1 to 2 weeks o Teach the pt importance of diet, care of the anal area, symptoms of bleeding complications, and avoidance of constipation and straining 7) CVA (focus on vision issues) • Cerebral vascular accident / Stroke • Treat as medical emergency • Know FAST (Facial drooping, Arm weakness, Speech difficulties, Time) • Sudden trouble seeing in one eye should be reported immediately for indication of a CVA • Women who experience migraine with aura are at an increased risk for stroke. 8) Acute kidney injury • Slight deterioration in function to severe impairment • Rise in serum creatinine and/or a reduction in urine output, and sometimes leads to development of azotemia (accumulation of nitrogenous waste products in the blood) • Hospitalized patients develop AKI at a high rate and have a high mortality rate • Common causes: o Prerenal: Hypovolemia, Decreased Cardiac Output, Decreased Peripheral Vascular Resistance, Decreased Renovascular Blood Flow o Intrarenal: Nephrotoxic injury, Interstitial Nephritis o Postrenal: BPH, bladder cancer, calculi formation, trauma • Clinical manifestations: o Urinary changes – oliguria o Hypovolemia o Metabolic Acidosis o Sodium balance o Potassium excess o Hematologic disorders o Waste product accumulation o Neurologic disorders • Diagnostic studies: o H&P o Identification of precipitating cause o Serum creatinine and BUN levels o Electrolytes o Urinalysis o Renal Ultrasound o Renal scan o CT scan • Primary treatment is to eliminate the cause, manage the signs and symptoms and prevent complications while the kidneys recover 9) Abscess • A swollen area within the body tissue, containing an accumulation of pus • The body’s immune system sends WBC to fight the infection • Painful, swollen lump that is filled with pus • S/S = chills, fever, pimples, redness, painful lump, pus, tenderness, swelling, swollen lymph nodes • Treatment includes draining the abscess and antibiotics • Types mentioned in MedSurg: Anorectal (p. 970), brain (p. 1338), lactational breast (p. 1207), lung (p. 512), peritonsillar (p. 484) 10) Amyotrophic Lateral Sclerosis (lung issues) • AKA Lou Gehrig’s Disease • A nervous system disease that weakens muscles and impacts physical function. • In this disease, nerve cells break down, which reduces functionality in the muscles they supply. The cause is unknown. • The main symptom is muscle weakness. • Medication and therapy can slow ALS and reduce discomfort, but there's no cure. • Muscular: muscle weakness, problems with coordination, stiff muscles, loss of muscle, muscle spasms, or overactive reflexes • Whole body: fatigue or feeling faint • Speech: difficulty speaking or vocal cord spasm • Also common: difficulty swallowing, drooling, lack of restraint, mild cognitive impairment, severe constipation, severe unintentional weight loss, shortness of breath, or difficulty raising the foot • Treatment includes: o Therapies o Supportive Care o Medications (glutamate blocker or muscle relaxant) o Surgery o Medical procedure 11) Neutropenic precautions • is a blood condition involving low levels of neutrophils, a type of white blood cell. Neutrophils fight infection by destroying harmful germs. Without enough neutrophils, you’re more likely to develop infections. Usually, neutropenia occurs after: chemotherapy, radiation therapy or taking certain medicines. Remember: Gown, Gloves, Mask to protect the patient from catching any foreign bodies that night cause an infection. If the patient leaves the room, they must have a mask on before leaving and it must remain on them at all times while they are outside the room. 12) Asthma (focus on exercise) • that is induced or exacerbated during physical exertion is called exercise induced asthma (EIA) or exercise induced bronchospasm (EIB). This typically occurs after vigorous exercise, not during it (jogging, aerobics, climbing stairs). Symptoms of EIA are pronounced during activities where there is exposure to cold, dry air. Like swimming in an indoor heated swimming pool is less likely to produce symptoms than downhill skiing. Airway obstruction may occur due to changes in the airway mucosa caused by hyperventilation during exercise, with either cooling or rewarming of air and capillary leakage in the airway wall. Characteristics would include: wheezing, cough, dyspnea and a tight chest. 13) Bronchoscopy and complications (perforation) • Bronchoscopy is a procedure in which the bronchi are visualized through a fiberoptic tube. It may be used for diagnostic purposes to obtain biopsy specimens and assess changes resulting from treatment. It is also used to remove mucus plugs or foreign bodies. Laser therapy, electrocautery, cryotherapy, and stents can be placed through a bronchoscope to achieve patency of an airway that has been completely or partially obstructed by tumors. It can be performed in an inpatient or outpatient procedure room or at the bedside. 14) Burns (focus on electrical) • Electrical burns are the result of intense heat generated from an electric current. The severity depends on the amount of voltage, tissue resistance, current pathways, surface area in contact with the current, and length of time that the current flow was sustained. Electrical burns put the patient at risk for dysrhythmias or cardiac arrest, severe metabolic acidosis, and myoglobinuria. Myoglobin is released into the circulatory system when a muscle is injured this can travel to the kidneys and block tubules causing kidney injury. • Burn treatment is related to injury severity. Severity is determined by the extent of the burn, as calculated by the percent of the total body surface area (TBSA) burned; depth of the burn (determined by the degree of tissue destruction); location of the burn (e.g., face, hands, perineum); and patient risk factors (e.g., age, past medical history). o Burns continue to be defined by degrees: first degree (same as sunburn), second degree, third degree, and fourth degree. The American Burn Association recommends a more precise definition and classifies burns according to depth of skin destruction: partial- thickness burns and full-thickness burns. o Partial- and full-thickness burn extent can be determined using TBSA based on two guides: Lund-Browder chart and Rule of Nines. Burn extent is often revised after edema subsides and demarcation of injury zones occurs. 15) Chronic back pain (focus on postop assessment) • Causes of chronic low back pain include degenerative disc disease, lack of physical exercise, prior injury, osteoporosis, obesity, and structural and postural abnormalities. Treatment can include weight reduction, analgesics, rest periods, heat or cold application, and exercise and activity to strengthen muscles and mobilize joints. Surgery may be indicated for severe chronic low back pain not responding to conservative care. Nurses are role models and teachers in promoting low back health through use of proper body mechanics and other means to reduce strain on the low back area. Assessment table 63-5 page 1503. 16) DASH diet • The Dash Diet is an eating plan used to reduce hypertension. It emphasizes fruits, vegetables, fat- free or low-fat milk products, whole grains, fish, poultry, beans, and seeds. Compared to the typical American diet this eating plan focuses on less red meats, salts, sweets, and sugar containing beverages. If a client follows this diet it is proven to significantly reduce high blood pressure; the decreases are comparable to the decrease’s clients have seen who use only medications. The dash diet also contains additional benefits like lowering cholesterol and reduces an overall intake in sodium. This diet is recommended for primary prevention of hypertension in the general population. 17) Cholecystitis (diet/ NPO) • Cholecystitis is inflammation of the gallbladder wall and most commonly associated with obstruction caused by gallstones or biliary sludge; older adults and critically ill patients can see this with no obstruction occurring. During an acute attack the gallbladder wall is edematous, hyperemic. The inflammation of the wall will cause scarring decreasing the function of the gallbladder. Nutritional therapy is very important for these patients. Teach to eat smaller, frequent meals with some fat content to promote emptying of the gallbladder. Rapid weight loss should be avoided. These patients should remain NPO, to rest the bowels and prepare for a cholecystectomy; after a cholecystectomy, patients should remain on a clear liquid diet and progress to a regular diet once bowel sounds have returned. It is sometimes encouraged to restrict high fat content foods for 4-6 weeks. Discharge dietary instructions include eating nutritious meals and avoiding excessive fat in the diet. • HESI HINTS: o Non-surgical management of a patient includes a low-fat diet, decompression of the stomach via NG tube, and medications for pain control and clotting if required. o Non-surgical removal of stones via ERCP may make the client feel sick; ERCP uses a scope that is placed in the gallbladder and the stones are crushed and left to pass on their own. These clients can become prone to develop pancreatitis. 18) Diverticulitis • Diverticulitis is the inflammation of one or more diverticula that results in obstruction, infection, and hemorrhage. Most commonly seen in the left descending sigmoid colon occurring in the weak points in the intestinal wall. The main contributing factor in the its development is a lack of dietary fiber intake. Clinical manifestations include left lower quadrant pain, increased flatus, and rectal bleeding; if there is an obstruction the patient will present with constipation alternating with diarrhea, abdominal distention, anorexia, and a low-grade fever. • HESI HINTS: o Diverticulitis is an inflammation of the diverticula (pouches), which can lead to perforation of the bowel. o Nutritional Therapy: Acute phase - NPO, graduating to liquids Recovery phase: No fiber or foods that irate the bowel Maintenance phase: High fiber diet with bulk forming laxatives (Metamucil) to prevent pooling of foods in the pouches where they can become inflamed; avoid small, poorly digested foods such as popcorn, nuts, and seeds. Increase fluids to 3L a day. 19) DVT (postop prevention) • To prevent postop DVT’s occurring in patients implement the following: • Early ambulation & performing regular leg exercises. If the patient is on bed rest you want to make sure to turn patient q2h. Compression stockings are part of prevention in the hospital setting after surgery to discharge. Intermittent compression devices are inflatable boots or sleeves that will compress the calf, thigh, or foot to improve venous return. Anticoagulants can be used as drug therapy for prevention of DVT’s. The goal for this therapy is to prevent the clot formation; prophylactically and when there is a confirmed DVT these medications are used to prevent new clot development, spread of the clot, and embolization. Signs and symptoms for a DVT include tenderness and redness in the calf area, asymmetry- inspect the legs from groin to feet and measure the diameters of the calves, and warm skin. Avoid restrictive clothing, teach to use electric razors (if on anticoagulants), and avoid moving or disrupting established clots. • HESI HINTS: o Advise patient to avoid straining, aspirin, and NSAIDS o Dietary precautions of taking Coumadin: clients may ingest foods high in vitamin K to maintain therapeutic blood levels based on their dietary intake. o Heparin prevents the conversion of fibrinogen to fibrin and prothrombin to thrombin inhibiting the clotting factor; because the clotting factor is prolonged, do not cause tissue trauma that can lead to bleeding. 20) External fixation (perfusion complications) • Metal pins are inserted into the bone and attached to external rods that will stabilize the fracture until surgery. This procedure is used to salvage extremities that would otherwise require amputation. Always assess the perfusion to the lower extremities using the 5 P’s; pallor, pulse, pain, paresthesia, and paralysis. o Pallor - a change in skin color caused by decreased perfusion blood supply; there is an arterial insufficiency. o Pain - Early sign of perfusion complications. The pain will be so severe that it is not relieved by any medications; pressure can cause this. o Paralysis - loss of movement caused by pressure on the nerves. o Paresthesia - This is a late sign of perfusion complications! Tingling and numbness occur as a result of the nerve supply being cut off causing neurovascular damage. o Pulselessness - Late sign of perfusion complications. Slow capillary refill times because of the pressure occurring on the blood vessels. This will indicate vascular dysfunction. • HESI HINTS: o Patients that are in traction (bucks or skeletal) - A trapeze bar can be offered to the client to help move the unaffected side of the body; this will give the client some independence. o Remember when assessing perfusion - assess the peripheral pulses at the foot. o Nursing intervention for a patient that complains of pain would be to administer the PRN pain medications; this will allow the nurse to see if the medication relieves the pain or not; assessing for perfusion. 21) Hyperparathyroidism and calculi • Hypercalcemia (high serum calcium) is caused by hyperparathyroidism in about two thirds of persons. Malignancies, especially from hematologic, breast, and lung cancers, cause the remaining third. Malignancies lead to hypercalcemia through bone destruction from tumor invasion or tumor secretion of parathyroid-related proteins, which stimulate calcium release from bones.7 More rare causes include thiazide diuretic use, prolonged immobilization, and increased calcium intake (e.g., use of calcium-containing antacids). Excess calcium acts like a sedative, leading to reduced excitability of muscles and nerves. Neurologic manifestations begin with fatigue, lethargy, weakness, and confusion and progress to hallucinations, seizures, and coma. Disturbances in cardiac conduction can lead to dysrhythmias, including heart block and ventricular tachycardia. Table 16-7 lists the causes and manifestations of hypercalcemia. • Management depends on the degree of hypercalcemia, patient’s condition, and the underlying cause. Patients with mild hypercalcemia should stop any medications related to hypercalcemia, start a diet low in calcium, increase weight-bearing activity, and maintain adequate hydration. The patient must drink 3000 to 4000 mL of fluid daily to promote the renal excretion of calcium and decrease the chance of kidney stone formation. Fluids that promote urine acidity (cranberry or prune juice) will help to prevent formation of stones. • serum calcium and phosphate levels by stimulating bone resorption of calcium, renal tubular reabsorption of calcium, and activation of vitamin D. Thus oversecretion of PTH is associated with increased serum calcium levels. Primary hyperparathyroidism affects 25 of 100,000 persons per year. • Hyperparathyroidism is classified as primary, secondary, or tertiary. o Primary hyperparathyroidism is due to an increased secretion of PTH leading to disorders of calcium, phosphate, and bone metabolism. The most common cause is a benign tumor (adenoma) in the parathyroid gland. Patients who have previously undergone head and neck radiation have an increased risk of developing a parathyroid adenoma. Long-term lithium therapy is also associated with primary hyperparathyroidism. The peak incidence of primary hyperparathyroidism is in the 40s and 50s. Women are twice as likely to develop primary hyperparathyroidism as men. o Secondary hyperparathyroidism is a compensatory response to conditions that induce or cause hypocalcemia, the main stimulus of PTH secretion. These conditions include vitamin D deficiencies, malabsorption, chronic kidney disease, and hyperphosphatemia. o Tertiary hyperparathyroidism occurs when there is hyperplasia of the parathyroid glands and a loss of negative feedback from circulating calcium levels. Thus there is autonomous secretion of PTH, even with normal calcium levels. This condition is seen in patients who have had a kidney transplant after a long period of dialysis treatment for chronic kidney disease (see Chapter 46). Excess levels of circulating PTH usually lead to hypercalcemia and hypophosphatemia. Multiple body systems are affected (Table 49-12). Decreased bone density can occur because of the effect of PTH on osteoclastic (bone resorption) and osteoblastic (bone formation) activity. In the kidneys the excess calcium cannot be reabsorbed, leading to increased urinary calcium levels (hypercalciuria). This urinary calcium, along with a large amount of urinary phosphate, can lead to calculi formation. • Clinical Manifestations and Complications of Clinical manifestations range from an asymptomatic person (diagnosed through testing for unrelated problems) to a patient with overt symptoms.21 The manifestations are associated with hypercalcemia (Table 49-12). Loss of appetite, constipation, fatigue, emotional disorders, shortened attention span, and muscle weakness, particularly in the proximal muscles of the lower extremities, are often noted. Complications include osteoporosis, renal failure, kidney stones, pancreatitis, cardiac changes, and long bone, rib, and vertebral fractures. 22) Hypothyroid and depression • Hypothyroidism is a deficiency of thyroid hormone that causes a general slowing of the metabolic rate. About 4% of the U.S. population has mild hypothyroidism, with about 0.3% having more severe disease. Hypothyroidism is more common in women than men. Subclinical hypothyroidism occurs when the TSH is greater than 4.5 mU/L, but the thyroxine (T4) levels are normal. Up to 10% of women older than 60 years have subclinical hypothyroidism.16 Patients with overt hypothyroidism have elevated TSH and decreased thyroxine levels. Critically ill patients may present with nonthyroidal illness syndrome (NTIS).17 Those with NTIS have low T3, T4, and TSH levels. Iodine deficiency is the most common cause of hypothyroidism worldwide. In the United States, the most common cause of primary hypothyroidism is atrophy of the thyroid gland. This atrophy is the end result of Hashimoto’s thyroiditis or Graves’ disease. These autoimmune diseases destroy the thyroid gland. Hypothyroidism may also develop after treatment for hyperthyroidism, specifically thyroidectomy or RAI therapy. Drugs such as amiodarone (Cordarone), which contains iodine, and lithium, which blocks hormone production, can cause hypothyroidism. • Clinical Manifestations Regardless of the cause, hypothyroidism has common features. It has systemic effects characterized by a slowing of body processes. Manifestations vary, depending on the severity and the duration of thyroid deficiency as well as the patient’s age at the onset of the deficiency. Symptoms may develop over months to years, unless hypothyroidism occurs after a thyroidectomy, after thyroid ablation, or during treatment with antithyroid drugs. The patient is often fatigued, lethargic, and experiences personality and mental changes, including impaired memory, slowed speech, decreased initiative, and somnolence. Many appear depressed. Weight gain is most likely a result of a decreased metabolic rate. In the older adult, the typical manifestations of hypothyroidism (fatigue, cold and dry skin, hoarseness, hair loss, constipation, and cold intolerance) may be attributed to normal aging. For this reason, the patient’s symptoms may not raise suspicion of an underlying condition. Older adults who have confusion, lethargy, and depression should be evaluated for thyroid disease. The mental sluggishness, drowsiness, and lethargy of hypothyroidism may progress gradually or suddenly to a notable impairment of consciousness or coma. This situation, termed myxedema coma, is a medical emergency. Myxedema coma can be precipitated by infection, drugs (especially opioids, tranquilizers, and barbiturates), exposure to cold, and trauma. It is characterized by subnormal temperature, hypotension, and hypoventilation. Cardiovascular collapse can result from hypoventilation, hyponatremia, hypoglycemia, and lactic acidosis. For the patient to survive myxedema coma, vital functions must be supported and IV thyroid hormone replacement administered. Self- Perception–Self-Concept Pattern. Many endocrine disorders may affect a patient’s self-esteem because of associated changes in physical appearance. For example, weight gain associated with hypothyroidism or exophthalmos and goiter associated with hyperthyroidism can cause problems related to body image. • Role-Relationship Pattern. Questions related to roles and relationships can highlight depression, chronic fatigue, and sleep disorders. With chronic fatigue, depression and anxiety, patients and their families will experience stressed relationships. Questions related to home life and the patient’s ability to fulfill their role in the family will aid in the identification of these disorders. 23) Liver abscess • Couldn’t find much on liver abscess in the book beside referencing septic shock I put some of the information and a couple of websites with info. o https://www.slideshare.net/nuorn/liver-abscess-5483030 o https://www.slideshare.net/farooqmarwat/live-abscess 24) Melanoma and patient teaching • Skin cancer is the most commonly diagnosed cancer.3 Skin cancers are either nonmelanoma or melanoma. The fact that skin lesions are so visible increases the likelihood of early detection and diagnosis. Early detection and treatment can often lead to a highly favorable prognosis. Teach patients to self-examine their skin at least on a monthly basis. The cornerstone of skin self- examination is the ABCDE rule.4 Examine skin lesions for Asymmetry, Border irregularity, Color change and variation, Diameter of 6 mm or more, and Evolving in appearance (Fig. 23-2). Emphasize that a persistent skin lesion that does not heal and lesions once flat and now raised, once small and recently growing, or changing in appearance are warning signs. These lesions must be examined by an HCP. • Clinical Manifestations About one fourth of melanomas occur in existing nevi or moles; about 20% occur in dysplastic nevi (Table 23-4). Melanoma frequently occurs on the lower legs and backs in women and on the trunk, head, and neck in men. Because most melanoma cells continue to produce melanin, melanoma tumors are often dark brown or black. Patients should consult their HCP immediately if their moles or lesions show any of the clinical signs (ABCDEs) of melanoma (Fig. 23-2). Any sudden or progressive change or increase in the ABCDE rule must be evaluated. • The ABCDEs of melanoma. A, Asymmetry: one half unlike the other half. B, Border irregularity: edges are ragged, notched, or blurred. C, Color: varied pigmentation; shades of tan, brown, and black. D, Diameter: greater than 6 mm (diameter of a pencil eraser). E, (not pictured) Evolving; changing appearance (change in shape, size, color, or other characteristic is noted over time). • Malignant Melanoma o Neoplastic growth of melanocytes anywhere on skin, eyes, or mucous membranes o Classification according to major histologic mode of spread o Potential invasion and widespread metastases o Irregular color, surface, and border Variegated color, including red, white, blue, black, gray, brown o Flat or elevated. Eroded or ulcerated o Often <1 cm in size o Most common sites in males are back, then chest. In females are legs, then back (Fig. 23- 2) o Surgical excision and possible sentinel lymph node evaluation o Possible use of adjuvant therapy after surgery if lesion >1.5 mm in depth o Correlation between survival rate and depth of invasion o Poor prognosis unless diagnosed and treated early o Spreading by local extension, regional lymphatic vessels, and bloodstream • The most important prognostic factor is tumor thickness at the time of diagnosis. Two methods to determine thickness are currently in use. The Breslow measurement indicates the depth of the tumor in millimeters (Fig. 23-4). The Clark level indicates the depth of invasion of the tumor; the higher the number, the deeper the melanoma. Treatment depends on the site of the original tumor, stage of the cancer, and patient’s age and general health. The staging of melanoma (stages 0 to IV) is based on tumor size (thickness),nodal involvement, and metastasis. In stage 0 the melanoma is confined to one place (in situ) in the epidermis. Melanoma is nearly 100% curable by excision if diagnosed at stage 0. The 5-year survival rate depends on sentinel node biopsy results, which indicate if metastasis has occurred. The presence of metastasis in the sentinel lymph 25) MI (use of thrombolytics) • A myocardial infarction (MI) occurs because of abrupt stoppage of blood flow through a coronary artery from a thrombus caused by platelet aggregation. This causes irreversible myocardial cell death (necrosis) in the heart muscle beyond the blockage (Figs. 33-8 and 33-9). • Most MIs occur in the setting of preexisting CAD • A STEMI caused by an occlusive thrombus creates STelevation in the ECG leads facing the area of infarction (seeFigs. 35-28 and 35-30). o A STEMI is an emergency situation. In order to limit the infarct size, the artery must be opened within 90 minutes of presentation. This can be done either by PCI or thrombolytic (fibrinolytic) therapy. o PCI is the first-line treatment if a hospital is capable of performing PCI. • NSTEMI, caused by a nonocclusive thrombus, does not cause ST segment elevation on the 12- lead ECG. Patients may or may not develop ST-T wave changes in the leads affected by the infarction. o NSTEMI patients do not go to the catheterization laboratory emergently but usually undergo the procedure within 12 to 72 hours if there are no contraindications. o Thrombolytic therapy is not indicated for NSTEMI patients. Thrombolytic therapy works by lysing infarct artery thrombi and achieving reperfusion, thereby reducing infarct size, preserving left ventricular function, and improving survival. 26) Nephrectomy postop management • Respiratory Status - auscultate the lungs to detect “wet” sounds indication of infections; demonstrate method of splinting incision for comfort when coughing and deep breathing. [Rationale: Flank incision cause pain with both inspiration and expiration. Therefore client avoids deep breathing and coughing, this can lead to respiratory difficulties, including pneumonia] • Circulatory Status- Check vital signs to de early signs of bleeding; monitor skin color and temp (pallor and cold skin are signs of shock); monitor urinary output ( decreases with circulatory collapse); monitor surgical site for frank bleeding [Rationale: the kidney is very vascular, bleeding is a constant threat, circulatory collapse will occur with hemorrhage and can occur quickly] • Pain relief status- administer narcotic analgesics as needed to relieve pain [Rationale: relief of pain will improve client’s cooperation with deep breathing exercises and early ambulation.] • Urinary status- Check output and drainage from all tubes; maintain accurate and stick I&O [Rationale: mechanical drainage of bladder will be implemented post surgery 27) Iron deficiency and diet choices/ education • Instruct in food selection and preparation to maximize intake of: Iron [ red meats, organ meats, whole wheat products, spinach and carrots (what what??)]; Folic acid [ green veggies, liver and citrus fruits]; Vitamin b12 :[ glandular meats {liver, brain, kidneys, sweetbreads- clearly a zombie diet} yeast, green leafy veggies, milk and cheese]; Instruct in need for Rx vitamin supplements: take iron on a empty tummy ( it enhances absorption- 1 hour pre meal and 2 hours post meal); Give vitamin C to enhance absorption; Administer B12 and folic acid orally except to clients with Pernicious Amenia who receive B12 PARENTALLY (a shot in the booty or hip does quite well); If parentally Iron is required... use Z track method (to prevent staining the skin. your pts will thank you.. can be permanent and that’s no bueno); Educate your pt about the fact that iron supplements may cause GI upset, and cause black stools; Give liquid iron threw a straw and immediate oral care to prevent teeth staining (cause we all know that’s a sexy look ); When giving Iron. DO use z track method and do use air bubble to avoid withdrawing medication into subcut tissue..DONT use DELTOID muscle, and DON’T massage the injection site 28) Osteomalacia diet • Eat foods high in Vitamin D Oily fish [Salmon, Mackerel, Sardines]; egg yolks; foods fortified with Vitamin D [cereal, bread, milk and yogurt]; vitamin D and calcium supplements (Consult your md before starting, your situation make require precautions.) 29) Parkinson’s diet • Soft, easy to chew foods, that are easy to swallow, thickened liquids to prevent or decrease aspiration /choking risk. 30) Periop care (goal with preoperative support) • The preoperative period includes client care before surgery (pre op); during surgery (intra op) and after surgery (post op): • Nurses Role: Educate and advocate; Reduce anxiety; Promote an uncomplicated peri-op period for Pt and family; Surgery is performed under aseptic conditions in with a hospital or an alternative setting (ambulatory center, HCP office); Pt safety is a serious concern during peri-op period; • History taking Pre-op: Age; Allergies meds: OTC, RX and herbals; topical antiseptics (esp Iodine); Current meds: OTC, RX and herbals (ask about ALL MEDICATIONS, many pts will exclude herbals and OTC because they don’t realize the will interact with other meds..); Pts PMH and Surgical hx, any problems they have had or immediate family members (like are you going to wake and start swinging on me or go hyperthermic {remember Malignant Hyperthermia runs in families but some pts might not know so use plain laymen’s terms and ask about PROBLEMS from anesthesia.}); tobacco, alcohol and drug use; Understanding of surgical procedure and risks involved ( if pt doesn’t STOP and call the Doc..he/she needs to explain it!!); coping resources; Cultural and ethical factors that might affect surgery. • Peri-op teaching: Regulations regarding valuables, jewelry, dentures, and hearing aids; Food and fluid restrictions SA NPO after midnight per RX of Doc; clear liquids may be given up to 6 hours post surgery for the NON RISK pt per RX of doc; Invasive procedures SA Urinary catheters, IVs, NG tubes, enemas and douches; Pre-op medications; Operating Room (THE LIGHTS THE LIGHTS ARE BLINDING and it’s cold), transportation, skin prep, post anesthesia. • Post-op stuffs: Respiratory Care (ventilation, incentive spirometer {10 times an hour while awake}, deep breather and splinting; Activity, ROM, leg exercises, early ambulation, and turning; Pain control {Pills, PCA or IM meds}; Dietary Restrictions; ICU/PACU orientation; • Pre-op Checklist: Consents [informed, surgical,] Signed within 24 hours and good for 45 days, signature must be obtained BEFORE narcotics or medications affecting cognition. Site marked by surgeon, before incision all team members confirm ID, Procedure, site of surgery, and consents [Time out]; H&P (good for 30 days); Chest radiograph; ECG; and UA preformed when required; H&H, F/E , glucose, type/crossmatch for blood; Old chart on hand; ID band ON PT with correct information, Contacts, glasses, dentures, partials, wigs, jewelry, artificial eyes, prostheses, make up and nail polish removed; Pt has voided or been cathed.; Pt in gown; VS taken; Pre-medications including ABX given; skin prep performed [wash skin with soap and water, do not remove hair unless it will interfere with the operation and remove it with electric clippers, follow shave with scrub and or shower antibacterial solution; Signature of nurse that everything is completed. • Intra-op: (from operating room to PACU admission): Maintain quiet during induction; maintain safety [Conduct pt id Right pt, right procedure, right anatomical site]; Insure sponge, needle, an instrument count is correct; Counts are done and verified and documented by two personnel Before, during, before closing incision and end of surgery; position pt to prevent injury; strictly adhere to asepsis during all procedures; ensure adequate function suction; take responsibility for correct labeling, handling, and deposition of any and all specimens; Monitor Physical status [ if excessive blood loss occurs, calculate risk to pt; report changes in Pulse, temp, respirations, and bp to surgeon and anesthesiologist/CRNA ASAP, ensure proper positioning of pt]; Provide emotional support to pt and family before/during/after; arrange to provide information and updates to family if complications, unexpected results or prolonged surgical time occur; communicate emotional state of pt to ALL healthcare team members. • Post-op: (admission from PACU until recovery)- on arrival to PACU- assess VS, LOC, Skin color and condition, dressing location and condition, IV fluids, drainage tubes, position, and O2 levels [remember what Ms D said use your eye balls and assessment skills don’t rely on your monitors or O2 saturation, first sign of Respiratory Failure ANXIETY]; Immediate post-op nursing care: monitoring for signs of shock and hemorrhage {hypotension, narrow pulse pressure, rapid weak pulse, cold moist skin, increased cap refill, decreased urine output; positioning of pt in lateral position (unless contraindicated; prevention of aspiration and allowing pt to cough,) side rails up; providing warmth with heated blanket; managing N/V with meds and NG suction; managing pain; check with anesthesiologist about intra-op meds before admin of pain meds; determine intra-op irrigations, and instillations of drains to help determine amount of drainage on dressing and in drains. • Common post-op complications: Urinary Retention (typically 8-12 hours post surgery)- monitor hydration and encourage oral intake, offer bedpan and assistance to commode; Pulmonary Problems: Atelectasis; Pneumonia and Embolus (typically 1-2 days post op): assist pt to turn, cough, deep breathe q 2; keep pt hydrated; early ambulation; early IS use. Wound healing problems: (5-6 days post op): teach splinting of incision when coughing, monitor for s/s of infection, malnutrition, dehydration, high protein diet [remember high protein diet and vitamin c aid the body in healing]; UTI (5-8 days post op): oral fluid intake, empty bladder q4-6, monitor I&O, avoid catheterization if possible. Thrombophlebitis (6-14 days post op): leg exercises q 8, early ambulation, Ted hose, SCDs, Remove ted hose q 8 and reapply, avoid any pressure that may occlude venous flow, do not raise knee gatch, do no place pillows under knees, low dose heparin. • Decreased GI peristalsis: Constipation, Paralytic Ileus (2-4 days post-op): NG tube (decompress), Limit use of Narcotics (they decrease peristalsis ), encourage ambulation. HESI HINT: wound dehiscence - separation of wound edges, most commonly vertical wounds; occurs after post op period, pts own granulation tissue is taking over the wound after absorption of the sutures. Evisceration of wound is protrusion of intestinal contents (of ab wound), more likely in older, diabetic, obese, malnourished and prolonged paralytic ileus. 31) Prostatectomy (cath leaking) • With a radical prostatectomy the entire prostate gland, seminal vesicles and part of the bladder neck are removed. After surgery, the patient has an indwelling catheter with a 30-mL balloon placed in the bladder. A drain is left in the surgical site to aid in removal of drainage from the area. Two major adverse outcomes after a radical prostatectomy are erectile dysfunction and urinary incontinence. Problems with urinary control may occur for the first few weeks after surgery because the bladder must be reattached to the urethra after the prostate is removed. Instruct the patient not to urinate around the catheter because this increases the likelihood of spasm. 32) Restless Leg syndrome (iron and ferritin) • Restless Leg Syndrome is a relatively common condition characterized by unpleasant sensory and motor abnormalities of one or both legs. RLS is believed to be related to a dysfunction in the brain’s basal ganglia circuits that use the neurotransmitter dopamine, which controls movements. Abnormal iron metabolism or brain iron deficiencies related to low serum ferritin may also play a role in RLS. 33) Secondary Tumor • Secondary tumors are the same type of cancer as the original cancer. For example, cancer cells may spread from the breast (primary cancer) to form new tumors in the lung (secondary tumor). The cancer cells in the lung are just like the new ones in the breast. 34) TURP (discharge planning) • Teaching of how to care for an indwelling catheter, managing urinary incontinence, maintaining adequate oral fluid intake, observing for signs and symptoms of UTI and wound infections, preventing constipation, avoid heavy lifting, and refraining from driving or intercourse after surgery. The patient may experience changes in sexual function after surgery as well such as retrograde ejaculation and erectile dysfunction. • The bladder may take up to 2 months to return to its normal capacity so instruct the pt to drink at least 2-3 L of fluid per day and to avoid irritants such as caffeine, citrus juices, and alcohol. 35) Basic nursing care and MRI • Provides both anatomic and hemodynamic information and can be used in conjunction with contrast medium. Before an MRI screen pt for metal parts and pacemaker in the body. Instruct the pt on the need to lie very still for up to 1 hour. Sedation may be necessary if pt is claustrophobic. 36) Obesity and cardiac disease – Med Surg book page 879 • Many health problems occur in obese people and at higher rates. • Obesity is associated with all of the following cardiovascular complications: o Hyperlipidemia o Sudden cardiac death / MI o Right sided-heart failure o Left ventricular hypertrophy o Coronary artery disease o Deep venous thrombosis o Atrial fibrillation o Hypertension o Cardiomyopathy o Venous stasis o Varicose veins 37) Venous leg ulcers (PVD) • Necrotic crater-like lesion usually found on lower leg at medial malleolus. Characterized by slow wound healing. Med surg book page 668 • Ulcers form over boney prominences, primarily toes, feet, and lower legs. MS page 804. • Nonhealing arterial ulcers and gangrene are the most serious complications. Amputation may be needed if infection cannot be controlled. MS page 804. • Causes: poor venous return, varicose veins, incompetent venous valves. MS book page 668 38) Complications with rhinoplasty • Pt may have difficulty adjusting to body image o Subtle swelling may be slow to resolve, delaying the achievement of a full cosmetic result for up to 1 year. • Edema and ecchymosis common – cold compresses and elevation of the heal can help minimize swelling and discomfort. • Pt needs education about preventing bleeding: o No nose blowing o No swimming o No heavy lifting o No strenuous exercise 39) TPN indications • Total Parenteral Nutrition: the administration of nutrients directly into the bloodstream, used when the GI tract can’t be used for ingestion, digestion, and absorption of essential nutrients. (Page 869 Med Surg Book) • Administered through a central intravenous access site or a peripherally inserted central venous catheter (PICC) (Page 319 HESI book) • Some complications consist of hyperglycemia, electrolyte imbalance, infection, and dehydration (Page 319 HESI Book) • TPN is used in short bowel syndrome which is inadequate absorption, GI fistula, bowel obstruction, prolonged bowel rest, severe malnutrition 40) Postop abdominal assessment • Avoiding postoperative catheterization, increasing oral fluid intake, emptying bladder every 4-6 hours, early ambulation are nursing interventions to prevent postoperative UTI (Page 59 red HESI book) • Early ambulation, limiting use of narcotic analgesics, NG tube decompression are nursing/medical interventions to prevent postoperative paralytic ileus. (Page 59 red HESI book) • Check for signs and symptoms of delayed gastrointestinal emptying, distention and flatulence, Hiccups, Nausea and Vomiting, and a postoperative ileus (Page 332 Med Surg book Fig. 19-1) • Ask patient about feeling nausea and if present assess severity using a verbal descriptor or numerical scale; if vomiting occurs assess quantity, characteristics, and color; assess for distention and bowel sounds; bowel sounds are frequently absent or diminished immediately in the postoperative period so auscultate all four quadrants to determine presence, frequency, and characteristics of sounds; Normal bowel motility is accompanied by the passage of gas or stool and the patient’s ability to tolerate oral intake without complaints of nausea or vomiting. (Page 342 Med Surg book) 41) Renal calculi (patient education) • Nephrolithiasis (kidney stone disease) Calculus refers to the stone lithiasis refers to stone formation. 5 categories: Calcium phosphate, Calcium oxalate, Uric acid, Cystine, and Struvite (magnesium ammonium phosphate). Most common is calcium stones but they can be mixed. Calculi can be found in various places in the urinary tract. (Page 1045 Med Surg book) • HESI Hint: Percutaneous nephrostomy is a needle or catheter that’s inserted through the skin into the calyx of the kidney. The stone may be dissolved by percutaneous irrigation with a liquid that dissolves the stone or by ultrasonic sound waves (lithotripsy) that can be directed through the needle or catheter to break up the stone, which then can be eliminated through the urinary tract. (Page 97 red HESI book) • Develop and implement a teaching plan that includes follow-up care because stones tend to recur, maintain a high fluid intake of 3 to 4 L/day, follow prescribed diet (based on composition of stone), avoid long periods of remaining in supine position. (Page 97 red HESI book) • HESI Hint: Location of the pain can help to determine the location of the stone. Flank pain usually means the stone is in the kidney or upper ureter. If the pain radiates to the abdomen or scrotum, the stone is likely to be in the ureter or bladder. (Page 96 red HESI book) 42) Antiinfectives and athletes foot • Tinea Pedis: various dermatophytes, commonly called athlete’s foot. Interdigital scaling and maceration. Scaly plantar surfaces sometimes with erythema and blistering. May be pruritic and possibly painful. Topical antifungal cream, gel, solution, spray, or powder are used to treat. (Page 418 Med Surg book) 43) Psoriasis PUVA (photochemotherapy) • Psoriasis: autoimmune chronic dermatitis that involves excessively rapid turnover of epidermal cell. Family predisposition and usually develops before age 40. It’s sharply demarcated silvery scaling plaques on reddish colored skin commonly on the scalp, elbows, knees, palms, soles, and fingernails. It itches, burns, and painful. It can be localized or general and intermittent or continuous. Symptoms can vary from mild to severe. (Page 419 Med Surg book) • Psoralen plus UVA light (PUVA): this is a photosensitizing drug given to patients for a prescribed amount of time before exposure to UVA. Given 2-4 times a week. Side effects of PO psoralen include nausea and vomiting, sunburn, and persistent pruritis. Perform frequent skin assessments because erythema is side effect of treatment. Use extreme caution in patients with liver or renal disease because slower metabolism and excretion can lead to prolonged photosensitivity. Patients need prescription protective eyewear that blocks 100% of UVL because the lens of the eye absorbs psoralen. Use eyewear for 24 hours after taking medication when outdoors or near a bright window. Continuous monitoring is needed because of the immunosuppressive effects of PUVA which include an increased risk of SCC (squamous cell carcinoma), BCC (basal cell carcinoma), and melanoma. (Page 420 Med Surg book) 44) MS and multiple falls • Multiple Sclerosis: demyelinating disease resulting in the destruction of CNS myelin and consequent disruption in the transmission of nerve impulses (Page 160 HESI book) • HESI HINT: Symptoms involving motor function usually begin in the upper extremities with weakness progressing to spastic paralysis. Bowel and bladder dysfunction occurs in 90% of cases. MS is more common in women. Progression is not “orderly.” (Page 161 HESI book) • HESI HINT: Drug therapy for MS clients: ACTH, cortisone, cyclophosphamide (Cytoxan), and other immunosuppressive drugs. Nursing implications for administration of these drugs should focus on the prevention of infection. (Page 161 HESI book) • Teach client that for muscle spasticity, stretch-hold-relax exercises are helpful, as are riding a stationary bicycle and swimming; take precautions against falls. Orient client to environment and teach strategies to maximize vision. (Page 161 HESI book) • Patients describe muscle weakness in the extremities which also causes problems with coordination and balance increasing the effects of being able to walk or stand. It can also cause partial or complete paralysis in worst cases. (Page 1384 Med Surg book) • It causes generalized muscle weakness, muscle fatigue, tingling and numbness, and ataxia (clumsiness.) (Page 1386 Med Surg book) 45) HDY and BP • hypotension can occur during hemodialysis due to rapid removal of vascular volume (hypovolemia), decreased cardiac output, and decreased systemic vascular resistance. The drop in BP during dialysis may precipitate lightheadedness, nausea, vomiting, seizures, vision changes, and chest pain from cardiac ischemia. The usual treatment for hypertension includes decreasing the volume of fluid being removed and infusion of 0.9% saline solution. p. 1090 46) Pyelonephritis and priority nursing • pyelonephritis is a kidney infection that is usually caused by E. coli. It starts in the lower urinary tract and moves up to the kidney. Priority nursing involves close monitoring for symptoms of septic shock (hypotension, tachycardia, and fever). A urinalysis, CBC, urine cultures, blood cultures, and ultrasounds are usually done. Parenteral antibiotics are usually given initially in the hospital. Opioid analgesics are given for pain. 1038 47) Cataract and postop care • Postoperative care includes topical antibiotic, topical corticosteroid or other anti-inflammatory agent, mild analgesia if necessary, eyepatch or shield and activity as prescribed by patient’s surgeon. Many physicians prefer that the patient avoid activities that increase the IOP, such as bending or stooping, coughing or lifting. p. 374 48) DM and current illness • In people with diabetes, wounds tend to heal more slowly and progress more quickly. It’s important to know complications associated with DM, and to closely monitor cuts, sores, infections, or any other illness. Common complication of diabetes are; cardiovascular disease, nerve damage (neuropathy), kidney damage (nephropathy), eye damage (retinopathy), foot damage, skin conditions, and hearing impairment. 49) Peptic ulcer signs/symptoms • Gastric ulcers has a burning or gaseous pressure in the epigastrium, pain occurs 1 to 2 hours after meals, if penetrating ulcer, food will aggravate or add more discomfort. There are normal to decreased gastric secretions. Nausea and vomiting, pyrosis, and weight loss is a common manifestation and it happens more in women. • Duodenal ulcers has a burning, cramping pressure-like pain across the midepigastrium and upper abdomen, and sometimes there’s back pain. Pain occurs 2 to 5 hours after meals and is periodic and episodic. Pain can be relieved with antacids alone or in combination with H2 receptor blocker, and food. There is an increase in gastric secretion. There is usually no weight loss and it occurs more in men. Vomiting not common. p. 912 50) Assessment of chronic hypoxia – MS book page 1613 - 1614 • Monitor for prolonged expirations • Monitor for crackles (pulmonary edema), absent/diminished breath sounds (atelectasis), and pleural friction rub – all suggest underlying cause. • Nasal flaring / increased work of breathing • Use of accessory muscles • Tripoding • SpO2 <80% • Paradoxic chest or abdominal wall movement with respiratory cycle • Cyanosis • Restlessness • Irritability • Altered mental status / confusion • Inceased lactic acid will lead to metabolic acidosis • BP and CO may fall/decrease • Renal function impairment • Edema 51) COPD interventions • Semi Fowlers position • Pursed lip Breathing • Chest physiotherapy • Incentive spirometer • O2 treatment • Bronchodilators: o B2 adrenergic agonist: Albuterol (short acting), salmeterol and formoterol (long acting) • Anticholinergic: ipratropium • Corticosteroids: Prednisone • Leukotriene modifiers: montelukast • Antibiotics • Vaccinations • Smoking cessations • Pulmonary rehabilitation Surgical management of COPD: Bullectomy, Lung volume reduction surgery • Postural drainage: airway clearance • Percussion: clears mucous from airways by vigorous beating mucous loose • Vibration: aimed to improve neuromuscular performance • Huff coughing: forced expiratory technique NEED TO KNOW !!! 52) Glucose monitoring • How to check: o Wash hands find place on the finger that has not been used recently you will be using the side of the and not the center of the pad o Wipe with alcohol, but the finger need stop be dry before puncturing it o Punctures wipe the first drop and use the second to get the reading • When to Check: o Check before meals o 2 hr. after if on insulin to ensure the insulin dose was sufficient. o Monitor when hypoglycemia is suspected o During times of illness check it in 4 hr. intervals o Teach for the PT to monitor before and after exercise 53) Antiinfectives administration and HIV/AIDS • The major drug classifications for HIV include nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), integrase strand transfer inhibitors (INSTIs), protease inhibitors (PIs), non- nucleoside reverse transcriptase inhibitors (NNRTIs), and entry/fusion inhibitors. Treatment regimens can have side effects and frequently interact with other medications. • Management of HIV is complicated by the many opportunistic diseases that can develop as the immune system deteriorates. • Examples of opportunistic diseases include Pneumocystis jiroveci pneumonia (PCP), Mycobacterium avium complex (MAC), and Kaposi sarcoma. • The goals of drug therapy in HIV infection are to decrease the viral load, maintain or raise CD4+ T-cell counts, prevent the development of HIV-related symptoms and opportunistic diseases, and delay disease progression. 54) Colon cancer; intestinal polyps • Adenomatous polyps are characterized by neoplastic changes in the epithelium and are closely linked to colorectal adenocarcinoma. Signs of colon cancer Rectal bleeding, abdominal pain, changes in bowel habits Early detection and removal of polyps is essential Beginning at age 50, both men and women at average risk for developing CRC should have screening tests done to detect both polyps and cancer or tests that primarily detect cancer. Colonoscopy is the gold standard for CRC screening. CRC prognosis and treatment correlate with stage of the disease. Treatments include endoscopic removal, surgical removal alone, surgical removal plus chemotherapy, or palliative chemotherapy for nonresectable CRC. The goals for the patient with CRC include normal bowel elimination patterns, quality of life appropriate to disease progression, relief of pain, and feelings of comfort and well-being. • Familial adenomatous polyposis (FAP) is the most common hereditary polyp disease. 55) MI in women • Light-headedness • Fainting • Dizziness • A pressure in the upper back • Pain or discomfort in one or both arms • Uncomfortable pressure, squeezing, fullness or pain in the center of your chest • A feeling of indigestion or reflux type pain • Feeling sick • Sleep disturbances 56) HF labs • Serum chemistries, cardiac biomarkers [Troponin, creatine kinase(CK), CK-MB, Myoglobin] BNP or NT-proBNP level, liver function test, thyroid function test, CBC, lipid profile, kidney function test, urinalysis. • Altered serum electrolytes (especially Na and K), increased BUN, creatinine, or liver function tests. Increased NT-proBNP or BNP. Chest xray demonstrating cardiomegaly, pulmonary congestion, and interstitial pulmonary edema. Echocardiogram showing increased chamber size, decreased wall motion, decreased EF or normal EF with evidence of diastolic failure. Atrial and ventricular enlargement on ECG. Decreased O2 saturation. 57) Pheochromocytoma • A rare condition caused by a tumor in the adrenal medulla. It effects the chromaffin cells, resulting in excess production of cetacholamines (epinephrine, norepinephrine). The most dangerous immediate effect of the disease is severe hypertension. If left untreated it may lead to encephalopathy, DM, cardiomyopathy, multiple organ failure, and death. • The most striking clinical manifestation is episodic hypertension accompanied by a severe pounding headache; tachycardia with palpitations; profuse sweating; and unexplained abdominal or chest pain. • The simplest and most reliable diagnostics test is a 24-hour urine collection. Measures fractioned metanephrines and cetacholamines. • Primary treatment is removal of tumor. A and B adrenergic receptor blockers are used to control BP for 10-14 days before surgery and will prevent an intraoperative hypertensive crisis. Therapy can cause orthostatic hypotension, so advise pt to make postural changes slowly. 58) Exophthalmos • Eyeball protrusion. Protrusion of globe beyond its normal position within bony orbit. Sclera often visible above iris when eyelids are open. Caused by intraocular or periorbital tumors, or Hyperthyroidism (result of fluid accumulation in eye and retroorbital tissue). 59) AIDS related dementia • Red table 59-2: One of the many causes of Dementia is AIDS. • I searched high and low for more information on this, but this is literally all there is! I’m sorry I don’t have more!) 60) Glomerulonephritis diet • Edema is treated by restricting sodium and fluid intake, and by administering diuretics. Dietary protein may be restricted if there is evidence of an increase in nitrogenous waste (e.g., elevated BUN). The dietary protein restriction varies with the degree of proteinuria. 61) Peritoneal dialysis teaching and care MS book page 1086-1087 • Monitor for s/s of infection: redness at site, tenderness, and drainage – report to HCP. • Report abd pain, cloudy peritoneal effluent, diarrhea, vomiting, abd distention – s/s of peritonitis • Self management skills are usually taught in a 3-7 day training program • Catheters can migrate – report to HCP • Increased abd pressure can cause hernia – report problems to HCP • Regular exercise and strength training can be beneficial for some pts to reduce lower back pain from increased intraabdominal pressure • Pink or slightly bloody effluent is common after peritoneal catheter placement. Bloody effluent overaal several days or the new appearance of blood in the effluent can indicate active intraabdominal bleeding and should be reported to the HCP immediately. 62) Pulmonary suctioning • Suctioning is 'the mechanical aspiration of pulmonary secretions from a patient with an artificial airway in place'. Suctioning is used to obtain mucus and other fluids (secretions) and cells from the windpipe (trachea) and large airways (bronchi) and is typically used in people who are on mechanical ventilation or have problems with nerves or muscles that make coughing less effective for bringing up secretions. Suctioning is used to obtain specimens for microscopic examination or culture when doctors need to identify what organism is causing a lung infection and to help remove secretions from the airways when cough is inadequate. • PROCEDURE: o Insert the catheter through the nose, tracheostomy tube or endotracheal tube. Do not be aggressive when inserting the tube through the nose. Once the catheter has been inserted to the appropriate depth, apply intermittent suction and slowly withdraw the catheter, using a twirling motion as the catheter is withdrawn. 63) Renal lithotripsy • Is a noninvasive procedure used to treat kidney stones that are too large to pass through the urinary tract? It uses ultrasonic energy or shock waves directly to the stone first located with fluoroscopy or ultrasound. The shock waves break a large stone into smaller stones that will pass through the urinary system. • COMPLICATIONS: hemorrhage, sepsis, abscess formation 64) Gout and allopurinol • Allopurinol oral tablet is available as a generic drug and as brand-name drugs. Brand names: Zyloprim and Lopurin. Allopurinol is also given as an injection by a healthcare provider in the hospital. Allopurinol oral tablet is used to treat gout, elevated serum uric acid levels, and recurrent kidney stones. Starting allopurinol can trigger a gout attack as the crystals begin to dissolve. Allopurinol should not be taken during a gout attack. However, if the patient is already taking allopurinol then they should continue the same dose. 65) Intestinal obstruction care • An intestinal obstruction is a potentially serious condition in which the intestines are blocked. The blockage may be either partial or complete, occurring at one or more locations. Obstructions are serious and need to be treated immediately. They may even require surgery. • TREATMENT: o Involves placing a NG tube through the nose into the stomach or intestine to help relieve abdominal distention and vomiting. o Before surgery, IV infusions that contain normal saline solution and potassium should be given to maintain fluid and electrolyte balance. o Sigmoidoscopy may successfully reduce a sigmoid volvulus. Colon decompression catheters may be passed through partially obstructed area via colonoscope to decompress the bowel before surgery. • Nursing assessment: o Take a careful history to obtain information about current symptoms and previous disease manifestations. • Intervention: o assess level of pain, locations, intensity, and duration. o Provide comfortable position and promote restful environment. o Administer analgesics as ordered. o Monitor for signs of dehydration and electrolyte imbalance. 66) Encephalopathy and lactulose • Lactulose appears to inhibit intestinal ammonia production by a number of mechanisms. Colonic metabolism of lactulose to lactic acid results in acidification of the gut lumen. This favors conversion of ammonium (NH4) to ammonia (NH3) and the passage of ammonia from tissues into the lumen. Lactulose is often used in the treatment of hepatic encephalopathy because of its efficacy and the fact that it has few serious side effects. Lactulose appears to inhibit intestinal ammonia production by a number of mechanisms. The conversion of lactulose to lactic acid and acetic acid results in the acidification of the gut lumen 67) IBD care and precautions • Crohn’s Disease Could be caused by combo of environmental factors and genetic predisposition No cure Treatment relies on meds for the acute inflammation and maintaining of remission Surgery is reserved for those unresponsive to meds or w/ life-threatening complications Total proctocolectomy (colon and rectum removed and anus closed w/ permanent ileostomy) o Assessment Abdominal pain (RLQ) Diarrhea, steatorrhea Constant fluid loss Low-grade fever Bowel-perf d/t increasing inflammation Anorexia r/t pain after eating Weight loss, anemia, malnutrition o Interventions Determine bowl elimination pattern, and control diarrhea with diet and medication as needed Diet low-residue, low-fat, high-protein high-calorie diet with NO dairy Vitamin and iron supps Avoid foods that cause diarrhea Avoid smoking, caffeinated beverages, pepper, and alcohol Monitor I’s and O’s and serum electrolytes Weigh at least twice a week Avoid smoking, caffeinated beverages, pepper, and alcohol Monitor I’s & O’s and serum electrolytes Weigh at least twice weekly o HESI Hint • Ulcerative Colitis GI tract usually accounts for only 100-200 mL of fluid loss per day, although it filters up to 8 L per day. Large fluid losses can occur if vomiting or diarrhea exists Causes bowel to narrow, shorten, and thicken due to muscular hypertrophy Diagnosed with sigmoidoscopy and colonoscopy which allows direct examination of the large intestinal mucosa o Assessment Diarrhea Abdominal pain and cramping Intermittent tenesmus (anal contractions) and rectal bleeding Liquid stools containing blood, mucus, and pus (10-20 liquid stools per day) Weakness and fatigue Anemia o Interventions Bowel elimination pattern Low-residue, low-fat, high-protein, high-calorie diet with NO dairy Vitamin and iron supps Avoids foods that cause diarrhea Avoid smoking, caffeinated beverages, pepper, and alcohol Monitor I’s and O’s and serum electrolytes Weigh at least twice a week o HESI hint Opiate drugs tend to depress gastric motility but should be given with caution. Assess for abdominal distention, abdominal pain, abdominal rigidity, signs and symptoms of shock-increased HR, and decreased BP, indicating possible perforation/GI bleed. o Goals of Treatment Rest the bowel Control the inflammation Combat infection Correct malnutrition Alleviate stress Provide symptomatic relief Improve quality of life 68) Rheumatoid arthritis labs • Positive RF in 80% • Autoantibodies formed by an antigen triggering the formation of abnormal IgG • Elevated erythrocyte sedimentation rate (ESR) • Presence of antinuclear antibody (ANA) • C-reactive protein (CRP) indicated by active inflammation • Antibodies to citrullinated peptide (anti-CCP) • Synovial fluid will be slightly cloudy, straw-colored fluid with many fibrin flecks 69) Raynaud’s patient teaching • Preventing of recurrent episodes • Wear loose, warm clothing as protection from the cold • Wear gloves when handling cold objects • Avoid temperature extremes • Immerse hands in warm water often to decrease the vasospasm • Stop using tobacco products and avoid caffeine and vasoconstrictive drugs (cocaine, amphetamines, ergotamine, pseudoephedrine) • Provide patients with stress management strategies as appropriate 70) Testicular cancer • Assessment o Early signs subtle and usually go unnoticed o Feeling of heaviness or dragging sensation in lower abdomen and groin o Painless lump or swelling on the testicle o Late Signs: Low back pain Weight loss Fatigue o HESI Hint High risk for developing testicular cancer in those whose testes have not descended into the scrotum or descended after age 6. Most common symptom is the appearance of a small, hard lump about the size of a pea on the front or side of the testicle. Testicular self-examination (TSE) should be done regularly at the same time every month by all males after 14. • TSE should be done after a shower by gently palpating the testes and cord to look for a small lump. Swelling may also be a sign of testicular cancer. o Interventions Postop after orchidectomy • Observe for hemorrhage • Active movement may be contraindicated Care for clients receiving radiation therapy Encourage genetic counseling • Sperm banking is often recommended before surgery Counsel that sexual functioning is usually not affected because the remaining testis undergoes hyperplasia, producing sufficient testosterone to maintain sexual functioning • Ejaculatory ability may be decreased but orgasm is still possible 71) Eczema triggers • Eczema (atopic dermatitis) is a Type-1, IgE-mediated allergic reaction • Triggers are normally pollen, food, drugs, and/or dust o First exposure causes IgE antibodies to be produced and bind to mast cells and basophils o Subsequent exposures cause the IgE bound to the mast cells and basophils to degranulate the cells and release chemical Review Topics Part 2 72) GI/Hepatic - Liver biopsy – MS book page 850-852 • Purpose: obtain hepatic tissue to use in establishing a dx of cancer or assessing and staging fibrosis or for following the progress of liver disease, such as chronic hepatitis. • Two Types – Open and Closed o Open involves making an incision and removing a wedge of tissue. It is done in the OR. o Closed or needle biopsy is a percutaneous procedure. Site is infiltrated with a local anesthetic and a needle is inserted between the sixth and seventh or eighth and ninth intercostals spaces on the right side. The pt lies supine with the right arm over the head. Instruct pt to expire fully and not breath when the needle is inserted. Ensure informed consent is signed before procedure. Post procedure: • Check v/s after q15mins x2; q30mins x4; q1hr x4. • Keep pt in bed flat for 12-14hrs. • Assess for complications such as bile peritonitis, shock, pneumothorax. 73) Table of GI studies and diagnostics (liver specific)? • Bile formation and excretion Diagnostics studies o Serum bilirubin: measures liver’s ability to conjugate and excrete bilirubin, allowing differentiation in between unconjugated and conjugated bilirubin in plasma. o Urinary bilirubin: measurement of urinary excretion of conjugated bilirubin. (reference interval 0 or negative) • Protein metabolism o Protein (serum): measurement of serum proteins made by liver. o Albumin: 3.5-5.0 g/dl o Globulin: 2.0-3.5 g/dl o Total Protein: 6.4-8.3 g/dl o A/G Ratio: 1.5: 1-2.5:1 o a-Fetoprotein: indications of hepatocellular cancer. <10 ng/ml (<10 mcg/L) o Ammonia: Conversion of ammonia to urea normally occurs in liver. Increase can result in hepatic encephalopathy secondary to liver cirrhosis. 15-45 mcg N/dl • Hemostatic function o Prothrombin time(PT): Determination of prothrombin activity. 11-16 sec o International normalized ratio(INR): standardized system of reporting PT based on a reference calibration model and calculated by comparing the patient’s PT with a control Value. 2-3 is the desired therapeutic level with warfarin depending on laboratory. o Vitamin K: Essential confactor for many clotting factors. 0.1-2.2 ng/ml • Serum Enzymes o Alkaline phosphatase(ALP): originates from bone and liver. Serum levels rise when excretion is impaired because of obstruction in biliary tract. 38-126 u/L depending on method and age. o Aspartate Amino transferase(AST): Elevated I liver damage and inflammation. 10-30 u/L o Alanine aminotransferase(ALT): Elevated in liver damage and inflammation 10-40 u/L o Glutamyl transpeptidase(GGT): Present in bilary tract( not in skeletal or cardiac muscle). Ncrease in hepatitis and alcoholic liver disease. More sensitive or liver dysfunction than ALP. 0-30 u/L • Lipid Metabolism o Cholesterol(serum): Synthesis and excretion by liver. Increase in biliary obstruction. Decrease in cirrhosis and malnutrition. <200 mg/dL varying with age. 74) GI/Hepatic - Hiatal hernia • Is a herniation of the esophagogastric junction and a portion of the stomach into the chest through the esophageal hiatus of the diaphragm. Hiatal hernias are the most common abnormality found on x-ray examination of the upper GI tract. They are common in older adults and occur more often in women. Many factors contribute to the development of hiatal hernia structural changes (weakening of the muscles in the diaphragm around the esophagogastric opening) occur with aging. • Clinical manifestations and complications: some people with hiatal hernia are asymptomatic. When present, manifestations of hiatal hernia are similar to those described for GERD. Complications that may occur with hiatal hernia include GERD, esophagitis, hemorrhage from erosion, stenosis, ulcerations of the herniated portion of the stomach, strangulation of the hernia, and regurgitation with tracheal aspiration. • Diagnostic studies: An esophagram (barium swallow), endoscopic visualization, other tests that are done are the same as those for GERD. • Nursing and interprofessional management: teach the patient to reduce intraabdominal pressure by eliminating constricting garments and avoiding lifting and straining, provide an acceptable LES pressure, and prevent movement of the gastroesophageal junction. • Gerontological considerations: Changes in lifestyle, including eliminated factors such as caffeinated containing beverages and chocolate and elevating the head of the bed on blocks may be challenging for the older adult. Laparoscopy procedures reduce the risk associated with surgical repair. An older patient with cardiovascular and pulmonary problems may not be a good candidate for surgical intervention. 75) Stroke-dysphagia-communication issues • Stroke can affect many body functions. The gag reflex may be impaired due to dysphagia, the inability to swallow foods or liquids arising from the throat or esophagus. Dysphagia ranges from mild difficulty to complete and painful blockage. Patients that have experienced a stroke must be assessed by a speech therapist to rule out dysphagia; the therapist will perform a swallowing evaluation before the patient’s oral intake is initiated. • During the acute stage of a stroke, the role of a nurse is to meet the patient’s psychological needs. Speech, comprehension, and language deficits are the most difficult problems for the patient and caregiver. The patient diagnosed with a stroke may experience aphasia, which may be receptive (loss of comprehension), expressive (inability to produce language) or global aphasia (total inability to communicate). Aphasia occurs when the stroke damages the dominant hemisphere of the brain that involves language comprehension. • Many stroke patients also experience dysarthria, a disturbance in the muscular control of speech. Impairment may involve pronunciation, articulation, and phonation. Dysarthria does not affect the meaning of communication or the comprehension of language, but it does affect the mechanics of speech. Some patients experience a combination of both, aphasia and dysarthria. 76) Teaching - Venous leg ulcers-teaching • Patient and caregiver teaching is very important because it should focus on self-care measurements. Teach the patient and caregiver to avoid trauma to the limbs and teach them proper foot and leg care to avoid additional skin trauma. Patients who have had dried, flaky, itchy skin should use daily moisturizer to decrease the itching and also to prevent cracking of the skin. Teach patient how to assess the wound for signs of infection with each dressing change. Be certain to discuss activity guidelines and proper limb positioning. Tell patients with CVI with or without a venous ulcer to avoid standing or sitting for long periods. Standing or sitting with the legs in a dependent position decreases blow flow to the lower extremities. Also, tell patients to frequently elevate their legs above the level of the heart to reduce edema. Encourage patient to begin a daily walking program once the ulcer heals. 77) venous vs arterial disease chart comparison in cardiac chapter Characteristics Peripheral Artery Disease Venous Disease Peripheral Pulses Decreased or absent Present, may be difficult to palpate with edema Capillary refill >3 sec <3 sec Ankle-brachial index Less than or equal to 90 >0.90 Edema Absent unless leg constantly in dependent position Lower leg edema Hair Loss of hair on legs, feet and toes Hair may be present or absent Ulcer Located usually in tip of toes or footrounded with minimal drainage, tissue looks blck or pale pink granulation Near medial malleoulus, irregular shape, moderate to large amount of drainage, tissue yellow slough or dark red Pain Intermittent claudication or rest pain in foot Dull ache or heaviness in calf or thigh Nails Thickened =, brittle Normal or thickened Skin Color Dependent rubor, elevation pallor Bronze-brown, varicose veins may be visible Skin Texture Thin, shiny, taut Skin thick, hardened, indurated Skin Temperature Cool, temperature gradient down the leg Warm, no temperature gradient Dermatitis Rarely occurs Frequent occurs Pruritus Rarely occurs Frequent occurs 78) Parkinson's-diet • Foods that are easily chewed • Adequate fiber and fruit to avoid constipation • Eat six small meals and allow time to adequately chew and swallow • Limit protein in the evening because vitamin B6 interferes with levodopa medication 79) Musculoskeletal Drugs/Indications/ actions/Outcomes - Gout-allopurinol • Gout – type of arthritis characterized by an increase in uric acid and the deposit od uric acid crystals in one or more joints. • Allopurinol – antigout agent o Indication – Prevention of attack of gouty arthritis and nephropathy. o Action – Lowers serum uric acid levels o Outcome – with maintenance doses future attacks are prevented 80) Pulmonary abscess-positioning • Supine with the HOB at 30* • If patient is vomiting place on their side. 81) BPH-nocturia difficulties • An enlarged prostate can close off the urethra making the bladder contract harder to push urine. • The bladder is unable to completely empty causing frequent trips to the bathroom especially at night. • Frequent waking up can lead to sleep deprivation, increase stress levels, and changes in mood. Prolonged sleep deprivation can lead to weight gain, increase in BP and other heart problems. 82) Antiinfectives/Outcomes - COPD & infection • Recurring respiratory infections during childhood are a risk factor for developing COPD. • People with COPD are at higher risk for catching colds, the flu and pneumonia. • In most cases antibiotics are prescribed to keep on hand for exacerbations caused by bacterial or viral infections. 83) Nursing Process/Documentation - TIA-resolution • TIA (transient ischemic attack): episode of neurologic dysfunction (without acute infarction of the brain) caused by ischemia of by either the focal brain, spinal cord or retinal. It is to be treated as a medical emergency as it can develop into an ischemic stroke. Teach patient to seek treatment for any stroke symptoms. S/S depend on which blood vessel is involved and which part of the brain is affected. • Nursing process o Health information Past health history; family history; medications (includes oral contraceptives, illegal substances, drug use, over the counter, etc.) Social history; nutritional-metabolic; elimination; cognitive perceptual. o Preventing a thrombus/embolus from forming Control of HTN and/or diabetes mellitus; no smoking; limiting alcohol. DRUG THERAPY: Prevention in the development of a thrombus/embolus: aspirin; if PT has a-fib, oral anticoagulation can include warfarin (Coumadin); statins can be effective in prevention of stroke for a PT with a hx of TIA. SURGICAL THERAPY: Carotid endarterectomy, blood flow in the carotid artery is improved by clearing the lesion; transluminal angioplasty, a catheter is inserted in the femoral artery and lead to the carotid where a stenosed artery is opened improving blood flow; stenting, can be done during angioplasty and is the less invasive procedure for revascularization, artery is held open by stents or the system improving patency. Post-operative care: management of BP; neurovascular checks; keeping PT’s leg straight for prescribed time; monitoring for stent occlusion, hemorrhage (retroperitoneal and as a complication of the insertion site). 84) Transfusion reaction-process pg 35 red hesi book • Acute hemolytic: stop transfusion; change tubing, then continue saline IV; tx for shock (if present); draw blood samples for testing: monitor urine output hourly; give diuretics as prescribed. • Febrile nonhemolytic: give antipyretics as prescribed • Mild allergic: give antihistamine as directed • Anaphylactic and severe allergic: stop transfusion; CPR • Circulatory overload: place PT in upright position with feet in dependent position; administer diuretics, O2, morphine; slow IV rate • Sepsis: ensure patent airway; obtain blood for culture; administer antibiotics; take vital signs q5 minute until stable. 85) Addison's disease-role of glucose (maybe with steroid therapy)? Pg 1179 med surg book • Glucocorticoids are administered at a schedule that reflects the normal circadian rhythm of the endogenous hormone secretion and aids in decreasing the side effects of the corticosteroid therapy. Review Topics Part 3 86) Acoustic neuroma-action • A unilateral benign tumor which originates in the area where the vestibulocochlear nerve enters the internal auditory canal (middle ear) with the offset of symptoms between the ages of 40 and 60. The trigeminal and facial nerves and arteries could be compressed and destroyed in the internal ear. For small tumors, surgery can preserve hearing and vestibular function; the surgery for tumors larger than 3 cm can lead to permanent hearing loss and facial paralysis. Tumor growth may be slowed preserving the facial nerve by stereotactic radiosurgery. • Symptoms of compressed facial/trigeminal nerves: unilateral/progressive sensorineural hearing loss; reduced touch sensation in the posterior ear canal; unilateral tinnitus; mild/intermittent vertigo. • Diagnostic tests: neurologic, audiometric, vestibular tests; CT scans; MRI • Patient teaching: report any clear, colorless, discharge from nose (may be cerebrospinal fluid and increases the risk of infection); teach importance of follow- up care post surgery to monitor hearing and for tumor reoccurrence. 87) Liver-compensating metabolic acidosis • Kidneys excrete additional acid and in return the lungs increase CP2 excretion. Kussmaul respirations are then noticed. 88) Feedings for low albumin • Hypoalbuminemia is the sign of protein-calorie malnutrition and chronic liver disease. It is viewed as the critical predictor to nutritional support and tolerance to enteral feeding in critically ill patients . It is essential for maintenance of plasma colloidal osmotic pressure, prevention of edema, and transport of certain drugs and nutrients. • Common symptoms are: o edema in legs or face, roughness and dryness of skin, jaundice, difficulty breathing, lethargy, irregular heartbeat, abnormal weight gain, less of an appetite, diarrhea, N/V. • Treatment is normalizing the albumin level are: o Change diet style by increasing the amount of protein in your diet which can include, nuts, eggs, and dairy products. o The person should stop drinking alcohol. o In critically ill patients, feeding through the gI is preferred. However getting it eternal still does not give these kinds of patients enough nutrition to restore albumin levels. o The best choice methods to restore albumin levels are through IV infusion and diet changes that include increasing protein levels. 89) Heart failure-blood admin technique • Blood transfusions for heart failure patients follow the normal administration of blood with some changes. To prevent the patient from going into fluid overload, doctors often order lasix before or in between units of blood or right after blood is given. o Check doctors orders ( How many units to give, rate, premedicatons, etc. o Inform patient of order and get consent. o Have lab cross and match patient if not already done so, when completed, and make sure patient has a working IV site o Check labs o Identify patient and allergies o Administer pre transfusion medications if ordered (Tylenol, Benadryl, Lasix) o Verify with another nurse blood product (Type and patient) o Start blood transfusion o If more than 1 unit repeat each action starting with giving medications in between and having another nurse verify blood and patient. 90) Dopamine-urine output • Dopamine is used for the correction of imbalances present in shock syndrome due to MIs, trauma, septicemia, open heart surgery, renal failure and CHF. To know if it is working, urine flow, heart function, and blood pressure are monitored. • Dopamine increases urine output by acting both centrally and peripherally. Periphery it causes increased renal blood flow, sodium exertion, and then urine volume. It induces smooth muscle relation causing vasodilation. It also causes efferent vasoconstriction by way f the endocrine effect increasing the glomerular filtration rate and diuresis. Naturesis, excretion of sodium in the urine. occurs through the hemodynamoc and direct tubular actions causing increased urine output. I just remember water follows salt in this case. 91) Gastroplasty POC • Gastroplasty is a surgical procedure performed on the stomach to decrease its size or repair a defect. It is most commonly performed with a bypass to reduce weight. It is also known as a stomach band. Complications of getting gastroplasty are narrowing of the communication lumen of the 2 parts of the stomach, dehiscence of the vertical staple line, cholelithiasis, gastric perforation, post operative fistulas, hepatic failure, gastritis, and intestinal obstruction 92) Myxedema coma-assess • Myxedema coma is defined as a severe hypothyroidism leading to decreased mental status, hypothermia, and other symptoms related to slowing of the function in multiple organs. It is a medical emergency with a high mortality rate. Myxedema coma is a loss of brain function as a result of severe, long standing low levels of thyroid hormone in the blood. • Signs: o swelling of the face (lips, eyelids, and tongue) o swelling and thickening of the skin anywhere on the body (lower legs especially). o respiratory depression o low sodium levels o Hypothermia o confusion or mental slowness o Shock o low O2 levels o high CO2 levels o coma o Seizures • Causes: o autoimmune conditions o surgical removal of the thyroid o radiation therapy o medication induced (Lithium or Amiodarone) o iodine deficiency or excess of iodine o pregnancy o immune system medications like those used in cancer treatments • Treatment: includes thyroid hormone replacement such as Synthroid (levothyroxine) and steroid treatments. 93) Pathophysiology pulmonary edema • An acute, life-threatening situation, in which the alveoli of the lungs is filled with serosanguineous (yellowish with small amounts of blood) fluid. • Clinical manifestations are distinct. The patient will present with dyspnea and orthopnea. JVD is often present and the most sensitive and specific sign for LV filling pressures. Respiration rate is usually greater than 30 breaths per minute, with the use of accessory muscles. • The most common cause is left-sided heart failure. • Other causative factors include: overhydration of IV fluids, inhaled toxins, pneumonia, severe hypoxia, oxygen toxicity, ARDS 94) Postop hip repair-hospital acquired infection POC • A hospital acquired infection occurs when a patient experiences an infection (most often pneumonia) 24-48 hours after being in the hospital and the infection was not present prior to their admission. • Encourage patient to cough and deep breath for pneumonia prevention. • Notify surgeon immediately if severe pain, deformity, or loss of function occurs. • Discuss personal risk factors for infection with surgeon. 95) Teaching for herpes zoster • Potentially contagious to anyone who has not had varicella or is immunocompromised • Incidence increases with age • Resembles chickenpox; linear distribution along dermatome of grouped vesicles and pustules on erythematous—usually outbreak occurs on trunk, face, and lumbosacral areas • Burning pain and neuralgia preceding outbreak—mild to severe pain during outbreak • Treatment includes: (Topical) wet compress, silver sulfadiazine//Silvadene to ruptured vesicles. (Systemic) Antiviral agents—acyclovir, famciclovir, valacyclovir. Analgesia for mild sedation at bedtime. Gabapentin—postherpetic neuralgia. • Vaccination available for shingle prevention in adults 50 years old or younger—Zostavax. 96) Patho of cluster headaches • The cause nor the pathophysiology of cluster headaches is fully known. • The pain is presumed to occur because of neuron activation in the ophthalmic branch of the trigeminal nerve. Irregularities in melatonin and cortisol involving to the hypothalamus can also indicate a dysfunction of circadian rhythm, linking this to cluster headaches. • Cluster headaches can last anywhere from 15 to 180 minutes and can occur 8 times in one day. 97) Purpose of preop drops for cataract surgery • The main purpose of the eye drops is to promote healing from the inflammation that is caused by the surgery and to fight infection. • There are two types of dilating eye drops the patient can receive. o Mydriatic: an alpha-adrenergic agonist that produces pupillary dilation by contraction of the iris dilator muscle. o Cycloplegic: an anticholinergic agent that produces paralysis of accommodation by blocking the effect of acetylcholine on the ciliary body muscles. Cycloplegics can also produce pupillary dilation by blocking the effect of acetylcholine on the iris sphincter muscle. 98) Diabetes type 2-candida • During nursing assessment candidiasis will be found in the oral cavity appearing as raised white patches on mucous membrane. Diabetic patients with this should seek immediate medical attention for the infection. You should encourage PT to brush daily and inform dentist of diabetic condition. Pg 1124 medsurge and 137 hesi book 99) IV pyelogram-dye reaction • A contrast media injected to view size of kidneys, ureters, bladder, and can locate cyst and tumors that can cause obstructions. Before giving dye check for iodine allergy to avoid anaphylactic shock pg 1027 medsurge 100) Diabetes-illness effect • Integumentary- skin infections, slow wound healing • Oral- periodontal disease, candidiasis • Eyes- cataracts, retinopathy • Cardio pulmonary- angina, dyspnea, Hypertension • Periphery- poor perfusion, hair loss, weakness, absent pulse, pallor, thick nails • Renal failure symptoms- edema face hands feet, nausea, UTI symptoms, fatigue • Neuromuscular- numbness, tingling, pain, burning • Pg 137 hesi 101) DVT discharge plan • Notify hcp of manifestations of bleeding • Restrictions on daily activities • Do not blow nose forcefully • Do not bend down with head below waist • Use only electric razors • Use soft tooth brushes • Keep track of how many pads used during menstruation • Contact hcp before having procedures • Pg 626 medsurge 102) Endometriosis teaching • Teach what each medication is used for and their side effects • Psychological support resources for severe pain, sexual difficulties secondary to dyspareunia, and infertility. • Pg med surge 1254 HESI Content to Cover on Renal & Reproductive 103) Renal dosing/issues with nephrotoxic drugs Red Box Table 44-3 • Renal damage can alter clearance of active drug metabolites, potentially causing accumulation. Altered renal function can also affect dosing intervals of renally- eliminated medications. o Allopurinol (Zyloprim) o Lithium (Lithobid) o Acyclovir (Valtrex) o Amantadine (Symmetrel) o Fexofenadine (Allegra) o Gabapentin (Neurontin) o Metoclopramide (Reglan) o Ranitidine (Zantac) o Rivaroxaban (Xarelto) o Fesoterodine (Toviaz) • Decrease the dose fir renal impairment and frequency decrease. This based on stage of impairment. Decrease albumin means decrease protein binding. NORM 3.5-5 • AVOID NSAIDS, aluminum or mag (laxatives or antacids • Decrease elimination= accumulation of drugs • MOST CONCERN: Digoxin, ABX, metformin, and opiods. 104) Hyperparathyroidsim and renal calculi ? Table 49-12 Renal system?(Pp. 1172) • Hyperparathyroidism is a condition involving an increased secretion of parathyroid hormone. PTH helps regulate serum calcium and phosphate levels by stimulating bone resorption of calcium, renal tubular reabsorption of calcium, and activation of vitamin D. In the kidneys the excess calcium levels cannot be reabsorbed, leading to increased urinary calcium. This urinary calcium, along with a large amount of urinary phosphate, can lead to calculi formation. • S&S HTN, angina, dysthymia, lethargy, anorexia, N/V 105) Post-op management post-nephrectomy care (pp. 1063). • Pt consume clear liquid immediately after surgery and then progress as tolerated. • Pt pain will be controlled with pain med like Tylenol 3. • Dressing will be covered with a bandage. You may see Dermabond. • Some pts will have a drain or two. Many are secured with a stich and need to come into office for removal. • Pt may even be sent home with a Foley in place. • No submerging into water if drains or catheter is in place. • Frequent ambulation • Pt will need an ultrasound after the procedure. This can be done four weeks after stent is put in. • UOP q 2 hours, check resp status and WATCH DIAGPHRAGM, check for paralytic ileus, wait for return of bowel sounds? • #1 respiratory status= pain mgmt., incentive spirometer Q2hr, early and frequent ambulation • #2 Abdominal distention= common cause: paralytic Ileus 24-48 or bowels sounds return, IV fluids until NPO done 106) Prostatectomy with leaking around the catheter? (Pp. 1278) • Urine leakage following laparoscopic radical prostatectomy (LRP) is a possible complication that may herald chronic urine incontinence. Intraoperative measures aiming to prevent this is not standardized. • Catheters remain 6-9 post op. • Leaking is caused by involuntary muscle contractions. • If pink or red tinged urine = increase fluids 107) TURP discharge planning • Return to normal activities 3-6 weeks after procedure. • Pt needs educated on: pt may experience problems urine control or leakage after sneezing or coughing. • Erection problems • Absence of semen or decrease in volume. • Burning or pain during urination. • Passing blood clots • Patient should rest often. • Returning to normal routine should be gradual. • Caterer 2-7 days teach care. • Teach Kegel exercises 10-20x hr. • Teach S&S of UTI • If constipation occurs increase bulk fiber and fluids 108) Renal calculi patient teaching • Change diet add more fruits and veggies. • Drink lots of water. • Eat foods with low oxalate levels • Eat less meat • Decrease calcium no milk, cheese or dairy. • No vitamin D 109) Pyelonephritis and priority nursing interventions? • This is a bacterial infection causing inflammation of the kidneys and is one of the most common diseases of the kidney. • Have patient finish all medications. Drink lots of cranberry juice or water. Wear cotton panties, emove wet clothes promptly, females need to wipe front to back. • S&S = chills, fever, malaise, flank pain, dysuria, frequency • Flank pain , dysuria, and frequency is usually bc E.coli. • Risk= UTI, pregnancy, tumor, obstruction. Coli • DX= UA • NC: Bedrest, ABX, antiseptics, pain, increase fluids 3000ml • Monitor temp, increase fluids, decrease protein, I & O, 110) Hemodialysis and blood pressure • Patients on hemodialysis are usually hypertensive. If the hypertension is persistent it may reflect imperfect volume control despite initiation of dialysis • Monitor for S&S of hypotension • Trendelenburg position • NS bolus 250 • No BP meds before dialysis • SBP 110-120 is ok • TX: stop or decrease dialysis, NS bolus • LAST-A1AA (Alpha 1 adrenergic)midodrine 111) Glomerulonephritis and diet recommendations • Diet should be less protein, [potassium, phosphorus, and salt. • Increase carbs • Increase protein = increase BUN • Restrict your salt intake to prevent to minimize fluid retention, swelling, and hypertension 112) Renal lithotripsy • Is a noninvasive procedure used to treat kidney stones that are too large to pass through the urinary tract? It uses ultrasonic energy or shock waves directly to the stone first located with fluoroscopy or ultrasound. The shock waves break a large stone into smaller stones that will pass through the urinary system. • Complications= hemorrhage, sepsis, abscess formation Recent HESI Test: 113) Patient with renal calculi, fever, flank pain, which is highest nursing priority • Alleviate pain • Maintain adequate renal functioning • Prevent complications • Provide information about disease process/prognosis and treatment needs. • FEVER is concern= increase water and take abx (pyelonephritis & sepsis) 114) CKD patient who missed dialysis 3 days ago, which diagnostics report immediately to the HCP? • Potassium levels, BUN and creatine • K+ • Hypovolemia • SOB • Edema • ABGS= bicarb • Protein • NA+ • Phos • GFR 115) Ileal conduit diversion surgery? What to report to the HCP? Focus on appearance of stoma color? Purplish or red and moist? Urine color and appearance? • This surgery includes taking a section of the small bowel to be used for the conduit. • 1st week = look dark or bruised, look swollen or blister like, have spongy or yellow tissue around it. • HEALTHY stoma= soft, moist, red or pink, shiny. • CALL DOCTOR: blood or hematuria • It should be free of rashes =, redness, scratches, bruising • No change in urine color, mucus threads normal post op. 116) Patient with hyperparathyroidism develops severe flank pain. Which action should RN take? Likely the question is pointing toward development of renal calculi from excess calcium? • Call doctor to get labs to check calcium levels. • Start fluids INCREASE • Access where pain is any what kind of pain. • Monitor fever= infection • Start phosphate binders, Ca+ and Vit D supplement 117) Renal colic pain priorities • NSAIDs over morphine • DOC = Toradol/ketorolac • Drugs to prevent muscle spasms • Opioids • Increase water, decrease Na+, decrease protein, decrease oxalate [Show More]
Last updated: 2 years ago
Preview 1 out of 38 pages
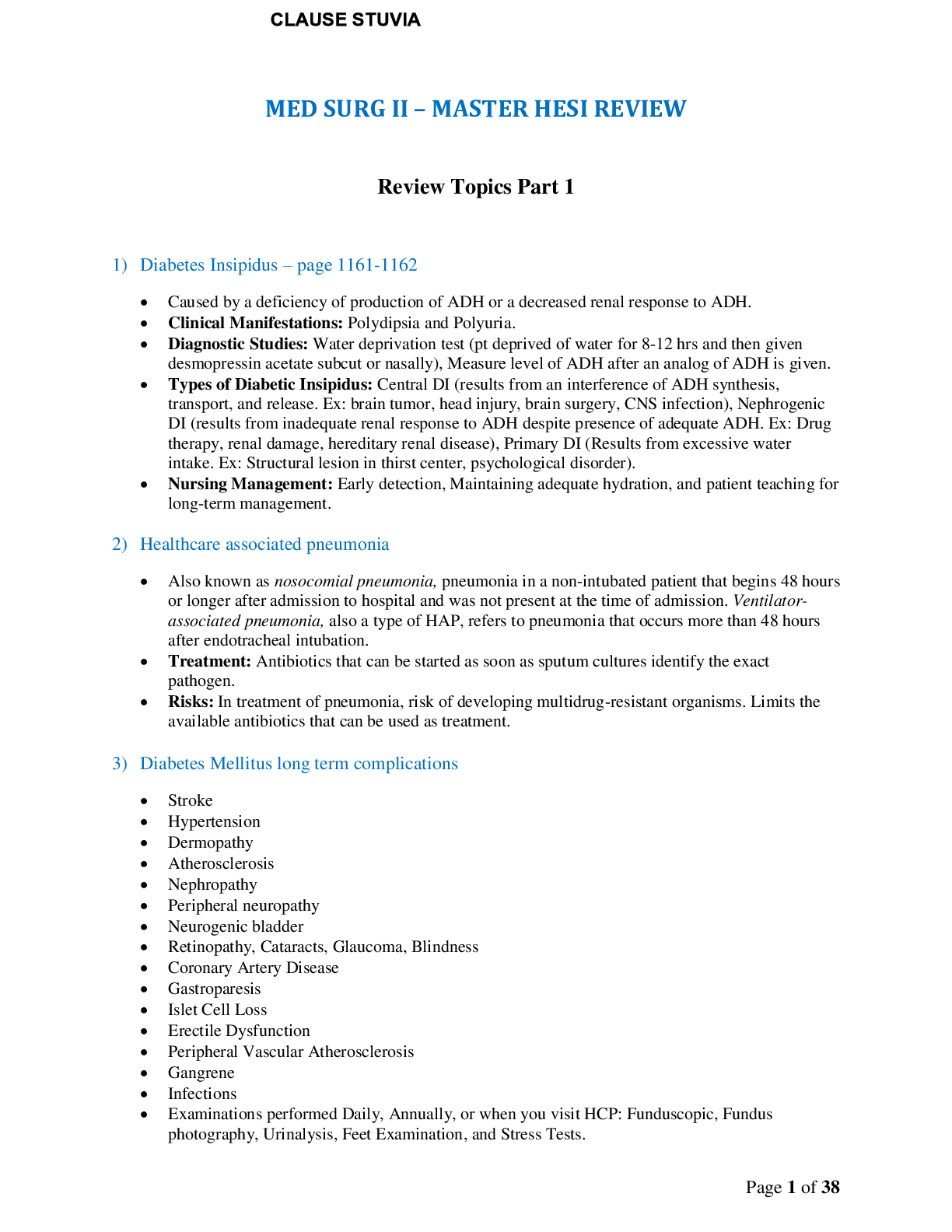
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 09, 2021
Number of pages
38
Written in
Additional information
This document has been written for:
Uploaded
May 09, 2021
Downloads
0
Views
95

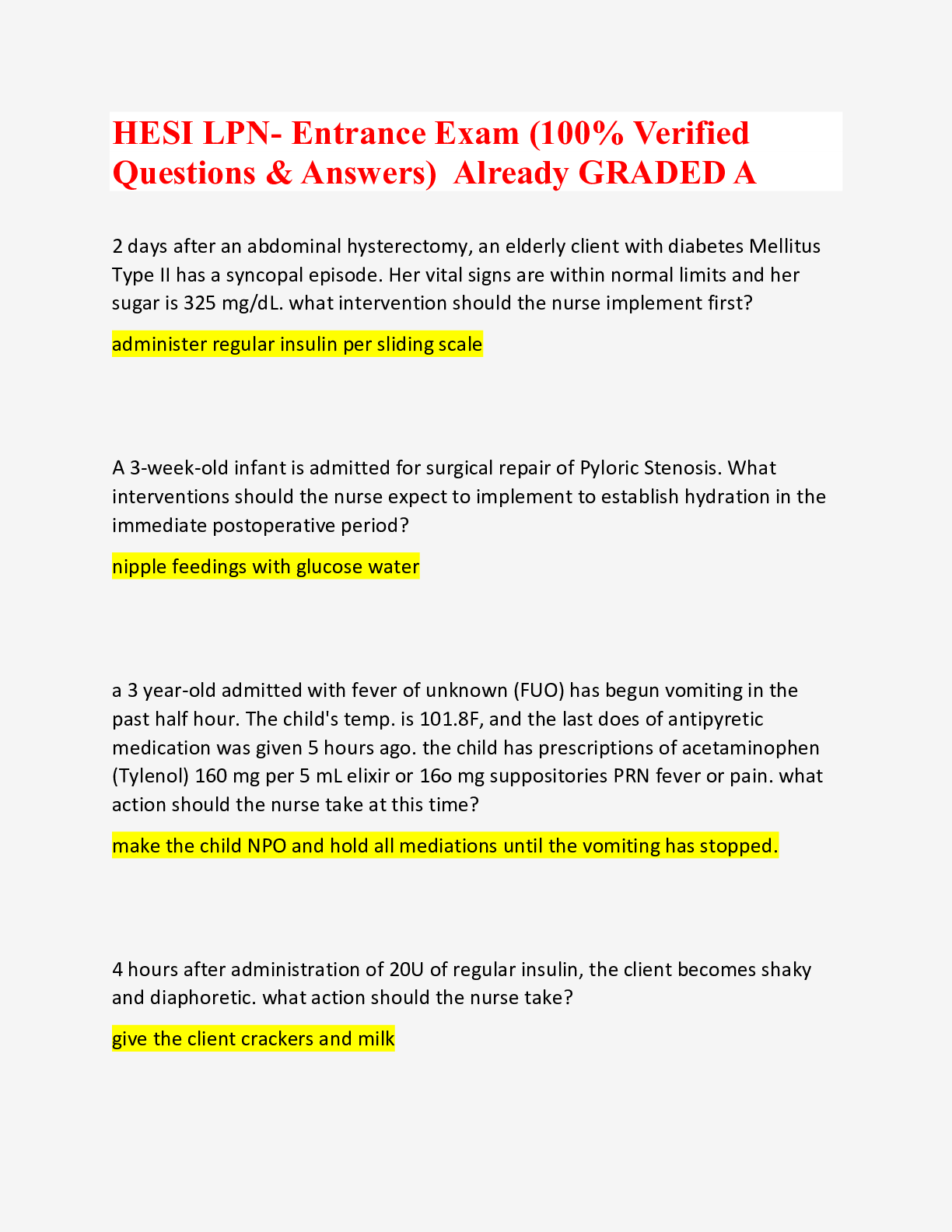

.png)



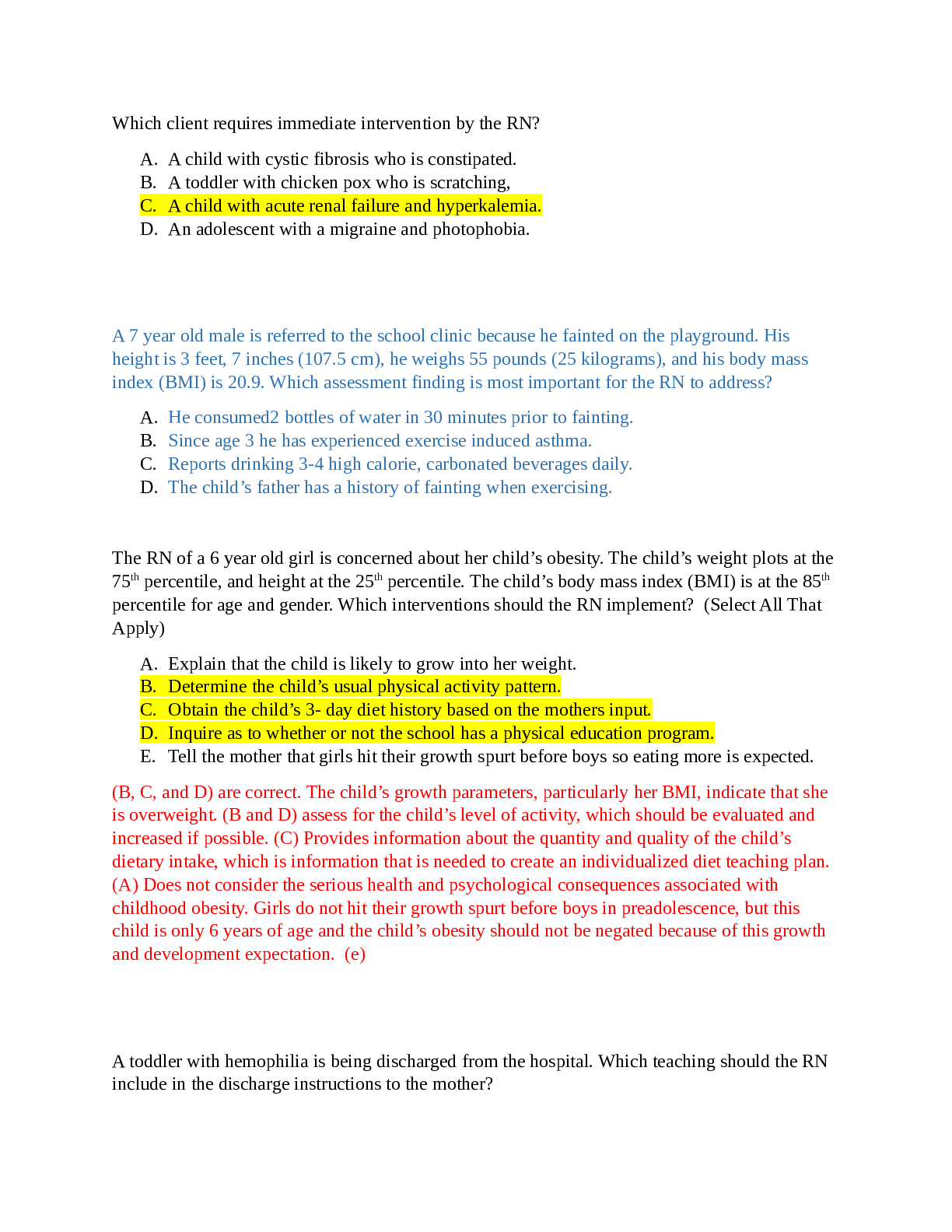
.png)