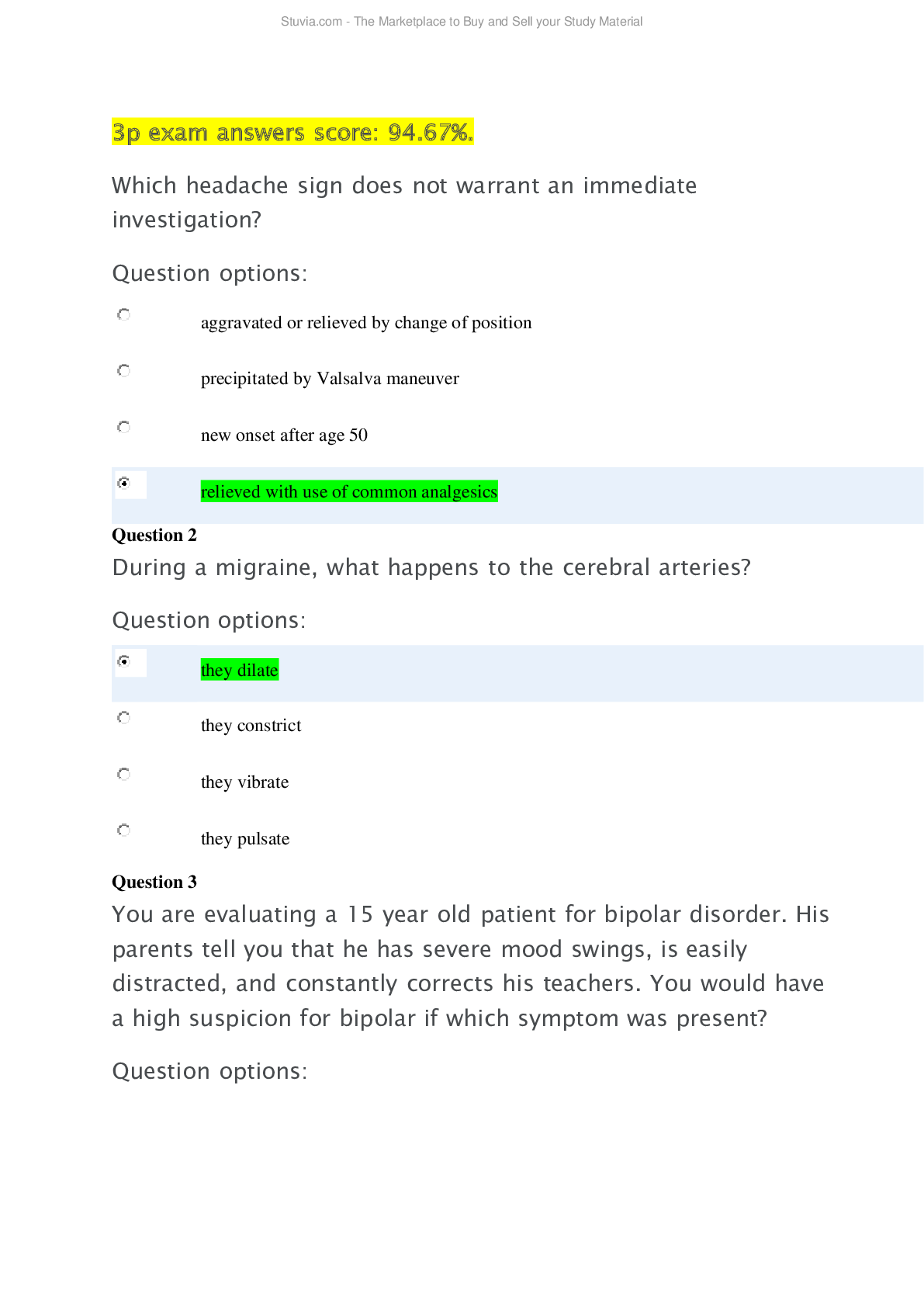
NRNP 6665 MIDTERM EXAM
$ 20
ATI RN NURSING CARE OF CHILDREN WELL CHILD
$ 15
Solutions Manual For Applied Multivariate Statistical Analysis 6th Edition By Richard A. Johnson, Dean W. Wichern
$ 30
Olympus Corporation Case Study
$ 7
.png)
CDL - Combination Vehicle Practice Test Latest 2022 Already Passed
$ 9.5
BICSI ITSMM Test Study Guide | 70 Questions | 100% Correct Answers
$ 6

C229 Task 1 Part B.docx C229 C229 Task 1 Part B Western Governers University B. Comm
$ 10
ATI RN NURSING CARE OF CHILDREN CYSTIC FIBROSIS INPATIENT CARE
$ 18
ESSENIAL CELL BIOLOGY 5TH EDITION CHAPTER 1-20 ALBERT HOPKINS TEST
$ 30

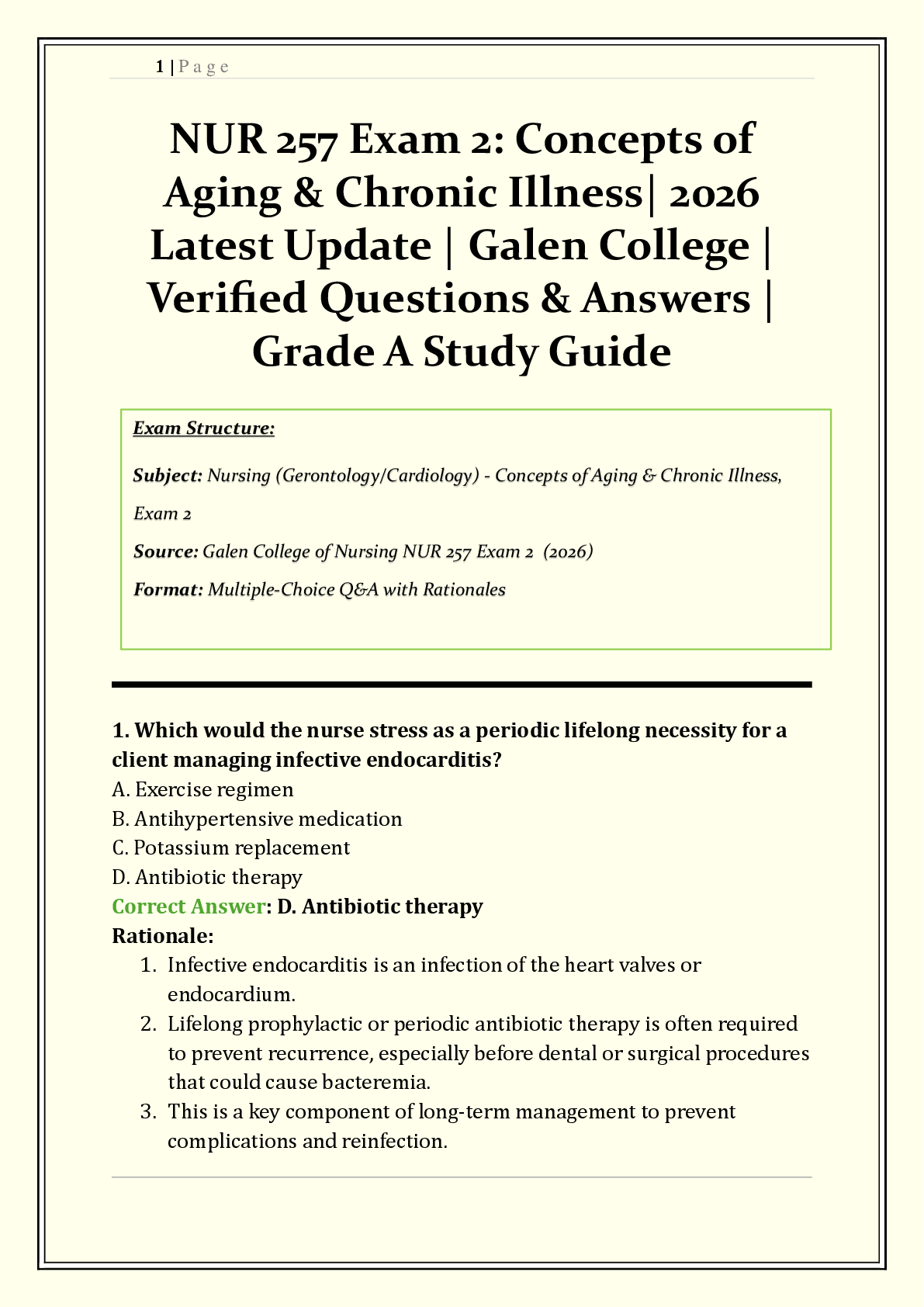
NRNP 6540 Week 10 Knowledge Check
$ 11.5
VADETS FINAL EXAM
$ 10
OCR 2024 GCSE Biology B Twenty First Century Science J257/01: Breadth in Biology (Foundation Tier) Question paper and Mark scheme Merged
$ 7
Unit 5: Comprehension Reading Strategies
$ 10
2023 AQA AS SPANISH 7691/3T/3V Paper 3 Speaking Mark scheme June 2023 [VERIFIED]
$ 7

West Coast EMT Block #3 Exam Study Guide
$ 9.5
COUN506 FINAL EXAM LATEST UPDATE 2023
$ 11
RNSG 2331 - Exam 2-Capstone-1.

_removed.png)



_removed.png)

_removed.png)
_removed.png)