*NURSING > QUESTIONS & ANSWERS > CHAMBERLAIN COLLEGE OF NURSING: COMPLEX CRITICAL NURSING 341 TEST 1. 100% correct (All)
CHAMBERLAIN COLLEGE OF NURSING: COMPLEX CRITICAL NURSING 341 TEST 1. 100% correct
Document Content and Description Below
Any treatment that is used to sustain life, including nutrition, fluids, antibiotics, blood products, and respiratory support, may be withdrawn in consultation with the patient and/or surrogate provid... ed that the patient has been deemed terminal or persistently vegetative. Any dose of anxiolytics or analgesics may be used to relieve suffering, although these may have the potential to hasten death. Life-sustaining treatment should not be withdrawn while the patient is receiving paralytic treatments. Death occurs as a consequence of the underlying disease, and the goal of care is to relieve suffering, not hasten death. 16. The patient’s husband is terrified by the prospect of removing life-sustaining treatments from the patient. He asks why anyone would do that. The nurse explains, a. “It is to save you money so you won’t have such a large financial burden.” b. “It will preserve limited resources for the hospital so other patients may benefit from them.” c. “It is to discontinue treatments that are not helping your wife and may be very uncomfortable for her.” d. “We have done all we can for your wife and any more treatment would be futile.” The goal of withdrawal of life-sustaining treatments is to remove treatments that are not beneficial and may be uncomfortable. DIF: Cognitive Level: Application REF: p. 40, 42 OBJ: Discuss concepts of end-of-life care, including palliative care; communication and conflict resolution; withholding or withdrawing therapy; and psychological support of the patient, family members, and healthcare providers. TOP: Nursing Process Step: Implementation 17. All of the patient’s children are distressed by the possibility of removing life-support treatments from their mother. The child who is most upset tells the nurse, “This is the same as killing her! I thought you were supposed to help her!” The nurse explains to the family, a. “This is a process of allowing your mother to die naturally after the injuries that she sustained in a serious accident.” b. “The hospital would never allow us to do that kind of thing.” c. “Let’s talk about this calmly, and I will explain why assisted suicide is appropriate in this case.” d. “She’s lived a long and productive life.” Forgoing life-sustaining treatments is not the same as active euthanasia or assisted suicide. Killing is an action causing another’s death, whereas allowing dying is avoiding any intervention that interferes with a natural death following illness or trauma. DIF: Cognitive Level: Application REF: p. 40 OBJ: Discuss concepts of end-of-life care, including palliative care; communication and conflict resolution; withholding or withdrawing therapy; and psychological support of the patient, family members, and healthcare providers. TOP: Nursing Process Step: Implementation MSC: NCLEX: Safe and Effective Care Environment 18. To prevent any unwanted resuscitation after life-sustaining treatments have been withdrawn, the nurse should ensure that: a. do-not-resuscitate (DNR) orders are written before discontinuation of the treatments. b. the family is not allowed to visit until the death occurs. c. DNR orders are written as soon as possible after the discontinuation of the treatments. d. the change-of-shift report includes the information that the patient is not to be resuscitated. DNR orders should be written before withdrawal of life support; this will prevent any unfortunate errors in unwanted resuscitation during the time period between initiation of withdrawal and the actual death. DIF: Cognitive Level: Application REF: p. 33 OBJ: Describe ethical and legal concerns related to end-of-life care. TOP: Nursing Process Step: Implementation MSC: NCLEX: Safe and Effective Care Environment 19. The patient’s husband is very upset because his wife, who is near death, has dyspnea and restlessness. The nurse explains to him that there are some ways to decrease her discomfort, including: a. respiratory therapy treatments. b. opioid medications given as needed. c. incentive spirometry. d. increased hydration. Dyspnea is best managed with close evaluation of the patient and the use of opioids, sedatives, and nonpharmacologic interventions (oxygen, positioning, and increased ambient air flow). DIF: Cognitive Level: Application REF: Figure 4-1 OBJ: Describe nursing interventions to support the patient and family during the end-of-life stage. TOP: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity 20. The patient’s husband, experiencing anticipatory grieving, tells the nurse that he doesn’t see any point in continuing to visit at the bedside, because the patient is unresponsive. The best response for the nurse supports him by saying, a. “You’re right, she is not aware of anything going on around her now.” b. “Although she is not responding, she may be able to hear you and benefit from your presence.” c. “I’ll call you if she starts responding again.” d. “Why don’t you check to see if any other family member would like to visit her?” The patient may still be able to hear despite appearing to be nonresponsive. DIF: Cognitive Level: Application REF: p. 42 OBJ: Describe nursing interventions to support the patient and family during the end-of-life stage. TOP: Nursing Process Step: Planning MSC: NCLEX: Psychosocial Integrity 21. Which of the following statements about comfort care is accurate? a. Withholding and withdrawing life-sustaining treatment are distinctly different in the eyes of the legal community. b. Each procedure should be evaluated for its effect on the patient’s comfort before being implemented. c. Only the patient can determine what constitutes comfort care for him or her. d. Withdrawing life-sustaining treatments is considered euthanasia in most states. The goal of comfort care is to provide treatments that do not cause pain or other discomfort to the patient. DIF: Cognitive Level: Comprehension REF: p. 38 OBJ: Discuss concepts of end-of-life care, including palliative care; communication and conflict resolution; withholding or withdrawing therapy; and psychological support of the patient, family members, and healthcare providers. TOP: Nursing Process Step: N/A MSC: NCLEX: Psychosocial Integrity MULTIPLE RESPONSE 1. Select interventions that may be included during “terminal weaning” include which of the following? (Select all that apply.) a. Complete extubation following ventilator withdrawal b. Discontinuation of artificial ventilation but maintenance of the artificial airway c. Discontinuation of anxiolytic and pain medications d. Titration of ventilator support based upon blood gas determinations e. Titration of ventilator support to minimal levels based upon patient assessment of comfort , B, E “Terminal weaning” may include titration of ventilator support to minimal levels, removal of the ventilator with maintenance of the artificial airway, and complete extubation. Pain and anxiolytic medications may be required to control dyspnea and anxiety that may accompany ventilator withdrawal. Blood gas determinations would be used in therapeutic ventilator management. DIF: Cognitive Level: Analysis REF: p. 40 | Fig. 4-1 | Clinical Alert OBJ: Describe nursing interventions to support the patient and family during the end-of-life stage. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 2. Which therapeutic interventions may be withdrawn or withheld from the terminally ill client? (Select all that apply.) a. Antibiotics b. Dialysis c. Nutrition d. Pain medications e. Simple nursing interventions such as repositioning and hygiene , B, C Any treatment that is life sustaining may be withheld from a terminally ill patient during the end of life. These treatments include nutrition, dialysis, fluids, antibiotics, respiratory support, therapeutic medications, and blood products. Any dose of analgesic or anxiolytic medication may be used to prevent suffering and should not be withdrawn. Dignity should be maintained during the course of dying. This would include ongoing provision of basic nursing care and comfort. DIF: Cognitive Level: Analysis REF: p. 40 | Box 4-3 OBJ: Describe ethical and legal concerns related to end-of-life care. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 3. Which interventions can the nurse use to facilitate communication with patients and families who are in the process of making decisions regarding end-of- life care options? (Select all that apply.) a. Communication of uniform messages from all healthcare team members b. An integrated plan of care that is developed collaboratively by the patient, family, and healthcare team c. Facilitation of continuity of care through accurate shift-to-shift and transfer reports d. Limitation of time for families to express feelings in order to control family grief e. Reassuring the patient and family that they will not be abandoned as the goals of care shift from aggressive treatment to comfort care , B, C, E Effective and consistent communication between the patient, family, and healthcare team members is required to promote positive outcomes during end-of-life care. Family members should be provided ample time to express feelings in order to improve the level of satisfaction and prevent dysfunctional bereavement patterns. DIF: Cognitive Level: Analysis REF: Box 4-2 OBJ: Describe nursing interventions to support the patient and family during the end-of-life stage. TOP: Nursing Process Step: Implementation MSC: NCLEX: Psychosocial Integrity 4. Palliation may include: (Select all that apply.) a. relieving pain. b. relieving nausea. c. psychological support. d. withdrawing life-support interventions. e. withholding tube feedings. , B, C Palliation includes relieving symptoms that may have a negative effect on the family or the patient. DIF: Cognitive Level: Analysis REF: p. 38 OBJ: Discuss concepts of end-of-life care, including palliative care; communication and conflict resolution; withholding or withdrawing therapy; and psychological support of the patient, family members, and healthcare providers. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 5. When providing palliative care, the nurse must keep in mind that the family may include which of the following? (Select all that apply.) a. Unmarried life partners of same sex b. Unmarried life partners of opposite sex c. Roommates d. Close friends e. Parents , B, D, E The definition of family varies and may include unmarried life partners of the same or opposite sex, close friends, and other close individuals who have no legal relationship with the patient. Ch 5 1. Nociceptors differ from other nerve receptors in the body in that they: a. adapt very little to continual pain response. b. inhibit the infiltration of neutrophils and eosinophils. c. play no role in the inflammatory response. d. transmit only the thermal stimuli. Nociceptors are stimulated by mechanical, chemical, or thermal stimuli. Nociceptors differ from other nerve receptors in the body in that they adapt very little to the pain response. The body continues to experience pain until the stimulus is discontinued or therapy is initiated. This is a protective mechanism so the body tissues being damaged will be removed from harm. Nociceptors usually initiate inflammatory responses near injured capillaries. As such, the response promotes infiltration of injured tissues with neutrophils and eosinophils. DIF:Cognitive Level: ComprehensionREF:p. 51 OBJ Discuss the physiology of pain and anxiety. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 2. A 45-year-old male postsurgical patient is on a ventilator in the critical care unit. He has been tolerating the ventilator well and has not required any sedation. He becomes tachycardic and hypertensive. His respiratory rate has increased to 28 breaths/min. The ventilator is set on synchronized intermittent mandatory ventilation (SIMV) at a rate of 10 breaths/min. The patient has been suctioned recently via his endotracheal tube, and his airway is clear. He responds appropriately to the nurse’s commands. The nurse should: a. assess the patient’s level of pain. b. decrease the SIMV rate on the ventilator. c. provide sedation as ordered. d. suction the patient again. Pulse, respirations, and blood pressure frequently result from activation of the sympathetic nervous system by the pain stimulus. Because the patient is postoperative, the patient should be assessed for the presence of pain and need for pain medication. Decreasing the SIMV does nothing because the patient is already overriding the ventilator. Providing sedation may calm the patient but will not solve the problem if the physiological changes are from pain. The patient has just been suctioned and his lungs are clear. There is no need to suction again. DIF:Cognitive Level: AnalysisREF:pp. 52-53 OBJ: Describe the positive and negative effects of pain and anxiety in critically ill patients. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 3. The assessment of pain and anxiety is a continuous process. When critically ill patients exhibit signs of anxiety, the nurse’s first priority is to: a. administer antianxiety medications as ordered. b. administer pain medication as ordered. c. identify and treat the underlying cause. d. reassess the patient hourly to determine whether symptoms resolve on their own. When patients exhibit signs of anxiety or agitation, the first priority is to identify and treat the underlying cause, which could be hypoxemia, hypoglycemia, hypotension, pain, or withdrawal from alcohol and drugs. Treatment is not initiated until assessment is completed. Medication may not be needed if the underlying cause can be resolved. DIF:Cognitive Level: ComprehensionREF:p. 53 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 4. Both the electroencephalogram (EEG) monitor and the Bispectral Index Score (BIS) or Patient State Index (PSI) analyzer monitors are used to assess patient sedation levels in critically ill patients. The BIS and PSI monitors are simpler to use because they: a. can only be used on heavily sedated patients. b. can only be used on pediatric patients. c. provide raw EEG data and a numeric value. d. require only five leads. The BIS and PSI have very simple steps for application, and results are displayed as raw EEG data and the numeric value. A single electrode is placed across the patient’s forehead and is attached to a monitor. These monitors can be used in both children and adults, and patients with varying levels of sedation. DIF:Cognitive Level: ComprehensionREF:pp. 57-58 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 5. The nurse is caring for a patient who requires administration of a neuromuscular blocking agent to facilitate ventilation with non-traditional modes. The nurse understands that neuromuscular blocking agents provide: a. antianxiety effects. b. complete analgesia. c. high levels of sedation. d. no sedation or analgesia. Neuromuscular blocking (NMB) agents do not possess any sedative or analgesic properties. Patients who receive NMBs must also receive a sedative agent. DIF:Cognitive Level: ApplicationREF:p. 60 OBJ: Discuss assessment and management challenges in subsets of critically ill patients. TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 6. The patient is receiving neuromuscular blockade. Which nursing assessment indicates a target level of paralysis? a. Glasgow Coma Scale score of 3 b. Train-of-four yields two twitches c. Bispectral index of 60 d. CAM-ICU positive A train-of-four response of two twitches using a peripheral nerve stimulator indicates adequate paralysis. The Glasgow Coma Scale does not assess paralysis; it is an indicator of consciousness. The Bispectral Index provides an assessment of sedation. The CAM-ICU is a tool to assess delirium. DIF:Cognitive Level: AnalysisREF:pp. 60-61 OBJ: Discuss assessment and management challenges in subsets of critically ill patients. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 7. The nurse is concerned that the patient will pull out the endotracheal tube. As part of the nursing management, the nurse obtains an order for: a. a Posey-type vest. b. a higher dosage of lorazepam. c. propofol. d. soft wrist restraints. Restraints are associated with an increased incidence of agitation and delirium. Therefore, the least restrictive methods of restraint are recommended, which is the soft wrist restraints. The Posey-type vest will not prevent self-extubation. The least amount of sedation is also recommended; therefore, neither increasing the dosage of lorazepam nor adding propofol is indicated and would likely prolong mechanical ventilation. DIF:Cognitive Level: AnalysisREF:p. 71, Table 5-11 OBJ:Identify nonpharmacological and pharmacological strategies to promote comfort and reduce anxiety.TOP:Nursing Process Step: Planning MSC:NCLEX: Physiological Integrity: Safety 8. Neuromuscular blocking agents are used in the management of some ventilated patients. Their primary mode of action is: a. analgesia. b. anticonvulsant. c. paralysis. d. sedation. These agents cause respiratory muscle paralysis. They do not provide analgesia or sedation. They do not have anticonvulsant properties. DIF:Cognitive Level: ComprehensionREF:p. 60 OBJ: Discuss assessment and management challenges in subsets of critically ill patients. TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 9. The most important nursing intervention for patients who receive neuromuscular blocking agents is to: a. administer sedatives in conjunction with the neuromuscular blocking agents. b. assess neurological status every 30 minutes. c. avoid interaction with the patient, because he or she won’t be able to hear. d. restrain the patient to avoid self-extubation. Neuromuscular blocking agents cause paralysis only; they do not cause sedation. Therefore, concomitant administration of sedatives is essential. Neurological status is monitored according to unit protocol. Nurses should communicate with all critically ill patients, regardless of their status. If the patient is paralyzed, restraining devices may not be needed. DIF:Cognitive Level: ApplicationREF:p. 60 OBJ: Discuss assessment and management challenges in subsets of critically ill patients. TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 10. The best way to monitor agitation and effectiveness of treating it in the critically ill patient is to use a/the: a. Confusion Assessment Method (CAM-ICU). b. FACES assessment tool. c. Glasgow Coma Scale. d. scale such as Richmond Agitation Sedation Scale. Various sedation scales are available to assist the nurse in monitoring the level of sedation and assessing response to treatment. The Richmond Agitation Sedation Scale is a commonly used tool that has been validated. The CAM-ICU assesses for delirium. The FACES scale assesses pain. The Glasgow Coma Scale assesses neurological status. DIF:Cognitive Level: ApplicationREF:p. 56 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 11. The nurse is caring for a patient receiving intravenous ibuprofen for pain management. The nurse recognizes which laboratory assessment to be a possible side effect of the ibuprofen? a. Elevated creatinine b. Elevated platelet count c. Elevated white blood count d. Low liver enzymes Ibuprofen can result in renal insufficiency, which may be noted in an elevated serum creatinine level. Thrombocytopenia (low platelet count) is another possible side effect. An elevated white blood count indicates infection. Although ibuprofen is cleared primarily by the kidneys, it is also important to assess liver function, which would show elevated liver enzymes, not low values. DIF:Cognitive Level: ComprehensionREF:Table 5-9 OBJ:Identify nonpharmacological and pharmacological strategies to promote comfort and reduce anxiety.TOP:Nursing Process Step: Evaluation MSC: NCLEX: Physiological Integrity 12. The nurse is assessing pain levels in a critically ill patient using the Behavioral Pain Scale. The nurse recognizes ________ as indicating the greatest level of pain. a. brow lowering b. eyelid closing c. grimacing d. relaxed facial expression The Behavioral Pain Scale issues the most points, indicating the greatest amount of pain, to assessment of facial grimacing. DIF:Cognitive Level: ComprehensionREF:Table 5-2 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 13. The nurse wishes to assess the quality of a patient’s pain. Which of the following questions is appropriate to obtain this assessment if the patient is able to give a verbal response? a. “Is the pain constant or intermittent?” b. “Is the pain sharp, dull, or crushing?” c. “What makes the pain better? Worse?” d. “When did the pain start?” If the patient can describe the pain, the nurse can assess quality, such as sharp, dull, or crushing. The other responses relate to continuous or intermittent presence (A), what provides relief (C), and duration (D). DIF:Cognitive Level: ComprehensionREF:p. 53 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 14. The nurse is assessing the patient’s pain using the Critical Care Pain Observation Tool. Which of the following assessments would indicate the greatest likelihood of pain and need for nursing intervention? a. Absence of vocal sounds b. Fighting the ventilator c. Moving legs in bed d. Relaxed muscles in upper extremities Fighting the ventilator is rated with the greatest number of points for compliance with the ventilator, and could indicate pain or anxiety. Absence of vocal sounds (e.g., no crying) and relaxed muscles do not indicate pain and are not given a point value. The patient may be moving the legs as a method of range of motion, not necessarily in response to pain. The patient needs to be assessed for restlessness if the movement is excessive. DIF:Cognitive Level: ApplicationREF:Table 5-3 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 15. The nurse is caring for four patients on the progressive care unit. Which patient is at greatest risk for developing delirium? a. 36-year-old recovering from a motor vehicle crash; being treated with an alcohol withdrawal protocol. b. 54-year-old postoperative aortic aneurysm resection with an elevated creatinine level c. 86-year-old from nursing home, postoperative from colon resection d. 95-year-old with community-acquired pneumonia; family has brought in eyeglasses and hearing aid From this list, the elderly, postoperative, nursing home resident is at greatest risk. The 96-year-old has been provided eyeglasses and a hearing aid, which will decrease the risk of delirium. Renal failure is a risk for delirium, but an elevated BUN does not always indicate renal failure. The 36-year-old is receiving medications as part of an alcohol withdrawal protocol, which should decrease the risk for delirium. DIF:Cognitive Level: AnalysisREF:Box 5-3 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 16. The nurse is caring for a patient with hyperactive delirium. The nurse focuses interventions toward keeping the patient: a. comfortable b. nourished c. safe d. sedated The greatest priority in managing delirium is keeping the patient safe. Sedation may contribute to development of delirium. Comfort and nutrition are important, but they are not priorities. DIF:Cognitive Level: ComprehensionREF:p. 58 OBJ: Identify nonpharmacological and pharmacological strategies to promote comfort, reduce anxiety, and prevent delirium. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 17. The nurse is caring for a critically ill trauma patient who is expected to be hospitalized for an extended period of time. Which of the following nursing interventions would improve the patient’s well-being and reduce anxiety the most? a. Arrange for the patient’s dog to be brought into the unit (per protocol). b. Contact the pet therapy department to bring a therapy dog in to visit. c. Secure the harpist to come and play soothing music for an hour every afternoon. d. Wheel the patient out near the unit aquarium to observe the tropical fish. Nonpharmacological approaches are helpful in reducing stress and anxiety, and each of these activities has the potential for improving the patient’s well-being. The patient is likely to benefit most from the presence of his or her own dog rather than the therapy dog. DIF:Cognitive Level: ApplicationREF:p. 66 OBJ: Identify nonpharmacological and pharmacological strategies to promote comfort, reduce anxiety, and prevent delirium. TOP: Nursing Process Step: Intervention MSC: NCLEX: Psychological Integrity 18. The nurse recognizes that which patient is likely to benefit most from patient-controlled analgesia? a. 21-year-old with a C4 fracture and quadriplegia b. 45-year-old with femur fracture and closed head injury c. 59-year-old postoperative elective bariatric surgery d. 70-year-old postoperative cardiac surgery; mild dementia The patient undergoing bariatric surgery (an elective procedure) is the best candidate for PCA. The quadriplegic would be unable to operate the PCA pump. The cardiac surgery patient with mild dementia may not understand how to operate the pump. Likewise, the patient with the closed head injury may not be cognitively intact. DIF:Cognitive Level: ApplicationREF:Box 5-6 OBJ: Identify nonpharmacological and pharmacological strategies to promote comfort, reduce anxiety, and prevent delirium. TOP: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity 19. The nurse is caring for a patient receiving benzodiazepine intermittently. The nurse understands that the best way to administer such drugs is to: a. administer around the clock, rather than as needed, to ensure constant sedation. b. administer the medications through the feeding tube to prevent complications. c. give the highest allowable dose for the greatest effect. d. titrate to a predefined endpoint using a standard sedation scale. The best approach for administering benzodiazepines (and all sedatives) is to administer and titrate to a desired endpoint using a standard sedation scale. Administering around the clock as well as giving the highest allowable dose without basing it on an assessment target may result in excessive sedation. For greatest effect, most benzodiazepines are given intravenously. DIF:Cognitive Level: ApplicationREF:p. 68 OBJ: Identify nonpharmacological and pharmacological strategies to promote comfort, reduce anxiety, and prevent delirium. TOP: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity 20. The nurse is concerned about the risk of alcohol withdrawal syndrome in a 45-year- old postoperative patient. Which statement indicates her understanding of management of this patient? a. “Alcohol withdrawal is common; we see it all of the time in the trauma unit.” b. “There is no way to assess for alcohol withdrawal.” c. “This patient will require less pain medication.” d. “We have initiated the alcohol withdrawal protocol.” The most important treatment of alcohol withdrawal syndrome is prevention. Many units have protocols that are initiated early to prevent the syndrome. Alcohol withdrawal syndrome is common; however, this statement does not indicate knowledge of management. The patient experiencing alcohol withdrawal may exhibit a variety of symptoms, such as disorientation, agitation, and tachycardia. Patients with substance abuse require increased dosages of pain medications. DIF:Cognitive Level: AnalysisREF:p. 71 OBJ: Identify nonpharmacological and pharmacological strategies to promote comfort, reduce anxiety, and prevent delirium. TOP: Nursing Process Step: Intervention MSC: NCLEX: Physiological Integrity MULTIPLE RESPONSE 1. Nonpharmacological approaches to pain and/or anxiety that may best meet the needs of critically ill patients include: (Select all that apply.) a. anaerobic exercise. b. art therapy. c. guided imagery. d. music therapy. , D Guided imagery is a powerful technique for controlling pain and anxiety, especially that associated with painful procedures. Similar to guided imagery, a music therapy program offers patients a diversionary technique for pain and anxiety relief. Anaerobic exercise is not a nonpharmacological approach for managing pain and anxiety. Most critically ill patients are not able to participate in art therapy. DIF:Cognitive Level: AnalysisREF:p. 66 OBJ:Identify nonpharmacological and pharmacological strategies to promote comfort and reduce anxiety.TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 2. Which of the following statements regarding pain and anxiety are true? (Select all that apply.) a. Anxiety is a state marked by apprehension, agitation, autonomic arousal, and/or fearful withdrawal. b. Critically ill patients often experience anxiety, but they rarely experience pain. c. Pain and anxiety are often interrelated and may be difficult to differentiate because their physiological and behavioral manifestations are similar. d. Pain is defined by each patient; it is whatever the person experiencing the pain says it is. , C, D Pain is defined by each patient, anxiety is associated with marked apprehension, and pain and anxiety are often interrelated. Critically ill patients commonly have both pain and anxiety. DIF: Cognitive Level: Comprehension REF: pp. 48-49 OBJ: Define pain and anxiety. TOP: Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity 3. Which of the following factors predispose the critically ill patient to pain and anxiety? (Select all that apply.) a. Inability to communicate b. Invasive procedures c. Monitoring devices d. Nursing care , B, C, D All of these factors predispose the patient to pain or anxiety. DIF:Cognitive Level: AnalysisREF:p. 49 OBJ: Identify factors that place the critically ill patient at risk for developing pain and anxiety. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 4. Choose the items that are common to both pain and anxiety. (Select all that apply.) a. Cyclical exacerbation of one another b. Require good nursing assessment for proper treatment c. Response only to real phenomena d. Subjective in nature , B, D Both pain and anxiety are subjective in nature. One can exacerbate the other in a vicious cycle that often requires good nursing assessment in order to manage the precipitating problem and break the cycle. Anxiety is a response to a real or perceived fear. Pain is a response to real or “phantom” phenomenon but always involves transmission of nerve impulses. Both relate to the patient’s perceptions of pain and fear. Anxiety is a response to real or perceived fear, and pain is a response to a real or “phantom” phenomenon. DIF:Cognitive Level: ComprehensionREF:p. 49 OBJ: Identify factors that place the critically ill patient at risk for developing pain and anxiety. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 5. Anxiety differs from pain in that: (Select all that apply.) a. it is confined to neurological processes in the brain. b. it is linked to reward and punishment centers in the limbic system. c. it is subjective. d. there is no actual tissue injury. , B, D Unlike pain, anxiety is linked to the reward and punishment centers in the limbic system of the brain. It is totally neurological and does not involve tissue injury. Like pain, it is a subjective phenomenon. Both anxiety and pain are subjective in nature. DIF:Cognitive Level: ComprehensionREF:p. 49, 51 OBJ iscuss the physiology of pain and anxiety. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 6. Factors in the critical care unit that may predispose the client to increased pain and anxiety include: (Select all that apply.) a. an endotracheal tube. b. frequent vital signs. c. monitor alarms. d. room temperature. , B, C, D Anxiety is likely to result from loss of control, the inability to communicate, continuous noise and lighting, excessive stimulation (including repeated vital sign measurements), lack of mobility, and uncomfortable room temperatures. Increased anxiety levels often lead to increased pain perception. DIF:Cognitive Level: ComprehensionREF:p. 48 OBJ: Identify factors that place the critically ill patient at risk for developing pain and anxiety. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 7. In the healthy individual, pain and anxiety: (Select all that apply.) a. activate the sympathetic nervous system. b. decrease stress levels. c. help remove one from harm. d. increase performance levels. , C, D In the healthy person, pain and anxiety are adaptive mechanisms used to increase performance levels or to remove one from potential harm. The “fight or flight” response occurs in response to pain and/or anxiety and involves the activation of the sympathetic nervous system. Pain and anxiety, however, can induce significant stress. DIF:Cognitive Level: KnowledgeREF:p. 51 OBJ: Describe the positive and negative effects of pain and anxiety in critically ill patients. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 8. The nurse is caring for a 48-year-old patient who is intubated and on a ventilator following extensive abdominal surgery. Although the patient is responsive, the nurse is not able to read the patient’s lips as the patient attempts to mouth the words. Which of the following assessment tools would be the most appropriate for the nurse to use when assessing the patient’s pain level? (Select all that apply.) a. The FACES scale b. Pain IntensityScale c. The PQRST method d. The Visual Analogue Scale , D The PQRST method and the Pain Intensity Scale require verbalization and/or writing to communicate pain level. The FACES scale and the Visual Analogue Scale can be used by simply having the patient point to the appropriate place. Because of this, they are the easiest to use with children, people with language barriers, and intubated patients. DIF:Cognitive Level: ApplicationREF:p. 54 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 9. In the critically ill patient, an incomplete assessment and/or management of pain or anxiety may be hampered by which of the following? (Select all that apply.) a. Administration of neuromuscular blocking agents b. Delirium c. Effective nurse communication and assessment skills d. Nonverbal patients , B, D Delirium appears in approximately 80% of patients in the intensive care unit. Delirium is characterized by changing mental status, inattention, disorganized thinking, and altered levels of consciousness. Patients in the intensive care unit may not be able to verbalize because of the presence of an artificial airway, sedative medication, neuromuscular blocking agents, or brain injury. Effective nurse-to-patient communication and assessment skills would facilitate assessment of pain and anxiety. DIF:Cognitive Level: ComprehensionREF:p. 58 OBJ: Describe methods and tools for assessing pain and anxiety in the critically ill patient. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 10. Which of the following are accepted nonpharmacological approaches to managing pain and/or anxiety in critically ill patients? (Select all that apply.) a. Environmental manipulation b. Explanations of monitoring equipment c. Guided imagery d. Music therapy , B, C, D Manipulating the environment so it appears less hostile helps decrease anxiety, as does continually reorienting the patient.. Focus techniques such as guided imagery and music therapy can create a state of relaxation. DIF:Cognitive Level: ComprehensionREF:p. 65 OBJ:Identify nonpharmacological and pharmacological strategies to promote comfort and reduce anxiety.TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 11. The nurse is caring for a postoperative patient in the critical care unit. The physician has ordered patient-controlled analgesia (PCA) for the patient. The nurse understands that the PCA: (Select all that apply.) a. is a safe and effective method for administering analgesia. b. has potentially fewer side effects than other routes of analgesic administration. c. is an ideal method to provide critically ill patients some control over their treatment. d. provides good quality analgesia. , B, D PCA is safe and effective, provides good-quality analgesia, and has potentially fewer side effects than other routes. PCA management is rarely appropriate for critically ill patients because most patients are unable to depress the button, or they are too ill to manage their pain effectively. DIF:Cognitive Level: ComprehensionREF:p. 67 OBJ:Identify nonpharmacological and pharmacological strategies to promote comfort and reduce anxiety.TOP:Nursing Process Step: Planning MSC: NCLEX: Physiological Integrity 12. A patient requires neuromuscular blockade (NMB) as part of treatment of refractive increased intracranial pressure. The nursing care for this patient includes: (Select all that apply.) a. administration of sedatives concurrently with neuromuscular blockade. b. dangling the patient’s feet over the edge of the bed and assisting the patient to sit up in a chair at least twice each day. c. ensuring that deep vein thrombosis prophylaxis is initiated. d. providing interventions for eye care, oral care, and skin care. , C, D Patients receiving NMB must be provided total care, including eye, skin, and oral care interventions. Patients are at high risk for deep vein thrombosis secondary to drug-induced paralysis and bed rest. Sedatives must be administered concurrently with NMB, because NMBs have no sedative effects. Although many critically ill patients are assisted to the chair, chair activity is not appropriate for patients receiving NMB; passive exercise is most appropriate. DIF:Cognitive Level: AnalysisREF:p. 60 OBJ: Discuss assessment and management challenges in subsets of critically ill patients. TOP:Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 13. The nurse is assessing the critically ill patient for delirium. The nurse recognizes which characteristics that indicate hyperactive delirium? (Select all that apply.) a. Agitation b. Apathy c. Biting d. Hitting e. Restlessness , C, D, E All except for apathy are characteristics of hyperactive delirium. Apathy is seen in hypoactive cases. Ch 7 1. The nurse is caring for a patient who is on a cardiac monitor. The nurse realizes that the sinus node is the pacemaker of the heart because it is: a. the fastest pacemaker cell in the heart. b. the only pacemaker cell in the heart. c. the only cell that does not affect the cardiac cycle. d. located in the left side of the heart. The cardiac cycle begins with an impulse that is generated from a small concentrated area of pacemaker cells high in the right atria called the sinoatrial node (sinus node or SA node). The SA node has the fastest rate of discharge and thus is the dominant pacemaker of the heart. The AV node has pacemaker properties and can discharge an impulse if the SA node fails. The ventricles have pacemaker capabilities if the sinus node or the AV node ceases to generate impulses. DIF: Cognitive Level: Comprehension REF: p. 95 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 2. One of the functions of the atrioventricular (AV) node is to: a. pace the heart if the ventricles fail. b. slow the impulse arriving from the SA node. c. send the impulse to the SA node. d. allow for ventricular filling during systole. The impulse from the SA node quickly reaches the atrioventricular (AV) node located in the area called the AV junction, between the atria and the ventricles. Here the impulse is slowed to allow time for ventricular filling during relaxation or ventricular diastole. The AV node has pacemaker properties and can discharge an impulse if the SA node (not the ventricle) fails. The electrical impulse is then rapidly conducted through the bundle of His to the ventricles (not the SA node) via the left and right bundle branches. DIF: Cognitive Level: Comprehension REF: p. 95 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 3. The normal rate for the SA node when the patient is at rest is: a. 40 to 60 beats per minute. b. 60 to 100 beats per minute. c. 20 to 40 beats per minute. d. more than100 beats per minute. The sinus node reaches threshold at a rate of 60 to 100 times per minute. Because this is the fastest pacemaker in the heart, the SA node is the dominant pacemaker of the heart. The AV node has an inherent rate of 40 to 60 beats per minute and the His-Purkinje system can fire at a rate of 20 to 40 beats per minute. Sinus tachycardia results when the SA node fires faster than 100 beats per minute. DIF: Cognitive Level: Knowledge REF: p. 97, 112 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 4. When assessing the 12-lead electrocardiogram (ECG) or a rhythm strip, it is helpful to understand that the electrical activity is viewed in relation to the positive electrode of that particular lead. When an electrical signal is aimed directly at the positive electrode, the inflection will be: a. negative. b. upside down. c. upright. d. equally positive and negative. When an electrical signal is aimed directly at the positive electrode, an upright inflection is visualized. If the impulse is going away from the positive electrode, a negative deflection is seen; and if the signal is perpendicular to the imaginary line between the positive and negative poles of the lead, the tracing is equiphasic, with equally positive and negative deflection. DIF: Cognitive Level: Comprehension REF: p. 98 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 5. The patient is admitted with a condition that requires cardiac rhythm monitoring. To apply the monitoring electrodes, the nurse must first: a. apply a moist gel to the chest. b. make certain that the electrode gel is dry. c. avoid soaps to avoid skin irritation. d. clip chest hair if needed. Adequate skin preparation of electrode sites requires clipping the hair, cleansing the skin, and drying vigorously (moisture gels are not applied). Cleansing includes washing with soap and water, or alcohol, to remove skin debris and oils. Before application, the electrodes are checked to ensure that the gel is moist. It is difficult for electrodes to adhere to the chest in the presence of chest hair. Clipping, not shaving, is recommended since shaving may create small nicks that can become a portal for infection. DIF: Cognitive Level: Application REF: p. 102 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 6. Electrocardiogram (ECG) paper contains a standardized grid where the horizontal axis measures time and the vertical axis measures voltage or amplitude. The nurse must understand that each horizontal box indicates: a. 200 milliseconds or 0.20 seconds duration. b. 40 milliseconds or 0.04 seconds duration. c. 3 seconds duration. d. millivolts of amplitude. ECG paper contains a standardized grid where the horizontal axis measures time and the vertical axis measures voltage or amplitude. Horizontally, the smaller boxes denote 0.04 seconds each or 40 milliseconds; the larger box contains five smaller boxes and thus equals 0.20 seconds or 200 milliseconds. DIF: Cognitive Level: Comprehension REF: p. 105 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 7. The nurse is examining the patient’s cardiac rhythm strip in lead II and notices that all of the P waves are upright and look the same except one that has a different shape and is inverted. The nurse realizes that the P wave with the abnormal shape is probably: a. from the SA node since all P waves come from the SA node. b. from some area in the atria other than the SA node. c. indicative of ventricular depolarization. d. normal even though it is inverted in lead II. Normally a P wave indicates that the SA node initiated the impulse that depolarized the atrium. However, a change in the shape of the P wave may indicate that the impulse arose from a site in the atria other than the SA node. The P wave represents atrial depolarization. It is usually upright in leads I and II and has a rounded, symmetrical shape. The amplitude of the P wave is measured at the center of the waveform and normally does not exceed three boxes, or 3 millimeters, in height. DIF: Cognitive Level: Analysis REF: p. 105 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 8. The QT interval is the total time taken for ventricular depolarization and repolarization. Prolongation of the QT interval: a. decreases the risk of lethal dysrhythmias. b. usually occurs when heart rate increases. c. increases the risk of lethal dysrhythmias. d. can only be measured with irregular rhythms. The QT interval is measured from the beginning of the QRS complex to the end of the T wave. This interval measures the total time taken for ventricular depolarization and repolarization. Abnormal prolongation of the QT interval increases vulnerability to lethal dysrhythmias, such as ventricular tachycardia and fibrillation. Normally, the QT interval becomes longer with slower heart rates and shortens with faster heart rates, thus requiring a correction of the value (QTc). Generally, the QT interval is less than half the RR interval. QTc accuracy is based on a regular rhythm. In irregular rhythms such as atrial fibrillation, an average QTc may be necessary because the QT varies from beat to beat. DIF: Cognitive Level: Comprehension REF: p. 107 OBJ: Explain the relationships between electrical and mechanical events in the heart. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 9. The patient has an irregular heart rhythm. To determine an accurate heart rate, the nurse first: a. identifies the markers on the ECG paper that indicate a 6-second strip. b. counts the number of large boxes between two consecutive P waves. c. counts the number of small boxes between two consecutive QRS complexes. d. divides the number of complexes in a 6-second strip by 10. Six-second method: A quick and easy estimate of heart rate can be accomplished by counting the number of P waves or QRS waves within a 6-second strip to obtain atrial and ventricular heart rates per minute. This is the optimal method for irregular rhythms. Identify the lines above the ECG paper that represent 6 seconds, and count the number of P waves within the lines; then add a zero (multiply by 10) to identify the atrial heart rate estimate for 1 minute. Next, identify the number of QRS waves in the 6-second strip and again add a zero to identify the ventricular rate. Large box method: In this method, two consecutive P and QRS waves are located. The number of large boxes between the highest points of two consecutive P waves is counted, and that number of large boxes is divided into 300 to determine the atrial rate in beats per minute. The number of large boxes between the highest points of two consecutive QRS waves is counted, and that number of large boxes is divided into 300 to determine the ventricular rate. This method is accurate only if the rhythm is regular. Small box method: The small box method is used to calculate the exact rate of a regular rhythm. In this method, two consecutive P and QRS waves are located. The number of small boxes between the highest points of these consecutive P waves is counted, and that number is divided into 1500 to determine the atrial rate in beats per minute. The number of small boxes between the highest points of two consecutive QRS waves is counted, and that number is divided into 1500 to determine the ventricular rate. This method is accurate only if the rhythm is regular. DIF: Cognitive Level: Application REF: p. 108 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 10. The nurse is calculating the rate for a regular rhythm. There are 20 small boxes between each P wave and 20 small boxes between each R wave. What is the ventricular rate? a. 50 beats/min b. 75 beats/min c. 85 beats/min d. 100 beats/min The rule of 1500 is used to calculate the exact rate of a regular rhythm. The number of small boxes between the highest points of two consecutive R waves is counted, and that number of small boxes is divided into 1500 to determine the ventricular rate. 1500/20 = 75 beats/min. This method is accurate only if the rhythm is regular. DIF: Cognitive Level: Application REF: p. 108 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 11. The patient is admitted with a fever and rapid heart rate. The patient’s temperature is 103° F (39.4° C).The nurse places the patient on a cardiac monitor and finds the patient’s atrial and ventricular rates are above 105 beats per minute. P waves are clearly seen and appear normal in configuration. QRS complexes are normal in appearance and 0.08 seconds wide. The rhythm is regular, and blood pressure is normal. The nurse should focus on providing: a. medications to lower heart rate. b. treatment to lower temperature. c. treatment to lower cardiac output. d. treatment to reduce heart rate. Sinus tachycardia results when the SA node fires faster than 100 beats per minute. Sinus tachycardia is a normal response to stimulation of the sympathetic nervous system. Sinus tachycardia is also a normal finding in children younger than 6 years. Both atrial and ventricular rates are greater than 100 beats per minute, up to 160 beats per minute, but may be as high as 180 beats per minute. Sinus tachycardia is regular or essentially regular. PR interval is 0.12 to 0.20 seconds. QRS interval is 0.06 to 0.10 seconds. P and QRS waves are consistent in shape. P waves are small and rounded. A P wave precedes every QRS complex, which is then followed by a T wave. The fast heart rhythm may cause a decrease in cardiac output because of the shorter filling time for the ventricles. Lowering cardiac out further may complicate the situation. The dysrhythmia itself is not treated, but the cause is identified and treated appropriately. For example, if the patient has a fever or is in pain, the infection or pain is treated appropriately. DIF: Cognitive Level: Analysis REF: p. 112 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 12. The nurse is working on the night shift when she notices sinus bradycardia on the patient’s cardiac monitor. The nurse should: a. give atropine to increase heart rate. b. begin transcutaneous pacing of the patient. c. start a dopamine infusion to stimulate heart function. d. assess for hemodynamic instability. Sinus bradycardia may be a normal heart rhythm for some individuals such as athletes, or it may occur during sleep. Assess for hemodynamic instability related to the bradycardia. If the patient is symptomatic, interventions include administration of atropine. If atropine is not effective in increasing heart rate, then transcutaneous pacing, dopamine infusion, or epinephrine infusion may be administered. Atropine is avoided for treatment of bradycardia associated with hypothermia. DIF: Cognitive Level: Application REF: p. 113 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 13. Which of the following is true about a patient diagnosed with sinus arrhythmia? a. The heart rate varies, dependent on vagal tone and respiratory pattern. b. Immediate treatment is essential to prevent death. c. Sinus arrhythmia is not well tolerated by most patients. d. PR and QRS interval measurements are prolonged. Sinus arrhythmia is a cyclical change in heart rate that is associated with respiration. The heart rate increases slightly during inspiration and slows slightly during exhalation because of changes in vagal tone. The ECG tracing demonstrates an alternating pattern of faster and slower heart rate that changes with the respiratory cycle. Interval measurements are normal. This rhythm is tolerated well, and no treatment is required. DIF: Cognitive Level: Knowledge REF: p. 113 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 14. The patient is admitted with sinus pauses causing periods of loss of consciousness. The patient is asymptomatic, awake and alert, but fatigued. He answers questions appropriately. When admitting this patient, the nurse should first: a. prepare the patient for temporary pacemaker insertion. b. prepare the patient for permanent pacemaker insertion. c. assess the patient’s medication profile. d. apply transcutaneous pacemaker paddles. AV nodal blocking medications (such as beta-blockers, calcium channel blockers, and digoxin) and increased vagal tone may cause sinus exit block. Causes are explored, and prescribed medications may need to be adjusted or discontinued. If patients are symptomatic, significant numbers of pauses may require treatment, including temporary (including transcutaneous) and permanent implantation of a pacemaker. DIF: Cognitive Level: Application REF: p. 114 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 15. The patient’s heart rate is 165 beats per minute. His cardiac monitor shows a rapid rate with narrow QRS complexes. The P waves cannot be seen, but the rhythm is regular. The patient’s blood pressure has dropped from 124/62 to 78/30. His skin is cold and diaphoretic and he is complaining of nausea. The nurse prepares the patient for: a. administration of beta-blockers. b. administration of atropine. c. transcutaneous pacemaker insertion. d. emergent cardioversion. If an abnormal P wave cannot be visualized on the ECG but the QRS complex is narrow, the term supraventricular tachycardia (SVT) is often used. This is a generic term that describes any tachycardia that is not ventricular in origin; it is also used when the source above the ventricles cannot be identified, usually because the rate is too fast. Treatment is directed at assessing the patient’s tolerance of the tachycardia. If the rate is higher than 150 beats per minute and the patient is symptomatic, emergent cardioversion is considered. Cardioversion is the delivery of a synchronized electrical shock to the heart by an external defibrillator. Beta-blockers are a possibility if the patient is not symptomatic. Atropine is used in the treatment of bradycardia. If atropine is not effective in increasing heart rate, then transcutaneous pacing is implemented. DIF: Cognitive Level: Analysis REF: p. 123 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation MSC: NCLEX: Physiological Integrity 16. The nurse is reading the cardiac monitor and notes that the patient’s heart rhythm is extremely irregular and there are no discernible P waves. The ventricular rate is 90 beats per minute, and the patient is hemodynamically stable. The nurse realizes that the patient’s rhythm is: a. atrial fibrillation. b. atrial flutter. c. atrial flutter with rapid ventricular response. d. junctional escape rhythm. Atrial fibrillation arises from multiple ectopic foci in the atria, causing chaotic quivering of the atria and ineffectual atrial contraction. The AV node is bombarded with hundreds of atrial impulses and conducts these impulses in an unpredictable manner to the ventricles. The atrial rate may be as high 700 and no discernible P waves can be identified, resulting in a wavy baseline and an extremely irregular ventricular response. Atrial flutter arises from a single irritable focus in the atria. The atrial focus fires at an extremely rapid, regular rate, between 240 and 320 beats per minute. The P waves are called flutter waves and may have a sawtooth appearance. The ventricular response may be regular or irregular based on how many flutter waves are conducted through the AV node. Atrial flutter with rapid ventricular response occurs when atrial impulses cause a ventricular response greater than 100 beats per minute. A junctional escape rhythm is a ventricular rate between 40 and 60 beats per minute with a regular rhythm. P waves may be absent, inverted, or follow the QRS complex. If a P wave is present before the QRS complex, the PR interval is shortened less than 0.12 milliseconds. QRS complex is normal. DIF: Cognitive Level: Analysis REF: p. 119 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 17. The patient’s heart rhythm shows an inverted P wave with a PR interval of 0.06 seconds. The heart rate is 54 beats per minute. The nurse recognizes the rhythm as a junctional escape rhythm, and understands that the rhythm is due to the: a. loss of sinus node activity. b. increased rate of the AV node. c. increased rate of the SA node. d. decreased rate of the AV node. Junctional escape rhythm occurs when the dominant pacemaker, the SA node, fails to fire. The normal heart rate of the AV node is 40 to 60 beats per minute, so the AV node rate has neither increased nor decreased. An increased SA node rate would override the AV node. DIF: Cognitive Level: Knowledge REF: p. 121 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 18. The patient’s heart rate is 70 beats per minute, but the P waves come after the QRS complex. The nurse correctly determines that the patient’s heart rhythm is: a. a normal junctional rhythm. b. an accelerated junctional rhythm. c. a junctional tachycardia. d. atrial fibrillation. The normal intrinsic rate for the AV node and junctional tissue is 40 to 60 beats per minute, but rates can accelerate. An accelerated junctional rhythm has a rate between 60 and 100 beats per minute, and the rate for junctional tachycardia is greater than 100 beats per minute. If P wave precedes QRS, it is inverted or upside down; the P wave may not be visible, or it may follow the QRS. If a P wave is present before the QRS, the PR interval is shortened less than 0.12 milliseconds. Atrial fibrillation arises from multiple ectopic foci in the atria, causing chaotic quivering of the atria and ineffectual atrial contraction. The AV node is bombarded with hundreds of atrial impulses and conducts these impulses in an unpredictable manner to the ventricles. DIF: Cognitive Level: Analysis REF: p. 121 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 19. The patient is having premature ventricular contractions (PVCs). The nurse’s greatest concern should be: a. the proximity of the R wave of the PVC to the T wave of a normal beat. b. the fact that PVCs are occurring, because they are so rare. c. if the number of PVCs are decreasing. d. if the PVCs are wider than 0.12 seconds. The peak of the T wave through the downslope of the T wave is considered the vulnerable period, which coincides with partial repolarization of the ventricles. If a PVC occurs during the T wave, ventricular tachycardia may occur. When the R wave of PVC falls on the T wave of a normal beat, it is referred to as the R-on-T phenomenon. PVCs may occur in healthy individuals and usually do not require treatment. The nurse must determine if PVCs are increasing in number by evaluating the trend. If PVCs are increasing, the nurse should evaluate for potential causes such as electrolyte imbalances, myocardial ischemia or injury, and hypoxemia. Runs of nonsustained ventricular tachycardia may be a precursor to development of sustained ventricular tachycardia. Because the stimulus depolarizes the ventricles in a slower, abnormal way, the QRS complex appears widened and has a bizarre shape. The QRS complex is wider than 0.12 seconds and often wider than 0.16 seconds. DIF: Cognitive Level: Analysis REF: pp. 123-124 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 20. The nurse notices ventricular tachycardia on the heart monitor. When the patient is assessed, the patient is found to be unresponsive with no pulse. The nurse should: a. treat with intravenous amiodarone or lidocaine. b. begin cardiopulmonary resuscitation and advanced life support. c. provide electrical cardioversion. d. ignore the rhythm since it is benign. Ventricular tachycardia (VT) is a rapid, life-threatening dysrhythmia originating from a single ectopic focus in the ventricles. Determine whether the patient has a pulse. If no pulse is present, provide emergent basic and advanced life-support interventions, including defibrillation. If a pulse is present and the blood pressure is stable, the patient can be treated with intravenous amiodarone or lidocaine. Cardioversion is used as an emergency measure in patients who become hemodynamically unstable but continue to have a pulse. It also may be used in nonemergency situations, such as when a patient has asymptomatic VT. DIF: Cognitive Level: Application| Cognitive Level: Analysis REF: p. 126 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation|Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 21. The nurse is talking with the patient when the monitor alarms and shows a wavy baseline without a PQRST complex. The nurse should: a. defibrillate the patient immediately. b. initiate basic life support. c. initiate advanced life support. d. assess the patient and the electrical leads. Ventricular fibrillation (VF) is a chaotic rhythm characterized by a quivering of the ventricles, which results in total loss of cardiac output and pulse. VF is a life-threatening emergency, and the more immediate the treatment is, the better the survival will be. VF produces a wavy baseline without a PQRST complex. Because a loose lead or electrical interference can produce a waveform similar to VF, it is always important to immediately assess the patient for pulse and consciousness. DIF: Cognitive Level: Analysis| Cognitive Level: Application REF: p. 126 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation|Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 22. The nurse notices that the patient has a first-degree AV block. Everything else about the rhythm is normal. The nurse should: a. prepare to place the patient on a transcutaneous pacemaker. b. give the patient atropine to shorten the PR interval. c. monitor the rhythm and patient’s condition. d. give the patient an antiarrhythmic medication. First-degree AV block is a common dysrhythmia in the elderly and in patients with cardiac disease. As the normal conduction pathway ages or becomes diseased, impulse conduction becomes slower than normal. It is well tolerated. No treatment is required. Continue to monitor the patient and the rhythm. DIF: Cognitive Level: Application| Cognitive Level: Analysis REF: p. 129 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Implementation|Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 23. The nurse understands that in a third-degree AV block: a. every P wave is conducted to the ventricles. b. some P waves are conducted to the ventricles. c. none of the P waves are conducted to the ventricles. d. the PR interval is prolonged. In first-degree AV block, a P wave precedes every QRS complex, which is followed by a T wave indicating complete conduction. It is represented on the ECG as a prolonged PR interval. Second-degree heart block refers to AV conduction that is intermittently blocked. Therefore, some P waves are conducted and some are not. Third-degree block is often called complete heart block because no atrial impulses are conducted through the AV node to the ventricles. DIF: Cognitive Level: Knowledge REF: pp. 131-132 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 24. The patient is asymptomatic but is diagnosed with second-degree heart block Mobitz I. The patient is on digitalis medication at home. The nurse should expect that: a. the patient has had an anterior wall myocardial infarction. b. the physician will order the digitalis to be continued in the hospital. c. a digitalis level would be ordered upon admission. d. the patient will require a transcutaneous pacemaker. Digitalis toxicity is a major cause of this rhythm, and further digitalis doses should not be given until a digitalis level is obtained. Other causes of Mobitz I include AV nodal blocking drugs, acute inferior wall myocardial infarction or right ventricular infarction, ischemic heart disease, and excess vagal response. This type of block is usually well tolerated and no treatment is indicated unless the dropped beats occur frequently. DIF: Cognitive Level: Analysis REF: pp. 129-130 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 25. The patient is scheduled to have a permanent pacemaker implanted. The patient asks the nurse, “How long will the battery in this thing last?” The nurse should answer, a. “Life expectancy is about 1 year. Then it will need to be replaced.” b. “Pacemaker batteries can last up to 25 years with constant use.” c. “Battery life varies depending on usage, but it can last up to 10 years.” d. “Pacemakers are used to treat temporary problems so the batteries don’t last long.” Implanted permanent pacemakers are used to treat chronic conditions. These devices have a battery life of up to 10 years, which varies based on the manufacturer’s recommendations. DIF: Cognitive Level: Knowledge REF: p. 132 OBJ: Explain the basic concepts of cardiac pacing. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 26. The patient is in chronic junctional escape rhythm with no atrial activity noted. Studies have demonstrated normal AV node function. This patient may be a candidate for which type of pacing? a. Atrial pacing b. Ventricular pacing c. Dual-chamber pacing d. Transcutaneous pacing Pacemakers may be used to stimulate the atrium, ventricle, or both chambers (dual-chamber pacemakers). Atrial pacing is used to mimic normal conduction and to produce atrial contraction, thus providing atrial kick. This is the case in the scenario provided. Ventricular pacing stimulates ventricular depolarization and is commonly used in emergency situations or when pacing is required infrequently. Dual-chamber pacing allows for stimulation of both atria and ventricles as needed to synchronize the chambers and mimic the normal cardiac cycle. However, with this patient, ventricular and AV function are normal. DIF: Cognitive Level: Analysis REF: p. 133 OBJ: Explain the basic concepts of cardiac pacing. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 27. The patient has a permanent pacemaker inserted. The provider has set the pacemaker to the demand mode at a rate of 60 beats per minute. The nurse realizes that: a. the pacemaker will pace only if the patient’s intrinsic heart rate is less than 60 beats per minute. b. the demand mode often competes with the patient’s own rhythm. c. the demand mode places the patient at risk for the R-on-T phenomenon. d. the fixed rate mode is safer and is the mode of choice. Pacemakers can be operated in a demand mode or a fixed rate (asynchronous) mode. The demand mode paces the heart when no intrinsic or native beat is sensed. For example, if the rate control is set at 60 beats per minute, the pacemaker will only pace if the patient’s heart rate drops to less than 60. The fixed rate mode paces the heart at a set rate, independent of any activity the patient’s heart generates. The fixed rate mode may compete with the patient’s own rhythm and deliver an impulse on the T wave (R-on-T phenomenon), with the potential for producing ventricular tachycardia or fibrillation. The demand mode is safer and is the mode of choice. DIF: Cognitive Level: Comprehension REF: p. 133 OBJ: Explain the basic concepts of cardiac pacing. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 28. The patient has a permanent pacemaker in place with a demand rate set at 60 beats/min. The cardiac monitor is showing a heart rate of 44 beats/min with no pacemaker spikes. The nurse realizes this as: a. normal pacemaker function. b. failure to capture. c. failure to pace. d. failure to sense. Failure to pace or fire occurs when the pacemaker fails to initiate an electrical stimulus when it should fire. The problem is noted by absence of pacer spikes on the rhythm strip. Causes of failure to pace include battery or pulse generator failure, fracture or displacement of a pacemaker wire, or loose connections. This is not normal pacemaker function. When the pacemaker generates an electrical impulse (pacer spike) and no depolarization is noted, it is described a failure to capture. On the ECG, a pacer spike is noted, but it is not followed by a P wave (atrial pacemaker) or a QRS complex (ventricular pacemaker). Common causes of failure to capture include output (milliamperes) set too low, or displacement of the pacing lead wire from the myocardium (transvenous or epicardial leads). Other causes of failure to capture include battery failure, fracture of the pacemaker wire, or increased pacing threshold as a result of medication or electrolyte imbalance. When the pacemaker does not sense the patient’s own cardiac rhythm and initiates an electrical impulse, it is called failure to sense. Failure to sense manifests as pacer spikes that fall too closely to the patient’s own rhythm, earlier than the programmed rate. The most common cause is displacement of the pacemaker electrode wire. DIF: Cognitive Level: Analysis REF: p. 135 | Figure 7-61 OBJ: Explain the basic concepts of cardiac pacing. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 29. The rhythm on the cardiac monitor is showing numerous pacemaker spikes, but no P waves or QRS complexes following the spikes. The nurse realizes this as: a. normal pacemaker function. b. failure to capture. c. failure to pace. d. failure to sense. When the pacemaker generates an electrical impulse (pacer spike) and no depolarization is noted, it is described a failure to capture. On the ECG, a pacer spike is noted, but it is not followed by a P wave (atrial pacemaker) or a QRS complex (ventricular pacemaker). Common causes of failure to capture include output (milliamperes) set too low, or displacement of the pacing lead wire from the myocardium (transvenous or epicardial leads). Other causes of failure to capture include battery failure, fracture of the pacemaker wire, or increased pacing threshold as a result of medication or electrolyte imbalance. This is not normal pacemaker function. Failure to pace or fire occurs when the pacemaker fails to initiate an electrical stimulus when it should fire. The problem is noted by absence of pacer spikes on the rhythm strip. Causes of failure to pace include battery or pulse generator failure, fracture or displacement of a pacemaker wire, or loose connections. When the pacemaker does not sense the patient’s own cardiac rhythm and initiates an electrical impulse, it is called failure to sense. Failure to sense manifests as pacer spikes that fall too closely to the patient’s own rhythm, earlier than the programmed rate. The most common cause is displacement of the pacemaker electrode wire. DIF: Cognitive Level: Analysis REF: p. 135 | Figure 7-62 OBJ: Explain the basic concepts of cardiac pacing. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity MULTIPLE RESPONSE 1. The normal width of the QRS complex is which of the following? (Select all that apply.) a. 0.06 to 0.10 seconds. b. 0.12 to 0.20 seconds. c. 1.5 to 2.5 small boxes. d. 3.0 to 5.0 small boxes. e. 0.04 seconds or greater. , C The waveform that initiates the QRS complex (whether it is a Q wave or an R wave) marks the beginning of the interval. The normal width of the QRS complex is 0.06 to 0.10 seconds. This width equals 1.5 to 2.5 small boxes. The normal PR interval is 0.12 to 0.20 seconds, three to five small boxes wide; not the QRS interval. A pathological Q wave has a width of 0.04 seconds and a depth that is greater than one fourth of the R wave amplitude; therefore, the QRS complex would be wider than that. DIF: Cognitive Level: Knowledge REF: p. 106 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 2. Which of the following are common causes of sinus tachycardia? (Select all that apply.) a. Hyperthyroidism b. Hypovolemia c. Hypothyroidism d. Heart Failure e. Sleep , B, D Common causes of sinus tachycardia include hyperthyroidism, hypovolemia, heart failure, anemia, exercise, use of stimulants, fever, and sympathetic response to fear or pain and anxiety. Hypothyroidism and sleep tend to slow the heart rate. DIF: Cognitive Level: Analysis REF: p. 112 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 3. Sinus bradycardia is a symptom of which of the following? (Select all that apply.) a. Calcium channel blocker medication b. Beta-blocker medication c. Athletic conditioning d. Hypothermia e. Hyperthyroidism , B, C, D Vasovagal response; medications such as digoxin or AV nodal blocking agents, including calcium channel blockers and beta-blockers; myocardial infarction; normal physiological variant in the athlete; disease of the sinus node; increased intracranial pressure; hypoxemia; and hypothermia may cause sinus bradycardia. Hyperthyroidism is a cause of sinus tachycardia. DIF: Cognitive Level: Analysis REF: pp. 112-113 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 4. The nurse is caring for a patient who has atrial fibrillation. Sequelae that place the patient at greater risk for mortality/morbidity include which of the following? (Select all that apply.) a. Stroke b. Ashman beats c. Pulmonary emboli d. Prolonged PR interval e. Decreased cardiac output , C, E One complication of atrial fibrillation is thromboembolism. The blood that collects in the atria is agitated by fibrillation, and normal clotting is accelerated. Small thrombi, called mural thrombi, begin to form along the walls of the atria. These clots may dislodge, resulting in pulmonary embolism or stroke. The ineffectual contraction of the atria results in loss of “atrial kick.” If too many impulses conduct to the ventricles, atrial fibrillation with rapid ventricular response may result and compromise cardiac output. Ashman beats are not clinically significant. No recognizable or discernible P waves are present; therefore, PR interval is absent. DIF: Cognitive Level: Analysis REF: p. 119 OBJ: Describe appropriate interventions for common dysrhythmias. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 5. Because of the location of the AV node, the possible P waveforms that are associated with junctional rhythms include which of the following? (Select all that apply.) a. No P wave b. Inverted P wave c. Shortened PR interval d. P wave after the QRS complex e. Normal P wave and PR interval , B, C, D Because of the location of the AV node—in the center of the heart—impulses generated may be conducted forward, backward, or both. With the potential of forward, backward, or bidirectional impulse conduction, three different P waveforms may be associated with junctional rhythms: When the AV node impulse moves forward, P waves may be absent because the impulse enters the ventricle first. The atria receives the wave of depolarization at the same time as the ventricles; thus, because of the larger muscle mass of the ventricles, there is no P wave. When the AV node impulse is conducted backward, the impulse enters the atria first. When depolarization occurs backward, an inverted P wave is created. Once the atria have been depolarized, the impulse moves down the bundle of His and depolarizes both ventricles normally. A short PR interval (<0.12 second) is noted. When the impulse is conducted both forward and backward, P waves may be present after the QRS complex. DIF: Cognitive Level: Knowledge REF: p. 120 OBJ: Interpret the basic dysrhythmias generated from the sinoatrial node, the atria, the atrioventricular node, and the ventricles. TOP: Nursing Process Step: Assessment MSC: NCLEX: Physiological Integrity 6. The patient is in third-degree heart block (complete heart block) and is symptomatic. The treatment for this patient is which of the following? (Select all that apply.) a. transcutaneous pacemaker. b. atropine IV. c. temporary transvenous pacemaker. d. permanent pacemaker. e. amiodarone IV. , C, D Treatments include transcutaneous or transvenous pacing and implanting a permanent pacemaker. Atropine reduces vagal tone, but that is not a cause of complete heart block and will produce more P waves, but the P waves will still not be associated with the QRS complexes. It is important to note that the only treatment is pacing. Amiodarone IV is used to suppress ventricular dysrhythmia and is not used to treat third-degree heart block. [Show More]
Last updated: 2 years ago
Preview 1 out of 43 pages
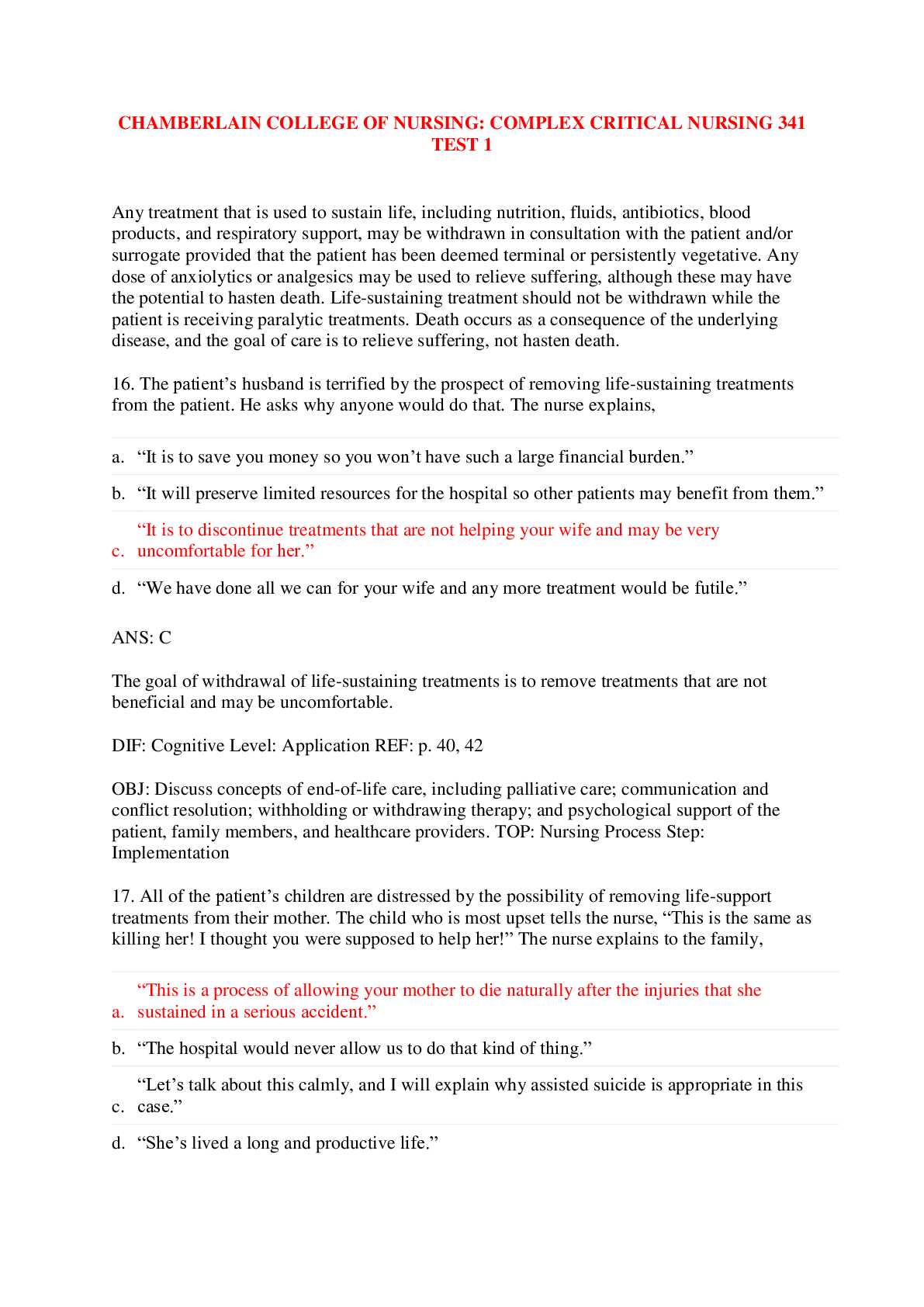
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$5.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 24, 2019
Number of pages
43
Written in
Additional information
This document has been written for:
Uploaded
Sep 24, 2019
Downloads
0
Views
144