*NURSING > EXAM > NURS 6560 Midtem Exam, Question and Answers, Latest Guide, Walden University. 2021 (All)
NURS 6560 Midtem Exam, Question and Answers, Latest Guide, Walden University. 2021
Document Content and Description Below
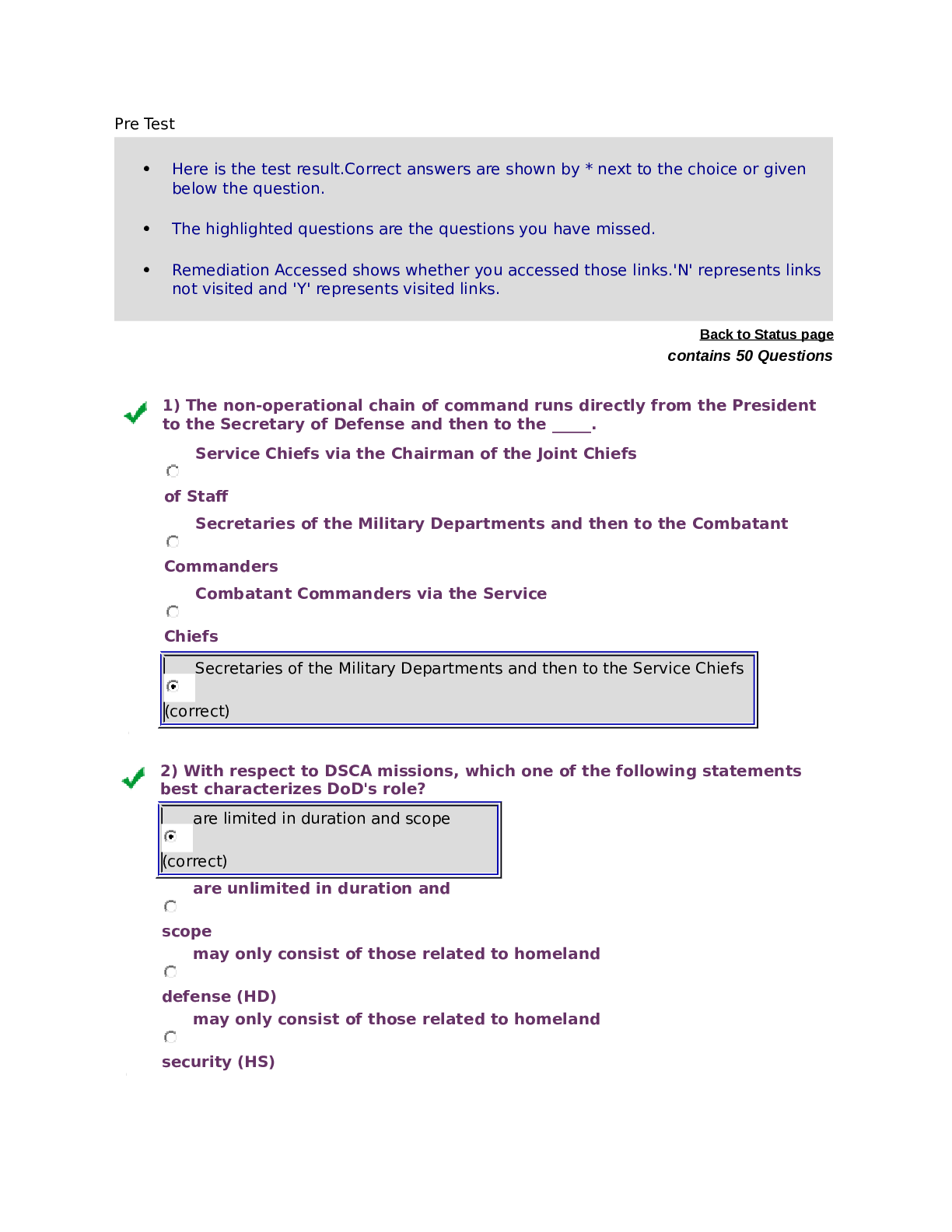
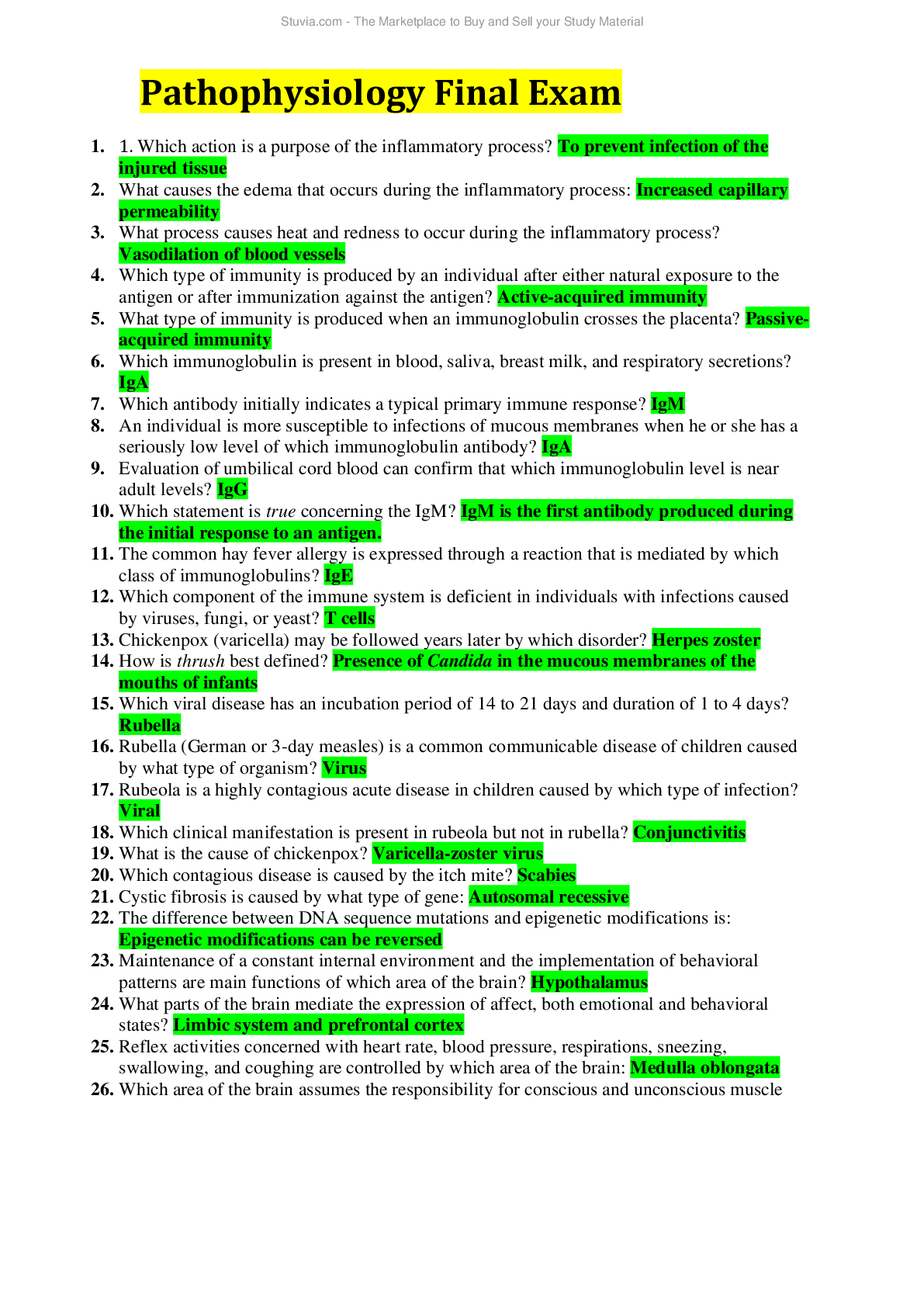
NURS 6560 Midterm Exam. Question 1 S. is a 59-year-old female who has been followed for several years for aortic regurgitation. Serial echocardiography has demonstrated normal ventricular function, bu... t the patient was lost to follow-up for the last 16 months and now presents complaining of activity intolerance and weight gain. Physical examination reveals a grade IV/VI diastolic aortic murmur and 2+ lower extremity edema to the midcalf. The AGACNP considers which of the following as the most appropriate management strategy? A. Serial echocardiography every 6 months B. Begin a calcium channel antagonist C. Begin an angiotensin converting enzyme (ACE) inhibitor D. Surgical consultation and intervention Question 2 An ascending thoracic aneurysm of > 5.5 cm is universally considered an indication for surgical repair, given the poor outcomes with sudden rupture. Regardless of the aneurysm’s size, all of the following are additional indications for immediate operation except: A. Comorbid Marfan’s syndrome B. Enlargement of > 1 cm since diagnosis C. Crushing chest pain D. History of giant cell arteritis Question 3 Jasmine is a 31-year-old female who presents with neck pain. She has a long history of injection drug use and admits to injecting opiates into her neck. Physical examination reveals diffuse tracking and scarring. Today Jasmine has a distinct inability to turn her neck without pain, throat pain, and a temperature of 102.1°F. She appears ill and has foul breath. In order to evaluate for a deep neck space infection, the AGACNP orders: A. Anteroposterior neck radiography B. CT scan of the neck C. White blood cell (WBC) differential D. Aspiration and culture of fluid Question 4 Mr. Draper is a 39-year-old male recovering from an extended abdominal procedure. As a result of a serious motor vehicle accident, he has had repair of a small bowel perforation, splenectomy, and repair of a hepatic laceration. He will be on total parenteral nutrition postoperatively. The AGACNP recognizes that the most common complications of parenteral nutrition are a consequence of: A. Poorly calculated solution B. Resultant diarrhea and volume contraction C. The central venous line used for infusion D. Bowel disuse and hypomotility Question 5 Mr. Mettenberger is being discharged following his hospitalization for reexpansion of his second spontaneous pneumothorax this year. He has stopped smoking and does not appear to have any overt risk factors. While doing his discharge teaching, the AGACNP advises Mr. Mettenberger that his current risk for another pneumothorax is: A. < 10% B. 25-50% C. 50-75% D. > 90 Question 6 One of the earliest findings for a patient in hypovolemic shock is: A. A drop in systolic blood pressure (SBP) < 10 mm Hg for > 1 minute when sitting up B. A change in mental status C. SaO2 of < 88% D. Hemoglobin and hematocrit (H&H) < 9 g/dL and 27% Question 7 Traumatic diaphragmatic hernias present in both acute and chronic forms. Patients with a more chronic form are most likely to be present with: A. Respiratory insufficiency B. Sepsis C. Bowel obstruction D. Anemia Question 8 The AGACNP is managing a patient in the ICU who is being treated for a pulmonary embolus. Initially the patient was stable, awake, alert, and oriented, but during the last several hours the patient has become increasingly lethargic. At change of shift, the oncoming staff nurse appreciates a profound change in the patient’s mental status from the day before. Vital signs and hemodynamic parameters are as follows: BP 88/54 mm Hg Pulse 110 bpm Respiratory rate 22 breaths per minute SaO2 93% on a 50% mask Systemic vascular resistance (SVR) 1600 dynes ∙ sec/cm5 Cardiac index 1.3 L/min Pulmonary capillary wedge pressure (PCWP) 8 mm Hg This clinical picture is most consistent with which shock state? A. Hypovolemic B. Cardiogenic C. Distributive D. Obstructive Question 9 When counseling patients to prevent postoperative pulmonary complications, the AGACNP knows that with respect to smoking cessation, the American College of Surgeons and National Surgical Quality Improvement Program guidelines are clear that patients who stop smoking _____ weeks before surgery have no increased risk of smokingrelated pulmonary complications. A. 2 B. 4 C. 6 D. 8 Question 10 Mitch C. is a 39-year-old male who is brought to the ED by paramedics. According to the report of a neighbor, Mitch was distraught over a breakup with his fiancée and attempted to commit suicide by mixing some chemicals from under his kitchen sink and drinking them; afterward he changed his mind and knocked on his neighbor’s door asking for help. Mitch is awake but stuporous, and the neighbor has no idea what he drank. Visual inspection of his mouth and oropharynx reveals some edema and erythema. He is coughing and has large amounts of pooling saliva. Mitch is not capable of answering questions but he appears in pain. Endoscopy reveals full thickness mucosal injury with mucosal sloughing, ulceration, and exudate. The AGACNP knows that the appropriate course of treatment must include: A.At least 6 hours of observation in the emergency department B. Periodic esophagram C. Aggressive fluid resuscitation D.Esophagogastrectomy Question 11 Jared V. is a 35-year-old male who presents for evaluation of a dry cough. He reports feeling well overall but notices that he gets out of breath more easily than he used to when playing soccer. A review of systems yields results that are essentially benign, although the patient does admit to an unusual rash on his legs. Physical examination reveals scattered erythematous nodules on both shins. There is no drainage, discomfort, or itch. Additionally, diffuse, mildly enlarged lymph nodes are appreciated bilaterally. Results of a comprehensive metabolic panel and complete blood count are within normal limits. Twelve-lead ECG reveals sinus bradycardia at 58 bpm. Chest radiography reveals bilateral hilar and mediastinal lymphadenopathy. The AGACNP suspects: A.Bronchiectasis B. Pulmonary fibrosis C. Sarcoidosis D.Lung carcinoma Question 12 Mrs. Miller is a 44-year-old female who is on postoperative day 1 following a total abdominal hysterectomy. Her urine output overnight was approximately 200 mL. The appropriate response for the AGACNP would be to order: A.A urinalysis and culture B. 1 liter of NSS over 8 hours C. Encourage increased mobility D.Liberalize salt in the diet Question 13 All of the following are risk factors for spontaneous pneumothorax except: A.Connective tissue disease B. Scuba diving C. Chronic obstructive pulmonary disease (COPD) D.Central line insertion Question 14 The AGACNP is going over preoperative information and instructions with a patient who is having a major transverse abdominal procedure tomorrow morning. The patient is very nervous and is asking a lot of questions. The AGACNP prescribes a sleeping agent because he knows that anxiety and sleeplessness may: A.Lead to hypoxia due to hyperventilation B. Increase the physiologic stress response postoperatively C. Contribute to risk of delirium and prolonged length of stay D.Decrease p.o. intake and produce nutritional risk Question 15 In a patient with thyroid nodules, which of the following is the diagnostic study of choice to rule out thyroid cancer? A.Radioiodine scanning B. Percutaneous needle biopsy C. CT scan D.Ultrasound Question 16 When counseling a patient about treatment modalities for achalasia, the AGACNP advised that which of the following is the treatment of choice? A.Calcium channel antagonists B. Intrasphincter botulinum injection C. Pneumatic dilation D.Myotomy and partial fundoplication Question 17 Mr. Liu is a 52-year-old male who has a history of thyroidectomy. He presents complaining of numbness and tingling in his legs and feet and generalized fatigue. Physical examination reveals a positive Chvostek’s sign. Which of the following laboratory studies should be ordered first? A.Renal function tests B. Parathyroid hormone C. Calcium D.Magnesium Question 18 V. is a 75-year-old male patient who, during a recent wellness evaluation, was found to have a new onset grade II/VI crescendo-decrescendo cardiac murmur at the 2nd intercostal space, right sternal border. He is symptom free and reports no limitations to his usual daily activity. He specifically denies activity intolerance or near syncope, and he is very active physically. Echocardiography reveals a mild aortic calcification. The AGACNP knows that ongoing management for R. V. must include: A.Annual or biannual serial echocardiography B. Modification of activity level C. Baseline cardiac catheterization D. Statin therapy Question 19 The lower esophageal sphincter is characterized by periods of intermittent relaxation called transient lower esophageal sphincter relaxations. These relaxations are independent of the relaxation triggered by swallowing and are the most common cause of: A. Physiologic reflux B. Symptomatic esophagitis C. Barrett’s metaplasia D.Esophageal carcinoma Question 20 While reviewing morning labs on a postoperative patient, the AGACNP notes that the patient’s basic metabolic panel is as follows: Na+ 132 mEq/L K+ 4.6 mEq/L Cl- 87 mEq/L CO2 25 mEq/L A normal saline infusion is ordered in an attempt to avoid: A.Hyperkalemia B. Hypernatremia C. Metabolic alkalosis D.Metabolic acidosis Question 21 W. is a 49-year-old man who presents for evaluation. He has a long history of alcohol and tobacco use, with a 65-year pack history and an admitted 14-drink-per-week alcohol habit. He is getting worried because he can no longer swallow his bourbon. He is not a good historian but he does admit to a 1+ year history of bloating, heartburn, and progressive difficulty swallowing food. He didn’t worry too much about his symptoms until he stopped being able to swallow bourbon. He thinks he has lost approximately 15 lbs in the last year. He denies any blood in his stool and has not had any vomiting. The AGACNP knows that the most likely diagnosis is: A.Zenker’s diverticulum B. Achalasia C. Esophageal carcinoma D.Hiatal hernia Question 22 Which of the following treatment modalities has no role in the treatment of shock? A.Lactated Ringer’s B. Fresh frozen plasma (FFP) C. Vasopressors D.Colloid solutions Question 23 The development of coronary artery disease (CAD) and, ultimately, plaque formation is a multifactorial process that includes endothelial injury from hypertension, cigarette smoking, and dyslipidemia. These events lead to endothelial cell dysfunction, which is theorized to result in: A.Decreased nitric oxide production B. Smooth muscle cell atrophy C. Collagen degradation D.Enlarged arterial lumen Question 24 Mr. Comstock is a 71-year-old male who presents with a general sense of feeling weak and unwell; he thinks he has the flu even though he received a flu vaccination this year. He describes a vague collection of symptoms, including weakness, nausea, dizziness, and “getting out of breath” very easily. He says he can barely climb the steps anymore without stopping to rest. Of the possible differential diagnoses, coronary artery disease (CAD) is high among the probabilities because of his age and gender. His physical examination is unremarkable except that he appears weak. His vital signs are as follows: temperature 98.0°F, pulse 100 bpm, respiratory rate 16 b.p.m., and BP 178/100 mm Hg. A chest radiograph is within normal limits with no acute pulmonary infection. A 12-lead ECG reveals inverted T waves in leads V1 to V5. The AGACNP is suspicious that most of his symptoms are: A. Psychosomatic B. Early congestive heart failure (CHF) C. Anginal equivalents D.Normal age-related changes Question 25 Mrs. Carpenter is a 59-year-old female who presents with an acute myocardial infarction. She is acutely short of breath and has coarse rales on auscultation. Physical examination reveals a grade V/VI systolic murmur, loudest at the point of maximal impulse with radiation to the midaxillary line. The AGACP recognizes: A. Acute mitral valve regurgitation B. Acute aortic valve regurgitation C. Acute cardiac tamponade D. Acute pulmonary embolus Question 26 Mr. Nelson is a 65-year-old male who has been advised that he is a candidate for coronary artery bypass grafting. He has been doing some internet research and is asking about whether or not he should have a “beating heart” bypass. Regarding off-pump coronary bypass grafting, the AGACNP advises Mr. Nelson that: A.There is a slightly higher risk of neurologic complications B. Long-term results suggest that the grafts do not stay open as long as those in traditional bypass grafting C. The incidence of off-pump bypass grafting has increased significantly in the last 10 years D.The off-pump procedure is considerably more expensive but is correlated with better long-term outcomes Question 27 Mrs. McCallum is a 48-year-old female who presents for evaluation of a vague set of gastrointestinal symptoms. She feels generally well and has always been healthy, but lately she has had a lot of heartburn and a sense of reflux in her throat. Most recently she has had a recurring sense of food getting stuck in her throat. The AGACNP knows that which diagnostic study should be performed first? A.Barium swallow B. Upper endoscopy C. Esophageal manometry D.Ambulatory pH monitoring Question 28 Mr. Key is a 53-year-old male patient who developed empyema following a serious bout of bacterial pneumonia. He presented as septic and was started immediately on intravenous antibiotics and drainage of the sinus cavity. Forty-eight hours later, he is much improved clinically and drainage has receded. The next step in his care would be: A.A CT scan B. Eloesser’s procedure C. Decortication D.Reexpansion Question 29 Mrs. Bowers is a 41-year-old patient who requires surgical management of osteomyelitis. She has a long history of methamphetamine use and has a BMI of 17.9 kg/m2 . She clearly is nutritionally depleted and volume contracted, but she has no clear chronic medical history except for unmedicated hypertension, which may be due to her chronic stimulant use. She denies alcohol use but admits to a 1½ pack a day cigarette habit. A primary postoperative concern for Mrs. Bowers is: A.Excess bleeding B. Thromboemboli development C. Poor wound healing D.Renal failure Question 30 The congenital diaphragmatic hernia that occurs more often in women and does not usually produce symptoms until midlife is known as: A.Zenker’s hernia B. Bochdalek’s hernia C. Morgagni’s hernia D.Atraumatic hernia Question 31 B. is a 67-year-old male who is being discharged following inpatient management for unstable angina. S. B. did not know that he had coronary artery disease (CAD) and in fact had not seen a health care provider for many years. While reviewing his lifestyle habits, he admits that he is obese, has poor eating habits, does not engage in any purposeful physical activity, and smokes two packs of cigarettes daily. He verbalizes that he is grateful that this was not a “real” heart attack and does not seem receptive to lifestyle management strategies. The AGACNP advises him that it is important to take this “warning” attack seriously because: A. 10% of patients with unstable angina will die of cardiovascular disease within 6 months B. 25% of patients with unstable angina will develop congestive heart failure within 6 months C. 65% of patients with unstable angina will have an ST elevation MI within 1 year D. 90% of patients with unstable angina will have cerebrovascular symptoms within 1 year Question 32 According to the American College of Surgeons (ACS), who among the following patients should have a chest radiograph as part of preoperative assessment? A.All patients > 40 years of age B. All patients who smoke cigarettes C. All patients having thoracic procedures D.All patients with cardiac disease Question 33 According to the Carpentier classification scheme of mitral valve regurgitation, a type I regurgitation is most likely due to: A.Cardiomyopathy B. Excessive leaflet motion C. Ruptured papillary muscles D.Rheumatic heart disease Question 34 V. is a 37-year-old female who is admitted via the emergency room after her roommate called emergency medical services (EMS). She has no significant medical history and does not know what is wrong with her. She has been feeling generally unwell for the last few days, and today she had an episode of confusion that scared her roommate to the extent that the roommate called EMS. Her physical examination reveals a temperature of 101.9°F, pulse of 110 bpm, respiratory rate of 20 breaths per minute, and blood pressure of 92/58 mm Hg. A comprehensive metabolic panel reveals a slightly elevated blood urea nitrogen (BUN)/creatinine but otherwise is normal. A white blood cell differential reveals a leukocyte count of 14,000 cells/µL with neutrophils of 83%. The AGACNP knows that these values are consistent with: A. Systemic inflammatory response syndrome (SIRS) B. High-output septic shock C. Neurogenic shock D.Multiple organ dysfunction syndrome (MODS) Question 35 Which shock state is worsened in the setting of mechanical ventilation? A. Septic B. Cardiac compressive C. Neurogenic D.Cardiogenic Question 36 B. is a 41-year-old male being admitted for surgical reduction of an open femur fracture sustained in a multiple vehicle collision. Preoperative assessment reveals that he is on beta-adrenergic antagonists after having been diagnosed with coronary artery disease approximately 1 month ago. He admits that he feels a little better but says he still gets pain in his chest when he exerts himself. He is pain free now. Vital signs are as follows: temperature 98.1°F, pulse 88 bpm, respiratory rate 18 breaths per minute, and blood pressure 142/86 mm Hg. The AGACNP knows that which of the following is the most important action before R. B. goes to the operating room? A.A cardiology consultation B. Blood pressure control C. Resuming beta-adrenergic antagonists D. Pain control Question 37 Cholesteatoma is a condition characterized by a collection of desquamated keratin leading to bony erosion in the ossicular chain and inner ear. The goal of surgery in cholesteatoma is: A. Production of a dry ear B. Preservation of sensorineural hearing C. Debridement of infection D.Restoration of the tympanic membrane Question 38 The AGACNP knows that when managing a patient with acute cardiogenic shock after myocardial infarction, all of the following pharmacologic agents may be used except: A.Opioids B. Diuretics C. Beta-adrenergic antagonists D.Anticholinergics Question 39 Mr. Baer is a 79-year-old man who is being admitted for a carotid endarterectomy. While performing his preoperative evaluation, the AGACNP appreciates two positive answers to the CAGE screening questionnaire. This is an indication for: A. Perioperative benzodiazepines for withdrawal syndrome B. Daily multivitamin and 100 mg of thiamine perioperatively C. Further diagnostic evaluation for alcoholism D.Delay of operation until completion of detoxification Question 40 According to the American College of Cardiology Foundation and the American Heart Association (ACCF/AHA), the recommendation regarding antiplatelet therapy in patients with cardiovascular disease preoperatively is that: A.Antiplatelet therapy should be held for 10 days preoperatively B. Cardiac consultation is required before an operation in patients who are on antiplatelet therapy C. Medications should be continued unless concerns about hemostasis are significant D.Antiplatelet therapy should be initiated in all high-risk cardiac procedures Question 41 Mr. Austin is a 64-year-old male who has a long history of mitral valve stenosis. His condition has developed to the extent that he has symptomatic congestive heart failure, and due to a variety of comorbidities he is not a candidate for surgery. Ongoing medical therapy for Mr. Austin should include: A.Anticoagulants B. Diuretics C. Antibiotics D.Inotropes Question 42 The progression of coronary artery plaque formation can lead to a variety of pathologic conditions. When subtotal plaque disruption occurs resulting in vasoconstriction, platelet activation, and embolization, it most commonly causes which clinical phenomenon? A.Endothelial cell dysfunction B. Prinzmetal’s angina C. Transmural myocardial infarction D.Non-ST elevation myocardial infarction Question 43 D. is a 29-year-old male who presents with a chief complaint of profound dizziness for the past 2 to 3 days. Further clarification reveals that he is having brief but intense episodes of a sense of the room spinning. He denies any history of head injury or discharge from the ear. The vertigo is reproduced easily with cervical rotation. The AGACNP knows that the most likely cause is: A.Cerebral tumor B. Ménière’s disease C. Adverse drug effect D.Benign paroxysmal positional vertigo (BPPV) Question 44 P.T. is a 61-year-old male who is seen in follow-up. He was initially seen for evaluation of dysphagia. An endoscopy was negative for malignancy and subsequent esophageal manometry supported a diagnosis of esophageal achalasia. While discussing implications and treatment options with P.T., the AGACNP tells him that the primary complication of achalasia is: A. Progressive esophageal discomfort B. Aspiration pneumonia C. Squamous cell carcinoma D.Long-term malabsorption problems Question 45 R. is a 51-year-old female who presents in shock following a penetrating injury to the spinal cord—her boyfriend reportedly stabbed her in the back with an unidentified kitchen utensil. The patient’s mental status is deteriorating, and her vital signs are as follows: temperature 97.2°F, heart rate 131 bpm, respirations 14 breaths per minute, and blood pressure 79/49 mm Hg. The AGACNP presumes neurogenic shock, with the injury likely: A.Not fully transecting the spinal cord B. At the level of T10 C. Precipitating sepsis D. Producing cardiovascular decompensation Question 46 Janet is a 34-year-old female with no significant medical history who is being evaluated for a planned uterine ablation. She has significant history of menorrhagia and has been unresponsive to a variety of medical therapies to try to stop the bleeding. Her history and physical examination are within normal limits. The AGACNP knows that Janet will require which one of the following preoperative diagnostic studies? A. Urinalysis B. Complete blood count C. 12-lead electrocardiogram D.Chest radiography Question 47 Best practices for assessing diseases of the thyroid gland include a thorough but targeted history, systematic physical examination, and selective use of appropriate diagnostic evaluation. The AGACNP knows that although serum T3 and T4 are not indicated routinely, a free T4 test is most useful in evaluating patients: A.With profound symptoms of hypothyroidism B. Following treatment for Graves’ disease C. To rule out autonomous toxic nodule D. At risk for thyroid cancer Question 48 Evaluation of cardiac valve disease must include: A.Chest radiography B. 12-lead ECG C. Echocardiography D.Chemical stress test Question 49 Jolene L. is a 36-year-old female who presents for an emergent cholecystectomy; she has had progressive acute pain for almost 1 week and now there is concern about gangrenous tissue. Of particular concern is the fact that she has Graves’ disease and has not been adherent to treatment. On admission, her temperature is 102.7°F, pulse is 158 bpm, and blood pressure is 180/114 mm Hg. She is tremulous and anxious. A 12-lead ECG reveals uncontrolled atrial fibrillation. Before cholecystectomy, Jolene must be treated with: A.Digitalis for heart rate control B. Radioactive ablation C. Beta-adrenergic antagonists D.Reserpine Question 50 W. is discussing his postoperative hip replacement expectations. He is advised that although he will have some discomfort, he should be vocal about asking for pain medication, because it is essential that he get out of bed and begin ambulating as soon as possible after his surgery. He expresses some fear and is concerned that his hip won’t heal properly if he walks on it. The AGACNP reassures him that he must begin ambulating quickly in order to decrease risk for: A.Decubitus ulcers B. Scar tissue formation C. Pneumonia D.Anxiety Question 51 H. is a 71-year-old male with small cell lung cancer; he has been treated with chemotherapy. Initially he had symptom improvement but now appears to have had a recurrence. On examination today, he is quite edematous and has gained 12 lbs since his office visit 1 week ago. A metabolic panel reveals a serum Na+ of 119 mEq/dL. The AGACNP knows that J. H. likely has: A.Brain metastasis B. Congestive heart failure (CHF) C. Syndrome of inappropriate antidiuretic hormone (SIADH) D.Metabolic alkalosis Question 52 According to the American College of Surgeons (ACS) and the National Surgical Quality Improvement Program (NSQIP) guidelines for preoperative evaluation of the geriatric patient, the preoperative evaluation should include all of the following except: A.Cognitive ability B. Functional status C. Competency assessment D. Frailty score Question 53 Improvements in both equipment and technique have led to the evolution of video-assisted thoracoscopic surgery (VATS) as being used most commonly for: A.Mediastinal lymph node dissection B. Resection of malignant tumor C. Metastasectomy D.Thoracic vertebral discectomy Question 54 Which of the following is a normal finding on postoperative day 8 of a carotid endarterectomy? A.A temperature of 100.5°F B. Serosanguinous drainage with some tenderness C. A flesh-colored induration along the entire length of the incision D.A fluctuant collection of milky fluid Question 55 Mrs. Evans is an 82-year-old female who is on postoperative day 3 following resection of a small bowel tumor. She is alert today and her nasogastric tube is removed. The AGACNP knows that if the recovery proceeds normally, Mrs. Evans may begin clear liquids: A.Immediately B. In 24 hours C. When bowel sounds return D.After a negative swallow study Question 56 When writing the initial postoperative progress note, the AGACNP should be sure to include all of the following except: A.A summary of the procedure and any significant deviations from normal B. An outline of the plan for postoperative management and follow-up C. The plan for ongoing monitoring D.Mechanism of DVT prophylaxis Question 57 T. is a 39-year-old male who presents to the hospital emergency room with a chief complaint of profound substernal chest pain. Results of the 12-lead ECG and cardiac enzymes test are normal. Vital signs are as follows: temperature 101.9°F, pulse 129 bpm, respirations 26 breaths per minute, and blood pressure 90/60 mm Hg. The patient is pale and clearly unwell, and physical examination reveals a systolic pericardial crunching sound. Which of the following additional pieces of history would make the AGACNP suspect acute mediastinitis? A.A 48 pack year smoke history B. A 2-day history of vomiting C. Aortic valve regurgitation D.Cardiac tamponade Question 58 Mrs. Van Doern is being examined on postop day 3 following surgical resection following a bowel obstruction. The postoperative course been unremarkable. Upon removal of the dressing, the incision is dry with staples intact. There is an approximately 0.5 cm erythema around the incision. There is no exudate. The patient demonstrates some discomfort on palpation of the site. The most appropriate approach to this patient includes: A.Leaving the wound open to air and medicating for pain B. Ordering a topical antibiotic, replacing the dressing with a nonadherent dressing, and following up in 2 days C. Beginning systemic antibiotics to cover skin flora D.Obtaining a white blood cell differential, redress the wound and reassess in the a.m. Question 59 K.T. is a 38-year-old female with a BMI of 39 kg/m2 who needs surgical reduction of a hiatal hernia. She is asking about the recovery process and says that she has read about something called the obesity paradox. She wants to know what that means with respect to her healing. The AGACNP explains that the paradox refers to the fact that: A. Obesity correlates with poor outcomes for some surgical procedures but not others. B. There is an inverse relationship between weight and surgical outcomes. C. Underweight patients have more surgical complications than obese patients. D. Planned weight loss preoperatively is indicated only when the BMI is > 40 kg/m2 . Question 60 Esophageal motility disorders are sometimes a consequence of systemic diseases such as scleroderma, Raynaud’s disease, and systemic lupus erythematosus. When patients with these diseases have gastroparesis, which medication should be added to the regimen? A. A proton pump inhibitor B. A histamine 2 receptor antagonist C. A calcium channel antagonist D. A promotility agent Question 61 S. is a 46-year-old female with metastatic breast cancer. She is currently off cycle for chemotherapy and generally is feeling well. Today, however, she presents feeling acutely unwell. She says that she has had coldlike symptoms over the last few days, including cough, nasal congestion, headache, and a hoarse voice in the mornings. Today she became acutely concerned because she feels as though her face and even shoulders look swollen and a bit discolored—bluish. She denies any nausea or vomiting but admits to feeling generally fatigued; she attribute it to her cancer. Recognizing the likely diagnosis, the AGACNP knows that treatment will likely include: A.Radiation B. Surgery C. Fibrinolytics D. Expansile stents Question 62 D. is a 61-year-old female patient who complaints of pleuritic chest pain and cough. During the history, she indicates that she occasionally has seen a little bit of blood in her sputum, but she thought it was from coughing so hard. What finally prompted her to come in was that she coughed up a “stone.” Recognizing that the patient might have broncholithiasis, the AGACNP asks about exposure to: A.Cigarettes B. Asbestos C. Bird excrement D. Swimming pools Question 63 Heart transplant is the surgical option for patients with congestive heart failure for whom medical therapies have failed. All of the following are contraindications to transplant except: A.New York Heart Association (NYHA) class IV status B. Obesity C. Elevated pulmonary vascular resistance D.Recent malignancy Question 64 Kelly T. is a 49-year-old female who is being admitted for aortic valve replacement. Her preoperative evaluation revealed an ascending thoracic aneurysm of 4.8 cm in diameter. Kelly has not had any aneurysm symptoms and is generally considered a very strong surgical candidate. The AGACNP knows that the standard of care dictates: A. Postponing her valve surgery due to the aneurysm B. Annual imaging of the aneurysm after her valve replacement C. Surgical repair of the aneurysm at the same time as valve replacement D. Surgical repair of the aneurysm after successful recovery from valve replacement Question 65 K. is a 39-year-old female who was admitted for evaluation of progressive activity intolerance, and chest radiography revealed a large right lower lobe pleural effusion. A pleural fluid tap was performed, but fluid analysis results were inconclusive and the cause of the effusion could not be identified. The AGACNP knows that which diagnostic study is most appropriate to identify the cause of pleural effusion when fluid analysis is inadequate? A. Scalene biopsy B. Video-assisted thoracoscopic surgery (VATS) C. Pleural needle biopsy D.Open surgical biopsy Question 66 While on call, the AGACNP is asked to evaluate a deteriorating patient. The patient was admitted for exacerbation of pneumonia and congestive heart failure (CHF). The systolic blood pressure is < 90 mm Hg, and the urine output is < 10 mL/hr. A 12-lead ECG reveals no acute processes but reveals previously noted changes that are consistent with bilateral atrial and ventricular enlargement and a marked left axis deviation. You insert a pulmonary artery (PA) line and anticipate which of the following pressures? (CI, cardiac index; PAOP, pulmonary artery occlusion pressure ; RAP, right atrial pressure) A.CI 1.3 L/min, PAOP 27 mm Hg, RAP 18 mm Hg B. CI 1.9 L/min, PAOP 12 mm Hg, RAP 6 mm Hg C. CI 2.4 L/min, PAOP 18 mm Hg, RAP 8 mm Hg D.CI 1.4 L/min, PAOP 7 mm Hg, RAP 4 mm Hg Question 67 A critically ill patient with multiple traumatic injuries sustained during a motor vehicle accident has had a pulmonary artery line inserted to follow cardiac pressures. Which of the following sets of pressures would be consistent with hypovolemic shock? (CI, cardiac index; CVP, central venous pressure; PCWP, pulmonary capillary wedge pressure) A.CI 1.3 L/min, PCWP 27 mm Hg, CVP 18 mm Hg B. CI 1.3 L/min, PCWP 6 mm Hg, CVP 4 mm Hg C. CI 2.3 L/min, PCWP 12 mm Hg, CVP 8 mm Hg D.CI 2.9 L/min, PCWP 16 mm Hg, CVP 6 mm Hg Question 68 Aggressive fluid resuscitation is indicated in all of the following shock states except: A.Hypovolemic B. Cardiogenic C. Obstructive D.Distributive Question 69 The risk-benefit ratio always is considered when evaluating patients with mitral valve disease as surgical candidates for valve correction. Who among the following patients is not considered a good operative candidate? A. A patient with severe mitral regurgitation and endocarditis with systemic embolization B. A patient with severe mitral regurgitation and left ventricular dysfunction C. A patient with severe mitral regurgitation and normal ventricular function D. A patient with severe mitral regurgitation and pulmonary hypertension Question 70 T. is a 29-year-old male who is recovering from an open fixation of a femur fracture sustained in a diving accident. He has an order for Dilaudid 1 mg IV q2h p.r.n. for pain. He is still having pain and requests more medication. The AGACNP considers that: A.This is the maximum dose for Dilaudid and nonpharmacologic measures should be maximized B. The dose may be increased to 2 mg and response assessed C. He may be opiate addicted, and this should be explored before the dose is increased D.An adjunct medication such as ibuprofen should be added to his regimen Question 71 Mrs. Saraceno is a 71-year-old female who had an episode of acute pulmonary edema following an endovascular aneurysm repair. She was managed successfully with a loop diuretic and is ultimately discharged on furosemide 60 mg daily and instructed to follow up with cardiology. She is seen in the office postoperatively 2 weeks after discharge. She has not yet seen a cardiologist but has continued all discharge medications. Her metabolic panel is as follows: Na+ 126 mEq/L K+ 4.0 mEq/L Cl- 93 mEq/L CO2 28 mEq/L BUN 40 mg/dL Cr 1.3 mg/dL The AGACNP recognizes that the patient likely has which abnormality as a consequence of diuretic overuse? A.Hyponatremia B. Hypokalemia C. Metabolic acidosis D.Intrarenal failure Question 72 Mrs. Hoffman is an 82-year-old female who is on postoperative day 4 following mastectomy for breast cancer. This morning her vital signs include a temperature of 101.2°F, pulse of 110 bpm, respiratory rate of 20 breaths per minute, and blood pressure of 100/70 mm Hg. The incisions look good and there is no physical finding or symptom of incision infection. The only abnormal physical finding is a significant tender edema on the right cheek and neck. In addition to ordering increased intravenous hydration and parenteral antibiotics to target Staphylococcus aureus, the AGACNP orders: A. Loop diuretics B. Chewing gum C. Ambulation D.Incentive spirometry Question 73 Kelly is a 50-year-old female who had chest radiography as part of a preoperative history and physical examination before an elective cosmetic procedure. [Show More]
Last updated: 2 years ago
Preview 1 out of 26 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 16, 2021
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Jun 16, 2021
Downloads
0
Views
78



.png)












.png)
.png)