ASSESSING THE ABDOMEN /GASTROINTESTINAL SYSTEM
Assessing the Abdomen/Gastrointestinal System CC–
Adv. Health Assessment & Diagnostic Reasoning Jessica Toney
Walden University September 24. 2018
...
ASSESSING THE ABDOMEN /GASTROINTESTINAL SYSTEM
Assessing the Abdomen/Gastrointestinal System CC–
Adv. Health Assessment & Diagnostic Reasoning Jessica Toney
Walden University September 24. 2018
Assessing the Abdomen/Gastrointestinal System
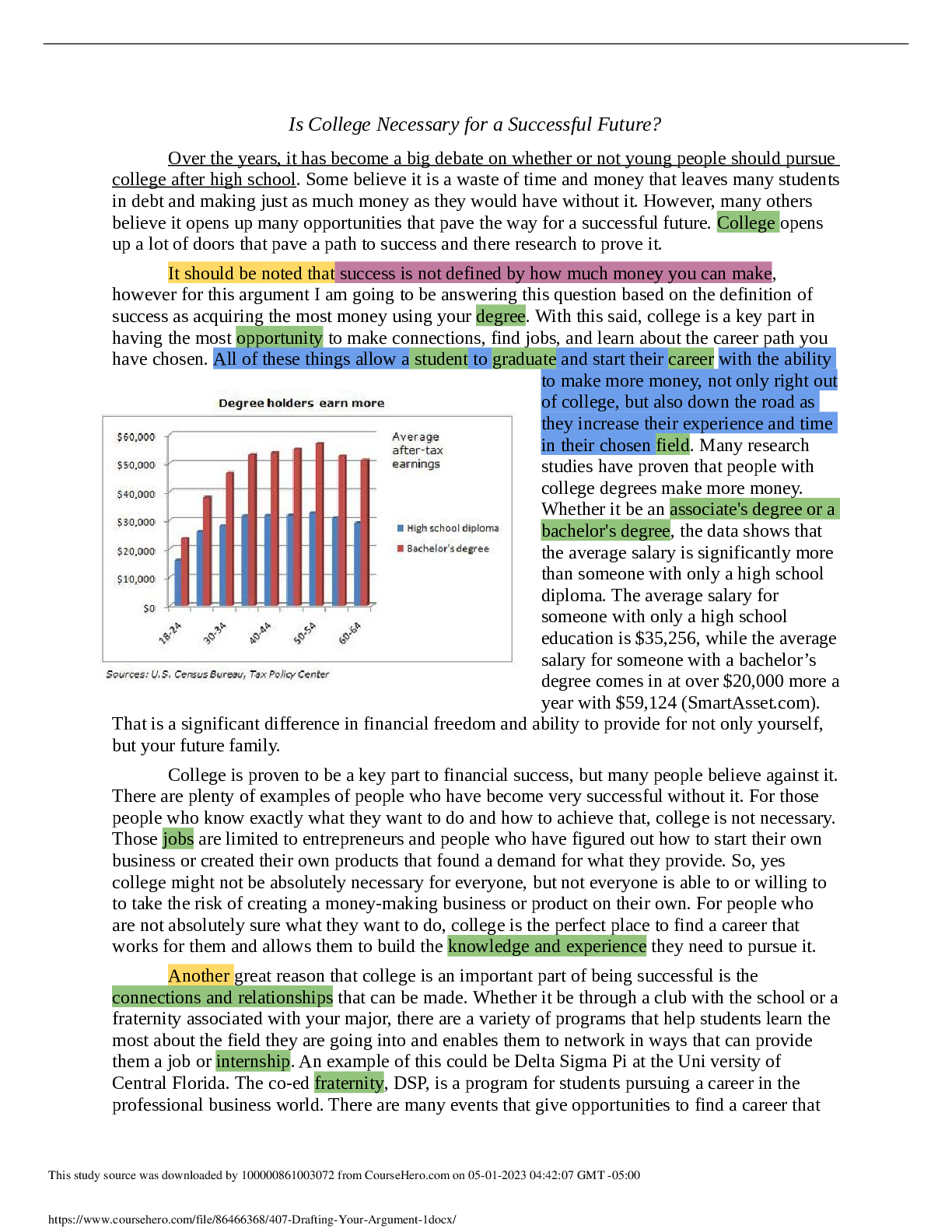
Surveying the abdomen area and influencing an authoritative analysis from subjective and objective data can be trying for the medical professional. It is vital to investigate the accumulated clinical data and bolster the right finding with current evidenced-based practice. In this paper. I will examine a SOAP note contextual investigation of a male who presents with generalized abdominal pain and other side effects. This paper will analyze the subjective and the objective information introduced and propose extra data that ought to be incorporated into this segment of the SOAP note. as confirmed by references to current academic writing. What's more. current confirmation from the literature will be introduced. analytic tests that would be indispensable to evaluate as basic information from the patient will be recorded with references to either bolster or negate this appraisal. As medical professionals. analytic tests must be bolstered with clinical avocation about why it is relevant to the right finding. In rundown. five conceivable differential determinations will be talked about and data assembled will either support or reject every analysis.
Subjective Data Analysis
I will analyze the subjective data of this case study. The data presented is as follows; CC; “My stomach hurts. I have diarrhea. and nothing seems to help.”
HPI; JR. 47-year-old white male. complains of having generalized abdominal pain that started 3 days ago. He has not taken any medications because he did not know what to take. He states the pain is a 5/10 today but has been as much as 9/10 when it first started. He has been able to eat. with some nausea afterwards.
PMH; HTN. Diabetes. hx of gastrointestinal bleed 4 years ago
Medications; Lisinopril 10mg. Amlodipine 5 mg. Metformin 1000mg. Lantus 10 units qhs
Allergies; NKDA
FMH; No history of colon cancer. father hx DM2. HTN. mother hx HTN. Hyperlipidemia. GERD
Social History; Denies tobacco use; occasional alcohol use. married. 3 children (1 girl. 2 boys)
The subjective information picked up from the patient amid this experience isn't as thorough as it ought to be upon the initial experience with the patient. Thorough subjective information is fundamental to determine the right diagnosis (Raleigh. and Allan. 2017). Having a thorough patient and family history is required with a specific end goal to survey and pick the right diagnostics (Epocrates Patient Resources. 2018).
The patient’s history of present illness was obscure and expected to incorporate more data. for example. the PQRST (provocation/palliation. quality. quantity. location. radiation and timing) technique for describing the pain (Young. 2017). Clinicians should look to recognize the dull. ineffectively limited. aching pain created by instinctively innervated organs. contrasted to the distinctively "sharp". The individual has generalized pain. yet I have no idea of what hastened it. The main component is that there is post-prandial queasiness in the wake of eating. Moreover. there is no portrayal of the intensity. for example. pulverizing. throbbing. sickening or shooting pain other than the scale used. In the initial complaint. the patient expresses that "his stomach hurts" yet it is critical to ask the patient which territory in his belly did it begin. This would help in deciding whether there are conceivably any organs in a specific quadrant of the belly included.
In addition. it is essential to incorporate into the history of present illness about any emesis that the patient had and also data about his last solid bowel movement or has there been any visible blood in the stool. Knowing in detail the shading and amount would moreover assist in deciding whether there is any bleeding of the gastrointestinal tract. Obtaining some information about what he ate and when he last ate would be noteworthy. It would likewise be fundamental to incorporate a 24-hour review of what he ate to decide whether anything was strange or if there are present sustenance that are aggravating to his gastrointestinal tract. Lastly. including the subjective evaluation of whether he had been out of the nation would discount any protozoal contaminations that could be suspected (Epocrates Patient Resources. 2018).
Alongside examine and investigating the history of present illness. is the patients past medical history. It was stated that he had a bleed four years back. however no other data is examined. I might want to know whether he was hospitalized. on the off chance that it was an upper or lower gastrointestinal bleed. if any surgical intercession was essential. and if any testing. for example. colonoscopy or GI series was performed. "The precise conclusion of GI bleeding depends on quick revival. risk assessment. and clinical analysis taken after by suitable authoritative examination which empowers particular mediation" (Kim. 2014).
Objective Data Analysis
I will analyze the objective data of this case study. The data presented is as follows;
Vital Signs; Temp 99.8; BP 160/86; RR 16; P 92; HT 5’10”; WT 248lbs
Cardiovascular; RRR. no murmurs Respiratory; CTA. chest wall symmetrical
Integumentary; Intact without lesions. no urticaria Abdomen; soft. hyperactive bowel sounds. pain in the LLQ
Diagnostics; None performed
The objective information introduced necessities to incorporate more basic audit of systems relevant to the subjective information. At first. there ought to be a general picture that expresses the patient is alert and oriented to person. place and time and if there is any present discomfort level. Neurological status would be critical to incorporate to decide whether the patient has any migraines. unsteadiness or changes in mentation. What's more. there ought to be a concise review of the patient’s head. eye. ears. nose. and throat. The objective information of patient's vital signs is critical to preclude potential shock and give a short clinical picture of patient status. The patient has a temp although low-grade and his blood pressure is hoisted in all likelihood because of discomfort or potential resistance with blood pressure regimen. Next. the integumentary assessment ought to have included skin turgor. capillary refill and condition of mucous membranes and eyes because of the risk that he may be dehydrated.
The abdominal assessment ought to have incorporated the investigation. auscultation. palpation and percussion each of the four quadrants. The complaints of discomfort in the left lower quadrant ought to have included whether there were any indications of organomegaly upon palpation. Palpation is a basic piece of target information to decide zones of delicacy and surveying organs for any irregularity (Lew. 2018). It additionally would have been vital to state whether the stomach area was flat or rounded. Furthermore. while surveying the abdomen. it is crucial to incorporate any regions of discoloration observed. Because of the patient’s size. distention of the stomach area could be standard. Be that as it may. distention could likewise infer gas. fluid. or ascites being present. A generalized distention can likewise be identified with ascites. especially when related with an everted umbilicus (Macaluso and McNamara .2012).
Adding percussion to the objective information will permit the separation between large bowel
hindrance (drum-like tympany) and ascites (moving dullness). Auscultation is of extremely constrained symptomatic utility. and prolonged auscultation for bowel sounds is an ineffectual utilization of time. in spite of the fact that it might uncover shrill sounds in early small bowel issues or the quietness experienced with ileus or any abdominal fiasco. (Macaluso and McNamara. 2012).
Assessment Support/Refute
The assessment information is left lower quadrant discomfort and gastroenteritis. I bolster the evaluation as the objective information being left lower quadrant torment from physical examination and the differential conclusion of gastroenteritis. Hyperactive bowel sounds are usually seen with gastroenteritis. Be that as it may. I discredit this assessment as essential parts in this evaluation segment inside a SOAP note are absent. This area ought to have included lab tests. results. diagnostics. differential determination. current co-morbidities. and plan to touch base at an exact analysis (Lew. 2018). Posting a few differential analyses would be indispensable from greatest to least improbable and where decisions are discussed more thoroughly. The assessment information isn't clear and expected to incorporate these means as this is the area that accumulates union of subjective and objective proof to land at the conclusion (Lew. 2018).
Diagnostic Evaluation
An early and exact diagnosis results in more precise management and. in this way. prompts better results (Gans. Pols. Stoker. & Boermeester. 2015). When diagnosing abdominal pain. the components of history. physical examination. radiography and lab results are indispensable. The patient’s history suggests that he is in danger for another gastrointestinal bleed so further diagnostics would be essential. In any case. the analytic tests that are basic to
consider for this situation would be a CBC (complete blood count). BMP (basic metabolic panel). stool culture. x-ray and CT exam.
The principal symptomatic test would be a CBC. Since the patient has a past filled with a GI bleed. this could preclude the reoccurrence of a bleed and give a suitable benchmark to the patient. Moreover. it would likewise demonstrate whether the patient has leukocytosis which would be confirmed for bacterial and viral etiology.
Next would be a BMP. This would give an exact picture into the electrolyte status of the patient. Because of the patient being diabetic. renal capacity is important as his creatinine. blood urea nitrogen and glucose level could be directly affected with dehydration. This test is important to execute as the patient has had tenacious loose bowels and is at high risk for direct to serious liquid exhaustion. Hypernatremia would be seen and also hypokalemia because of looseness of the bowels (Epocrates Patient Resources. 2018).
Third. a few stool tests and cultures would be material to this patient’s diagnostics. Testing for mysterious blood in the stool would decide the appearance or nonappearance of potential GI bleeding. Fast antigen testing would test for stool latex agglutination or chemical immunoassay for infections. Also. performing a stool reverse transcriptase PCR (RT-PCR) or multiplex PCR can distinguish rotavirus. norovirus. astrovirus or adenovirus. Affirmation of gastroenteritis in spite of the fact that not ordinarily utilized can be analyzed by polymerase chain response (PCR). antigen-recognizing compound immunoassays (EIAs). immunofluorescence examines (IFAs). microscopy. serology. and viral culture. Lastly. completing a stool culture for ova and parasites would decide bacterial or parasitic etiology.
Next. would be abdominal radiographs. be that as it may but there is no place for ordinary radiography in the work-up of patients with abdominal pain because of the absence of added
value on top of clinical evaluation (Gans. Pols. Stoker. & Boermeester. 2015). The patient had complaints of generalized pain that was appeared to be limited amid the objective information to left lower quadrant there may or may not be an incentive in obtaining an abdominal x-ray.
Lastly. Computed tomography (CT) prompts the most astounding affectability and specificity in patients with acute abdominal pain. Positive prescient value of ultrasound is equivalent with CT and subsequently favored as the primary imaging methodology because of the drawbacks of computed tomography; negative or uncertain ultrasound is trailed by CT (Gans. Pols. Stoker. & Boermeester. 2015).
Differential Diagnosis
1. Viral Gastroenteritis
Evidence Accepting;
Viral gastroenteritis is a disease of your digestive organs that commonly causes watery looseness of the bowels. pain or cramping in your abdomen. queasiness or vomiting. and now and then fever (National Institute of Diabetes and Digestive and Kidney Diseases. 2018). Viral gastroenteritis incorporates at least three watery stools inside 24 hours with indications enduring under 7 days and incorporates just one of the accompanying; fever. queasiness. vomiting. pain in the abdomen. spasms. loose stools. and blood or mucous in stools (Lausch et al. 2017).
The information underpins the conclusion of viral gastroenteritis as the patient had stomach pain. fever. loose stools and queasiness. His discomfort decreased recently in the past couple of days and as expressed above side effects for the most part is under 7 days.
Symptomatic tests depend on clinical introduction. Notwithstanding. since the patient exhibits the side effect of loose stools. there ought to be blood tests done to guarantee electrolyte status is ideal and that there isn't broad volume loss. A CBC and BMP would be fitting as well.
2. Bacterial Gastroenteritis Evidence Rejecting;
Clinical introduction of bacterial gastroenteritis incorporates the accompanying; high ever. bloody stools. or serious loose stools. Vomiting with high fever. discomfort. anorexia. looseness of the bowels enduring longer than 14 days and extreme industrious stomach pain are the present trademark side effects of bacterial gastroenteritis. This way this differential determination is rejected. In the event that bacterial gastroenteritis was suspected. microscopy and culture would indicate proof of fecal leukocytes and positive lactoferrin immunoassay.
Culture would indicate there is campylobacter jejuni. salmonella species and conceivable enteropathogenic Escherichia coli present. The patient does not have any of these manifestations or demonstrative tests pending which disproves this determination.
3. Gastritis
Evidence Rejecting;
Gastritis is a typical bacterial contamination and can be caused by various things.
Clostridium welchii is ordinarily observed in destructive agents. for example. alcohol. In the patient’s social history. it states he has periodic ETOH use. Be that as it may. unreasonable alcohol utilization is related with gastritis. Alcohol causes destruction of sulfhydryl mixes in gastric mucosa. Helicobacter pylori contamination is related with abuse of antiinflammatory medications and ETOH. In the patients subjective and objective information there is no proof supporting that the patient is a drunkard or is utilizing NSAIDS. There is no family history of gastritis or H pylori disease. Side effects of gastritis incorporate iron deficiency. early satiety. unexplained weight reduction. dynamic dysphagia and continuous vomiting. Testing for gastritis incorporates fecal antigen testing to recognize H pylori antigen and this has a > 90% affectability
(Cherdantseva. et al. 2014). Moreover. a CBC would be justified which would indicate lessened hemoglobin. hematocrit and leukocytosis with left shift.
4. Diverticulitis
Evidence Rejecting;
Diverticulitis presents with fever. leukocytosis. left lower quadrant discomfort. bleeding from the rectum. obstruction and pelvic delicacy on advanced rectal exam. This patient has a lowgrade fever yet no appearance of leukocytosis or obstruction in the evaluation. A few analytic tests are requested quickly including a CB and xray on assumption of diverticulitis. A CBC would demonstrate polymorphonuclear leukocytosis. CBC results ought to be considered at first experience with understanding when diverticulitis is suspected. Next would be the xray which would demonstrate pneumoperitoneum. ileus. delicate tissue densities and free air in inside aperture. No analytic tests appeared on the objective appraisal and the subjective
information examined above does not infer this is diverticulitis.
5. Colorectal Cancer
Evidence Rejecting;
Colorectal disease appears when there is a family history. In the present contextual analysis there is no family history of colorectal tumor which would prompt dismissing this finding. Side effects of colon growth incorporate adjusted entrails propensities. iron deficiency. colonic polyps and positive family history. On the off chance that clinical side effects were available separating tests. for example. CBC and including a computed tomography would be proper which indicates highlights of carcinoma. stricture and hindrance (Epocrates Patient Resources. 2018). There is no confirmation proposing from objective and subjective information backing this differential analysis.
6. Bowel Obstruction of the large intestine Evidence Rejecting;
Upon physical appraisal of a patient with an obstruction area there would be be distention and rigidity. Bowel sounds are hypoactive or missing. Agony is steady and increments with coughing. profound breathing and movement. Likewise. there is no proof that the patient is in respiratory trouble as proven by the respiratory rate of 16 and the target information of lungs clear to auscultation and symmetry of chest. "Recognition of a gastric outlet or extensive intestine hindrance in a patient who is generally sound or with an earlier growth history should raise the doubt of an undiscovered hidden or repetitive disease" (Mills. and Chen. 2011). The patient for this situation examined has hyperactive abdominal sounds. a delicate belly and there is no subjective information expressing that there is enhanced discomfort with motion.
Trademark indications of hinderance include colicky discomfort an inability to pass flatus or excrement in 1224 hours (Epocrates Patient Resources. 2018).
Tests to request would be a CBC. renal capacity. serum amylase/lipase. coagulation examine and erect xray. CBC would demonstrate leukocytosis and conceivable iron deficiency related with potential aperture. Renal capacity is required for potential increased blood urea nitrogen or creatinine that would demonstrate kidney disappointment and dehydration. Serum amylase and lipase is quite often raised with any abdominal issue. Coagulation studies would be available in sepsis from aperture from an extensive obstruction. Lastly. erect x ray would demonstrate sign of rupture of the bowel (Epocrates Patient Resources. 2018).
Conclusion
Taking everything into account. the above data gave broad clinical research and upheld the determination of gastroenteritis. Clear proposals for development in the subjective and objective information and evaluation were made and bolstered with references. Proper assessment information was incorporated with the determination of gastroenteritis and analytic tests that were material to help the appraisal alongside objective and subjective information. Differential findings were talked about alongside demonstrative testing and thinking. As future diagnosticians. it is fundamental to utilize contextual analyses as an apparatus to help rule out malady processes to determine the legitimate treatment of patients.
References
Cherdantseva. L. A.. Potapova. O. V.. Sharkova. T. V.. Belyaeva. Y. Y.. & Shkurupiy. V. A. (2014). Association of Helicobacter pylori and iNOS production by macrophages and lymphocytes in the gastric mucosa in chronic gastritis. Journal of Immunology Research. 1(4). Retrieved from http;//dx.doi.org/10.1155/2014/762514
Epocrates Patient Resources. (2018). Retrieved from https;//online.epocrates.com/diseases/20234/Viralgastroenteritisinadults/Diagnostic Tests
Gans. S. L.. Pols. M. A.. Stoker. J.. Boermeester. M. A. (2015). Guideline for the Diagnostic Pathway in Patients with Acute Abdominal Pain. Digestive Surgery. 32(1);2331
Kim. B. S. M.. Li. B. T.. Engel. A.. Samra. J. S.. Clarke. S.. Norton. I. D.. & Li. A. E. (2014).
Diagnosis of gastrointestinal bleeding; A practical guide for clinicians. World Journal of Gastrointestinal Pathophysiology. 5(4). 467–478. http;//doi.org/10.4291/wjgp.v5.i4.467
Lausch. K. R.. Westh. L.. Kristensen. L. H.. Lindberg. J.. Tarp. B.. & Larsen. C. S. (2017). Rotavirus is frequent among adults hospitalized for acute gastroenteritis. Dan Med J. 64(1). A5312.
Lew. V. (2018). SOAP Notes. Retrieved from https;//www.ncbi.nlm.nih.gov/books/NBK482263/ Macaluso. C. R.. & McNamara. R. M. (2012). Evaluation and management of acute abdominal
pain in the emergency department. International Journal of General Medicine. 5. 789– 797. http;//doi.org/10.2147/IJGM.S25936
Mills. A. M.. & Chen. E. H. (2011). Abdominal pain in special populations. Emergency Medicine Reports. 32(7). 81–91.
National Institute of Diabetes and Digestive and Kidney Diseases. (2018). Definition & Facts for Viral Gastroenteritis. Retrieved from https;//www.niddk.nih.gov/health information/digestivediseases/viralgastroenteritis/definitionfacts
Raleigh. M.. & Allan. H. (2017). A qualitative study of advanced nurse practitioners' use of physical assessment skills in the community; shifting skills across professional boundaries. Journal of Clinical Nursing. 26(1314). 20252035.
Young. K. D. (2017). Assessment of Acute Pain in Children. Clinical Pediatric Emergency Medicine. 18(4). 235241.
[Show More]