*NURSING > SHADOW HEALTH > Shadow Health All Modules Cases Instructor Keys TINA JONES (All)
Shadow Health All Modules Cases Instructor Keys TINA JONES
Document Content and Description Below
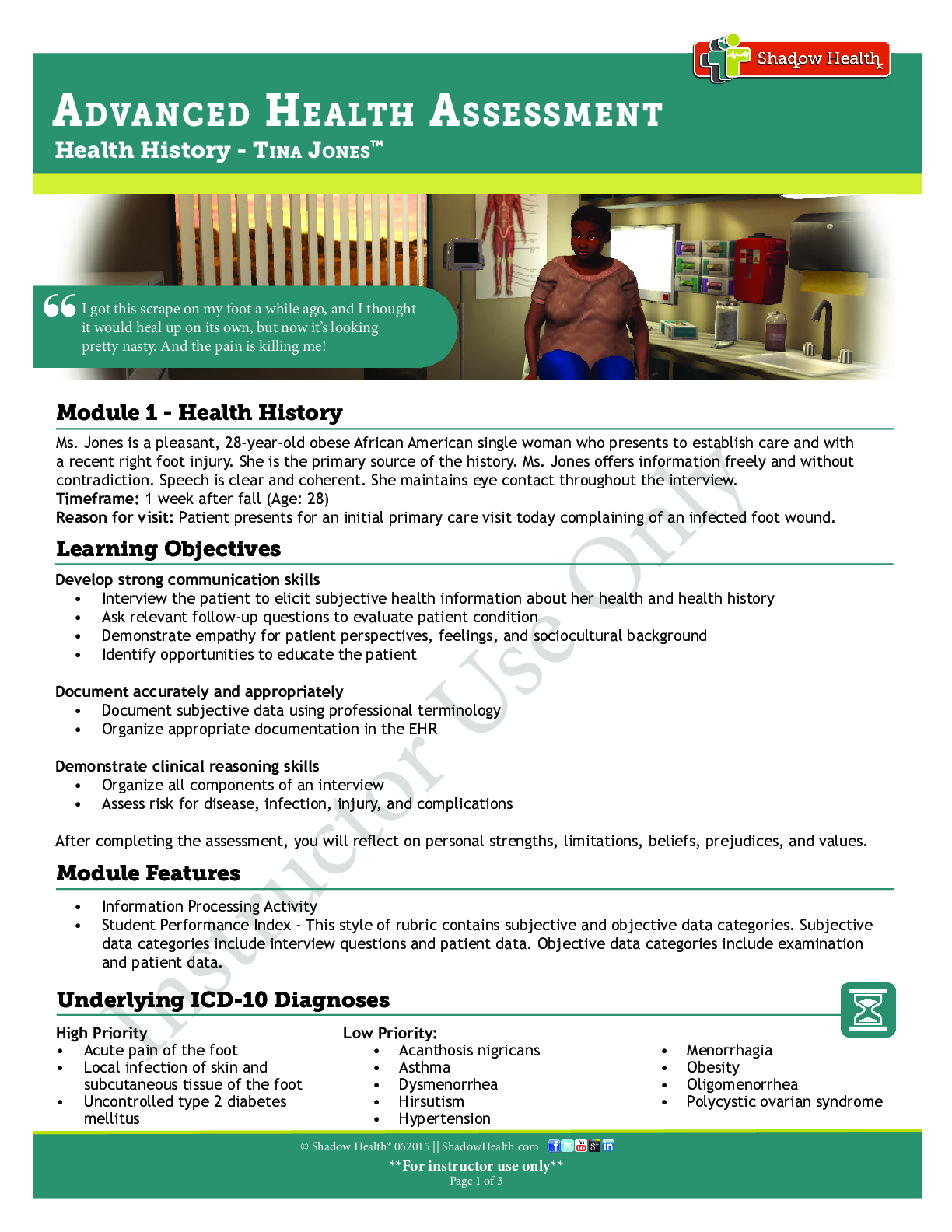
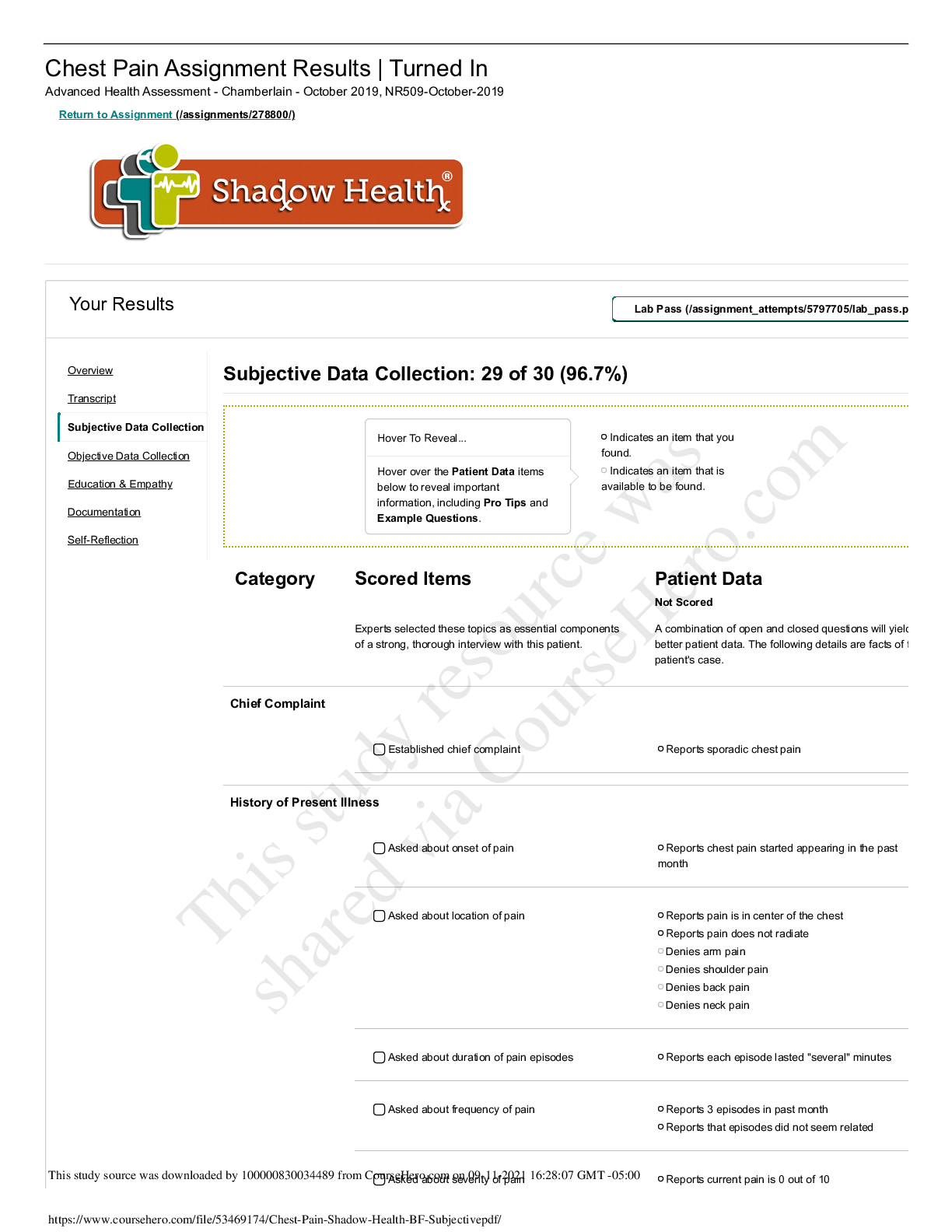
ADVANCED HEALTH ASSESSMENT Health History - TINA JONES™ © Shadow Health® 062015 || ShadowHealth.com **For instructor use only** Page 1 of 3 Instructor Use Only Ms. Jones is a pleasant, 28 -y... ear- old obese African American single woman who presents to establish care and with a recent right foot injury. She is the primary source of the history. Ms. Jones off ers information freely and without contradiction. Speech is clear and coherent. She maintains eye contact throughout the interview. Timeframe: 1 week after fall (Age: 28) Reason for visit: Patient presents for an initial primary care visit today complaining of an infected foot wound. Module 1 - Health History Develop strong communication skills • Interview the patient to elicit subjective health information about her health and health history • Ask relevant follow-up questions to evaluate patient condition • Demonstrate empathy for patient perspectives, feelings, and sociocultural background • Identify opportunities to educate the patient Document accurately and appropriately • Document subjective data using professional terminology • Organize appropriate documentation in the EHR Demonstrate clinical reasoning skills • Organize all components of an interview • Assess risk for disease, infection, injury, and complications After completing the assessment, you will refl ect on personal strengths, limitations, beliefs, prejudices, and values. Learning Objectives High Priority • Acute pain of the foot • Local infection of skin and subcutaneous tissue of the foot • Uncontrolled type 2 diabetes mellitus Low Priority: • Acanthosis nigricans • Asthma • Dysmenorrhea • Hirsutism • Hypertension • Menorrhagia • Obesity • Oligomenorrhea • Polycystic ovarian syndrome Underlying ICD- 10 Diagnoses • Information Processing Activity • Student Performance Index - This style of rubric contains subjective and objective data categories. Subjective data categories include interview questions and patient data. Objective data categories include examination and patient data. Module Features I got this scrape on my foot a while ago, and I thought it would heal up on its own, but now it’s looking “ pretty nasty. And the pain is killing me!ADVANCED HEALTH ASSESSMENT Health History - TINA JONES™ © Shadow Health® 062015 || ShadowHealth.com **For instructor use only** Page 1 of 3 Instructor Use Only One week after sustaining the cut, Tina Jones develops an infection in the cut on the bottom of her foot; she seeks treatment when the infection starts to swell and produce pus. Day 1 (Onset): Tina was at home, going down the back steps, and she tripped. She turned her ankle and scraped the bottom of her foot. The wound bled, but she stopped the bleeding quickly and cleaned the wound. She worried that she had sprained her ankle, and her mom drove her to the ER. (“a week ago”) The ER did an x ray (no broken bones), gave her a prescription for Tramadol, and sent her home. In the following days, her ankle seemed fi ne not as serious as she thought. Day 2 - 4: She cleaned the wound dutifully, twice a day, with soap and water or hydrogen peroxide, let it dry, put Neosporin on it, and bandaged it. The wound wasn’t getting worse, but it wasn’t healing, either. She expresses that she “took really good care of it.” Tina was able to go to work and attend school. Day 4: Tina went to her cousin’s house, where she encountered cats and experienced wheezing. She tried two puff s on her albuterol inhaler, and she had to do a third puff . (“three days ago”) Day 5 - 6: Tina noticed pus in the wound, and swelling, redness and a warm feeling in her foot. Her pain increased to the point she was unable to walk. She began to take the Tramadol to try to manage the pain, but it didn’t resolve the pain completely. She missed class and work. (“two days ago”) On the night of Day 6: Tina started to run a fever. They took her temperature at home, and it was 102. (“last night”) Morning of Day 7: Tina fi nally recognizes that her foot infection is not going to get better, and her mom takes her to the nurse practitioner to get the foot looked at. History of Present Illness Medications 1. Acetaminophen 500- 1000 mg PO prn (headaches) 2. Ibuprofen 600 mg PO TID prn (menstrual cramps) 3. Tramadol 50 mg PO BID prn (foot pain) 4. Albuterol 90 mcg/spray MDI 2 puff s Q4H prn (last use: “a few months ago”) Vitals • Weight (kg) - 88 • BMI - 30.5 • Heart Rate (HR) - 82 • Respiratory Rate (RR) - 16 • Pulse Oximetry - 99% • Blood Pressure (BP) - 139/87 • Blood Glucose - 117 • Temperature (F) - 98.9 • Penicillin: rash • Denies food and latex allergies • Allergic to cats and dust. When she is exposed to allergens she states that she has runny nose, itchy and swollen eyes, and increased asthma symptoms. Allergies Printable “Answer Key” available within the Shadow Health DCE. Subjective and Objective Model Documentation • Symptoms - Foot pain and discharge • Diagnosis - Infected foot wound Chief ComplaintADVANCED HEALTH ASSESSMENT Health History - TINA JONES™ © Shadow Health® 062015 || ShadowHealth.com **For instructor use only** Page 1 of 3 Instructor Use Only Abnormal Findings Reported during Chief Complaint interview • Reports open foot wound and throbbing pain • Rates present pain at a 7 out of 10 • Discharge, redness, swelling, and warmth around foot wound • Reports a fever last night and presents with a fever of 101.1 F • Pain aff ects ability to walk, job performance, and class attendance Reported during Past Medical History interview • Diagnosed with asthma in childhood and uses an inhaler 2 to 3 times per week • Allergic to penicillin, dust and cats, which cause wheezing • Diagnosed with Type 2 diabetes • Does not currently take medication for diabetes and does not monitor blood glucose • Heavy menstrual fl ow, heavy cramping, and irregular periods • Occasional headaches and eye strain • Increased thirst and more frequent urination • Recent 10lb unintentional weight loss • Habitual diet soda drinking Assessment Right foot wound with evidence of infection Plan 1. Clean wound with normal saline and redress with clean gauze. 2. Educate patient on when to seek emergent care, signs and symptoms of infection, and daily wound care. 3. Return to clinic one week to re-evaluate wound and assess need for antibiotics.© Shadow Health® 072015 || ShadowHealth.com **For instructor use only** Page 1 of 3 HEENT - TINA JONES™ ADVANCED HEALTH ASSESSMENT Instructor Use Only For the last week, Tina has experienced sore, itchy throat, itchy eyes, and runny nose. She states that these symptoms started spontaneously and have been constant in nature. She has treated her throat pain with occasional throat lozenges which has “helped a little”. She states that her nose “runs all day” and has clear discharge. She denies cough and recent illness. She denies fevers, chills, and night sweats. Timeframe: 1 month after establishing primary care (Age: 28) Reason for visit: Patient presents complaining of nose and throat symptoms. Module 2 - HEENT Develop strong communication skills • Interview the patient to elicit subjective health information about her health and health history • Ask relevant follow-up questions to evaluate patient condition • Demonstrate empathy for patient perspectives, feelings, and sociocultural background • Identify opportunities to educate the patient Document accurately and appropriately • Document subjective data using professional terminology • Organize appropriate documentation in the EHR Demonstrate clinical reasoning skills • Organize all components of an interview • Assess risk for disease, infection, injury, and complications After completing the assessment, you will refl ect on personal strengths, limitations, beliefs, prejudices, and values. Learning Objectives “My throat has been sore and itchy for a week now, and my nose won’t stop running. It’s not getting “ worse, but it’s not going away either. J30.1, Allergic rhinitis due to pollen Underlying ICD- 10 Diagnoses • Student Performance Index - This style of rubric contains subjective and objective data categories. Subjective data categories include interview questions and patient data. Objective data categories include examination and patient data. Module Features© Shadow Health® 072015 || ShadowHealth.com **For instructor use only** Page 1 of 3 HEENT - TINA JONES™ ADVANCED HEALTH ASSESSMENT Instructor Use Only Ms. Jones is a pleasant 28-year-old African American woman who presented to the clinic with complaints of sore, itchy throat, itchy eyes, and runny nose for the last week. She states that these symptoms started spontaneously and have been constant in nature. She does not note any specifi c aggravating symptoms, but states that her throat pain seems to be worse in the morning. She rates her throat pain as 4/10. She has treated her throat pain with occasional throat lozenges which has “helped a little”. She states that she has some soreness when swallowing, but otherwise no other associated symptoms. She states that her nose “runs all day” and is clear discharge. She has not attempted any treatment for her nasal symptoms. She states that her eyes are constantly itchy and she has not attempted any eye specifi c treatment. She denies cough and recent illness. She has had no exposures to sick individuals. She denies changes in her hearing, vision, and taste. She denies fevers, chills, and night sweats. She has never been diagnosed with seasonal allergies, but does note that her sister has “hay fever”. History of Present Illness Medications 1. Albuterol 90 mcg/spray MDI 2 puff s Q4H prn (Wheezing: “when around cats,” last use in the past week) 2. Acetaminophen 5001000 mg PO prn (headaches 3. Ibuprofen 600 mg PO TID prn (cramps) Vitals • Weight (kg) - 89 • BMI - 30.8 • Heart Rate (HR) - 80 • Respiratory Rate (RR) - 16 • Pulse Oximetry - 99% • Blood Pressure (BP) - 141/82 • Blood Glucose - 199 • Temperature (F) - 99.1 • General: Denies changes in weight, fatigue, weakness, fever, chills, and night sweats. • Head: Denies history of trauma. Denies current headache. • Eyes: She does not wear corrective lenses, but notes that her vision has been worsening over the past few years. She complains of blurry vision after reading for extended periods. Denies increased tearing or itching prior to this past week. • Ears: Denies hearing loss, tinnitus, vertigo, discharge, or earache. • Nose/Sinuses: Denies rhinorrhea prior to this episode. Denies stuffi ness, sneezing, itching, previous allergy, epistaxis, or sinus pressure. • Mouth/Throat: Denies bleeding gums, hoarseness, swollen lymph nodes, or wounds in mouth. No sore throat prior to this episode. • Respiratory: She denies shortness of breath, wheezing, cough, sputum, hemoptysis, pneumonia, bronchitis, emphysema, tuberculosis. She has a history of asthma, last hospitalization was age 16 for asthma, last chest XR was age 16. Her current inhaler use has been her baseline of 2-3 times per week. Review of Systems Printable “Answer Key” available within the Shadow Health DCE. Subjective and Objective Model Documentation • Symptoms - Sore and itchy throat, runny nose, itchy eyes • Diagnosis - Allergic rhinitis Chief Complaint© Shadow Health® 072015 || ShadowHealth.com **For instructor use only** Page 1 of 3 HEENT - TINA JONES™ ADVANCED HEALTH ASSESSMENT Instructor Use Only Abnormal Findings Subjective (Reported by Tina) • Reports sore and itchy throat for the past week • Associated symptoms are red, itchy eyes and runny nose • Reports unrelated occasional headaches and eye strain Objective (Found by the student performing physical exam) • Oropharynx slightly erythematous with mild cobblestoning • Injection visible on conjunctiva • Nasal mucosa pale and boggy • Observable intermittent cough • Left fundus with sharp disc margins, no hemorrhages; right fundus with mild • retinopathic changes • Visual acuity: 20/40 right eye, 20/20 left eye • Acanthosis nigricans noted on neck [Show More]
Last updated: 2 years ago
Preview 1 out of 30 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$11.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 16, 2021
Number of pages
30
Written in
Additional information
This document has been written for:
Uploaded
Jul 16, 2021
Downloads
1
Views
187










_removed.png)


