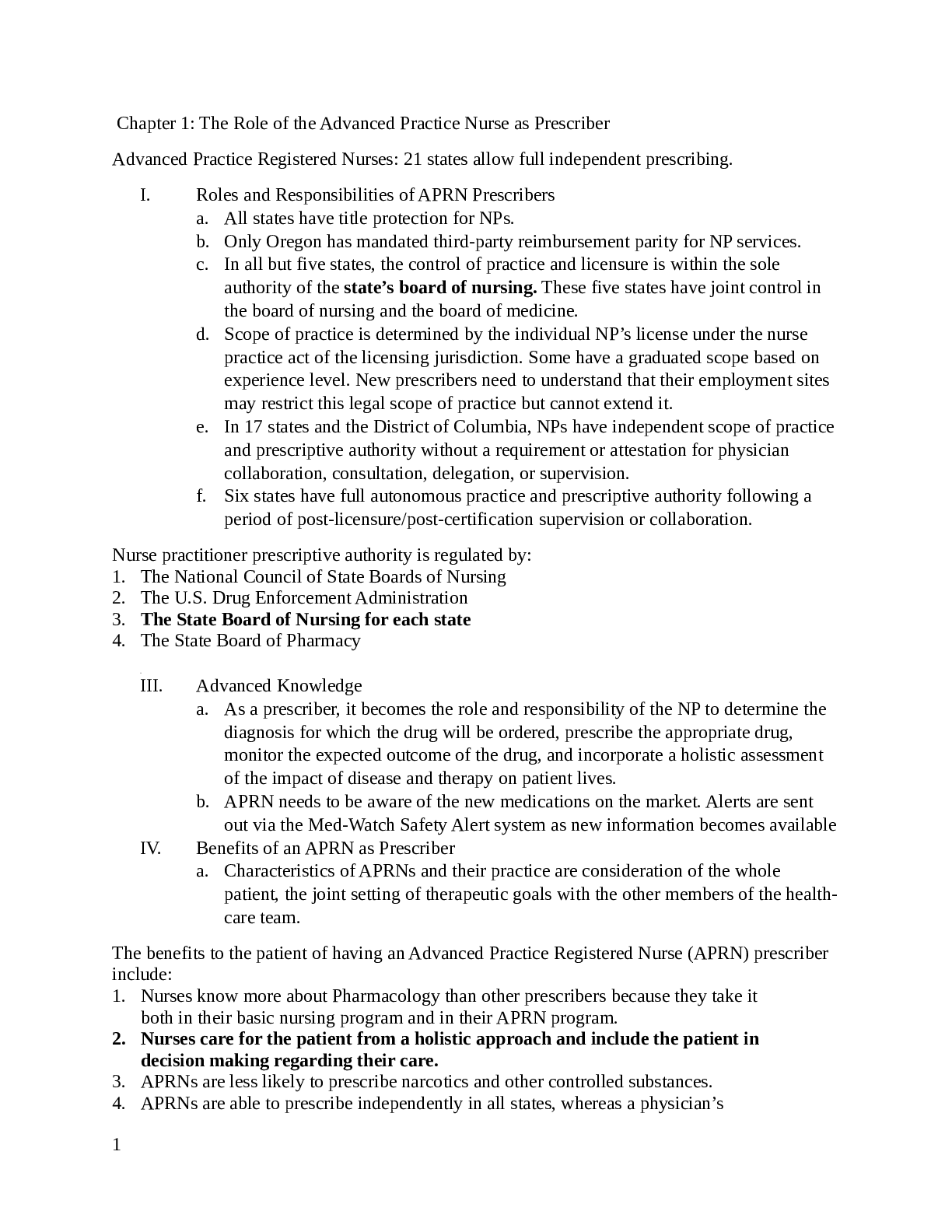
Chapter 1: The Role of the Advanced Practice Nurse as Prescriber
Advanced Practice Registered Nurses: 21 states allow full independent prescribing.
I. Roles and Responsibilities of APRN Prescribers
a. All states have
...
Chapter 1: The Role of the Advanced Practice Nurse as Prescriber
Advanced Practice Registered Nurses: 21 states allow full independent prescribing.
I. Roles and Responsibilities of APRN Prescribers
a. All states have title protection for NPs.
b. Only Oregon has mandated third-party reimbursement parity for NP services.
c. In all but five states, the control of practice and licensure is within the sole
authority of the state’s board of nursing. These five states have joint control in
the board of nursing and the board of medicine.
d. Scope of practice is determined by the individual NP’s license under the nurse
practice act of the licensing jurisdiction. Some have a graduated scope based on
experience level. New prescribers need to understand that their employment sites
may restrict this legal scope of practice but cannot extend it.
e. In 17 states and the District of Columbia, NPs have independent scope of practice
and prescriptive authority without a requirement or attestation for physician
collaboration, consultation, delegation, or supervision.
f. Six states have full autonomous practice and prescriptive authority following a
period of post-licensure/post-certification supervision or collaboration.
Nurse practitioner prescriptive authority is regulated by:
1. The National Council of State Boards of Nursing
2. The U.S. Drug Enforcement Administration
3. The State Board of Nursing for each state
4. The State Board of Pharmacy
II.
III. Advanced Knowledge
a. As a prescriber, it becomes the role and responsibility of the NP to determine the
diagnosis for which the drug will be ordered, prescribe the appropriate drug,
monitor the expected outcome of the drug, and incorporate a holistic assessment
of the impact of disease and therapy on patient lives.
b. APRN needs to be aware of the new medications on the market. Alerts are sent
out via the Med-Watch Safety Alert system as new information becomes available
IV. Benefits of an APRN as Prescriber
a. Characteristics of APRNs and their practice are consideration of the whole
patient, the joint setting of therapeutic goals with the other members of the healthcare team.
The benefits to the patient of having an Advanced Practice Registered Nurse (APRN) prescriber
include:
1. Nurses know more about Pharmacology than other prescribers because they take it
both in their basic nursing program and in their APRN program.
2. Nurses care for the patient from a holistic approach and include the patient in
decision making regarding their care.
3. APRNs are less likely to prescribe narcotics and other controlled substances.
4. APRNs are able to prescribe independently in all states, whereas a physician’s
1
assistant needs to have a physician supervising their practice.
V. Clinical Judgment in Prescribing
a. Is there a clear indication for drug therapy?
i. Increased awareness of the limitations of drugs i.e. antibiotic resistance
b. What drugs are effective in treating this disorder?
i. Nationally recognized guidelines including NIH, Agency for Health Care
Quality help by publishing disease-specific treatment guidelines.
c. What is the goal of therapy with this drug?
i. Short-term cure or long-term management?
d. Under what conditions is it determined that a drug is not meeting the goal and a
different therapy or drug should be tried?
e. Are there unnecessary duplications with other drugs that the patient is already
taking?
f. Would an OTC drug be just as useful as a prescription drug?
i. This can be helpful or hurtful to patients, as insurance will stop covering
OTC medications.
g. What about cost?
i. Newer the drug the higher the cost. Awareness is key because of factors
likely to lead to poor adherence related to finances.
h. Where is the information to answer these questions?
i. Micromedex, Lexicomp, Epocrates, and the FDA
Criteria for choosing an effective drug for a disorder include:
1. Asking the patient what drug they think would work best for them
2. Consulting nationally recognized guidelines for disease management
3. Prescribing medications that are available as samples before writing a prescription
4. Following U.S. Drug Enforcement Administration guidelines for prescribing
VI. Collaboration with other Providers
a. Physicians: initially MDs were the teachers of NPs.
i. Physicians look at pharmacology based on understanding biochemistry
and prescribing for a given pathophysiology. The emphasis is on the
disease and the drug, with less on the impact on the patient. They are weak
in patient education
ii. NPs approach for prescribing places an equal emphasis on understanding
the impact the drug will have on the patient. Strong patient education
teaching skills.
b. Pharmacists: must have a doctorate. Extensive knowledge about patho and take an
active role in determining the best drug to prescribe.
c. Other APRNs: share “clinical pearls” from their knowledge base
d. Physician Assistants: not autonomous. Similar hierarchy as NPs
e. Nurses not in Advance Practice Roles
2
i. Diabetic educators, wound care nurses
VII. Canadian Nurse Practitioner Practice
a. Similar to US. Determined by province
VIII. Current Issues and Trends in Health Care and Their Effect on Prescriptive Authority
a. Autonomy and Prescriptive Authority: we have overcome the cannot prescribe,
diagnose and admit but turf wars remain.
b. Interdisciplinary Teams: lets all play nice in the sand box
c. Level of Education of Team Members: we should all become DNPs
d. Reimbursement: we should all get paid the same, pay is a practice barrier.
Nurse practitioner practice may thrive under health-care reform because of:
1. The demonstrated ability of nurse practitioners to control costs and improve
patient outcomes
2. The fact that nurse practitioners will be able to practice independently
3. The fact that nurse practitioners will have full reimbursement under health-care
reform
4. The ability to shift accountability for Medicaid to the state level
Chapter 2: Review of Basic Principles of Pharmacology
I. Pharmacology – The Study of Drugs
a. Drug: any chemical substance that produces a measurable biological response.
II. How New Drugs are Developed
a. Preclinical: testing medications in cells, isolated tissues and organs, and lab
animals.
b. Clinical: working with the FDA must prove that the drug is safe and effective.
Starts out with a small healthy cohort, then on actually targeted patients and then
spread out cohorts.
III. Drug Responses: drugs must overcome homeostasis to be effective.
a. Dose-Response Curves: the higher the concentration of a drug at its site of action,
the more the drug will bind to the receptor and the greater will be the response.
b. Two Types of Drug Responses:
i. Quantal: Responses that may or may not occur. If we measure as either
occurring or absent it is quantal.
1. Ex. Sleep, rash, seizures, pregnancy, and death.
ii. Graded: biological effects that can be measured continually up to the
maximum responding capacity of the biological system. Easier to manage
clinically because we can see the effects and then adjust the dose.
1. Ex. BP, HR, diuresis, bronchodilation, FEV1, Pain and coma scale
iii. They are not mutually exclusive. I.e. Adjusting seizure medications to
have fewer occurrences (graded), even though the goal is to be seizure free
(quantal).
c. Expressing Drug Responses
3
i. Dose response curves provide information on the relationship between
dosage or concentration and responses for one or more drugs.
ii. Drugs are compared using potency, efficacy, intrinsic activity and
selectivity.
1. Potency, how much drug is needed to produce a biological
response.
2. Efficacy, ability of the drug to produce a maximum effect at any
dosage.
3. Intrinsic activity is similar to efficacy; however it is used to
describe the ability of a drug to produce a response once it has
occupied specific receptors.
d. Drug Selectivity: a ratio of the dose or concentration producing the undesired
effect to the dose or concentration producing the desired effect.
i. Therapeutic index is a special ratio describing drug selectivity versus the
lethal dose.
e. Drug Responses in the Real World, using the placebo effect to create a baseline
for measurement of the dose-effect curve.
f. Brand versus Generic Drugs: After the original drug patent expires other
companies can manufacture generic drugs using the same amount of active
ingredient as the brand.
IV. Receptors: large protein molecules that interact with and mediate the action of drugs.
They determine the relationship between dose and effect, the selectivity of drugs, and
the actions pharmacological antagonists.
a. Ion Channel Receptors: transmits signals across the cell membrane by increasing
the flow of ions and altering the electrical potential.
i. Responses have rapid onset and short duration.
b. Receptors Coupled to G Proteins:
c. Transmembrane Receptors: extracellular hormone-binding domain and an
intracellular enzyme domain that phosphorylates the amino acid tyrosine.
d. Intracellular Receptors Regulating Gene Expression:
e. Enzymes
f. Drug Action at Receptors:
i. Agonists: drugs that produce receptor stimulation and conformational
change every time they bind. Overtime they can downregulate the
numbers of that specific receptor and become desensitized.
ii. Antagonists: drugs that occupy receptors without stimulating them. They
prevent other molecules, such as agonists, from producing a response.
1. Beta-blockers, if abruptly discontinued can cause an exaggerated
response.
g. Disease States and Receptors
h. Non-receptor Mechanisms
V. Pharmacokinetics
a. Absorption
4
i. Parental Administration: injection, given when immediate effect is
required, ingredients are destroyed or not absorbed in the GI tract, or when
patient is unable to take oral medication.
1. IV is the fastest route and is the standard for which other routes are
compared too.
ii. Oral: most common and convenient. Slower, requiring time to open or
dissolve to enter systemic circulation. Liver is the location of drug
metabolism before reaching the bloodstream.
iii. Sites of Administration: Higher concentrations are achieved when meds
are given closest to the desired target.
iv. Bioavailability: not all meds are dissolved or absorbed or survive liver
passage, only a fraction makes it to the bloodstream. Range from 10-90%
1. Important for drugs with narrow therapeutic ranges or sustainedrelease mechanisms
v. Peak Blood Levels: the speed at which drugs enter the bloodstream, faster
the speed the increase in toxicity and adverse effect. Phenytoin for
example needs peak and trough levels drawn to determine if the drug is in
the therapeutic range.
1. Steady state is when the amount of drug in the body remains
constant, usually occurs after 4 to 5 half-lives.
b. Distribution: process of drugs moving throughout the body.
i. Properties that affect distribution
1. Henderson-Hasselbalch Relationship, protein binding, transport
systems, and volume of distribution
2. Albumin is critical to the distribution of drugs to target tissues
3. The blood-brain barrier lows the entry of many drugs into and
from the brain cells.
c. Metabolism: process of changing one chemical into another, and either creates or
uses energy. Liver is the main center for drug metabolism because it is the first
organ encountered by drugs from the GI tract and contains high amounts of drugmetabolizing enzymes. “First-pass metabolism”
i. Drugs that have a significant first-pass effect are rapidly metabolized by
the liver and may have little if any desired action.
ii. Phase 1 and phase 2 reactions change drug molecules to a form that an
excretory organ can excrete.
iii. Metabolism and Half-life: drugs should be administered at dosing
intervals that are close to their half-life. Half-life is the time required for
the amount of drug in the body to decrease by 50%.
d. Drug Interactions: alterations in biotransformation are responsible for many
interactions.
e. Excretion: principal organs of excretion are kidneys, lungs, biliary system, and
intestines.
5
i. Renal: primary organ for most drugs that create metabolites that are watersoluble.
ii. Renal excretion of drugs: the rate is dependent on renal blood flow,
molecular drug size, the charge, the degree of protein binding, and tubular
acidity.
iii. Biliary excretion: drugs can enter bile and then be excreted into the
intestinal tract when bile is released.
iv. Other sites:
1. Pulmonary (lungs): occurs for any volatile material present in the
body. Important for anesthetic gases and alcohol
[Show More]