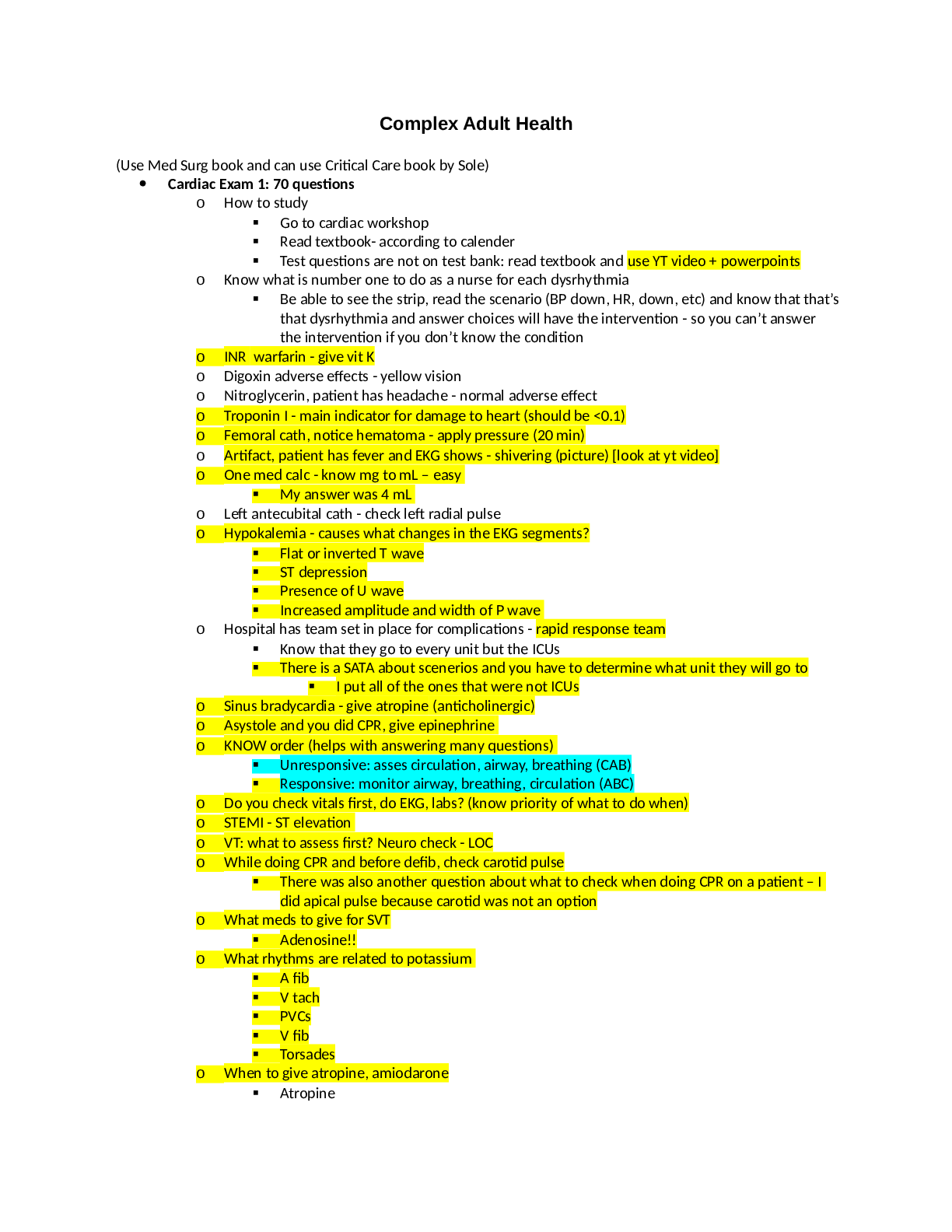
*NURSING > STUDY GUIDE > NUR 2092 - Health Assessment Exam 2 Study Guide (All)
NUR 2092 - Health Assessment Exam 2 Study Guide
Document Content and Description Below
Health Assessment Exam 2 Study Guide (additionally use the chapter summaries at the end of the PPT) Vital Signs What are the normal ranges of vital signs for an adult Temperature: Normal o... ral temperature in a resting person is 37° C (98.6° F), with a range of 35.8° C to 37.3° C (96.4° F to 99.1° F) Normal temperature is influenced by the following: a. Diurnal cycle of 1° F to 1.5° F, with trough occurring in early morning hours and peak occurring in late afternoon to early evening b. Menstruation cycle in women: progesterone secretion, occurring with ovulation at midcycle, causes a 0.5° F to 1.0° F rise in temperature that continues until menses c. Exercise: moderate to hard exercise increases body temperature d. Age: wider normal variations occur in infant and young child due to less effective heat control mechanisms; in older adults, temperature usually lower than in other age groups, with a mean of 36.2° C (97.2° F) Pulse: Stroke volume: amount of blood every heart beat pumps into aorta. ‘ a. Palpating peripheral pulse gives rate and rhythm of heartbeat, as well as local data on condition of artery, Radial pulse usually palpated while vital signs measured, Using pads of the first three fingers, palpate radial pulse at flexor aspect of wrist laterally along radius bone. Push until strongest pulsation is felt. If rhythm is regular, count number of beats in 30 seconds and multiply by 2. If irregular count for full minute start zero for first pulse felt and move up from there. Rate, rhythm, force, elasticity. b. In resting adult, normal heart rate range is 60 to 100 beats per minute (bpm) Respirations: a. Normally, person’s breathing is relaxed, regular, automatic, and silent. Because most people are unaware of their breathing, do not mention that you will be counting respirations, because sudden awareness may alter normal pattern. Instead, maintain your position of counting radial pulse and unobtrusively count respirations. b. Count for 30 seconds or a full minute if you suspect an abnormality. Blood Pressure: Blood pressure (BP) is force of blood pushing against side of its container, vessel wall. Strength of push changes with event in cardiac cycle. - Systolic pressure: maximum pressure felt on artery during left ventricular contraction, or systole - Diastolic pressure: elastic recoil, or resting, pressure that blood exerts constantly between each contraction Pulse pressure: difference between systolic and diastolic -Reflects stroke volume Mean arterial pressure (MAP): pressure forcing blood into tissues, averaged over cardiac cycle. Average BP in young adult is 120/80 mm Hg; varies normally with many factors: -Age: gradual rise through childhood and into adult years -Gender: after puberty, females show a lower BP than males; after menopause, females higher than males. -Race: African American adult’s BP usually higher than White persons of same age. O2- Healthy person with no lung disease and no anemia normally has an SpO2 of 97% to 98% Why would you use the bell vs the diaphragm of the stethoscope? a. Diaphragm most often because its flat edge is best for high-pitched sounds—breath, bowel, and normal heart sounds. b. Bell end piece has a deep, hollow, cuplike shape. It is best for soft, low-pitched sounds such as extra heart sounds or murmurs. Oxygenation • Lung Assessment o Tell me about different breath sounds, locations of them and how they would be described Normal- Discontinuous- discrete, crackling sounds. Continuous- Connected, musical sounds (wheezing) o Tell me the order and how you would do a respiratory assessment Inspection, Palpation, Percussion, Auscultation o Tell me objective signs you would notice that a client has chronically poor oxygenation Low oxygen saturations, Shallow and frequent breaths, diminished lung sounds. • Tell me when you would put the client in a Semi-Fowler’s position or tripod position and why Tripod position- would be used with a patient with Emphysema during the inspection phase maximum expansion of the chest. Semi-Fowler’s position cardiac, respiratory, or neurological problems and is often optimal for patients who have nasogastric tube in place. • LifeSpan Considerations: Safety Issues - Hand Hygiene Wash your hands—this is the single most important step to decrease microorganism transmission. • Tell me about the physiology of respiration r/t CO2 - • Tell me which body systems are involved in the process of normal gas exchange. o Respiratory system and Cardiovascular and Nero • Tell me how you would perform a nasal assessment and what would you expect to find o Inspect external nose for symmetry, any deformity, or lesions. Palpation: test patency of each nostril palpate the sinus area. Inspect with nasal speculum nasal mucosa, septum, and turbinates. o Symmetric, no deformity or skin lesions. Mucosa pink, no discharge, lesions, or polyps, no septal deviations or perforations, Sinuses no tenderness to palpation. • Tell me how and when you would use pursed lip breathing o When someone is having trouble breathing. Inhale slowly through the nose keeping mouth closed. Exhale through the mouth with mouth puckered as if giving a kiss. Breathing should be slow and steady. • Tell me the physiologic benefits of smoking cessation o • Tell me how anemia affects gas transport in the body o With the reduction of healthy hemoglobin to transport o2 or co2 thus there is less of these gases moving through the body at a time decreasing gas transport. • Tell me how you would assess for cyanosis in a dark-skinned client o Cyanosis can be detected by assessing the skin and nail beds for a dull lifeless color. The soles of the feet and the toenails are less pigmented, which can enable detection of cyanosis or duskiness in the lower extremities. • Tell me abnormalities of the shape of the chest cavity and do they develop o Barrel Chest- normal aging and also with chronic emphysema and asthma as a result of hyperinflation of lungs. o Pectus Carinatum- A forward protrusion of the sternum, with ribs sloping back at either side and vertical depressions along costochondral junctions (pigeon breast). Less common than pectus excavatum, this minor deformity requires no treatment. If severe, surgery may be indicated. o Pectus Excavatum- A markedly sunken sternum and adjacent cartilages (also called funnel breast). Depression begins at second intercostal space, becoming depressed most at junction of xiphoid with body of sternum. More noticeable on inspiration. Congenital, usually not symptomatic. When severe, sternal depression may cause embarrassment and a negative self-concept. Surgery may be indicated. o Scoliosis- S-shaped curvature of the thoracic and lumbar spine, usually with involved vertebrae rotation. Note unequal shoulder and scapular height and unequal hip levels, rib interspaces flared on convex side. More prevalent in adolescent age-groups, especially girls. Mild deformities are asymptomatic. If severe (>45 degrees) deviation is present, scoliosis may reduce lung volume, and person is at risk for impaired cardiopulmonary function. Primary impairment is cosmetic deformity, negatively affecting self-image. Refer early for treatment, possible surgery. o Kyphosis- An exaggerated posterior curvature of the thoracic spine (humpback) that causes significant back pain and limited mobility. Severe deformities impair cardiopulmonary function. If the neck muscles are strong, compensation occurs by hyperextension of head to maintain level of vision. o Kyphosis has been associated with aging, especially the familiar “dowager's hump” of postmenopausal osteoporotic women. However, it is common well before menopause. It is related to physical fitness; women with adequate exercise habits are less likely to have kyphosis. • How would you assess thoracic expansion? Tactile Fremitus? Egophony? o Thoracic expansion- Ask the person to take a deep breath. Watch your thumbs move apart symmetrically and note smooth chest expansion with your fingers. Any limitation in thoracic expansion is easier to detect on the anterior chest because greater range of motion exists with breathing here. o Assess tactile (or vocal) fremitus. Fremitus is a palpable vibration. Sounds generated from the larynx are transmitted through patent bronchi and the lung parenchyma to the chest wall, where you feel them as vibrations. Use either the palmar base (the ball) of the fingers or the ulnar edge of one hand and touch the person's chest while he or she repeats the words “ninety-nine” or “blue moon.” These are resonant phrases that generate strong vibrations. Start over the lung apices and palpate from one side to another o Egophony- Auscultate the chest while the person phonates a long “ee-ee-ee-ee” sound. Normally you should hear “eeeeeeee” through your stethoscope. Over area of consolidation or compression the spoken “eeee” sound changes to a bleating long “aaaaa” sound. Perfusion • Circulatory Assessment o Functions of the CV system Provides oxygen, nutrients, and hormones to cells, removes carbon dioxide and waste products from cells, Maintains body temperature by distributing heat produced by metabolic activity. o Tell me how you would do a circulatory head to toe assessment To evaluate carotid arteries, person can be sitting. To assess jugular veins and precordium, person should be supine with head and chest slightly elevated. Palpation of carotid artery they should be normally contour is smooth with a rapid upstroke and slower downstroke, and the normal strength is 2+ or moderate. Findings should be the same on both sides. And only one artery should be palpated at a time. Auscultation performed by lightly apply bell of stethoscope over carotid artery at three levels: Angle of jaw, Midcervical area, Base of neck. Auscultation of the carotid artery should be done lightly without compressing the artery because it could create a false sound. Palpate apical impulse by Localize apical impulse precisely by using one finger pad. Asking person to “exhale and then hold it” aids examiner in locating pulsation; may need to roll person midway to left to find it; note that this also displaces apical impulse farther to left. Palpate across precordium. By using palmar aspects of your four fingers, gently palpate apex, left sternal border, and base, searching for any other pulsations. Auscultation listen to the 4 heart valve areas these are second right interspace: aortic valve area, second left interspace: pulmonic valve area, left lower sternal border: tricuspid valve area, fifth interspace at around left midclavicular line: mitral valve area o How do you assess right sided vs. left sided heart failure. o Tell me about Hypoxia and how you would assess for it. o Tell me how you would assess for hypertension. o Tell me what heart sounds you hear at each listening point and where would you find them (slides: APETM) o Tell me what the phases of the cardiac cycle are S-1/S-2 and what heart sounds you would hear o Tell which valves are heard closing during S1 and S2 S1 Mitral, tricuspid valves close S2 Aortic, pulmonic valves close o Tell me how you would assess each peripheral pulse (carotid, brachial, radial, popliteal, pedal) o Tell me how you assess for edema and stage edema. Read in the book about assessing pitting edema o Read in the chapter on the differences between arterial insufficiency ulcers and venous ulcers Arterial (Ischemic) Ulcer Buildup of fatty plaques on intima (atherosclerosis) plus hardening, calcification of arterial wall (arteriosclerosis). S: Deep muscle pain in calf or foot, claudication (pain with walking); pain at rest indicates worsening of condition. O: Coolness, pallor, elevational pallor, and dependent rubor; diminished pulses; systolic bruits; signs of malnutrition (thin, shiny skin; thick-ridged nails; atrophy of muscles); distal gangrene. Ulcers occur at toes, metatarsal heads, heels, and lateral ankle and are characterized by pale ischemic base, well-defined edges, and no bleeding. Venous (Stasis) Ulcer- After acute DVT or chronic incompetent valves in deep veins. Venous ulcers account for 80% of lower leg ulcers. S: Aching pain in calf or lower leg, worse at end of day, worse with prolonged standing or sitting. Itching with stasis dermatitis. O: Lower leg edema that does not resolve with diuretic therapy. Firm, brawny edema; coarse, thickened skin; pulses normal; brown pigment discoloration; petechiae; dermatitis. Venous stasis causes increased venous pressure, which then causes red blood cells (RBCs) to leak out of veins and into skin. RBCs break down to hemosiderin (iron deposits), which are brown pigment deposits. Borders are irregular. Venous ulcers are shallow and may contain granulation tissue. A weepy, pruritic stasis dermatitis may be present. Ulcers occur at medial malleolus and are characterized by bleeding, uneven edges. o See chapter summary on PPT Tissue Integrity • Integumentary Assessment o Anatomy and Physiology of the Skin The skin is the body’s largest organ system it covers 20 square feet of surface area in adults. It’s poupous is to guards body. Skin has two layers Epidermis: outer highly differentiated layer. Basal cell layer forms new skin cells. Outer horny cell layer of dead keratinized cells. Dermis: inner supportive layer. Connective tissue or collagen, elastic tissue, beneath these layers is a subcutaneous layer of adipose tissue. o Functions of the skin Skin is waterproof, protective, and adaptive. Protection from environment Prevents penetration Perception Temperature regulation Identification Communication Wound repair Absorption and excretion Production of vitamin D o Tell me how you would assess for nail health and abnormalities in an adult o Tell me how you would describe different types of rashes, primary vs. secondary lesions and skin abnormalities; review examples of types of lesions. Eg. Macule vs. papule. Describe what you see o Tell me how to assess for skin color changes r/t cyanosis in a client with dark skin colors o Tell me signs and symptoms of skin cancer and the ABCDE rule Teach skin self-examination using ABCDE rule to detect suspicious lesions • A: asymmetry • B: border • C: color • D: diameter • E: elevation and enlargement o Tell me how you would assess normal vs abnormal lymph nodes and locations of chains o Tell me how you would do a complete skin assessment; history interview sheet and physical assessment o Tell me how you would assess for skin temperature o Tell me signs and symptoms of hypoxia or cyanosis on the skin/nails o What questions might you ask in a focused health history if some has a skin condition? o See Chapter Summary on PPT and interview sheet HEENT Sensory Perception • Tell me about the process of visual accommodation (distance, close, pupil response, etc.) • Tell me how you would inspect the ear of an adult vs. child o As you inspect the external ear, note the size of the auditory meatus. Choose the largest speculum that fits comfortably in the ear canal and attach it to the otoscope. Tilt the person's head slightly away from you toward the opposite shoulder. This method brings the obliquely sloping eardrum into better view. o Pull the pinna up and back on an adult or older child; this helps straighten the S-shape of the canal (Fig. 15-7). (Pull the pinna down on an infant and a child younger than 3 years [see Fig. 15-13]). Hold the pinna gently but firmly. Do not release traction on the ear until you have finished the examination and the otoscope is removed. • Tell me about the Rinne test and what you would expect to find. o Is used primarily to evaluate loss of hearing in one ear. It compares perception of sounds transmitted by air conduction to those transmitted by bone conduction through the mastoid. • Tell me how a nurse could do basic hearing tests and vision tests and what are their names and what do the results mean o Snellen Eye Chart- Place the Snellen alphabet chart in a well-lit spot at eye level. Position the person on a mark exactly 20 feet from the chart. Use an opaque card to shield one eye at a time during the test; inadvertent peeking may result when shielding the eye with the person's own fingers. o Confrontation Test- This test screens for loss of peripheral vision. It compares the person's peripheral vision with your own, assuming that yours is normal. Position yourself at eye level about 2 feet away. Looking straight at you, the person covers one eye with an opaque card (here the right eye) as you cover the opposite eye. o Weber Test o Rinne Test • Tell me how to do an HEENT assessment; use the lab sheet to review. What are you looking for in the nose and throat? o Head, Eye, Ear, Nose and Throat Exam is usually the initial part of a general physical exam, after the vital signs. o □ headache □ dizziness □ earache □ hearing loss □ tinnitus □ vision change □ eye pain/sensitivity □ excessive tearing □ eyeglasses/contact use □ glaucoma □ rhinorrhea □ nasal congestion □ postnasal drip □ sinus pain □ nosebleeds □ hay fever □ sore throat □ mouth sores □ hoarseness □ toothache □ bleeding gums □ dentures • Common developmental issues in the elderly and risk factors • See chapter summary on PPT Thermoregulation • Tell me about the body’s mechanisms for thermoregulation Abdominal GI/GU • How do you conduct a GI/GU assessment? Order of assessment and what are you looking for • How do you listen for bowel sounds? What is considered hyper or hypo? When would you hear hyper or hypo? What do you do if you don’t hear any bowel sounds? o Hyperactive sounds are loud, high-pitched, rushing, tinkling sounds that signal increased motility. o 2. Hypoactive or absent sounds follow abdominal surgery or with inflammation of the peritoneum • What are common symptoms of GU--kidney/bladder issues or infections? • How might you assess a client for a hernia? Peritoneal irritation? • Locations of the internal organs • See the chapter summaries on PPT Breast • Risk Factors for cancer; recommended age for Mammograms based on the American Cancer Society • Abnormalities Terms &/or What it is, how you do it or assess for it, what does it mean Bruit in Carotid or Abdominal Aortic Arteries- Bruit, also called vascular murmur, is the abnormal sound generated by turbulent flow of blood in an artery due to either an area of partial obstruction or a localized high rate of blood flow through an unobstructed artery. Murmur- murmur is an unusual sound heard between heartbeats. Murmurs sometimes sound like a whooshing or swishing noise. Petechiae- Petechiae are tiny, circular, non-raised patches that appear on the skin or in a mucous or serous membrane. They occur as the result of bleeding under the skin. Pulse Oximetry- Pulse oximetry is a test used to measure the oxygen level (oxygen saturation) of the blood. It is an easy, painless measure of how well oxygen is being sent to parts of your body furthest from your heart, such as the arms and legs. Subjective Data vs. Objective Data (definitions and examples) Auscultate- examine a patient by listening to sounds from (the heart, lungs, or other organs), typically using a stethoscope. Hypoxia- is a condition in which the body or a region of the body is deprived of adequate oxygen supply at the tissue level. Erythema- superficial reddening of the skin, usually in patches, as a result of injury or irritation causing dilatation of the blood capillaries. Origin Chest Excursion- Diaphragmatic excursion is the movement of the thoracic diaphragm during breathing. Normal diaphragmatic excursion should be 3–5 cm, but can be increased in well-conditioned persons to 7–8 cm. This measures the contraction of the diaphragm. It is performed by asking the patient to exhale and hold it. Jaundice- is a condition in which the skin, whites of the eyes and mucous membranes turn yellow because of a high level of bilirubin, a yellow-orange bile pigment. Jaundice has many causes, including hepatitis, gallstones and tumors. Cyanosis- is the bluish or purplish discoloration of the skin or mucous membranes due to the tissues near the skin surface having low oxygen saturation. Tachypnea- abnormally rapid breathing. Dyspnea- difficult or labored breathing. Inspection- Palpation- is a method of feeling with the fingers or hands during a physical examination. The health care provider touches and feels your body to examine the size, consistency, texture, location, and tenderness of an organ or body part. Auscultation- the action of listening to sounds from the heart, lungs, or other organs, typically with a stethoscope, as a part of medical diagnosis. Origin Percussion Normal Lung Sounds (location to hear them and names) The bronchial breath sounds over the trachea has a higher pitch, louder, inspiration and expiration are equal and there is a pause between inspiration and expiration. The vesicular breathing is heard over the thorax, lower pitched and softer than bronchial breathing. Expiration is shorter and there is no pause between inspiration and expiration. The intensity of breath sound is higher in bases in erect position and dependent lung in decubitus position. The breath sounds are symmetrical and louder in intensity in bases compared to apices in erect position. No adventitious sounds are heard. Adventitious Lung Sounds (location and names) Tachy vs. brady prefix and how it relates to cardiac and lung tachy fast bready slow Continued......................... [Show More]
Last updated: 2 years ago
Preview 1 out of 18 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$15.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 25, 2021
Number of pages
18
Written in
Additional information
This document has been written for:
Uploaded
Jan 25, 2021
Downloads
0
Views
90