Biology > STUDY GUIDE > NSG 331 Exam 2 study guide 2019/2020 – Marian University | NSG331 Exam 2 study guide 2019/2020 (All)
NSG 331 Exam 2 study guide 2019/2020 – Marian University | NSG331 Exam 2 study guide 2019/2020
Document Content and Description Below
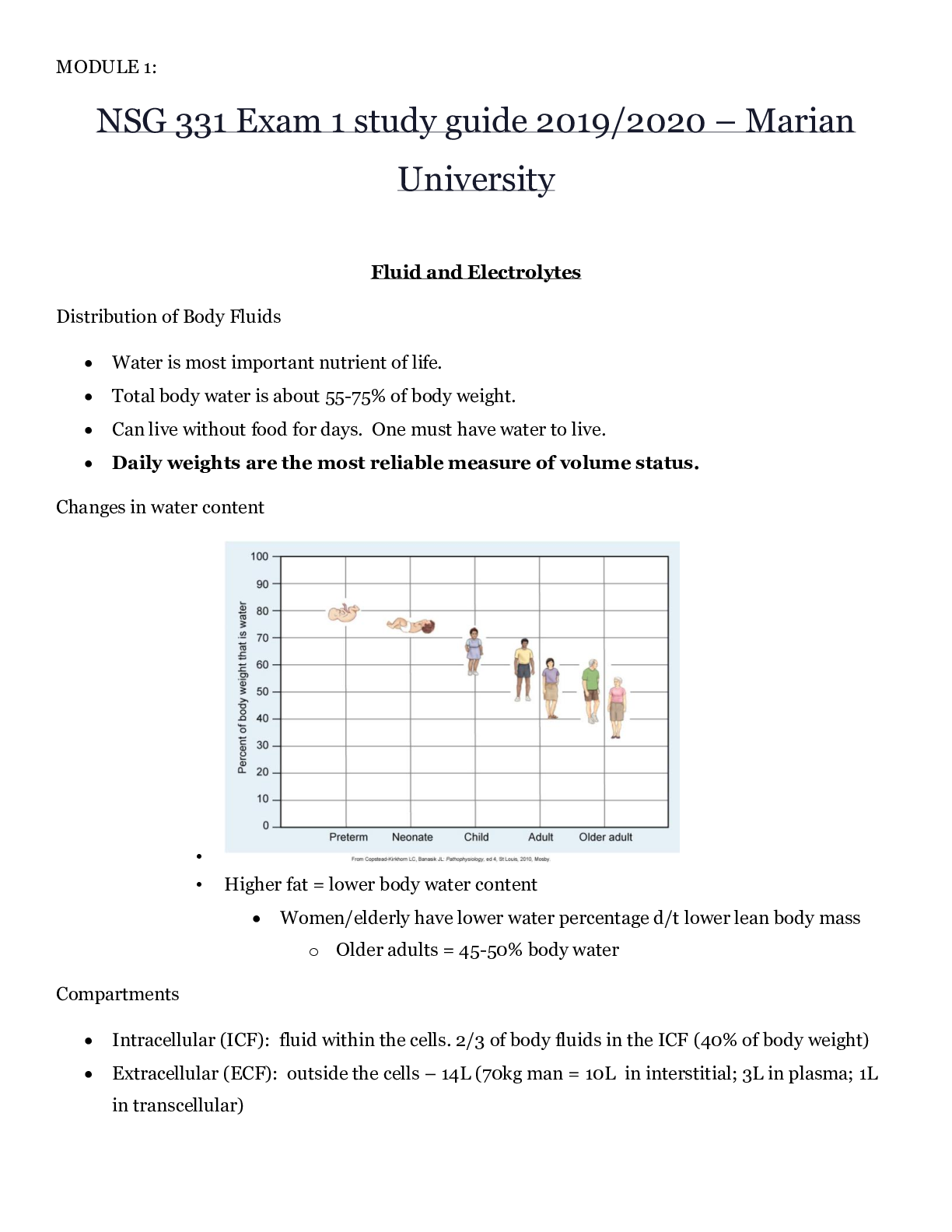
NSG 331 Exam 2 study guide 2019/2020 – Marian University Care of the Adult in the Perioperative Setting Case study • J.D., a 45-year-old female, presents to the surgeon’s office for presur... gical workup for right breast lumpectomy. • Ambulatory/Outpatient setting and elective goal is cure. Nurses Role in the pre-op setting • Knowledge of disorder that requires the surgery along with comorbidities. • ID patient’s response to stress of surgery • Knowledge of the results of appropriate preoperative diagnostic tests. • ID risks and complications • Knowledge of documentation and communicating of important preoperative assessment findings are essential for quality care. • Avoid repetition, know pre-surgery needs • Interview – one of the most important • Communicate findings to others Case Study continued… • J.D. is accompanied by her husband. • She tells you she has two school-age children. • She states that she is here because her breast biopsy was positive for cancer and she anticipates that the lumpectomy will remove all cancer. • The nurse should (in the interview) • Obtains patients’ health history including drug and food allergy • Provides information and clarifies info about surgery including anesthesia • Assess the patient’s emotional state and readiness for surgery, including his or her expectations about the surgical outcome Case Study Assessment • J.D. tells you she has a history of hypertension, for which she takes HCTZ daily. • She recently was diagnosed with type 2 diabetes and is currently controlled with an oral agent and diet. • The nurse should establish baseline data (vitals, blood sugar, and if she took her meds today or not?) • Psychological status – reinforce coping strategies • Physiological status – factors contributing to risk • Plan of care **safety Nursing Assessment Goals ** Overall goal is to identify risk factors and plan care to ensure patient safety throughout the surgical experience. • Establish baseline data for comparison in the intraoperative and postoperative period • Determine the patient’s psychological status to reinforce the use of coping strategies during the surgical experience • Determine physiological factors directly or indirectly related to the surgical procedure that may contribute to operative risk factors • Identify and document surgical site • Identify drugs, OTC medications, and herbs taken that may affect surgical outcome • Review results of preoperative diagnostic studies • Identify cultural and ethnic factors that may affect surgical experience • Determine receipt of adequate information from surgeon to sign informed consent • Determine that consent form is signed and witnessed and if given enough info Psychosocial assessment • Excessive stress response can be magnified and affect recovery • Influencing factors • Age • Past experiences • Current health • Socioeconomic status • Use common language & avoid medical jargon • Use translators if needed because familiar language… • Decreases level of anxiety • Communicate all concerns to surgical team • Nurse’s role is to assess the patient for potential or actual stressors that could negatively affect surgery. • Most common psychological factors are ANXIETY, FEAR, AND HOPE • Anxiety can impair cognition, decision making, and coping abilities • Anxiety can arise from • Lack of knowledge • Unrealistic expectations ♣ Stories heard in media and/or by friends • Information lessens anxiety • Inform the physician if any further information is needed or if anxiety is excessive • Anxiety may arise from conflict with interventions (i.e., Jehovah’s witness and blood transfusions) and religious or cultural beliefs • Identify beliefs and discuss with surgeon and operative staff Case study continued… • J.D. states that her mother and aunt have a history of breast cancer resulting in mastectomy. • She appears anxious and you note constant fidgeting. • J.D. states that she is here because her breast biopsy was positive for cancer. • She anticipates that the lumpectomy will remove all cancer. • She has had no other surgeries. Psychosocial Assessment continued… • Fears • Death or disability ♣ Notify the HCP if severe because it may prompt postponement ♣ Influence outcome • Pain ♣ Consult with ACP ♣ Reassure the patient that drugs are available for anesthesia and analgesia during surgery – will not lead to addiction ♣ Confirm drugs will be available and encourage patient to ask before pain becomes severe! ♣ Teach the patient how to use a pain intensity scale. • Mutilation/alteration in body image ♣ Assess concerns nonjudgmentally ♣ Can happen in both radical (amputation) and minor (breast biopsy) surgeries. • Anesthesia ♣ ACP for consult ♣ May arise from fear of the unknown, personal experiences, or tales of other bad experiences. ♣ Many fear losing control while under anesthesia, or brain damage/paralysis • Disruption of life functioning ♣ Range from fear of permanent disability to temporary loss ♣ Include family and financial concerns ♣ Consultations PRN w/ caregiver, social worker, psychologist or financial advisor • Hope • May be strongest positive coping mechanism • Never deny/minimize b/c it could negate positive mental attitude necessary for a quick and full recovery • Repair (plastic surgery for burns), rebuild (total joint replacement) or save/extend a life (repair of an aneurysm or transplant) • Assess and support Case study continued… • J J.D. is currently taking HCTZ, glipizide (Glucotrol), multivitamin, fish oil, and a daily low-dose aspirin. • She reports an allergy to penicillin, resulting in a rash. • Nursing concerns • HTN, hypoglycemia, bleeding from aspirin and fish oil, PCN allergy considered, and latex allergy, fish oil can raise fasting glucose levels • All OTC drugs, herbs, recreational drugs, and tobacco Past Health history • Previous health problems and surgeries o Does patient understand need for surgery? ♣ Ex. Patient schedule for a total knee replacement may indicate it is because increasing pain and immobility • Document the reason for past hospitalizations o Including past surgeries and dates. o Identify any problems with previous surgeries ♣ Ex wound infection or drug reaction • Ask women about menstrual cycle and obstetric history o Date of last period, number of pregnancies, history of C sections Family health history • Any inherited traits? • Parent with heart and/or endocrine disease o Ex. HTN, sudden cardiac death, or MI • Adverse reactions to or problems with anesthesia o Ex. Malignant hyperthermia has a genetic predisposition. Measures can be used to decrease complications associated with this condition can be taken. Medications • The interaction of the patient’s current drugs and anesthetics can increase or decrease the desired physiological effect of the anesthetics. o Opiods and prescribed drugs for chronic health conditions (heart disease, HTN, depression, seizure disorder, DM) ♣ Antidepressants – can potentiate the effect of opioid agents that can be used for anesthesia ♣ Antihypertensive – may predispose the patient to shock from the combined effect of the drug and the vasodilator effect of some anesthetic agents ♣ Insulin – may require adjustments during the perioperative period because of increased metabolism, decreased oral intake, stress, and anesthesia ♣ Antiplatelet – inhibit platelet aggregation and may contribute to postoperative bleeding o Surgeons may instruct patients to withhold these drugs before surgery ♣ The drugs below present a problem: ♣ Longterm anticoagulant therapy (warfarin) ♣ Rivaroxaban (Xarelto) ♣ Dabigatran (Pradaxa) ♣ Apixaban (Eliquis) • The options for patients taking this medication are determined by patient history and nature of surgery and include: o Continuing therapy o Withholding for a time before and after surgery o Withholding the therapy and starting subcutaneous or IV heparin therapy during the perioperative period. o Herbs and dietary supplements – discontinue 2-3 weeks prior to surgery ♣ They can cause harmful effects ♣ Patient taking anticoagulants and antiplatelets, herbal supplements can produce excessive postoperative bleeding that may require a return to the OR. ♣ Avoid: • Astragalus and ginseng – raise BP before and during surgery • Garlic, Vitamin E, gingko, and fish oils – increase bleeding • Kava and valerian – cause excessive sedation o Recreational drugs (alcohol, tobacco, opioids, marijuana, cocaine, and amphetamines) ♣ Stress that recreational drugs use may affect the type and amount of anesthesia. ♣ When patients become aware of risks they will usually be truthful. ♣ Chronic alcohol – potential lung, liver, and GI damage. • Liver function decrease, metabolism of anesthetic agents is prolonged, nutritional status is altered, and the potential for postoperative complications increases. • Alcohol withdrawal can also occur. Allergies • Drug intolerance and drug allergies • Document and put an allergy arm band on patient when necessary • Also include nondrug allergies (food, latex, pollen, animals) • Patients with a history of allergic reactions are more at risk for hypersensitivity to drug given in anesthesia. • Latex allergy o Risks factors – long-term, multiple exposures to latex (health care and rubber industry), hay fever, asthma, and food allergies to eggs, avocado, bananas, chestnuts, potatoes, and peaches) Review of systems • Body systems review o Confirms the presence or absence of diseases o Alerts to areas to closely examine o Provide essential data to determine specific preoperative tests o Confirms the presence or absence of diseases o Alerts to areas to closely examine o Provide essential data to determine specific preoperative tests o RESULTS SHOULD BE IN CHART BEFORE SURGERY • Cardiovascular system o Report ♣ Any cardiac problems so they can be monitored during the intraoperative period • HTN, angina, dysrhythmias, heart failure, or MI ♣ Cardiac consult for recent MI, valvular heart disease, implantable cardioverter - defibrillator ♣ Inquire about current treatment and level of functioning • Presence of pacemaker/ICD or use of cardiac drugs o 12-lead electrocardiogram (ECG) – results in chart prior to surgery o Coagulation studies – results in chart prior to surgery o CV assessment provides what other data on what other measures need to be done ♣ Ex. Patient on diuretic therapy needs potassium levels drawn ♣ Ex patient with history of HTN, may need vasoactive drugs to maintain BP during surgery ♣ Ex. Patient with prosthetic heart valve may need prophylactic antibiotics to reduce endocarditis risk ♣ Venous thromboembolism (VTE) prophylaxis • TED hose and SCDs • Respiratory system o Inquire about recent airway infections ♣ Procedure could be cancelled because of increased risk of laryngo/bronchospasm, decreased SaO2, or problems with respiratory secretions. o History of dyspnea, coughing, or hemoptysis reported to operative team (ACP and surgeon) o Smokers should be encouraged to stop smoking 6 weeks before procedure ♣ Decreases risk of complications during and after surgery o Sleep apnea, obesity, and airway deformities affect respiratory function should be noted. ♣ Ex. People with sleep apnea may need to bring equipment ♣ Baseline pulmonary function tests and arterial blood gases may be ordered preoperatively. o COPD or asthma ♣ Asthma – ask about inhaled or oral steroids and triggers ♣ High risk for atelectasis and hypoxemia • Nervous system o Evaluation of neurologic functioning ♣ Inquire about any history of strokes, transient ischemia attacks, spinal cord injuries, myasthenia gravis, Parkinson’s disease, and multiple sclerosis along with any treatment. ♣ Assess the patient’s ability to respond to questions, follow commands, and maintain orderly thought patterns. ♣ Vision or hearing loss can influence results ♣ Record the ability to pay attention, concentrate, and respond appropriately. ♣ Cognitive deficits can affect informed consent and cause adverse outcomes during and after surgery ♣ Older person’s baseline cognitive function is crucial for intraoperative and postoperative evaluation • Older adults are more prone to adverse outcomes because of stressors like: • Dehydration, hypothermia, anesthesia • Can cause emergence delirium, which is a condition that may be falsely labeled as senility or dementia. • Genitourinary system o History of urinary or renal diseases ♣ Chronic kidney disease and repeated UTIs ♣ Present state and current treatment? o Renal dysfunction contributes to ♣ Fluid and electrolyte imbalances ♣ Increased risk of infection ♣ Impaired wound healing ♣ Altered response to drugs and their elimination o Renal function tests – BUN and creatinine o Note problems voiding, and inform operative team ♣ Male- enlarged prostate that could effect catheterization o Assess women for possibility of pregnancy ♣ Most places require pregnancy test ♣ Maternal and fetal exposure to anesthetic in the first trimester should be avoided. • Hepatic system o Liver is involved in glucose homeostasis, fat metabolism, protein synthesis, drug and hormone metabolism, and bilirubin formation and excretion o Liver detoxifies many anesthetics and adjunctive drugs o Hepatic dysfunction may increase risk of postoperative complications ♣ Clotting abnormalities and adverse reaction to drugs o Consider risk for liver disease if there is a history of jaundice, hepatitis, alcohol abuse, or obesity • Integumentary system o History of skin problems o Assess the skin especially at the incision site for rashes, breakdown, or other issues. o History of pressure ulcers ♣ Extra padding during procedure ♣ Affects postoperative healing o Body art such as tattoos, piercings are common ♣ When possible avoid pigmented area for injections, blood draws, and IV sites. • Musculoskeletal system o Identify joints affected with arthritis o Mobility restrictions may affect positioning and ambulation intra and post op. ♣ Any mobility aids should be brought with patient on day of surgery. o Report problems affecting neck or lumbar spine to ACP ♣ Neck - can affect airway management ♣ Spinal anesthesia delivery may be difficult if patient cannot flex spine • Endocrine system o Patients with diabetes mellitus are especially at risk for ♣ Hypo/hyperglycemia – monitor blood glucose and get a baseline • Check with ACP to see if patient should take insulin on the day of surgery. ♣ Ketosis ♣ Cardiovascular alterations ♣ Delayed wound healing – glycosylated vessels ♣ Infection o Thyroid dysfunction ♣ Surgical risk because of alterations of metabolic state ♣ Baseline labs ♣ Check with ACP about drug administration o Addison’s ♣ Crisis or shock can occur if a patient abruptly stops taking steroids ♣ Stress of surgery may require additional IV steroids Case study continued… • Considering her diabetic history, what assessment is important for J.D. the morning of surgery? • Endocrine system – blood sugar and insulin treatment • Glucose done in the morning and insulin done by anesthesiologist • Thyroid lab tests • Immune system • Patients with history of compromised immune system or use of immunosuppressive drugs record it. • Corticosteroids used in immunosuppressive may be tapered before surgery. • Delayed wound healing and Increased risk for infection in the immunosuppressed patients • Patient with acute infections (upper respiratory, sinusitis, influenza) usually postpone surgery • Patient with chronic infections (hepatitis B or C, AIDS, or TB) may still have surgery • Take infection control precautions to protect the patient and the staff • Fluid and electrolyte status • Vomiting, diarrhea, or preoperative bowel preps can cause imbalances ♣ Ex. Planned surgery for a patient with cholecystitis who has been vomiting for several days • Identify drugs that alter F and E status such as diuretics • Evaluate serum electrolyte levels before surgery • NPO status ♣ Surgery delay may also lead to dehydration ♣ Patients with or at risk for dehydration may require additional fluids and electrolytes before surgery • Older adults are high risk for imbalances ♣ There is a narrow margin for over-hydration and under-hydration • Nutritional status • Deficits include overnutrition and undernutrition ♣ Provide extra padding to underweight patients to prevent pressure ulcers ♣ May be protein and vitamin A, C, and B deficient • If severe it could postpone surgery because they are essential for wound healing • Supplement protein may be given to malnourished • OLDER ADULT is often at risk ♣ Identify dietary habits that may affect recovery (e.g., caffeine) • Caffeine headache is often confused with spinal headaches if the preoperative data is not recorded. • Give caffeine postoperative to these patients when possible • Obesity ♣ Stresses cardiac and pulmonary systems ♣ Notify the OR so they can get special equipment ♣ Makes access to the surgical site and anesthesia administration more difficult ♣ Increased risk of wound dehiscence, infection, and incisional hernia ♣ Slower recovery from anesthesia because adipose tissue is vascular so the inhalants are absorbed in the adipose tissue and leave the body more slow. ♣ Slower wound healing Nursing Assessment: EXAM • Complete a physical examination prior to surgery • Document relevant findings and share with the perioperative team • Obtain and evaluate results of laboratory tests & make sure they are in chart • Monitor blood glucose for patients with diabetes • Antiplatelet requires blood coagulation studies • Diuretic therapy requires potassium level • Methicillin-resistant staphylococcus aureus – may be given prophylaxis antibiotics Case study continued… • What teaching should be given to J.D. before the day of surgery? • Review of what happens • What does she need to know on the day of surgery? • Reinforce pre-operative education • Answer any questions • Inform of preoperative IV • Pain medication – make sure they ask before pain gets to severe • Describe the operating room • J.D. signs her consent in the presence of the surgeon in his office before the day of surgery. • Informed consent – the nurse should verify consent is signed, witnessed and in chart • Husband does not have to agree • J.D. reports to the outpatient ambulatory surgical center on the day of her surgery. • How will you help to get her ready for the OR? Nursing Management • Preoperative teaching may be minimal or extensive • It increases patient satisfaction and can reduce fear, anxiety, and stress • May decrease complication, length of stay, and recovery time after discharge • Teaching must be informative and based on patient safety after discharge with included written material to reinforce plan to the caregiver • Discharge teaching is required for all patients. • Anxiety and fear may limit the patient’s learning ability • 3 TYPES OF PREOPERATIVE TEACHING (patient dependent) • Sensory – patient find out what they will see, hear, smell, and feel during surgery. • Ex. May tell them to OR will be cold, but they can ask for a blanket; the lights in the OR are bright; or many unfamiliar sounds and smells • Process – may not want specific details but just the general flow of what is going to happen. • Ex. The patient will be transferred to the holding area, visited by the nurse and ACP before transfer to the OR, and waking up in the PACU. • Procedural – patients desire details that are more specific. • Ex. An IV line will be started while the patient is in the holding area and the surgeon will mark the operative area with an indelible marker to verify the surgical site. • Share the teaching to the postoperative nurse so learning can be evaluated and to avoid duplicated teaching • General surgery information • All patients should be taught deep breathing, coughing, and early ambulation and WHY they are doing it. • Contraindicated surgeries include: craniotomy and tonsillectomy • Inform the patients and caregivers if tubes, drains, monitoring devices, or special equipment will be used after surgery • Also educate how to use the incentive spirometer, PCA pumps, and how to rate pain • Also include in specific surgery information • Ambulatory surgery information • Education should take place before the day of surgery • NPO status is important • Prevents aspiration and postoperative N/V • If not followed, surgery could be postponed or cancelled • Legal preparation for surgery • Making sure all forms are signed and are present in the patient’s chart • Making sure the patient and caregiver understand what is going to happen. • Consent forms: surgery and blood transfusion • Surgeon is responsible for obtaining the informed consent but the nurse is the patient advocate making sure they really understand • The consent can be withdrawn at any time even after signed. • True medical emergency may override an informed consent • The next of kin can give consent, but if not reachable the surgeon can make the decision to treat if it is life threatening • In this case the nurse needs to complete an even report because it is an occurrence that is inconsistent with routine agency practice. • Day-of-surgery preparation • Final preoperative teaching, assessment, and report of pertinent findings • Make sure all preoperative orders are done and chart is complete • Verification of signed consent • Labs • History and physical examination • Baseline vitals • Proper skin preparation • Completed nursing notes and surgical site is identified and marked by surgeon ***patient should agree • Hospital gown • Patient should not wear any cosmetics • Observation of skin color is important • Remove nail polish for pulse oximeter • Valuables are returned to family member or locked up • Dentures, contacts, glasses, prostheses are removed • Hearing aids are left in the patient’s ear. • Identification and allergy bands on wrist • Encourage the patient to void before drugs are given and before transfer to OR. • This prevents involuntary elimination and urinary retention Preoperative Medications • PO medication with a small sip of water 60 to 90 minutes before surgery (unless told otherwise) • Subcutaneous injections and IV drugs are usually given to the patient after arrival in the preoperative holding area or OR. • INFORM THE PATIENT ON WHAT TO BE EXPECTED (DROWSINESS) • Benzodiazepines – sedative and amnesic properties • Anticholinergics – reduce secretions • Opioids – decrease pain and intraoperative anesthetic requirements • Antiemetics – decrease N/V • Antibiotics • Patients’ that have prosthetic heart valves to prevent endocarditis • Patient with previous joint replacements • Patient undergoing surgery with wound contamination is a potential risk (GI surgery) • Most often given IV and are usually started preoperatively (30 to 60 minutes before incision) • β-Adrenergic blockers (β-blockers) – control BP or reduce the chances of MI and cardiac arrest in patient with HTN and/or CAD • Insulin – patients with DM to control blood glucose • Eye drops – for patient undergoing cataract or other eye surgery • Transportation to the OR • Record method of transport (stretcher or wheelchair) and the person who transported the patient • Provide communication “handoff” • Situation • Background • Assessment • Recommendation • Caregivers directed to waiting room • Special concerns • Culturally competent care • Cultures often determines one’s pain, family expectations, and ability to verbally express needs • They may want family to be included in any decision makings • Get a translator if needed • Geriatric considerations (65 or older) • Common procedures: cataracts, coronary or vascular procedures, prostate surgery, herniorrhaphy, cholecystomy, and joint repair or replacement. • Older adult may view the hospital as a place to die or a stepping-stone to the nursing home. HELP DECREASE ANXIETY AND FEARS • Risks associated with anesthesia and surgery increase in older adults. • It relates normal aging process that compress the organ function, reduce reserve capacity, and limit the body’s ability to adapt to stress • Obtain a H&P, preoperative lab tests, ECG, and a chest xray to help with anesthesia planning • May have sensory deficits • Access and record baseline sensory and cognitive function • a legal representative of the patient may need to be present to provide consent for surgery if the patient cannot sign. • CAREGIVER SUPPORT IS CRITICAL IN THE CONTINUITY OF CARE FOR THIS POPULATION. A 68-year-old male scheduled for a herniorrhaphy at an ambulatory surgical center expresses concern that he will not have enough care at home and asks if he can stay in the hospital after the surgery. The best response by the nurse is • “Who is available to help you at home after the surgery?” • Rationale: Ambulatory surgery patients are discharged on the day of surgery. The nurse should determine and anticipate what level of care is needed after the surgery. The nurse would be able to provide instructions to both the patient and the caregiver related to the patient’s needs after surgery. Preoperative instruction that is appropriate for all patients includes • Physical procedures or preparation required before surgery • Rationale: Not all patients will deep breath and cough after surgery (such as after cranial surgery) or need to be NPO (nothing by mouth). Detailed instructions about the procedure may increase anxiety and are not usually helpful to the patient. Patients should have instruction on physical procedures or preparation required before surgery. Anticipatory guidance decreases anxiety and fear. Intraoperative Care Case Study • M.C., a 56-year-old male, comes to the surgical suite with his girlfriend the morning of his scheduled surgery to replace his left knee. • He has a diagnosis of osteoarthritis of his left knee, as well as a history of hypertension. Physical Environment • Department layout • Surgical suite is a controlled environment designed to minimize the spread of pathogens and allow a smooth flow of patients, staff, and equipment needed to provide safe patient care. • Divided into three areas: • Unrestricted area • Where people in street clothes can interact with those in surgical attire • Includes points of entry for patients (holding areas), staff (locker room), and information (nursing station or control desk) • Semi-restricted • Includes the surrounding support areas and corridors. • Only authorized staff are allowed • All staff need to wear surgical attire and cover head and facial hair • Restricted • Masks are required to supplement surgical attire • Ex. The OR, scrub sink, and sterile core • Holding area- identify and assess the patient before transferring to the OR. • Surgical Care Improvement Project (SCIP) measures to implement here (GOAL IS TO PREVENT COMPLICATIONS FROM SURGERY) • Drug administration • Patient warming • Application of sequential compression devices (SCDs) • Minor procedures (ex. Inserting IV catheters) • National Patient Safety Goals (NPSGs) require a pre-procedure verification process, including: • Verification of relevant documentation (H&P, signed consent forms, nursing and pre-anesthesia assessment) • Required blood products, implants, devices, and special equipment • Diagnostic and radiology test results • Procedure site marked by surgeon (if possible with patient’s involvement) Operating Rooms o Geographically, environmentally, and aseptically controlled o Restricted inflow and outflow of personnel o Preferred location is next to PACU and surgical ICU o Filters o Controlled airflow o Positive air pressure o UV lighting – it reduces that number of microorganisms o No dust-collecting surfaces o Materials resistant to corroding effects of strong disinfectants o Ensure proper functioning and electrical safety of equipment o The communication system provides a mean for the delivery routine and emergency messages - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Clinical Manifestations of Disorders of the Ear A. Pain (Otalgia) B. Hearing Loss C. Vertigo – sense of movement/spinning around the person – stimulated by head movement D. Dizziness E. Nystagmus – abnormal eye movement – twitching of the eyeball – blurring of vision with head/eye movement F. Tinnitus G. Ear Drainage (Otorrhea) Subjective Data ♣ Past health history o Frequency of acute middle ear infections (otitis media) o Surgical procedures o Perforations of the eardrum o Drainage - Otorrhea o History of mumps, measles, or scarlet fever o Head injuries o Food and environment allergies o Patient stated symptoms ♣ Medications o Ototoxic – aminoglycosides, NSAIDs, salicylates, antimalarial, chemo, diuretics o Aspirin amount and frequency – can cause tinnitus ♣ Surgery o Myringotomy - ventilation holes placed in tympanic membrane o Tympanoplasty – surgical repair of tympanic membrane o Tonsillectomy o Adenoidectomy ♣ Elimination pattern ♣ Onset of hearing loss ♣ Measures by patient to preserve hearing – ear plugs ♣ Alcohol, sodium, and supplement intake - effects amount of endolymph in inner ear ♣ Activity-exercise pattern ♣ Sleep-rest pattern ♣ History of teeth grinding Physical Exam and Diagnostic Tests • Inspection and palpation of external ear and tympanum • Tests for Auditory Acuity (Weber and Rinne, Audiometry – hearing acuity, Tympanogram) • Tests for Vestibular Function (Romberg, Electronystagmography, Platform posturography) • Noninvasive tests: CT, MRI, X-ray Use of Otoscope • • Up and back • Select speculum slight smaller than ear canal • Hold while stabilizing with fingers on patient’s cheek Normal Eardrum • • Trauma o Mastoiditis • Causes o Inflammation of the mastoid resulting from repeated middle ear infections (otitis media) o Acute mastoiditis is rare R/T antibiotics o Chronic mastoiditis leads to cholesteatoma- a cyst in the middle ear or mastoid system • Diagnosis o Symptoms o Otoscopic exam o Culture of drainage o Sinus x-ray, MRI, CT scan • Clinical Manifestations o Postauricular pain and tenderness o Otorrhea: drainage o Mastoid area red and edematous o Fever, headache o Otoscope- cholesteatoma: benign mass of epithelium cells and cholesterol ♣ Enlarges and can destroy adjacent bones (ossicles) unless surgically removed • Collaborative Care o Otic and systemic antibiotics o Possible evacuation of drainage and debris o Tympanoplasty o Mastoidectomy – removes infection portions of mastoid bone o Analgesics • Nursing Management o Education on treatment plan o Post op management following tympanoplasty with or without mastoidectomy ♣ Impaired hearing to be expected – packing in ear Tympanoplasty • Chronic otitis media- common surgery • Surgical reconstruction of a perforated tympanic membrane, can also restore inner ear structures • Outpatient • Improve hearing • Nursing management • Post-op teaching • Position flat or on side with operative side up • Change cotton ear packing daily • Assess amount and type of drainage • Reduce n/v, dizziness • Pre and Post-Op Care • No aspirin for 1 week prior • Pre and post op audiograms and tympanograms • Post op, lie on nonoperative ear • Antibiotics • Keep packing in ear • Avoid excessive exercise • Sneeze with mouth open, blow nose one nostril at a time • No airplane travel for one month Ostosclerosis • A hereditary autosomal dominant disease – most common cause of hearing loss in young adults • New abnormal spongy bone fixates the stapes • The stapes can’t vibrate and sound is not conducted • Common in white women and worsened by pregnancy • Clinical Manifestations • Progressive conductive hearing loss • Tinnitis • Bone conduction is better than air on the Rinne test • Audiogram indicates conductive hearing loss • Otoscope examination – reddish blue tympanum = Schwartz’ sign • Vascular and bone changes within the middle ear • Rinne – tuning fork test – hearing by bone conduction • Audiogram – air conduction • Rinne + Audiogram = good bone conduction and poor air conduction = air-bone gap • Difference of 20-25 dB between air and bone = osteosclerosis • Collaborative Treatment • 1. Fluoride supplement po with Vit D and Calcium may mature spongy bone growth • 2. Amplification: hearing aids • 3. Surgical- stapedectomy with graft or prosthesis – conscious sedation Meniere’s Disease • Usual onset 30-60 years old • Every 5 of 100 persons • Cause is unknown o Trauma o Recent viral infection o Allergies o Genetic predisposition • Aural: feeling of fullness in the ear • S&S: sudden attacks of vertigo, tinnitus, hearing loss, nausea, vomiting • After attack: vertigo 2-4 hrs, dizziness, unsteadiness, gait changes, depression, moody, VS WNL, hearing loss • Disorder that affects both vestibular and auditory function • Caused by excess endolymph in the vestibular and semicircular canals • Remission and relapses without apparent causes • Clinical Manifestations o Episodic incapacitating vertigo o Tinnitis or a roaring sound o Fluctuating progressive sensorineural hearing loss o Feeling pressure or fullness in the ear (aural) o Attacks increase in frequency and symptoms • Diagnosis o Diagnosis: ♣ History and physical ♣ Diagnostic testing • Audiometric tests – speech discrimination, tone decay • Vestibular tests – caloric test, positional test – Romberg • Electronystagmography • Neurologic exam • Glycerol test • Collaborative Care o Acute Attacks ♣ Drug therapy • Antihistamine • Anticholinergics • Benzodiazepines • Antiemetics • Antivertigo drugs ♣ Bedrest o Non-acute management ♣ Diuretics ♣ Antihistamines ♣ Calcium channel blockers ♣ Antivertigo drugs ♣ Benzodiazepines ♣ Low sodium diet, restrict caffeine, alcohol, nicotine, foods with MSG • Nursing Management o Safety o Potential hearing loss o Fluid and electrolyte balance o Minimize vertigo o Minimize modifiable stressors o Avoid flickering lights/watching TV o Sudden head movement • Surgical Intervention o Indications ♣ Frequent attacks that incapacitate ♣ Quality of life is affected ♣ Possible loss of job o Options ♣ Endolymphatic shunt ♣ Vestibular nerve resection ♣ Labyrinthotomy ♣ Labyrinthectomy Acoustic Neuroma • Slow growing benign tumor of the 8th cranial nerve • Early diagnosis important – can grow and press on trigeminal and facial nerves and arteries with internal canal • Develops in the internal auditory canal • Presses on the nerve, sending false signals to the brain • Equal in men and women at middle age – between 40 and 60 • Usually unilateral, reduced touch sensation in posterior ear canal, unilateral tinnitus, vertigo (intermittent) • Collaborative Treatment o Dx- MRI, CT o Treatment- surgical removal with a neurosurgeon and neurologist o Preserve facial nerve function – stereotactic radio-surgery o Approach depends on if there is hearing loss o Complications- facial nerve damage, cerebrospinal fluid leak, infection, cerebral edema ♣ Large tumors (larger than 3mm ) and surgery can leave hearing loss and facial paralysis Types of Hearing Loss • • Ototoxic Mediations o Damage the vestibulocochlear nerve (eighth cranial nerve) o Cause hearing loss, tinnitus or disturbances in equilibrium o Examples: aspirin, aminoglycosides, furosemide, etc. • Conductive Hearing Loss • Ear Obstructions - cercumen • Infection-Otitis Media with effusion (fluid), Mastoiditis • Trauma – perforation of the tympanic membrane • Otosclerosis • Narrowing on the external ear canal • Speaks softly because can hear their own voice, and can hear better in a noisy environment • Audiogram – better hearing through bone than through air conduction o Hearing loss greater than 40-50 dB – hearing aid Sensorineural Hearing Loss ♣ Presbycusis • Hearing loss due to aging • Causes • Aging process • Injury to hair cells of organ of Corti • Atrophy to lymph-producing cells, and blood vessels in wall of cochlea interrupting nutrients • Changes • External Ear: incr. cerumen; incr. hair growth; loss of elasticity • Middle Ear: atrophy of tympanic membrane • Inner Ear: hair cell degeneration; neuron degeneration; calcification of ossicles; vestibular apparatus changes. • Brain: decline in ability to filter sounds • Assessment Findings • External Ear: impacted ear canal; visible hair; collapsed ear canal. • Middle Ear: Conductive hearing loss • Inner Ear: diminished sensitivity to high-pitched sounds; impaired speech reception; alteration is balance and body orientation. • Brain: sensitive to loud noises, inability to hear in loud environments • Sudden Hearing Loss – sudden, unexpected loss of hearing (usually in one ear) – medical emergency • Congenital • Noise-induced • Benign and Malignant Tumors • Meniere’s Disease • Vaccines – MMR – Rubella first 8 weeks of pregnancy – avoid pregnancy 3 months after vaccines, test for Abs • Ototoxic substances Sensorineural vs. Conductive Hearing Loss • Sensorineural o Impaired function of inner ear or vestibulocochlear nerve (CN VIII) o Causes: hereditary, trauma, infection, immune disease, DM o Sounds are muffled – audiogram = loss of 2000-4000 dB o Hearing aid may only make sounds louder, not clearer • Conductive o Outer or middle ear conditions prevent transmission of sound via air to inner ear. o Causes: otitis media, mastoiditis, impaction, foreign bodies, otosclerosis o Presence of bone-air gap o Person speaks softly o Find cause and treat. o Hearing aid Cochlear Implant • Profound sensorineural bilateral hearing loss – ideal = loss of hearing after acquiring speech and language • Stimulates the auditory nerve • The microphone and signal processor is outside the body- implanted electrodes • 1 year, adult with profound hearing loss, extensive rehab, MRI will inactivate the device • Nursing Measures to Enhance Communication with Hard of Hearing • Speak normally and slowly • Do not over exaggerate facial expressions. • Use simple sentences • Rephrase: use different words • Do not shout • Do not cover your mouth when speaking • Maintain eye contact. • Draw attention with hand movements • Avoid careless expression • Avoid distracting environments [Show More]
Last updated: 2 years ago
Preview 1 out of 130 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jul 04, 2020
Number of pages
130
Written in
Additional information
This document has been written for:
Uploaded
Jul 04, 2020
Downloads
0
Views
169