*NURSING > EXAM > NR 509 APEA Cardio (updated) – Chamberlain College of Nursing | NR 509 APEA Cardio (updated) (All)
NR 509 APEA Cardio (updated) – Chamberlain College of Nursing | NR 509 APEA Cardio (updated)
Document Content and Description Below
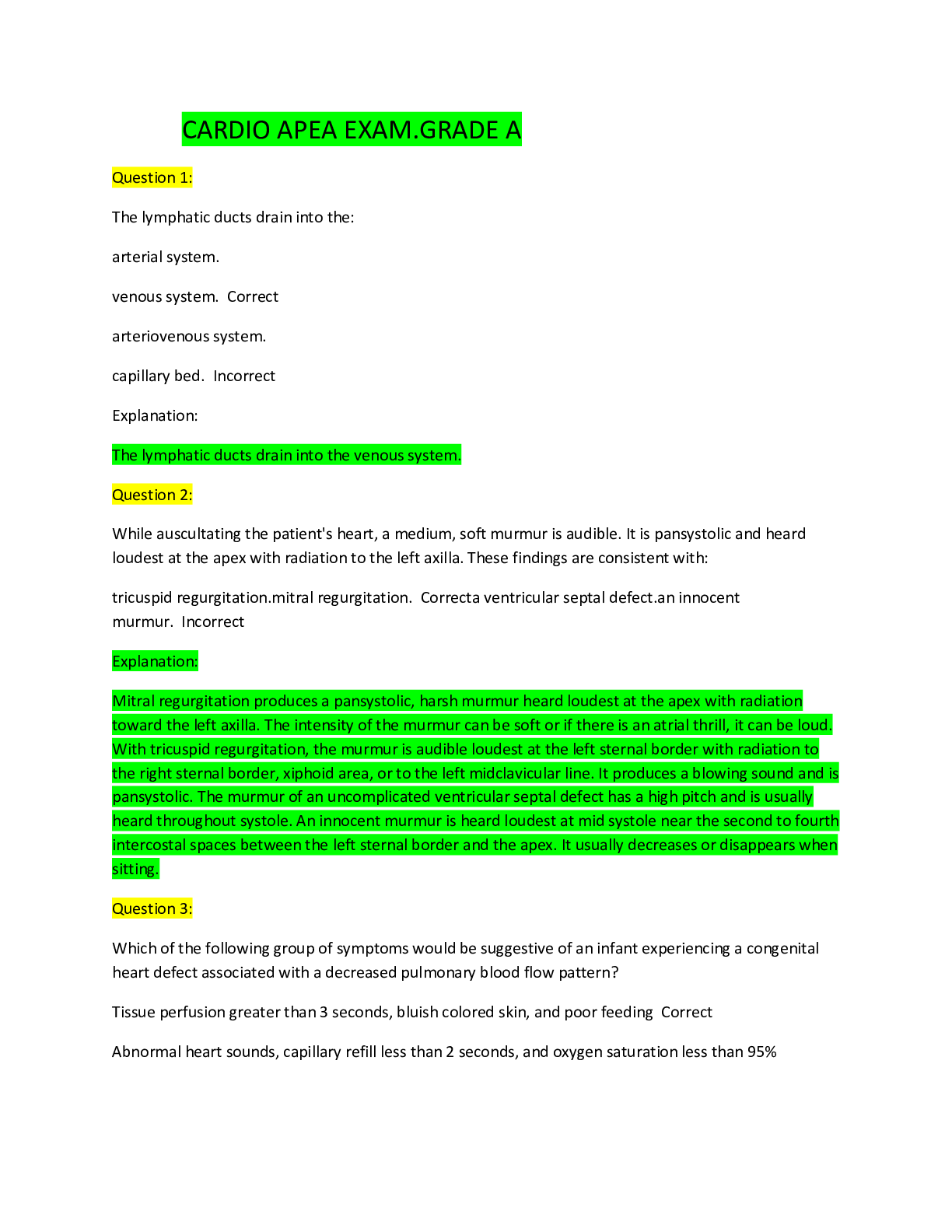
NR 509 APEA Cardio (updated) – Chamberlain College of Nursing Question 1: The lymphatic ducts drain into the: arterial system. venous system. arteriovenous system. capillary bed. In ... Explanation: The lymphatic ducts drain into the venous system. Question 2: While auscultating the patient's heart, a medium, soft murmur is audible. It is pansystolic and heard loudest at the apex with radiation to the left axilla. These findings are consistent with: tricuspid regurgitation.mitral regurgitation. a ventricular septal defect.an innocent murmur. In Explanation: Mitral regurgitation produces a pansystolic, harsh murmur heard loudest at the apex with radiation toward the left axilla. The intensity of the murmur can be soft or if there is an atrial thrill, it can be loud. With tricuspid regurgitation, the murmur is audible loudest at the left sternal border with radiation to the right sternal border, xiphoid area, or to the left midclavicular line. It produces a blowing sound and is pansystolic. The murmur of an uncomplicated ventricular septal defect has a high pitch and is usually heard throughout systole. An innocent murmur is heard loudest at mid systole near the second to fourth intercostal spaces between the left sternal border and the apex. It usually decreases or disappears when sitting. Question 3: Which of the following group of symptoms would be suggestive of an infant experiencing a congenital heart defect associated with a decreased pulmonary blood flow pattern? Tissue perfusion greater than 3 seconds, bluish colored skin, and poor feeding Abnormal heart sounds, capillary refill less than 2 seconds, and oxygen saturation less than 95% Capillary refill less than 2 seconds, tissue perfusion less than 3 seconds, and oxygen saturation greater than 95% Poor feeding, audible heart murmur, and oxygen saturation greater than 95% Explanation: Infants with defects resulting from decreased pulmonary blood flow have cyanosis because of desaturated blood entering systemic circulation and/or because of the inability to get blood to the lungs. Tetralogy of Fallot (TOF), pulmonary atresia and tricuspid atresia all fall in this category and are considered cyanotic defects. Due to the ventricular septal defect in TOF, the absence of the tricuspid valve or pulmonary valve in tricuspid and pulmonary atresia, one should hear abnormal heart sounds either due to the murmur in TOF or single heart sounds of S1 or S2 in pulmonary atresia or tricuspid atresia. Usually these infants have activity intolerance and therefore, experience failure to thrive because of their inability to consume enough formula to gain weight appropriately. Capillary refill is usually prolonged due to poor oxygenation and poor perfusion secondary to the defect as well as the O2 sats being lower than normal, sometimes even in the 80% range. Question 4: Right atrial pressure can be determined by: palpating the carotid pulse. In identifying the pulsations of the right jugular vein. analyzing the arterial blood gases. assessing for dependent edema. Explanation: Jugular venous pressure reflects pressure in the right atrium and is best assessed from pulsations in the right internal jugular vein. This is an indicator of cardiac function and right heart hemodynamics. Palpating the carotid artery denotes arterial pressure; analyzing blood gases reflects the status of the arterial blood. Assessing for dependent edema is a reflection of heart failure and poor venous return and not atrial pressure. Question 5: When assessing the heart rate of a healthy 13-month-old child, which one of the following sites is the most appropriate for this child? Apical pulse at the 5th intercostal space right midclavicular line Apical pulse between the 3rd and 4th intercostal space in the left midclavicular line Apical pulse to the right of the midclavicular line in the 3rd intercostal space Apical pulse in the 5th intercostal space left midclavicular line In Explanation: The apical pulse in a 13-month-old is auscultated for a full minute between the 3rd and 4th intercostal space to the left of the midclavicular line. The only time one would auscultate the right midclavicular line would be if the child had situs inversus or dextrocardia. Question 6: The infraorbital or maxillary, buccinator, and supramandibular lymph nodes drain lymphatic fluid from the: palpebral conjunctiva and the skin adjacent to the ear within the temporal region. eyelids, the conjunctiva, and the skin and mucous membrane of the nose and cheek. mouth, throat, and face. In posterior part of the temporoparietal region. Explanation: The facial lymph nodes (infraorbital or maxillary, buccinator, and supramandibular) drain lymphatic fluid from the eyelids, the conjunctiva, and the skin and mucous membranes of the nose and cheek. Tonsillar, submandibular, and submental nodes (anterior and superficial cervical lymph nodes) drain lymphatic fluid from portions of the mouth, throat, and face. The preauricular nodes drain lymphatic fluid from the palpebral conjunctiva as well as the skin adjacent to the ear within the temporal region. The posterior auricular lymph nodes drain lymphatic fluid from the posterior part of the temporoparietal region. Question 7: The external iliac lymph nodes drain lymphatic fluid from the following areas except the: urinary bladder. prostate. uterus. gluteal region. Explanation: The external iliac lymph nodes receive lymphatic fluid from the umbilicus, urinary bladder, prostate or uterus, and the upper vagina. The internal iliac lymph nodes receive lymphatic fluid from all pelvic viscera, deep part of the perineum, and the gluteal region. Question 8: The amplitude of the pulse in a patient in cardiogenic shock would most likely appear: bounding. thready. normal. as a bruit. Explanation: The amplitude of the pulse correlates with pulse pressure. Small, thready, or weak pulses occur in patients in cardiogenic shock. Bounding pulses are seen in patients in aortic insufficiency. A bruit is not typically associated with pulse amplitude. It is associated with stenosis or turbulent arterial blood flow. Usually the presence of a bruit requires further investigation and is not in itself diagnostic. Question 9: When auscultating the heart for aortic insufficiency, ask the patient to: lie supine and inhale. exhale while standing. turn to the left side and breath deeply. sit up, lean forward, and exhale. Explanation: To bring the left ventricular outflow tract closer to the chest wall to listen for aortic insufficiency, ask the patient to sit up, lean forward, and exhale. Question 10: The horizontal superficial inguinal lymph nodes are located in the anterior thigh below the inguinal ligament and drain lymphatic fluid from all of these areas except: lower abdomen. buttock. In testes. lower vagina. Explanation: The horizontal superficial inguinal nodes lie in a chain high in the anterior thigh below the inguinal ligament. They drain the superficial portions of the lower abdomen and buttock, the external genitalia (but not the testes), the anal canal and perianal area, and the lower vagina. Question 11: When auscultating the point of maximal impulse (PMI), apex of the heart, in an adult, the stethoscope is placed at the: third intercostal space to the left of the midclavicular line. fifth intercostal space to the left of the midclavicular line. fourth intercostal space to the right of the midclavicular line. fifth intercostal space to the right of the midclavicular line. In Explanation: To auscultate the apex of the heart in an adult, the proper placement of the stethoscope should be at the fifth intercostal space to the left of the midclavicular line. Question 12: Deep cervical lymph nodes drain lymphatic fluid from the: head and neck. breasts. mouth, throat, and face. posterior part of the temporoparietal region. In Explanation: The deep cervical lymph nodes drain all of the lymphatic fluid from the head and neck. Axillary lymph nodes drain most of the lymphatic fluid of the breast. Tonsillar, submandibular, and submental nodes (anterior and superficial cervical lymph nodes) drain lymphatic fluid from portions of the mouth , throat, and face. The posterior auricular lymph nodes drain lymphatic fluid from the posterior part of the temporoparietal region. Question: Which of the following symptoms would necessitate the need for further evaluation in the newborn? Blue hands and feet within an hour after birthBlood glucose level 45 mg/dl.Dusky cyanotic when crying Deep sleep one hour after birth Explanation: An infant who is dusky and becomes cyanotic when crying is showing poor cardiovascular adaptation to extrauterine life and requires further evaluation. Acrocyanosis, blue feet and hands, is not central cyanosis and is an expected finding during the early neonatal life. Normal glucose levels for a newborn are 40-60 mg/dL. Infants enter the period of deep sleep or decreased activity when they are about one hour old. Question: Symptoms of acrocyanosis in the newborn include: bluish color of the tongue.bluish color of the mucous membranes.bluish color of the feet. bluish color of the abdomen. Explanation: Shortly after birth, cyanosis of the hands, feet, and perioral area are common findings and typically resolve in 24 - 48 hours. A blue color around the lips and philtrum is a relatively common finding shortly after birth. The skin in the infant is usually well perfused, and the tongue and mucous membranes in the mouth are pink, a finding that assures that central cyanosis is not present. Question: A heart rate of 100-180 beats per minute in an adult is considered: normal sinus rhythm.sinus tachycardia. supraventricular tachycardia.ventricular tachycardia. Explanation: A normal heart rate in an adult is between 60 / 100 beats per minute. Tachycardia is over 100 beats / minute. Rates that exceed 180 beats / minute are usually supraventricular. Normal sinus rhythm is a measurement of the hearts electrical activity, not mechanical activity. Ventricular tachycardia is rapid and chaotic ventricular activity. Question: Tissue ischemia is usually observed when assessing a patient with peripheral artery disease (PAD). What other symptom could be observed? Peripheral edemaIntermittent claudication. A brownish discoloration to the skin of the affected leg InBounding pulses in the affected leg Explanation: With peripheral vascular disease, arterial peripheral blood flow is impeded resulting in inadequate tissue perfusion and oxygenation. This leads to intermittent claudication, ischemia muscle pain precipitated by a predictable amount of exercise and relieved by rest. Other symptoms include pale cool skin, cyanosis, audible bruits, diminished or absent pulses, and thickened and opaque nails. Usually by the time the symptoms appear, the artery is 75% narrowed. Peripheral edema and brownish discoloration of the skin would be consistent with venous disease. Bounding pulses may reflect hypertension. Question: When performing a cardiovascular assessment on a healthy 2-year-old child: expect to hear a swooshing sound during diastole.place the stethoscope over the fifth intercostal space to the left of the mid-clavicular line.auscultate the heart sounds in all four cardiac areas. expect to hear an S4 sound. Explanation: When performing cardiac assessment on the child, the heart sounds should be auscultated in all 4 cardiac areas: aortic, pulmonic, tricuspid, and mitral areas. In children younger than 7 years of age, the point of maximum impact (PMI) is auscultated at the third or fourth intercostal spaces, and one should not hear swooshing sounds as this would be indicative of a pathological heart murmur, especially if heard during diastole. S4 sound is produced by the atrium forcefully contracting against a stiffened ventricle. It is also a dull, low pitched sound. The presence of S4 usually indicates cardiac disease secondary to a decrease in ventricular compliance caused by either ventricular hypertrophy or myocardial ischemia. Question: A disparity between the brachial and femoral pulses in a 4-month-old could indicate: an atrial septal defect (ASD).Tetralogy of Fallot. Incoarctation of the aorta (COA). tricuspid atresia (TA). Explanation: In coarctation of the aorta (COA), there is a disparity of pulses between the upper and lower extremities due to the narrowing of the descending aorta resulting in decreased blood flow to the lower extremities. The other choices do not present with these findings. - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Question: A patient complains of increased pain in the calf muscles and buttocks especially after walking or riding his bicycle. He states that the pain stops after he sits still for about 2-3 minutes. This condition may be associated with: intermittent claudication. Raynaud's disease.deep venous thrombosis.superficial thrombophlebitis. Explanation: Episodic muscular ischemia induced by exercise, due to atherosclerosis of large or medium-sized arteries, is defined as intermittent claudication. The pain is usually associated with the calf muscles, but also may be in the buttock, hip, thigh, or foot, depending on the level of obstruction. Rest usually stops the pain within a few seconds. Reynaud's disease usually affects the distal portions of the fingers. Deep venous thrombosis (DVT) and superficial thrombophlebitis are venous disorders. With DVT's, the pain feels tight or squeezing and often presents in the calf. Superficial thrombophlebitis is local and presents along the course of a superficial vein . Question: A condition that presents with symptomatic limb ischemia upon exertion is termed: neurogenic claudication.intermittent claudication.atherosclerotic peripheral vascular disease. Raynaud's disease. Explanation: Atherosclerotic peripheral artery disease presents with symptomatic limb ischemia with exertion. Pain or cramping in the legs that occurs with exertion and is relieved by rest is termed intermittent claudication. Pain with walking or prolonged standing, radiating from the spinal area into the buttocks, thighs, lower legs, or feet, may be seen with neurogenic claudication. Raynaud's disease usually presents with numbness or tingling in the distal portions of one or more fingers aggravated by cold or emotional stress. Question: Absent or diminished pulses in the wrist could be indicative of: varicosities.right-sided heart failure.venous insufficiency.arterial occlusive disease. Explanation: Absent or diminished pulses at the wrist are found in arterial occlusive disease such as acute embolic occlusion, in Buerger’s disease, or thromboangiitis obliterans. Varicosities, venous insufficiency, and right-sided heart failure are consistent with venous conditions. Question: In older adults, the presence of heart sound S4 suggests: hypertension. heart failure. Inan aortic aneurysm.aortic stenosis. Explanation: An S4 heart sound occurs when the atria contract and force blood into a left ventricle that is non-compliant. This can be the result of diastolic heart failure, hypertension, infraction, or others. It is known as the "atrial gallop". This is always abnormal. Question: A patient describes chest pain as pressing, squeezing, and tight lasting between 1 and 3 minutes. These symptoms are more characteristic of: myocardial infarction. costochondritis.pericarditis.dissecting aortic aneurysm. Explanation: Myocardial infarction is described as pressing, squeezing, tight, heavy and occasionally burning. Chest pain described as persistent, sharp, and knife-like is characteristic of pericarditis and pleuritic pain. With costochondritis, the pain may be stabbing, sticking, or dull and aching. A dissecting aortic aneurysm is described as ripping and tearing. Question: When auscultating the heart, a scratchy, continuous murmur is audible during atrial systole and ventricular systole and diastole. This finding may be indicative of a: pericardial friction rub. venous hum.patent ductus arteriosus.ventricular septal defect. Explanation: Cardiovascular sounds that extend beyond one phase of the cardiac cycle are considered continuous murmurs. Pericardial friction rubs usually produces a scratchy, scraping sound with a high pitch. They are heard best with the diaphragm and are associated with friction from cardiac movement in the pericardial sac. If they are heard in atrial systole and ventricular systole and diastole, then the diagnosis is made. Venous hums are benign sounds resulting from turbulence in the jugular veins. They can produce a humming or roaring sound and are heard best with the bell of the stethoscope during diastole. Venous hums are common in children and may be present in patients who have anemia or hyperthyroidism. The murmur of a patent ductus arteriosus produces a harsh, machine-like sound and is loudest during late systole. The murmur of an uncomplicated ventricular septal defect has a high pitch and is usually heard throughout systole. Question: The anterior mediastinal lymph nodes drain lymphatic fluid from the: anterior chest wall.upper part of the abdominal wall.thymus, thyroid gland and the anterior part of the pericardium. breasts. Explanation: The anterior mediastinal lymph nodes drain lymphatic fluid from the thymus, thyroid, and the anterior part of the pericardium. The anterior chest wall is drained by the anterior pectoral nodes. These nodes also aid in draining much of the lymphatic fluid from the breast. The axillary lymph node drainage area includes the breasts, upper part of the abdominal wall, the upper part of the back, pectoral region, and upper limbs. Question: To assess the murmur of aortic insufficiency, position the patient: supine.sitting leaning forward. supine with head elevated 30 degrees and turned partly to the left side.standing. Explanation: The preferred position for the patient when assessing an aortic insufficiency murmur is sitting leaning forward. This position moves the heart closer to the chest wall. The other positions are not effective in assessing this murmur. Question: A pediatric patient presents with erythema marginatum, chorea, and a heart murmur. These symptoms are consistent with: Kawasaki Disease.rheumatic heart disease. infectious endocarditis. Insickle cell disease. Explanation: Classic symptoms of rheumatic heart disease include, erythema marginatum, chorea (aimless uncontrollable movement of the extremities), murmur, joint pain, and shortness of breath. These are usually preceded by history of a recent streptococcal infection. Kawasaki disease presents with unexplained fever for five days along with four of these five symptoms: bilateral non-purulent conjunctivitis, cervical lymphadenopathy, edema of the hands and/or feet, strawberry tongue, and a macular rash. Endocarditis presents with fever, lethargy, petechiae, neurological involvement, Janeway lesions and Osler's nodes. Sickle cell disease may present with several symptoms: chronic hemolytic anemia, delayed growth and development, renal and neurological dysfunction, and retinopathy. Question: When auscultating the heart; S1 sound, is located at the apex of the heart and signifies: closure of the pulmonic and aortic valves.closure of the mitral and tricuspid valves. both ventricles filling rapidly.an increased resistance to ventricular filling. Explanation: S1 sound is heard at the apex of the heart (5ICS MCL) and produces a dull, low-pitched sound ("lub"). It signifies the closing of the mitral and tricuspid valves. The "dub" is the S2 sound and is heard at the base of the heart. It signifies closure of the aortic and pulmonic valves. The S3 sound is heard at the apex and signifies rapid filling of the ventricles. The S4 sound is heard at the tricuspid and mitral areas and signifies an increased resistance to ventricular filling. Question: A patient with cirrhosis develops portal hypertension as indicated by the presence of: splenomegaly. bleeding gums.jaundice.muscle wasting. Explanation: Development of portal hypertension is related to the obstruction to portal blood flow which causes an increase in portal venous pressure resulting in splenomegaly, ascites, and collateral venous channels; para-umbilical and hemorrhoidal veins, cardia of the stomach and into the esophagus. Muscle wasting is seen in cirrhosis but it is related to poor nutritional intake and not to portal hypertension. Jaundice is already present in cirrhosis due to the inability of the liver to conjugate the excessive bilirubin and is not directly related to portal hypertension. Bleeding gums would be related to the insufficient amount of Vitamin K production in the liver. Question: Pain with walking or prolonged standing, radiating from the spinal area into the buttocks, thighs, lower legs, or feet, may be seen with: neurogenic claudication. intermittent claudication.atherosclerotic peripheral vascular disease.Raynaud's disease. Explanation: Pain with walking or prolonged standing, radiating from the spinal area into the buttocks, thighs, lower legs, or feet, may be seen with neurogenic claudication. Pain or cramping in the legs that occurs with exertion and is relieved by rest is termed intermittent claudication. Atherosclerotic peripheral artery disease presents with symptomatic limb ischemia with exertion. Raynaud's disease usually presents with numbness or tingling in the distal portions of one or more fingers aggravated by cold or emotional stress. Question: Why would a newborn with patent ductus arteriosus receive a prostaglandin inhibitor (indomethacin)? To maintain Ductus Arteriosus patencyTo reduce fluid overload on the pulmonary circulation To improve oxygenation of systemic circulation InTo improve contractility of the left ventricle Explanation: Indomethacin is a prostaglandin inhibitor (nonsteroid antiinflammatory drug [NSAID]) and causes constriction of the ductus arteriosus and by closing the ductus. Oxygenated blood is shunted to the systemic circulation and this reduces fluid overload on the pulmonary circulation. The other choices are not actions of indomethacin. The blood is already oxygenated so it does not need to go to the lungs and there is no problem with ventricular contractility. Question: When assessing a 3-year-old African American child, the most likely cause of black, dusky mucous membranes is related to: jaundice. pallor. erythema. cyanosis. Explanation: In dark skinned children, black, dusky mucous membranes are significant for cyanosis. The mucous membranes are the best areas to identify cyanosis in African American children. Erythema is denoted as a dusky red or violet color over the body. The other choices are not characteristic of cyanosis. [Show More]
Last updated: 2 years ago
Preview 1 out of 57 pages
 – Chamberlain College of Nursing.png)
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Aug 23, 2020
Number of pages
57
Written in
Additional information
This document has been written for:
Uploaded
Aug 23, 2020
Downloads
0
Views
54







 – University of the People.png)