PATHOPHYSIOLOGY 370 FINAL EXAM STUDY GUIDE.
Document Content and Description Below
Chapter 1:
PATHOPHYSIOLOGY 370 FINAL EXAM STUDY GUIDE
1. Etiology: study of causes or reasons for a particular injury. Idiopathic (unknown) vs Iatrogenic (unintended/unwanted medical treatment
...
). Risk Factor: a factor that increases the likelihood of disease.
2. Pathogenesis: development or evolution of disease from initial stimulus to ultimate expression of manifestations of the disease.
3. Clinical Manifestations: Signs (objective) vs Symptoms (subjective).
4. Stages and Clinical Course: Latent period (time between exposure of tissue to injurious agent, first appearance of S&S), Prodromal period (indicating onset of disease), Acute phase (disease/illness reaches its full intensity).
5. Acute clinical course: short-lived, may have severe manifestations.
6. Chronic clinical course: may last months to years, sometimes follows an acute course.
7. Treatment implications: understanding the etiology, pathogenesis, and clinical consequences of a particular disorder/disease/illness may determine which treatments could be helpful.
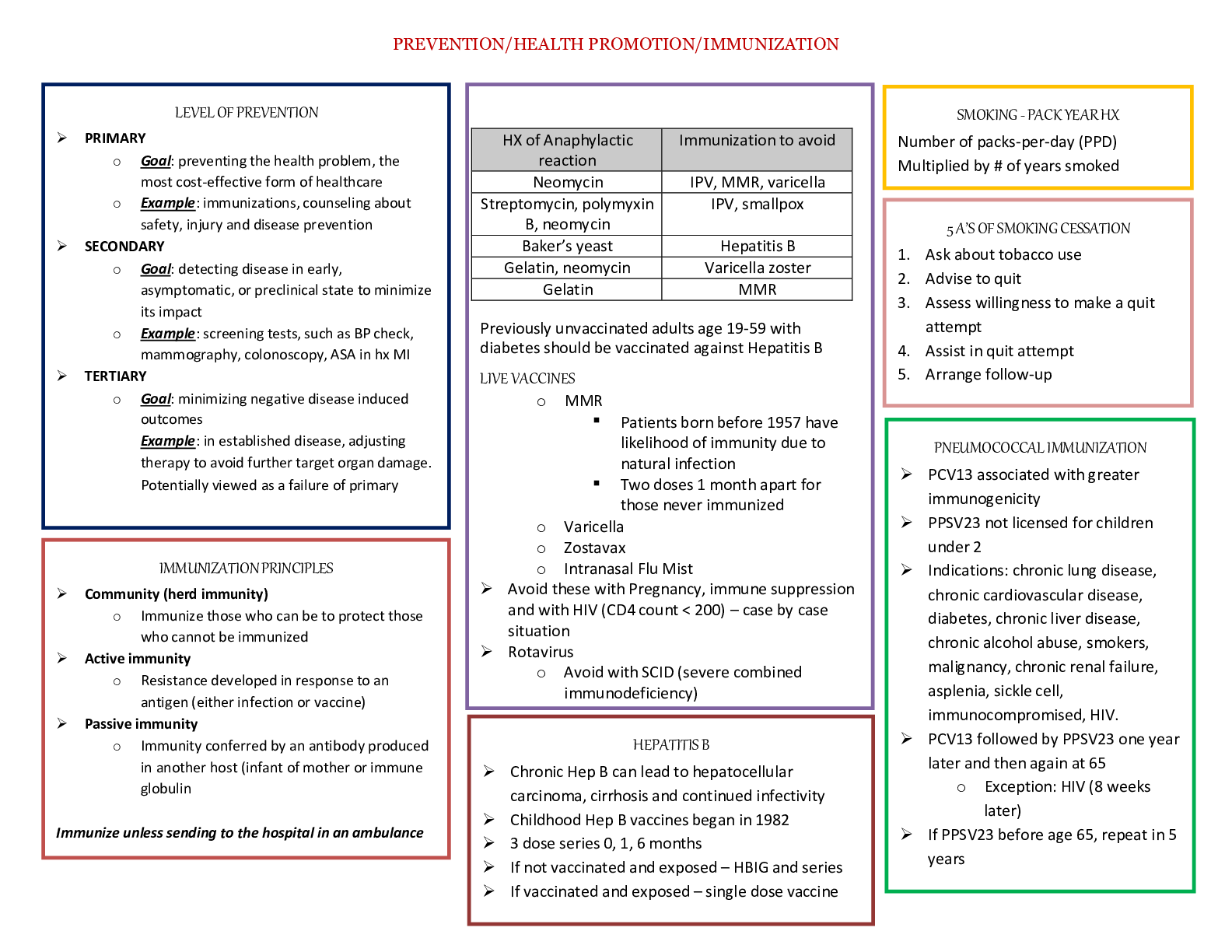
8. Considerations: culture, age, gender, situation, time. 9. Levels of Prevention:
Primary: altering susceptibility or reducing exposure for susceptible persons (vaccination). Secondary: early detection, screening, and management of disease.
Tertiary: rehabilitation, supportive care, reducing disability, and restoring effective functioning.
10. Subclinical: disease that has no recognizable clinical findings. Distinct from a clinical disease which has S&S that can be recognized. Subclinical disease ex. Diabetes, hypothyroidism, RA until they turn into clinical diseases.
Chapter 2:
1. Homeostasis: ideal set point; response: mechanistic, predictable series of orchestrated internal events.
2. Types of parameters to control: osmolarity, temperature, pH, nutrients, water, Na+, Ca2+, oxygen, hormones.
3. Allostasis: ability to adapt to challenges; maintains or reestablishes homeostasis in light of environmental and lifestyle changes.
4. Stressors: agents or conditions that endanger homeostasis (physical, chemical, emotional, biological, social, or cultural; vary in scope, intensity, and duration.
5. Feedback control systems adapt to changes to restore homeostasis.
6. Stress can be beneficial: increase energy and alertness, keeps us focused on the problem at hand.
7. Risk factors: NOT stressors, but conditions or situations that increase the likelihood of encountering a stressor.
8. Han Selye’s GAS:
Alarm Reaction: arousal of CNS begins, fight-or-flight response sympathetic NS involved. Epinephrine, NE, and other hormones are released, causing an increase in HR, contractility, oxygen intake (respiratory rate), and mental activity.
Resistance: activity of the nervous and endocrine systems in an attempt to return to homeostasis. Allostatic state: refers to the activity of various systems in attempting to restore homeostasis.
Exhaustion: point where body can no longer return to homeostasis. Allostatic overload: “cost” of body’s organs and tissues for an excessive or ineffectively regulated allostatic response. Organ damage begins (onset of disease).
9. Other responses: corticotropin-releasing hormone (CRH) production, antidiuretic hormone release (vasopressin), Sympathetic nervous system (SNS) activation and catecholamines (E and NE), renin- angiotensin-aldosterone pathway activation (increase BP, increased blood volume).
10. Stressful stimuli excite receptors which relay to the hypothalamus the stress response is then mediate by E/NE and glucocorticoids (cortisol).
11. SNS stimulation causes vasoconstriction of most blood vessels because of activation of alpha 1 Adrenergic receptor’s by NE.
12. Cortisol: stress hormone. Diverts metabolism from building tissues to supply energy to deal with the stress. Primary glucocorticoid. Promotes appetite. Causes S&S of chronic stress. Increased blood glucose, stronger sympathetic system effect on heart rate.
*Hypothalamus (CRH) Anterior Pituitary (ACTH) Adrenal Cortex (cortisol) alters
glucose, fat, protein metabolism, suppresses inflammatory and immune responses.
13. Antidiuretic Hormone (ADH): vasopressin, causes vasoconstriction, makes kidneys reabsorb water from urine to blood.
14. Fight or Flight Response: rapid response to trauma, emergency. Epinephrine and norepinephrine released. Both attach to adrenergic receptors.
Norepinephrine: causes vasoconstriction and raises BP, reduces gastric secretions, increases night and far vision.
Epinephrine: enhances myocardial contractility, increases HR and CO, causes bronchodilation, increases glucose release from the liver (glycogenolysis).
• Pain, fear, low BP (hypothalamus) SNS activated (SNS neurons)Norepinephrine (adrenal medulla)
epinephrine released into blood heart (increase HR and contractility)/ Blood Vessels (vasoconstrict skin, gut, and kidney) increased BP
15. Renin-Angiotensin-Aldosterone Pathway: activated by sympathetic system, decreased blood flow to kidneys. ANG1: weak vasoconstriction. Angiotensin-converting enzyme (ACE). ANG II: stronger
vasoconstriction, also stimulates the adrenal cortex to release aldosterone. Aldosterone released. Na+/K+ ATPase in nephrons activated (kidneys reabsorb Na+ and H2O, kidneys secrete K+.
• Kidneys release ReninConverts angiotensin to ANG I (ACE)ANG IIAdrenal
CortexAldosteroneKidneysReabsorb Na+ and water (increases blood volume and BP) and secrete K+
16. Endorphins: endogenous opioids- raises pain threshold and produces sedation and euphoria. 17.Oxytocin: produced during childbirth and lactation, associated with bonding and social attachment,
thought to moderate stress response and produce a calming effect.
18. Stress Affects the Immune System: by decreasing immune cell production, decreasing thymus activity, overall stress and cortisol suppresses the immune system.
19. Types of Stress
(1) Physiologic Stress: stress-induced changes in body functions, detected by body’s normal regulatory sensors, the body alters function to restore normal balance. When balance is restored, negative feedback stops the reaction.
(2) Psychosocial Stress: refers to events of psychosocial or social origin which challenge homeostasis. Adverse environments or life experiences (natural disasters, war, loss of job). Position in a social hierarchy, isolation, discrimination. Directly affects the CNS. Turns on the stress responses, even when the body’s internal sensors have not detected imbalance.
(3) Acute Stress: pounding headache, cold, moist skin, stiff neck. Activates neural pathways that mediate arousal, alertness, focused attention, aggression. Can be detrimental.
(4) Chronic Stress: long term. sympathetic activity and cortisol are elevated, complications result from reduced immune response. Long-term exposure can lead to serious health problems because it disrupts most body systems.
20. PTSD: chronic stress, sympathetic system is activated, cortisol levels are decreased, due to life threatening events, less than half of people exposed to traumatic experiences suffer from PTSD.
21. PTSD 3 Symptoms: intrusion (flashbacks), avoidance (emotional numbing, depression), hyperarousal (increased irritability, increased concern over safety, difficulty concentrating. Memory problems, sleep disturbances, excessive anxiety.
22. Adaptation to Stress Determined By: physiologic reserve, time, health status, age, genetic endowment, hardiness, psychosocial factors, nutrition, sleep-wake cycle.
23. Tx of Stress Disorders: relaxation response, imagery, music therapy, massage therapy, biofeedback.
Chapter 4:
1. Reversible Cell Injury
Hydropic swelling: due to accumulation of water. 1st manifestation of most forms of reversible cell injury. Results from malfunction of NA+/K+ pump with accumulation of intracellular Na+. Any injury that results in loss of ATP will also result in swelling: Characterized by large, pale cytoplasm, dilated ER, swollen mitochondria, cells in organs increase in size and weight.
Intracellular Accumulations: excess accumulations of substances. Leads to injury thru toxicity, immune response, taking up cellular space. Characterized by accumulation of excessive amounts of normal intracellular substance, abnormal substances from faulty metabolism synthesis, particles that the cell is unable to degrade. Common site of accumulation= Liver.
2. Cellular Adaptation
Atrophy: cells shrink and reduce function, generally caused by ischemia, nutrient starvation, decreased functional demand, disuse, denervation, and persistent cell injury.
Hypertrophy: increase in cell mass and augmented function capacity; generally caused by increased cellular protein content and increase functional demand.
Hyperplasia: increase in functional capacity related to an increase in cell number due to mitotic division; caused by increase physiologic demand, hormonal stimulation, persistent cell injury, chronic irritation of epithelial cells.
Metaplasia: replacement of one differentiated cell type with another. Fully reversible when injurious stimulate is removed.
Dysplasia: disorganized appearance of cells because of abnormal variations in size, shape, and arrangement. Cause by adaptive effort to persistent injury gone astray. Significant potential to transform into cancerous cells.
3. Irreversible Cell Injury
Necrosis: Cell death, usually due to ischemia or toxic injury. Occurs when injury is too severe. Pain, inflammation, loss of function, elevated serum of enzyme levels.
Coagulative: most common, begins with ischemia, ends with degradation of plasma \membrane.
Liquefactive: liquefaction of lysosomal enzymes, formation of abscess or cyst from dissolved tissue (brain).
Fat necrosis: death of adipose tissue, appears as chalk white area, usually due to trauma or pancreatitis.
Caseous necrosis: characteristic of lung damage secondary to TB, resembles clumpy cheese.
Gangrene: cellular death (necrosis) in a large area of tissue. Due to interruption of blood supply.
Dry Gangrene: form of coagulative necrosis characterized by blackened, dry, wrinkled tissue separated by a line of demarcation from healthy tissue.
Wet Gangrene: form of liquefactive necrosis, found in internal organs, rapidly fatal.
Gas Gangrene: results from infection of necrotic tissue by anaerobic bacteria (Clostridium), characterized by formation of gas bubbles in damaged muscle tissue, can be rapidly fatal.
Apoptosis: programmed cell death. Can occur in response to injury. Severe cell damage increased p53 (triggers cells death). Does not cause inflammation.
4. Ischemia: interruption of blood flow. Causes tissue hypoxia. Results in power failure in the cell. Most common cause of cell injury and injures cells faster than hypoxia alone. Disruption of O2 + accumulation of metabolic waste (lactic acidosis) = cell dysfunction. Can be reversible but not after plasma, mitochondria, and lysosomal membraned are damaged.
5. Nutritional Injury: not having adequate amounts of fats, carbs, proteins, vitamins, and minerals which are essential to normal cell function. May result from poor intake, altered absorption, inefficient cellular uptake, chronic alcoholism, poverty, acute/chronic illness.
6. Infectious/Immunologic Injury: bacteria and viruses. Added injury may occur indirectly b/c immune system was triggered.
7. Chemical Injury: toxic chemicals or poisons.
8. Physical/Mechanical Injury: abrupt change in ATM pressure, electricity, ionizing radiation, extreme change in temperature.
9. Cellular Aging: progressive decline in proliferation and reparative capacity of cells, exposure to environmental factors, DNA damage, accumulation of metabolic damage, inability to adapt.
Chapter 7
1. Cancer: develop from a mutation in a single cell that grows without the control that characterized normal cell growth, do not die off, and may spread to other sites.
2. Neoplasia: “new growth” and implies abnormality of cellular growth. Can be both malignant or benign.
3. Tumor: a mass. Can be malignant or benign.
4. Malignant: cancer
5. Benign: can be easily cured.
6. Epidemiology: Men 1:2 risk, women 1:3 risk. 5-year survival rate: 66%. 1/3 of cancer deaths are attributed to lifestyle factors (tobacco, alcohol, sexual exposure, obesity). Additional risk factors: viruses, radiation, exposure, chemicals, genes, hormones, compromised immune system.
7. Tobacco Use: lung cancer (worst survival rate), pancreatic, kidney, bladder, mouth, esophageal, and cervical cancers.
8. Classification: classified by the tissue or cells it originates from Epithelial tissue: carcinomas
Glandular tissue: adenocarcinomas Connective/Muscle/Bone tissue: sarcomas Brain tissue/Spinal Cord: gliomas Pigment cells: melanomas
Plasma cells: myelomas Lymphatic tissues: lymphomas Leukocytes: leukemia Erythrocytes: erythroleukemia
9. Cell Cycle/Growth Factor Receptors: # of cells produced = # of cells that die. Cells divide only when told to by growth factors which cause stable cells to enter the. Cycle and divide.
10. Growth Factors: attach to receptors an often work by affecting the G proteins turning on enzymes and second messengers to signal the cell to divide.
11. Carcinogen: potential cancer-causing agent
12. Grading vs Staging: stage= describes the size of a tumor and how far it has spread. Grade=appearance of the cancerous cells.
13. Proto-oncogene: the normal genes that code for normal proteins used in cell division
14. Oncogenes: mutated proto-oncogenes (introduced by a retrovirus, lost/damaged DNA sequence, error in replication). * Still codes for the proteins needed for cell division but might produce too much protein, an abnormal protein, protein turns on/of f by itself, protein that should be made by a different cell.
15. Tumor Suppressor Genes: form checkpoint tumor-suppressor proteins that usually stop division of mutated cells. Keep most mutations from developing into cancers. AKA cyclins/cyclin-dependent kinases. Low activity = more cancers.
16. Multistep Nature of Carcinogenesis: Initiation (initial mutation occurs) Promotion (mutated cells are
stimulated to divide) Progression (tumor cells compete with one another and develop more mutations which make them more aggressive).
17. Differentiated cells: normal cells that are different from one another. When UNDIFFERENTIATED the cells rapidly divide and form malignant tumors. When DIFFERENTIATED the cells mutate and form benign tumors.
18. Benign Tumors: cells look like normal tissue cells and may perform the normal function of the tissues.
May lead to over secretion. Usually have a capsule around them, do not invade neighboring tissues, but can damage nearby organs by compressing them.
19. Malignant Tumors: cells do not look like normal adult cells, do not perform normal functions of the organ, may secrete hormones of other tissues. No clear boundaries and send “legs” into surrounding tissue.
Divide rapidly. Can compress and/or destroy surrounding tissues. Commonly produce telomerase (enzyme that repairs telomeres = basic immortality.
20. Metastasis: process by which cancer cells escape their tissue of origin and initiate new colonies of cancer in distant sites. Cells in a primary tumor develop the ability to escape and travel in the blood. Occurs in 3 ways: circulation through the circulatory and lymphatic system, accidental transplantation during surgery, spreading to adjacent organs and tissues.
21. Manifestations of Cancer:
a. Changes in organ function: organ damage, inflammation, failure, benign tumors may overproduce normal organ secretions, malignant tumors may cause overproduction, but more commonly decrease production of normal organ secretions.
b. Nonspecific signs of tissue breakdown: protein wasting, bone breakdown
c. Paraneoplastic Syndrome: consequences of hormones being secreted by tumor cells.
d. Bone Marrow Suppression: contributes to anemia, leukopenia (low WBC), and thrombocytopenia (low platelets).
e. Local effects of tumor growth: bleeding, compression of blood vessels, compression of lymph vessels (edema), compression of hollow organs, compression of nerves. (pain, paralysis).
f. Cancer Cachexia: weight loss, generalized weakness, increased metabolic rate, loss of appetite, nausea/vomiting.
g. Pain
h. Immune System Suppression
Chapter 10
1. Immune System 3 Functions: defend body against invasion or infection by pathogens (antigens), remove dead or damaged cells, attempt to recognize, remove abnormal cells (cancer cells).
2. 3 Lines of Defense: physical and chemical barrier to infection (skin, mucous membrane), inflammatory response, immune response (innate vs adaptive).
3. Innate Immunity: always present, requires no previous exposure. Non-specific (doesn’t distinguish), immediate response, involves NK cells and neutrophils/macrophages.
4. Inflammation: important part of innate immunity, increases vascular permeability, vasodilation, emigration of leukocytes, phagocytosis, chronic inflammation.
5. Inflammation Manifestations: redness, swelling, heat, pain, loss of function.
6. Purpose of Inflammation: neutralize and destroy invading agents, limit spread and prepare tissue for repair.
7. Adaptive Immunity: attacks specific antigens, slower response but more effective to 2nd exposure, involved B and T lymphocytes, includes cell-mediated/humoral immunity.
8. Stem cells: made in bone marrow. 9. B cells: mature in bone marrow.
10.T cells: mature in thymus.
11. Cell Mediated Immunity involves phagocytic cells that attack specific antigen, mediated by T lymphocytes.
12. Cytotoxic T Cells (CD8+): bind to surface of infected cells (MHC I), disrupt the membrane, and destroy before infecting other cells.
13. Helper T Cells (CD4+): stimulate B cells to mature into plasma cells which make antibodies. Stimulated by macrophages (MHC II) that display antigens.
14. Suppressor T Cells: reduce the humoral response.
15. Humoral Immunity: antibody proteins in the blood that attack the specific antigen, mediated by B lymphocytes. B lymphocytes can also become memory B cells which stay to fight future infections without needing a Helper T to tell them to.
16. Primary Immune Response:
Macrophages eat antigen and present it to TH cells TH cells activate B cells B cells become plasma cells and produce antibodies plasma antibody levels rise.
*Can take 2-3 weeks, vaccination produces a primary immune response because B cells become memory cells.
17. Secondary Immune Response: B memory cells respond to antigen immediately plasma antibody levels rise within days. Booster shots cause a secondary immune response so antibody levels will be
high before the disease is encountered.
18. IgG: 80% of plasma antibodies. Is the major antibacterial/antiviral antibody, crosses placenta, smallest.
Easily leaves bloodstream.
19. IgA: body secretions, protects against resp and GI infx.
20. IgM: first antibody produced during an immune response (primary), major antibody on B cells. 21.IgE: initiates inflammatory and allergic reactions.
22.IgD: found on surface of B cells with IgM, mainly acts as antigen receptor to stimulate B cells. 23.Excessive Immune Response: autoimmunity, hypersensitivity
24. Deficient Immune Response: absent or depressed
25. Autoimmunity: immune system. Recognized an individual’s own cells as foreign. Triggered by gender (f>m), chronic infx, stress, genetics. Tx of corticosteroids, tumor necrosis factor inhibitors that cause cell death, therapeutic plasmapheresis where components of disease is removed.
26. Hypersensitivity: normal immune response that is either inappropriately triggered, excessive, produces undesirable effects; usually does not occur on the first exposure.
TYPES 1, 2, 3: mediated by antibodies produced by B lymphocytes.
TYPE 4: mediated by. T cells and do not require antibodies.
Type 1: allergic, strong genetic or hereditary linkage regarding IgE response. Mast cells and basophils are principle effector cells. Tx: antihistamines, beta-adrenergic (decrease bronchoconstriction), corticosteroids, anticholinergics (block parasympathetic), IgE therapy. (inhibits IgE binding to mast cells), Epinephrine (adrenergic agent).
Type 2: tissue specific, cytotoxic, or cytolytic hypersensitivity. Occurs when antibodies attack antigens on surface of specific cells or tissues, causing lysis. Rh-neg MOTHER.
Type 3: immune complex reaction. Immune/phagocytic systems fail to remove antigen-antibody immune complexes. Not tissue specific. Ex: lupus, immune complex glomerulonephritis.
27. Primary Immunodeficiency Disorders: may be congenital, genetic, or acquired. Are rare and often sex linked (X chromosome), suspected with recurring infx.
28. Secondary Immunodeficiency Disorders: caused by excessive or defective neuroendocrine responses. Excessive: increased corticosteroid increases infx susceptibility, Defective: low corticosteroid increases susceptibility to autoimmunity.
Chapter 13
1. Total Blood Volume: 75.5 ml/kg in men, 66.5 ml/kg in women. 7%-8% of body weight. 5-6 L. Blood cells: 45% of blood volume, Plasma 55%.
2. Plasma: contains plasma proteins (serum albumin, globulin, fibrinogen) which are formed in liver, regulatory proteins (hormones, enzymes), organic constituents (products of tissue metabolism, nutritive organic materials), inorganic constituents (electrolytes, iron).
3. Transfusion reactions involve RBC destruction caused by recipient bodies. 4. Iron deficiency has low MCHC, MCH, MCV.
5. CO2 transported in the bloodstream as bicarbonate ion. 6. Bilirubin can detect excessive RBC lysis.
7. Blood Cells
Erythrocytes (RBC): transport oxygen, remove CO2, buffer blood pH. Last 120 days b/c membranes become weakened, they have no nuclei so cannot make new membranes, and they break as the squeeze through capillaries.
Leukocytes (WBC): act primarily in tissues but circulate in blood/lymph, form immune antibodies. Platelets: circulating fragments of megakaryocytes, form blood clots and control bleeding, 1/3 of platelets are in reserve in the spleen.
8. Adult Hemoglobin: 2 alpha chains, 2 beta chains; each chain hold a iron containing heme group that oxygen binds to. ~15 g of Hgb per 100 ml of blood.
9. Erythropoiesis: decreased blood oxygen, kidneys secrete EPO, bone marrow stimulated, created new red blood cells.
10. Spleen: houses WBC that are ready to process RBC’s, creating unconjugated bilirubin (toxic) from the hemoglobin.
11. Unconjugated Bilirubin:
turns into bilirubinemia jaundice
OR liver links it to glucuronic acid conjugated bilirubin bile
12. Hemoglobinemia: build-up of Hgb in blood, makes plasma red. 13.Iron is NECESSARY for RBC production.
14. Hemoglobinuria: makes urine dark.
Break in capillaries outside the spleen release of Hgb into blood Hemoglobinemia
Hemoglobinuria
15. Anemia: abnormally low Hgb level, number of RBCs, or both which results in low oxygen carrying capacity of the blood. Indication of some disease process or alteration in body function.
16. Compensatory Mechanism to restore tissue oxygenation: increased HR, CO, circulatory rate, flow to vital organs, increase in 2,3-DPG in RBC.
17. Causes of Anemia: blood loss, hemolysis, impaired RBC production.
18. Anemias:
Iron-Deficient: most common
Megaloblastic: inhibition of DNA synthesis in RBC production.
Pernicious: lack of intrinsic factor from parietal cells which leads to B12 deficiency. Aplastic: stem cell disorder caused by bone marrow depression, caused by toxic, radiant, or immunologic injury to bone marrow. Leads to pancytopenia.
Chronic: lack of EPO
19. Hemolytic Anemias:
Membrane Disorder- Hereditary Spherocytosis: spherical rather than biconcave RBC’s (genetic).
Acquired Hemolytic Anemias
Hemolytic Disease of the Newborn: fetal RBC’s cross placenta and stimulate production of maternal antibodies against fetal RBC’s
***Glucose. 6 phosphate dehydrogenase deficiency, hemolytic anemia is most often triggered by bacterial or viral infections or by certain drugs.
Hemoglobinopathies (inherited disorders): sickle cell, thalassemia
20. Thalassemia: genetic defect results in reduced rate of synthesis of one of the globin chains as well as increase hemolysis.
Alpha: defective gene for alpha chain synthesis, may gave 1-4 defective genes, affects both fetal and adult Hb, in fetus gamma Hb may form, in adult beta HB may form.
Beta: defective gene for beta chain, may have 1-2 defective genes, affects only adult Hb, alpha Hb may form.
21. Sickle Cell Disease: point mutation in beta chains of Hbg. When Hgb is deoxygenated the beta chains link together forming long protein rods that make cell sickle. Sickle cells. Cause vascular occlusion, pain, severe anemia, blocked capillaries, infarctions, jaundice. Tx is stem cell transplant.
22. Polycythemia: excess of RBC’s, increases blood viscosity and volume.
- Polycythemia Vera: neoplastic transformation of bone marrow stem cells.
- Secondary Polycythemia: due to chronic hypoxemia with resultant increase in EPO.
- Relative Polycythemia: due to dehydration. 23.Fetal Hbg: CANNOT SICKLE b/c there is no beta chains.
24.Circulatory System FCN: deliver oxygen to the body tissues while removing carbon dioxide produced by metabolism.
Chapter 14:
1. Hemostasis: arrest of bleeding or prevention of blood loss after blood vessel injury. Involves vessel wall, platelets, plasma coagulation proteins.
2. Hemophilia: inability to clot. prolonged bleeding time, prolonged aPTT (intrinsic, time it takes for blood to clot, determines if blood thinning therapy is effective), normal platelet count.
3. Vitamin K deficiency in newborns present with melena (GI), bleeding from the umbilicus, and hematuria 4. Vitamin K deficiency: normal bleeding time, normal platelet count, increase PT (extrinsic, prothrombin
time: measures time for blood to clot) and INR (ensures that results from a PT test are the same from one lab to another).
5. Coagulation assessment: PT/INR, aPTT, bleeding time. 6. Aspirin thins blood so it can prolong bleeding time.
7. Cancer can cause thrombocytopenia because the bone marrow isn’t working normally and doesn’t make enough platelets.
8. Disseminated intravascular coagulation (DIC): condition in which blood clots form throughout the body, blocking small blood vessels. S&S of chest pain, SOB, leg pain, problems speaking. Usually caused by inflammation, infection, or cancer.
9. Dysfunction of the liver can lead to a clotting factor deficiency. Liver is in charge of synthesis of clotting and inhibitor factors, quantitative and qualitative platelet defects from liver disease.
10. Platelet normal count: 150k to 400 k.
11. Primary Hemostasis: initial response, vessel vasoconstricts to prevent blood loss and forms platelet plug.
12. Secondary Hemostasis: involves formation of a fibrin clot through intrinsic pathway (blood comes into contact with altered vascular endothelium) and extrinsic pathway (crush injury). Both pathways lead to prothrombin to thrombin, fibrinogen to fibrin (clot), called the coagulation cascade.
13. Final Stage: clot retraction
14. Thrombocytopenia: decreased thrombocytes, below 50k. Prolonged bleeding time, petechiae (pinpoint red spots), purpura (red or purple discoloration). Commonly caused by bone marrow suppression, immunization, alcohol ingestion. General Mechanisms- decreased platelet production, decreased platelet survival, splenic sequestration, intravascular dilution of circulating platelets.
15. Thrombocytosis: high platelet count, may bleed or clot, transitory (stress/physical exercise), primary (polycythemia vera or chronic granulocytic leukemia), or secondary (response to hemorrhage, disease process, or splenectomy.
Chapter 15
1. Circulatory Circuit: absorption and delivery of nutrients, O2 uptake and delivery, waste removal
2. Lymphatic Circuit: specialized system of channels and tissues, reabsorbs fluid that leads from vascular network into the interstitial and returns to general circulation.
3. Thrombosis vs embolism: thrombus is a blood clot that forms in a vein. An embolus is anything that moves through a blood vessel until it reaches a smaller blood vessel. An embolus is often a small piece of a blood clot that broke off.
4. Arterial occlusions vs venous occlusions: arterial occlusions are commonly caused by atherosclerosis (fatty deposits inside a blood vessel), while venous occlusions are often the result of thrombosis (a blood clot in a blood vessel)
5. Peripheral edema is a result of venous thrombosis.
6. Artery Structure (inner to outer): tunica intimamediaadventitial
7. Vascular Endothelium: food and O2 pass into tissues, wastes and CO2 pass from tissues into blood, created compounds that cause constriction or dilation, creates growth factors that can stimulate smooth muscle, forms a smooth lining of the blood vessels that resist clot formation, created compounds that promote clot formation.
8. Arteriosclerosis/Atherosclerosis: hardening and loss of elasticity of the arteries. Athero is a type of arterio. Results from formation of fatty lesions in the intimal lining of large and medium sized arteries.
Lipids get into vascular endothelium WBC try to clear away and cause foam cells WBC and vascular endothelium release growth factors that promote plaque formation plaque blocks the arteries.
9. Lipoproteins: the more protein, the higher the density
10. Atherosclerosis Develops: because a) scavenger cells encounter fatty deposits in the artery lining and try to destroy by oxidizing. Oxidized fats injure the endothelium, clots form and release growth factors, smooth muscle grows over the fatty core or b) tries to remove the fats by eating them and they become foam cells in the core of the plaque.
11. HDL: goes out into peripheral tissues and picks up lipids, then carry it back to the liver.
12. Aneurysms: localized blood-filled dilation of arterial vessels. Walls of artery weakens and stretches, risk of rupture and hemorrhage, risk of clot formation, frequently found in cerebral circulation and thoracic/abdominal aorta
13. DVT vs varicose veins: DVT are blood clots that form in the deep veins of the legs and may travel to lungs or cause a pulmonary embolism or blood clot in the lung because a part of the clot may break off. Varicose veins are superficial, large, swollen, and twisted veins caused by increased blood pressure in the veins.
14. True Aneurysm: involves all 3 layers of the artery wall.
15. False Aneurysm: a collection of blood leaking out of the lumen but confined next to the vessel.
Chapter 16
1. Systolic BP: peak (higher) pressure, during systole. Reflects the amount of blood ejected with each beat (stroke volume) and compliance of the aorta and large arteries. Increases with age as the aorta and arteries lose elasticity.
2. Diastolic BP: lowest pressure, during diastole. Reflects closure of the aortic valve, the energy stored in elastic fibers of the large arteries, and the resistance to flow through arterioles into the capillaries
3. BP control involves both cardio and renal system:
4. Hypertension: increases morbidity and mortality with heart/kidney disease, stroke, peripheral vascular disease.
5. Primary/Essential Hypertension: idiopathic disorder, most common form; systolic blood pressure is a major risk factor for subsequent cardiovascular disease.
Diuretics: decrease vascular volume, CO, and PR.
B-adrenergic Receptor Blockers: decrease HR, CO, and renin release by kidneys.
ACE inhibitors: inhibit conversion of ANG I to ANG II, therefore reducing ANG II’s effect on vasoconstriction and aldosterone levels.
Angiotensin II receptor blockers
Calcium Channel Blockers: decrease PR by inhibiting movement of Ca2+ into arterial smooth muscle. Central a2-adrenergic agonists: decrease sympathetic outflow.
Central a1-adrenergic antagonists: cause vasodilation. Vasodilators: decrease PR.
6. Secondary Hypertension: attributed to specific identifiable pathology or condition. Accounts for only 5- 10%. Can be corrected or cured by surgery or treatment.
7. Hypertension Emergency vs urgency. Emergency: Systolic higher than 180 and/or diastolic higher than 120. Urgent: systolic higher than 140 or diastolic higher than 90.
8. Renal Hypertension: caused by decreased renal blood flow resulting in excessive release of renin, activating the RAA, causing peripheral vasoconstriction and sodium retention.
9. Hypotension Symptoms: fainting, nausea, dizziness, blurred/faded vision. Means that the heart, brain, and other parts of the body are not getting enough blood.
10. End organ damage of hypertension: heart- increased myocardial work resulting in heart failure, left ventricular hypertrophy, angina due to low blood flow. Brain- increased pressure in cerebral vasculature, hemorrhage, stoke, or TIA. Kidney- glomerular damage results in chronic kidney disease and failure.
Peripheral vascular disease (PVD). Eyes: affects microcirculation of the eyes.
11. Adrenocortical Disorders: excess aldosterone and glucocorticoids (cortisol) production, increases sodium and water retention.
12. Blood Pressures:
Normal: Less than 120 and less than 80
Elevated: 120-129 and less than 80
High Blood Pressure Hypertension Stage 1: 130-139 or 80-89
High Blood Pressure Hypertension Stage 2: 140 or higher or 90 or higher Hypertensive Crisis: higher than 180 and/or higher than 120
13. Coarctation of the Aorta: narrowing of the aorta, thus ejection of a large stroke volume into a narrow aorta causes increase in systolic BP.
14. Importance of Sodium in hypertension: higher amounts of sodium means more water retention which increases blood pressure. Water follow sodium, sodium goes into cell, the cell now has more water in it.
15. Action of ACE inhibitors: produces vasodilation by inhibiting the form of ANG II. This vasoconstrictor is formed by renin acting on circulating angiotension to form ANG I. Inhibitors prevent ACE enzyme from producing ANG II. ANG II would narrow the blood vessels and cause pressure to go up and heart to work harder.
16. Obesity/Obstructive sleep apnea
17. Complications of orthostatic hypotension: form of low BP that happens when you stand up from sitting or lying down. Can cause dizziness, faint. Can be caused by dehydration, low blood sugar, overheating. When you stand gravity causes blood to pool in your legs an abdomen which decreases blood pressure because there’s less blood circulating to the heart. Baroreceptors near the heart and neck usually send a signal to the brain which signals the heart to beat faster, pump more blood, which stabilizes BP. Can cause falls, stroke (bc of swings in BP), cardiovascular disease.
Chapter 18
Right side
• Blood enters the heart through two large veins, the inferior and superior vena cava, emptying oxygen-poor blood from the body into the right atrium.
• As the atrium contracts, blood flows from your right atrium into your right ventricle through the open tricuspid valve.
• When the ventricle is full, the tricuspid valve shuts. This prevents blood from flowing backward into the atria while the ventricle contracts.
• As the ventricle contracts, blood leaves the heart through the pulmonic valve, into the pulmonary artery and to the lungs where it is oxygenated.
Left side
• The pulmonary vein empties oxygen-rich blood from the lungs into the left atrium.
• As the atrium contracts, blood flows from your left atrium into your left ventricle through the open mitral valve.
• When the ventricle is full, the mitral valve shuts. This prevents blood from flowing backward into the atrium while the ventricle contracts.
• As the ventricle contracts, blood leaves the heart through the aortic valve, into the aorta and to the body.
1. Disorders that affect the whole heart: pericardial disorders, coronary heart disease, myocardial diseases. Can cause symptoms of both right and left sided heart failure.
2. Pericarditis: inflammation of the pericardium, may restrict the hearts movement due to pericardial effusion (serous exudate filling the pericardial cavity; this may lead to cardiac tamponade: accumulation of exudate compressing the heart, causing reduced ventricular filling), or constrictive pericarditis (fibrous scar tissue makes pericardium stick to the heart). May cause ECG and pain.
3. Coronary Heart Disease: characterized by impaired coronary blood flow, usually result of atherosclerotic coronary arteries leading to cardiac ischemia. Also, through thrombus formation, coronary vasospasm, endothelial cell dysfunction. Divided into 2 types: chronic ischemic heart disease and Acute Coronary Syndrome (represents spectrum of ischemic coronary disease ranging from unstable angina through myocardial infarction).
4. Coronary Heart Disease: atherosclerosis blocks coronary arteries, ischemia. May cause angina, heart attack, cardiac arrythmias, conduction deficits, heart failure, or sudden death.
5. Chronic Ischemic Heart Disease: imbalance in blood supply and demand for oxygen. Less Blood (atherosclerosis, vasospasm, thrombosis); Higher oxygen demand (stress, exercise, cold).
6. Stable angina: pain when hearts oxygen demand increases. 7. Variant angina: pain when coronary arteries spasm.
8. Stable vs Unstable angina. Stable: during exercise/physical activity. Unstable: symptoms while resting.
9. Silent myocardial ischemia: oxygen is deprived to the heart.
10. Acute Coronary Syndromes: ECG changes (T wave inversion, ST segment depression or elevation, abnormal Q wave), Serum cardiac markers (proteins releases from necrotic cells: myoglobin, creatine kinase, troponin).
11. LDL and Heart Disease: LDL causes the build-up of fatty deposits in the arteries which reduced or blocks the flow. Of blood and oxygen to the heart.
12. Myocardial Infarction: chest pain (crushing, constrictive), SNS response (GI distress, nausea, vomiting, tachycardia, vasoconstriction, anxiety, restlessness, feeling of impending doom), hypotension and shock (weakness in arms and legs).
13. Complications of acute coronary syndrome: coronary arteries branch of f the aorta after it leaves the heart.
Causes pumping problems due to MI, abnormal rhythms, pericarditis, blood clots, ventricular aneurysm.
14. Hypertrophic Cardiomyopathy: unusually thick ventricles, not enough room for blood to fill. Defects in contractile proteins make cells too weak. They hypertrophy to do the same amount of work as normal cells. Less space to fill with blood. Need more oxygen and perform less efficiently.
15. Restrictive cardiomyopathy: ventricles too stiff to stretch and fill.
16. MI, Myocarditis: ventricles are too weak to pump out blood due to inflammation of the heart. 17.Dilated Cardiomyopathy: Ventricles are too weak to pump out blood due to weakened, enlarged heart. 18.Peripartum Cardiomyopathy: Weak heart, final months of pregnancy.
19. MI tests: ECG, chest x ray, angiogram, ST elevation on ECG.
20. AV valves: Mitral (L) or tricuspid (R). 21.Semilunar: aortic (L) or pulmonary (R).
22. Heart Murmurs: valve defect, blood going through defective valves make noise; identify them by where they are, how they sound, when they happen.
23. Stenosis: valves do not open all the way; harder to force blood through. Will hear a murmur when the valve is open.
24. Regurgitant: valves do not close all the way; it leaks when it should be closed. Will hear a murmur when valve should be closed.
25. Mitral Valve Disorders (L): stenosis (narrowing), regurgitation (blood leaking), prolapse. 26.Aortic Valve Disorders (L): stenosis, regurgitation
27. Congenital Heart Defects:
Atrial Septal Defect: allows blood flow between atrias. Ventricular Septal Defects: allows blood flow between ventricles.
Endocardial Cushion Defects: no separation between the chambers of the heart. Coarctation of the aorta: narrowing of the aorta.
Patent Ductus Arteriosus: the ductus arteriosus (which connects the aorta and pulmonary artery) remains open, allows blood to flow between the two vessels.
Pulmonary Stenosis: pulmonary valve harder to open.
Transposition of the great vessels: 2 major vessels that carry blood from heart (aorta/pulmonary artery) are switched.
28. Shunts: opening or connection that lets blood move from one side of the circulation to the other. Most shunts occur in the heart and move blood usually L to R because L side is stronger.
29. Shunts are normal before birth.
30. Foramen Ovale: blood goes from R to L atrium, bypassing the lungs
31. Ductus Arteriosus: blood goes from the pulmonary trunk to aorta, bypassing the lungs. 32.Ductus Venosus: blood goes from the visceral veins to vena cava, bypassing the liver.
Chapter 19
1. Heart failure: impaired ability of the heart to pump blood to maintain sufficient CO to meet metabolic demands of tissues and organs. Results in congestion of blood flow in the systemic or pulmonary venous circulation. Most common reason for hospitalization in those >65 years of age.
2. Heart Failure: potential consequence of most cardiac disorders such as MI, high BP, degenerative conditions (cardiomyopathies), excessive work demands, volume overload
3. High-output Failure: supranormal output but inadequate due to excessive metabolic needs, anemia, arteriovenous shunting.
4. Low-output Failure: impaired heart pumping due to ischemic heart disease and cardiomyopathy.
5. Systolic Failure: impaired ejection of blood from the heart due to decreased contractility, volume overload, or pressure overload.
6. Diastolic Failure: impaired filling of heart due to smaller ventricular chamber size, hypertrophy, poor compliance.
7. Right-Sided Heart Failure: impairs ability to move deoxygenated blood from system to pulmonary circulation. Symptoms: awakening at night with SOB, SOB during exercise, coughing, wheezing, edema in ankles, legs, feet, abdomen, need to urinate, weight gain.
8. Left-Sided Heart Failure: impairs pumping of blood from the low-pressure pulmonary to the high-pressure arterial circulation. Fluid may back up in the lungs cause SOB< frothy sputum.
9. Adaptive Mechanisms to CO: SNS, RAA, Frank-starling mechanism, myocardial hypertrophy and remodeling.
10. Paroxysmal Nocturnal Dyspnea: sudden SOB during sleep. Symptom of COPD, pneumonia, heart failure.
Heart failure occurs when heart muscle struggles to pump blood throughout body, can lead to fluid buildup in lungs aka pulmonary edema and make it difficult to breathe.
11. Frank-Starling Curve: the heart increases SV by increasing ventricular EDV, which increases myocardial fiber stretch to optimize actin and myosin overlap. (helps fibers stretch out to pump more blood).
12. Left-Sided Heart Failure: Right heart lungs fill with fluidLeft Heart (diastolic: does not accept enough
blood from lungs)Systolic: LV does not pump enough blood to bodyBody lacks blood.
13. Right-Sided Heart Failure: Right heart (Systolic: RV does not pump enough blood to the lungs)Lungs (lungs do not oxygenate enough blood) left heartbody fikls with blood Diastolic: RV does not accept enough blood from the body.
14. Pulmonary Edema: Capillary fluid moves into alveoli and lungs become stiffer, harder to inhale, less gas exchange, crackles, frothy sputum, Hgb not completely oxygenated.
15. CO and Heart Failure: to maintain CO the heart might increase HR or increase SV. If it can’t there will be backup of blood into the lungs, swelling in ankles, abdomen, low output symptoms such as fatigue, low urine output, lightheadedness.
16. Heart Failure Tx: relieve symptoms, improve QOL, surgical repair, Ace inhibitors, diuretics, B-adrenergic blocking agents, digitalis, restriction of salt intake, pacemaker.
Chapter 20
1. Circulatory Shock: acute failure of circulatory system to supply peripheral tissue and organs of the body with an adequate blood supply, resulting in cellular hypoxia. Not a specific disease but can occur in the course of many diseases.
2. Pathogenesis: inadequate cellular oxygenation (from decreased CO, maldistribution of blood flow, reduced blood oxygen content), impaired tissue oxygenation results in cellular hypoxia which causes anaerobic
metabolism, free radical production, macrophage induction, and failure of microcirculation to auto- regulate blood flow leads to activation of coagulation.
3. Compensatory Mechanism of Shock: homeostatic mechanisms are sufficient to maintain adequate tissue perfusion despite a reduction in CO, SNS activation attempts to maintain BP even though CO has fallen, progressive stage of shock is marked by hypotension and marked tissue hypoxia (lactate production increases with anaerobic metabolism, lack of ATP leads to cellular swelling, dysfunction, death, and cellular/organ dysfunction result from oxygen-free radicals, release of inflammatory cytokines, and activation of the clotting cascade).
4. Hypovolemic: loss of whole blood, loss of plasma, loss of extracellular fluid. Inadequate filling of vascular compartment and reduced venous return. Occurs when there is an acute loss of 15% to 20% circulating blood volume. Loss of plasma (severe burns), loss of whole blood (hemorrhage), loss of extracellular fluid (GI fluids lost in vomiting or diarrhea), dehydration. Tx: fluid replacement and control of source of volume loss.
5. Cardiogenic: alteration in cardiac function. Decreased CO lowers BP. SNS responds, vasoconstriction increases resistant to blood flow, increased workload on heart worsens heart failure. Usually a result of severe ventricular dysfunction due to myocardial infarction (MI, heart attack, loss of blood to heart), ineffective pumping caused by cardiac arrhythmias, ventricular septal defect, ventricular aneurysm, acute disruption of valvular function, problems associated with open heart surgery. Low CO= reduced oxygen delivery to tissues. Therapy aimed at improving CO and myocardial oxygen delivery, decreasing workload, inotropic, afterload reducing agents, intraaortic balloon counter pulsation, ventricular assist devices, heart transplantation.
6. Obstructive: inability of heart to fill properly, obstruction to outflow from the heart. Signs of right heart failure are seen. Common causes include pulmonary embolism, cardiac tamponade, tension
pneumothorax. Rapid management of underlying obstruction is required to prevent cardiovascular collapse. EX: pulmonary embolism, cardiac tamponade.
7. Distributive: loss of sympathetic vasomotor tone, presence of vasodilating substance in the blood, presence of inflammatory mediators. Characterized by excessive vasodilation and peripheral pooling of blood. There is not enough blood to fill the circulatory system (CO inadequate due to reduced preload), blood flow decreases, less blood is returned to the heart, less blood is circulated to the body. Includes anaphylactic, neurogenic, septic. Caused by decreased sympathetic activity (neurogenic; brain or spine injury, insulin shock, emotion, drug overdose; Tx: vasopressors), vasodilator substances in blood (type 1 allergic hypersensitivity), inflammatory response to infection (sepsis), vessel damage from severe hypovolemia (decreased blood volume).
8. Anaphylactic Shock: result of excessive mast cell degranulation mediated by IgE antibodies in response to antigen. Mast cells release vasodilatory mediators resulting in severe hypotension (histamine, kinins, leukotrienes, prostaglandins), bronchoconstriction makes breathing more difficult. Clinical symptoms: hives, bronchoconstriction, stridor, wheezing, itching. Tx: maintenance of air way, epinephrine, antihistamines, vasopressors, and fluids.
9. Sepsis or Systemic Inflammatory Response Syndrome (SIRS): results from severe systemic inflammatory response to infection. Inflammatory mediators released into the circulation (tumor necrosis factor, interleukins, prostaglandins. Cause systemic signs of inflammation: fever and increased respiration, respiratory alkalosis, vasodilation, hypotension, increased capillary permeability with edema, warm flushed skin. Activate inflammatory pathways (coagulation, complement system). Tx: improve blood flow distribution and managing infection with antibiotics, fluids, improve cardiac and vascular performance.
10. Activated Protein C: drotecogin alfa- a recombinant form of activated protein C. Blocks clotting, blocks inflammation, increases survival of the most seriously ill sepsis patients, may cause bleeding.
11. Sepsis: caused by body’s response to infection. Body normally releases chemicals into the bloodstream to fight an infection. Sepsis occurs when the body’s response to the chemicals is out of balance and triggers changes that can damage multiple organ systems.
12. Complications of Shock: complications are inflammatory in nature, excessive immune response leads to leaking capillaries, damage from proteolytic enzymes, and systemic activation of the clotting and complement systems.
13. Acute Respiratory Distress Syndrome (ARDS): exudate enters alveoli and blocks gas exchange making inhaling more difficult, neutrophils enter alveoli and release inflammatory mediators that make pulmonary capillaries leaky; releases proteolytic enzymes, produce oxygen-free radicals.
14. Acute Renal Failure: renal vasoconstriction cuts off urine production (acute renal failure), continued vasoconstriction leads to hypoperfusion which cuts off renal oxygen supply, renal tubular cells die =acute tubular necrosis (ATN) associated with decreased excretion of waste products (creatinine, urea).
15. Multiple Organ Dysfunction Syndrome: most common causes (sepsis), initiated by immune mechanisms that are overactive/destructive, altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention, kidneys/lungs/liver/brain/heart, most frequent cause of death in noncoronary ICU, mortality rates vary 30-100%.
Chapter 22
1. Airway: autonomic nervous system controls the diameter of the airways and consequently, resistance to airflow, via contraction and relaxation of smooth muscle. PNS = bronchoconstriction via vagus nerve and cholinergic receptors. SNS = bronchodilation via beta 2- adrenergic receptors.
2. Obstructive Pulmonary Disorders: manifested by increased resistance to airflow (difficulty exhaling). 3. Dry cough is a common sign of viral pneumonia.
4. Immunosuppression is a risk factor for active pulmonary TB.
5. Bacterial pneumonia S&S: productive cough, parenchymal infiltrates on x ray. 6. TB X Ray: ghon tubercle.
7. IgE: associated with inhaled allergens in asthma.
8. Allergic form of asthma: inflammation, mucosal edema, and bronchoconstriction 9. Alveolar destruction: caused by a lack of alpha anti-trypsin.
10.Recurrent infection can cause hypersecretion of mucus in chronic bronchitis. 11.All Obstructive Pulmonary Disorders: characterized by resistance to air flow. 12.Obstructions in lumen wall: asthma, bronchitis.
13.Obstruction from increasing pressure around outside of lumen: emphysema. 14.Obstruction of airway lumen: bronchiectasis, cystic fibrosis.
15. COPD leads to barrel chest due to air trapping.
16. Asthma: airway obstruction that is reversible, airway inflammation, increased airway responsiveness to a variety of stimuli. Most common chronic disease of children; genetics, eczema, African American risk factors.
17. Extrinsic Asthma (allergic): ½ of asthma cases. An IgE mediated response to specific antigens, with antibody production. Mechanism: IgE is produced in response to allergen exposure, bins to mast cells and cause the release of histamines, leukotrienes, prostaglandins, bradykinins, serotonin. Increased microvascular permeability, bronchoconstriction. Epithelial damage, smooth muscle, and mucous gland hypertrophy, mucus in lumen.
18. Intrinsic Asthma (non-allergic): no antibodies produced, caused by exercise, stress, aspirin, an exposure to pulmonary irritants (smoke, cleaning agents). These irritants cause usual asthmatic response of hypersensitive smooth muscles to constrict, airway inflammation and increased mucus production.
19. Asthma: common symptoms of wheezing, tight chest, dyspnea, cough, increased sputum production.
Severe attacks use accessory muscles of respiration, intercoastal retractions, distant breath sounds with inspiration, orthopnea, agitation, tachycardia, tachypnea. TX: avoid triggers, air purifiers, remove allergens, desensitization, oxygen therapy, corticosteroids, mast cell inhibitors.
20. Chronic Bronchitis: form of COPD where there is persistent narrowing of the airway due to chronic inflammation, scarring, and excessive mucus production. Chronic or recurrent productive cough lasting more than 3 months per year for 2 or more years. Damage not reversible. Type B COPD Blue Bloaters. Caused by cigarette smoke, rpt airway infx, genetics, inhalation of irritants. Pathogenesis: chronic inflammation/swelling of bronchial mucosa resulting in scarring, hyperplasia of bronchial mucous, increased bronchial wall thickness, pulmonary hypertension. SOB, excessive sputum, cyanosis, polycythemia, excessive body fluids. Tx: bronchodilator therapy, remove secretions, prevent muscle fatigue, low dose oxygen. **LEADS TO COR PULMONALE DUE TO INCREASED PULMONARY VASCULAR
RESISTANCE. Thick mucus, fibrosis, and smooth muscle hypertrophy are parts of airway obstruction in CB. Also common to see chronic cough.
21. Emphysema: destruction of alveoli and small airways due to release of proteolytic enzymes from immune cells, occurs in smokers, Type A COPD or pink puffers. Common in mining, welding, asbestos.
Pathogenesis: alveolar destruction is due to release of inflammatory cells (neutrophils, macrophages) that degrade lung proteins. Smoking also inhibits a protective enzyme, a1-antitrypsin, that normally keeps proteolytic enzymes in check. Genetic a1-antitrypsin is an uncommon cause of emphysema. Loss of elastic tissue in lungs.
22. Emphysema Respiratory Problems: a decrease in surface area for gas exchange, airway collapse due to loss of radial traction. Manifests as dyspnea, weight loss, use of accessory muscles to breathe, a low/flat diaphragm, barrel chest, pursed-lip breathing, leaning forward to breath, cough, cyanosis. Tx: cessation of smoking, oxygen therapy.
23. Acute asthma attack: associated with wheezing, coughing, chest tightness, use of accessory muscles.
Complication: status asthmaticus
24. Pink Puffers: usually emphysema; by sustaining high ventilatory effort, a patient can have blood oxygen levels that are generally maintained near normal. SOB, increased ventilatory effort, use accessory muscles, pursed-lip breathing.
25. Blue Bloaters: cannot increase respiration enough to maintain oxygen levels, cyanosis (blue skin) and polycythemia, cor pulmonale (change in RV of heart due to respiratory disorders).
26. Bronchiectasis: aneurysm-like dilation of the bronchioles. Bronchiolar dilations serve as pockets of infection, producing foul-smelling sputum. Pathogenesis: recurrent infection of bronchial wall leads to persistent dilation, recurrent inflammation results in destruction of wall, destruction process leads to loss of ciliated epithelium. Chronic, productive cough, digital clubbing, treatment centers on antibiotic therapy and removal of secretions. Tx: remove secretions, abx.
27. Cystic Fibrosis: autosomal recessive disorder of chloride and water transport proteins affecting exocrine glands and mucus cells. Leads to dehydration and mucosal thickening in the respiratory and intestinal tract. Thick mucus secretions cause airway obstruction and air trapping. Obstructs pancreatic and biliary ducts. Tx removal of secretions, abx therapy.
Chapter 23
1. Restrictive Pulmonary Disorders: category of respiratory diseases characterized by a loss of lung compliance, resulting in decreased lung expansion and increased lung stiffness. Causes include
alterations in lung parenchyma (alveoli, bronchioles), pleura, chest wall, neuromuscular function. Characterized by decrease in VC, TLC, FRC, and RV. The greater the decrease in lung volume, greater the severity of disease. Decreased PaO2, normal or decreased PaO2, increased pH (alkalosis).
2. ARDS: characterized by hypoxemia.
3. Occupational Lung Diseases: result from inhalation of toxic gases or foreign particles, atmospheric pollutants have large effect.
4. Pneumoconiosis: caused by inhalation of inorganic dust particles, greater the exposure the worse it gets. 5. Pneumothorax (collapsed lung): air leaks into space between lung/chest wall, air pushes on the outside of
lung making it collapse. Characterized by tracheal shift and respiratory distress. Air that enters the pleural space during inspiration but is unable to exit during expiration leads to tension pneumothorax.
6. Pneumothorax and ARDS: types of restrictive respiratory disorders.
7. Anthracnosis: coal miner’s lung or black lung
8. Silicosis: silica inhalation
9. Interstitial lung disease: honeycomb appearance, immunological in nature, and loss of alveolar walls. 10.Asbestosis: asbestos inhalation
11. Pathogenesis of all: pollutants interfere and. Paralyze cilia resulting in impaired clearance effect and inability to remove mucus/dust/foreign particles, etc. Alveolar macrophages try to engulf and remove particles by secreting lysosomes. Secreted enzymes damage alveolar wall causing deposition of fibrous material.
12. Clinical Manifestations: pneumoconiosis produces no S&S in early stage, progressive cough, dyspnea, cor pulmonale, resp failure, chronic hypoxemia.
13. TX: preventative measure, corticosteroids, bronchodilators, oxygen therapy, ventilator, deep breathing. 14.Sarcoidosis: presence of CD4+ cells, non-productive cough, granulomas, fatigue, weight loss, and fever.
15. Pleural Effusion: “water on the lungs” characterized by dyspnea, diminished breath sounds, and tracheal shift.
16. Pickwickian Syndrome: increased abdominal size forces thoracic contents upward into chest cavity, decreases lung expansion and diaphragmatic shortening. Chest Wall deformity.
17. Sleep Apnea Syndrome: soft tissue deposits in neck and predispose person to upper airway obstruction. 18.Obese Chest Wall Deformities Manifestations: decreased alveolar ventilation, hypoxemia, sleepiness, SOB,
polycythemia, cor pulmonale, impotence, headache.
19.TX: oxygen therapy, caloric intake energy deficit, aerobic exercise, gastric bypass or stapling.
Chapter 24
1. Abnormalities in Body Fluid: can occur in volume, concentration, electrolyte composition of body fluid.
2. Extracellular fluid: contained outside cells.
3. Interstitial: between cells, rich in Na, Cl, HCO3, and proteins.
4. Magnesium-aluminum antacids are a risk factor for hypophosphatemia
5. Vascular compartment: in blood vessels, rich in proteins.
6. Intracellular fluid: contained inside cells, rich in K, Mg 2+, inorganic and organic phosphates, and proteins. Low in Na and Cl.
7. Hyperparathyroidism is a risk factor for hypercalcemia.
8. Hypocalcemia and hypomagnesemia both increase neuromuscular excitability. 9. Vomiting (emesis) can cause metabolic alkalosis.
10.Diarrhea can cause metabolic acidosis. 11.Hypernatremia: confusion.
12. Hypokalemia: muscle weakness, cardiac dysrhythmias are manifestations of moderate to severe hypokalemia.
13. Chronic alcoholism: cause for hypomagnesemia.
14. Decreased ADH can cause hypernatremia
15. Hyponatremia: characterized by confusion, lethargy, coma, seizures.
16. Kidneys: fluid balance regulates the amount and makeup of body fluids, ADH from pituitary- reabsorb water, aldosterone- reabsorb Na+, secrete K-. Acid Base balance: secrete and reabsorb H+ and HCO3.
17. High osmolarity causes thirst which increases water intake, ADH release which reabsorbs from urine. 18.Low osmolarity causes lack of thirst and decreased ADH release so water is lost in urine.
19. Sodium: 135-145 mEq/L. Regulates extracellular fluid volume and osmolarity.
20. Potassium: 3.5-5.0. mEq/L. Maintains intracellular osmolarity, controls cell resting membrane potential, needed for Na K pump, exchanged for H. to buffer changes in blood pH, KH exchange occurs in the tissues and in the distal tubule of the nephron.
21. Cell Firing: stimulus: some Na channels open; at threshold more Na channels open, rushing in, making the cell positive (depolarizing); action potential: cell responds, contracts. K channels open making the cell negative again (repolarization), Na K pump removes the Na from the cell and pumps the K back in.
22. Hyperkalemia: raises resting potential toward threshold. Cells fire more easily, if resting potential reaches threshold, Na gates open and won’t close.
23. Hypokalemia: lowers resting potential away from threshold, cells fire less easily.
24. Calcium: 9-11 mg/dL, 4.5-5.5 mEq/L. Extracellular: blocks Na gates in nerve and muscle cells, clotting, leaks into cardiac muscle, causing it to fire, intracellular: needed for all muscle contraction, acts as second messenger in many hormone and neurotransmitter pathways.
25. Hypercalcemia: blocks more Na gates, nerves are less able to fire. 26.Hypocalcemia: blocks fewer Na gates, nerves fire more easily.
27. Magnesium: 1.5-2.5 mEq/L. Cofactor in ATP, DNA replication, mRNA production.
28. Normal pH: 7.35-7.45, cellular function is impaired when pH of body fluids becomes abnormal. H blocks Na gates.
29. Relationship between metabolic alkalosis and hypokalemia: due to low extracellular potassium concentration potassium shifts out of cells. Excess sodium increases extracellular volume and the loss of hydrogen ions creates a metabolic alkalosis.
30. Headaches are an early sign of metabolic acidosis.
31. Regulators of Acid-Base: Buffers- chemicals that prevent large changes in pH by releasing or taking up H, mostly HCO3, normal ratio of bicarbonate to carbonic acid is 20:1, any deviation alters blood pH. Respiratory System: hyper/hypoventilation alters Co2. Renal system: excretes or retains metabolic acids.
32. Hyperventilation can cause respiratory alkalosis. 33.Hypoventilation is compensatory mechanism for metabolic alkalosis.
34.Respiratory Acidosis: increased Co2, increased carbonic acid, increased H (low pH), increased bicarbonate 35.Respiratory alkalosis: decreased CO2, decreased carbonic acid, decreased H (high ph), decreased
bicarbonate.
36. Metabolic Acidosis: increased metabolic acids which raised H and lowers pH, decreased bicarbonate. 37.Metabolic Alkalosis: decreased H which increased pH, increased bicarbonate.
Chapter 27, 29
1. S&S of Kidney Stones: differ in their size and location. Acute renal colic pain (intermittent sharp pain) or flank pain (stones within the kidney). Pain associated with nausea, vomiting, diaphoresis, tachycardia, and tachypnea. Once stone reaches bladder there is a reduction in pain
2. Common Composition of Renal Calculi: calcium. Urine becomes too saturated with specific solute, then form crystals if the concentration is too great (supersaturation). Usually begin development in the nephron and kidney pelvis. Crystallization is enhanced when a person is dehydrated or has high levels
of solute in the kidney from excessive excretion (calcium, uric acid). Calcus matrix consists of protein, sugar, glucosamine, bound water, and organic ash.
3. Polycystic Kidney Disease:
4. Glomerulonephritis: inflammation of the glomeruli that results in chronic renal failure. Activated complement attracts neutrophils and monocytes. They release lysosomal enzymes that damage the glomerular cell walls. This increases permeability, and the loss of negative charge. Results in enhanced protein filtration, all affecting GFR. Most common in boys age 3-7.
5. S&S of Renal Cancer:
6. Uric acid crystals in renal calculi from gouty arthritis:
7. Hematuria is the most frequent and initial symptom of bladder cancer.
8. Vesicoureteral reflux (backup into the ureters) can lead to recurrent cystitis. 9. E coli is the cause for majority of UTIs.
10.Sexually active women are more prone to TI. 11.Ureterocele is a cystic dilation of the ureter. 12.Smoking is a risk factor for bladder cancer.
13. Stress vs urge incontinence. STRESS: weakening of or damage to the muscle used to prevent urination (pelvic floor and the urethral sphincter). URGE: result of overactivity of the detrusor muscle which controls the bladder
14. Characteristics of cystitis: mucosal inflammation and congestion. The detrusor muscle of the bladder becomes hyperactive, decreasing bladder capacity and leading to reflux into the ureters. This transient reflux can cause acute or chronic pyelonephritis if the bacteria ascends to the kidney.
15. Function of the kidneys: regulation of extracellular fluid volume and blood pressure, regulation of osmolarity, maintenance of ion balance (especially Na+, K+, and Ca2+), homeostatic regulation of pH (removal or conservation of H+ or HCO3 - ), excretion of wastes, production of hormones (synthesize
erythropoietin (regulates RBC synthesis) (synthesize renin (regulates hormones involved in sodium balance and BP homeostasis).
16. UTI: common bacterial infections that enter through the urethra or bloodstream ● Bacterial infections include: ● E. coli ● Staphylococcus ● Can occur in the upper or lower urinary tract ● Upper UTIs are more serious because they can cause renal damage.
17. UTI Risk Factors: urinary obstruction and reflux (urine from urethra move back into bladder, or bladder into ureters; results in urine remaining in the bladder and acts as a medium for microbial growth), neurogenic disorders that impair bladder emptying, sexually active women, postmenopausal women (estrogen increases antimicrobials, tightens junctions), diabetics, men with prostate disease, elderly, urinary catheterization (bacteria on the catheter).
18. r washout phenomenon (bacteria are removed from the bladder and urethra during voiding), protective mucus, local immune responses and IgA, normal bacterial flora, peristalsis of ureters facilitate movement of urine from the renal pelvis through the ureters into the bladder, phagocytic cells remove bacteria from the urinary tract.
19. UTI Manifestations depends on whether the infection involves the lower (bladder) or upper (kidney) urinary tract and whether the infection is acute or chronic. Majority are acute uncomplicated bladder infections in women. Burning and dysuria, lower abdominal or back discomfort, cloudy and foul-smelling urine, fever.
20. Glomerular Damage: 2 types of immune mechanisms have been implicated in glomerular disease. A: antiglomerular antibodies leaving the circulation and reacting with fixed glomerular antigens in the basement membrane. B: Circulating antigen-antibody complexes become trapped in the membrane as they get filtered in the glomerulus.
21. Glomerular Damage: proliferative: number of cells increase, sclerotic: amount of extracellular matrix increases, membranous: thickness of glomerular capillary wall increases. All can decrease the efficiency of filtration. Allows blood cells, lipids, or proteins to pass into the urine.
22. Glomerulonephritis: inflammation of the glomeruli that results in chronic renal failure. Activated complement attracts neutrophils and monocytes. They release lysosomal enzymes that damage the glomerular cell walls. This increases permeability, and the loss of negative charge. Results in enhanced protein filtration, all affected GFR. Occurs at any age but most common in boys 3-7.
23. Pyelonephritis: inflammation affecting the tubules interstitium and renal pelvis. Results in urinary urgency and frequency, burning during urination, dysuria, nocturia, hematuria caused by UTI. Cloudy urine with a fishy odor resulting from bacteria in the urine and subsequent leukocyte response.
Temperature, shaking chills, nausea, vomiting, anorexia, and general fatigue caused by infection. More common in females because shorter urethra, lack of antibacterial prostatic secretions. Incidence increases with age.
24. Acute Pyelonephritis: inflammation caused by E Coli that primary affects the interstitial area and the renal pelvis or the renal tubules.
25. Chronic Pyelonephritis: progressive process, scarring and deformation of the renal calices and pelvis, loss of tubular function and ability to concentrate urine give rise to polyuria and nocturia and mild proteinuria. Severe hypertension is a contributing factor. Is a significant cause of renal failure.
26. Cystitis: infection of the bladder that results in inflammation and congestion. The detrusor muscle of the bladder becomes hyperactive, decreasing bladder capacity and leading to reflux into the ureters. This transient reflux can cause acute or chronic pyelonephritis if the bacteria ascends to the kidney. Results in dysuria and suprapubic pain, urinary frequency and urgency, cloudy, malodorous, possibly bloody urine, fever, nausea, vomiting.
Chapter 28
1. Different phases of acute tubular necrosis:
2. Process of anemia and renal osteodystrophy in end stage renal disease: kidneys do not make EPO so bone marrow makes fewer RBC’s. Renal Osteodystrophy: bone disease that occurs because kidneys fail to maintain proper levels of calcium and phosphorus in the blood.
3. Causes of chronic kidney disease: end result of irreparable damage to the kidneys, destruction of renal nephrons, and a marked decrease in the GFR.
4. Secondary conditions associated with end stage chronic renal disease: diabetes, hypertension, glomerulonephritis, polycystic kidney disease, vesicoureteral (causes urine to back up into the kidney).
5. Different phases of acute kidney injury: PRERENAL: decreased renal blood supply leads to shock, dehydration, vasoconstriction. INTRINSIC: kidney tubule function is decreased, and kidney structure is damaged because of ischemia, toxins, and intratubular obstruction.
6. Ischemia leads to acute tubular necrosis.
7. Renal failure: kidneys fail to remove metabolic end products from the blood, regulate the fluid, electrolyte, and pH balance of the extracellular fluids. When kidneys fail less waste is removed, more waste remains in the blood, nitrogenous compounds build up in the blood (BUN: blood urea nitrogen, creatinine (waste product from muscle)).
8. Renal Fcn approximated by initial creatinine level/current creatinine level.
9. Acute Renal Failure: abrupt in onset and often reversible if recognized early and treated appropriately. Is a rapid decline in renal function sufficient to increase blood levels of nitrogenous wastes, impair fluid and electrolyte balance, decrease GFR (as a result excretion of nitrogenous wastes is reduced and fluid and electrolyte balance cannot be maintained). (CAN BE FIXED)
10. GFR is calculated with age, race, gender, height, weight, and serum creatinine. Normal GFR = > 90 mL/min.
11. Acute Renal Failure: prerenal (decreased renal blood supply causing shock, dehydration, vasoconstriction), postrenal (urine flow is blocked causing stones, tumors, enlarged prostate), intrinsic (kidney tubule function is decreased, kidney structure damage, ischemia, toxins, intratubular obstruction.
12. Chronic Renal Failure: end result of irreparable damage to the kidneys, developing slow over years.
Reduced kidney function due to destruction of renal nephrons and a marked decrease. Symptoms are not evident until disease is advanced because of the compensatory ability of the kidneys. Fewer nephrons are functioning so the remaining nephrons must filter more and hyperperfused and hypertrophy (CANNOT BE FIXED).
13. CRF Development 4 Stages: diminished renal reserve (nephrons are working as hard as they can), renal insufficiency (nephrons can no longer regulate urine density), renal failure (nephrons can no longer keep blood composition normal), end stage renal disease (dialysis, kidney transplant, GFR < 15 mL/min).
14. Uremia: urine in the blood. Renal filtering function decreases altered fluid and electrolyte balance (making acidosis, hyperkalemia, salt wasting, hypertension), wastes build up in the blood (increasing creatinine and BUN, toxic to CNS, RBCs, platelets), kidney metabolic functions decrease (decreased EPO, vit D activation).
15. Cardiovascular Consequences of CRF: decreased blood viscosity, increased blood pressure, decreased oxygen supply.
16. Azotemia: CRF decreased ability to excrete nitrogenous wastes increase BUN results in
azotemia.
17. Metabolic Acidosis: CRF decrease ability to excrete H+ increase H+ in blood decrease blood pH
metabolic acidosis Or
CRF decrease ability to reabsorb HCO3 less bicarbonate is present to buffer H+ in the blood
decrease blood pH metabolic acidosis
18. Hypertension: CRF increase RAA activity increase vascular volume and peripheral resistance
hypertension
19. Anemia: CRF decrease EPO production fewer RBCs formed.
Or
CRF increase levels of nitrogenous wastes blood cells damaged/destroyed; RBC production suppressed.
20. Altered Drug Sensitivity: CRF altered rates of drug excretion. CRF altered levels of plasma proteins
fewer proteins available to bind drugs. CRF uremia alters metabolism of some drugs.
Chapter 31
1. Disorders: congenital, acquired, infectious, neoplastic.
2. Erectile Dysfunction: impotence or inability to achieve or maintain an erection sufficient for satisfactory sexual performance.
3. Primary Impotence: inability to attain an erection throughout life, often related to psychiatric problems or adolescent vascular trauma.
4. Secondary Impotence: no longer able to develop erections; had previous erections. Can be caused by peripheral vascular disease, endocrine problems, medications, trauma, iatrogenic causes, psychological causes.
5. ED Tx: determine psychogenic or organic cause. Surgical Intervention (insertion or inflatable or semirigid prosthesis), intracavernous injection (vasoactive meds: papaverine, phentolamine prostaglandin E), Selective inhibitors of cyclic guanosine monophosphate (cGMP): Viagra, Levitra, Cialis. Vacuum device.
6. Cryptorchidism poses a risk for testicular cancer.
Chapter 33
7. Testicular Torsion: when the tissues around the testicle are not attached well. Can cause the testes to twist around the spermatic cord. This cuts of f blood flow to the testicle and causes pain and swelling.
8. S&S of prostatic enlargement (BPH= benign prostatic enlargement): urinary frequency, nocturia, dysuria, dribbling at the end of urination, inability to completely void.
1. Amenorrhea: ABSENCE or suppression of menstruation, no menses. Causes include hormonal disturbances, stress, neoplasms. Tx: aimed at the underlying cause, hormonal supplementation, surgery (tumor removal).
2. Metrorrhagia: bleeding BETWEEN menstrual periods, causes slight bleeding from endometrium during ovulation, uterine malignancy, cervical erosions, endometrial polyps, estrogen therapy.
3. Hypomenorrhea: DEFICIENT AMOUNT of menstrual flow, reduced flow. Causes: endocrine or systemic disorders interfering with hormones, partial obstruction of menstrual flow.
4. Oligomenorrhea: INFREQUENT >35 DAYS. Caused by endocrine/systemic disorder causing failure to ovulate.
5. Polymenorrhagia: INCREASED FREQUENCY <21 DAYS of menstruation <21 days. Causes: endocrine/systemic disorder causing ovulation.
6. Menorrhagia: HEAVY BLEEDING increase in amount or duration of bleeding; prolonged and heavy bleeding. Caused by heavy lesions of reproductive organs.
7. Dysfunctional Uterine Bleeding: abnormal endometrial bleeding not associated with tumors, inflammation, pregnancy, trauma, or hormonal effects. Most common around time of menarche (immaturity in functioning of the pituitary and ovary) and menopause (progressive function and failure of the ovary to produce estrogen).
8. Pregnancy related disorders: iron deficiency anemia, GDM, depression, anxiety, hypertension, hyperemesis, infections
9. Uterine Prolapse: uterus descends into the vagina. Pelvic floor muscles and ligaments become weak and can’t support the uterus.
10. Endometriosis: tissue similar to the tissue normally lining the inside of the uterus lines the outside of the uterus.
11. Leiomyomas: a fibroid. Benign smooth muscle tumor that very rarely become cancer. Can occur in any organ but most commonly formed in the uterus, small bowel, and esophagus. Polycythemia may occur because EPO is part of paraneoplastic syndrome.
12. Vulvovaginitis is commonly caused by candida albicans.
Chapter 41
1. Anabolism: insulin, anabolic steroids. Available foodstuffs (in blood), glucose, amino acids, free fatty acids (liver can convert amino acids and free fatty acids into ketones) stored foodstuffs (in cells), glycogen, proteins, triglycerides.
2. Catabolism: glucagon, epinephrine, cortisol. Stored foodstuffs (in cells), glycogen, proteins, triglycerides available foodstuffs (in blood), glucose, amino acids, free fatty acids.
3. Pancreas: exocrine and endocrine. Exocrine: released digestive juices through a duct to the
duodenum. Endocrine: release hormones into the blood.
4. Islets of Langerhans: a key player in the endocrine systems control of metabolism is the pancreas. Alpha Cells: glucagon. Beta Cells: insulin and amylin. Delta Cells: somatostatin. F Cells: pancreatic polypeptide.
5. Glucagon: causes cells to release stored food into blood; increases blood glucose.
6. Insulin: allows cells to take up glucose from blood; lowers blood glucose. Released in biphasic manner; 1st phase peaks at 3-5 min, 2nd phase begins at 2 min and continues ~60 min or until stimulus stops.
7. Amylin: slows glucose absorption in small intestine; suppressed glucagon secretion (lowers blood glucose).
8. Somatostatin: decreased GI activity; suppresses glucagon and insulin secretion.
9. Insulin Promotes Anabolism and Lowers Plasma Glucose by increasing glucose transport into most insulin-sensitive cells, enhancing cellular utilization and storage of glucose, enhancing utilization of amino acids, and promotes fat synthesis.
10. Type 1 DM: pancreatic beta cell destruction predominantly by an autoimmune process. 11.Type 2 DM: a combination of beta cell dysfunction and insulin resistance.
12. Other types: genetic defects in insulin production (beta cells), genetic defects in insulin action, disease of the exocrine pancreas, diabetes secondary to other disease: endocrinopathies, drug/chemical/infection-induced diabetes, gestational DM.
13. Type 1 DM: insulin deficiency resulting from pancreatic beta cell destruction. 5-10% of people with DM have type 1. Usually diagnosed between 5 and 20 years of age. Etiology may be immune-mediated or idiopathic (without autoimmune markers). Overproduction of glucagon stimulates glycogenolysis and glycogenesis, leading to hyperglycemia and glucosuria, causing polyuria, polydipsia, polyphagia, and ketoacidosis (elevated ketone bodies used as energy as an alternative to glucose). Requires exogenous insulin replacement to reverse the catabolic state, control blood glucose levels and prevent ketosis.
14. Type 2 DM (insulin resistant diabetes): impaired ability of tissues to use insulin accompanied by a relative lack of insulin or impaired release of insulin from dysfunctional beta cells. Accounts for 90% to 95% of persons with diabetes but is becoming common in obese and children (non-Caucasian and elderly are disproportionately affected). Insulin levels are normal or elevated initially but become insulin deficient. Pathophysiology involves both genetic and acquired factors. Polyuria, polydipsia, and polyphagia may be more subtle. Ketoacidosis is uncommon. *** Impaired insulin secretion,
carbohydrate absorption, increased basal hepatic glucose production, decreased insulin-stimulated glucose uptake. Tx: peripheral glucose uptake: thiazolidinediones. Hepatic glucose output: biguanides.
15. Metabolic Syndrome: combination of type 2 diabetes, atherosclerosis, and hypertension. Have atleast 3 of the following: central obesity (40 vs 35 in M vs F), BP > 130/85 (or taking BP meds), increased fasting blood glucose > 110 mg/dL, elevated fasting plasma triglyceride above 150 mg/dL or taking meds, low plasma HDL-C levels (lower than 40 in men, 50 in women.
16. Gestational Diabetes: refers to glucose intolerance that is detected first during pregnancy. Closely resembles type 2. Most likely precipitated by the presence of placental hormones. Occurs in 2-14% of pregnancy, usually in women with hx of diabetes, glucosuria in family, history of stillbirth, obesity, AMA, 5+ pregnancies. Tx: diet, exercise, and blood glucose/ketone monitoring.
17. Osmolarity in DM: when blood glucose in high, increased blood osmolarity can cause cells to shrink to the hypertonic solution. Nerve cells produce intracellular osmoles to keep their osmolarity balanced with the blood. When the client brings blood glucose back to normal, the nerve cells are hyperosmolar to the blood and gain water, swelling. Nerve damage may be caused by swelling.
18. Diabetic Neuropathy: somatic neuropathy: diminished perception of vibration, pain, and temperature.
Hypersensitivity to light touch; occasionally severe “burning” pain.
19. Autonomic Neuropathy: defects in vasomotor and cardiac responses. Impaired motility of the gastrointestinal tract, inability to empty the bladder, sexual dysfunction.
20. Carb counting, exercise, and insulin are therapies for Type 1 DM. 21.Microvascular complications of DM include retinopathy and nephropathy. 22. Diabetic neuropathy is due to decrease in myoinositol transport. 23.Type 2 DM is due to insulin resistance and b cell dysfunction.
24. Obesity is a major predictor in Type 2 DM.
Chapter 40
25. Polyuria, polydipsia, polyphagia are clinical findings for Type 1 DM. 26.Type 1 DM is due to pancreatic b cell destruction.
27. Hypoglycemia will present with tremors.
28. Type 2 DM is associated with nonketotic hyperosmolality.
29. HbA1c levels are most important in evaluating DM long term.
1. Hypothalamus (pituitary axis): releasing hormones from the hypothalamus tell the pituitary what to release into the blood. Trophic hormones from the pituitary tell specific peripheral glands to grow and produce their hormones.
2. Hypo/Hypersecretion can occur in the hypothalamus/pituitary (secondary) or the hormone-producing gland (primary) or the target tissue. Etiology can be congenital, infectious, autoimmune, neoplastic, idiopathic, iatrogenic.
3. Pituitary Hormones: GH, FSH and LH (stimulate gonads), TSH (stimulates thyroid), ACTH (stimulates adrenal cortex).
4. Thyroid: releases T3 and T4. Both are carried by binding proteins since they are steroid hormones. T3 stimulates metabolism. T4 is inactive until converted to T3 in the issues. Both exert negative feedback on the hypothalamus.
5. Lack of Iodine: T3 and T4 are not made. There is no negative feedback. TRH and TSH continue to be made. The thyroid may grow in response to TSH.
6. Actions of Thyroid Hormone: increases metabolic rate and protein synthesis. With increased metabolism, there is an increase in cardiovascular function (oxygen consumption, blood volume, cardiac output, etc.). Enhances GI function and increases appetite. Necessary for normal growth and development in children (mental development and sexual maturity). Myelin and synapse formation. Enhances neural control of muscle, making them react more vigorously.
7. Congenital Hypothyroidism: affects 1 in 5000 infants who appear normal at birth because of maternal thyroid hormone, but if untreated can lead to cretinism, a form of preventable mental retardation since thyroid hormone is essential for brain development and growth.
8. Acquired Hypothyroidism: hashimotos thyroiditis, thyroidectomy, iodine deficiency. Develops later in life because of a primary disease of the thyroid gland or secondary to disorders of hypothalamic or pituitary origin. Causes a general slowing down of metabolic processes. Most common cause id Hashimoto thyroiditis, an autoimmune destruction of the thyroid gland. Weakness and fatigue, a tendency to fain weight despite a loss of appetite and cold intolerance. Brittle nails, thinning hair, dry and thin skin. Bradycardia.
9. Hyperthyroidism (Graves Disease): autoimmune disorder, abnormal stimulation of the thyroid gland by thyroid-stimulating immunoglobins, TSI, that act as TSH. Goiter and exophthalmos or bulging of eyeballs. Thyroid tumors.
10. Hyperthyroidism Manifestations: increased O2 consumption, increased sympathetic system, nervousness, irritability, fatigability, weight loss, despite large appetite, tachycardia, shortness of breath, excessive sweating, muscle cramps, heat intolerance.
11. Parathyroid Hormone: normal level is 8.5-10.5 mg/dL. Extracellular, blocks Na gates in nerve and muscle cells, clotting, leaks into cardiac muscle causing it to fire; intracellular needed for muscle contraction, acts as a second messenger in many hormone and neurotransmitter pathways.
12. Parathyroid Hormone: secreted from PT gland. Is a major regulator of plasma Ca and phosphate. PTH raises Ca and mobilizes Ca from bones (activates osteoclasts), enhances renal reabsorption of Ca, indirectly increases intestinal absorption of Ca through its influence on Vit D.
13. Hypoparathyroidism: deficient PTH secretion, resulting in hypocalcemia. May be due to congenital absence of parathyroid gland, as in DiGeorge gland; acquired deficiency of PTH after neck surgery,
autoimmune disease or infection, magnesium deficiency. Manifestations: tetany and muscle cramps, convulsions, hypotension, lethargy, anxiety, personality changes.
14. Hyperparathyroidism: hypersecretion of PTH, may be due to secondary hyperparathyroidism- involves hyperplasia of the parathyroid gland due to renal failure (reduced production of active vitamin D, impairs calcium absorption. Primary hyperparathyroidism- common disorder, due to hyperplasia of the parathyroid gland. Manifestations: hypercalcemia and increased calcium in urine filtrate and potential development of kidney stones. Chronic bone resorption may produce diffuse demineralization, pathologic fractures, cystic bone lesion, and skeletal abnormalities.
15. Excessive growth hormone in adults leads to acromegaly. 16.Diabetes insipidus is a result from inadequate ADH secretion. 17.The synthesis of thyroid hormone is inhibited by iodine deficiency.
Chapter 37, 38
1. Liver: digestive organ: bile salt secretion for fat digestion, processing and storage of fats, carbs, proteins, and processing and storage of vitamins and minerals. Endocrine organ: regulation of carb, fat, and protein metabolism. Metabolism of glucocorticoids, mineralocorticoid, sex hormones. Hematologic organ: temporary storage of blood, removal of bilirubin from blood stream, hematopoiesis in certain disease states, synthesis of blood-clotting factors. excretory organ: excretion of bile pigment and cholesterol, urea synthesis, detoxification of drugs and other foreign substances.
2. Liver failure leads to:
Hematologic disorders: anemia, coagulation defects, leukopenia.
Endocrine disorders: fluid retention, hypokalemia, disordered sexual functions. Skin disorders: jaundice, red palms
Hepatorenal syndrome: low kidney function due to liver failure via constriction of the renal blood flow, leads to azotemia (i.e. urea).
3. Other S&S: abdominal pain/tenderness from liver inflammation, nausea and anorexia from systemic effects of inflammation, fatigue and weight loss from failure of hepatic metabolism, peripheral edema from accumulation of fluid retained because of decreased plasma protein production and loss of albumin with ascites (accumulation of fluid in the peritoneal cavity).
4. Gallstones are more common in women.
5. Untreated acute cholecystitis may lead to gangrene.
6. Alcoholism is associated with more than half the cases of pancreatitis.
7. Chronic cholecystitis can lead to biliary sepsis, calcified gallbladder, and porcelain gallbladder. 8. Gallstones are composed of cholesterol.
9. Elevated serum lipase and amylase levels are associated with pancreatitis. 10.Chronic pancreatitis may lead to DM.
11. Cholecystitis: inflammation of the gallbladder, often caused by cholelithiasis, or gallstones, which is caused by precipitation of substances contained in bile, mainly cholesterol and bilirubin.
12. Factors contributing to gallstone formation: abnormalities in the composition of bile, stasis of bile, inflammation of the gallbladder. Associated with obesity and occurs frequently in women, especially those with multiple pregnancies or those taking OCP’s because it results in more cholesterol excretion into the bile.
13. Bile in the Intestines emulsifies fats so they can be digested. Passes on to the large intestine: bacteria convert it to urobilinogen, some is lost in feces, most is reabsorbed into the blood and returned to the liver for reuse/filtered out by the kidneys and made into urine.
14. Pancreas: endocrine and exocrine organ. The exocrine pancreas secretes digestive proteolytic enzymes that breakdown proteins, starches, and fats. Enzymes are secreted in the inactive form and become activated in the intestine.
15. Exocrine Pancreas releases digestive juices through a duct to the duodenum. 16.Endocrine pancreas: released hormones into the blood and makes insulin, glucagon, etc.
17. Biliary Reflux: gallbladder contracts bile is sent down common bile duct blockage forms and
bile cannot enter the duodenum bile goes up pancreatic duct bile in pancreas disrupts tissues; digestive enzymes activated
18. Autodigestion of the Pancreas: activated enzymes begin to digest the pancreas cells and results in severe pain and inflammation producing large volumes of serous exudate hypovolemia. Enzymes
(amylase, lipase) appear in the blood. Areas of dead cells undergo fat necrosis calcium from the
blood deposits in them hypocalcemia.
19. Acute Pancreatitis: inflammation of the pancreas, severe, life-threatening. Associated with the escape of activated pancreatic enzymes into the pancreas and surrounding tissues. Causes fat necrosis, or autodigestion, of the pancreas and produce fatty deposits in the abdominal cavity with hemorrhage from necrotic vessels.
20. Chronic Pancreatitis and Pancreatic Cancer: similar signs. Often have digestive problems because of the inability to deliver enzymes to the duodenum, glucose control problems because of damage to islets of Langerhans, signs of biliary obstruction because of underlying bile tract disorders or duct compression tumors.
21. HEP B is transmitted by exposure to blood or semen. 22.Hepatitis will present with an increase in urine bilirubin,
23.Acute Hep B will present with a positive Hep B surface antigen HBsAG. 24.Steatohepatitis is an accumulation of fat in the liver cells.
Chapter 36
1. Bowels: digest foods (involves a corrosive solution and potentially pathogenic bacteria), absorbs food into the blood while keeping the corrosive substance and bacteria inside the gut, keeps the solution moving down the bowel at the right rate for digestion and absorption.
2. Gastroesophageal varices will be present with a h/o alcoholism with hematemesis and profound anemia.
3. Esophageal varices are associated with portal hypertension. 4. Dumping syndrome seen after gastric bypass surgery.
5. Chemo may cause stomatitis. 6. H. Pylori causes chronic gastritis.
7. Rupture of esophageal varices has a high mortality rate. 8. Necrotizing enterocolitis is associated with bloody diarrhea. 9. Colon cancer has a warning sign of change in bowel habits.
10.Celiac sprue is a malabsorptive disorder from a reaction to gluten containing foods. 11.Barrett esophagus is a preneoplastic condition.
12. Hiatal hernia will present with heartburn.
13. Gastric ulcers can present with epigastric pain relieved by food.
14. Appendicitis presents with acute right lower quadrant pain associated with rebound tenderness and systemic signs of inflammation.
15. Inflammation and Damage to the Bowel wall can lead to hemorrhage (anemia), perforation (periostitis), decreased mucosal function (malabsorption), decreased bacterial containment (sepsis).
16. Hemorrhage above the stomach: frank hematemesis (vomiting of blood).
17. Hemorrhage into the stomach with partial digestion of blood: coffee-grounds vomit. 18.Hemorrhage in the intestine with blood mixing into stools: occult blood 19.Hemorrhage into the intestines with large volumes of blood: melena (black feces). 20.Hemorrhage in the rectum: red blood coating stools.
21.Peptic Ulcer Disease (PUD): peptic ulcers are lesion in the mucosal membrane extending below the epithelium, can develop in the lower esophagus, stomach, pylorus, duodenum, or jejunum. Most common in men between ages 20 and 50. Exacerbated by alcohol or tobacco.
22.H Pylori is a major cause of ulcers. Can damage stomach lining. Passed through saliva, is well adapted to survive acidic stomach environment, releases a toxin that destroys gastric and duodenal mucosa. This reduces the epithelium’s resistance to acid digestion. NSAID’s contribute to PUD by inhibiting the secretion of prostaglandins which block ulcerations.
23. PUD Predisposing Factors: blood type (Type A: gastric ulcers, Type O: duodenal ulcers), H pylori, exposure to irritants contribute to accelerating gastric acid emptying and promoting mucosal breakdown, emotional stress because of the increased stimulation of acid and pepsin secretion and decreased mucosal defense, physical trauma, normal aging, genetics, NSAIDs.
24. Tx: H pylori abx, avoid predisposing factors.
25. IBS: normally, segmental muscle contractions mix intestinal contents while peristalsis propel the contents through the GI tract, motor activity is most propulsive in the proximal (stomach) and distal portions of the intestine, activity in the rest of the intestine is slow, permitting nutrient and water absorption.
26. IBS: the autonomic nervous system, which innervates the large intestine, doesn’t cause the alternating contractions and relaxations that propel stools smoothly toward the rectum. Chronic
>3 months functional disorder. S&S: abdominal pain, fluctuations in stool frequency and
consistency, excess gas, sense of incomplete evacuation, abdominal distention, nausea, bloating, mucus in stool.
27. Constipation: spasmodic intestinal contractions that set up a partial obstruction by trapping gas and stools. Causes distention, bloating, gas pain resulting in constipation.
28. Diarrhea: dramatically increased intestinal motility. Eating or cholinergic stimulation triggers the contents of the small intestine to rush into the large intestine, dumping watery stools and irritating the mucosa, resulting in diarrhea.
29. IBS caused by hormonal changes, ingestion of irritation, lactose intolerance, laxative abuse, anxiety and depression.
30. Tx: antidiarrheal, antispasmodic, increased fiber.
31. Gastrointestinal Bleeding: upper- originates in the first part of the GI tract- the esophagus, stomach, or duodenum. Bleeding from ingestion of caustic poisons or stomach cancer. Most often caused by peptic ulcers, gastritis, esophageal varices, Mallory-Weiss tears.
32. Peptic Ulcer Disease (Upper GIB): erosions of the digestive tract wall (usually stomach or duodenum). Mucous membrane breaks down, are unable to counteract the harsh stomach acid, causing bleeding. NSAIDS, aspirin, alcohol, tobacco, and H Pylori promote gastric ulcers.
33. Gastritis (Upper GIB): general inflammation of stomach wall or inability of gastric lining to protect itself from acids, can result in bleeding. NSAIDS, steroids, alcohol, burns, and trauma can cause gastritis.
34. Esophageal Varices (Upper GIB): swelling in veins of esophagus or stomach usually result from liver disease and portal hypertension. Varices most commonly result from alcoholic liver cirrhosis (scarring), high mortality rate.
35. Mallory-Weiss Tear (upper GIB): tear in the mucosa or submucosa of the esophageal or stomach wall. Often as a result of forceful or prolonged vomiting. Tears also occur after seizures, forceful coughing or laughing, childbirth, excessive alcohol, trauma.
36. Lower GI bleeding originates in the GI tract, small intestines, large intestines, rectum, and anus. 37.Diverticulosis (lower GI): small out-pockets form on large intestine wall.
38. Angiodysplasia (lower GI): malformation of the blood vessels in the wall of the GI tract. Elderly and people with CKF develop the disease most often.
39. Polyps: noncancerous tumors of the GI tract, occurring mostly in people older than 40. May transform into cancer.
40. Hemorrhoids and fissures: swellings of veins in and around your rectum. Repeating stretching from straining at stool causes them to bleed. Anal fissures are tears in the anal wall that cause bleeding. Forceful straining during passage of hard stool usually causes such tears.
Chapter 44
1. Cerebral aneurysms present with a severe, sudden headache. 2. Risk factors and symptoms for meningitis.
3. Encephalitis is caused by a viral infection.
4. During acute stroke it is important to distinguish between ischemic vs hemorrhagic: ischemic- caused by an interruption of blood flow in a cerebral vessel (common type of stroke 70-80%). Hemorrhagic- caused by bleeding into brain tissue, usually from a blood vessel rupture caused by hypertension, aneurysms, arteriovenous malformations, or head injury.
5. Stroke of one side of cerebral hemisphere will affect the contralateral side. 6. BP is a risk factor for hemorrhagic stroke.
7. Cerebral aneurysm results in subarachnoid hemorrhage. 8. Acute hypertension is a risk factor for hemorrhagic stroke.
9. Parkinson disease is a deficiency of dopamine in substantia nigra. 10. Parkinson disease will give rest tremor and skeletal muscle rigidity. 11. Pain is subjective and difficult to measure.
12. One common cause of acute pain is headache.
13. Migraine will present as severe, pounding headache with nausea and photophobia. 14. Multiple myeloma has a common symptom of bone pain.
15. Lateral curvature, increase in periods of rapid growth, uneven shoulders, scapular prominence, and respiratory complications are all characteristics of scoliosis.
16. Diabetes, smoking, and poor diet can lead to delayed healing in fracture.
17. Paget’s disease is excessive bone resorption followed by excessive formation of fragile bone.
18. The most common site for Paget’s disease is the lower spine. 19. Osteomyelitis is hematogenous.
20. Osteosarcoma is a malignant bone forming tumor.
21. Osteomalacia is a bone disorder that comes from insufficient Vitamin D in adults. Rickets is the term used for children.
22. Early menopause is a risk factor for osteoporosis.
23. Malunion is a fractured bone that heals with poor alignment. 24. Different types of fractures:
Transverse: straight across
Oblique: straight across but diagonal. Spiral: a literal spiral around the bone
Comminuted: chunk in the middle that is crushed into pieces. Segmental: 1-inch chunk that can be taken out
Butterfly
Impacted: two bones smash into each other
25. Muscle strains are caused by abnormal contractions. 26. Osteoporosis can lead to bone fractures.
27. Phases of bone healing.
28. Difference between osteoarthritis and rheumatoid arthritis. 29. SLE is autoimmune
30. SLE has a classic presentation of a butterfly rash.
31. Ankylosing spondylitis has inflammation, stiffness, and fusion of spinal joints. 32. Gouty arthritis is an inadequate renal excretion of uric acid.
33. Rheumatoid arthritis is a systemic inflammatory condition.
34. Disturbed uric acid metabolism, crystalline deposits in bony and connective tissue, cardiac involvement, and renal involvement are all characteristics of gout.
[Show More]
Last updated: 3 years ago
Preview 1 out of 57 pages