EMPOWERING. UNITING. ADVANCING All Nurses | PANDEMIC THE COVID-19 Crisis
Document Content and Description Below
EMPOWERING. UNITING. ADVANCING.
Spring 2020 allnurses.com
PANDEMIC
THE COVID-19
CRISISMembership
has its privileges
• FREE registration
• FREE support
• FREE magazine alerts for new issu
...
es
• FREE content alerts
• Networking
• Job Search
• Anonymous posting (real name optional)
allnurses.com is all about anonymity. Anonymity allows nurses to
share insights, to post questions freely without fear of losing their
job, and to learn and gain from other’s experiences.
Tap NOW to Become a Member
Become a member today for FREE!Spring 2020 allnurses 3
Multiple Locations.
One Mission.
Live Your Best Life.
Hundreds
of Career
Opportunities
Tap Photos to
Find Your New
Career.4 Spring 2020 allnurses
Dave Smits C.E.O.
EMPOWERING. UNITING. ADVANCING.
EDITORS / CONTRIBUTING WRITERS
Mary Watts, BSN, RN
Natalia Dabrowska, MSN-CNL, RN
Dr. Kristi Miller, PhD
Kathy Day, RN
Brian Sorenson
allnurses is published quarterly by
allnurses.com, Inc., 7900 International Dr., Suite 300, Bloomington, MN 55425
All rights reserved. Reproduction in whole or part without written
permission of the publisher is prohibited. The opinions of contributing writers
to this publication do not necessarily reflect the views of allnurses.com, Inc.
Copyright © 2020 by allnurses.com. All rights reserved.
Products featured within these pages do not constitute an endorsement by
allnurses.com.
7900 International Drive, Suite 300
Bloomington, MN 55425
Phone: 612-816-8773
email: [email protected]
Website: allnurses.com
Gregg Knorn
Sales Director
[email protected]
Mary Watts
Content & Community Director
[email protected]
Brian Sorenson
Marketing Director
[email protected]
Joe Velez
Technology Director
[email protected]
Julie Bollinger
Business Operations Director
[email protected]
Resources
CDC.gov
COVID-19 Global Cases
Financial Times COVD-19 charts
Project N95
American Red Cross
allnurses.com COVID-19 forum
ARTICLE CONTEST!
HOW IS COVID-19
AFFECTING YOUR LIFE?
click for more info and to submit
winners will share the $300 prize
ANYONE CAN ENTER!
CONTENT MUST COMPLY WITH OUR RULES AND TERMS
OF SERVICE. NO SOLICITATION. MINIMUM OF 600 WORDS.
NO PLAGIARISM. ARTICLES WILL BE REVIEWED BY STAFF
PRIOR TO PUBLICATION. YOU MAY SUBMIT MUTIPLE
ARTICLES. CHECK GRAMMAR, PUNCTUATION, AND
SPELLING PRIOR TO SUBMISSION.Contents
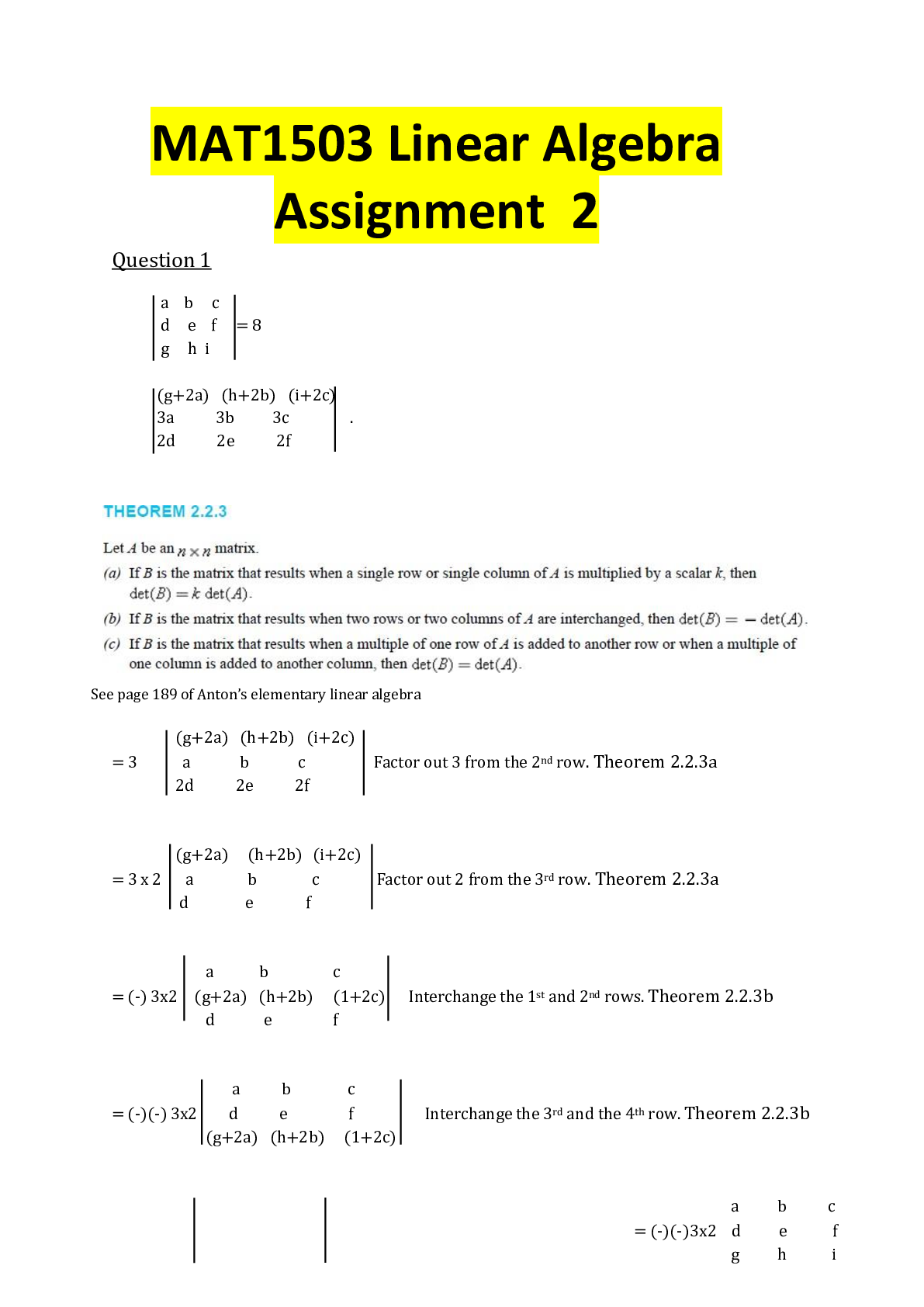
36
Warm Weather Will
Slow the Virus and
Other Bad Advice
By Dr. Kristi Miller
The COVID-19 Battle
Cry for Retired Nurses
By Kathy Day, RN
Shelter in Place, Stay at
Home... What Does it Mean?
A COVID-19 Dilemma:
Where are all the PPEs?
By Mary Watts, BSN, RN
The Real War Against
COVID-19 in America
By Natalia Dabrowska, MSN-CNL, RN
The Origins of COVID-19
46
7
16
10
326 Spring 2020 allnurses
The COVID-19 pandemic is and
likely will be the top story for not
only nurses and medical professionals but the population as a whole for
the forseeable future.
With a pandemic like the one
currently ravaging the globe, there
are stories fron the front lines which
need to be heard. Nurses treating
patients in hallways, waiting rooms,
and tents is now a common occurrence.
Shortages of once commonplace
equipment as seemingly basic as
N95 masks have seen the concerned
citizens of America take to their
sewing machines to make masks for
nurses, doctors, and other medical
profesionals.
The exponential growth in
COVID-19 cases in “hot zones” in
the states of New York, California,
Washington, Louisiana, and Florida
We welcome your story ideas.
Reach us at
[email protected]
Editor’s Note
Contact us
shows that the work of nurses in these
and other locations is likely just beginning. Even more startling is how
the COVID-19 pandemic is playing
out in Italy, France, Spain, and other
European countries.
While phrases such as social
distancing, shelter in place, and
flattening the curve are becoming
commonplace in conversations being
heard across the country and around
the globe, talk only goes so far.
With all of that having been said,
this issue of allnurses Magazine is
all about what seems to be the only
issue in the nursing universe today
– COVID-19. We have insight and
stories from all corners of the country. Data on the pandemic both in the
United States and around the globe.
Now, more than ever, we want to extend a huge THANK YOU to nurses
both here and abroad. Stay safe and
stay healthy.
Connect
allnursesrock
allnursescom
allnurses
@allnurses
@allnurses
allnurses
Brian Sorenson
Editor, allnurses MagazineSpring 2020 allnurses 7
It started in California with Governor Gavin Newsom
ordeering residents to “shelter in place”. New York Governor Andrew Cuomo quickly followed suit by requiring
residents to stay indoors except for essential trips and
services. Since those two orders came down, 16 states
and a number of cities have announced stay-at-home
orders.
But what is the difference between “stay at home” and
“shelter in place”? Here’s what we’ve been able to learn
so far.
Essentially, sheltering in place means staying at home,
the order from San Francisco’s Department of Public
Health says.
“Widespread testing for COVID-19 is not yet available but is expected to increase in the coming days,”
the mandate from San Francisco’s Department of
Health says. “This order is necessary to slow the rate
of spread.”
“‘Shelter in place’ is a scary term for people,” New
York Governor Andrew Cuomo said during a news
conference on Thursday. “I believe communication
is important, and I believe words are important.
Say what you mean and don’t say what might alarm
people.”
What does a shelter-in-place
order prohibit?
In the San Francisco Bay Area, the mandate prohibits going outside, with certain exceptions for
different groups of people. Vulnerable people, which
include the elderly, minors and people with disabilities, should not go out at all, according to the
order. Anyone who is at risk of severe illness from
COVID-19 is also urged to stay inside.
Who is exempt from a
shelter-in-place order?
People can leave their house for “essential activities,” which include getting medical supplies, going to
the doctor or getting supplies needed to adequately
work from home. They can also go out to get groceries.
People can also go out to run, walk or hike as long
Shelter in Place,
Stay at Home
What it means, where it’s happening,
and how it can help8 Spring 2020 allnurses
as they maintain the requirements of social distancing and stay at least six feet away from other individuals.
Those whose work is considered “essential” are
also permitted to leave the house to continue their
work. Essential businesses include health care facilities, grocery stores and other food markets, banks,
media services, hardware stores, laundromats and
delivery services, among others.
Where are these orders
in effect?
As of this writing, sixteen states including Washington, New Mexico, Hawaii, Wisconsin, West
Virginia, Michigan, Indiana, New Jersey, Oregon,
Illinois, New York, Connecticut, California, Louisiana, Ohio and Delaware have announce statewide
stay-at-home orders. Non-essential businesses in
Nevada, Maryland, Pennsylvania, Kentucky and
Massachusetts have been ordered to close but these
states have stopped short of issuing stay-at-home
orders. A number of cities including Atlanta, Philadelphis, New Orleans, Kansas City and St. Louis
have also issued stay-at-home orders.
How does it help?
While data is still in the very early stages, the San
Francisco area has seem a leveling off of identified
cases of COVID-19. Officials are hoping that these
orders – while they vary in inclusiveness – serve to
stem the tide of COVID-19 infections and, in turn,
prevent a wave of individuals who require hospitalization. In short, staying at home or sheltering in
place leads to another current phrase – flattening
the curve.
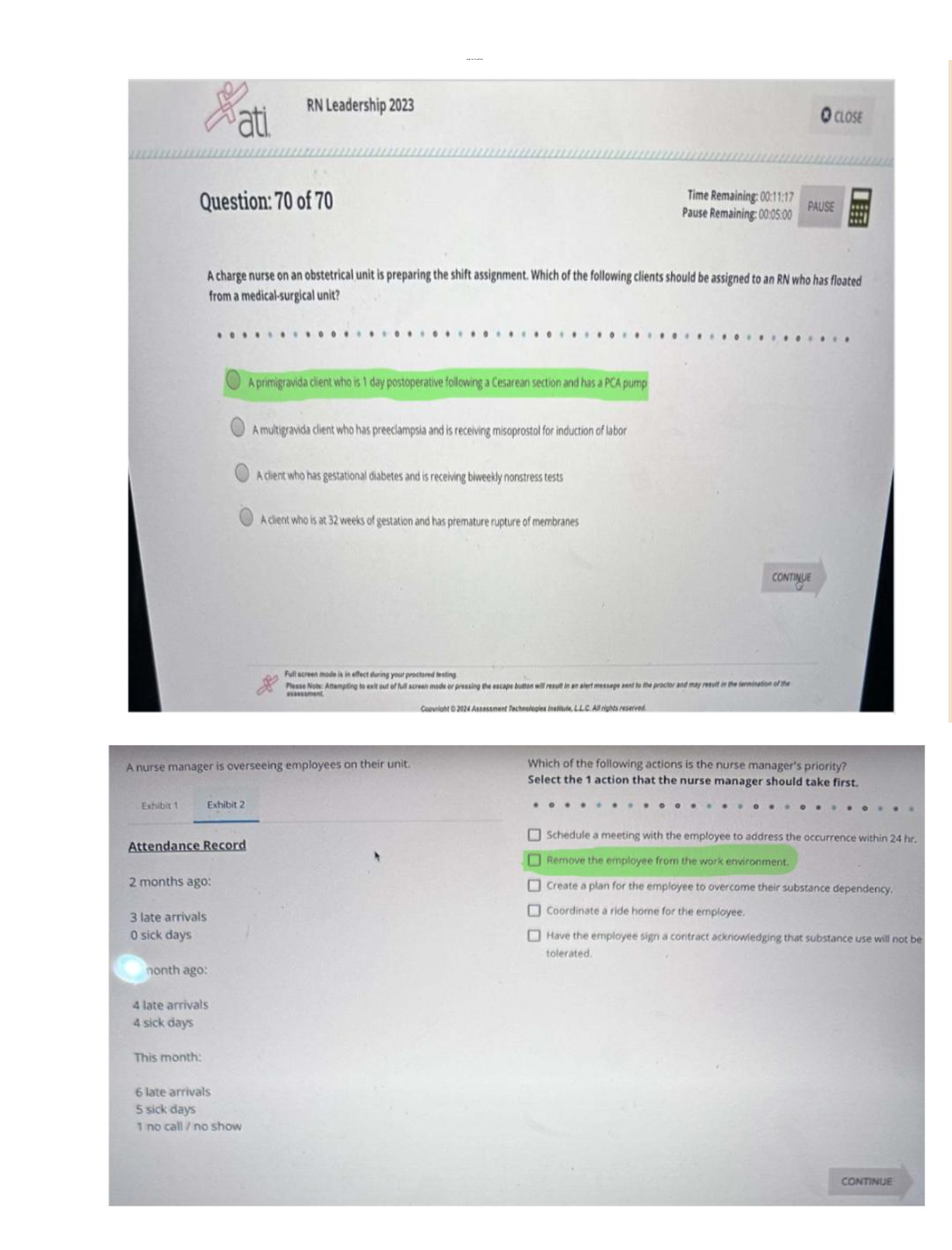
Are these measures helping? Possibly. The charts
below show a comparison between New York and
California. Judge for yourself.
via https://www.sfchronicle.com/health/article/NY-has-10-times-the-coronavirus-cases-CA-has-Why-15154692.php
Virus’ explosive
growth in New York
Case totals as of 6 PM Tuesday, March 24
Coronavirus cases have surged in New
York compared with California. Early
California public health responses, including shelter-in-place orders, may be
one reason. New York has also tested
for more people than California.Spring 2020 allnurses 9
ONLINE RN
TO BSN
Open doors.
Expand your career.
LEARN MORE10 Spring 2020 allnurses
The Real
War Against
COVID-19 in
America
By Natalia Dabrowska, MSN-CNL, RNSpring 2020 allnurses 1112 Spring 2020 allnurses
Change for the Future
In all the craziness in the midst of COVID-19, it
is easy to only focus on the present, but we cannot
forget to elicit change for the future as well. If we
don’t do it now, it may never be done. No more
pushing it off or putting it on the back burner with,
“Well this is how it’s always been.” That clearly
does not work.
Shortages of Staff and
Equipment
I am currently working across three different
hospitals navigating this pandemic. Like everywhere else in the country, there is a shortage
of masks, equipment, PPE, possibly ventilators
and beds. There is also already a shortage of
nurses and staff on a GOOD day, without these
huge spikes of hospitalizations flooding in. Well
here’s some news that nurses have always known:
There is not actually a shortage of nurses—There
is a shortage of nurses willing to work UNDER
THESE CONDITIONS.
Case and point: While we are being called to
the front lines without proper gear, being rationed
protective equipment, we ourselves are not being
rationed. For instance, my main job is as a pediatric pulmonary nurse coordinator. I have two other
nurses who share this same role with me. Usually
one of us is in the office, one of us is with patients,
and the third may work on the Cystic Fibrosis registry and research. In an effort to reduce exposure
to patients, we cancelled all non-urgent appointSpring 2020 allnurses 13
ments, testing, research, etc. This put all THREE
of us coordinators in the office the same day.
One of our doctors was fuming. She said each of
our chances of contracting COVID-19 is OVER
50% and if one falls down we ALL fall down.
Still, administration and management did not
budge. They continue to lead “updates” via zoom
meetings, where they sit on camera in sweatshirts
from the comfort of their own homes while we put
ourselves at risk.
A Time for Change
This is the first sign that it is time for change.
There is no room in healthcare for people who
choose to sit at home rather than jump into the
trenches when patients and entire communities
need us. The reason our Healthcare System so
often fails us is because there is NO room for it to
be business-driven and for-profit for a small group
of individuals ready to cash it all in.
Why Weren’t We Ready?
THAT is why we were not ready for something
like this. We should have been ready. There is no
excuse. Yet we weren’t because we have non-medical people making decisions along with medical
people who somehow never even put hands on
a patient. These are the people we let run the
show and it is shown time and time again that this
FAILS.
We are one of the most developed first world
countries on this planet and we continue to have
one of the worst healthcare systems. We have high
rates of maternal mortality, infant death, and others. There is NO excuse for this. We work shortstaffed or with unsafe assignments while “higher
up” people don’t care.
What they care about is apologizing to the patient who had a meltdown because the cafeteria put
orange juice on their lunch tray instead of apple
juice by mistake. They don’t support the patient’s
nurse who gets blamed for this even though she
kept a very sick patient alive that day while juggling 5 others for 12 or 16 hours. It is too often
a thankless job. And yet, the nurse who does this
day in and day out is the one who does NOT get
listened to about making changes and improving
workflow, patient care, and safety.
Who Cares About
Employees’ Health?
We give all of ourselves for a system that does
not even realize it would collapse without us. This
is even better shown with this example during this
pandemic: One of our CRNA’s worked side-byside a doctor during a five-hour surgery. This
“We should have
been ready. There is
no excuse.”doctor later became symptomatic and tested positive for COVID-19. The hospital told the CRNA
that he was exposed but could not get tested and
that he should self-monitor—but come to work
still. This group of CRNA’s later bought their own
respirators because the hospital could not provide
them with enough. Instead of applauding this, the
hospital told them they cannot wear them because
IT MIGHT MAKE PATIENTS AND VISITORS
NERVOUS. So, who cares
about our employees’ health
as long as we minimize any
concern for everyone else
(who is in even more danger
if our exposed employees are
walking around unprotected)?
We are at war during this
time with COVID-19. We
are at war and we are not
properly equipping our soldiers. We are at war and our
generals are sitting at home
hoping that not all of us fall
while fighting their battle
for them. We are at war and
having to sacrifice ourselves.
Make no mistake- medicine is built off of the sacrifices of our soldiers. We give up bathroom breaks,
lunch breaks, holidays with families, weekends,
sleep, and more. We even risk ourselves when we
know we shouldn’t. I once ripped my gloves off at a
micro-preemie delivery when it was believed mom
had an unknown infection. We had finally gotten
the tiny endotracheal tube in the right spot, about
6cm at the lip, and I had to tape it in place, with
what you can imagine was a tiny, tiny piece of tape.
This is always a rush to ensure we do not lose the
tube and get the baby stable as soon as possible.
The tape kept sticking my gloves and I couldn’t
peel it off, so I finally ripped
off the gloves and thereby
exposed myself to this baby
covered in maternal fluid.
I did this and do things
like this, because we all do
at some point in our careers,
because in this game of life
and death we try to win at
life as much as possible. We
do this because when we
have a really hard shift or a
death, part of what heals us
is being able to look back
on the situation and say, “I
did everything I could have
possibly done. I gave it my
all. We all did our best.”
My fear is that we may not
be able to say this when we
look back at COVID-19.
We are already at a loss and
drowning. We don’t have the equipment to do our
best and we may get knocked out in the process.
So we while we continue to try the best we can with
what we have, we cannot forget that when this war
“We are already at a
loss and drowning”Spring 2020 allnurses 15
is over, our war on the healthcare system is just
beginning.
Enough is Enough
We have to continue to come together and rise.
We finally have to say enough is enough and not
back down anymore. We have to storm the streets
and government buildings the way we are storming
the hospitals to fight this thing. We have to demand
safe staffing ratios. We have to demand appropriate
compensation. We have to demand a complete reform of the structure. We have to demand putting
selfless, medically competent people in charge to
pioneer our hospitals—those who come into the
trenches with us when we need leadership and all
hands on deck. We need to make our healthcare
system something better than using drowning
nurses as pillars and Press Ganey scores as the
entire foundation while our “leaders” sit on top in
the ivory tower.
Now More Than Ever
The time is now. No, actually, the time was
yesterday, was years ago, but the next best time
is now. We owe it to ourselves and we owe it
to our patients. We owe it to our communities
and to all those who will be joining this humbling workforce after us. These burdens we
have been carrying on our backs can be eased
with a paradigm shift. It is time to rebuild.
This war may be our hardest and most challenging one yet, but it is the most necessary,
now more than ever. Have something to say?
Click here to comment!16 Spring 2020 allnurses
A COVID-19
Dilemma:
Where are
all the PPEs?
By Mary Watts, BSN, RNSpring 2020 allnurses 17
The deadly Coronavirus Pandemic has evolved
into a much faster-growing monster than anticipated by many, infecting more than anyone could
imagine. Hospitals are filling up with Coronavirus
patients. ICU beds and ventilators are in short
supply. As frightening as the virus is, the doctors
and nurses on the front line of care are worried
more about the lack of adequate personal protective equipment including N95 masks, surgical
gowns, gloves, and eye gear. Without the proper
protection, doctors and nurses are risking their
lives daily as well as endangering their patients and
their families as they care for those infected with
the virus. Several healthcare professionals have
already been infected; some have even succumbed
to the disease.
Recommended Protective
Equipment
The Centers for Disease Control and Prevention
recommends health care workers should wear
protective gowns, gloves, goggles and masks while
treating potential and confirmed cases of Covid-19
to avoid exposure. But, to add to the frustration of
doctors and nurses, there has been some disagreement over which masks are needed. Previously, the
CDC advised this use of tight-fitting respirators
like the N95 or powered air-purifying respirators
(PAPRs) which cover the entire head. In early
March, the CDC updated its recommendation
by saying that regular surgical masks are an
acceptable option when examining or treating a
coronavirus patient. More than likely, this change
was based primarily on the “mask shortage” rather
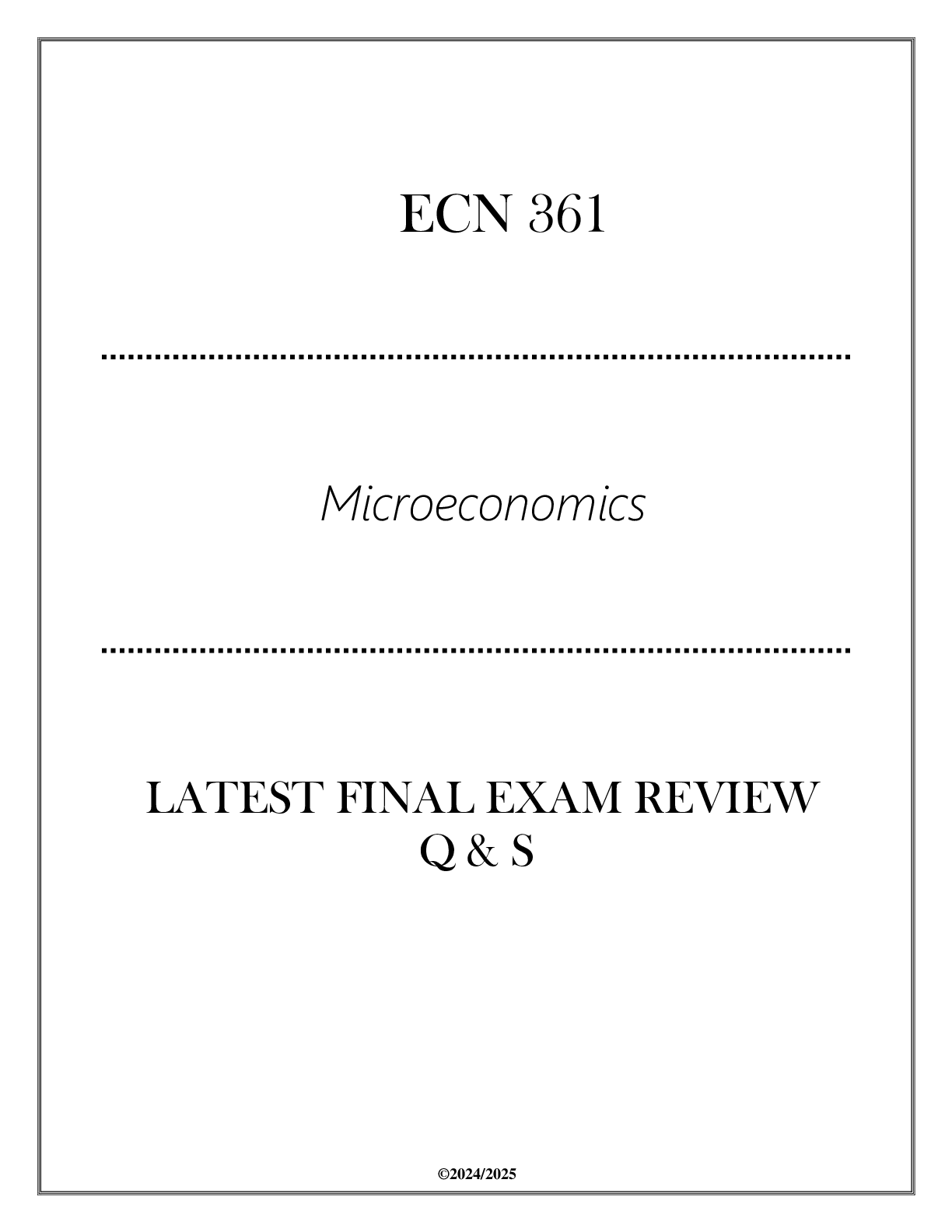
Eye Protection
Goggles or face shield
Respirator or
medical mask
N95 respirator,
if available
Gown
Closed securely
at the back
Gloves
Pulled up over
gown sleeves
Current CDC recommendations
for healthcare workers
“N95 masks are being reused indefinitely.
Since I worked PACU I hadn’t been sized, so
I was given a one size fits all mask. We aren’t
sanitizing them. The plan is to throw them in
a paper bag, and put them somewhere safe so
we can use them again during the next shift.”18 Spring 2020 allnurses
than on healthcare professional and patient safety.
Due to the shortage, many hospitals are requiring their staff to reuse
their masks, whether it be surgical masks or N95 respirators many
times, sometimes for up to 30 days, unless they become soiled.
Homemade Masks??
The CDC also stated the following:
“In settings where facemasks are not available, HCP might use homemade masks (e.g., bandana, scarf) for care of patients with COVID-19
as a last resort. However, homemade masks are not considered PPE,
since their capability to protect HCP is unknown. Caution should be
exercised when considering this option. Homemade masks should ideally be used in combination with a face shield that covers the entire front
(that extends to the chin or below) and sides of the face.” [via]
As a result of this statement, mask-making groups popped up all over
the country, trying to do whey they could to help protect the healthcare
providers.
So what’s all the fuss about? Isn’t a
mask a mask?
The FDA website offers a comparison of N95 respirators and surgical
masks, both of which are examples of PPEs that are used to protect the
wearer from airborne particles and from liquid contaminating the face.
Surgical masks
• Loose-fitting; does not provide complete protection
• Help block large-particle droplets, splashes, sprays, or splatter
that may contain viruses and bacteria
• Does not filter or block very small particles in the air that may be
transmitted by coughs, sneezes, or certain medical procedures
(COVID-19 is a small-particle)
• Not intended to be used more than once.
N95 Respirators
• A respiratory protective device designed to achieve a very close
facial fit and very efficient filtration of airborne particles
• Blocks at least 95 percent of very small (0.3 micron) test particles
• The filtration capabilities of N95 respirators exceed those of
surgical masks
• Not intended for public use
• Not intended to be reused
From the lists, you can see that nurses and doctors should be using a
tightly fitted N95 respirator designed to keep out more particles.
“I feel like our
government thinks this
is adequate protection
for us. And nothing will
change until we die. And
I don’t want to be one of
the deaths.”
“While I understand
people’s wants and
desires to help, I do
not feel that these are
acceptable alternatives.
We might as well go
in with no masks. I’d
personally rather use my
N95 for a week straight
than a mask that offers
virtually no protection.”
“This shines a light on
how the public truly has
no understanding of virus
transmission and how our
medical protective gear
works.
What scares me is that the
government feels these
are going to be acceptable
for us and that Americans
are answering the need
for our healthcare
workers, when they are
not.”Spring 2020 allnurses 19
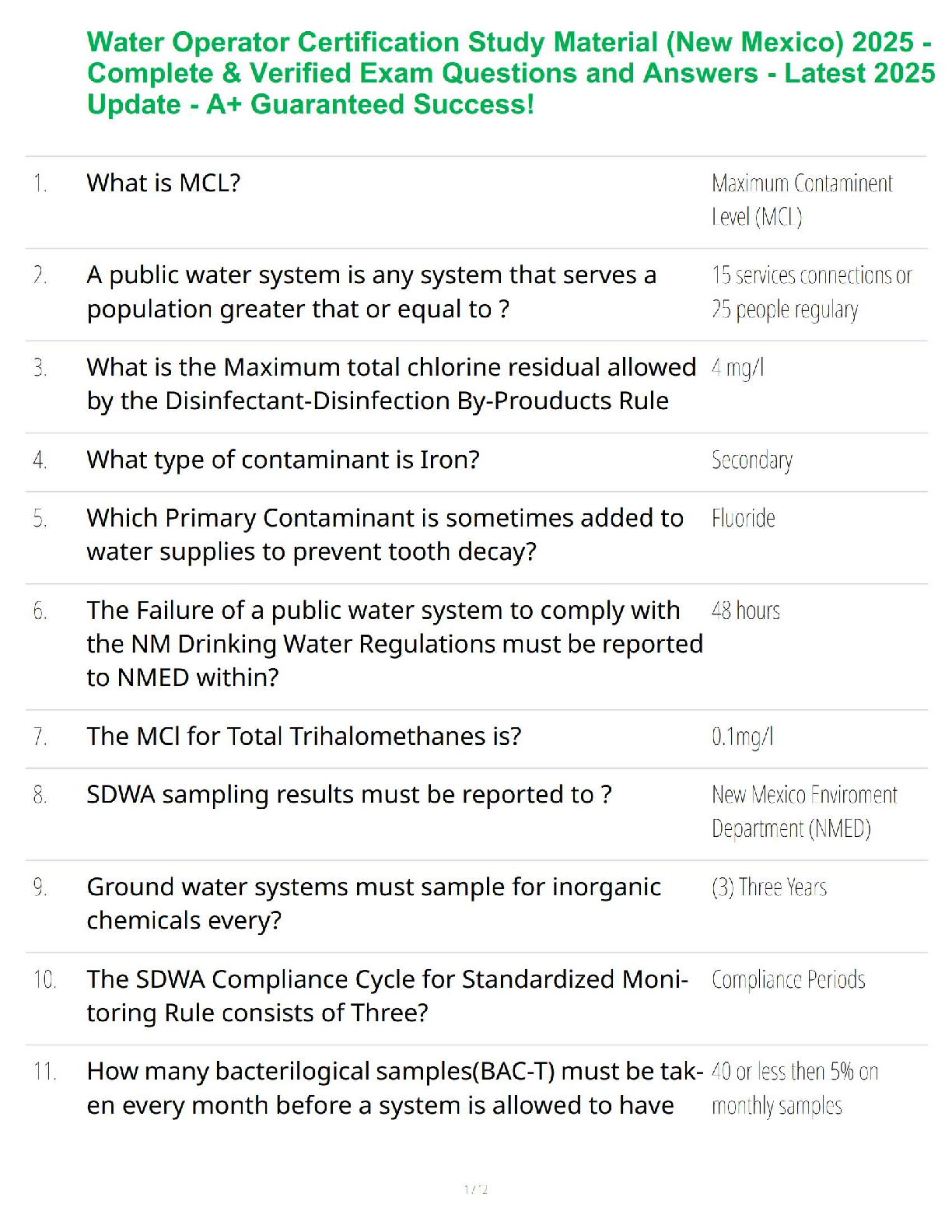
Centers for Disease Control
and Prevention
National Institute for Occupational
Safety and Health
Surgical Mask N95 Respirator
Testing and
Approval
Cleared by the U.S. Food and Drug
Administration (FDA)
Evaluated, tested, and approved by
NIOSH as per the requirements in
42 CFR Part 84
Intended Use
and Purpose
Fluid resistant and provides the wearer
protection against large droplets,
splashes, or sprays of bodily or other
hazardous fluids. Protects the patient
from the wearer’s respiratory emissions.
Reduces wearer’s exposure to particles
including small particle aerosols and
large droplets (only non-oil aerosols).
Face Seal Fit Loose-fitting Tight-fitting
Fit Testing
Requirement
No Yes
User Seal Check
Requirement
No Yes. Required each time the respirator
is donned (put on)
Filtration Does NOT provide the wearer with a
reliable level of protection from inhaling
smaller airborne particles and is not
considered respiratory protection
Filters out at least 95% of airborne
particles including large and small
particles
Leakage Leakage occurs around the edge of the
mask when user inhales
When properly fitted and donned,
minimal leakage occurs around edges
of the respirator when user inhales
Use Limitations Disposable. Discard after each patient
encounter.
Ideally should be discarded after each
patient encounter and after aerosolgenerating procedures. It should
also be discarded when it becomes
damaged or deformed; no longer
forms an effective seal to the face;
becomes wet or visibly dirty; breathing
becomes difficult; or if it becomes
contaminated with blood, respiratory
or nasal secretions, or other bodily
fluids from patients.
Understanding the Difference
! WARNING
Lorem ipsum dolor sit amet,
consectetur adipiscing elit. Nullam
scelerisque leo et eros convallis
condimentum. Phasellus tincidunt,
volutpat vitae.20 Spring 2020 allnurses
What’s Being Done to Get
More Masks and Other
Equipment?
Project Airbridge
A planeload of health care supplies arrived in
New York City on Sunday, March 29, from China.
This is part of an effort the White House says will
expedite the arrival of goods that are badly needed
to fight the coronavirus pandemic. According to
a White House statement, the shipment included
130,000 N95 masks, nearly 1.8 million other face
masks and gowns, more than 10.3 million gloves
and more than 70,000 thermometers. This is the
first of about 20 flights through early April for
a public-private partnership it’s calling Project
Airbridge.
Thank You
Hopefully, all healthcare professionals and
frontline responders will receive what they need to
provide protection for themselves, their patients,
and their families while continuing this battle
against a deadly Coronavirus. Until then, nurses
will continue to show up and provide compassionate care...because that’s what nurses do. They are
indeed heroes, and for that we thank you! Your
service and dedication does not go unnoticed.
If you want to share your story, please go to allnurses.com. We have a special COVID-19 Disaster forum where you can safely and anonymously
talk with other nurses.
References
https://www.nytimes.com/interactive/2020/03/11/us/virus-health-workers.html
https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/face-masks.html
https://www.fda.gov/medical-devices/personal-protective-equipment-infection-control/n95-respirators-and-surgical-masks-face-masks
https://www.npr.org/sections/coronavirus-live-updates/2020/03/29/823543513/project-airbridge-to-expeditearrival-of-needed-supplies-white-house-saysSpring 2020 allnurses 21
EASIER
YOUR JOB HUNT
JUST GOT
Nurses are more
in-demand than ever
before and finding your
new nursing career is
easier than ever. allnurses Jobs has been
rebuilt from the ground
up and is easier to use
than ever before.
Don’t wait. Get started
today!
Search Smarter22 Spring 2020 allnurses
January
31
Suspension of
Entry as
Immigrants
and Nonimmigrants of
Persons who
Pose a Risk of
Transmitting
2019 Novel
Coronavirus
COVID-19
cases in
United States:
6
February
29
Suspension of
Entry as
Immigrants and
Nonimmigrants
of Certain
Additional
Persons Who
Pose a Risk of
Transmitting
Coronavirus
COVID-19
cases in
United States:
60
March
1
Vice President
Pence and
Secretary Azar
Add Key
Administration
Officials to the
Coronavirus
Task Force
COVID-19
cases in
United States:
65
March
6
President
Trump at
Signing of the
Coronavirus
Preparedness
and Response
Supplemental
Appropriations
Act
COVID-19
cases in
United States:
289
March
11
White House
Coronavirus Task
Force Announces
Community
Mitigation
Strategies For
Seattle, Santa
Clara;
President Trump
addresses nation
COVID-19
cases in
United States:
1,248
The COVID-19 Response from the White HouseSpring 2020 allnurses 23
March
13
“The entry into
the United States
of all aliens who
were physically
present within
the United
Kingdom during
the 14-day period
preceding their
entry or attempted entry into the
United States is
hereby suspended
and limited”
Source: WhiteHouse.gov / worldometers.info
March
13
National
Emergency
Concerning
the Novel
Coronavirus
Disease
(COVID-19)
Outbreak
COVID-19
cases in
United States:
2,157
March
16
Call to Action
to the Tech
Community on
New Machine
Readable
COVID-19
Dataset
“15 Days to
Slow the
Spread”
COVID-19
cases in
United States:
4,503
March
20
Cooperative
action taken
with Canada
and Mexico to
close borders
in an effort to
slow the
spread of
COVID-19;
approval of
New York
disaster
declaration
COVID-19
cases in
United States:
25,500
March
22
Presidential
approval of
Washington
state
disaster
declaration
March
29
Presidential
approval of
disaster
declarations
in five states
COVID-19
cases in
United States:
43,800
COVID-19
cases in
United States:
142,46024 Spring 2020 allnurses
COVID-19
by the
numbers
With science there are inevitably numbers. With the COVID-19 pandemic, the numbers are everywhere. What can be learned from the numbers,
though? At their core, the infection rates seen in Italy and Spain are staggering. What would those numbers look like is the United States experienced the
same rate of infection? What is the maximum rate of infection that the United
States could experience before the healthcare system experiences a complete
breakdown? How many ventilators are there in the United States? How many
ICU beds are there in the United States? While those questions may seem
overwhelming, let’s attempt to get some answers.Spring 2020 allnurses 2526 Spring 2020 allnurses
December
31
Chinese Health
officials inform
the WHO about a
cluster of 41
patients with a
mysterious pneumonia. Most are
connected to
Huanan Seafood
Wholesale
Market.
January
1
Huanan
Seafood
Wholesale
Market
closes.
January
7
Chinese
authorities
identify a
new type of
coronavirus
(called novel
coronavirus
or nCoV).
January
11
China records
its first death
January
13
First coronavirus case
outside of
China is
reported in
Thailand.
January
20
First US case
is reported: a
35-year-old
man in
Snohomish
County,
Washington.
Jan
23
Wuh
plac
quar
Hub
prov
follo
days
The numbers are staggering. What began was identified in 41 patients in the city of Wuhan as a mysterious
pneumonia on December 31, 2019 has become a global
pandemic. The spread, though, didn’t happen overnight.
It took 14 days before the first case outside of China
was identified – this time in Thailand. A full 21 days after the initial December 31 report, the first case of what
was then billed as Wuhan Coronavirus or Novel Coronavirus was identified in the United States. A single case
in Washington state on January 30, 2020. Three days
later, on January 23, the chinese city of Wuhan is placed
under quarantine and the province of Hubei follows suit
days later.
As of this writing on April 22, 2020 the United
States has identified over 840,000 COVID-19 cases – a
virus which didn’t have that name until February 11.
How did we arrive at this level of a global pandemic – a
pandemic which has resulted in over 2,600,000 identified cases of COVID-19 and over 182,000 deaths from
the virus? What is the outlook for COVID-19 around
the globe and in the United States? Are American hospitals prepared for the onslaught of COVID-19 cases?
COVID-19 epicenter in Italy
Case totals as of 3 PM Wednesday, April 22 (statista.com)
In Europe, the epicenter of the global COVID-19
pandemic has been in Italy where over 187,000
cases of the virus have been identified. The hardest
hit region in Lombardy, in northern Italy. Lombardy
has seen over 69,000 COVID-19 cases with over
12,740 deaths – a mortality rate of 18.4%.
Lombardy region
69,092 cases
12,740 deaths
10,060,574 populationSpring 2020 allnurses 27
nuary
3
han is
ced under
rantine,
bei
vince
ows within
s.
January
30
WHO
declares a
global
public-health
emergency.
January
31
President
Trump bans
foreign
nationals
from entering
the US if they
were in China
within the
prior two
weeks.
February
2
First death
outside
China is
recorded
in the
Philippines
February
7
Chinese
whistleblower
Li Wenliang
dies.
February
9
Death toll in
China
surpasses
that of the
2002-2003
SARS
epidemic,
with 811
deaths
recorded.
Hubei province
67,801 cases
3,186 deaths
COVID-19 epicenter in China 57,237,740 population
Case totals as of 2 PM Monday, March 30
While COVID-19 did spread outside of the Hubei
province in China – where the city of Wuhan is
located – the overwhelming majority of cases were
contained near the assumed origin of the virus.28 Spring 2020 allnurses
February
11
WHO announces
that the new
coronavirus
disease will be
called
"COVID-19."
February
12
Coronavirus
cases start to
spike in
South Korea.
February
19
Iran outbreak
begins.
February
21
Italy outbreak
begins.
February
29
US reports
first death on
American
soil.
March
8
Italy places
all 60 million
residents on
lockdown.
M
1
W
d
o
p
P
Tr
al
2
co
Explosive spread
Case totals as of 3 PM Monday, March 30
The first map (below) depicts global
COVID-19 case totals on March 2,
2020. The map at left shows how
COVID-19 cases have spread over the
course of one month.
Global COVID-19 Infections | March 2, 2020
Via https://www.healthmap.org/covid-19/Spring 2020 allnurses 29
March
11
WHO
declared the
outbreak a
pandemic.
President
Trump bans
ll travel from
26 European
ountries.
March
13
A US national
emergency is
declared over
the novel
coronavirus
outbreak.
March
17
A leaked
federal plan
warns the
new coronavirus pandemic "will
last 18
months or
longer" and
may come in
"multiple
waves" of
infections.
March
17
Italy reports
475
COVID-19
deaths, the
highest
single-day
death toll for
any country
since the
outbreak
began.
March
19
Nearly all US
states declare
a state of
emergency.
March
22
About 1 in 3
Americans
are under
lockdown as
12 states
issue
stay-at-home
orders.
March
23
New York
City confirms
21,000 cases,
making it the
biggest
epicenter of
the outbreak
in the US.
Global COVID-19 Infections | March 30, 202030 Spring 2020 allnurses
United States
839,836 cases
46,079 deaths
328,239,523 population
If the United States experienced COVID-19 at the scale of Italy
Population Infections Rate of Infection Percentage Requiring
Mechanical Ventilation
United States 328,239,523 1,017,542* .31% 125,157**
Italy 60,317,546 187,327 .31% 19,620**
Statistics from America’s COVID-19 Hot Spots
COVID-19 Statistics: United States and Italy
Population density calculated per square mile. Percentage tested reflects the percen
Data from http://covidtracking.com/, https://www.arcg
Positive Cases: 33,261
Deaths: 1268
Percentage Tested: .76%
State Pop.: 39,512,223
Population Density: 251
Positive Cases: 27,495
Deaths: 856
Percentage Tested: 1.29%
State Pop.: 21,477,737
Population Density: 375.9
Positive Cases: 33,059
Deaths: 1,468
Percentage Tested: 1.22%
State Pop.: 12,671,821
Population Density: 231.4
Positive Cases: 24,854
Deaths: 1,405
Percentage Tested: 3.06%
State Pop.: 4,648,794
Population Density: 107.2
CALIFORNIA FLORIDA ILLINOIS LOUISIANA
*Infections in United States assumes an identified infection rate equal to that of Italy, .31%
**Percentage requiring mechanical ventilation (12.3%) is from a study by Kenneth McIntosh, MD via
https://www.uptodate.com/contents/coronavirus-disease-2019-covid-19Spring 2020 allnurses 31
Italy
187,327 cases
25,085 deaths
60,317,546 population
ntage of each state’s total population. Case totals as of 3 PM Wednesday, April 22
gis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6
Positive Cases: 251,690
Deaths: 14,828
Percentage Tested: 3.34%
State Pop.: 19,453,561
Population Density: 419.3
Positive Cases: 32,967
Deaths: 2,700
Percentage Tested: 1.17%
State Pop.: 9,986,857
Population Density: 174.7
Is America prepared for a potential tidal wave of
COVID-19 cases? The short answer, unfortunately, is
no. If the United States were to experience infection
levels at the rate which Italy has seen, our healthcare
system would buckle under the pressure of such an
influx of patients. With shortages of Personal Protective Equipment (PPE) and ventilators being seen
in New York, many improvements need to be seen to
improve what many view as a bleak outlook for caring
for COVID-19 infected patients in America.
Hospital beds per 1,000 people
Median age
Ventilators available
Ventilators per 100,000 residents
SOURCES: https://en.wikipedia.org/wiki/List_of_countries_by_hospital_beds
https://en.wikipedia.org/wiki/List_of_countries_by_median_age
https://meduza.io/en/feature/2020/03/21/the-ventilator-problem
UNITED STATES
2.77
UNITED STATES
38.1
UNITED STATES
68k
UNITED STATES
18.8
ITALY
3.18
ITALY
45.5
ITALY
5k
ITALY
8.3
Italy began a quarantine of the country’s epicenter
– Lombardy – in early March and soon extended the
lockdown to the entire country. While the COVID-19
virus appears to still be spreading, the daily increase of
cases has slowed.
NEW YORK MICHIGAN32 Spring 2020 allnurses
One of the original names which was tossed
about – Novel Coronavirus – pinpoints just how
we arrived at a world on lockdown. This is the first
time that this particular strain – SARS-CoV-2 –
has appeared in humans. Due to its recent appearance in the human population, there is no natural
immunity to the virus. Its “newness” in the global
population coupled with how easily it spreads, its
lifespan on surfaces, and how mobile humans are
makes for the perfect storm.
A new virus. A mobile population. Simple transmission. Quick replication of viral cells. All of the
ingredients were there. The question still remains,
how did a virus new to the human population
appear in humans?
In a research paper published in the journal
Nature Medicine, Kristin Anderson, PhD who is
an associate professor of immunology at Scripps
Research explained “By comparing the available
genome sequence data for known coronavirus
strains, we can firmly determine that SARS-CoV-2
originated through natural processes.” That statement alone should put to rest various conspiracy
theories circulating online relating to the virus
being a biological weapon developed by either the
United States or Chinese governments.
Natural evolution evidence
The evidence for natural evolution was supported by data on SARS-CoV-2’s backbone -- its overall molecular structure. If someone were seeking
to engineer a new coronavirus as a pathogen, they
would have constructed it from the backbone of
a virus known to cause illness. But the scientists
found that the SARS-CoV-2 backbone differed
Where
and
did the virus
come from
How did it spread so fast
The Origins of COVID-19Spring 2020 allnurses 33
substantially from those of already known coronaviruses and mostly resembled related viruses found
in bats and pangolins.
Possible origins
One scenario regarding the evolution of the
virus to its current state is that nutural selection in
a non-human host played a role before its jump to
humans. This was the case with both SARS (civets)
and MERS (camels). Researchers have propsed
bats as the most likely reservoir for SARS-CoV-2
as it is very similar to a coronavirus found in bats.
There are no documented cases of direct bat to
human transmission, though, making an intermediate host a likely piece of the COVID-19 puzzle.
The other proposed scenario is that a non-pathogenic version of the virus jumped from an animal
host to humans, then evolved to its current state
with a segment of the human population. One
possibility is that pangolins, an armadillo-like
mammal found in Asia and Africs, played a part in
the transmission due to an RBD structure found to
be very similar to that of SARS-CoV-2. A coronavirus from a pangolin could possibly have been
transmitted to a human, either directly or through
an intermediary host such as civets or ferrets.
Causes of COVID-19’s
rapid spread
Discussed in a recent Scientific American
podcast, editor W. Wayt Gibbs and Washington
Governor Jay Inslee broke down examples of how
COVID-19 was able to spread so rapidly.
“Let me give you one example from here in
Washington. On March 10, despite stern official
warnings not to gather in groups, 56 people met
for an event in Skagit County. All of them were
apparently healthy at the time. But 10 days later,
43 of those 56 people have either been confirmed
to have COVID-19 or are showing symptoms
of the disease. Experts suspect that one or more
people in the group was a so-called “supershedder,” someone who has yet to show symptoms but is
transmitting lots of infectious virus.”
An infection rate of over 76% from one ill-advised gathering. While the specific method of
transmission is unknown, there are numerous
possibilities.
Respiratory and fomites
“[Fomites] refers to transmission from surfaces.
The average person touches their face 2- or 3,000
times a day—three to five times every waking minute. In between, we’re touching doorknobs, water
fountains, elevator buttons and each other. Those
things become fomites.”
“The NIH researchers ... sprayed infectious
droplets onto cardboard, stainless steel and plastic.
Then they checked the spatter as time passed to
see how quickly the viral particles dried out and fell
apart.”
CARDBOARD
• 4 hours before live virus started to fall
significantly
• Quite infectious 8 hours later
STAINLESS STEEL
• Infectious after 24 hours
The results from the National Institute of Health
SOURCES: https://www.sciencedaily.com/releases/2020/03/200317175442.htm
https://www.scientificamerican.com/podcast/episode/covid-19-how-and-why-the-virus-spreads-quickly/34 Spring 2020 allnurses
tests show that infection without people immediately present can still occur. This is in addition to
the confirmed spread via respiratory droplets.
Silent transmission
During a World Health Organization study of
94 COVID-19 patients in China, tests were performed to determine when they became infections
and when they stopped shedding the virus.
The results showed that patients tended to
become less infectious as their symptoms progressed. Additional findings concluded that the
largest amount of viral shedding occured two days
before they felt ill.
Those finding are what has led to social distancing, washing hands thoroughly for 20 seconds, and other campaigns to slow the spread of
COVID-19.
Germs from a
cough or sneeze
can travel
6 to 8 feet
“Maintaining at least 6 feet of space between yourself and another person...they
call it social distancing. I wasn’t even being
social in the first place! I’m going to the
grocery store to get some food, and they
want me to adhere to “social distancing”.
Call it what it really is! “Infection-prevention distance”, the “germ reduction zone”,
the “safety zone”, the “I-don’t-want-toget sick zone”. You put the word “social”
followed by a word that makes people
feel restricted- as in “distancing”, you are
bound to get a few rebels. They should’ve
labeled it something else. This is more
than just a social issue – for some it
could mean life or death.”
Calling social distancing
what it really is...Spring 2020 allnurses 35
Be a part of what
makes us great.36 Spring 2020 allnurses
Warm Weather
Will Slow the
Virus and Other Bad Advice
Look at a world map of where the coronavirus
has spread and the answer seems obvious though
these cases may be travel-related and not linked to
seasonality. The World Health Organization states
that from the evidence so far, COVID-19 can be
transmitted in all areas, including those with hot
and humid climates.
Though the flu peaks in February along with
RSV and the common cold, experts don’t know if
the coronavirus will behave in the same way. The
most recent article on this topic that I could find
is from the New York Times, published on March
22, 2020. Experts state in this article that “Wherever the temperatures were colder, the number of
the cases started increasing quickly,” In the US
southern states like AZ, FL and TX are seeing
slower growth of the outbreak. This is supported
by two other studies (one from Spain and Finland, the other from China). The virus thrives in
dry conditions between 28.3 and 49 degrees F.
HOWEVER (and this is a big however for scientists like myself – none of these studies has been
peer reviewed.) Even if warm temperatures make
the virus less effective, it will still be transmitted.
It might be tougher for the virus to survive in the
air or on surfaces for long periods, but it will still
be contagious for hours. It’s going to be 4-6 weeks
before we have a clear picture of this situation.
SO much is unknown, and even if the virus slows
during warmer months it could return with ferocity in the fall.
Other misconceptions about what will help
prevent infection:
1. Gargling with warm water
No evidence, though it may provide comfort
2. Drinking hot water frequently to flush the
virus into the stomach
No evidence: infections often begin after we’ve
been exposed to thousands or millions of viral
particles, so sweeping a few down the oesophagus
is unlikely to have much of an impact.
3. Blasting hot air
No evidence – you might kill a few, but there are
millions. A steaming bowl of hot soup will provideSpring 2020 allnurses 37
There’s a lot of bad information out there.
This article discusses some of the top
false claims being spread on the internet. As
nurses, it is crucial that we have the most accurate, up-to-date information for our
patients, family and friends. They trust
us to know what’s going on.
comfort and may kill a few more, but aiming a hair
dryer at your face isn’t going to help.
4. Ingesting colloidal silver
No evidence
5. Getting some sun
No evidence
6. Taking your vitamins (garlic, pepper, elderberry, mint, vitamin C)
No evidence.
This one will get me the most kickback, I know
it, but I stand by it. My statement: If you take supplements you’ll get better in 7 days, if you don’t, it
will take a week.
You can help people understand that though
one person may have personal experience with
one of these tactics working for them, that is called
“anecdotal” evidence and does not apply to the
general population as a whole. Scientific evidence
is based upon large data sets, not just one person’s
experience. Remind folks that once the virus is in
your blood stream, or in your respiratory system,
most of these strategies will not work. There’s a
video telling folks to raise the temperature of their
nostrils to 130 degrees. That sounds great, except,
how can you raise the temperature of your blood to
130 degrees? Boiling your blood will most certainly kill you much more quickly than coronavirus.
What we do know:
Coronavirus is also known as COVID-19. It is a
virus which is a collection of proteins and lipids, so
antibiotics won’t help treat it. There is no known
cure. It passes person to person by physical contact
and it can live on hard surfaces and in the cough
of a sick person’s respiratory droplets. Anyone can
get it and carry it, but people over 65 are more
likely to die from it, as are folks in high risk categories. New studies suggest that though it is mainly
transmitted as respiratory droplets, it can go
airborne depending on heat and humidity, which
means if someone carrying the virus sneezes in
the Walmart, you might breathe in those particles
up to two hours later. It has a long latency period
(it may incubate for up to 14 days), so you might
spread it to lots of people before you even know you38 Spring 2020 allnurses
have it. We don’t have enough resources to deal
with everyone getting sick at the same time, so we
have to slow the spread of the virus (shoot, I can’t
even find a thermometer).
“Sound preparation base on scientific evidence
is what is needed at this time.”
– UNICEF
1. Wash your hands often
2. Stay home
3. Avoid touching your face
4. Stay home
5. Practice social distancing
6. Stay home
7. Cover your mouth when you cough
8. Stay home
9. Disinfect surfaces
10. Did I mention you should stay home?
There is a spark of hope. Outbreaks in China
and South Korea appear to be stabilizing, but that
seems to be due to intervention by the authorities
(lockdowns, travel restrictions), and not due to
anything related to the virus itself.
Finally – thank you to all the folks who cannot
stay home. Those of you who go in to work every
day to fight the good fight – I want you to know,
I’m not buying or using gloves or masks because I
am fully aware of how they work (and don’t work…
those folks at the grocery store make me cry…) and
if you know how I can send you some or donate to
help get you what you need, post the link and I’ll
do it.
Nurses on the frontlines, you are my heroes.
Thank you.
Coronavirus situation in the US
Total deaths as of 8:11am Apr 22 BST
Graphic: Steven Bernard and Cale Tilford
Sources: Johns Hopkins University, CSSE; Worldometers; FT research
© FT
Alabama
186
Alabama
186
Alaska
9
Alaska
9
Arizona
208
Arizona
208 Arkansas
43
Arkansas
43
California
1,268
California
1,268
Colorado
449
Colorado
449
Connecticut
1,423
Connecticut
1,423
Delaware
82
Delaware
82
DC
112
DC
112
Florida
884
Florida
884
Georgia
818
Georgia
818
Hawaii
12
Hawaii
12
Idaho
51
Idaho
51
Illinois
1,468
Illinois
1,468
Indiana
630
Indiana
630
Iowa
83
Iowa
83
Kansas
107
Kansas
107 Kentucky
171
Kentucky
171
Louisiana
1,405
Louisiana
1,405
Maine
36
Maine
36
Maryland
584
Maryland
584
Massachusetts
1,961
Massachusetts
1,961
Michigan
2,700
Michigan
2,700
Minnesota
160
Minnesota
160
Mississippi
183
Mississippi
183
Missouri
189
Missouri
189
Montana
12
Montana
12
Nebraska
38
Nebraska
Nevada 38
163
Nevada
163
New Hampshire
42
New Hampshire
42
New Jersey
4,753
New Jersey
4,753
New Mexico
65
New Mexico
65
New York
14,828
New York
14,828
N Carolina
213
N Carolina
213
N Dakota
13
N Dakota
13
Ohio
557
Ohio
557
Oklahoma
164
Oklahoma
164
Oregon
78
Oregon
78
Pennsylvania
1,564
Pennsylvania
1,564
Rhode Island
171
Rhode Island
171
S Carolina
135
S Carolina
135
S Dakota
7
S Dakota
7
Tennessee
157
Tennessee
157
Texas
517
Texas
517
Utah
32
Utah
32
Vermont
40
Vermont
40
Virginia
324
Virginia
324
Washington
652
Washington
652
W Virginia
27
W Virginia
27
Wisconsin
242
Wisconsin
Wyoming 242
6
Wyoming
6
Puerto Rico
64
Puerto Rico
64
Statewide ‘stay at home’ order*
Advisory ‘stay at home’ order**
*Includes 'shelter in place' orders
**Includes Kentucky's ‘healthy at home’ order
Dr. Kristi Miller, aka Safety Nurse is an Assistant Professor of
nursing at USC-Upstate and a Certified Professional in Patient
Safety. She is also a mother of four who loves to write so
much that she would probably starve if her phone didn’t remind her to take a break. Her work experiences as a hospital
nurse make it easy to skip using the bathroom to get in just
a few more minutes on the computer. She is obsessed with
patient safety. Please read her blog, Safety Rules! on allnurses.
com. She is doing research into the relationship between participation in Root Cause Analysis and patient safety attitudes
(contact her if you are interested). In the guise of Safety Nurse,
she is sending a young Haitian woman to nursing school and
you can learn more about that adventure: https://www.gofundme.com/rose-goes-to-nursing-school
Have something to say?
Click here to comment!Spring 2020 allnurses 39
Where do you see your nursing career going?
The demand for nurse practitioners is on the rise, with no signs of slowing down. And
as the demand grows, so does the pay — with median salaries already at $113,930*.
That’s well above the median salary for those with their bachelor’s in nursing. Start
preparing now with an online nursing degree from Maryville University.
• Choose from 5 concentrations – FNP, AGPCNP, AGACNP, PNP, or PMHNP
• 100% online – no campus visits required
• Complete clinicals locally in your preferred setting
• CCNE accredited
• Ranked among “America’s Top Colleges” – Forbes, 2019
• Programs start in fall, spring, and summer
GET PROGRAM DETAILS40 Spring 2020 allnurses
Tweets
from the
Front Lines
In the war against COVID-19, information is moving fast and
conditions are changing by the minute. The social network Twitter
has proven itself to be integral in bringing change and communicating
the struggles nurses are facing both on and off the job. We’ve chosen
to showcase some of the most impactful messages recently shared
by nurses across the country.Spring 2020 allnurses 4142 Spring 2020 allnurses
Good
News!
The battle against COVID-19 is real
and it is ugly. But amongst all of the
sadness, there is positivity. Americans
and American companies are stepping
up to aid in the fight against a seemingly
invisible enemy.
The Four Seasons Will
Provide Free Rooms
For NYC Hospital
Workers On The Front
Lines Of COVID-19
Brooklyn Distillers Turn
Waste Alcohol Into
Hand Sanitizer
Sharing A Free Pair
For Healthcare
Governor Andrew Cuomo announced on Twitter yesterday that the Four Seasons Hotel on 57th Street will provide
“FREE lodging to doctors, nurses & medical personnel
currently working to respond to the COVID-19 pandemic.”
Thanks to the ambitious work of two distillers at Brooklyn-based Kings County Distillery who researched World
Health Organization and Centers for Disease Control guidelines for hand sanitizers, the distillery now has 1,000 bottles
ready for the public.
Crocs is now offering free pairs of shoes to health
care workers fighting on the front lines against the
coronavirus.
Health care workers can place an order for their
free Crocs on crocs.com. It’s part of the “A Free
Pair for Healthcare” program, according to a
release from Crocs.Spring 2020 allnurses 43
Aspen University offers an online RN to BSN completion program for registered nurses who have
an associate degree or diploma in nursing and wish to pursue a baccalaureate degree.
With a liberal arts foundation, our RN-to-BSN program builds on initial nursing preparation to
prepare nurses for a broader scope of practice with a useful understanding of the cultural, political,
economic, and social issues that affect patients and influence care delivery. It is designed for adult
learners wishing to complete their undergraduate degree without the on-campus class requirement.
Finish Fast – Complete in 12 months (8-week courses)
Enjoy Flexibility – 10 courses with start dates every 2 weeks
Accredited – CCNE accreditation
Affordable – Tuition and fees only $10,550
Pay Monthly – Opt to pay $250 per month
Achieve Educational Goals and Career Mobility
• Network as you learn
• Interact with respected nursing leaders and fellow professionals
• 1-on-1 with instructors
We understand trying to fit education into an already busy schedule. We created interactive, flexible, facilitated, online courses designed to fit around your lifestyle.
Go from RN to BSN online at a remarkably low cost.44 Spring 2020 allnurses
COVID-19
Breaking the Myths
The Online Home of over 1,000,000 Nurses and Nursing Students.
MYTH 1: COVID-19 will go away in the Summer months.
WRONG. Previous pandemics didn’t follow weather patterns. Additionally, Summer in the northern
hemisphere is Winter in the southern hemisphere.
MYTH 2: COVID-19 will spread more in the Summer months due to mosquito bites.
WRONG. COVID-19 spreads via respiratory droplets, not blood.
MYTH 3: If you can hold your breath for 10 seconds, you don’t have COVID-19.
WRONG. Most youg patients with Coronavirus will be able to hold their breath for longer than 10
seconds. And many elderly without the virus won’t be able to do it.
MYTH 4: Since COVID-19 tests are difficult to find, we shuld donate blood and the blood bank will
test for it.
WRONG. No blood banks are testing for COVID-19. Blood donation is a selfless action. You should
be mtivated for the right reasons.
MYTH 5: Coronavirus lives in the throat. So drink lots of water so the virus is pushed into the stomach where the acid will kill it.
WRONG. The virus may gain entry via throat but it penetrates into the host cells. You can’t wash it
away. Excessive water will only make you run to the toilet.
MYTH 6: All this social distancing is an over reaction. You’ll see that the virus won’t cause much
damage.
WRONG. A lower number of cases proves that social distancing is working.
MYTH 7: Car accidents kill 30,000 people annually. What’s the big deal with COVID-19?
WRONG. Car accidents are not contagious, their fatalities don’t double every three days, they don’t
cause mass panic or a market crash.
MYTH 8: Hand sanitizers are better than soap and water.
WRONG. Soap and water actually kills and washes away the virus from skin (it can not penetrate our
skin cells) plus it also cleans visible soiling of hands. Don’t worry if Purell was sold out at your supermarket.
MYTH 9: One of the best strategies to prevent COVID-19 is to clean every door knob in your home
with disinfectants.
WRONG. Hand washing/maintaining 6ft distance is best practice. Unless you’re caring for a COVID
patient at home, your home surfaces should not be a big risk.
via @FaheemYounus – Faheem Younus, MD is
Chief Quality Officer and Chief of Infectious Diseases, University of Maryland UCH.Spring 2020 allnurses 45
CONTAGION
PREVENTION
PERSONAL
CONTACT
AIR BY COUGH
OR SNEEZE
CONTAMINATED
OBJECTS
MAINTAIN A DISTANCE
OF SIX FEET WITH PEOPLE
WASH YOUR
HANDS OFTEN
AVOID CONTACT
WITH SICK PEOPLE
ALWAYS COVER YOUR
COUGH OR SNEEZE
CLEAN SURFACES
REGULARLY
NO GROUPS LARGER
THAN 10 PEOPLE
11
Why is COVID-19 different?
What makes the new coronavirus so dangerous to humans is simply that it’s “novel,” meaning it’s
new to humans, so we don’t have any way to fight it. This is the first time it has ever circulated in
humans.
Additionally, there is no cure. While testing of both anti-viral medications and vaccines is underway,
it’s unlikely that there will be a vaccine to prevent COVID-19 for at least a year.
Regarding seasonal dissipation – much like the seasonal flu – there are no indications regarding a
slowdown in the spread of COVID-19 as the weather warms in the northern hemisphere. There has
been some evidence emerging from China that COVID-19 cases may be waning, but nobody is certain if or when that will happen.
What can I do?
Wash your hands frequently and thoroughly for at least 20 seconds using soap and water. Avoid
touching your face – including eyes, nose, and mouth – with unwashed hands. Don’t openly cough
into the air – even if you presume to be otherwise healthy. If you or a family member are sick, isolate
at home for the recommended 14 days. If you can find a regular facemask for an ill person, that may
prevent the spread of droplets. Lastly, clean surfaces frequently. A preliminary study showed that this
virus could last three days – or longer – on surfaces.
COVID-19
Health & Safety Tips
The Online Home of over 1,000,000 Nurses and Nursing Students.46 Spring 2020 allnurses
The COVID-19
Battle Cry for
Retired Nurses
The COVID-19 epidemic brought me
back to work after 20 years of retirement
By Kathy Day, RN
Just a few weeks ago, I was helping with a list
of classmates from my nursing school class of
1970. Yes, it was so we could plan our 50th
class reunion. I was looking at the young
fresh faces on my class photo, including my
own. I have worked as a patient
safety advocate for the past
10 years, as a volunteer. I
have not worked clinically for 20 years. It is
surreal for me to be
out of school for 50
years. All of those
anniversary festivities have been canceled.Spring 2020 allnurses 47
As those party planning emails came, the news
on TV was getting more urgent about this new
virus. COVID 19 had floated around for a few
months. We heard stories about it when a bunch
of people got sick on cruises. There were decisions
being made about whether or not those people
should be allowed back into the US. There were
some pretty frightening images of the Chinese who
were all wearing masks on the streets and many
were dying. Some of the dying were doctors.
The news got more and
more scary
The few nursing home patients in Washington
State became the beginnings of an epicenter for
this disease. Then New York City, then parts of
California. Just a few weeks later, here we are.
Every State is affected including Maine with our
very small, but older population.
The news is dire, every single day. Every day citizens are stocking up on face masks and hand sanitizers and clearing shelves of other necessities like
toilet paper and food staples. There isn’t enough
PPE for nurses, doctors and other frontline workers. There aren’t enough testing materials so that
every single person who is exposed to COVID 19,
or who has a risk factor or who may even have some
symptoms, can be tested. We are all being trusted
to socially distance ourselves, or to self-quarantine if we have a risk factor or symptoms. All of us
are being asked to stay away from others and stay
at home as much as possible. Basically we must
consider every person around us to be infected…it
helps us to socially distance.
Businesses and borders
are closed
Still, irresponsible Spring breakers gathered in
FL and other warm places, and COVID spread.
Some large churches held big gatherings and
services in spite of all of the warnings, and COVID
spread. A few of our Senators and Representatives
got it. Tom Hanks and his wife got it. This virus
doesn’t care how famous, religious, rich or powerful you are….it will invade your body. It is a great
opportunist.
My son is out of work as of Friday. My husband
and I have been spending most of our days at home,
but we drive somewhere daily. Our little dog has
been the star of our isolation show, and we take him
everywhere with us. One day we enjoyed a short
trip to the coast of Maine, and I am so luck to be so
close to such beauty.
And, this old nurse is going back to work
I knew there was something I could do. I communicated with other healthcare workers and with
my patient safety colleagues. The effort to keep
patients away from crowded clinics and ERs meant
that someone was going to have to keep telling
them that it was the safest thing for them, unless
they had life threatening symptoms.
I called my local hospital. I asked if they had
considered using retired nurses for some sort of
telephone triage line. They hadn’t but they were
very excited about my idea. Some of their staff
was working on a phone tree and an algorithm. I
offered to work from home, taking calls. I also offered to recruit other retired nurses to do the same.
So, I have recruited 5 other nurses. 4 of us have
had our physicals and background checks done
already. We hope to be working within the week.
We all can help ...
We all can help, even those of us who are “older’, retired and at a higher risk of disease. Find a
way. And for those nurses who are working with
COVID 19 patients on the front lines, my hat off
to you. Your courage and dedication just blows
me away. I do hope that most of you will not face
a shortage of needed PPE, and yes, I do know that
some of you already have.
We are all in this together. Doing what the experts are telling us is our social responsibility, but
nurses young and old can do so much more. We all
need to stand together albeit remotely.
Have something to say?
Click here to comment!48 Spring 2020 allnurses
Worth a
Thousand Words
The written word is powerful but as the old adage goes, a picture is worth a thousand
words. The pictures (or photos if you’re a stickler) from the front lines of the war against
COVID-19 will forever be etched in the minds of millions. Here are some of them...
A parking garage at Nashville, Tennessee’s Vanderbilt Hospital was converted to be used
for patient overflow for the expected tidal wave of COVID-19 cases. Davis County – where
Nashville is located – has seen nearly 300 COVID-19 cases.Spring 2020 allnurses 49
A plea from the nurses and doctors in the Emergency Department at Saolta Group
University Hospital in Galway, Ireland.
Kious Kelly, a nurse
manager at a Manhattan hospital, has
quickly become the
face of the battle to
obtain Personal Protective Equipment
for nurses. The 48
year-old who worked
at Mt. Sinai Hospital
may have been the
first nurse in New
York to pass away
from COVID-19.50 Spring 2020 allnurses
[Show More]
Last updated: 11 months ago
Preview 5 out of 50 pages






.png)

.png)







.png)


.png)
.png)


.png)


















.png)



.png)

 – University of the People.png)

.png)
.png)


.png)









.png)