*NURSING > STUDY GUIDE > Galen College of Nursing NUR 242NUR 242 Test 3 Recaps Units 7 & 8 (1) (All)
Galen College of Nursing NUR 242NUR 242 Test 3 Recaps Units 7 & 8 (1)
Document Content and Description Below
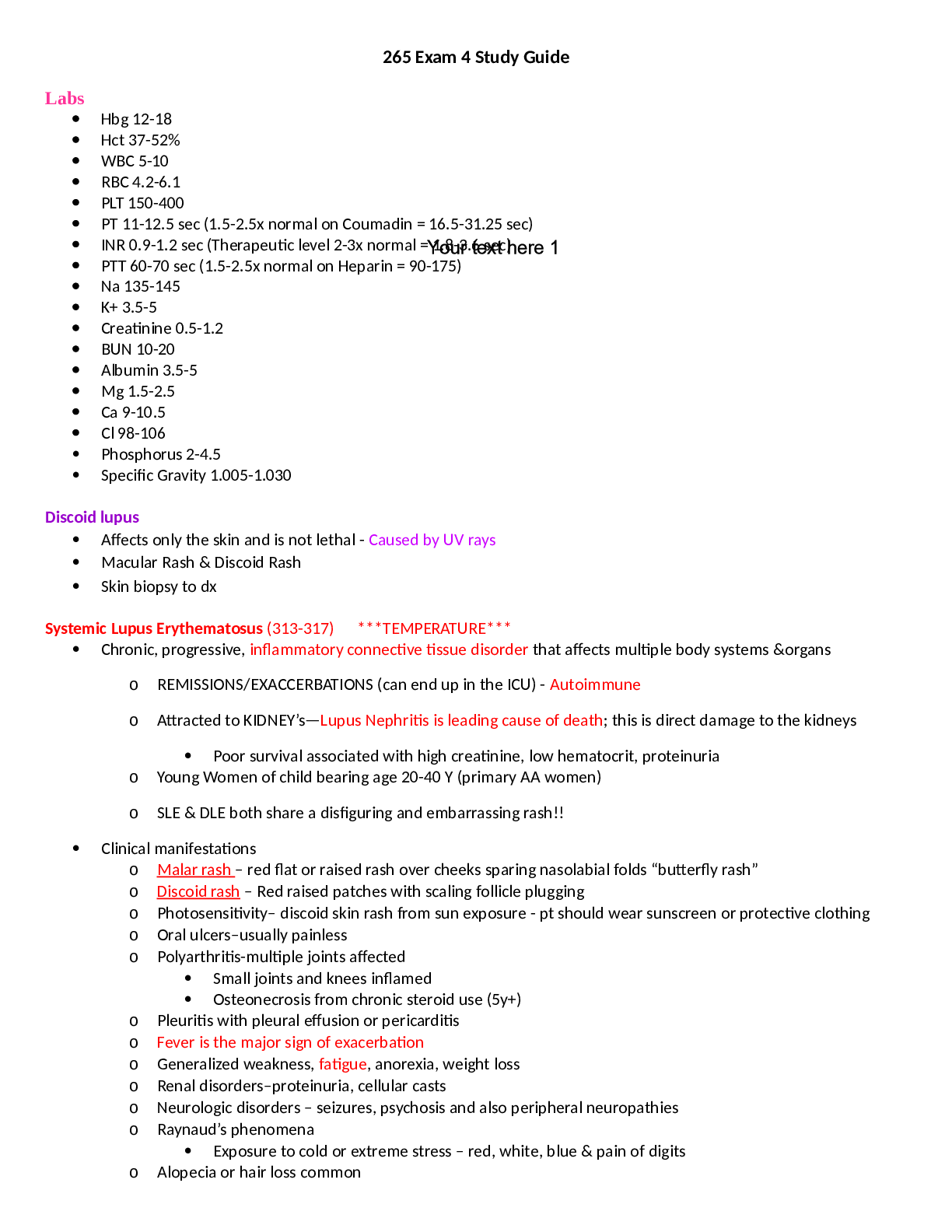
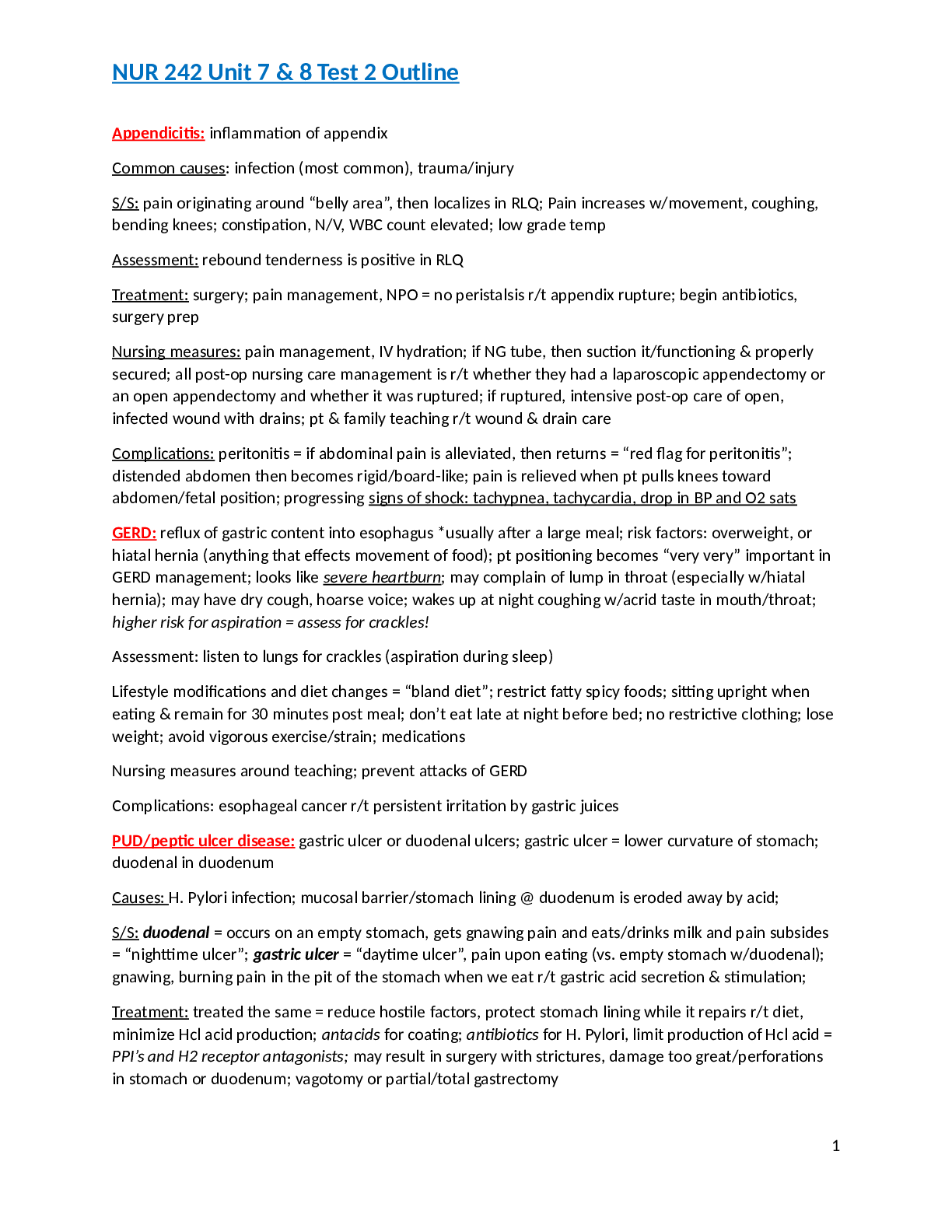
NUR 242 Unit 7 & 8 Test 2 Outline Appendicitis: inflammation of appendix Common causes: infection (most common), trauma/injury S/S: pain originating around “belly area”, then localizes in RLQ; ... Pain increases w/movement, coughing, bending knees; constipation, N/V, WBC count elevated; low grade temp Assessment: rebound tenderness is positive in RLQ Treatment: surgery; pain management, NPO = no peristalsis r/t appendix rupture; begin antibiotics, surgery prep Nursing measures: pain management, IV hydration; if NG tube, then suction it/functioning & properly secured; all post-op nursing care management is r/t whether they had a laparoscopic appendectomy or an open appendectomy and whether it was ruptured; if ruptured, intensive post-op care of open, infected wound with drains; pt & family teaching r/t wound & drain care Complications: peritonitis = if abdominal pain is alleviated, then returns = “red flag for peritonitis”; distended abdomen then becomes rigid/board-like; pain is relieved when pt pulls knees toward abdomen/fetal position; progressing signs of shock: tachypnea, tachycardia, drop in BP and O2 sats GERD: reflux of gastric content into esophagus *usually after a large meal; risk factors: overweight, or hiatal hernia (anything that effects movement of food); pt positioning becomes “very very” important in GERD management; looks like severe heartburn; may complain of lump in throat (especially w/hiatal hernia); may have dry cough, hoarse voice; wakes up at night coughing w/acrid taste in mouth/throat; higher risk for aspiration = assess for crackles! Assessment: listen to lungs for crackles (aspiration during sleep) Lifestyle modifications and diet changes = “bland diet”; restrict fatty spicy foods; sitting upright when eating & remain for 30 minutes post meal; don’t eat late at night before bed; no restrictive clothing; lose weight; avoid vigorous exercise/strain; medications Nursing measures around teaching; prevent attacks of GERD Complications: esophageal cancer r/t persistent irritation by gastric juices PUD/peptic ulcer disease: gastric ulcer or duodenal ulcers; gastric ulcer = lower curvature of stomach; duodenal in duodenum Causes: H. Pylori infection; mucosal barrier/stomach lining @ duodenum is eroded away by acid; S/S: duodenal = occurs on an empty stomach, gets gnawing pain and eats/drinks milk and pain subsides = “nighttime ulcer”; gastric ulcer = “daytime ulcer”, pain upon eating (vs. empty stomach w/duodenal); gnawing, burning pain in the pit of the stomach when we eat r/t gastric acid secretion & stimulation; Treatment: treated the same = reduce hostile factors, protect stomach lining while it repairs r/t diet, minimize Hcl acid production; antacids for coating; antibiotics for H. Pylori, limit production of Hcl acid = PPI’s and H2 receptor antagonists; may result in surgery with strictures, damage too great/perforations in stomach or duodenum; vagotomy or partial/total gastrectomy 1 NUR 242 Unit 7 & 8 Test 2 Outline Teaching: Lifestyle changes = limit stress, alcohol/caffeine consumption, stop smoking, diet; prevent formation/exacerbation of PUD; complications: gastric ulcer = chronic gastritis, high risk for stomach cancer (if add PUD & bad diet r/t nitrates, pickled foods, smoked/charred foods & meats; smoking (stop smoking! It aggravates ulcerative condition); possibly peritonitis; Partial or total gastrectomy surgery can lead to dumping syndrome: post-op complication of partial/total gastrectomy; self-limiting, pt needs to wait it out and will resolve itself just needs to rest until is subsides. No other treatment. S/S: pt feels like they’re having a Heart attack = tachycardia, N/V/D, diaphoresis, chest pain, palpitations, abdominal cramping, clammy, generalized weakness, vertigo/dizziness; pt can’t do anything when it is happening. Just rest/lie down and wait it out; 15-20 minutes after eating, lasts 20-30 minutes r/t SNS response Treatment: controlled through diet = avoid large intakes of simple carbs (white flour, sugar, rice, pasta, bread, tortillas, fruits w/out pulp especially, juices, regular soft drinks; diet drinks okay but sorbitol will cause diarrhea; no fluids/don’t drink anything before or with meal; fat content of meals delays absorption of carbs into intestines so fats/proteins will help episode; Procedures to review: Esophagogastroduodenoscopy: EGD visual inspection of stomach, esophagus and duodenum; done under moderate sedation = recovery post-procedure; medication/anesthetics knock out gag reflex, so monitor for gag reflex post-op, will be NPO for approx. 6-8 hours post procedure, even though gag reflex will return within 1-2 hours. Meds will be completely out of system after 6-8 hours, so can drink fluids (NPO status lifted after 6-8 hrs). [Show More]
Last updated: 2 years ago
Preview 1 out of 21 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$9.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 07, 2021
Number of pages
21
Written in
Additional information
This document has been written for:
Uploaded
Sep 07, 2021
Downloads
0
Views
59





.png)
.png)

.png)