*NURSING > SHADOW HEALTH > NR509 Cardiovascular Physical Assessment Assignment | Completed | Shadow Health (All)
NR509 Cardiovascular Physical Assessment Assignment | Completed | Shadow Health
Document Content and Description Below
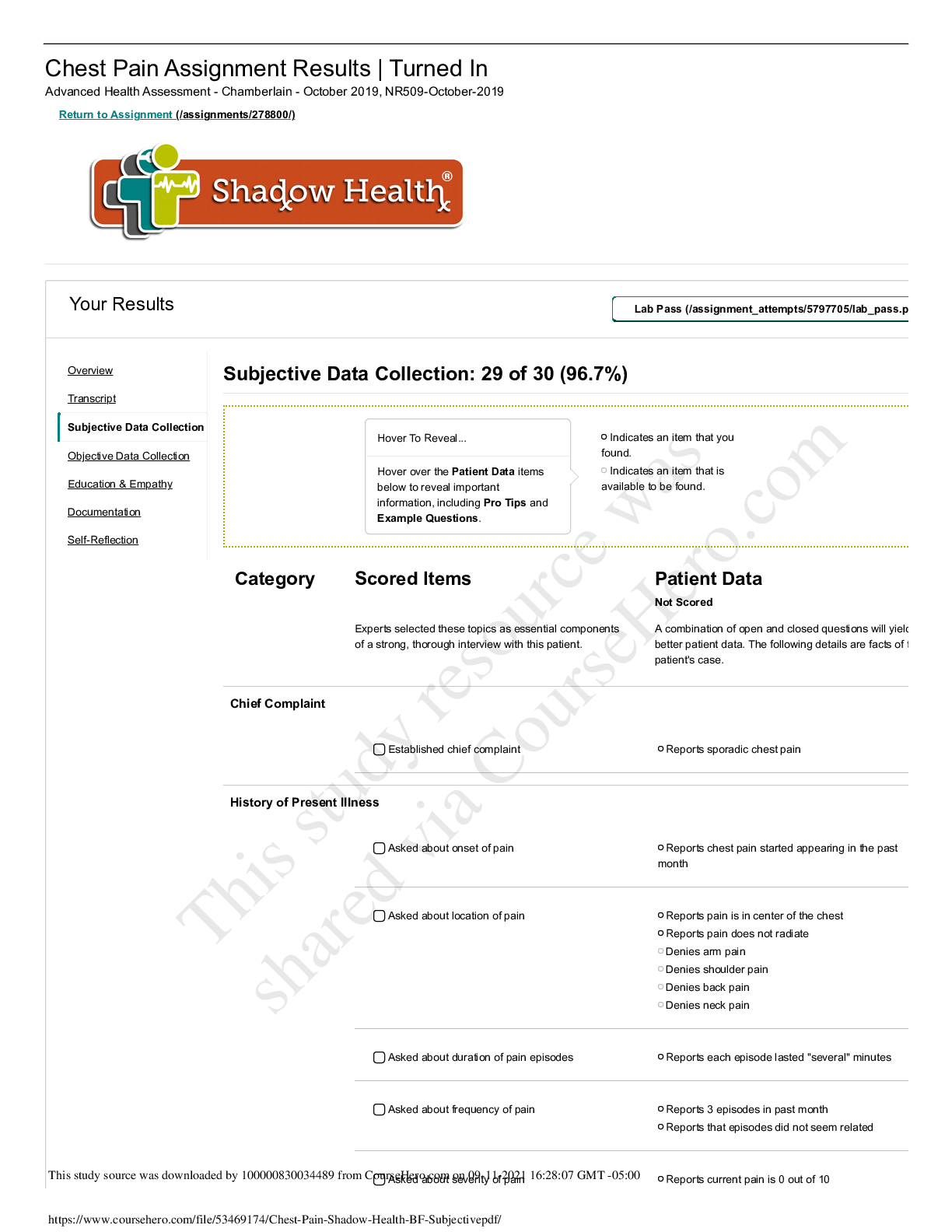
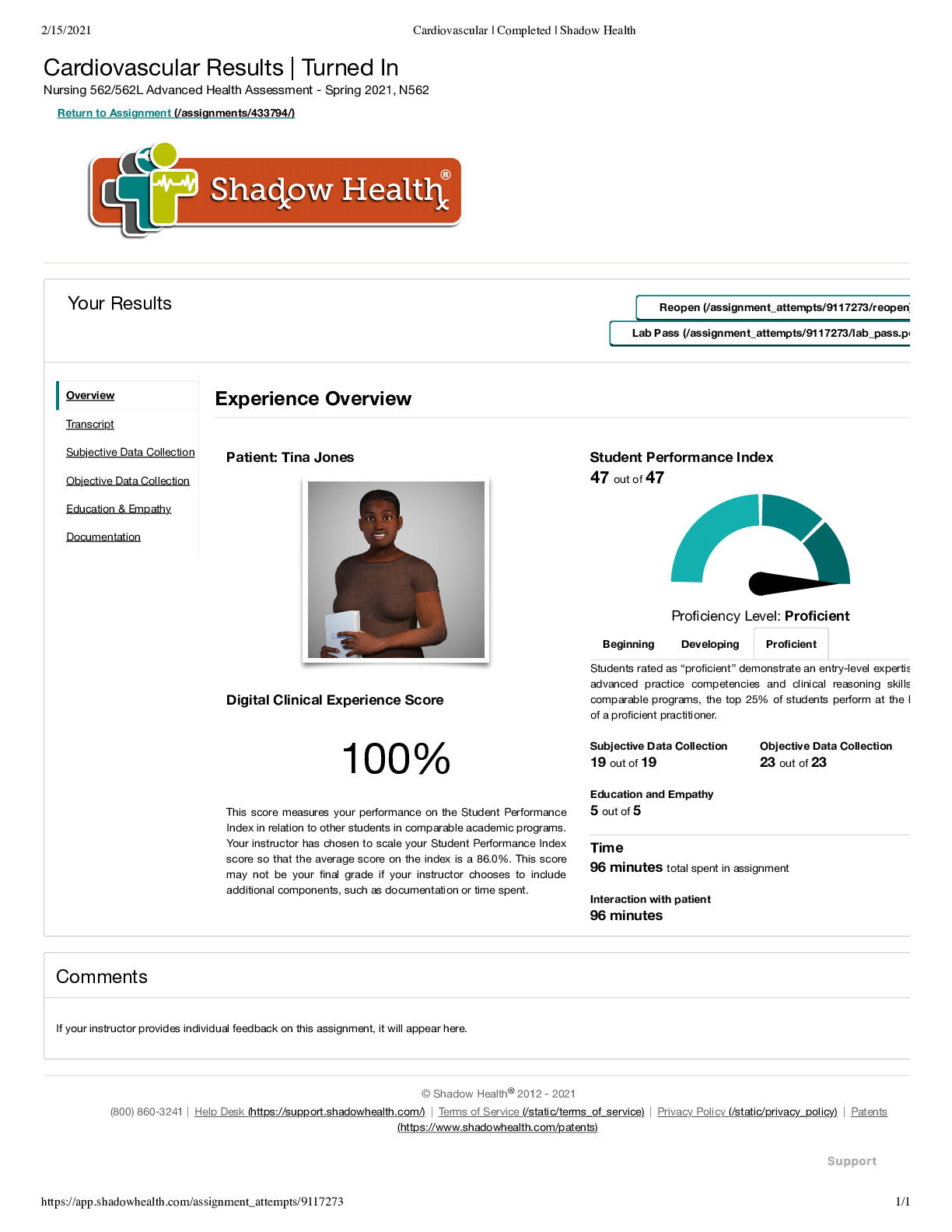
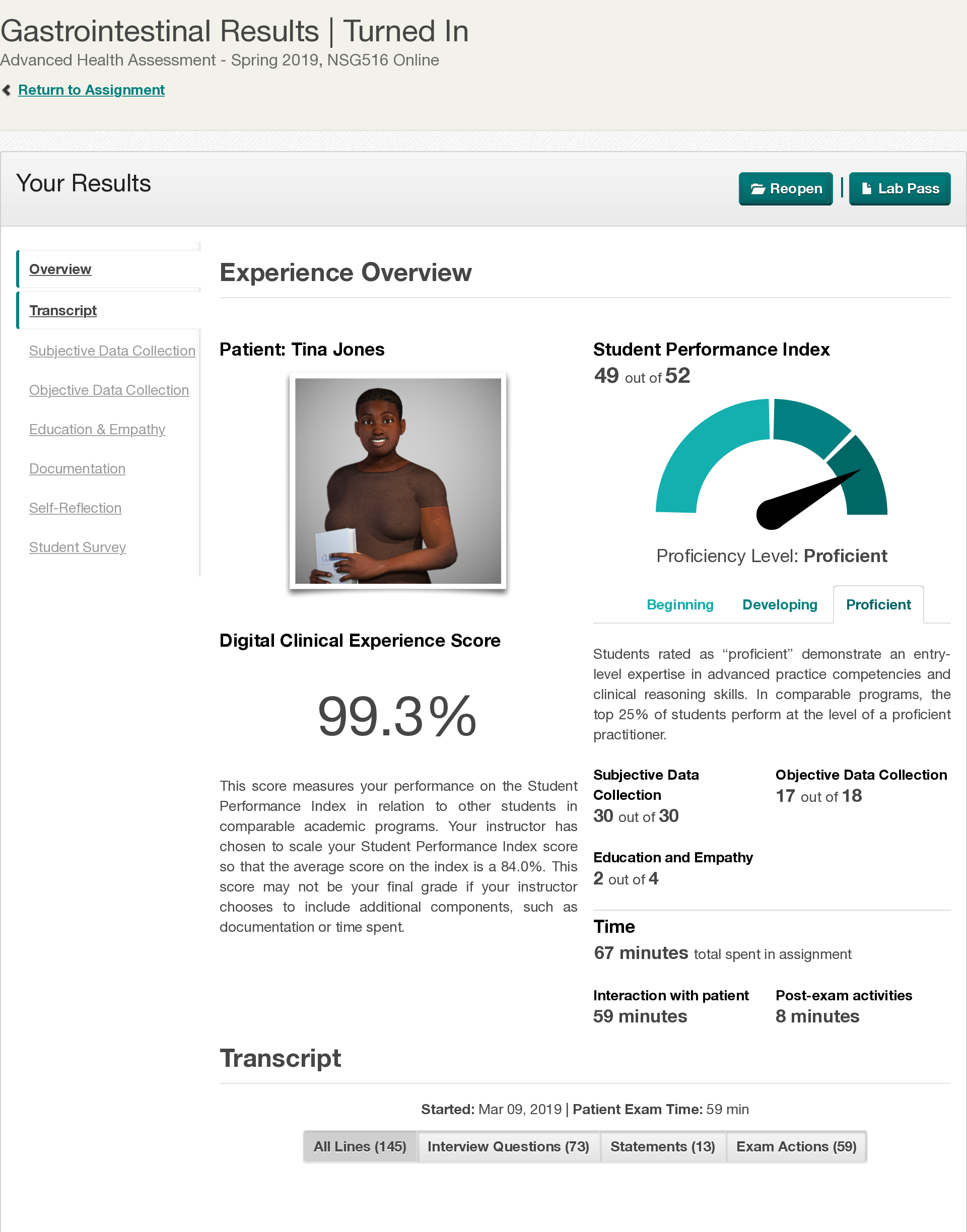
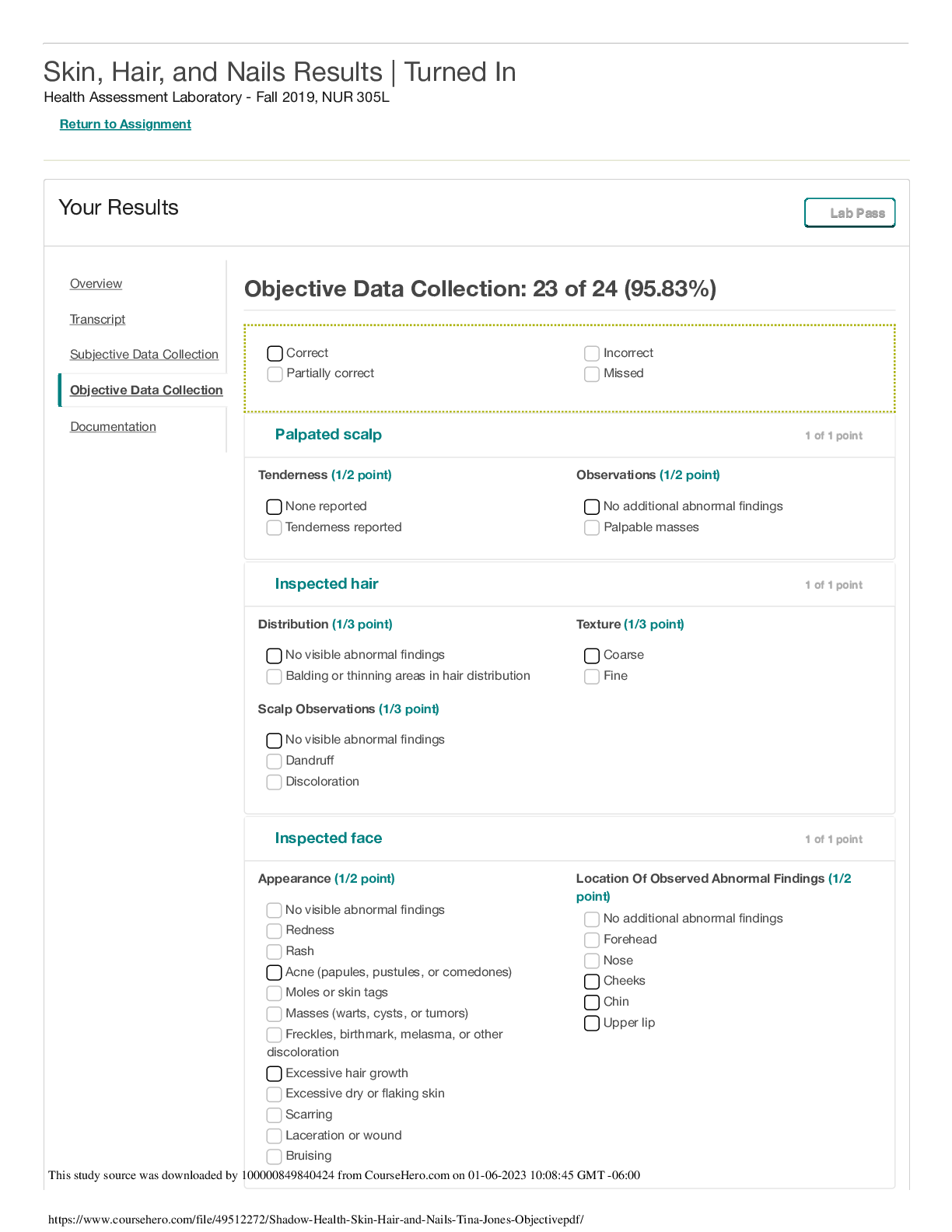
NR509 Cardiovascular Physical Assessment Assignment | Completed | Shadow Health Student Documentation Subjective TJ, 28 years, Female, African American CC: Heart palpitations, "heart beating too fa ... st" HPI: Tina, a 28 year old african american female, came into the clinic with complaints of her "heart beating too fast" and "faster than usual." It started about a month ago when work and school started to become more stressful and busy. She has had 3 to 4 episodes total and the episodes last between 5 and 10 minutes. She described the palpitations as "pounding" or "thumping." She feels anxiety as the symptoms start to appear. She states that the symptoms are worse in the morning, but physical activity or eating do not make them worse. Patient has not attempted any form of treatment for the palpitations. Current medications: Fluticasone 110mcg per 2 puffs daily Albuterol 90mcg per puff, 2 puffs as needed Acetaminophen 500-1000mg as needed for headaches Ibuprofen 600mg as needed for menstrual cramps Allergies: Environmental: Cats, Dust Medication: Penicillen No new allergies since last visit. Medical History: Diagnosed with Asthma and Type 2 Diabetes. Patient denies a diagnosis of high blood pressure, but states that it is on the high side. She does not check it regularly. ER visit for foot wound 3 months ago Past history of hospitilizations for asthma. Last one was many years ago. Patient has no known history of heart disease or high cholesterol. Social History: Patient notes a heightned stress level lately due to work and school. She also has feelings of anxiety. Patient's diet seems to be average. Patient consumes a high amount of caffeine including diet soda and up to two energy drinks a day. Patient does not exercise regulalry. Patient drinks occasionally with the last drink being two weeks ago. Patient does not smoke. Patient does not do drugs. Family History: Family has history of Cornoray Artery Disease, high cholesterol, hypertension, stroke, and obesity. ROS: General: Patient denies any recent illnesses, denies fever, denies nausea, reports low energy. Cardio: Patient denies shortness of breath, chest pain, edema, circulation problems, easy bleeding, and dizziness. Ms. Jones is a pleasant 28-year-old African American woman who presented to the clinic with complaints of 3-4 episodes of rapid heart rate over the last month. She is a good historian. She describes these episodes as “thumping in her chest” with a heart rate that is “way faster than usual”. She does not associate the rapid heart rate with a specific event, but notes that they usually occur about once per week in the morning on her commute to class. The episodes generally last between 5 and 10 minutes and resolve spontaneously. She does not know her normal heart rate or her heart rate during these episodes. She denies chest pain during the episodes, but does endorse discomfort of 3/10 which she attributes to associated anxiety regarding her rapid heart rate. She denies shortness of breath. She denies any association of symptoms with exertion. She has no known cardiac history and has never had episodes prior to this last month. She has not attempted any treatment at home and states that she is only coming to the clinic today because her family has expressed concern regarding these episodes. Social History: Ms. Jones has a job at a copy and shipping store and is a student at Shadowville Community College. She states that she has been feeling more “stressed” lately due to her school and work. She has been feeling tired at the end of the day. She denies any specific changes in her diet recently, but notes that she has not been drinking as much water as her normal. Breakfast is usually a muffin or pumpkin bread, lunch is a sandwich, dinner is a homemade meal of a meat and vegetable, snacks are French fries or pretzels. Over the past month she has increased her consumption of diet soda and “energy” drinks due to her feelings of tiredness. She generally drinks 2 energy drinks before class to “keep her focused” but states that they also make her “jittery”. She denies use of tobacco, alcohol, and illicit drugs. She does not exercise. Review of Systems: General: Denies changes in weight, but complains of end of day fatigue. She denies fevers, chills, and night sweats. She complains of intermittent dizziness. • Cardiac: Denies a diagnosis of hypertension, but states that she has been told her blood pressure was high in the past. She checks it at CVS periodically. At last check it was “140/80 or 90”. She denies known history of murmurs, angina, previous palpitations, dyspnea on exertion, orthopnea, paroxysmal nocturnal dyspnea, or edema. She has never had an EKG. • Respiratory: She denies shortness of breath, wheezing, cough, sputum, hemoptysis, pneumonia, bronchitis, emphysema, tuberculosis. She has a history of asthma, last hospitalization was age 16 for asthma, last chest XR was age 16. • Hematologic: She denies history of anemia [Show More]
Last updated: 3 years ago
Preview 1 out of 5 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$8.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Sep 13, 2021
Number of pages
5
Written in
All
Additional information
This document has been written for:
Uploaded
Sep 13, 2021
Downloads
0
Views
104