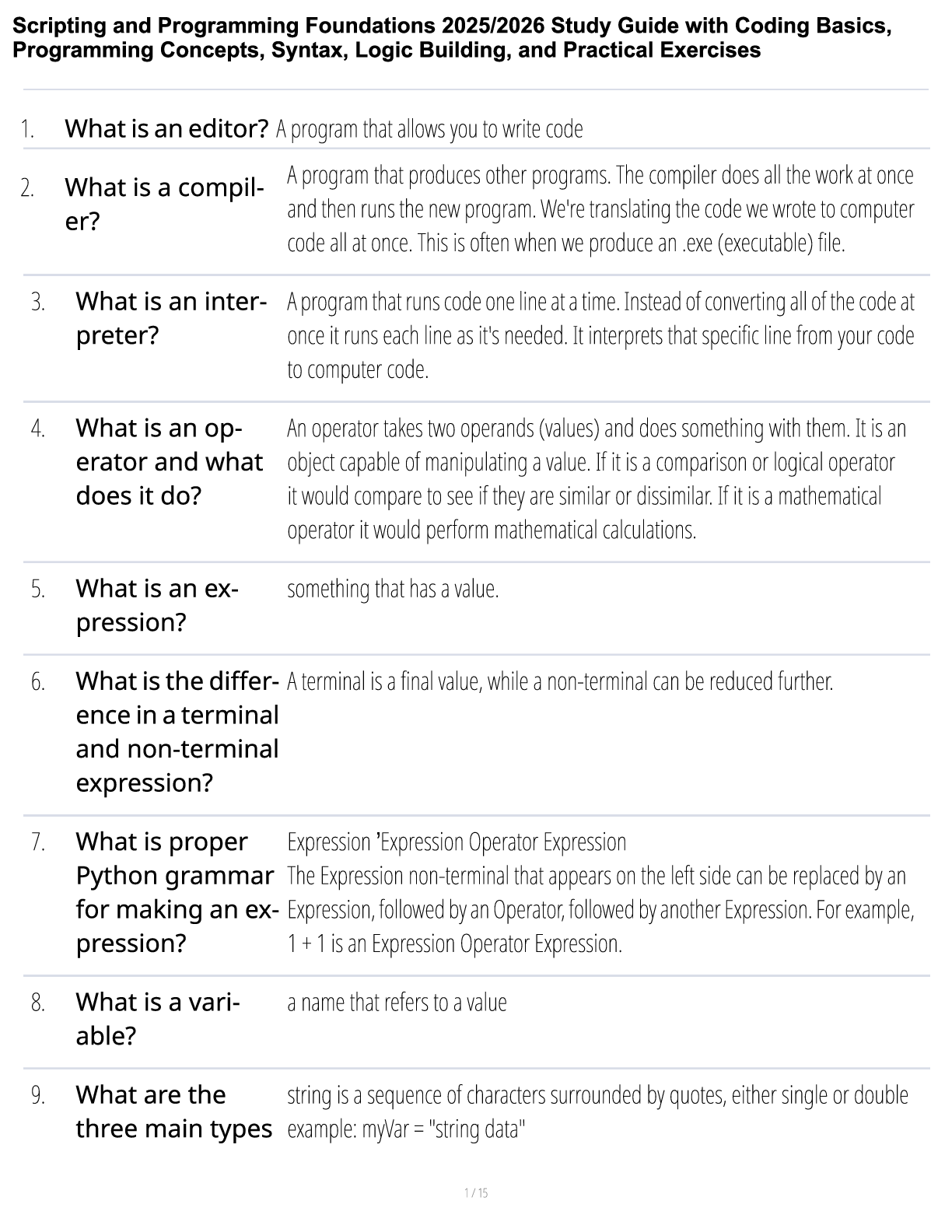
NUR 1060 Exam #1 Study Guide
This exam will consist of 48 multiple choice questions
2 Math questions
Assessment
¾
Assessment, diagnosis, outcome identification, planning, implementation, and
evaluation
...
NUR 1060 Exam #1 Study Guide
This exam will consist of 48 multiple choice questions
2 Math questions
Assessment
¾
Assessment, diagnosis, outcome identification, planning, implementation, and
evaluation
The interview
¾ Process of communication
Process of Communication: Receiving
• Awareness of messages you send is only part of process
• Words and gestures must be interpreted in a specific context to have meaning
• Receiver attaches meaning determined by his or her past experiences, culture, self-
concept, and current physical and emotional state
• Successful communication requires mutual understanding by sender and receiver
• Patients’ health problems intensify communication because patients depend on you to
get better
• Communication can be learned and polished when you are a beginning practitioner
• Communication is a tool, as basic to quality health care as tools of inspection or
palpation
Process of Communication: Internal Factors
• Awareness of internal and external factors and their influence allows you to maximize
communicating skill
• Internal factors
• Liking others
• Empathy
• Ability to listen
Process of Communication: External Factors
• Ensure privacy
• Refuse interruptions
• Physical environment
• Dress
• Note-taking may be unavoidable
• Cannot rely completely on memory for details of previous illnesses or
review of body systems
• Tape and video recording
Challenges of Note-Taking
• Breaks eye contact too often
• Shifts attention away from person, diminishing his or her sense of importance
• Interrupts patient’s narrative flow
• Impedes observation of patient’s nonverbal behavior
• May be threatening to patient’s discussion of sensitive issues
¾
Techniques of Communication
• Introducing the interview
•
• Data-gathering phase
• Verbal skills include questions to patient and your responses to what is said
• Two types of questions
• Open-ended
• Closed
• Each has a different place and function in interview
Open-Ended Questions
• Ask for narrative responses
• State topic only in general terms
• Use them in the following situations:
• To begin interview
• To introduce a new section of questions
• Whenever the patient introduces a new topic
Closed or Direct Questions
• Ask for specific information
• Elicit short one- or two-word answers, a yes or no answer, or a forced choice
• Use them in the following situations:
• After opening narrative to fill in details person may have left out
• When you need many specific facts about past health problems or during review
of systems
• To move the interview along
¾ Be particularly familiar with the following: Interviewing the older adult, people with
special needs, sexually aggressive people, crying, and patient with substance abuse
¾
Subjective Data- What the person says
Objective Data- What you obtain through physical examination
Assessment techniques
¾
Cultivating Your Senses
• The examiner will use the senses—sight, smell, touch, and hearing—to gather data
during physical examination
• Senses will be focused to assess each person’s health state
• Skills performed one at a time, in this order:
• Inspection
• Palpation
• Percussion
• Auscultation
Inspection
• Close, careful scrutiny, first of individual as a whole and then of each body system
• Begins when you first meet person with a general survey
• As you proceed through examination, start assessment of each body system with
inspection
• Inspection always comes first
• Inspection requires
• Good lighting
• Adequate exposure
• Occasional use of instruments, including otoscope, ophthalmoscope, penlight, or
nasal and vaginal specula, to enlarge your view
Palpation
• Palpation applies sense of touch to assess the following:
• Texture
• Temperature
• Moisture
• Organ location and size
• Swelling, vibration, or pulsation
• Rigidity or spasticity
• Crepitation
• Presence of lumps or masses
• Presence of tenderness or pain
Palpation Techniques
• Different parts of hands are best suited for assessing different factors
• Fingertips: best for fine tactile discrimination of skin texture, swelling, pulsation,
determining presence of lumps
• Fingers and thumb: detection of position, shape, and consistency of an organ or
mass
• Dorsa of hands and fingers: best for determining temperature because skin here is thinner than on palms
• Base of fingers or ulnar surface of hand: best for vibration
Palpation Sequence
• Start with light palpation to detect surface characteristics and accustom person to being
touched
• Then perform deeper palpation when needed
• Intermittent pressure better than one long continuous palpation
• Avoid any situation in which deep palpation could cause internal injury or pain
• Bimanual palpation requires use of both hands to envelop or capture certain body parts
or organs, such as kidneys, uterus, or adnexa, for more precise delimitation
•
Percussion
• Tapping person’s skin with short, sharp strokes to assess underlying structures
• Percussion has following uses:
• Mapping location and size of organs
• Signaling density of a structure by a characteristic note
• Detecting a superficial abnormal mass
• Percussion vibrations penetrate about 5 cm deep
• Deeper mass would give no change in percussion
• Eliciting pain if underlying structure is inflamed
• Eliciting deep tendon reflex using percussion hammer
•
Percussion Methods
• Two methods of percussion can be used
• Direct, sometimes called immediate, the striking hand directly contacts body wall
• Indirect, or mediate, using both hands, the striking hand contacts stationary
hand fixed on person’s skin
Auscultation
• Listening to sounds produced by body
• Most body sounds are soft and must be channeled through a stethoscope
• Stethoscope does not magnify sound, but it blocks out extraneous sounds
• Of all the equipment you will use, the stethoscope quickly becomes a personal
instrument
• Once you can recognize normal sounds, you can distinguish the abnormal sounds
and “extra” sounds
¾
¾
Genogram – 1 general question
¾
¾
Vital Signs: Temperature
• Cellular metabolism requires a stable core, or “deep body,” temperature of a mean of
37.2° C (99° F)
• Body maintains steady temperature through a thermostat, or feedback mechanism,
regulated in hypothalamus of brain
• Thermostat balances heat production (from metabolism, exercise, food digestion, external factors) with heat loss (through radiation, evaporation of sweat, convection, conduction)
• Various routes of temperature measurement reflect body’s core temperature
• Normal temperature is influenced by the following:
• Diurnal cycle of 1° F to 1.5° F, with trough occurring in early morning hours and
peak occurring in late afternoon to early evening
• Menstruation cycle in women: progesterone secretion, occurring with ovulation at midcycle, causes a 0.5° F to 1.0° F rise in temperature that continues until menses
• Exercise: moderate to hard exercise increases body temperature
• Age: wider normal variations occur in infant and young child due to less effective heat control mechanisms; in older adults, temperature usually lower than in other age groups, with a mean of 36.2° C (97.2° F)
• Oral temperature accurate and convenient
• Oral sublingual site has rich blood supply from carotid arteries that quickly responds to
changes in inner core temperature
• Normal oral temperature in a resting person is 37° C (98.6° F), with a range of 35.8° C to
37.3° C (96.4° F to 99.1° F)
• Rectal measures 0.4° C to 0.5° C (0.7° F to 1° F) higher
• Axillary temperature is safe and accurate for infants and young children when
environment is reasonably controlled
• Take rectal temperature only when other routes are not practical, for example, for comatose or confused persons, for persons in shock, or for those who cannot close mouth because of breathing or oxygen tubes, wired mandible, or other facial dysfunction or if no tympanic membrane thermometer equipment is available
¾
Vital Signs: Pulse
• Stroke volume: amount of blood every heart beat pumps into aorta
• About 70 mL in adult
• Force flares arterial walls and generates pressure wave, felt in periphery as pulse
• Palpating peripheral pulse gives rate and rhythm of heartbeat, as well as local
data on condition of artery
• Radial pulse usually palpated while vital signs measured
• Using pads of the first three fingers, palpate radial pulse at flexor aspect of wrist
laterally along radius bone
• Push until strongest pulsation is felt
• If rhythm is regular, count number of beats in 30 seconds and multiply by 2
• Although 15-second interval is frequently practiced, any one-beat error in
counting results in a recorded error of four beats per minute
• The 30-second interval is most accurate and efficient when heart rates are
normal or rapid and when rhythms are regular
• However, if rhythm is irregular, count for full minute
• As you begin counting interval, start your count with “zero” for first pulse
felt
Second pulse felt is “one,” and so on
• Assess pulse for the following:
• Rate
• Rhythm
• Force
• Elasticity
• Sinus arrhythmia: one irregularity commonly found in children and young adults
¾
Vital Signs: Respirations
• Normally, person’s breathing is relaxed, regular, automatic, and silent
• Because most people are unaware of their breathing, do not mention that you will be counting respirations, because sudden awareness may alter normal pattern
• Instead, maintain your position of counting radial pulse and unobtrusively count
respirations
• Count for 30 seconds or a full minute if you suspect an abnormality
• Avoid 15-second interval; the result can vary by a factor of + or –4, which is
significant with small number
• Also, a fairly constant ratio of pulse rate to respiratory rate exists, which is about
4:1
• Normally, both pulse and respiratory rates rise as a response to exercise or
anxiety
¾ - including perimeter for stages of BP
¾
• Blood pressure (BP) is force of blood pushing against side of its container, vessel wall
• Strength of push changes with event in cardiac cycle
• Systolic pressure: maximum pressure felt on artery during left ventricular
contraction, or systole
• Diastolic pressure: elastic recoil, or resting, pressure that blood exerts constantly
between each contraction
• Pulse pressure: difference between systolic and diastolic
• Reflects stroke volume
Mean arterial pressure (MAP): pressure forcing blood into tissues, averaged over cardiac cycle
¾
Average BP in young adult is 120/80 mm Hg; varies normally with many factors:
o Age: gradual rise through childhood and into adult years
o Gender: after puberty, females show a lower BP than males; after menopause,
females higher than males
o Race: African American adult’s BP usually higher than White person’s of same
age
The incidence of hypertension is twice as high in African Americans as in Whites; reasons for difference not understood fully but appear to be due to genetic heritage and environmental factors
¾ Understand the difference between nociceptive and neuropathic pain
Phase 1—Transduction
o Occurs in response to noxious stimuli
o Release variety of chemical mediators
▪ Substance P, histamine, prostaglandins, serotonin, and bradykinin
o Neurotransmitters lead to pain propagation.
▪ Along sensory afferent nerve fibers to spinal cord and terminate in dorsal
horn
▪ Second set of neurotransmitters carry pain signal—substance P,
glutamate and adenosine triphosphate (ATP).
Phase 2—Transmission
o Pain impulse moves from level of spinal cord to brain.
o If pain is not stopped it moves via various ascending fibers within the
spinothalamic tract to the thalamus.
Phase 3—Perception
o Consciousness of awareness of pain signal
o Cortical structures such as limbic system account for emotional response to pain.
o Only when “pain” has reached the cortical structures can it be perceived as pain.
Phase 4—Modulation
o Body has built-in mechanism to slow down and stop the process of a painful
stimulus that inhibits and blocks pain.
o Descending pathways release third set of neurotransmitters to produce analgesic
effect.
o Neurotransmitters include
o serotonin; norepinephrine; neurotensin; γ-aminobutyric acid (GABA); and our
own endogenous opioids, β-endorphins, enkephalins, and dynorphins.
¾
Indicates type of pain that does not adhere to typical phases inherent in nociceptive
pain
Pain due to a lesion or disease in the somatosensory system
o Neuropathic pain implies an abnormal processing of pain message that is difficult
to assess and treat.
o Often perceived long after site of injury heals
Conditions that may lead to development
o Diabetes mellitus, herpes zoster (shingles), HIV/AIDS, sciatica, trigeminal
neuralgia, phantom limb pain, and/or chemotherapy
Diagnosis
o Sustained on a neurochemical level that cannot be identified by x-ray,
computerized axial tomography (CAT) scan, or magnetic resonance imaging (MRI
)
o Electromyography and nerve-conduction studies are needed.
o The abnormal processing of neuropathic pain impulse can be continued by
peripheral or central nervous system.
Proposed mechanisms
o Spontaneous and repetitive firing of nerve fibers, almost seizure like in activity
o Central neuron excitability (wind-up)
o Minor stimuli can lead to significant pain.
¾
Acute pain
o Short-term and self-limiting:
▪ Often follows a predictable trajectory, and dissipates after an injury heals
o Self-protective purpose:
▪ Acute pain warns individual of actual or potential tissue damage.
o Incident pain:
▪ Type of acute pain that occurs predictably with certain movements
Chronic pain
can be further divided into malignant (cancer related) and nonmalignant.
o In contrast, chronic (or persistent) pain is diagnosed when pain continues for 6
months or longer.
▪ It can last 5, 15, or 20 years and beyond.
o Malignant pain often parallels pathology created by tumor cells.
o Pain induced by tissue necrosis or stretching of an organ by growing tumor.
▪ The pain fluctuates within the course of the disease
o Chronic nonmalignant pain is often associated with:
▪ musculoskeletal conditions, such as arthritis, low back pain, or
fibromyalgia
Chronic pain can be further divided into malignant (cancer related) and nonmalignant.
o Does not stop when the injury heals
▪ It persists after the predicted trajectory.
o Outlasts its protective purpose
▪ The level of pain intensity does not correspond with the physical findings.
o Unfortunately, many patients with chronic pain are not believed.
▪ Often labeled as malingers, attention seekers, drug seekers, and so forth
¾
Subjective Pain
Defined as an unpleasant sensory and emotional experience
Associated with actual or potential tissue damage or described in terms of such damage
o Pain is always subjective.
o Pain is whatever the experiencing person says it is, existing whenever he or she
says it does.
o Subjective report is gold standard of pain assessment.
o Because pain occurs on a neurochemical level, clinician cannot base diagnosis of pain exclusively on physical examination findings, although these findings can lend support.
Objective Pain
Physical examination process can help you understand the nature of the pain.
o Is it an acute or chronic condition?
o Physical findings may not always support patient’s pain complaints, particularly
for chronic pain syndromes.
o Pain should not be discounted when objective, physical evidence is not found.
o Based on the patient’s pain report, make every effort to reduce or eliminate pain with appropriate analgesic and nonpharmacologic intervention.
American Pain Society
o Important to establish a diagnosis for the cause of acute pain is a priority but
symptomatic treatment should be started during the investigation process.
o Patient comfort will better lead to cooperating with diagnostic procedures.
Joints
o Note size, contour, and circumference of joint.
o Check active or passive range of motion.
o Joint motion normally causes no tenderness, pain, or crepitation.
Muscle and skin
o Inspect skin and tissues for color, swelling, and any masses or deformity.
Abdomen
o Observe for contour and symmetry.
o Palpate for muscle guarding and organ size.
o Note any areas of referred pain.
¾
Although pain should not be considered a “normal” part of aging, it is prevalent.
o Older adults with history of comorbidities—should anticipate pain.
o Older adults often deny having pain
▪ for fear of dependency, further testing or invasive procedures, cost, and
fear of taking painkillers or becoming a drug addict.
o Observe for changes in functional behavior and/or behavioral cues.
o Comorbidity of dementia may prevent patient from identifying and describing
pain—observe behaviors—use PAINAD scale.
Skin cancer
¾
• Promoting health and self-care
• Teach skin self-examination using ABCDE rule to detect suspicious lesions
• A: asymmetry
• B: border
• C: color
• D: diameter
• E: elevation and enlargement
Signs/symptoms of melanoma
¾
• Annular or circular
o Begins in center and spreads to periphery
• Confluent
o Lesions run together
• Discrete
o Distinct and separate
• Grouped
o Cluster of lesions
• Gyrate
o Twisted, coiled, or snakelike
• Target or iris
o Resembles iris of eyes, concentric rings
• Linear
o Scratch, streak, line, or stripe
• Polycyclic
o Annular lesions grow together.
• Zosteriform
o Linear arrangement following a unilateral nerve route
¾
¾
● Macule
Papule
Nodule
Wheal
Vesicle/ Bulla
Cyst
Pustule
¾
¾
Elasticity
o Loses elasticity; skinfolds and sags
Sweat and sebaceous glands
o Decrease in number and function, leaving skin dry Senile purpura
o Discoloration due to increasing capillary fragility
Skin breakdown due to multiple factors
o Cell replacement is slower and wound healing is delayed.
Hair matrix
o Functioning melanocytes decrease, leading to gray fine hair
¾
o Dehydration, in the mucous membrane are dry, lips look parched and cracked.
Extreme dryness is fissured resembling cracks in a dry lake bed.
¾
Other:
¾
• Crepitus describes any grinding, creaking, cracking, grating, crunching, or popping that
occurs when moving a joint
Standard precaution
Using a stethoscope – appropriate use of the bell and diagram (types of sounds)
Please note:
The above guide is only meant to enhance the material you have already been studying and may not be all inclusive
[Show More]