Case 1: Back Pain
A 42-year-old male reports pain in his lower back for the past month. The pain sometimes radiates to his left leg. In determining the cause of the back pain, based on your knowledge of anatomy, what ne
...
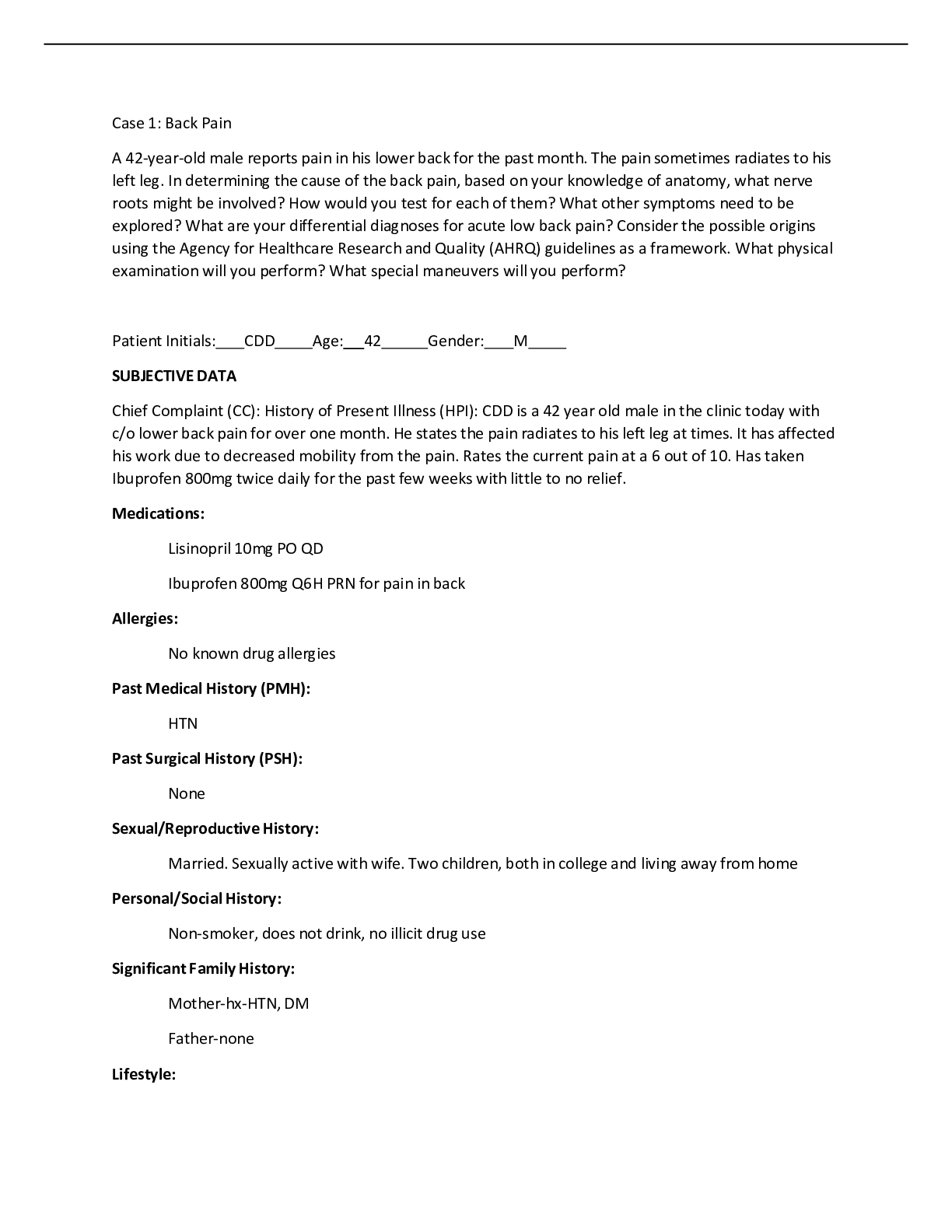
Case 1: Back Pain
A 42-year-old male reports pain in his lower back for the past month. The pain sometimes radiates to his left leg. In determining the cause of the back pain, based on your knowledge of anatomy, what nerve roots might be involved? How would you test for each of them? What other symptoms need to be explored? What are your differential diagnoses for acute low back pain? Consider the possible origins using the Agency for Healthcare Research and Quality (AHRQ) guidelines as a framework. What physical examination will you perform? What special maneuvers will you perform?
Patient Initials: CDD Age: 42 Gender: M
SUBJECTIVE DATA
Chief Complaint (CC): History of Present Illness (HPI): CDD is a 42 year old male in the clinic today with c/o lower back pain for over one month. He states the pain radiates to his left leg at times. It has affected his work due to decreased mobility from the pain. Rates the current pain at a 6 out of 10. Has taken Ibuprofen 800mg twice daily for the past few weeks with little to no relief.
Medications:
Lisinopril 10mg PO QD
Ibuprofen 800mg Q6H PRN for pain in back
Allergies:
No known drug allergies
Past Medical History (PMH):
HTN
Past Surgical History (PSH):
None
Sexual/Reproductive History:
Married. Sexually active with wife. Two children, both in college and living away from home
Personal/Social History:
Non-smoker, does not drink, no illicit drug use
Significant Family History:
Mother-hx-HTN, DM Father-none
Lifestyle:
Electrician by trade, works in a local plant 40 hours a week. Active in the gym, goes several times per week. Married for over 15 years, two sons in college.
Immunization History:
His immunizations are up to date. TDap 2013. Influenza October 1, 2015.
Review of Systems:
General: Denies fatigue, fever, chills, night sweats, and recent weight changes HEENT: No swelling in the throat. He denies throat pain. No abnormalities noted. Respiratory: Denies dyspnea, cough
CV: Denies
GI: Denies N/V/D
GU: No change in his urinary pattern.
Neuro: No syncopal episodes or dizziness, no paresthesia, headaches. No change in memory or thinking patterns; no twitches or abnormal movements; no history of gait disturbance or problems with coordination. No falls or seizure history.
Integument/Heme/Lymph: denies
Endocrine: denies Allergic/Immunologic: No known drug allergies. OBJECTIVE DATA
Physical Exam:
Vital signs:
Temperature 98.6
Pulse 78
RR 18
BP 112/72
Weight 182lb Height 5’11
Neurological: awake, alert, oriented to person, place and time Skin: warm, dry, no breakdown noted
Lungs: clear bilaterally
Cardiovascular: regular rate, S1S2 present
Abdomen: bowel sounds active x4 quadrants, no tenderness noted Peripheral vascular: No edema, pulses present and strong
HEENT: no abnormalities noted.
Musculoskeletal: low back pain that radiates to left leg with mobility limitation. Denies history of arthritis, gout, and musculoskeletal injury.
Diagnostic tests:
X-Ray lumbar spine
CT Cervical spine/lumbar spine
Differential Diagnosis (DDx):
Herniated lumbar disc-A herniated disk refers to a problem with one of the disks between the vertebrae that stack up to make the spine (Lama et al., 2014). A herniated disk can irritate nearby nerves and result in pain, numbness or weakness in an arm or leg (Lama et al., 2014). Diagnosis usually includes: CT lumbar spine, X-ray and an MRI.
Sciatica- The sciatic nerve begins at your spinal cord, goes through the hips and buttocks, and then branches down each leg (Emary, 2015). This nerve is the body’s longest nerve and one of the most important ones, as it has a direct effect on the ability to control the legs/feet (Emary, 2015). Diagnosis is usually done with a physical exam that will include testing the muscle strength and reflexes to determine if pain is a result from doing so (Emary, 2015). Also, a CT lumbar spine, X-ray and an MRI will be done.
Muscle strain- Muscle strain is damage to a muscle or its attaching tendons (Benjamin, 2012). This can occur when putting extreme pressure on muscles during the course of normal daily activities, with sudden heavy lifting, during sports, or while performing work tasks (Benjamin, 2012). A physical exam is done, and possibly an X-ray to rule out other diagnosis. Resting, with the use of NSAIDs is the most common course of treatment (Benjamin, 2012).
Spinal Stenosis- Spinal stenosis is a narrowing of the open spaces within the spine, which can put pressure on the spinal cord and the nerves that travel through the spine from the arms and legs (Ammendolia, 2014). Spinal stenosis occurs most often in the lower back and the neck. Spinal stenosis is most commonly caused by wear/tear changes in the spine related to osteoarthritis (Ammendolia, 2014).
Ankylosing Spondylitis- Ankylosing spondylitis is an inflammatory disease that can cause some of the vertebrae in the spine to fuse together (Bond, 2013). X-rays shows changes in joints and bones, though the visible signs of ankylosing spondylitis may not be evident early in the disease (Bond, 2013).
Ammendolia, C. (2014). Degenerative lumbar spinal stenosis and its imposters: three case studies. Journal Of The Canadian Chiropractic Association, 58(3), 312-319 8p. Retrieved from: http://web.b.ebscohost.com.ezp.waldenulibrary.org/ehost/pdfviewer/pdfviewer?vid=10&sid=170f1c32- 41ce-459b-8d12-eca3f64ce3ab%40sessionmgr112&hid=125
Benjamin, B. E. (2012). Interosseous Muscle Strains. Massage & Bodywork, 27(3), 108-111 4p. Retrieved from: http://web.b.ebscohost.com.ezp.waldenulibrary.org/ehost/detail/detail?vid=8&sid=170f1c32- 41ce-459b-8d12-eca3f64ce3ab%40sessionmgr112&hid=125&bdata=JnNpdGU9ZWhvc3QtbGl2ZQ%3d
%3d#AN=108129119&db=rzh
Bond, D. (2013). Ankylosing spondylitis: diagnosis and management. Nursing Standard, 28(16-18), 52-59 8p. doi:10.7748/ns2013.12.28.16.52.e7807
[Show More]










.png)