NURSING 602 Module 2 Questions for Self-Study,100% CORRECT
Document Content and Description Below
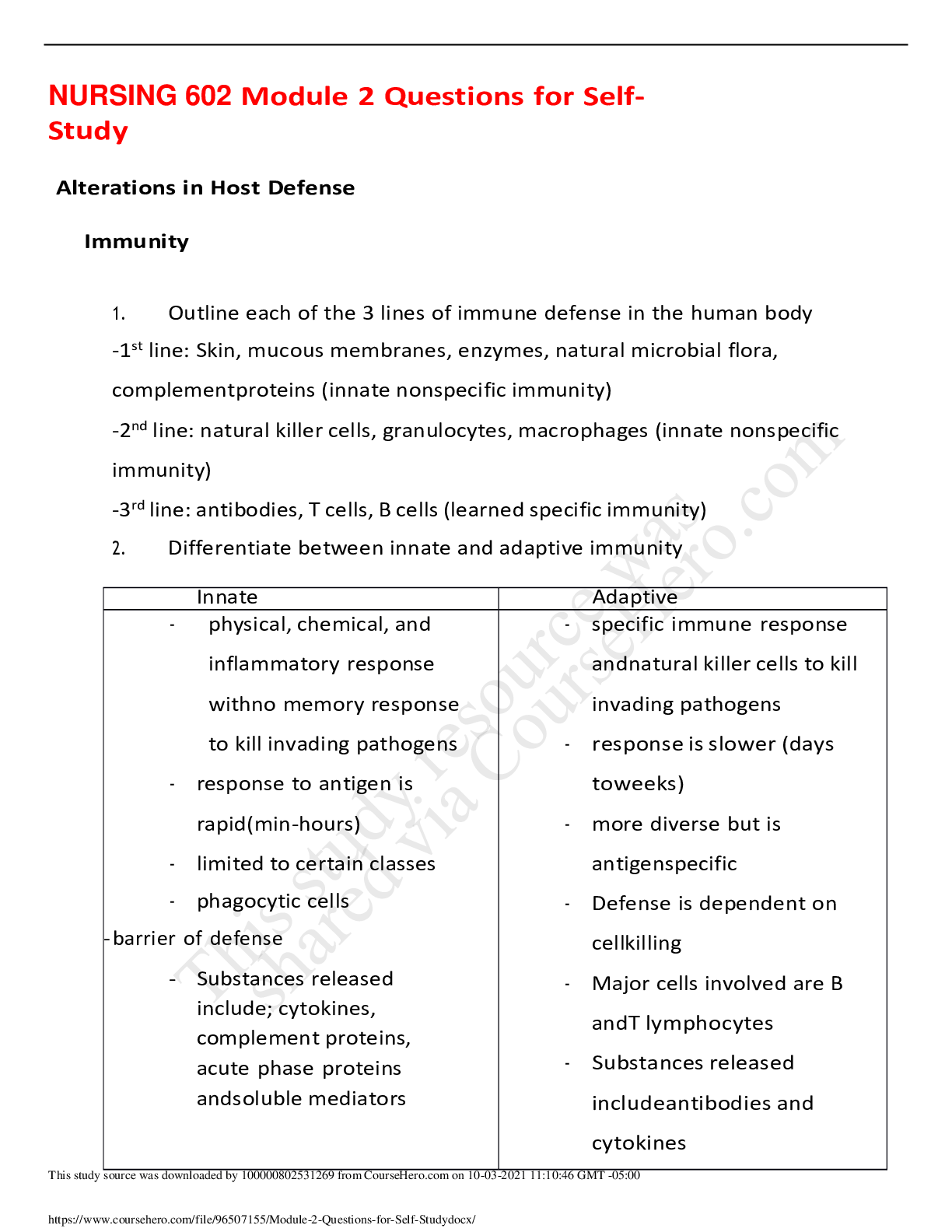
NURSING 602 Module 2 Questions for Self-Study Alterations in Host Defense Immunity 1. Outline each of the 3 lines of immune defense in the human body -1st line: Skin, mucous membranes, enzym ... es, natural microbial flora, complement proteins (innate nonspecific immunity) -2nd line: natural killer cells, granulocytes, macrophages (innate nonspecific immunity) -3rd line: antibodies, T cells, B cells (learned specific immunity) 2. Differentiate between innate and adaptive immunity Innate Adaptive - physical, chemical, and inflammatory response with no memory response to kill invading pathogens - response to antigen is rapid (min-hours) - limited to certain classes - phagocytic cells - barrier of defense - Substances released include; cytokines, complement proteins, acute phase proteins and soluble mediators - specific immune response and natural killer cells to kill invading pathogens - response is slower (days to weeks) - more diverse but is antigen specific - Defense is dependent on cell killing - Major cells involved are B and T lymphocytes - Substances released include antibodies and cytokines 3. Describe the difference between humoral and cell-mediated immunity -humoral (antibody-mediated response): involves B cells that recognize antigens or pathogens that are circulating the lymph of blood. It involves neutralization, lysis, and phagocytosis. -depends on B-lymphocytes, responsible for plasma cell production of immunoglobins, antibodies to specific antigen formation, antigen-antibody complexes formation Phases of the humoral response ▪ Primary response when antigen is first introduced ▪ Lag before the antibody is detected in serum ▪ The lag involves processing of the antigen presenting cell (APC) ▪ Recognition by T-helper cells ▪ Secondary response occurs with subsequent exposure to the antigen ▪ Antibody levels rise higher and memory cells are producing specific antibodies -cell mediated: host defenses that are mediated by antigen-specific T cells and various nonspecific cells of the immune system. - T regulatory cells are important for suppression of regulatory response -responsible for delayed hypersensitivity and transplant rejection Inflammation 1. Describe the components of the inflammatory response -brief vasoconstriction, formation of platelets to clot, releases prostaglandins and histamine to dilate blood flow to the area, increases capillary permeability, chemotaxis (neutprohils move out of the blood stream and into the injury site, diapedesis (neutrophils migrate to the injury site), phagocytosis (neutrophils eat the bacteria), tissue repair begins (fibroblasts repair the wound with collagen) -the purpose: ▪ Neutralization and destruction of invading agents ▪ Limitation of the spread of the harmful agents to other cells or surrounding tissues ▪ Preparation of the damaged tissue for repair 2. What is the underlying physiology of the cardinal signs of inflammation? -heat, redness, swelling, loss of function 3. Outline the roles that phagocytes and mast cells have in the inflammatory response -Chemotaxis: phagocytes neutrophils release chemotactic factors and attract more neutrophils. They then engulf bacteria and viruses, killing them. -Mast cells: stimulated by bacteria, viruses, injury, interleukin-1, antibody IgE- mediated then de-granulize. 4. Summarize the role of the complement proteins in during inflammation -activation of the complement cascade enhances the ability of antibodies and phagocytic cells to illuminate pathogens, then amplification and direct cell lysis occurs 5. Outline the role of cellular mediators in inflammation and fever -initiations of the acute inflammatory response, recruit other granulocytes and phagocytic cells induce adherence molecules, augment chemotaxis, promote leukocyte proliferation), remove debris, promote repair and regeneration. -the role is to remove debris and promote antibody synthesis Mediators also promote repair and regeneration by induction of fibroblast growth and production of collagen. Disorders of Host Defense 1. Differentiate between the different characteristics and types and of hypersensitivity reactions—give examples of each disorder - 1: IgE mediated mast cell and antigen result in degranulation (2-30 min to develop) o Allergies to food, pollen, contact dermatitis - 2: IgG or IgM (antibody-mediated cytotoxic) antibodies recognize and react with antigens presented on the cell (5-8 hours) binds to antigen on cells surfaces. o Blood transfusions, Rh incompatibility, graves disease - 3: Immune complexes (antigen-antibody complexes), insoluble immune complexes, deposit at various sites (2-8 hours) releases into the blood or body fluids o Arthritis, glomerulonephritis, serum sickness, vasculitis - 4: antigen – specific effector T cells (delayed 1-3 days) o Nickle allergy, poison ivy, contact dermatitis 2. Describe the possible theories regarding the causes of autoimmune disorders -a breakdown of tolerance creates sequestered antigens -an infectious disease which created foreign antigens can initiate reactions via molecular mimicry - formation of neoantigens which produce an allergic-type reaction -hapten creation that leads to a reaction against a normal antigen or protein 3. Discuss the pathophysiology of SLE - is a chronic multisystem inflammatory disease and is a failure of mechanisms to maintain self-tolerance - caused by antibodies to antinuclear antigens causing tissue damage 4. Outline the common clinical presentation/features of SLE -mouth and nose ulcers - lungs: pleuritis, pneumonitis, PE, pulmonary hemorrhage -Kidneys; blood in urine High fever Headache Butterfly rash and red patches Hair loss Pain in joints, swollen joints, arthritis Anemia, high BP Endocarditis, atherosclerosis, inflammation of the pericardium 5. Compare the direct and indirect pathway of acute transplant rejection -acute: occurs within the first few months of transplant, direct lysis of graft cells, recruitment of inflammatory cells -chronic: occurs over a long period of time, cytokines may stimulate the fibrosis of tissues -endothelial activation 6. Describe the clinical stages of the infective process Incubation: initial exposure Prodromal: occurrence of initial symptoms Invasive: rapid multiplication of the pathogen Convalescence: successful removal of infectious agent 7. Differentiate among secretory, inflammatory, and hemorrhagic diarrhea Secretory- watery, attachment to enterocytes at lumen of small bowel Inflammation- invasion of mucosal lumen, associated with fever, cramp diarrhea, salmonella, shigella Hemorrhagic- inflammatory diarrhea, clinical presentation varies according to site GI tract affected and the type of invading organism [Show More]
Last updated: 3 years ago
Preview 1 out of 9 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 03, 2021
Number of pages
9
Written in
All
Additional information
This document has been written for:
Uploaded
Oct 03, 2021
Downloads
0
Views
112