*NURSING > Study Notes > NURS 6751/ 1-17 Valvular Heart Disease (Cardiology, mitral valve, Valvular heart disease) | Best doc (All)
NURS 6751/ 1-17 Valvular Heart Disease (Cardiology, mitral valve, Valvular heart disease) | Best document to help ACE in your exam | Already GRADED A.
Document Content and Description Below
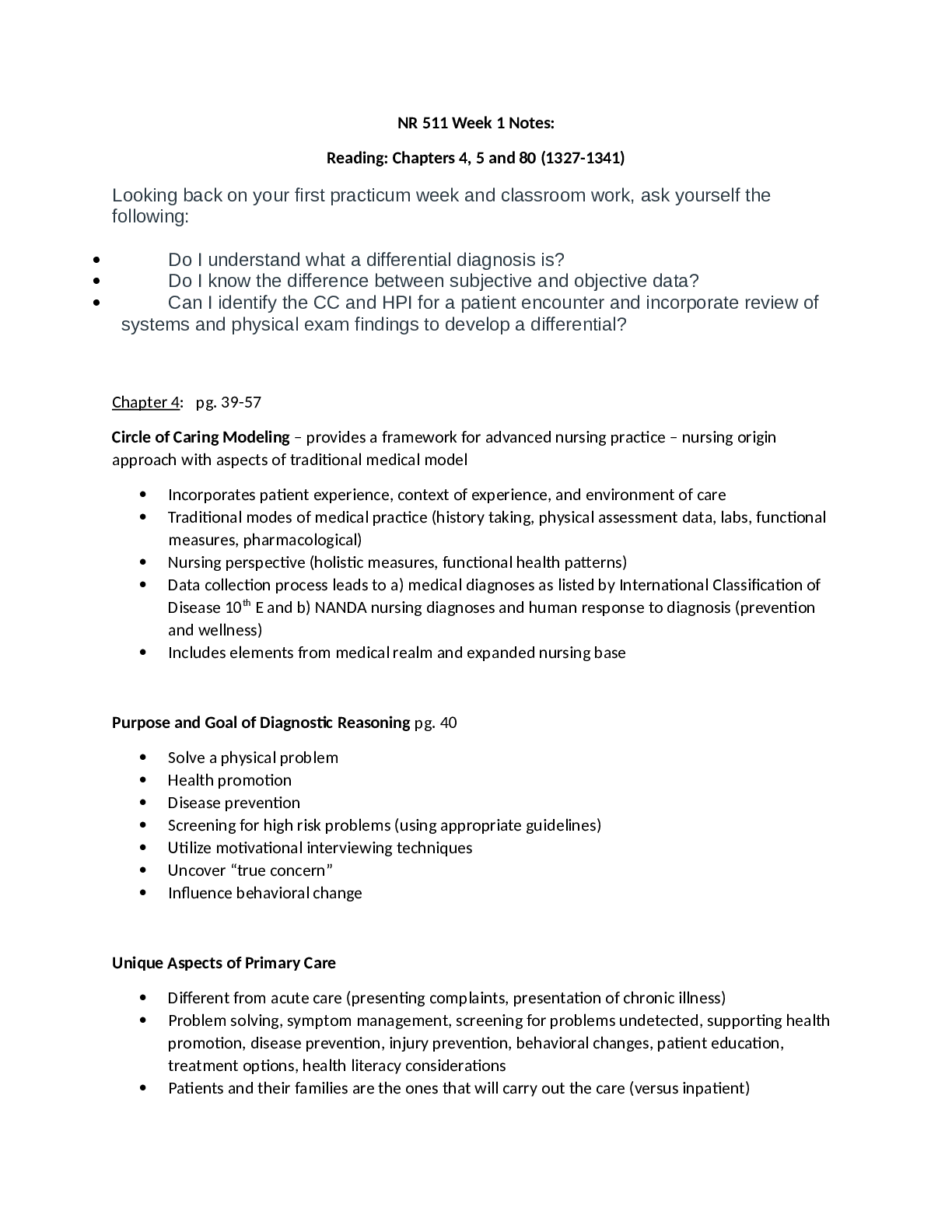
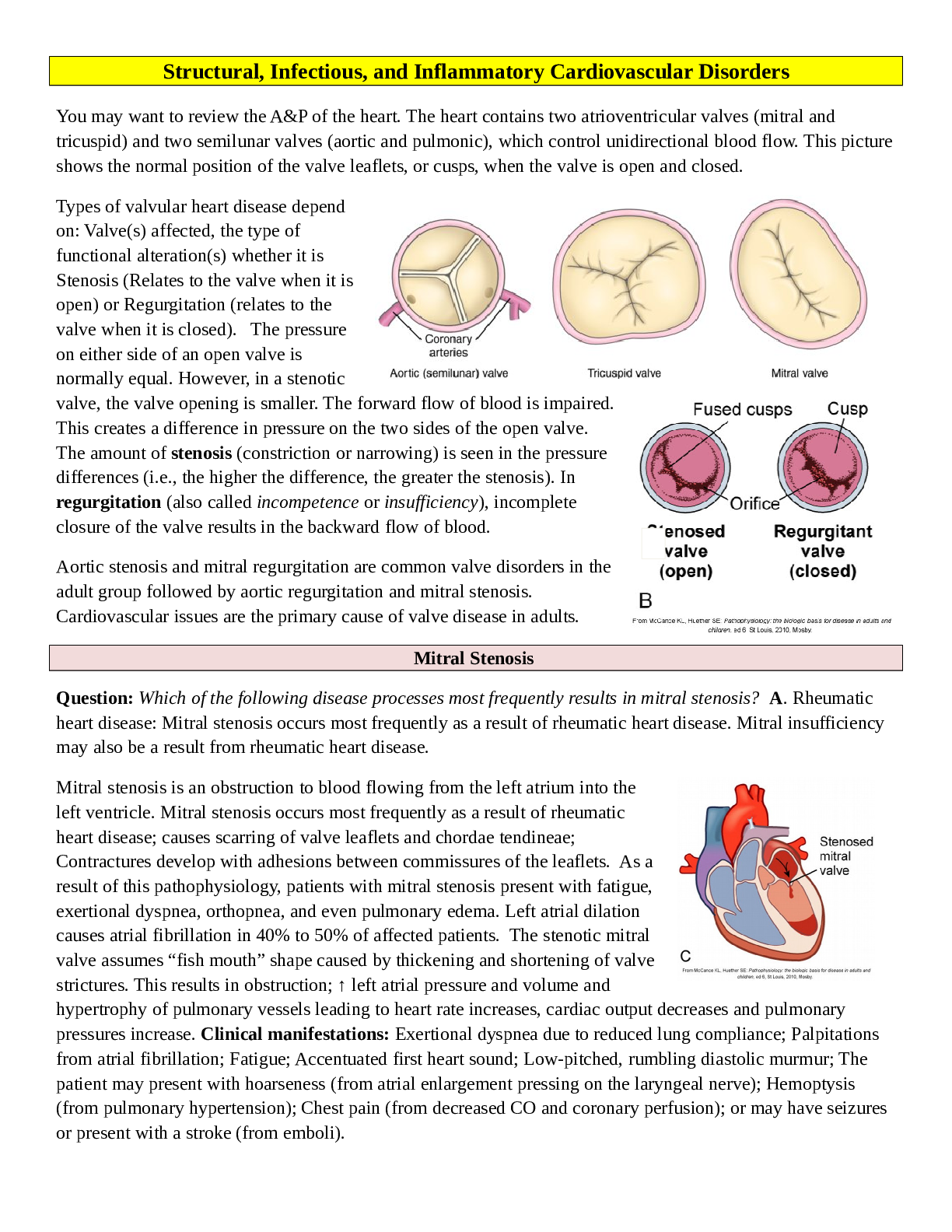
Valvular Heart Disease • Valvular Heart Disease o Occurrence & survival have improved because ▪ Better diagnostic techniques • The prevalence of valvular heart disease in the United States i... s currently around 2.5% and is expected to increase significantly with the aging of the population. This form of heart disease continues to be an important cause of perioperative morbidity and mortality. In the past 25 years there have been major advances in understanding the natural history of valvular heart disease and in improving cardiac function in patients with valvular disorders. ▪ Improved medical management ▪ Improved surgical management • Better valves o The development of better noninvasive methods of monitoring ventricular function, improved prosthetic heart valves, and better techniques for valve reconstruction as well as the formulation of guidelines for selecting the proper timing for surgical intervention have resulted in better outcomes in these patients. • Better repair methods for valves that have gone bad o Anesthetic management is dependent on predicting the reaction to changes encountered perioperatively ▪ How you manage them depends on the nature of the valvular problem & how the drugs you give them will effect these valvular problems • Valvular Stenosis ▪ When the valve gets smaller, stenotic o Orifice is constricted and narrowed o Impedes forward flow of blood o Increases workload of chamber “behind” the valve ▪ Whatever chamber (whether atria or ventricle) is trying to push blood through the smaller opening increases resistance via Ohm’s law o Increased pressure required to maintain flow ▪ If we want flow to remain same & increase resistance, we must increase pressure. The increase pressure means whatever chamber is pumping must increase the work it is doing o Eventually chamber fails ▪ Eventually whatever chamber that is affected will fail • Valvular Regurgitation o Orifice doesn’t close properly o Blood (that was just pumped out) leaks into “upstream” chamber ▪ Bad aortic valve, blood leaks back into the ventricle ▪ Bad mitral valve, leaks back into the atria o Increased volume of blood that must be pumped ▪ Must pump more blood due to the leaking o Increased volume in chambers ▪ The normal reaction by the heart is to increase volume in chambers, doesn’t necessarily have to work harder, just pump more volume o Eventually chamber fails ▪ Whether stenotic or valvular, will usually lead to failure • Valvular Heart Disease o Gradual hemodynamic changes compensated for, usually by hypertrophy ▪ Hypertrophy of chambers usually occurs slowly enough so that the heart will maintain blood flow & pt will be asymptomatic ▪ Eventually heart will be stressed or chamber will become bad, leading to failure ▪ Failure can be undiagnosed for 30 years, but may present during surgery when heart is stressed o Eventually ▪ Myocardial dysfunction • Valvular heart disease places a hemodynamic burden on the left and/or right ventricle that is initially tolerated as a result of various compensations of the cardiovascular system. o However, hemodynamic overload eventually leads to cardiac muscle dysfunction, congestive heart failure (CHF), or even sudden death. • Management of patients with valvular heart disease during the perioperative period requires an understanding of the hemodynamic alterations that accompany valvular dysfunction. The most frequently encountered cardiac valve lesions produce pressure overload (mitral stenosis, aortic stenosis) or volume overload (mitral regurgitation, aortic regurgitation) on the left atrium or left ventricle. Anesthetic management during the perioperative period is based on the likely effects of drug-induced changes in cardiac rhythm and rate, preload, afterload, myocardial contractility, systemic blood pressure, systemic vascular resistance, and pulmonary vascular resistance relative to the pathophysiology of the specific valvular lesion. ▪ CHF • Usually seen as heart failure o Acute changes can result in sudden death ▪ Usually in relation to an MI. These can result in sudden death ▪ Either an MI or you can have an aortic valve rupture & these are catastrophic • Preoperative Evaluation o Severity of heart disease ▪ Preoperative evaluation of patients with valvular heart disease includes assessment of (1) the severity of the cardiac disease, (2) the degree of impaired myocardial contractility, and (3) the presence of associated major organ system disease. o Degree of impairment of contractility/LV function ▪ Everything is focused on the LV o Assessment of co-morbidities ▪ DM, COPD, Pulmonary HTN o Physiologic compensatory adjustments ▪ Folks that have regurg tend to be tachycardic. This is one of the body’s compensatory mechanisms to the regurgitation. You don’t want to overcome this tachycardia by making them bradycardic, because you may put them into failure ▪ Recognition of compensatory mechanisms for maintaining cardiac output such as increased sympathetic nervous system activity and cardiac hypertrophy as well as consideration of current drug therapy are important. o Pharmacological management ▪ Usually these patients are followed by cards, but make sure meds make sense o Presence of prosthetic heart valves ▪ Sometimes you have to treat them differently ▪ The presence of a prosthetic heart valve introduces special considerations in the preoperative evaluation, especially if noncardiac surgery is planned. • History & Physical o Determine functional status ▪ Will give you a good indication of ability to undergo stress during surgery ▪ If patients can run several miles with no problem, they can probably withstand anesthesia without difficulty ▪ Sedentary lifestyle, chest pain walking from parking lot, may not tolerate anesthesia well ▪ Questions designed to define exercise tolerance are necessary to evaluate cardiac reserve in the presence of valvular heart disease and to provide a functional classification according to the criteria established by the New York Heart Association (Classification system is below). ▪ When myocardial contractility is impaired, patients complain of dyspnea, orthopnea, and easy fatigability. A compensatory increase in sympathetic nervous system activity may manifest as anxiety, diaphoresis, and resting tachycardia. o Murmur characteristics ▪ CHF is a frequent companion of chronic valvular heart disease, and its presence is detected by noting basilar chest rales, jugular venous distention, and a third heart sound. • Typically, elective surgery is deferred until CHF can be treated and myocardial contractility optimized. ▪ Disease of a cardiac valve rarely occurs without an accompanying murmur, reflecting turbulent blood flow across the valve. The character, location, intensity, and direction of radiation of a heart murmur provide clues to the location and severity of the valvular lesion. o Dysrhythmias ▪ A-fib creates its own set of concerns ▪ Cardiac dysrhythmias are seen with all types of valvular heart disease. Atrial fibrillation is common, especially with mitral valve disease associated with left atrial enlargement. Atrial fibrillation may be paroxysmal or chronic. o Angina with or without ▪ With CAD, it is a comorbidity ▪ Perfectly clear coronary arteries with angina is usually associated with an increase in muscle mass due to valvular problem (hypertrophy) ▪ Angina pectoris may occur in patients with valvular heart disease even in the absence of coronary artery disease. It usually reflects increased myocardial oxygen demand due to ventricular hypertrophy. ▪ The demands of this thickened muscle mass may exceed the ability of even normal coronary arteries to deliver adequate amounts of oxygen. ▪ Valvular heart disease and ischemic heart disease frequently co-exist. • 50% of patients with aortic stenosis who are older than 50 years of age have associated ischemic heart disease. The presence of coronary artery disease in patients with mitral or aortic valve disease worsens the long-term prognosis, and mitral regurgitation due to ischemic heart disease is associated with an increased mortality. • New York Heart Association – Functional Status Classification o “I’ve never seen this used. Cards may use it, but I’ve never seen it.” o Class I – Asymptomatic o Class II – Symptoms w/normal activity ▪ None at rest o Class III – Symptoms w/minimal activity ▪ None at rest o Class IV – Symptoms at rest • Murmurs o Knowing the state of the valves during the cardiac cycle will help predict lesion ▪ Murmurs occur when blood is moving through valves o Systole ▪ Aortic – open ▪ Pulmonic – open ▪ Mitral – closed ▪ Tricuspid – closed ▪ If you hear a murmur during systole, it will probably be a mitral problem (will probably have a mitral regurg problem as blood is flowing back through what should be a closed mitral valve). Blood should be flowing out of aorta because it is open, so that is normal. You don’t usually hear a murmur during systole, so it is usually a mitral problem. ▪ Correction: may hear a murmur during systole due to aortic stenosis. Stenosis creates turbulence. Murmur during systole = mitral regurg or aortic stenosis. ▪ During systole, the aortic and pulmonic valves are open, and the mitral and tricuspid valves are closed. • Therefore, a heart murmur that occurs during systole is due to stenosis of the aortic or pulmonic valves or incompetence of the mitral or tricuspid valves. o Diastole ▪ The opposite ▪ Will either be aortic regurg or mitral stenosis ▪ “So just keep those things straight in your head” ▪ During diastole, the aortic and pulmonic valves are closed, and the mitral and tricuspid valves are open. • Therefore, a diastolic heart murmur is due to stenosis of the mitral or tricuspid valves or incompetence of the aortic or pulmonic valves. • Drug Therapy o Get a detailed drug list ▪ Beta blockers ▪ Digitalis • Controls rate for folks that have a-fib ▪ Nitrates • If they have angina ▪ Antidysrhythmics ▪ CC blockers ▪ ACE inhibitors • Control BP & things like that ▪ Diuretics • To control fluid volume ▪ Anticoagulants • For a-fib to prevent generation of clots ▪ Modern drug therapy for valvular heart disease may include β-blockers, calcium channel blockers, and digitalis for heart rate control; angiotensin-converting enzyme inhibitors and vasodilators to control blood pressure and afterload; and diuretics, inotropes, and vasodilators as needed to control heart failure. o Ensure drugs make sense ▪ The big thing is to make sure drugs make sense. If patient has no drugs with diagnosed valve problem, ask the last time they’ve seen cardiology o Continue meds until day of surgery o Incorporate chronic meds into anesthesia care plan ▪ If on BB & get tachy, use a BB. Don’t get creative. Use what their body is used to. Not a time to think outside the box. ▪ Antidysrhythmic therapy may also be necessary. ▪ Certain cardiac lesions such as aortic and mitral stenosis require a slow heart rate to prolong the duration of diastole and improve left ventricular filling and coronary blood flow. ▪ The regurgitant valvular lesions such as aortic and mitral regurgitation require afterload reduction and a somewhat faster heart rate to shorten the time for regurgitation. ▪ Atrial fibrillation requires a controlled ventricular response so that activation of the sympathetic nervous system, as during tracheal intubation or in response to surgical stimulation, does not cause sufficient tachycardia to significantly decrease diastolic filling time and stroke volume. • ECG Findings o P mitrale – enlarged atrium ▪ Enlarged or notched P wave ▪ Occurs due to enlarged atrium secondary to regurg problem ▪ The electrocardiogram (ECG) often exhibits characteristic changes due to valvular heart disease. Broad and notched P waves (P mitrale) suggest the presence of left atrial enlargement typical of mitral valve disease. o Axis deviation ▪ Indicative of hypertrophy ▪ Left and right ventricular hypertrophy can be diagnosed by the presence of left or right axis deviation and high voltage. o Dysrhythmias ▪ Other common ECG findings include dysrhythmias, conduction abnormalities, and evidence of active ischemia or previous myocardial infarction. o Conduction abnormalities o Ischemia o Previous MI • Echocardiography o Recent echo results are essential ▪ To assess for changes & to make sure they are optimized o Findings provide info regarding ▪ Valve area • How big is the valve ▪ Transvalvular pressure gradients • Estimates pressure gradients across valve which determines how bad their condition is • Transvalvular pressure gradients determined at the time of cardiac catheterization indicate the severity of the valvular heart disease. ▪ Amount of regurgitation ▪ Amount of stenotic flow • Mitral and aortic stenosis are considered to be severe when transvalvular pressure gradients are more than 10 mm Hg and 50 mm Hg, respectively. • In patients with mitral stenosis or mitral regurgitation, measurement of pulmonary artery pressure and right ventricular filling pressure may provide evidence of pulmonary hypertension and right ventricular failure. • However, when CHF accompanies aortic stenosis, transvalvular pressure gradients may be smaller because of the inability of the dysfunctional left ventricular muscle to generate a large gradient. ▪ Degree of hypertrophy in the LV ▪ Contractility of the LV o Catheterization can also be done if you need more info ▪ Cardiac catheterization can provide information about the presence and severity of valvular stenosis and/or regurgitation, coronary artery disease, and intracardiac shunting and can help resolve discrepancies between clinical and echocardiographic findings. o The size and shape of the heart and great vessels and pulmonary vascular markings can be evaluated by chest radiography. On a posteroanterior chest radiograph cardiomegaly can be established if the heart size exceeds 50% of the internal width of the thoracic cage. Abnormalities of the pulmonary artery, left atrium, and left ventricle can be noted along the left heart border, and right atrial and right ventricular enlargement along the right heart border. Enlargement of the left atrium can result in elevation of the left mainstem bronchus. Valvular calcifications may be identified. Vascular markings in the peripheral lung fields are sparse in the presence of significant pulmonary hypertension. o Echocardiography with color flow Doppler imaging is essential for noninvasive evaluation of valvular heart disease (Table 2-2, above). It is particularly useful in evaluating the significance of cardiac murmurs such as systolic ejection murmurs when aortic stenosis is suspected and in detecting the presence of mitral stenosis. It permits determination of cardiac anatomy and function, presence of hypertrophy, cavity dimensions, valve area, transvalvular pressure gradients, and the magnitude of valvular regurgitation. • Prosthetic Heart Valves o Mechanical – durable, highly thrombogenetic ▪ Made out of carbon fibers & titanium ▪ More durable, but tend to generate more emboli ▪ If healthy person, will usually get a mechanical valve that will usually last 20 years. You can usually tolerate being on Coumadin that long ▪ Prosthetic heart valves may be mechanical or bioprosthetic. ▪ Mechanical valves are composed primarily of metal or carbon alloys and are classified according to their structure, such as caged-ball, single tilting-disk, or bileaflet tilting-disk valves. o Bioprosthetic – less durable, less thrombogenetic ▪ Porcine or bovine or human valve. They can even take the pulmonic valve & use that as aortic valve ▪ Less durable and less thrombolic ▪ If an older person, don’t want to be on Coumadin to increase risk of ICH, so they will probably die of something else before their valve gives out ▪ Bioprostheses may be heterografts, composed of porcine or bovine tissues mounted on metal supports, or homografts, which are preserved human aortic valves. ▪ Prosthetic valves differ from one another with regard to durability, thrombogenicity, and hemodynamic profile. • Mechanical valves are very durable, lasting at least 20 to 30 years, whereas bioprosthetic valves last about 10 to 15 years. • Mechanical valves are highly thrombogenic and require long-term anticoagulation. Because bioprosthetic valves have a low thrombogenic potential, long-term anticoagulation often is not necessary. o Mechanical valves are preferred in patients who are young, have a life expectancy of more than 10 to 15 years, or require long-term anticoagulation therapy for another reason, such as atrial fibrillation. o Bioprosthetic valves are preferred in elderly patients and in those who cannot tolerate anticoagulation. o Change is murmur or click indicates a problem ▪ This means something is loosening/tightening up & needs to be evaluated o Complications ▪ Valve thrombosis • Prosthetic heart valves can be associated with significant complications whose presence should be considered during the preoperative evaluation (Table 2-3). Because of the risk of thromboembolism, patients with mechanical prosthetic heart valves require long- term anticoagulant therapy. ▪ Systemic emboli • Usually an emboli ▪ Structural failure ▪ Hemolysis • Usually a subclinical amount of hemolysis, causing gallstones, etc. • Subclinical intravascular hemolysis, evidenced by an increased serum lactate dehydrogenase concentration, decreased serum haptoglobin concentration, and reticulocytosis, is noted in many patients with normally functioning mechanical heart valves. The incidence of pigmented gallstones is increased in patients with prosthetic heart valves, presumably as a result of chronic low-grade intravascular hemolysis. • Severe hemolytic anemia is uncommon, and its presence usually indicates valvular dysfunction or endocarditis. ▪ Paravalvular leak ▪ Endocarditis • Increased risk of endocarditis, an infective process in the heart that can be mild or life threatening • Antibiotic prophylaxis is necessary to decrease the perioperative risk of infective endocarditis. • Anticoagulation o Anticoagulated due to increased risk of clot formation ▪ Will be chronically anticoagulated o Determine if anticoagulation needs to be halted (depends on surgery planned) ▪ Whether you stop anticoagulation or not depends on surgery. Hip replacement = must come off Coumadin. Be in consultation with surgeon to acquire expected EBL. ▪ Patients may need to discontinue anticoagulation before surgery. However, this temporary discontinuation of anticoagulant therapy puts patients with mechanical heart valves or atrial fibrillation at risk of arterial or venous thromboembolism due to a rebound hypercoagulable state and to the prothrombotic effects of surgery. The risk of thromboembolism is estimated to be about 5% to 8%. Anticoagulation may be continued in patients with prosthetic heart valves who are scheduled for minor surgery in which blood loss is expected to be minimal. When major surgery is planned, however, warfarin is typically discontinued 3 to 5 days preoperatively. o Heparin window if anticoagulation must be maintained ▪ Stop Coumadin about 3 days before surgery & place them on Heparin IV. Keep them anticoagulated with Heparin. Stop Heparin the AM of surgery, draw coags & make sure it is back to baseline, so you “open the window.” Do surgery. Then put them back on heparin asap after surgery, then switch them back from Heparin to Coumadin when they can take PO meds. ▪ Heparin has a much shorter DOA than Coumadin. ▪ Intravenous unfractionated heparin or subcutaneous low-molecular-weight heparin is administered after discontinuation of warfarin and continued until the day before or the day of surgery. The heparin can be restarted postoperatively when the risk of bleeding has lessened and can be continued until effective anticoagulation is again achieved with oral therapy. When possible, elective surgery should be avoided in the first month after an acute episode of arterial or venous thromboembolism. ▪ Anticoagulant therapy is particularly important in parturients with prosthetic heart valves, because the incidence of arterial embolization is greatly increased during pregnancy. However, warfarin administration during the first trimester can be associated with fetal defects and fetal death. Therefore, warfarin is discontinued during pregnancy and subcutaneous standard or low- molecular-weight heparin is administered until delivery. Low-dose aspirin therapy is safe for the mother and fetus and can be used in conjunction with the heparin therapy. • Bacterial Endocarditis o Standards established by American Heart Association ▪ Endocarditis is an infective process, usually with valves. Can destroy heart valves & cause a lot of vegetative growth/bacterial growth within heart which can cause emboli & get shot up into your brain & cause strokes ▪ The most recent AHA Guidelines for the Prevention of Infective Endocarditis (2007) represent a radical departure from prior recommendations and dramatically reduce the indications for antibiotic prophylaxis. o Old standard – if they had a murmur give them antibiotics for any invasive procedure (getting your teeth cleaned or having pulmonary surgery) o New standard ▪ ADL more important than surgery for determining risk of exposure • ADLs like brushing your teeth or picking your nose actually cause more instances of endocarditis than procedures within the hospital. So all the doses of antibiotics were a waste. You will benefit more from brushing your teeth qday than getting abx when going to the dentist. • Current scientific data suggest that infective endocarditis is more likely to result from frequent exposure to bacteremia associated with daily activities than from bacteremia associated with dental, gastrointestinal, or genitourinary tract procedures. o For example, maintenance of good oral health and oral hygiene reduces bacteremia associated with normal daily activities (chewing, teeth brushing, flossing, use of toothpicks, etc.) and is more important than prophylactic antibiotics in reducing the risk of endocarditis. o Endocarditis prophylaxis may prevent an exceedingly small number of cases of endocarditis, if any, in at-risk patients. o It also appears that the risk of antibiotic-associated adverse events exceeds the benefits of endocarditis prophylaxis overall and that the common use of antibiotic prophylaxis promotes the emergence of antibiotic-resistant organisms. ▪ Treat those who would suffer the most if infected • These are the high risk patients (next slides) • Experts feel that infective endocarditis prophylaxis should be administered not to individuals with a high cumulative lifetime risk of contracting endocarditis but rather to individuals at highest risk of adverse outcomes if they develop endocarditis. • It appears that only a very small group of patients with heart disease are likely to have the most severe forms and complications of endocarditis. The conditions associated with this high risk are listed in Table 2-4 (lecture notes below). The new AHA guidelines target endocarditis prophylaxis only to patients with these conditions. The recommendations regarding which antibiotic to use for endocarditis prophylaxis are not dissimilar from previous recommendations. • Bacterial Endocarditis o High risk patients ▪ Prosthetic valve ▪ Previous infective endocarditis ▪ Congenital heart disease (not associated with their valves) • Unrepaired cyanotic disease • Repairs with prosthetic materials • Incomplete/inadequate repairs ▪ s/p heart transplant • Bacterial Endocarditis Recommendation o When to give prophylaxis ▪ Dental procedures ▪ Invasive procedures of respiratory tract (bronch for biopsy), musculoskeletal tissue (infected), or (infected) skin structures ▪ Invasive procedures of INFECTED skin, musculoskeletal tissue, or skin structures • Won’t need abx for gallbladder surgery, but would need for abscess drainage o Not recommended for GU or GI procedures o In summary, the major changes in the updated AHA guidelines for infective endocarditis prophylaxis are these: ▪ (1) Antibiotic prophylaxis for infective endocarditis is recommended only under a very few conditions. ▪ (2) Antibiotic prophylaxis is recommended for dental procedures that involve manipulation of gingival tissues or the periapical regions of the teeth, or perforation of the oral mucosa. ▪ (3) Antibiotic prophylaxis is recommended for invasive procedures, that is, those that involve incision or biopsy of the respiratory tract or infected skin, skin structures, or musculoskeletal tissue. ▪ (4) Antibiotic prophylaxis is not recommended for genitourinary or gastrointestinal tract procedures. • Mitral Stenosis o Usually if you have stenosis of a valve, then the leaflets are screwed up, so very commonly you will have regurg (and vice versa). We will talk about them independently, but usually they are in conjunction o Females > Males ▪ Mitral stenosis primarily affects females. o Primary cause is rheumatic fever ▪ No longer very common in U.S. ▪ Very common in developing countries, so you will see it in the immigrant populations ▪ The most common cause of mitral stenosis is rheumatic heart disease. The incidence of rheumatic fever in developed countries is very low, but the disease continues to be common in developing countries. o Slow onset of symptoms (20-30 years) before people become symptomatic ▪ The mitral valve gets more & more stenotic over time ▪ Diffuse thickening of the mitral leaflets and subvalvular apparatus, commissural fusion, and calcification of the annulus and leaflets are typically present. This process occurs slowly, and many patients do not become symptomatic for 20 to 30 years after the initial episode of rheumatic fever. Over time, the mitral valve becomes stenotic, and CHF, pulmonary hypertension, and right ventricular failure may develop. o Eventually untreated patients develop ▪ CHF • Very often R CHF (occurs in LA, backs up into lungs, then into the RV) ▪ Pulmonary HTN • Dyspnea, things like that ▪ R Ventricular failure o Isolated MS in about 40% of cases ▪ About 60% will have mitral stenosis & some form of aortic regurg ▪ Rheumatic heart disease presents as isolated mitral stenosis in about 40% of patients. If aortic and/or mitral regurgitation accompany mitral stenosis, there is often evidence of left ventricular dysfunction. • Mitral Stenosis o Other Causes ▪ Rheumatoid arthritis • Bad disease. Causes a lot of congenital problems related to collagen in the valve ▪ Systemic Lupus Erythematosus ▪ Congenital valvular disease • Born with it ▪ Carcinoid syndrome ▪ Much less common causes of mitral stenosis include carcinoid syndrome, left atrial myxoma, severe mitral annular calcification, endocarditis, cor triatriatum, rheumatoid arthritis, systemic lupus erythematosus, congenital mitral stenosis, and iatrogenic mitral stenosis after mitral valve repair. o Presenting S&S (pulmonary-related d/t blood backing up into lungs) ▪ DOE ▪ Orthopnea • Sleep sitting up ▪ Paroxysmal nocturnal dyspnea • Get SOB when sleeping & will wake up ▪ Patients with mitral stenosis typically exhibit dyspnea on exertion, orthopnea, and paroxysmal nocturnal dyspnea as a result of high left atrial pressure. Left ventricular contractility is usually normal. • Pathophysiology o Impairment of flow of blood from LA to LV ▪ The normal mitral valve orifice area is 4 to 6 cm2. Mitral stenosis is characterized by mechanical obstruction to left ventricular diastolic filling secondary to a progressive decrease in the size of the mitral valve orifice. o Creates an increase in L atrial volume & pressure ▪ This valvular obstruction produces an increase in left atrial volume and pressure. o Gradually causes L atrial dilation (commonly causes A Fib) ▪ Because it gets bigger (due to volume increase), it disrupts normal conduction path in left atrium, causing a-fib ▪ However, stroke volume will decrease during stress-induced tachycardia or when effective atrial contraction is lost, as with atrial fibrillation. o LV volume & pressure maintained at rest – during mild disease ▪ With mild mitral stenosis, left ventricular filling and stroke volume are maintained at rest by an increase in left atrial pressure. o LV contractility often preserved (decreases with tachycardia) ▪ You’re not really affecting LV, so there is not a lot of change. The LV does not hypertrophy here. o Increase in pulmonary venous pressure ▪ Pulmonary edema when pulmonary pressure > plasma oncotic pressure • Blood is backing up from LA from pulmonary arteries, causing pulmonary edema. This occurs when pulmonary pressure gets greater than plasma oncotic pressure. Blood backs up, so when pulm hydrostatic pressure is greater than pulm oncotic pressure, it draws fluid in, giving you pulm edema • Overt pulmonary edema is likely when the pulmonary venous pressure exceeds plasma oncotic pressure. If the increase in left atrial pressure is gradual, there is an increase in lymphatic drainage from the lungs and thickening of the capillary basement membrane that enables patients to tolerate an increased pulmonary venous pressure without development of pulmonary edema. • Over time changes in the pulmonary vasculature result in pulmonary hypertension, and eventually right-sided heart failure may occur. Left ventricular function is usually preserved. Episodes of pulmonary edema typically occur with atrial fibrillation, sepsis, pain, and pregnancy. ▪ Decreased pulmonary compliance ▪ Increased work of breathing ▪ DOE • Will eventually progress to hypoxia and pulmonary HTN • Symptoms usually develop when mitral valve area is less than 1.5 cm2. As the disease progresses the pulmonary venous pressure is increased in association with the increase in left atrial pressure. The result is transudation of fluid into the pulmonary interstitial space, decreased pulmonary compliance, and increased work of breathing, which leads to progressive dyspnea on exertion. • Mitral Stenosis Dx o Echo findings ▪ MVG is how much pressure atrium has to generate to push blood through. When it gets greater than >10, that’s when blood gets backed up & you run into problems. ▪ “KNOW the normal & severes” ▪ Echocardiography is used to assess the anatomy of the mitral valve, including the degree of leaflet thickening, calcification, changes in mobility, and extent of involvement of the subvalvular apparatus. The severity of mitral stenosis is assessed by calculation of mitral valve area and measurement of the transvalvular pressure gradient. Echocardiography also allows evaluation of cardiac chamber dimensions, pulmonary hypertension, left and right ventricular function, and other valvular disease, and examination of the left atrial appendage for the presence or absence of thrombus. ▪ Patients with mitral stenosis usually become symptomatic when the size of the mitral valve orifice has decreased at least 50%. When the mitral valve area is less than 1 cm2, a mean atrial pressure of about 25 mm Hg is necessary to maintain adequate left ventricular filling and resting cardiac output. Pulmonary hypertension is likely if the left atrial pressure is above 25 mm Hg over the long term. When the mitral transvalvular pressure gradient is higher than 10 mm Hg (normal value is <5 mm Hg), it is likely that mitral stenosis is severe. When mitral stenosis is severe, any additional stress such as fever or sepsis may precipitate pulmonary edema. Normal Mild Severe Orifice (cm2) 4-6 1.6-2.0 <1.0 MVG (mmHg) <5 6 >10 • Mitral Stenosis Dx o Opening snap early in diastole ▪ It is a “snap” instead of the normal “lub” ▪ Clinically, mitral stenosis is recognized by the characteristic opening snap that occurs early in diastole and by a rumbling diastolic heart murmur best heard at the apex or in the left axilla. Vibrations set in motion by the opening of the mobile but stenosed valve cause the opening snap. Calcification of the valve and greatly reduced leaflet mobility result in disappearance of the opening snap. o Rumbling diastolic murmur in apex or left axilla ▪ It is turbulent as it is coming through stenotic valve o ECG – broad notched “P” wave ▪ Broad notched P waves on the ECG suggest left atrial enlargement. o LA enlargement on CXR ▪ Left atrial enlargement is often visible on chest radiographs as straightening of the left heart border and elevation of the left mainstem bronchus. The "double density" of an enlarged left atrium, mitral calcification, and evidence of pulmonary edema or pulmonary vascular congestion may also be seen. o A – fib is common. That is a hint that there is mitral valve stenosis ▪ Atrial fibrillation is present in about 1/3 of patients with severe mitral stenosis. o Stasis of blood in the distended left atrium predisposes patients with mitral stenosis to a higher risk of systemic thromboembolism. Venous thrombosis is also more likely because of the decreased physical activity of these patients. • Mitral Stenosis Treatment o Diuretics to reduce mild pulmonary edema ▪ When symptoms of mild mitral stenosis develop, diuretics can decrease the left atrial pressure and relieve symptoms. o A Fib treatment ▪ Rate control (beta blockers, CCB, Digoxin) • If atrial fibrillation occurs, heart rate control may be achieved with digoxin, β-blockers, calcium channel blockers, or a combination of these medications. Control of the heart rate is critical because tachycardia impairs left ventricular filling and increases left atrial pressure. ▪ Anticoagulation (Coumadin til INR is 2.5-3x normal) • Anticoagulation is required in patients with mitral stenosis and atrial fibrillation, because the risk of embolic stroke in such patients is about 7% to 15% per year. Warfarin is administered to a target international normalized ratio (INR) of 2.5 to 3.0. o Valvular repair or replacement ▪ Definitive treatment ▪ They always want to try to repair rather than replace. To replace, you take out ring around leaflets, which screws up geometry ▪ Surgical correction of mitral stenosis is indicated when symptoms worsen and pulmonary hypertension develops. ▪ Mitral stenosis can sometimes be corrected by percutaneous balloon valvotomy. If heavy valvular calcification or valve deformity is present, surgical commissurotomy, valve reconstruction, or valve replacement is performed. In patients with concomitant severe tricuspid regurgitation (due to pulmonary hypertension), tricuspid valvuloplasty or ring annuloplasty can be performed together with the mitral valve surgery. • Anesthetic Management o Avoid ▪ Tachycardia (decrease LV filling) • Want to maximize amount that gets into atria. If you have tachycardia, you have decreased preload, which decreases cardiac output. Want to keep them at a low-normal HR ▪ A – Fib (sinus tach or a rapid ventricular response with atrial fibrillation) • Avoid a-fib. If they have a-fib, they have no atrial kick which decreases filling • Management of anesthesia for noncardiac surgery in patients with mitral stenosis includes prevention and treatment of events that can decrease cardiac output or produce pulmonary edema. • The development of atrial fibrillation with a rapid ventricular response significantly decreases cardiac output and can produce pulmonary edema. Treatment consists of cardioversion or intravenous administration of amiodarone, β-blockers, calcium channel blockers, or digoxin. ▪ Increase in central blood volume, as associated with overtransfusion or head-down positioning • Increased risk of pulmonary edema with hypervolemia • Want to keep them euvolemic • Excessive perioperative fluid administration, placement in Trendelenburg's position, or autotransfusion via uterine contraction increases central blood volume and can precipitate CHF. ▪ Decrease in SVR/hypotension • Causes reflex tachycardia o Avoid hypotension which is usually associated with a decrease in SVR. Normal reflex with this is tachycardia. You don’t want hypotension because you don’t want to create tachycardia o In patients with severe mitral stenosis, a sudden decrease in systemic vascular resistance may not be tolerated, because the normal response to hypotension— that is, a reflex increase in heart rate—itself decreases cardiac output. o If necessary, systemic blood pressure and systemic vascular resistance can be maintained with vasoconstrictor drugs such as phenylephrine. Use of vasopressin may also be considered since it has minimal effect on pulmonary artery pressure. ▪ Hypoxia or hypercarbia that may exacerbate pulmonary hypertension and evoke right heart failure • Worsens existing pulmonary hypertension o Due to pulmonary vasoconstriction caused by hypoxia or hypercarbia o Pulmonary hypertension and right ventricular failure may be precipitated by numerous factors, including hypercarbia, hypoxemia, lung hyperinflation, and an increase in lung water. Right ventricular failure may require support with inotropic and pulmonary vasodilating drugs. • Mitral Regurgitation o Usually occurs along with mitral stenosis ▪ Mitral regurgitation due to rheumatic fever is usually associated with some degree of mitral stenosis. o Isolated regurg results from cardiac injury ▪ MI ▪ Papillary muscle dysfunction • Isolated regurg is usually associated with problems with papillary muscles or chordae tendineae ▪ Rupture of chordae tendineae • If you have problems here, leaflets within the ventricles will get floppy, causing backflow of blood into the atrium ▪ Isolated mitral regurgitation can be associated with ischemic heart disease or result from papillary muscle dysfunction, mitral annular dilation, or rupture of chordae tendineae. o Other causes ▪ Endocarditis – infection of endocardium ▪ Severe MVP (mitral valve prolapse) ▪ Lupus ▪ RA ▪ Other causes of mitral regurgitation include endocarditis, mitral valve prolapse, trauma, congenital heart disease (such as an endocardial cushion defect), left ventricular hypertrophy, cardiomyopathy, myxomatous degeneration, systemic lupus erythematosus, rheumatoid arthritis, ankylosing spondylitis, and carcinoid syndrome. • Mitral Regurgitation Pathophysiology o Backflow of blood from LV into the LA during systole o Decrease in LV forward stroke volume and CO ▪ Instead of pushing blood through aorta, it is going back into the atria ▪ The basic hemodynamic derangement in mitral regurgitation is a decrease in forward left ventricular stroke volume and cardiac output. A portion of every stroke volume is regurgitated through the incompetent mitral valve back into the left atrium, which results in left atrial volume overload and pulmonary congestion. o Regurg causes ▪ LA volume overload • Pushing blood back into the atrium that the atrium just pushed out. This volume overloads them, causing pulmonary congestion. Now we are sacrificing left ventricular forward flow & CO. ▪ Pulm congestion o Regurg of >60% of stroke volume is severe ▪ Patients with a regurgitant fraction of more than 0.6 are considered to have severe mitral regurgitation. • Mitral Regurgitation Pathophysiology o Determinants of regurg ▪ Size of opening of mitral valve • Probably the first and most important determinant • The bigger the opening, the more blood that will backflow into the atrium ▪ Heart rate • The longer the patient is in systole, the more opportunity there is for regurgitation o If they are bradycardic, they have more risk for regurg than if they are tachycardic ▪ Pressure gradients across mitral valve • Left ventricular compliance o The greater the pressure gradient against forward flow, the more regurgitant flow that will occur • Afterload o If we increase SVR, we increase afterload, so more blood will go back into atrium than through the aorta. So we want to keep the afterload low. If it is high, the path of least resistance will be back into the atria. We want forward flow of blood, we don’t want it backing up, so we will keep SVR low (within reason) & avoid an increase in SVR. ▪ The fraction of left ventricular stroke volume that regurgitates into the left atrium depends on (1) the size of the mitral valve orifice; (2) heart rate, which determines the duration of ventricular ejection; and (3) pressure gradients across the mitral valve. • Such gradients are related to left ventricle compliance and impedance to left ventricular ejection into the aorta. • Pharmacologic interventions that increase or decrease systemic vascular resistance have a major impact on the regurgitant fraction in patients with mitral regurgitation. • Isolated Mitral Regurgitation o Can remain symptom free for many years ▪ LV enlarges & becomes more compliant • Because it is pumping that blood out again that it just tried to pump out the first time, so it is increasing the volume that the LV sees • Myocardial ischemia as a result of mitral regurgitation is uncommon, because the increased left ventricular wall tension is quickly dissipated as the stroke volume is rapidly ejected into the aorta and left atrium. When mitral regurgitation develops gradually, the volume overload produced by mitral regurgitation transforms the left ventricle into a larger, more compliant chamber that is able to deliver a larger stroke volume. This occurs through a dissolution of collagen weave, remodeling of the extracellular matrix, rearrangement of myocardial fibers, and addition of new sarcomeres with the development of ventricular hypertrophy. ▪ LA enlarges & becomes more compliant • Patients with isolated mitral regurgitation are less dependent on properly timed left atrial contraction for left ventricular filling than are patients with co-existing mitral or aortic stenosis. Patients with rheumatic fever–induced mitral regurgitation are most likely to exhibit marked left atrial enlargement and atrial fibrillation. o Alterations allow for accommodation of increased volume w/o increase in LA pressure ▪ LA & LV tend to become big & floppy. They do this because they are trying to accommodate for more volume, because instead of blood going forward through the aorta, it is kind of getting passed around through LV/RA (?) ▪ Development of ventricular hypertrophy and increased compliance of the left atrium permit the accommodation of the regurgitant volume without a major increase in left atrial pressure. This allows patients to maintain cardiac output and remain free of pulmonary congestion, and to be asymptomatic for many years. The combination of mitral regurgitation and mitral stenosis results in volume and pressure overload of the left atrium and a markedly increased left atrial pressure. Atrial fibrillation, pulmonary edema, and pulmonary hypertension develop much earlier in these patients than in those with isolated mitral regurgitation. o Eventually failure results if untreated o Acute onset results in pulmonary edema and/or cardiogenic shock ▪ Precipitous decrease in CO which can cause cardiogenic shock ▪ Both of these can kill you within 20 minutes ▪ Because there has been no time for development of left atrial or left ventricular compensation, acute mitral regurgitation presents as pulmonary edema and/or cardiogenic shock. • Ventricular Hypertrophy o Eccentric – seen with mitral regurg (see this in response to increase in volume. Becomes big & floppy to accommodate more volume). Eccentric hypertrophy seen on right of image below. ▪ Chamber volume increases ▪ Walls become thin ▪ Compliance increases ▪ Response to volume • You get big & floppy; dilated o Concentric ▪ Chamber decreases ▪ Walls thicken • Muscle gets thicker, causing the chamber size to get smaller. The volume of the chamber decrease. Because the muscle gets thicker, the compliance of the muscle decreases. This is a response to pressure. This is what you get with aortic stenosis. LV has to increase the pressure. If you increase the work the muscle does, the muscle gets bigger. We get concentric hypertrophy. Because it is bigger, it is less compliant. This is the response to an increase in pressure. ▪ Compliance decreases ▪ Response to pressure • You get thick & stiff; image in the middle (looks like letter “C” for concentric) • If you squeeze harder, you will get bigger muscles • Mitral Regurgitation Dx o Holosystolic apical murmur radiating to axilla ▪ …pushes blood back into the atrium. Will hear this all throughout systole. ▪ Mitral regurgitation is recognized clinically by the presence of a holosystolic apical murmur with radiation to the axilla. o Hypertrophy via CXR, ECG (as axis deviation), echo ▪ Cardiomegaly can also be detected on physical examination. Severe mitral regurgitation can produce left atrial and left ventricular hypertrophy detectable on ECG and chest radiograph. o Echo findings ▪ Regurgitant fraction • Mild 20% - 30% • Moderate 30% - 50% • Severe >55% • Percentage = percent of the stroke volume. It is what percent of the stroke volume is regurgitating back into the atrium. ▪ Echocardiography confirms the presence, severity, and often the cause of the mitral regurgitation. Left atrial size and pressure, left ventricular wall thickness, cavitary dimensions, ventricular function, and pulmonary artery pressure can be measured. In addition, the left atrial appendage can be evaluated for the presence of thrombus. Many methods exist to determine the severity of mitral regurgitation. These include color flow and pulsed wave Doppler echocardiographic examination of the mitral valve with calculation of regurgitant volume and regurgitant fraction and measurement of the area of the regurgitant jet. The presence of a V wave in a pulmonary artery occlusion pressure waveform reflects regurgitant flow through the mitral valve, and the size of this V wave correlates with the magnitude of the mitral regurgitation. ▪ If the severity of mitral regurgitation is in doubt or mitral valve surgery is planned, cardiac catheterization, including coronary angiography, is necessary. o Usually no angina unless they have CAD ▪ People who have concentric hypertrophy, because their cardiac muscle increases, often have angina even if they have no CAD. This is because they have more muscle, which increases O2 requirement. ▪ Mitral regurg = much less likely to have angina • Mitral Regurgitation Treatment o Valve repair better than replacement ▪ So you don’t mess with the contraction of the ventricle from the geometrical damage from surgical replacement o Better results if done before significant LV damage ▪ Unlike stenotic valve lesions, regurgitant cardiac valve lesions often progress insidiously, causing left ventricular damage and remodeling before symptoms have developed. Early surgery may be warranted to prevent left ventricular muscle dysfunction from becoming severe or irreversible. o Prognosis better if done before EF < 60% ▪ Survival may be prolonged if surgery is performed before the ejection fraction is less than 60% or before the left ventricle is unable to contract to an end-systolic dimension of 45 mm (normal <40 mm). Patients with an ejection fraction of less than 30% or a left ventricular end-systolic dimension of more than 55 mm do not experience improvement with mitral valve surgery. o Symptomatic patients should have repair even if EF is normal ▪ The problem is that it is insidious and occurs without you knowing it. Big sign is dyspnea. If found early, they will repair early as possible. You want to avoid changes in LV. Once changes in LV occur, LV is remodeled & becomes remodeled. You cannot repair these. ▪ Symptomatic patients should undergo mitral valve surgery even if the ejection fraction is normal. Mitral valve repair, if possible, is preferred to mitral valve replacement because it restores valve competence, maintains the functional aspects of the mitral valve apparatus, and avoids insertion of a prosthesis. The mitral valve apparatus is very important in supporting left ventricular function. The absence of the subvalvular apparatus causes distortion of left ventricular contractile geometry and impairment of left ventricular ejection. In patients in whom the valve and its apparatus cannot be preserved, valve replacement is done, but there is a postoperative decline in left ventricular ejection fraction. • Although vasodilators are useful in the medical management of acute mitral regurgitation, there is no apparent benefit to long-term use of these drugs in asymptomatic patients with chronic mitral regurgitation. For symptomatic patients, angiotensin-converting enzyme inhibitors or β-blockers (particularly carvedilol) and biventricular pacing have all been shown to decrease functional mitral regurgitation and improve symptoms and exercise tolerance. ▪ EARLIER IS BETTER • Anesthesia Management o Avoid ▪ Bradycardia (slightly increased HR is best) • More time for blood to regurg into the atrium • These patients are usually tachy in the 90s because this is their body’s adjustment, so keep them in this range. • Management of anesthesia for noncardiac surgery in patients with mitral regurgitation includes prevention and treatment of events that may further decrease cardiac output. The goal is to improve forward left ventricular stroke volume and decrease the regurgitant fraction. Maintenance of a normal to slightly increased heart rate is recommended. Bradycardia may result in severe left ventricular volume overload. ▪ Increased SVR/afterload (use nitroprusside) • Causes increased resistance to forward flow, increasing backflow of blood • Probably will be on CCB or hydralazine or something like that • Increases in systemic vascular resistance can also cause decompensation of the left ventricle. Afterload reduction with a vasodilator drug such as nitroprusside with or without an inotropic drug will improve left ventricular function. In most patients, cardiac output can be maintained or improved with modest increases in heart rate and modest decreases in systemic vascular resistance. The decrease in systemic vascular resistance caused by regional anesthesia may be beneficial in some patients. Preoperative sedation and anticholinergics are usually well tolerated. ▪ Cardiac depression • Bad. Avoid drug-induced myocardial depression. o Intraop monitoring with a TEE to track regurgitant flow ▪ Especially if you are using vasoactive drugs like Nipride to tweak CO. it would be really nice to have a TEE to track & titrate Nipride. ▪ Monitor the magnitude of regurgitant flow with a pulmonary artery catheter (size of the V wave) and/or echocardiography • Mitral Valve Prolapse o Prolapse of leaflet into LA during systole ▪ Mitral valve prolapse (MVP) is defined as the prolapse of one or both mitral leaflets into the left atrium during systole with or without mitral regurgitation. o Most common lesion 1% - 2.5% have mitral valve prolapse ▪ MVP is the most common form of valvular heart disease, affecting 1% to 2.5% of the U.S. population. o Isolated or w/regurg ▪ When mitral valves prolapse, can … back into the atrium ▪ With MVP people, it can be severe enough to cause regurg ▪ If severe, MVP can cause regurg o Female > males ▪ It is more common in young women. o Often a benign finding (causes no problems, completely benign, may hear murmur) ▪ Although it is usually a benign condition, MVP can have devastating complications such as cerebral embolic events, infective endocarditis, severe mitral regurgitation requiring surgery, dysrhythmias, and sudden death. Patients with MVP and abnormal mitral valve morphology appear to be the subset of patients at risk for these complications. o Managed like mitral regurg if regurg is present • Mitral Valve Prolapse o Associated with ▪ Marfan syndrome (creates problems with collagen, like Lupus) ▪ Rheumatic fever ▪ Myocarditis ▪ Lupus ▪ MVP can be associated with Marfan's syndrome, rheumatic carditis, myocarditis, thyrotoxicosis, and systemic lupus erythematosus. ▪ These are diseases related to collagen problems ▪ People with these diseases have problems with valves o Midsystolic click and late systolic murmur – if regurg is present ▪ Will hear midsystolic click which is the leaflet popping back into atrium ▪ If regurg is present, will hear late systolic murmur ▪ You won’t hear it until ventricles are about halfway through systole, then you will hear click ▪ It is associated with the auscultatory findings of a midsystolic click and a late systolic murmur. • Aortic Stenosis o Increasingly common as population ages ▪ Aortic stenosis is a common valvular lesion in the United States, and its incidence is increasing as the U.S. population grows older. ▪ Stenosis is when the valvular open starts to open, gets stenotic ▪ One of the primary risk factors is an increase in age ▪ As general population increases in age, you will see more people with aortic stenosis ▪ If you have a problem with valve opening, you will probably have problem closing & will have some degree of regurg o Risk factors ▪ Calcification of valve leaflets • Calcification associated with increase in age • Two factors are associated with development of aortic stenosis. • The first is degeneration and calcification of the aortic leaflets and subsequent stenosis. o This is a process of aging. ▪ Bicuspid aortic valve • The second factor is the presence of a bicuspid rather that a tricuspid aortic valve. • Aortic stenosis develops earlier in life (30 to 50 years of age) in individuals with a bicuspid aortic valve than in those with a tricuspid aortic valve (60 to 80 years of age). o Risk factors the same as with CAD ▪ Since the initial study by Goldman and colleagues in 1977 showing that patients with aortic stenosis had an increased risk of perioperative cardiac complications, many studies have demonstrated that patients with aortic stenosis have an increased risk of perioperative mortality and of nonfatal myocardial infarction regardless of the presence or absence of risk factors for coronary artery disease. The perioperative risk attributable to aortic stenosis is independent of the risk attributable to coronary artery disease. o Almost always occurs with aortic regurg ▪ Aortic stenosis is almost always associated with some degree of aortic regurgitation. o Other causes include rheumatic heart disease and infective endocarditis. Aortic stenosis is associated with risk factors similar to those of ischemic heart disease, such as systemic hypertension and hypercholesterolemia. • Bicuspid Aortic Valve o Most people have 3 leaflets to an aortic valve (tricuspid), so there is a bigger opening o Some people only have bicuspid (only have 2 leaflets) o 2 of the leaflets are joined o These people will have a smaller, stenotic opening if everything else is the same o This is not a rare finding • Aortic Stenosis Pathophysiology o Diminished blood flow from LV into aorta during systole ▪ Decreased blood flow from LV into aorta during systole ▪ The ventricle overcomes this because if we have increasing resistance & want to have same flow, we must increase pressure ▪ This increases workload of heart, which increases muscle mass (concentric hypertrophy) ▪ Obstruction to ejection of blood into the aorta caused by a decrease in the aortic valve area necessitates an increase in left ventricular pressure to maintain stroke volume. The normal aortic valve area is 2.5 to 3.5 cm2. Transvalvular pressure gradients higher than 50 mm Hg and an aortic valve area of less than 0.8 cm2 are characteristic of severe aortic stenosis. o Causes increased LV pressure ▪ Concentric Hypertrophy • Muscle itself increases in thickness, volume of chamber decreases, compartment itself decreases compliance (gets stiffer)…leading to a whole different type of CHF we will talk about later • Because there is stenotic opening, there is a point in which an increase in pressure doesn’t cause an increase in flow. There is a limit in which the heart can pump & it is also time limited • You tend to have a fixed CO or a CO that is not as dynamic as it would be with another heart • If you’re exercising & have stenotic aortic valve, you may be able to increase CO to a degree, but at some point, you’re not going to be able to increase CO by increasing SV because you will have reached a limit where the heart can’t pump anymore or can’t pump as effectively & get enough of the SV out. So these people tend to have fixed CO • Angina pectoris may occur in patients with aortic stenosis despite the absence of coronary disease. This is due to an increase in myocardial oxygen requirements because of concentric left ventricular hypertrophy and the increase in myocardial work necessary to offset the afterload produced by the stenotic valve. In addition, myocardial oxygen delivery is decreased because of the compression of subendocardial blood vessels by the increased left ventricular pressure. ▪ Decreased compliance o Ischemia secondary to ▪ Increased myocardial mass • If have CAD, then they really have a high incidence of ischemia • Even if clear coronaries, they still have a risk of ischemia because there is more heart muscle with hypertrophy, increasing demand/work ▪ Increased work required • Increased work, so we are asking muscle to pump harder, thus increasing demand ▪ Decreased subendocardial blood flow • During contraction of LV, blood flow tends to be decreased. The higher the wall tension is created, the more decreased the blood flow is. The increase in pumping requirement & muscle mass increases mass which decreases blood flow. Increasing demand by making it work harder, but decreasing blood flow as we are increasing blood flow. So these people are very prone to developing ischemia & angina whether they have CAD or not o Syncope (exercise induced drop in SVR) o CHF ▪ Especially when associated with exercise or sympathetic stimulation, but usually exercise ▪ When exercising you vasodilate skeletal muscles to get more blood to them, but if you have a fixed CO, you cannot pump harder, so you vasodilate but won’t be able to pump more blood because you have a fixed CO because of stenotic valve, so you have a decreased SVR which will eventually lead to a decrease in VR, which will lead to a decrease in CO, decreasing perfusion to the brain, causing you to pass out during a syncopal episode ▪ The origin of syncope in patients with aortic stenosis is controversial but may reflect an exercise- induced decrease in systemic vascular resistance that remains uncompensated because cardiac output is limited by the stenotic valve. ▪ LV will eventually give out, causing CHF ▪ Will talk about diastolic HF next week, which is caused by a filling problem, not necessarily a pumping problem ▪ Ventricle gets so thick/stiff that it cannot fill with enough blood & starts to fail ▪ CHF can be due to systolic and/or diastolic dysfunction. • Aortic Stenosis Pathophysiology o MTPG – amount filled from one valve to another to generate flow o “Know the severe. So when you get less than .8, you start having severe. If TVP gets above 50, you start having problems bc this is severe AS.” o Second pic ▪ Stenotic valve which limits outflow, causing increased LV systolic pressure, causing concentric hypertrophy with increased mass, causing LV failure (muscle gets thick, chamber gets smaller, compliance decreases, getting stiff) ▪ Also creates increased LV ejection time. The ventricle, bc it has to pump through a limited amount of space or limited opening, it takes longer to pump, so you have an increase in LV ejection time, so basically an increase in systole. ▪ Increase in LV systolic pressure leads to an increase in myocardial O2 consumption (increase in demand) ▪ LVET also means if you are demanding more time for systole, you leave less time for diastole (diastole creates coronary perfusion). Increase in LVET increases consumption & decreases supply ▪ Increase in LVDP leads to a decrease in myocardial O2 supply (because of the pressure across the wall/the wall tension pressure) ▪ Decrease in aortic pressure because you’re pumping less blood into aorta bc the ventricle can’t get blood through aortic valve, so less blood decreases pressure. Aortic pressure is what drives coronary artery perfusion (they come off right after aortic valve at base of aorta), so pressure in aorta is what pushes blood through the coronary arteries. So if we decrease that pressure, we decrease pressure perfusing coronaries, which decrease perfusion of myocardium ▪ All lead to decrease in myocardial O2 supply, leading to ischemia & LV failure ▪ Hypertrophy is a compensatory mechanism, but if problem is not corrected then the LV will fail and you will get HF • Aortic Stenosis Dx o Crescendo-decrescendo systolic murmur o Systolic murmur over aorta radiating to neck ▪ Characteristic noises caused by plaque in carotids (bruit) ▪ Sometimes bruits can be confused with this aortic systolic murmur. So if you hear something in neck, could be bruit due to clogged carotids or could be AS ▪ On physical examination, auscultation reveals a characteristic systolic murmur heard best in the aortic area. This murmur may radiate to the neck and mimic a carotid bruit. Because patients with aortic stenosis frequently have concomitant carotid artery disease, this finding deserves special attention. Because many patients with aortic stenosis are asymptomatic, it is important to listen for the systolic murmur of aortic stenosis in older patients scheduled for surgery. o Typical progression of S&S ▪ Angina – 5 yrs to death ▪ Syncope – 3 yrs to death ▪ DOE/CHF – 2 yrs to death • Unless there is a correction made o CXR o ECG ▪ The classic clinical symptoms of critical aortic stenosis are angina pectoris, syncope, and dyspnea on exertion, a manifestation of CHF. The onset of these symptoms has been shown to correlate with an average time to death of 5, 3, and 2 years, respectively. About 75% of symptomatic patients will die within 3 years if they do not have a valve replacement. ▪ Will see LV hypertrophy ▪ Chest radiography may show a prominent ascending aorta due to poststenotic aortic dilation. The ECG may demonstrate left ventricular hypertrophy. ▪ L axis deviation (that is pretty diagnostic) ▪ Exercise stress testing may be an additional strategy to evaluate asymptomatic patients with moderate to severe aortic stenosis to identify those with poor exercise tolerance and/or an abnormal blood pressure response to exercise. Patients with exercise-induced symptoms might benefit from aortic valve replacement. o Echo findings ▪ Can look and see if you have bicuspid or tricuspid valve ▪ Can estimate pressures across valve ▪ Can estimate valve opening size ▪ Can look at EFs ▪ Can do serial monitoring of progression of disease ▪ Echocardiography with Doppler examination of the aortic valve provides a more accurate assessment of the severity of aortic stenosis than does clinical evaluation, and patients can be followed echocardiographically to assess the progression of their disease. Findings include identification of a trileaflet versus a bileaflet aortic valve, thickening and calcification of the aortic valve, decreased mobility of the aortic valve leaflets, left ventricular hypertrophy, and left ventricular systolic or diastolic dysfunction. Aortic valve area and transvalvular pressure gradients can be measured. ▪ Cardiac catheterization (and coronary angiography) may be necessary when the severity of aortic stenosis cannot be determined by echocardiography. • Aortic Stenosis Treatment o Asymptomatic patients are medically managed ▪ In asymptomatic patients with aortic stenosis, it appears to be safe to continue medical management and to delay valve replacement surgery until symptoms develop. However, there is a small risk of sudden death or rapid progression of symptoms and then sudden death. o Symptomatic patients require repair ▪ Once you start developing symptoms (first symptom is usually angina), then they will start doing repair ▪ Mortality approaches 75% within 3 years after development of critical aortic stenosis unless the aortic valve is replaced. Even though most patients with aortic stenosis are elderly, the risks of valve replacement surgery are acceptable unless there are also serious comorbid diseases that can worsen outcome. o Repair improves LV EF & reduces S&S ▪ Aortic valve replacement relieves the symptoms of aortic stenosis dramatically, and the ejection fraction usually increases. o Repair often combined with CABG when patient also has CAD ▪ Especially if pt is older, they will have CABG AVR (CABG & valve repair done at same time) ▪ Coronary revascularization is often done at the time of aortic valve replacement in patients with both aortic stenosis and coronary artery disease. ▪ Percutaneous aortic balloon valvotomy has been shown to be beneficial in adolescents and young adults with congenital or rheumatic aortic stenosis. However, adults with acquired aortic stenosis experience only temporary relief of symptoms with this procedure. Balloon valvotomy may occasionally be useful for palliation of aortic stenosis in patients who are not candidates for aortic valve replacement. • Anesthetic Management o Patients with aortic stenosis coming for noncardiac surgery are at high risk of major perioperative cardiac complications, and the risk of these complications increases with the complexity of the surgery. Hence, it is important to ascertain the severity of the aortic stenosis preoperatively. Management of anesthesia in patients with aortic stenosis includes the prevention of hypotension and any hemodynamic change that will decrease cardiac output. o Maintain NSR ▪ Outward pumping problem but also filling problem due to concentric hypertrophy ▪ Maintain NSR to maintain atrial kick, which is very important for these people in filling ▪ Cannot sustain a-fib ▪ Normal sinus rhythm must be maintained, because the left ventricle is dependent on a properly timed atrial contraction to produce an optimal left ventricular end-diastolic volume. Loss of atrial contraction, as during junctional rhythm or atrial fibrillation, may produce a dramatic decrease in stroke volume and blood pressure. o Maintain normal heart rate ▪ Avoid tachycardia – less time for filling & emptying of forward flow • Not too fast, not too slow • Normal = their normal, what they came in with • The heart rate is important because it determines the time available for ventricular filling, for ejection of the stroke volume, and for coronary perfusion. A sustained increase in heart rate decreases the time for left ventricular filling and ejection and reduces cardiac output. ▪ Avoid bradycardia – overdistension of LV • This can cause pulmonary edema & CHF • A decrease in heart rate can cause overdistention of the left ventricle. o Avoid hypotension ▪ Decreases coronary blood flow • Will decrease coronary O2 supply ▪ Reflex tachycardia • We want to avoid tachycardia ▪ Hypotension reduces coronary blood flow and results in myocardial ischemia and further deterioration in left ventricular function and cardiac output. Aggressive treatment of hypotension is mandatory to prevent cardiogenic shock and/or cardiac arrest. o Optimize fluids ▪ Promotes adequate LV filling • Not too little, not too much • Want to optimize fluids to promote LV filling ▪ Optimize intravascular fluid volume to maintain venous return and left ventricular filling o CPR is ineffective ▪ Because of the stenotic valve; prevents forward flow with CPR. Resistance cannot be overcome ▪ Cardiopulmonary resuscitation is not effective in patients with aortic stenosis because it is difficult, if not impossible, to create an adequate stroke volume across a stenotic aortic valve with cardiac compression. • Aortic Regurgitation o Retrograde flow due to failure of aortic leaflets to close properly ▪ Aortic regurgitation results from failure of aortic leaflet coaptation caused by disease of the aortic leaflets or of the aortic root. ▪ Problem with leaflets of aortic valve. Leaflet problem usually has something to do with something getting on valve & preventing it from closing properly. • Infective endocarditis o This is like getting algae on your valves. The algae junk can break off, become embolism & go to brain. Also prevents valve from closing properly & creates regurg. • Rheumatic fever • Bicuspid valve o Don’t close like they are supposed to • Anorexigenic drugs • Common causes of leaflet abnormalities are infective endocarditis, rheumatic fever, bicuspid aortic valve, and the use of anorexigenic drugs. ▪ Problem with aortic root (where the aorta and LV meet and where these leaflets attach to) • Aortic dissection o Aortic roots = where leaflets, aorta, LV come together o Dissection is bad, usually life threatening • Rheumatoid arthritis o Collagen problems. Cause weakening of aortic root & increase risk of dissection • Marfan syndrome o Will usually have aortic valve repairs • Abnormalities of the aortic root causing aortic regurgitation include idiopathic aortic root dilation, hypertension-induced aortoannular ectasia, aortic dissection, syphilitic aortitis, Marfan's syndrome, Ehlers-Danlos syndrome, rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. Acute aortic regurgitation is usually the result of endocarditis or aortic dissection. • Aortic Regurgitation Pathophysiology o Decrease in CO due to backflow of blood from aorta into LV during diastole ▪ The basic hemodynamic derangement in aortic regurgitation is a decrease in cardiac output because of regurgitation of a part of the ejected stroke volume from the aorta back into the left ventricle during diastole. o Results in a volume & pressure overload of LV ▪ This results in a combined pressure and volume overload on the left ventricle. o “Pure” regurg causes LV ▪ Eccentric hypertrophy • Usually if you have pure regurg, it will cause eccentric hypertrophy • This is when you have regurg without stenosis • The LV will expand by the ventricle wall thinning, then it will get floppy. This is the ventricles response to compensating for the increase in volume that it keeps seeing • If this happens chronically, you can get big floppy ventricle that is asymptomatic for a while • With aortic regurgitation, the entire stroke volume is ejected into the aorta. Because the pulse pressure is proportional to the stroke volume and aortic elastance, the increased stroke volume increases systolic pressure, and systolic hypertension increases afterload. • The left ventricle compensates by developing hypertrophy and enlarging to accommodate the volume overload. Because of the increased oxygen requirements necessitated by left ventricular hypertrophy and the decrease in aortic diastolic pressure, which reduces coronary blood flow, angina pectoris may occur in the absence of coronary artery disease. ▪ Dilation o Acute AR is life threatening ▪ Usually associated with dissection. This drops your CO acutely & most people do not survive this ▪ The left ventricle can usually tolerate the chronic volume overload. However, if left ventricular failure occurs, left ventricular end-diastolic volume increases dramatically and pulmonary edema develops. ▪ Compared to patients with chronic aortic regurgitation, patients with acute aortic regurgitation experience severe volume overload in a ventricle that has not had time to compensate. This typically results in coronary ischemia, rapid deterioration in left ventricular function, and heart failure. • Aortic Regurgitation Pathophysiology o Regurgitant flow depends on ▪ Time available for blood flow • The more time you have during diastole, the more regurg you will have ▪ Pressure gradients • The higher the SVR, the more regurg you will have ▪ The magnitude of the regurgitant volume depends on (1) the time available for the regurgitant flow to occur, which is determined by the heart rate; and (2) the pressure gradient across the aortic valve, which is dependent on the systemic vascular resistance. o Regurgitant flow decreased by ▪ Tachycardia • There is a limit to tachycardia. Would rather have them faster than slower ▪ Decreased SVR • Don’t want to decrease it too much, but would rather have lower SVR than higher SVR ▪ The magnitude of aortic regurgitation is decreased by tachycardia and peripheral vasodilation. o Widened pulse pressures ▪ Increased stroke volume = increased SBP • Widened PP • LV pumping really hard to get extra blood out ▪ Decreased aortic diastolic pressure • Will be very low because the blood that the ventricle just pumped out is being sent back into ventricle instead of pumping forward o Graph ▪ Increase LV volume, increases LV mass, causes LV dysfunction, which leads to LV failure ▪ Increased SV, increased systolic pressure, causing LV dysfunction & increased myocardial O2 demand, increase in LVET ▪ Decrease in aortic diastolic pressure (this is what is perfusing coronary arteries), causes a decrease in myocardial O2 supply ▪ Increased LVET decreases diastolic time, decreasing myocardial supply ▪ Decreased ESV decreases O2 supply ▪ This will all lead to ischemia & failure ▪ Increase in LVEDP which means you’ve got blood accumulating into LV (?) which will back up into atria, then lungs, causing edema • Aortic Regurgitation Dx o Echo findings ▪ Ejection fraction (<55%) • This is concerning • A helpful indicator of left ventricular function in the presence of aortic regurgitation is the echocardiographically determined end-systolic volume and ejection fraction, both of which remain normal until left ventricular function becomes impaired. Indeed, surgery is recommended before the ejection fraction decreases to less than 55% and left ventricular end-systolic volume increases to more than 55 mL. ▪ LV end-systolic volume (>55 ml) • These numbers are trigger points. When you reach these, something needs to be done o Diastolic murmur along L sternal boarder ▪ Aortic regurgitation is recognized clinically by its characteristic diastolic murmur, heard best along the right sternal border, and peripheral signs of a hyperdynamic circulation, including a widened pulse pressure, decreased diastolic blood pressure, and bounding pulses. ▪ In addition to the typical murmur of aortic regurgitation, there may be a low-pitched diastolic rumble (Austin-Flint murmur) that results from fluttering of the mitral valve caused by the regurgitant jet. o Wide pulse pressures ▪ Bounding pulses (can be felt clinically in someone you wouldn’t expect bounding pulses; like at rest) o Decreased diastolic pressure o As with mitral regurgitation, symptoms of aortic regurgitation may not appear until left ventricular dysfunction is present. Symptoms at this stage are manifestations of left ventricular failure (dyspnea, orthopnea, fatigue) and coronary ischemia. With chronic aortic regurgitation, evidence of left ventricular enlargement and left ventricular hypertrophy may be seen on the chest radiograph and ECG. Echocardiography will reveal any anatomic abnormalities of the aortic valve, including leaflet perforation or prolapse, and will identify any abnormalities in the aortic root and aortic annulus. Left ventricular size, volume, and ejection fraction can be measured, and Doppler examination can be used to identify the presence and severity of aortic regurgitation. Many methods exist to quantify aortic regurgitation. These include regurgitant jet width as a percentage of overall left ventricular outflow tract width, pressure half- time, and diastolic flow reversal in the descending aorta. Cardiac catheterization and cardiac magnetic resonance imaging may be useful for grading aortic regurgitation if echocardiography is insufficient. • Aortic Regurgitation Treatment o Replacement before LV damage even if asymptomatic ▪ Ejection fraction (<55%) ▪ LV end-systolic volume (>55 ml) ▪ Goal here is to fix it early ▪ Will have valve replacement even if asymptomatic. This is opposed to aortic stenosis, where you are medically managed until you start getting symptomatic. With aortic regurg, want to prevent eccentric hypertrophy so will repair immediately ▪ Surgical replacement of a diseased aortic valve is recommended before the onset of permanent left ventricular dysfunction, even if patients are asymptomatic. ▪ The operative mortality for isolated aortic valve replacement is approximately 4%. It is higher if there is concomitant aortic root replacement or coronary artery bypass grafting or if there are substantial comorbidities. The mortality rate of asymptomatic patients with normal left ventricular size and function is less than 0.2% per year. In contrast, symptomatic patients have a mortality rate greater than 10% per year. o Acute AR requires immediate surgery ▪ In acute aortic regurgitation, immediate surgical intervention is necessary, because the acute volume overload results in heart failure. ▪ Alternatives to aortic valve replacement with a prosthetic valve include a pulmonic valve autograft (Ross procedure) and aortic valve reconstruction. o Medical management focused on ▪ Decrease systolic hypertension (Nipride) • This will decrease SVR ▪ Improved LV function (dobutamine) ▪ Medical treatment of aortic regurgitation is designed to decrease systolic hypertension and left ventricular wall stress and improve left ventricular function. • Intravenous infusion of a vasodilator such as nitroprusside and an inotropic drug such as dobutamine may be useful for improving left ventricular stroke volume and reducing regurgitant volume. • Long-term therapy with nifedipine or hydralazine can be beneficial and may delay the need for surgery in asymptomatic patients with good left ventricular function. • Anesthesia Management o Avoid ▪ Bradycardia (keep HR > 80 BPM) • The longer they are in diastole, the more regurg will be • Management of anesthesia for noncardiac surgery in patients with aortic regurgitation is designed to maintain forward left ventricular stroke volume. • The heart rate must be kept above 80 beats per minute because bradycardia, by increasing the duration of diastole and thereby the time for regurgitation, produces acute left ventricular volume overload. ▪ Increased SVR • Increased afterload promotes regurg • An abrupt increase in systemic vascular resistance can also precipitate left ventricular failure. ▪ Myocardial depression • Don’t want to depress heart more because it is already working as hard as it can • The compensations for aortic regurgitation may be tenuous, and anesthetic-induced myocardial depression may upset this delicate balance. • If left ventricular failure occurs, it is treated with a vasodilator to reduce afterload and an inotrope to increase contractility. • Overall, modest increases in heart rate and modest decreases in systemic vascular resistance are reasonable hemodynamic goals during anesthesia. General anesthesia is the usual choice for patients with aortic regurgitation. • New Frontiers o The big thing in valvular disorders is to be able to do this percutaneously o Just like doing a cath, they will come through fem artery or straight through apex of heart, feed it into LV, then deploy a valve without ever having to open pt. Less traumatic than having to do sternal incision, open heart up, having to put them on bypass for 3-4 hours. More common to do aortic than mitral valve. o http:// www.nejm.org/ doi/ full/ 10.1056/ NEJMoa1008232. [Show More]
Last updated: 2 years ago
Preview 1 out of 35 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Oct 21, 2021
Number of pages
35
Written in
Additional information
This document has been written for:
Uploaded
Oct 21, 2021
Downloads
0
Views
105


.png)