NR 511 Week 1 Notes:
Reading: Chapters 4, 5 and 80 (1327-1341)
Looking back on your first practicum week and classroom work, ask yourself the following:
• Do I understand what a differential diagnosis is?
• Do I kn
...
NR 511 Week 1 Notes:
Reading: Chapters 4, 5 and 80 (1327-1341)
Looking back on your first practicum week and classroom work, ask yourself the following:
• Do I understand what a differential diagnosis is?
• Do I know the difference between subjective and objective data?
• Can I identify the CC and HPI for a patient encounter and incorporate review of systems and physical exam findings to develop a differential?
Chapter 4: pg. 39-57
Circle of Caring Modeling – provides a framework for advanced nursing practice – nursing origin approach with aspects of traditional medical model
• Incorporates patient experience, context of experience, and environment of care
• Traditional modes of medical practice (history taking, physical assessment data, labs, functional measures, pharmacological)
• Nursing perspective (holistic measures, functional health patterns)
• Data collection process leads to a) medical diagnoses as listed by International Classification of Disease 10th E and b) NANDA nursing diagnoses and human response to diagnosis (prevention
and wellness)
• Includes elements from medical realm and expanded nursing base
Purpose and Goal of Diagnostic Reasoning pg. 40
• Solve a physical problem
• Health promotion
• Disease prevention
• Screening for high risk problems (using appropriate guidelines)
• Utilize motivational interviewing techniques
• Uncover “true concern”
• Influence behavioral change
Unique Aspects of Primary Care
• Different from acute care (presenting complaints, presentation of chronic illness)
• Problem solving, symptom management, screening for problems undetected, supporting health promotion, disease prevention, injury prevention, behavioral changes, patient education,
treatment options, health literacy considerations
• Patients and their families are the ones that will carry out the care (versus inpatient)
Nursing and the Medical Model
• Nursing – consideration of individual and family responses to actual or potential threats to health, helping patients cope with disease processes, anticipates human distress, works on the level of what an illness experience means to the patient
• Medical – new diagnostic reasoning possibilities, new treatment options for specific problems
• NP designs a treatment or health promotion plan - patients are actively involved in their own care
Patient-Advanced Practice Nurse Linkage Model
• Clinical judgement – happens in a dialogue with the patient (not in the NP mind alone)
• Effective and satisfactory encounters require quality communication and agreement about what the encounter is meant to accomplish (common goals, understand the patient’s goal for the
encounter)
• This model includes interactions between patient factors, nurse factors, and context
• Patient Factors – symptom experience, resources, supports, commitments/obligations, personal history, attention, goals
• Nurse Factors – Knowledge (human development, disease trajectory, family dynamics, psychological theory, spirituality, experience), Skill (interviewing, physical exam, teaching, counseling), Attitude (Openness, courage, persistence, honesty, respect, confidence, humility, attention, presence)
• Context – Purpose of the visit, time constraints, resource constraints
• Johnson’s phases of encounter – establishing agenda, elicit information from the patient, include being alert to cues and helping to problem solve, conduct physical exam, attend to comfort level,
preparing and informing, developing a plan of care and using a teachable moment (patient centered teaching)
• NP personalizes solutions-based o knowing the patient
• NP’s communication style is biopsychosocial or biomedical
• Biopsychosocial – higher patient satisfaction and better adherence to treatment plan
Clinical Process – Limitations: Human Memory Limitations
• Information process model – used to understand diagnostic reasoning – comprised of short (7 bits of data at a time, holds new pieces of info and elements of patient history and physical data) and long term memory (unlimited, ability to retrieve a fact depends on frequency with which fact is brought forward to use and on organizational structure like body systems and functional health patterns systems of data organization)
• Information processing model leaves out human experience (emotional responses, interactions,
empathize, being invested in patients)
Critical Thinking pg. 42
• Critical thinking – reflective thinking – process involves questioning ones thinking to determine whether all possible avenues have been explored and whether the conclusions are being drawn based on evidence
• Supports clinical judgement – humility in thought processes (know that even experienced thinkers can make mistakes)
• Systematic way of generating creative ways of thinking about problems
• Returns one to an examination of the strength of evidence for a given conclusion (hard evidence i.e. labs, plus subjective impressions, subjective information, etc.)
• Creativity in developing potential problem lists
• Includes systematic thinking that evaluates each new piece of data as it either supports some diagnostic hypotheses or reduces the likelihood of others
Intuition pg.43
• Develops with experience – long experience in that particular setting, based on unconscious thought that is probably an exquisite matching machine
• Characterizes expert practice but is not a goal in and of itself (ability to reflect on one’s thinking processes opens the process to analysis, sharing, and improvement
Developing Expertise
• Practicums help gain skill to graduate at advanced beginner level
• Table 4.1 pg. 43
• Novice – rule-based actions, unaware of context
• Advanced beginner – sensitive to aspects of the situation, able to formulate principles, needs help setting priorities
• Competent – goal-directed actions, feeling of mastery based on experience, deliberate planning
• Proficient – sees situation as a whole, immediate grasp of meaning, recognizes patterns of normalcy or aberrance, uses maxims to guide action
• Expert – transcends rules, intuitive grasp of the wholeness of situation, creative response to particularities of situation, flexible response to situations
Diagnostic Process Overview
• Diagnostic Process: a) collecting data from variety of sources (H&P, diagnostics) generating a working hypothesis about the cause of patient’s signs and symptoms
• Uses probabilistic reasoning, pattern matching, planning, problem solving, critical reflection
• Described by steps in nursing process or clinical reasoning process
• Expert clinicians – generate a list of possible diagnoses early in the encounter (include patient’s age, demographics, and risk factors)
• Data acquisition during H&P is best if hypothesis driven (information is selected and gathered that is related to list of potential diagnoses)
• Novice = “shotgun” approach – ask a little about everything that might be possible without considering which diagnoses are most likely
• Hypothesis driven data – data would confirm or disprove a specific hypothesis and is specifically sought and recorded
• Competing hypotheses must be ruled out by seeking nonconfirmatory data
• Priority list of hypotheses is subject to change
• Careful not to have completely symptom driven data collection or will leave out important concepts (such as health promotion)
• Data clusters “chunks”: May recognize that pieces are missing, do not fit, or are not right with hypothesis
• Do not ignore discrepant data
• Persistence in finding all pieces of data for a coherent picture
• “we see what we expect to see”
• Maxim of practice: “Common things occur commonly” – think horses, not zebras- mostly encounter most common diagnoses, not rare ones (still can include them in problem list but
consider lower probability)
• Be on alert for most serious conditions (abdominal pain – ruptured ectopic preg, AAA, ruptured appendix versus gas)
• Must obtain data to rule out life threatening / serious conditions
• Cluster related problems together (diagnoses that frequently occur together such as DM, obesity, HTN, hyperlipidemia) – lifestyle recs are usually the same, meds may differ: Approach
the core diagnosis – this may alleviate the other issues (addressing the underlying/core problem resolves the associated problems)
• Table 4.2 pg. 44 – Habits that support clinical judgement: data acquisition (use systematic or
hierarchically organized approach, general to specific, review multiple systems), hypothesis formulation (generate early in encounter, develop competing hypotheses, consider life or function threatening problems, consider rare diagnoses but label as rare), hypothesis evaluation (recognize interrelation of diagnoses, consider probabilities in context, consider likelihood of altering course of problem with treatment, rule out life or function threatening problems), problem naming (choose most fundamental problem and include multiple perspectives of biopsychosocial, spiritual, medical, nursing, include illness prevention and health promotion), goal setting (include patient in goal setting, make goals explicit and realistic), therapeutic option consideration (include modalities from multiple paradigms, consider patient preferences, consider context and cost in economic and human terms), evaluation (plan for follow up visit or phone call, consider symptom or treatment logs or diaries, measure and document the outcome of your practice for the individual, report effectiveness of your practice in the aggregate)
• Table 4.3 pg. 45: Errors in Diagnostic Reasoning: data collection (not obtaining all relevant clues,
misjudging important clues, overemphasizing clues that favor top hypotheses, forgetting that some data are unreliable, ignoring pertinent negative findings), hypothesis (not generating enough competing hypotheses, oversimplifying, not generating hypotheses early, not including the correct diagnosis on hypothesis list, failing to revise hypothesis list aka “premature closure”, selecting “favorite” hypotheses, generating too many hypotheses and “getting lost”, overestimating low probability hypotheses, underestimating high probability situations
• New hypotheses rarely emerge during physical exam unless patient can not see and causes no
symptoms (i.e., skin lesion) – usually PE is problem focused to rule In or rule out competing diagnoses
• Reach a working diagnosis
• Discuss management plan with patient - goals, guidelines according to EBP, realistic plans – always include follow up in treatment plans
• Physical Exam – verify hypotheses, screen out unlikely alternative diagnoses
Elements of the Diagnostic Process:
• History of Present Illness: taking history is first step in diagnostic reasoning process (for episodic care this is the chief complaint and HPI) – elicit the patient’s story and what does the patient think may be wrong
• HPI is NOT used for periodic screening, establishing care, or to follow up on an existing problem
• “What is the most important issue for us to deal with today” especially if long list of complaints – schedule follow up for additional issues to be addressed
• HPI – OLDCARTS
• PMH – refines hypothesis list, rules in or out hypothesis, identifies risk factors: childhood / other illnesses, hospitalizations, surgical history, trauma, pregnancies, psychiatric diagnoses, travel,
medications, immunization status, allergies (vs adverse effect), health maintenance practice / risk reduction
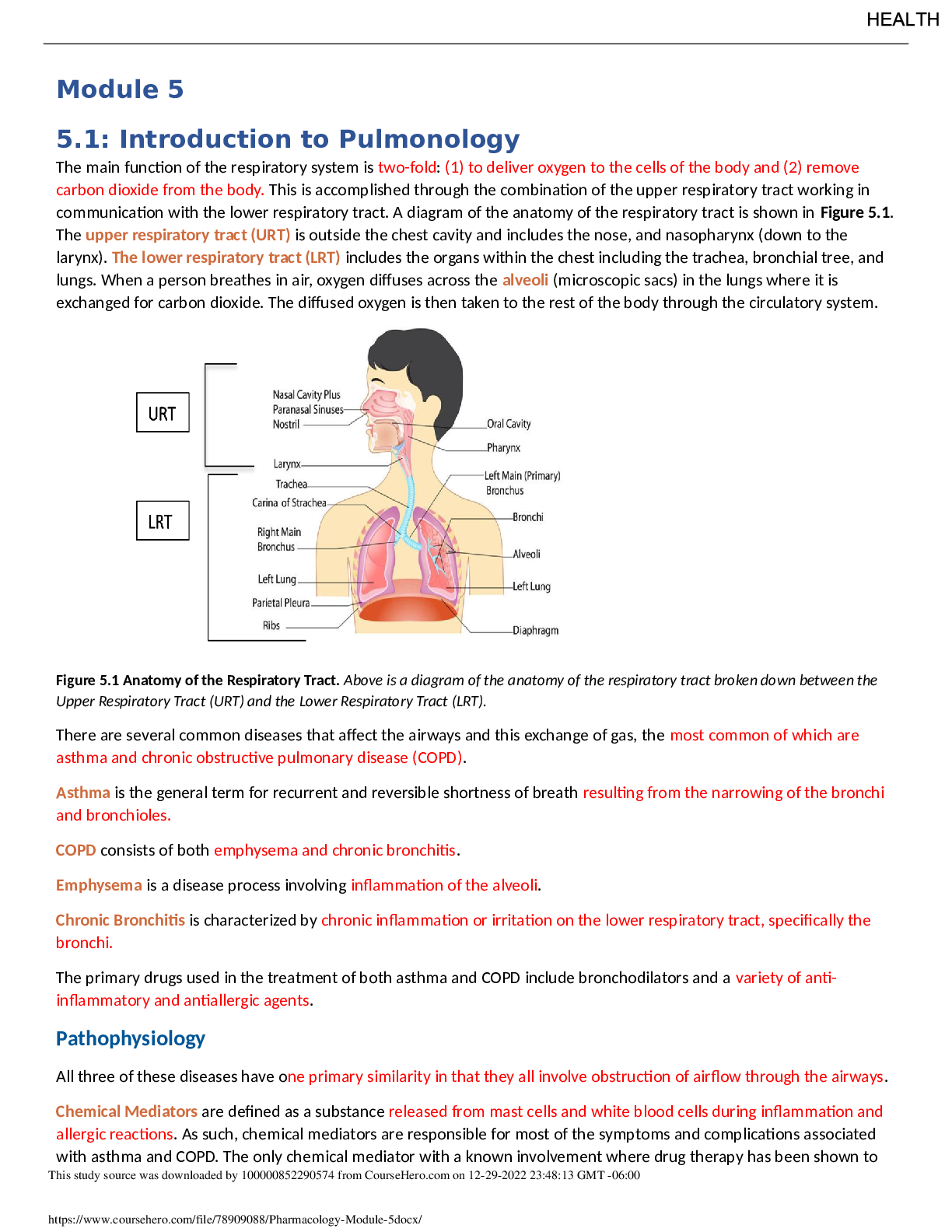
• FH – risk factors identification. Draw a genogram (see pg. 47 Figure 4.2) or list major diseases
(diabetes, heart disease, arthritis, psychiatric problems, alcoholism, cancer)
• SH- work patterns (ask about work if retired due to exposure), alcohol, tobacco, drugs (medical) and hobbies, resources activity level (nursing) – can record full functional health pattern info here
• ROS – subjective data, organized by body system
• Functional Health Patterns (by Marjory Gordon) – a database for determining nursing diagnoses
– enhanced ability to influence lifestyle changes and offer support and coping with diagnoses – reflects a nursing approach. Sleep/Rest, Activity/Exercise, Nutrition and how it is affected by illness. Inability to carry out any normal, day to day function is a RED FLAG that a potentially serious disease process may be developing - purpose Is to determine the extent of the illness effects on the ability to live their “normal” life. Accommodations needed, even short term?
See page 48
o Health Perception
o Health Management
o Nutrition / Metabolic
o Elimination
o Activity / Exercise
o Sleep / Rest
o Cognitive / Perceptual Concept (hearing, vision, memory, learning, pain/discomfort)
o Self-perception / Self-Concept (describe self, self-confidence, angry or depressed)
o Role relationship / self-perception / self-concept (who lives with you, friends, work, responsibilities)
o Sexuality / Reproductive / Role Relationship (changes, safe sex, birth control)
o Coping / stress tolerance (support friend, coping, turn to alcohol/drugs)
o Value / belief (religious, priorities, HCPOA or living will)
Physical Exam pg.49
• Clarifies diagnostic hypothesis and detects unanticipated problems of which the patient is unaware
• Head to toe if comprehensive
• Body systems may be tailored to working hypothesis list
Diagnostic Tests
• Confirm or Rule out diagnostic hypotheses
• Screening (lead poisoning in children)
• Usefulness depends on specificity, sensitivity, and predictive value
• Prevalence - # of cases present in a given population at a particular point in time
• Incidence – total # of cases in a specific time period
• # of cases of flu in a year (incidence) versus number of people who have the flu on a given day (prevalence)
• Monitor progress in chronic conditions
• False positives, false negatives
• Sensitivity is greater when fewer false negatives (BE sensitive, I really am positive) - # of true positives divided by # of people tested who really have the disease
• Specificity – greater when fewer false positives (I specifically do NOT have it) - # of true negatives divided by the # of individuals tested who really do NOT have the disease
• Predictive value – important consideration – given a positive test result, what is the likelihood that the patient actually has the condition? Is in part dependent on the prevalence of the condition
• Positive predictive value = True positives divided by all positives
• Negative predictive value = true negatives divided by all negatives
• Consider cost, convenience, sensitivity and specificity, and the risk of missing a condition
• Will the test result affect the treatment plan?
• USPSTF, EBP guidelines for screening tests
Differential Diagnosis
• A list of possible diagnoses in priority order
• Considered when discussing a case
• One approach is considering a problem “from the skin in” – helps avoid premature closure
• Always include conditions that are life, organ, or function threatening
Developing a Management Plan
• Use clinical judgement in how to best manage these problems
• Consider a Multiparadigm Approach to Nursing
• Basic level = symptom relief, advanced level = functional patterns
Documentation: SOAP
• Subjective (CC, HPI, PMH, ROS)
• Objective (vitals, physical exam findings, pertinent negatives included, flow sheets to track data)
• Assessment (active problems being managed at the current visit, chronic problems and effectiveness of control i.e. DM II, poorly controlled, Obesity, Poorly controlled)
o If no clear diagnostic picture, name the complaint (Abdominal Pain R/O IBS or Cough, viral bronchitis vs. allergy)
• Plan (in detail, specific directions for each intervention) – list short- and long-term goals that explain the rationale for the plan / interventions
o 3 sections
1. Diagnostic testing to be done
2. Educational approaches
3. Follow up plans
Ethics
• 4 Pillars of Bioethics:
1. Respect for autonomy (informed and voluntary decision)
2. Nonmaleficence (do no harm)
3. Beneficence (benefits)
4. Justice (fairness)
Chapter 5 – Evidence-Based Practice pg. 59-72
Evidence Based Practice
• Using findings from the systematic review and appraisal of the most reliable studies to provide the best evidence for making decisions about health care in combination with expertise and practice-based knowledge and patient preference
• Pg. 59 Box 5.1 – Key steps in Implementing EBP
1. Ask clinical question
2. Collect most relevant EB from review of literature
3. Integrate evidence with expertise, knowledge, patient preference
4. Evaluate changes in outcome after implementing into practice
5. Disseminate findings
• Involves gathering information from the published literature to make decisions about its application to clinical practice
• Question is used to search literature for already completed studies that you can critically appraise to answer your clinical question
• Includes phenomenological and grounded theories studies that evaluate for understanding human experiences of health
• Stetler Model – method to address the need to use nursing research findings in practice
Best Practice Guidelines
• Agency for Health Care Policy and Research aka Agency for Health Care Research and Quality
• AHRQ guidelines – reference for HCPs, framework for insurance utilization review, quality assurance, and reimbursement, medical malpractice
• AHRQ 3 parts to initiative:
1. Institution of EBP centers – private-public partnership with AHRQ and HCO to produce evidence reports and tech assessments on priority health topics (topics are nominated by providers, must meet criteria outline on pg. 61, evidence reports are used to form state and federal policy)
2. Development of National Guideline Clearing House (NGC) – partnership with AHRQ and American Association of Health Plans and the AMA – NGC is online -widespread availability through online platform
3. Product research and evaluation – aim to develop evidence to use in guidelines, implementation strategies, and assess quality of outcomes when EBP is used
• See pg. 61 Box 5.2 Criteria for Inclusion of CPG in NGC
• See pg. 62 Box 5.3 for CPG guidelines published by organizations
Practice Standards and Guidelines
• Standards = framework for practice
• Guidelines = individual patient care decisions – provide a reference point and general direction for clinical decision making
• Practice Standards = to be used under ALL circumstances – define correct overall practice
• ANA practice standards a) clinical practice and b) professional performance
Development of Evidence-Based Practice Guidelines
• Essential components of guideline formation:
1. Identification / Clarification of the topic
2. Establishment of an expert panel
3. Systematic Review of Literature
4. Development of evidence-based tables
5. Writing draft recommendations based on the evidence
6. External review of the recommendations
7. Final acceptance of the revised recommendations by the panel
• Must appraise the quality of the evidence used to make each recommendation and then grading the recommendation based on the level of evidence
• Melnyk and Fineout-Overholt to rate evidence on a scale of I-VII
1. Level 1 – Systematic Review or Meta-Analysis of RCTs Systematic reviews (aka meta- analysis) are the highest level of evidence on which to base a change in practice
• Joanna Briggs – Levels:
1. Experimental Designs
2. Quasiexperimental designs – evaluate the effectiveness of an intervention but the subjects are NOT randomly assigned – control of extraneous variables and standardization of treatment are implemented
3. Observational / Analytical designs
4. Observational / Descriptive Studies / Case studies – useful to address prognosis or causation
- study is initiated AFTER disease has developed – cases (people with disease) and control (people without the disease) – observational because the do not manipulate the exposure (intervention)- course of disease is studied without interruption – potential for selection bias
- most commonly used epidemiological study design (Framingham Heart Study, Nurses’ Health Study)
5. Expert opinion and bench research
• FDA – requires evidence of drug’s efficacy from 2 randomized control trials before approving a drug
• Descriptive research – accurately portray the characteristics of a population or a clinical situation
– can be quantitative (descriptive statistics, frequencies, means, modes) or qualitative (narrative format to increase understanding of dimensions of phenomena – phenomenology, ethnography, grounded theory, historical analysis)
• Case Studies – single descriptive, likelihood of decreased objectivity, describe the history of 1
individual or a small group of patients in story form – value to alert a provider to an adverse event or rare disease or to ad to provider’s knowledge base – NO INFERENCES can be made to the general population
Evaluation of Clinical Practice Guidelines
• Author, Date of Revision or Origination
• Clinical Importance
• Strength of recommendation (determined by the strength of available evidence used to make the recommendation
• Applicable to your patients
Evaluating the Evidence to Change Practice
• Distinguishing between intermediate and clinical outcomes is critical before applying research findings to practice
• Outcome = dependent variable in the study. Intermediate outcomes (measurements – bone density, HgB, eosinophil), Clinical outcomes (measures such as the number of hip fractures, a person’s functional status, peak flow values, or the number of acute asthma exacerbations experienced)
• Improvement in intermediate outcomes does not necessarily lead to improvement in clinical outcomes (don’t substitute intermediate outcomes for clinical outcome data – fluoride for BMD values example – fluoride improved BMD values but did not reduce # of fractures
Developing a Point of Care Strategy
• Ask a clinical question
• Have evidence resources readily available (National Guideline Clearinghouse, Cochrane Collaboration, Essential Evidence Plus, Up to Date, Dynamed, Skyscape, Pepid primary care)
• Complete the search using those resources
• Examine the results of the search – consider the level of evidence the search provided (meta- analysis, systematic reviews)
• Apply the findings to the individual patient
• Pg. 68 Box 5.4 Framework for Point of Care Search Strategy for EBP
Nursing Science: Building the Evidence for Practice pg. 69
• Critically appraising studies regarding the appropriate use of results is one of the most important skills clinicians will need to use in practice
• Use a framework for guidance
• Pubmed and CINAHL are commonly used
• Framework provides an organized approach to interpreting the information found in a variety of articles
Clinical Decision Making and the Patient’s Health Care Decisions
• 2 main steps:
1. Collecting and analyzing evidence (data) on the benefits, risks, and costs of various options
2. Making a judgement about how to use the evidence to achieve the health outcome desired (includes provider experience and knowledge of available resources in the area)
Chapter 80: pg. 1327 – 1341 The Business of Advanced Practice Nursing
Medicare pg. 1328
• Providers submit application via Provider Enrollment Chain and Ownership System (PECOS) or paper format
• Medicare provides NPI number for billing to be used in HIPAA transactions
• Agreement is to provide services for payment according to MCR fee for schedule
• CMS Payment policy – based on annual physician and nonphysician provider fee schedule
• NPs are reimbursed at 85% of the physician fees, patient responsible for 20% - NP fees are typically 15% lower than physician fees)
• MCR: Covers 80% of physician fees, patient responsible for 20%. May have secondary insurance to cover their 20%
• MCR annual deductible
• Part A deductible (hospital) $1316
o Out of pocket hospital fees
1. Days 1-60 no additional fees
2. Days 61-90 $329 / day coinsurance
3. Days 91 + - $685 coinsurance per “lifetime reserved day” – limit total of 60 reserved days per lifetime
4. Beyond lifetime reserved days – ALL costs
• Part B (Outpatient) $183 / year
o Then patient responsibility is 20%
o CMS providers are required to attempt to collect the co-payments and deductible patient payments prior to services rendered
Medicare Access and CHIP Reauthorization Act
• MACRA 2016 – focuses on value: Quality and Resource Utilization
• Repealed Sustainable Growth Rate formula
• Created a Quality Payment Program
• Pay for performance / outcomes-based system
• Has 2 Payment and Reporting Models that the provider can choose from (if don’t choose, will automatically be placed in MIPS)
1. MIPS: Merit Based Incentive Systems - providers face a potential 4% reduction in part B payments by20019, increasing to 9% after that or payment increases of 4% per year based on demonstration of quality care at lower costs
o 3 Quality Reporting Categories:
1. Physician Quality
2. Value Based Payment Modifier
3. Meaningful Use
2. APM: Advanced Alternative Payment Model -
o Specific Requirements for Participation
o Participants must demonstrate an earning potential of 5% of MCR Part B incentive payment
o Providers will need to realign practices into accountable care organizations (ACO)P, Clinically integrated networks (CINs), or integrated delivery networks (IDN)
o May benefit from a team-based care approach under this model
o Rfalequires Risk Bearing: Risk of paying the lower of a) losing 8% of revenues when MCR expenditure is higher than expected or b) Repaying CMS up to 3% of total MCR Expenditure – for monetary loss, use of EMR by 50% of providers year 1, 75% year 2, and a state based payment on quality measures similar to MIPS
Medicare Advantage Plans
• Medicare MCOs
• Approved by CMS as alternate carries for MCR beneficiaries
• All benefits of MCR plus additional services
• High medical utilization – when pay out exceeds CMS fixed payments, plan incurs a loss
Opting Out of MCR
• Lasts for 2 years
• Can’t bill CMS
• Charge rate can be 115% of MCR rates, can only collect 95% of the MCR fee
• MCR will pay 75% of the PFS, patient pays remaining 20% of total fees, provider collects 95% payment of MCR fee
• Not subject to CMS Billing Restrictions
• Can reduce malpractice threshold
• Limits referrals: No participating MCR physician can refer patients to physicians who have opted out of MCR
• Opt Out physician must keep malpractice coverage or maintain a minimum of $250K to cover any malpractice claims that may come up
• NPs working under an opt out physician can NOT bill MCR
• Higher Risk for malpractice – varies by state, usually state requirements usually require $250K in escrow for malpractice if no insurance
Medicaid
• Offers medical assistance to low income families/individuals
• Jointly funded by state and federal
• Federal – assists states in providing medical care to people who meet the programs financial eligibility criteria
• Payment made directly to providers who have agreed to lower Medicaid reimbursement
• Exceptions: Hospitals that care for a disproportionate amount of Medicaid patients and hospice care
• Co-payment is exempt for emergency and family planning services
• Federal contribution matches state contribution
• State guidelines on reimbursement
Utilizing Financial Statements pg. 1335
• Balance Sheet – quantifies net worth of the business at a set time (monthly, quarterly, yearly)
• Operating or Income Statement – compares revenue to expenses in a period of time
• Cash-Flow Statement – details the movement of cash in and out of business
• Net Income Statement – demonstrates whether assets grew as a result of the year’s business activities
Current Procedural Technology (CPT)
• official procedural coding rules and guidelines required when reporting medical services and procedures performed
• Purchase yearly
• Health Care Financing Administration (HCFA) – created in 1977 to coordinate Medicare and Medicaid (were each separately run by SSA and by SRS)
• HCFA implemented the CPT codes that were developed by the AMA to provide service descriptions and reimbursement rates
• MCOs now also use CPT codes
• Reimbursement rates are set by the Resource Based Relative Value Scale (approved by Congress)
• Coding Rules: 3 things that affect cost calculation: a) physician’s work or medical expertise (54% of RVU b) practice overhead expenses (41% of RVU) c) professional liability and malpractice expenses (derived from a formula)
• Allows uniformity in management reporting, medical review, education, outcome measurement, and medical research
• CPT codes are 5-digit codes
• 3 levels of CPT codes: a) Cat I = codes used in contemporary medical practice b) Cat II – tracking codes used for new or performance measures c) Cat III – temporary coding used for new procedures, technology, and services
• Updates each October, implemented in January
• Category 1: 6 Sections
1. Evaluation and Management (E&M)
2. Anesthesiology
3. Surgery
4. Radiology
5. Pathology
6. Medicine
• If no CPT code exists that accurately identifies the provided services, each of the 6 sections has an “unlisted” code category
CPT Modifiers and Add on Codes
• Add on codes accompany a primary procedure code
• These indicate additional time spent with the patient (“prolonged service codes”)
• Can’t be used alone – use with the appropriate primary or level of E&M code
• Modifier – provides a means to report that a service or procedure has been altered by the circumstances of its use
“Incident To”
• “Incident to a physician’s professional service” is a billing phrase related to services furnished under the direct supervision of a physician
• Services are related to the course of treatment resulting from an initial visit with the physician and administered by a nonphysician (physician does not have to be in the room, but must be in the same suite or office)
• Nonphysician – (RN or NP, etc.) must be an employee of, leased by, or performing as an independent contractor of the physician
• In this situation, services may be billed under the physician’s provider number and reimbursement is made at 100% of the physician fee
• NPs may bill and be reimbursed using their own NPI when a physician is not on site or in the office, reimbursed at only 85% of the PFS
CPT Level II Codes
• Healthcare Common Procedure Coding System sets yearly
• Included are drug administration, pharmaceuticals, and durable medical equipment
• Payment may nor may NOT be associated with these codes, but necessary for tracking
Evaluation and management documentation:
• 7 Components that define level of E&M Services
1. History
2. Examination
3. Medical decision making
4. Counselling
5. Coordination of Care
6. Time
• See pg. 1339 Table 80.2 – E&M Chart Audit Tool
Value Measurement pg. 1340
• Know about fraud, abuse, compliance plans, HIPAA, risk management, performance improvement, quality indicators, EHR integration, telemedicine, etc.
• Fraud and Abuse Compliance Plans: ethical conflicts arise when providers balance competing pressure affected by professional values, changes in delivery systems, and financial regulations
• MCR requires % of charts be audited
• False Claims Act – fines and damages can be levied up to 3 times the claim amount, mandatory penalties of 5K-10K per claim
• Medicare Recovery Audit Contractors and Medicare Integrity Contractors recover payment errors
• Compliance Plan – compliance officer identifies and assists in developing and maintaining a plan that includes practice safeguards to prevent fraud and abuse
• HIPAA: Part 1 – protects health insurance coverage for workers and their families when they change or lose job, Part 2 – requires DHHS to establish national standards for EHR transactions, national identifiers for providers, health, plans and employers, security and privacy of health data
• Risk management – an extension of performance improvement – prevent undesirable events
and minimize impact of financial loss due to malpractice (product recalls, compliance with accreditation, contracts, workman’s comp, etc.)
• HEDIS: Health plan Employer Data and information set – performance reporting that is required by CMS – a set of standardized performance measures identified as indicators for consumers so they can evaluate the quality and cost aspects of health care delivery. Based on current health issues (cancer, diabetes, asthma, heart disease) – overseen by National Committee of Quality Assurance
• Value Based Healthcare – Deficit Reduction Act of 2005, programs of hospital acquired
conditions (HACs), etc. aimed at lowering health-care costs and safeguarding MCR trust fund – 14 categories of HACs: ACA defines readmissions (admission within 30 days to same or other hospital), readmission Dx of MI, HF, PNA, compares readmission rates to national standards to compare for adjustments (considers clinical relevant factors)
[Show More]



.png)