1. Nurse practitioner prescriptive authority is regulated by:
A. The National Council of State Boards of Nursing
B. The U.S. Drug Enforcement Administration
C. The State Board of Nursing for each state
D. The State B
...
1. Nurse practitioner prescriptive authority is regulated by:
A. The National Council of State Boards of Nursing
B. The U.S. Drug Enforcement Administration
C. The State Board of Nursing for each state
D. The State Board of Pharmacy
2. Physician Assistant (PA) prescriptive authority is regulated by:
A. The National Council of State Boards of Nursing
B. The U.S. Drug Enforcement Administration
C. The State Board of Nursing
D. The State Board of Medical Examiners
3. Clinical judgment in prescribing includes:
A. Factoring in the cost to the patient of the medication prescribed
B. Always prescribing the newest medication available for the disease process
C. Handing out drug samples to poor patients
D. Prescribing all generic medications to cut costs
4. Criteria for choosing an effective drug for a disorder include:
A. Asking the patient what drug they think would work best for them
B. Consulting nationally recognized guidelines for disease management
C. Prescribing medications that are available as samples before writing a prescription
D. Following U.S. Drug Enforcement Administration (DEA) guidelines for
prescribing
5. Nurse practitioner practice may thrive under health-care reform due to:
A. The demonstrated ability of nurse practitioners to control costs and improve patient
outcomes
B. The fact that nurse practitioners will be able to practice independently
C. The fact that nurse practitioners will have full reimbursement under health-care
reform
D. The ability to shift accountability for Medicaid to the state level
Chapter 2.Pharmacokinetic Basis of Therapeutics and Pharmacodynamic
MULTIPLE CHOICE
1. A patient’s nutritional intake and lab work reflects hypoalbuminemia. This is critical to prescribing because:
A. Distribution of drugs to target tissue may be affected
B. The solubility of the drug will not match the site of absorption
C. There will be less free drug available to generate an effect
D. Drugs bound to albumin are readily excreted by the kidney
2. Drugs that have a significant first-pass effect:
A. Must be given by the enteral (oral) route only
B. Bypass the hepatic circulation
C. Are rapidly metabolized by the liver and may have little if any desired action
D. Are converted by the liver to more active and fat-soluble forms
3. The route of excretion of a volatile drug will likely be:
A. The kidneys
B. The lungs
C. The bile and feces
D. The skin
4. Medroxyprogesterone (Depo Provera) is prescribed IM to create a storage reservoir of the drug. Storage reservoirs:
A. Assure that the drug will reach its intended target tissue
B. Are the reason for giving loading doses
C. Increase the length of time a drug is available and active
D. Are most common in collagen tissues
5. The NP chooses to give cephalexin every 8 hours based on knowledge of the drug’s:
A. Propensity to go to the target receptor
B. Biological half-life
C. Pharmacodynamics
D. Safety and side effects
6. Azithromycin dosing requires the first day’s dose be twice those of the other 4 days of the prescription. This is considered a loading dose. A loading dose:
A. Rapidly achieves drug levels in the therapeutic range
B. Requires four to five half-lives to attain
C. Is influenced by renal function
D. Is directly related to the drug circulating to the target tissues
7. The point in time on the drug concentration curve that indicates the first sign of a therapeutic effect is the:
A. Minimum adverse effect level
B. Peak of action
C. Onset of action
D. Therapeutic range
8. Phenytoin requires a trough level be drawn. Peak and trough levels are done:
A. When the drug has a wide therapeutic range
B. When the drug will be administered for a short time only
C. When there is a high correlation between the dose and saturation of receptor sites
D. To determine if a drug is in the therapeutic range
9. A laboratory result indicates the peak level for a drug is above the minimum toxic concentration. This means that the:
A. Concentration will produce therapeutic effects
B. Concentration will produce an adverse response
C. Time between doses must be shortened
D. Duration of action of the drug is too long
10. Drugs that are receptor agonists may demonstrate what property?
A. Irreversible binding to the drug receptor site
B. Up-regulation with chronic use
C. Desensitization or down-regulation with continuous use
D. Inverse relationship between drug concentration and drug action
11. Drugs that are receptor antagonists, such as beta blockers, may cause:
A. Down-regulation of the drug receptor
B. An exaggerated response if abruptly discontinued
C. Partial blockade of the effects of agonist drugs
D. An exaggerated response to competitive drug agonists
12. Factors that affect gastric drug absorption include:
A. Liver enzyme activity
B. Protein-binding properties of the drug molecule
C. Lipid solubility of the drug
D. Ability to chew and swallow
13. Drugs administered via intravenous (IV) route:
A. Need to be lipid soluble in order to be easily absorbed
B. Begin distribution into the body immediately
C. Are easily absorbed if they are nonionized
D. May use pinocytosis to be absorbed
14. When a medication is added to a regimen for a synergistic effect, the combined effect of the drugs is:
A. The sum of the effects of each drug individually
B. Greater than the sum of the effects of each drug individually
C. Less than the effect of each drug individually
D. Not predictable, as it varies with each individual
15. Which of the following statements about bioavailability is true?
A. Bioavailability issues are especially important for drugs with narrow therapeutic
ranges or sustained release mechanisms.
B. All brands of a drug have the same bioavailability.
C. Drugs that are administered more than once a day have greater bioavailability than
drugs given once daily.
D. Combining an active drug with an inert substance does not affect bioavailability.
16. Which of the following statements about the major distribution barriers (blood-brain or fetal- placental) is true?
A. Water soluble and ionized drugs cross these barriers rapidly.
B. The blood-brain barrier slows the entry of many drugs into and from brain cells.
C. The fetal-placental barrier protects the fetus from drugs taken by the mother.
D. Lipid soluble drugs do not pass these barriers and are safe for pregnant women.
17. Drugs are metabolized mainly by the liver via Phase I or Phase II reactions. The purpose of both of these types of reactions is to:
A. Inactivate prodrugs before they can be activated by target tissues
B. Change the drugs so they can cross plasma membranes
C. Change drug molecules to a form that an excretory organ can excrete
D. Make these drugs more ionized and polar to facilitate excretion
18. Once they have been metabolized by the liver, the metabolites may be:
A. More active than the parent drug
B. Less active than the parent drug
C. Totally “deactivated” so that they are excreted without any effect
D. All of the above
19. All drugs continue to act in the body until they are changed or excreted. The ability of the body to excrete drugs via the renal system would be increased by:
A. Reduced circulation and perfusion of the kidney
B. Chronic renal disease
C. Competition for a transport site by another drug
D. Unbinding a nonvolatile drug from plasma proteins
20. Steady state is:
A. The point on the drug concentration curve when absorption exceeds excretion
B. When the amount of drug in the body remains constant
C. When the amount of drug in the body stays below the MTC
D. All of the above
21. Two different pain meds are given together for pain relief. The drug-drug interaction is:
A. Synergistic
B. Antagonistic
C. Potentiative
D. Additive
22. Actions taken to reduce drug-drug interaction problems include all of the following EXCEPT:
A. Reducing the dose of one of the drugs
B. Scheduling their administration at different times
C. Prescribing a third drug to counteract the adverse reaction of the combination
D. Reducing the dosage of both drugs
23. Phase I oxidative-reductive processes of drug metabolism require certain nutritional elements. Which of the following would reduce or inhibit this process?
A. Protein malnutrition
B. Iron deficiency anemia
C. Both A and B
D. Neither A nor B
24. The time required for the amount of drug in the body to decrease by 50% is called:
A. Steady state
B. Half-life
C. Phase II metabolism
D. Reduced bioavailability time
25. An agonist activates a receptor and stimulates a response. When given frequently over time the body may:
A. Up-regulate the total number of receptors
B. Block the receptor with a partial agonist
C. Alter the drug’s metabolism
D. Down-regulate the numbers of that specific receptor
26. Drug antagonism is best defined as an effect of a drug that:
A. Leads to major physiologic psychological dependence
B. Is modified by the concurrent administration of another drug
C. Cannot be metabolized before another dose is administered
D. Leads to a decreased physiologic response when combined with another drug
27. Instructions to a client regarding self-administration of oral enteric-coated tablets should include which of the following statements?
A. “Avoid any other oral medicines while taking this drug.”
B. “If swallowing this tablet is difficult, dissolve it in 3 ounces of orange juice.”
C. “The tablet may be crushed if you have any difficultly taking it.”
D. “To achieve best effect, take the tablet with at least 8 ounces of fluid.”
28. The major reason for not crushing a sustained release capsule is that, if crushed, the coated beads of the drugs could possibly result in:
A. Disintegration
B. Toxicity
C. Malabsorption
D. Deterioration
29. Which of the following substances is the most likely to be absorbed in the intestines rather than in the stomach?
A. Sodium bicarbonate
B. Ascorbic acid
C. Salicylic acid
D. Glucose
30. Which of the following variables is a factor in drug absorption?
A. The smaller the surface area for absorption, the more rapidly the drug is absorbed.
B. A rich blood supply to the area of absorption leads to better absorption.
C. The less soluble the drug, the more easily it is absorbed.
D. Ionized drugs are easily absorbed across the cell membrane.
31. An advantage of prescribing a sublingual medication is that the medication is:
A. Absorbed rapidly
B. Excreted rapidly
C. Metabolized minimally
D. Distributed equally
32. Drugs that use CYP 3A4 isoenzymes for metabolism may:
A. Induce the metabolism of another drug
B. Inhibit the metabolism of another drug
C. Both A and B
D. Neither A nor B
33. Therapeutic drug levels are drawn when a drug reaches steady state. Drugs reach steady state:
A. After the second dose
B. After four to five half-lives
C. When the patient feels the full effect of the drug
D. One hour after IV administration
34. Up-regulation or hypersensitization may lead to:
A. Increased response to a drug
B. Decreased response to a drug
C. An exaggerated response if the drug is withdrawn
D. Refractoriness or complete lack of response
Chapter 3. Impact of Drug Interactions and Adverse Events on Therapeutics
MULTIPLE CHOICE
1. Which of the following patients would be at higher risk of experiencing adverse drug reactions (ADRs):
A. A 32-year-old male
B. A 22-year-old female
C. A 3-month-old female
D. A 48-year-old male
2. Infants and young children are at higher risk of ADRs due to:
A. Immature renal function in school-age children
B. Lack of safety and efficacy studies in the pediatric population
C. Children’s skin being thicker than adults, requiring higher dosages of topical
medication
D. Infant boys having a higher proportion of muscle mass, leading to a higher volume
of distribution
3. The elderly are at high risk of ADRs due to:
A. Having greater muscle mass than younger adults, leading to higher volume of
distribution
B. The extensive studies that have been conducted on drug safety in this age group
C. The blood-brain barrier being less permeable, requiring higher doses to achieve
therapeutic effect
D. Age-related decrease in renal function
4. The type of adverse drug reaction that is the result of an unwanted but otherwise normal pharmacological action of a drug given in the usual therapeutic doses is
A. Type A
B. Type B
C. Type C
D. Type D
5. Digoxin may cause a Type A adverse drug reaction due to:
A. Idiosyncratic effects
B. Its narrow therapeutic index
C. Being a teratogen
D. Being a carcinogen
6. Changes in the individual pharmacokinetic parameters of adsorption, distribution, or elimination may result in high concentrations of the drug in the body, leading to which type of adverse drug reaction?
A. Type A
B. Type C
C. Type D
D. Type E
7. According to the World Health Organization Classification, Type B adverse reactions are:
A. When a drug is a teratogen
B. When a drug is carcinogenic
C. A delayed ADR, such as renal failure
D. An allergic or idiosyncratic response
8. Sarah developed a rash after using a topical medication. This is a Type allergic drug reaction.
A. I
B. II
C. III
D. IV
9. A patient may develop neutropenia from using topical Silvadene for burns. Neutropenia is a(n):
A. Cytotoxic hypersensitivity reaction
B. Immune complex hypersensitivity
C. Immediate hypersensitivity reaction
D. Delayed hypersensitivity reaction
10. Anaphylactic shock is a:
A. Type I reaction, called immediate hypersensitivity reaction
B. Type II reaction, called cytotoxic hypersensitivity reaction
C. Type III allergic reaction, called immune complex hypersensitivity
D. Type IV allergic reaction, called delayed hypersensitivity reaction
11. James has hypothalamic-pituitary-adrenal axis suppression from chronic prednisone (a corticosteroid) use. He is at risk for what type of adverse drug reaction?
A. Type B
B. Type C
C. Type E
D. Type F
12. The treatment for a patient who experiences hypothalamic-pituitary-adrenal axis suppression while taking the corticosteroid prednisone, a Type C adverse drug reaction, is to:
A. Immediately discontinue the prednisone
B. Administer epinephrine
C. Slowly taper the patient off of the prednisone
D. Monitor for long-term effects, such as cancer
13. The ACE inhibitor lisinopril is a known teratogen. Teratogens cause Type _ adverse drug reaction.
A. A
B. B
C. C
D. D
14. Cardiac defects are a known Type D adverse drug reaction to lithium. Lithium causes a Type D adverse drug reaction because it is:
A. An immunosuppressant
B. A carcinogen
C. A teratogen
D. An antiseizure medication
15. Immunomodulators such as azathioprine may cause a delayed adverse drug reaction known as a Type D reaction because they are known:
A. Teratogens
B. Carcinogens
C. To cause hypersensitivity reactions
D. Hypothalamus-pituitary-adrenal (HPA) axis suppressants
16. A 24-year-old male received multiple fractures in a motor vehicle accident that required significant amounts of opioid medication to treat his pain. He is at risk for Type adverse drug reaction when he no longer requires the opioids.
A. A
B. C
C. E
D. G
17. Drugs that may cause a Type E adverse drug reaction include:
A. Beta blockers
B. Immunomodulators
C. Antibiotics
D. Oral contraceptives
18. Unexpected failure of drug therapy is a Type adverse drug reaction, commonly caused by .
A. B; cytotoxic hypersensitivity
B. B; idiosyncratic response
C. C; cumulative effects of drug
D. F; drug-drug interaction
19. Clopidogrel treatment failure may occur when it is co-administered with omeprazole, known as a Type adverse drug reaction.
A. A
B. C
C. E
D. F
Chapter 4. Principles of Pharmacotherapy in Children
MULTIPLE CHOICE
1. The Pediatric Research Equity Acts requires:
A. All children be provided equal access to drug research trials
B. Children to be included in the planning phase of new drug development
C. That pediatric drug trials guarantee children of multiple ethnic groups are included
D. All applications for new active ingredients, new indications, new dosage forms, or
new routes of administration require pediatric studies
2. The Best Pharmaceuticals for Children Act:
A. Includes a pediatric exclusivity rule which extends the patent on drugs studied in
children
B. Establishes a committee that writes guidelines for pediatric prescribing
C. Provides funding for new drug development aimed at children
D. Encourages manufacturers specifically to develop pediatric formulations
3. The developmental variation in Phase I enzymes has what impact on pediatric prescribing?
A. None, Phase I enzymes are stable throughout childhood.
B. Children should always be prescribed lower than adult doses per weight due to low
enzyme activity until puberty.
C. Children should always be prescribed higher than adult doses per weight due to
high enzyme activity.
D. Prescribing dosages will vary based on the developmental activity of each enzyme,
at times requiring lower than adult doses and other times higher than adult doses based on the age of the child.
4. Developmental variation in renal function has what impact on prescribing for infants and children?
A. Lower doses of renally excreted drugs may be prescribed to infants younger than
age 6 months.
B. Higher doses of water soluble drugs may need to be prescribed due to increased
renal excretion.
C. Renal excretion rates have no impact on prescribing.
D. Parents need to be instructed on whether drugs are renally excreted or not.
5. Topical corticosteroids are prescribed cautiously in young children due to:
A. They may cause an intense hypersensitivity reaction
B. Hypothalamic-pituitary-adrenal (HPA) axis suppression
C. Corticosteroids are less effective in young children
D. Young children may accumulate corticosteroids leading to toxic levels
6. Liza is breastfeeding her 2-month-old son and has an infection that requires an antibiotic. What drug factors influence the effect of the drug on the infant?
A. Maternal drug levels
B. Half-life
C. Lipid-solubility
D. All of the above
7. Drugs that are absolutely contraindicated in lactating women include:
A. Selective serotonin reuptake inhibitors
B. Antiepileptic drugs such as carbamazepine
C. Antineoplastic drugs such as methotrexate
D. All of the above
8. Zia is a 4 month old with otitis media. Education of his parents regarding administering oral antibiotics to an infant includes:
A. How to administer an oral drug using a medication syringe
B. Mixing the medication with a couple ounces of formula and putting it in a bottle
C. Discontinuing the antibiotic if diarrhea occurs
D. Calling for an antibiotic change if the infant chokes and sputters during
administration
9. To increase adherence in pediatric patients a prescription medication should:
A. Have a short half-life
B. Be the best tasting of the effective drugs
C. Be the least concentrated form of the medication
D. Be administered 3 or 4 times a day
ANS: B PTS: 1
10. Janie is a 5-month-old breastfed infant with a fever. Treatment for her fever may include:
A. “Baby” aspirin
B. Acetaminophen suppository
C. Ibuprofen suppository
D. Alternating acetaminophen and ibuprofen
Chapter 5. Principles of Pharmacotherapy in Pregnancy and
Lactation
MULTIPLE CHOICE
1. The client has been prescribed Doxylamine (Unisom) for treatment of nausea and vomiting during pregnancy. What aspect of the client’s history will cause the nurse to contact the primary health care provider?
a. Arthritis
b. Depression
c. Asthma
d. Hyperglycemia
2. The nurse is teaching a group of pregnant women the importance of adequate nutrition for the fetus. The nurse instructs the clients that folic acid deficiency during preconception and early in pregnancy can result in:
a. skeletal defects.
b. neural tube defects.
c. intrauterine growth retardation.
d. small-for-gestational-age infants.
3. A client is ordered to receive iron and antacids. The nurse teaches the client that iron and antacids should be administered:
a. at the same time.
b. 2 hours apart.
c. with the antacid first.
d. with the iron first.
4. A client, 10 weeks pregnant, complains of severe nausea of pregnancy. Meclizine (Bonine) is prescribed. The client reports to the nurse that she has begun to experience dizziness. What is the highest priority nursing intervention?
a. Contact the pharmacist; this indicates an overdosage of the medication.
b. Contact the physician; this is an expected side effect of the medication.
c. Contact the pharmacist; this indicates incorrect preparation of the medication.
d. Contact the physician; this is an adverse reaction to the medication.
5. A client complains of severe pregnancy-related nausea and is placed on Meclizine (Bonine). The nurse notes in the client history that the client is undergoing treatment for glaucoma. What is the highest priority nursing intervention?
a. Recognize that one of the off-label uses for the drug is treatment of glaucoma.
b. Contact the pharmacist; the dosage of the drug should be decreased when
glaucoma is present.
c. Recognize that use of the drug when glaucoma is present may result in a fatal
reaction.
d. Contact the physician; the drug should be used with caution when glaucoma is
present.
6. Betamethasone (Celestone) is ordered for a client in preterm labor. The client asks the nurse what the medication will do to help her. The nurse explains to the client that the medication will:
a. help her to breathe more effectively during the labor process.
b. prevent her infant from developing respiratory distress syndrome.
c. help her infant to breathe more effectively during the labor process.
d. prevent her from developing congestive heart failure during labor.
7. A client is admitted to the labor and delivery unit and is being treated with terbutaline
(Brethine). The nurse plans the client’s care with the knowledge that this medication is used to:
a. induce labor.
b. decrease uterine contractions.
c. stimulate fetal heart rate.
d. enhance placental blood flow.
8. The client is being treated with hydralazine hydrochloride (Apresoline). What would be a positive outcome for the client as a result of treatment with this medication?
a. Diastolic BP is maintained between 90 and 110 mm Hg.
b. Diastolic BP is maintained between 70 and 90 mm Hg.
c. Systolic BP is maintained between 100 and 120 mm Hg.
d. Systolic BP is maintained between 90 and 110 mm Hg.
9. A client diagnosed with pregnancy-induced hypertension (PIH) is treated with magnesium sulfate. The nurse tells the client that the purpose of this treatment is to:
a. prolong labor.
b. prevent seizures.
c. increase blood pressure.
d. stimulate urination.
10. A prenatal client discloses that she takes high doses of vitamins. Which is the most accurate instruction that the nurse can provide in response to the client’s statement?
a. “High levels of vitamins may cause harm to the fetus.”
b. “Only water-soluble vitamins may be harmful during pregnancy.”
c. “Megadoses of vitamins are associated with positive birth outcomes.”
d. “Vitamin supplementation is not needed during pregnancy.”
11. A pregnant woman experiences constipation. The nurse anticipates that which laxative may be used first after activity and dietary methods are unsuccessful?
a. Mineral oil
b. Psyllium (Metamucil)
c. Lactulose
d. Milk of magnesia
12. The client is scheduled for treatment with betamethasone (Celestone). The nurse anticipates that this medication will be administered via the _ route.
a. oral
b. intravenous
c. intramuscular
d. subcutaneous
13. The client is scheduled for treatment with betamethasone (Celestone). The nurse anticipates that the medication will be administered to the client during which week or before of her pregnancy.
a. 38
b. 36
c. 35
d. 33
14. The healthcare provider orders hydroxyzine (Vistaril) for a client in labor. To achieve a positive outcome, the nurse plans to administer the drug via which route?
a. Intradermally
b. Intravenously
c. Intramuscularly via Z-track technique
d. Subcutaneously via Z-track technique
15. An epidural block is ordered for a primipara client in labor. The nurse anticipates that this epidural block will be given when the cervix is dilated at centimeters.
a. 2 to 3
b. 3 to 4
c. 4 to 5
d. 5 to 6
16. A client is being treated with an ergot alkaloid medication. Which observation would cause the nurse to contact the primary healthcare provider?
a. Hypertension
b. Itching
c. Jugular vein distention
d. Seizure activity
17. The client is scheduled for an epidural anesthetic as she delivers. What will be the highest priority nursing intervention?
a. Administer 1 L of an isotonic IV solution and encourage use of a bedpan after
spinal anesthesia.
b. Administer 500 mL of a hypotonic IV solution and assess the level of
consciousness because the patient is sedated.
c. Administer 500 mL of a hypertonic IV solution and assess fetal heart rate and
progress of labor as per pregnancy protocol.
d. Administer 1 L of hypotonic IV solution and allow the client to ambulate during
the spinal anesthesia.
18. The best candidate for treatment with dinoprostone (Cervidil) is the woman who needs her:
a. labor stopped.
b. cervix ripened.
c. labor stimulated.
d. labor prolonged.
19. Which will most likely be part of the nursing care of a woman postcaesarean section with spinal anesthesia?
a. Early ambulation to avoid constipation
b. Fluid restrictions to decrease blood volume
c. Lying flat 6 to 8 hours to avoid spinal headache
d. IV antibiotics to avoid postpartum infection
20. The client is scheduled to be treated with Oxytocin by nasal spray. The nurse plans to administer the drug:
a. 2 to 3 minutes after the client nurses her baby.
b. 2 to 3 minutes before the client nurses her baby.
c. after delivery of the placenta.
d. as delivery of the placenta is imminent.
MULTIPLE RESPONSE
1. A young women in labor, G1P0, is diagnosed with pregnancy-induced hypertension (PIH). She is ordered to receive magnesium sulfate. What are the other components of her nursing care? (Select all that apply.)
a. Maintaining a quiet environment
b. Assessing vital signs and fetal heart tones frequently
c. Providing large amounts of PO and IV fluids to maintain fluid volume
d. Allowing the woman to ambulate ad lib
e. Assessing for clonus and deep tendon reflexes
f. Monitoring urine hourly for protein
Chapter 6. Principles of Pharmacotherapy in Elderly Patients
MULTIPLE CHOICE
1. Principles of prescribing for older adults include:
A. Avoiding prescribing any newer high-cost medications
B. Starting at a low dose and increasing the dose slowly
C. Keeping total dose at lower therapeutic range
D. All of the above
2. Sadie is a 90-year-old patient who requires a new prescription. What changes in drug distribution with aging would influence prescribing for Sadie?
A. Increased volume of distribution
B. Decreased lipid solubility
C. Decreased plasma proteins
D. Increased muscle to fat ratio
3. Glen is an 82 year old who needs to be prescribed a new drug. What changes in elimination should be taken into consideration when prescribing for Glen?
A. Increased GFR will require higher doses of some renally excreted drugs
B. Decreased tubular secretion of medication will require dosage adjustments
C. Thin skin will cause increased elimination via sweat
D. Decreased lung capacity will lead to measurable decreases in lung excretion of
drugs
4. A medication review of an elderly person’s medications involves:
A. Asking the patient to bring a list of current prescription medications to the visit
B. Having the patient bring all of their prescription, over-the-counter, and herbal
medication to the visit
C. Asking what other providers are writing prescriptions for them
D. All of the above
5. Steps to avoid polypharmacy include:
A. Prescribing two or fewer drugs from each drug class
B. Reviewing a complete drug history every 12 to 18 months
C. Encouraging the elderly patient to coordinate their care with all of their providers
D. Evaluating for duplications in drug therapy and discontinuing any duplications
6. Robert is a 72 year old who has hypertension and angina. He is at risk for common medication practices seen in the elderly including:
A. Use of another person’s medications
B. Hoarding medications
C. Changing his medication regimen without telling his provider
D. All of the above
7. To improve positive outcomes when prescribing for the elderly the nurse practitioner should:
A. Assess cognitive functioning in the elder
B. Encourage the patient to take a weekly “drug holiday” to keep drug costs down
C. Encourage the patient to cut drugs in half with a knife to lower costs
D. All of the above
8. When an elderly diabetic patient is constipated the best treatment options include:
A. Mineral oil
B. Bulk-forming laxatives such as psyllium
C. Stimulant laxatives such as senna
D. Stool softeners such as docusate
9. Delta is an 88 year old who has mild low back pain. What guidelines should be followed when prescribing pain management for Delta?
A. Keep the dose of oxycodone low to prevent development of tolerance
B. Acetaminophen is the first-line drug of choice
C. Avoid prescribing NSAIDs
D. Add in a short-acting benzodiazepine for a synergistic effect on pain
10. Robert is complaining of poor sleep. Medications that may contribute to sleep problems in the elderly include:
A. Diuretics
B. Trazodone
C. Clonazepam
D. Levodopa
Chapter 7 Principles of Pharmacotherapy in Pain
Management
MULTIPLE CHOICE
1. Different areas of the brain are involved in specific aspects of pain. The reticular and limbic systems in the brain influence:
A. The sensory aspects of pain
B. The discriminative aspects of pain
C. The motivational aspects of pain
D. The cognitive aspects of pain
2. Patients need to be questioned about all pain sites because:
A. Patients tend to report the most severe or important in their perception
B. Pain tolerance generally decreases with repeated exposure
C. The reported pain site is usually the most important to treat
D. Pain may be referred from a different site to the one reported
3. The chemicals that promote the spread of pain locally include:
A. Serotonin
B. Norepinephrine
C. Enkephalin
D. Neurokinin A
4. Narcotics are exogenous opiates. They act by:
A. Inhibiting pain transmission in the spinal cord
B. Attaching to receptors in the afferent neuron to inhibit the release of substance P
C. Blocking neurotransmitters in the midbrain
D. Increasing beta-lipoprotein excretion from the pituitary
5. Age is a factor in different responses to pain. Which of the following age-related statements about pain is NOT true?
A. Preterm and newborn infants do not yet have functional pain pathways.
B. Painful experiences and prolonged exposure to analgesic drugs during pregnancy
may permanently alter neuronal organization in the child.
C. Increases in pain threshold in older adults may be related to peripheral
neuropathies and changes in skin thickness
D. Decreases in pain tolerance are evident in older adults
6. Which of the following statements is true about acute pain?
A. Somatic pain comes from body surfaces and is only sharp and well-localized.
B. Visceral pain comes from the internal organs and is most responsive to
acetaminophen and opiates.
C. Referred pain is present in a distant site for the pain source and is based on
activation of the same spinal segment as the actual pain site.
D. Acute neuropathic pain is caused by lack of blood supply to the nerves in a given
area.
7. One of the main drug classes used to treat acute pain is NSAIDs. They are used because:
A. They have less risk for liver damage than acetaminophen
B. Inflammation is a common cause of acute pain
C. They have minimal GI irritation
D. Regulation of blood flow to the kidney is not affected by these drugs
8. Opiates are used mainly to treat moderate to severe pain. Which of the following is NOT true about these drugs?
A. All opiates are scheduled drugs which require a DEA license to prescribe.
B. Opiates stimulate only mu receptors for the control of pain.
C. Most of the adverse effects of opiates are related to mu receptor stimulation.
D. Naloxone is an antagonist to opiates.
9. If interventions to resolve the cause of pain (RICE) are insufficient, pain medications are given based on the severity of pain. Drugs are given in which order of use?
A. NSAIDs, opiates, corticosteroids
B. Low-dose opiates, salicylates, increased dose of opiates
C. Opiates, non-opiates, increased dose of non-opiate
D. Non-opiate, increased dose of non-opiate, opiate
10. The goal of treatment of acute pain is:
A. Pain at a tolerable level where patient may return to activities of daily living
B. Reduction of pain with a minimum of drug adverse effects
C. Reduction or elimination of pain with minimum adverse reactions
D. Adequate pain relief without constipation or nausea from the drugs
11. Which of the following statements is true about age and pain?
A. Use of drugs that depend heavily on the renal system for excretion may require
dosage adjustments in very young children.
B. Among the NSAIDs, indomethacin is the preferred drug because of lower adverse
effects profiles than other NSAIDs.
C. Older adults who have dementia probably do not experience much pain due to loss
of pain receptors in the brain.
D. Acetaminophen is especially useful in both children and adults because it has no
effect on platelets and has fewer adverse effects than NSAIDs.
12. Pain assessment to determine adequacy of pain management is important for all patients. This assessment is done to:
A. Determine if the diagnosis of source of pain is correct
B. Determine if the current regimen is adequate or different combinations of drugs
and non-drug therapy are required
C. Determine if the patient is willing and able to be an active participant in his or her
pain management
D. All of the above
13. Pathological similarities and differences between acute pain and chronic pain include:
A. Both have decreased levels of endorphins
B. Chronic pain has a predominance of C-neuron stimulation
C. Acute pain is most commonly associated with irritation of peripheral nerves
D. Acute pain is diffuse and hard to localize
14. A treatment plan for management of chronic pain should include:
A. Negotiation with the patient to set personal goals for pain management
B. Discussion of ways to improve sleep and stress
C. An exercise program to improve function and fitness
D. All of the above
15. Chronic pain is a complex problem. Some specific strategies to deal with it include:
A. Telling the patient to “let pain be your guide” to using treatment therapies
B. Prescribing pain medication on a “PRN” basis to keep down the amount used
C. Scheduling return visits on a regular basis rather than waiting for poor pain control
to drive the need for an appointment
D. All of the above
16. Chemical dependency assessment is integral to the initial assessment of chronic pain. Which of the following raises a “red flag” about potential chemical dependency?
A. Use of more than one drug to treat the pain
B. Multiple times when prescriptions are lost with requests to refill
C. Preferences for treatments that include alternative medicines
D. Presence of a family member who has abused drugs
17. The Pain Management Contract is appropriate for:
A. Patients with a history of chemical dependency or possible inappropriate use of
pain medications
B. All patients with chronic pain who will require long-term use of opiates
C. Patients who have a complex drug regimen
D. Patients who see multiple providers for pain control
Chapter 8. Principles of Antimicrobial Therapy
MULTIPLE CHOICE
1. A nurse is ordered to draw blood levels for a person receiving an antibiotic. The nurse is aware that peaks and troughs of serum antibiotic levels are monitored for drugs with a:
a. narrow therapeutic index.
b. large therapeutic index.
c. long half-life.
d. short half-life.
2. A client’s medication warrants peak and trough levels to be drawn. The nurse is aware that if the peak level of the drug is too high, what could occur?
a. Mild side effects
b. Inadequate drug action
c. Slow onset of drug action
d. Drug toxicity
3. Drug concentration is important for the eradication of bacterial infection. It is desired to keep the drug dose:
a. below minimum effective concentration.
b. above minimum effective concentration.
c. below minimum toxic level.
d. above minimum toxic level.
4. With continuous use of antibiotics, antibiotic resistance result because:
a. bacteria are producing fewer mutations.
b. the immune system has enhanced ability to fight infection.
c. mutant bacteria are surviving antibiotic use.
d. fewer new antibiotics have been produced.
5. A client with otitis media is ordered to receive amoxicillin (Amoxil). The client discloses to the nurse that she is allergic to penicillin. What is the highest priority action on the part of the nurse?
a. Notify the healthcare provider that the client is allergic to penicillin.
b. Encourage the client to take the dose under close monitoring.
c. Administer half of the amoxicillin dose under supervision.
d. Report the amoxicillin order to the supervisor.
6. A client has relayed instructions from a physician regarding an allergy to a type of antibiotic therapy. The nurse would question which instruction?
a. Wear a Medic Alert bracelet that indicates the allergy.
b. Avoid all penicillin-type drugs.
c. Inform all healthcare providers of the allergy.
d. Restrict fluids when taking the antibiotic.
7. When antibacterials are prescribed for the treatment of an infection and a culture is ordered, what should happen next?
a. The initial dose of the antibiotic should be given before the culture is taken.
b. The culture should be taken before the initial dose of the antibiotic is given.
c. The culture should be taken any time after the antibiotic therapy begins.
d. The culture may be taken at any time before or during antibiotic therapy.
8. A client at an outpatient clinic is ordered to receive ampicillin (Omnipen) for an infection. Which nursing intervention related to penicillins would the nurse question?
a. Verify that the client is not allergic to penicillin.
b. Obtain culture before administering the first dose of medication.
c. Instruct client to discontinue penicillin when temperature is normal.
d. Encourage the client to increase fluid intake.
9. Most beta-lactam antibiotics are excreted through the kidneys. The nurse should assess the client’s renal function by monitoring which levels?
a. Blood urea nitrogen and serum creatinine
b. Creatinine phosphokinase and alkaline phosphatase
c. White blood cell count and red blood cell count
d. Hemoglobin and hematocrit
10. A client is ordered to receive a cephalosporin to treat a bacterial infection. Regarding monitoring of the client, the highest priority action on the part of the nurse includes assessing the client for which side effects?
a. Nausea, vomiting, and diarrhea
b. Photophobia and phototoxicity
c. Pain with urination and blood in the urine
d. High fevers and sweating
11. A client has been receiving a cephalosporin for 20 days to treat a severe bacterial infection. The client complains of mouth pain, and the nurse assesses white patches in the client’s mouth. What is the highest priority action on the part of the nurse?
a. Provide mouth care with glycerin swabs.
b. Encourage the client to drink more fluids.
c. Notify the physician and describe symptoms.
d. Administer analgesia for the mouth pain.
12. A client who reports an allergy to penicillin is ordered to receive cephalexin (Keflex). The correct action for the nurse is to:
a. administer the medication as ordered with additional fluids.
b. administer the medication and carefully observe for allergic reaction.
c. call the physician to change the order because of the allergy history.
d. administer another antibiotic after consulting the pharmacist.
13. The client has been ordered treatment with Cefaclor as well as erythromycin. The nurse anticipates what effect from the interaction of the medications?
a. Increased action of the Cefaclor
b. Decreased action of the Cefaclor
c. Anaphylactic reaction to the Cefaclor
d. Toxic action of the Cefaclor
14. The client has been ordered Cefazolin. The nurse anticipates an increase in the client’s
from this medication?
a. BUN and serum creatinine
b. serum potassium
c. serum calcium
d. serum white blood cells
15. The client has been ordered to be treated with amoxicillin. The highest priority instruction that the nurse should give the client related to diet while on the medication is to avoid:
a. green leafy vegetables.
b. beef and other red meat.
c. coffee, tea, and colas.
d. acidic fruits and juices.
16. The client has been ordered treatment with Wycillin. The nurse notes that the solution is milky in color. What is the highest priority action on the part of the nurse?
a. Call the pharmacist and report the milky color.
b. Add normal saline to dilute the medication.
c. Call the physician and report the milky appearance.
d. Administer the medication as ordered by the physician.
17. The client has been ordered treatment with Amoxil. The client reports to the nurse that she has developed symptoms of vaginitis. The highest priority action on the part of the nurse is to recognize this as:
a. an expected side effect of the medication.
b. a life-threatening reaction to the drug.
c. evidence of development of a superinfection.
d. evidence of an anaphylactic reaction.
Chapter 9. Complementary and Alternative Medicines
MULTIPLE CHOICE
1. A good history of herb and supplement use is critical before prescribing because approximately of patients in the United States are using herbal products.
A. 10%
B. 5%
C. 38%
D. 70%
2. A potential harmful effect to patients who take some herbal medication is:
A. Constipation
B. Lead poisoning
C. Diarrhea
D. Life-threatening rash
3. A thorough understanding of herbs is critical to patient safety. An example is the use of cinnamon to treat Type II diabetes. It is important the patient uses Ceylon cinnamon, as the commercially available cassia cinnamon contains:
A. Coumadin, which may lead to bleeding problems
B. Coumarin, which can cause liver and kidney damage
C. Cinnamic aldehyde, which is toxic to the kidney
D. Cinnamate eugenol, which is toxic to the liver
4. Traditional Chinese medicine utilizes yin (cooling) versus yang (warming) in assessing and treating disease. Menopause is considered a time of imbalance, therefore the Chinese herbalist would prescribe:
A. Herbs which are yang in nature
B. Herbs that are yin in nature
C. Ginger
D. Golden seal
5. According to Traditional Chinese Medicine, if a person who has a fever is given a herb that is yang in nature, such as golden seal, the patient’s illness will:
A. Get worse
B. Get better
C. Not be adequately treated
D. Need additional herbs to treat the yang
6. In Ayurvedic medicine treatment is based on the patient’s dominant dosha, which is referred to as the person’s:
A. Vata
B. Pitta
C. Kapha
D. Prakriti
7. Herbs and supplements are regulated by the Food and Drug Administration.
A. True
B. False
8. When melatonin is used to induce sleep, the recommendation is the patient:
A. Take 10 mg 30 minutes before bed nightly
B. Take 1 to 5 mg 30 minutes before bed nightly
C. Not take melatonin more than three nights a week
D. Combine melatonin with zolpidem (Ambien) for the greatest impact on sleep
9. Valerian tea causes relaxation and can be used to help a patient fall asleep. Overdosage of valerian (more than 2.5 gm/dose) may lead to:
A. Cardiac disturbances
B. Central nervous system depression
C. Respiratory depression
D. Skin rashes
10. The standard dosage of St John’s Wort for the treatment of mild depression is:
A. 300 mg daily
B. 100 mg three times a day
C. 300 mg three times a day
D. 600 mg three times a day
11. Patients need to be instructed regarding the drug interactions with St John’s Wort, including:
A. MAO inhibitors (MAOIs)
B. Serotonin reuptake inhibitors (SSRIs)
C. Over-the-counter (OTC) cough and cold medications
D. All of the above
12. Ginseng, which is taken to assist with memory, may potentiate:
A. Aricept
B. Insulin
C. Digoxin
D. Propranolol
13. Licorice root is a common treatment for dyspepsia. Drug interactions with licorice include:
A. Antihypertensives, diuretics, and digoxin
B. Antidiarrheals, antihistamines, and omeprazole
C. Penicillin antibiotic class and benzodiazepines
D. None of the above
14. Patients should be warned about the overuse of topical wintergreen oil to treat muscle strains, as overapplication can lead to:
A. Respiratory depression
B. Cardiac disturbance
C. Salicylates poisoning
D. Life-threatening rashes
15. The role of the NP in the use of herbal medication is to:
A. Maintain competence in the prescribing of common herbal remedies
B. Recommend common over-the-counter herbs to patients
C. Educate patients and guide them to appropriate sources of care
D. Encourage patients to not use herbal therapy due to the documented dangers
Chapter 10. Pharmacogenomics
MULTIPLE CHOICE
1. Genetic polymorphisms account for differences in metabolism, including:
A. Poor metabolizers (PMs) who lack a working enzyme
B. Intermediate metabolizers (IMs) who have one working, wild-type allele and one
mutant allele
C. Extensive metabolizers (EMs), with two normally functioning alleles
D. All of the above
2. Up to 21% of Asians are ultra-rapid 2D6 metabolizers, leading to:
A. A need to monitor drugs metabolized by 2D6 for toxicity
B. Increased dosages needed of drugs metabolized by 2D6, such as the SSRIs
C. Decreased conversion of codeine to morphine by CYP 2D6
D. The need for lowered dosages of drugs, such as beta blockers
3. Rifampin is a nonspecific CYP450 inducer that may:
A. Lead to toxic levels of rifampin and must be monitored closely
B. Cause toxic levels of drugs, such as oral contraceptives, when co-administered
C. Induce the metabolism of drugs, such as oral contraceptives, leading to therapeutic
failure
D. Cause nonspecific changes in drug metabolism
4. Inhibition of P-glycoprotein by a drug such as quinidine may lead to:
A. Decreased therapeutic levels of quinidine
B. Increased therapeutic levels of quinidine
C. Decreased levels of a co-administered drug, such as digoxin, that requires P-
glycoprotein for absorption and elimination
D. Increased levels of a co-administered drug, such as digoxin, that requires P-
glycoprotein for absorption and elimination
5. Warfarin resistance may be seen in patients with VCORC1 mutation, leading to:
A. Toxic levels of warfarin building up
B. Decreased response to warfarin
C. Increased risk for significant drug interactions with warfarin
D. Less risk of drug interactions with warfarin
6. Genetic testing for VCORC1 mutation to assess potential warfarin resistance is required prior to prescribing warfarin.
A. True
B. False
7. Pharmacogenetic testing is required by the Food and Drug Administration (FDA) prior to prescribing:
A. Erythromycin
B. Digoxin
C. Cetuximab
D. Rifampin
8. Carbamazepine has a Black Box warning recommending testing for the HLA-B*1502 allele in patients with Asian ancestry prior to starting therapy due to:
A. Decreased effectiveness of carbamazepine in treating seizures in Asian patients
with the HLA-B*1502 allele
B. Increased risk for drug interactions in Asian patients with the HLA-B*1502 allele
C. Increased risk for Stevens-Johnson syndrome in Asian patients with HLA-B*1502
allele
D. Patients who have the HLA-B*1502 allele being more likely to have a resistance to
carbamazepine
9. A genetic variation in how the metabolite of the cancer drug irinotecan SN-38 is inactivated by the body may lead to:
A. Decreased effectiveness of irinotecan in the treatment of cancer
B. Increased adverse drug reactions, such as neutropenia
C. Delayed metabolism of the prodrug irinotecan into the active metabolite SN-38
D. Increased concerns for irinotecan being carcinogenic
10. Patients who have a poor metabolism phenotype will have:
A. Slowed metabolism of a prodrug into an active drug, leading to accumulation of
prodrug
B. Accumulation of inactive metabolites of drugs
C. A need for increased dosages of medications
D. Increased elimination of an active drug
11. Ultra-rapid metabolizers of drugs may have:
A. To have dosages of drugs adjusted downward to prevent drug accumulation
B. Active drug rapidly metabolized into inactive metabolites, leading to potential
therapeutic failure
C. Increased elimination of active, nonmetabolized drug
D. Slowed metabolism of a prodrug into an active drug, leading to accumulation of
prodrug
12. A provider may consider testing for CYP2D6 variants prior to starting tamoxifen for breast cancer to:
A. Ensure the patient will not have increased adverse drug reactions to the tamoxifen
B. Identify potential drug-drug interactions that may occur with tamoxifen
C. Reduce the likelihood of therapeutic failure with tamoxifen treatment
D. Identify poor metabolizers of tamoxifen
Chapter 11. Contact Dermatitis
MULTIPLE CHOICE
1. When choosing a topical corticosteroid cream to treat diaper dermatitis, the ideal medication would be:
A. Intermediate potency corticosteroid ointment (Kenalog)
B. A combination of a corticosteroid and an antifungal (Lotrisone)
C. A low potency corticosteroid cream applied sparingly (hydrocortisone 1%)
D. A high potency corticosteroid cream (Diprolene AF)
2. Topical immunomodulators such as pimecrolimus (Elidel) or tacrolimus (Protopic) are used for:
A. Short-term or intermittent treatment of atopic dermatitis
B. Topical treatment of fungal infections (Candida)
C. Chronic, inflammatory seborrheic dermatitis
D. Recalcitrant nodular acne
3. Long-term treatment of moderate atopic dermatitis includes:
A. Topical corticosteroids and emollients
B. Topical corticosteroids alone
C. Topical antipruritics
D. Oral corticosteroids for exacerbations of atopic dermatitis
4. Severe contact dermatitis caused by poison ivy or poison oak exposure often requires treatment with:
A. Topical antipruritics
B. Oral corticosteroids for 2 to 3 weeks
C. Thickly applied topical intermediate-dose corticosteroids
D. Isolation of the patient to prevent spread of the dermatitis
5. When a patient has contact dermatitis, wet dressings with Domeboro solution are used for:
A. Cleaning the weeping area of dermatitis
B. Bathing the patient to prevent infection
C. Relief of inflammation
D. Providing a barrier layer to protect the surrounding skin
6. Topical corticosteroids are used to treat several disorders. Topical corticosteroids are contraindicated for treatment of which of the following conditions?
a. Psoriasis c. Eczema
b. Contact dermatitis d. Rosacea
7. A topical corticosteroid may be used to treat facial eczema. What instruction must be given to a patient for whom a topical corticosteroid is prescribed for treatment of facial eczema?
a. “Be careful not to get any of the medication in your eyes.”
b. “Stay out of strong sunlight while using the medication.”
c. “Put a thin layer of medication on once a day just before you go to bed for the
night.”
d. “Check before you use it that the medication is labeled fluorinated.”
8. Group I topical corticosteroids may cause adverse reactions. A patient who is being treated with a group I topical corticosteroid must be closely monitored for
a. increased hepatic enzymes. c. epithelial keratopathy.
b. HPA suppression. d. bone marrow depression.
9. Treatment with gentamicin (Garamycin) may present disadvantages for the patient. A renal patient’s use of the drug may lead to
a. deterioration of the immune system.
b. risk of liver damage secondary to systemic absorption.
c. occurrence of secondary retroviral infection.
d. ototoxicity.
9. The topical antiviral drug acyclovir (Zovirax) is used to treat several different conditions. Which of the following conditions is an unlabeled use for acyclovir (Zovirax)?
a. Herpes genitalis c. Herpes labialis
b. Herpes simplex virus types I and II d. Epstein-Barr virus
10. Lindane (Kwell, Scabene) is used to treat several different disorders. For which disorder is the use of lindane (Kwell, Scabene) contraindicated?
a. Pediculosis pubis c. Scabies
b. Sarcoptes scabiei d. Seizures
15. Scabies treatment for a 4-year-old child includes a prescription for:
A. Permethrin 5% cream applied from the neck down
B. Pyrethrin lotion
C. Lindane 1% shampoo
D. All of the above
16. Vanessa has been diagnosed with scabies. Her education would include:
A. She should apply the scabies treatment cream for an hour and wash it off
B. Scabies may need to be retreated in a week after initial treatment
C. All members of the household and close personal contacts should be treated
D. Malathion is flammable and she should take care until the solution dries
17. Catherine has head lice and her mother is asking about what products are available that are not neurotoxic. The only non-neurotoxin head lice treatment is:
A. Permethrin 1% (Nix)
B. Lindane shampoo
C. Malathion (Ovide)
D. Benzoyl alcohol (Ulesfia)
Chapter 12. Fungal Infections of the Skin
MULTIPLE CHOICE
1. A nurse is caring for a patient who is on amphotericin B. On morning rounds the patient reports weakness, numbness, and a tingling sensation in his feet. What would be a priority action by the nurse?
A. Encourage the patient to increase fluid intake. C. Keep the bed in a low position and the side rails up at all times.
B. Use strict aseptic technique for drug administration D. Reduce the drug dosage.
2. A nurse is monitoring the fluid input and output of a 26-year-old woman who is on amphotericin B. Which of the following would the nurse report immediately to the physician?
A. Orange-colored urine C. A high concentration of the drug in the urine
B. Urine output above 500 mL/g of the drug administered D. Serum creatinine level of 3.5 mg/dL
3. The nurse is assessing a patient who is about to receive antifungal drug therapy. Which condition, if found in the patient, would be of most concern?
A. Diabetes mellitus
B. Liver disease
C. Pulmonary disease
D. Bleeding disorders
4. The nurse is preparing an infusion of amphotericin B for a patient who has a severe fungal infection. Which intervention is appropriate regarding the potential adverse effects of amphotericin B?
A. Discontinuing the infusion immediately if fever, chills, or nausea occur
B. Gradually increasing the infusion rate until the expected adverse effects occur
C. If fever, chills, or nausea occur during the infusion, administering medications to
treat the symptoms
D. Before beginning the infusion, administering an antipyretic and an antiemetic drug
5. The nurse is administering one of the lipid formulations of amphotericin B. When giving this drug, which concept is important to remember?
A. The lipid formulations may be given in oral form.
B. The doses are much lower than the doses of the older drugs.
C. The lipid formulations are associated with fewer adverse effects than the older
drugs.
D. There is no difference in cost between the newer and older forms.
6. A patient is infected by invasive aspergillosis, and the medical history reveals that the patient has not been able to tolerate several antifungal drugs. The nurse anticipates an order for which medication to treat this infection?
A. fluconazole (Diflucan)
B. micafungin (Mycamine)
C. caspofungin (Cancidas)
D. nystatin (Mycostatin)
7. During therapy with amphotericin B, the nurse will monitor the patient for known adverse effects that would be reflected by which laboratory result?
A. Serum potassium level of 2.7 mEq/L
B. Serum potassium level of 5.8 mEq/L
C. White blood cell count of 7000 cells/mm3
D. Platelet count of 300,000 per microliter
8. A patient has received a prescription for a 2-week course of antifungal suppositories for a vaginal yeast infection. She asks the nurse if there is an alternative to this medication, saying, “I don’t want to do this for 2 weeks!” Which is a possibility in this situation?
A. A single dose of a vaginal antifungal cream
B. A one-time infusion of amphotericin B
C. A single dose of a fluconazole (Diflucan) oral tablet
D. There is no better alternative to the suppositories.
9. Dwayne has classic tinea capitis. Treatment for tinea on the scalp is:
A. Miconazole cream rubbed in well for 4 weeks
B. Oral griseofulvin for 6 to 8 weeks
C. Ketoconazole shampoo daily for 6 weeks
D. Ciclopirox cream daily for 4 weeks
10. Nicolas is a football player who presents to clinic with athlete’s foot. Patients with tinea pedis may be treated with:
A. OTC miconazole cream for 4 weeks
B. Oral ketoconazole for 6 weeks
C. Mupirocin ointment for 2 weeks
D. Nystatin cream for 2 weeks
11. Jim presents with fungal infection of two of his toenails (onychomycosis). Treatment for fungal infections of the nail includes:
A. Miconazole cream
B. Ketoconazole cream
C. Oral griseofulvin
D. Mupirocin cream
Chapter 13 Viral Infections of the Skin
MULTIPLE CHOICE
1. A patient who is diagnosed with shingles is taking topical acyclovir, and the nurse is providing instructions about adverse effects. The nurse will discuss which adverse effects of topical acyclovir therapy?
A. Insomnia and nervousness
B. Temporary swelling and rash
C. Transient burning when applied
D. This medication has no adverse effects.
2. The nurse is administering intravenous acyclovir (Zovirax) to a patient with a viral infection. Which administration technique is correct?
A. Infuse intravenous acyclovir slowly, over at least 1 hour.
B. Infuse intravenous acyclovir by rapid bolus.
C. Refrigerate intravenous acyclovir.
D. Restrict oral fluids during intravenous acyclovir therapy.
3. A patient is receiving cidofovir (Vistide) as part of treatment for a viral infection, and the nurse is preparing to administer probenecid, which is also ordered. Which is the rationale for administering probenecid along with the cidofovir treatment?
A. Probenecid has a synergistic effect when given with cidofovir, thus making the
antiviral medication more effective.
B. The probenecid also prevents replication of the virus.
C. Concurrent drug therapy with probenecid reduces the nephrotoxicity of the
cidofovir.
D. The probenecid reduces the adverse gastrointestinal effects of the cidofovir.
4. Instructions for applying a topical antibiotic or antiviral ointment include:
A. Apply thickly to the infected area, spreading the medication well past the borders
of the infection
B. If the rash worsens, apply a thicker layer of medication to settle down the infection
C. Wash hands before and after application of topical antimicrobials
D. None of the above
5. When prescribing topical penciclovir (Denavir) for the treatment of herpes labialis (cold sores) patient education would include:
A. Spread penciclovir liberally all over lips and area surrounding lips
B. Penciclovir therapy is started at the first sign of cold sore outbreak
C. Skin irritation is normal with penciclovir and it should resolve
D. The penciclovir should be used a minimum of 2 weeks to prevent recurrence
MULTIPLE RESPONSE
1. A patient who is diagnosed with genital herpes is taking topical acyclovir. The nurse will provide which teaching for this patient? (Select all that apply.)
A. “Be sure to wash your hands thoroughly before and after applying this medicine.”
B. “Apply this ointment until the lesion stops hurting.”
C. “Use a clean glove when applying this ointment.”
D. “If your partner develops these lesions, then he can also use the medication.”
E. “You will need to avoid touching the area around your eyes.”
F. “You will have to practice abstinence when these lesions are active.”
Chapter 14 Bacterial Infections of the Skin
Test Bank
MULTIPLE CHOICE
1. When reviewing the allergy history of a patient, the nurse notes that the patient is allergic to penicillin. Based on this finding, the nurse would question an order for which class of antibiotics?
a. Tetracyclines
b. Sulfonamides
c. Cephalosporins
d. Quinolones
2. The nurse is providing teaching to a patient taking an oral tetracycline antibiotic. Which statement by the nurse is correct?
a. “Avoid direct sunlight and tanning beds while on this medication.”
b. “Milk and cheese products result in increased levels of tetracycline.”
c. “Antacids taken with the medication help to reduce gastrointestinal distress.”
d. “Take the medication until you are feeling better.”
3. When reviewing the medication orders for a patient who is taking penicillin, the nurse notes that the patient is also taking the oral anticoagulant warfarin (Coumadin). What possible effect may occur as the result of an interaction between these drugs?
a. The penicillin will cause an enhanced anticoagulant effect of the warfarin.
b. The penicillin will cause the anticoagulant effect of the warfarin to decrease.
c. The warfarin will reduce the antiinfective action of the penicillin.
d. The warfarin will increase the effectiveness of the penicillin.
4. A patient is receiving his third intravenous dose of a penicillin drug. He calls the nurse to report that he is feeling “anxious” and is having trouble breathing. What will the nurse do first?
a. Notify the prescriber.
b. Take the patient’s vital signs.
c. Stop the antibiotic infusion.
d. Check for allergies.
5. During drug therapy with a tetracycline antibiotic, a patient complains of some nausea and decreased appetite. Which statement is the nurse’s best advice to the patient?
a. “Take it with cheese and crackers or yogurt.”
b. “Take each dose with a glass of milk.”
c. “Take an antacid with each dose as needed.”
d. “Drink a full glass of water with each dose.”
6. The nurse is monitoring a patient who has been on antibiotic therapy for 2 weeks. Today the patient tells the nurse that he has had watery diarrhea since the day before and is having abdominal cramps. His oral temperature is 101° F (38.3° C). Based on these findings, which conclusion will the nurse draw?
a. The patient’s original infection has not responded to the antibiotic therapy.
b. The patient is showing typical adverse effects of antibiotic therapy.
c. The patient needs to be tested for Clostridium difficile infection.
d. The patient will need to take a different antibiotic.
7. The nurse is monitoring for therapeutic results of antibiotic therapy in a patient with an infection. Which laboratory value would indicate therapeutic effectiveness of this therapy?
a. Increased red blood cell count
b. Increased hemoglobin level
c. Decreased white blood cell count
d. Decreased platelet count
8. The nurse is reviewing the sputum culture results of a patient with pneumonia and notes that the patient has a gram-positive infection. Which generation of cephalosporin is most appropriate for this type of infection?
a. First-generation
b. Second-generation
c. Third-generation
d. Fourth-generation
9. A patient will be having oral surgery and has received an antibiotic to take for 1 week before the surgery. The nurse knows that this is an example of which type of therapy?
a. Empirical
b. Prophylactic
c. Definitive
d. Resistance
10. During drug therapy for pneumonia, a female patient develops a vaginal superinfection. The nurse explains that this infection is caused by
a. large doses of antibiotics that kill normal flora.
b. the infection spreading from her lungs to the new site of infection.
c. resistance of the pneumonia-causing bacteria to the drugs.
d. an allergic reaction to the antibiotics.
11. The nurse is preparing to use an antiseptic. Which statement is correct regarding how antiseptics differ from disinfectants?
a. Antiseptics are used to sterilize surgical equipment.
b. Disinfectants are used as preoperative skin preparation.
c. Antiseptics are used only on living tissue to kill microorganisms.
d. Disinfectants are used only on nonliving objects to destroy organisms.
12. A patient with a long-term intravenous catheter is going home. The nurse knows that if he is allergic to seafood, which antiseptic agent is contraindicated?
a. chlorhexidine gluconate (Hibiclens)
b. hydrogen peroxide
c. povidone-iodine (Betadine)
d. isopropyl alcohol
MULTIPLE RESPONSE
1. During antibiotic therapy, the nurse will monitor closely for signs and symptoms of a hypersensitivity reaction. Which of these assessment findings may be an indication of a hypersensitivity reaction? (Select all that apply.)
a. Wheezing
b. Diarrhea
c. Shortness of breath
d. Swelling of the tongue
e. Itching
f. Black, hairy tongue
2. The nurse is reviewing the medication history of a patient who will be taking a sulfonamide antibiotic. During sulfonamide therapy, a significant drug interaction may occur with which of these drugs or drug classes? (Select all that apply.)
a. Opioids
b. Oral contraceptives
c. Sulfonylureas
d. Antihistamines
e. phenytoin (Dilantin)
f. warfarin (Coumadin)
OTHER
1. A patient will be receiving amoxicillin suspension 300 mg via a gastrostomy tube every 8 hours. The medication comes in a bottle that contains 400 mg/5 mL. How many milliliters will the nurse administer with each dose? (Record answer using one decimal place.)
2. A patient will be receiving penicillin G potassium, 12 million units daily in divided doses every 4 hours IVPB. How many units will the patient receive for each dose?
Chapter 15. Psoriasis
MULTIPLE CHOICE
1. Appropriate initial treatment for psoriasis would be:
A. An immunomodulator (Protopic or Elidel)
B. Wet soaks with Burrow’s or Domeboro solution
C. Intermittent therapy with intermediate potency topical corticosteroids
D. Anthralin (Drithocreme)
2. Patient education when prescribing the Vitamin D3 derivative calcipotriene for psoriasis includes:
A. Apply thickly to affected psoriatic areas two to three times a day
B. A maximum of 100 grams per week may be applied
C. Do not use calcipotriene in combination with their topical corticosteroids
D. Calcipotriene may be augmented with the use of coal tar products
3. Whart is the peak onset age of Psoriasis
A. 16-22 C. 57-60
B. 30-34 D. Both A and C
4. A patient with psoriasis needs to apply a lubricating lotion to a psoriatic plaque. The health provider recommends which of the following types of substances?
A. Alcohol C. Emollient
B. Astringent D. Antiseptic
5. Patients who are treated with greater than 100 grams per week of topical calcipotriene for psoriasis need to be monitored for:
A. High vitamin D levels
B. Hyperkalemia
C. Hypercalcemia
D. Hyperuricemia
2. Jesse is prescribed tazarotene for his psoriasis. Patient education regarding topical tazarotene includes:
A. Tazarotene is applied in a thin film to the psoriasis plaque lesions
B. Apply liberally to all psoriatic lesions
C. Apply tazarotene to non-affected areas to prevent breakout
D. Tazarotene may cause hypercalcemia if overused
Chapter 16. Acne Vulgaris and Rosacea
MULTIPLE CHOICE
1. Mild acne may be initially treated with:
A. Topical combined antibiotic
B. Minocycline
C. Topical retinoid
D. OTC benzoyl peroxide
2. Tobie presents to clinic with moderate acne. He has been using OTC benzoyl peroxide at home with minimal improvement. A topical antibiotic (clindamycin) and a topical retinoid adapalene (Differin) are prescribed. Education of Tobie would include:
A. He should see an improvement in his acne within the first 2 weeks of treatment
B. If there is no response in a week, double the daily application of adapalene
(Differin)
C. He may see an initial worsening of his acne that will improve in 6 to 8 weeks
D. Adapalene may cause bleaching of clothing
3. Josie has severe cystic acne and is requesting treatment with Accutane. The appropriate treatment for her would be:
A. Order a pregnancy test and if it is negative prescribe the isotretinoin (Accutane)
B. Order Accutane after educating her on the adverse effects
C. Recommend she try oral antibiotics (minocycline)
D. Refer her to a dermatologist for treatment
4. The most cost-effective treatment for two or three impetigo lesions on the face is:
A. Mupirocin ointment
B. Retapamulin (Altabax) ointment
C. Topical clindamycin solution
D. Oral amoxicillin/clavulanate (Augmentin)
5. Rodesa usually starts in this part of a person’s lifespan
A. Adolescant C. Teen
B. Midlife D. Todler
1
6. Initial drug therapy choices should include a
A. topical agent. C. isotrentinion
B. oral antibiotics D. benzoyl peroxide
Chapter 17 Ophthalmic Disorders
MULTIPLE CHOICE
1. The Centers for Disease Control recommends all newborn infants receive prophylactic administration of within 1 hour of birth.
A. Gentamicin ophthalmic ointment
B. Ciprofloxacin ophthalmic drops
C. Erythromycin oral suspension
D. Erythromycin ophthalmic ointment
2. Conjunctivitis in a child that is accompanied by acute otitis media is treated with:
A. Sulfacetamide 10% ophthalmic solution (Bleph-10)
B. Bacitracin/polymyxin B (Polysporin) ophthalmic drops
C. Ciprofloxacin (Ciloxan) ophthalmic drops
D. High-dose oral amoxicillin
3. Twenty-year-old Annie comes to clinic complaining of copious yellow-green eye discharge. Gram stain indicates she most likely has gonococcal conjunctivitis. While awaiting the culture results, the plan of care should be:
A. None; wait for the culture results to determine the course of treatment
B. Ciprofloxacin (Ciloxan) ophthalmic drops
C. IM ceftriaxone
D. High-dose oral amoxicillin
4. Education of women who are being treated with ophthalmic antibiotics for conjunctivitis includes:
A. Throwing away eye makeup and purchasing new
B. Redness and intense burning is normal with ophthalmic antibiotics
C. When applying eye ointment, set the tip of the tube on the lower lid and squeeze in
inch
D. Use a cotton swab to apply ointment, spreading the ointment all over the lid and in the conjunctival sac
5. Sadie was prescribed betaxolol ophthalmic drops by her ophthalmologist to treat her glaucoma. Oral beta blockers should be avoided in patients who use ophthalmic beta blockers due to:
A. There may be an antagonistic reaction between the two
B. The additive effects may include bradycardia
C. They may potentiate each other and cause respiratory depression
D. The additive effects may cause metabolic acidosis
6. David presents to clinic with symptoms of allergic conjunctivitis. He is prescribed cromolyn sodium (Opticrom) eye drops. The education regarding using cromolyn eye drops includes:
A. He should not wear his soft contacts while using the cromolyn eye drops
B. Cromolyn drops are instilled once a day to prevent allergy symptoms
C. Long-term use may cause glaucoma
D. He may experience bradycardia as an adverse effect
7. Choose the type of ophthalmic medication that can result in glaucoma, cataracts, or secondary infection.
A. Sympathomimetics C. Anesthetics
B. Antivirals D. Steroids
8. Prescription of timolol maleate can result in several serious adverse reactions. Select the condition that is considered to be a common side effect of treatment with timolol maleate.
A. Chronic heart failure C. Diabetes
B. Bradycardia D. Blurred vision
9. Which situation shows appropriate use of an ophthalmic anesthetic for a patient with eye pain?
A. Presence of a foreign object in the eye
B. Facilitation of examination of the eye
C. Pain that is worsened by light
D. Underlying problem of a herpes simplex infection
10. The patient is suffering from glaucoma and is scheduled to begin treatment with carbachol (Carboptic). The health care provider knows to monitor the patient closely for evidence of which effect of the drug?
A. Dilation of the iridic sphincter C. Mydriasis
B. Increased outflow of aqueous humor D. Vasoconstriction of collecting
channels
11. The patient is being treated with the drug pilocarpine (Pilocar). He complains of eye irritation. The most appropriate response of the health care provider is:
A. This could be symptomatic of retinal detachment.
B. This is an unexpected, idiosyncratic response to the medication.
C. This is an expected adverse reaction to the medication.
D. This could be symptomatic of iridic cysts.
12. As the patient continues to undergo treatment with pilocarpine (Pilocar), he begins to experience itching of the eye. The most appropriate response of the health care provider is:
A. This could be symptomatic of pinpoint hemorrhaging within the eye.
B. This is an expected adverse reaction to the medication, and treatment to relieve this
symptom will be initiated.
C. This is an unexpected, idiosyncratic response to the medication; the patient must
be switched to a different drug.
D. This could be symptomatic of retinal damage.
13. A patient with an eye injury requires an ocular examination to detect the presence of a foreign body. Which drug would a health care provider expect to be of most use in this examination?
A. Rose bengal C. Fluorexon
B. Fluorocaine D. Isoflurophate
14. Which drug would a health care provider recommend to a patient who complains of dry eyes?
A. Proparacaine (Alcaine) C. Polyvinyl alcohol (Hypotears)
B. Tetracaine (Pontocaine) D. Naphazoline (AK-Con)
Chapter 17 Ophthalmic Disorders
MULTIPLE CHOICE
1. The Centers for Disease Control recommends all newborn infants receive prophylactic administration of within 1 hour of birth.
A. Gentamicin ophthalmic ointment
B. Ciprofloxacin ophthalmic drops
C. Erythromycin oral suspension
D. Erythromycin ophthalmic ointment
2. Conjunctivitis in a child that is accompanied by acute otitis media is treated with:
A. Sulfacetamide 10% ophthalmic solution (Bleph-10)
B. Bacitracin/polymyxin B (Polysporin) ophthalmic drops
C. Ciprofloxacin (Ciloxan) ophthalmic drops
D. High-dose oral amoxicillin
3. Twenty-year-old Annie comes to clinic complaining of copious yellow-green eye discharge. Gram stain indicates she most likely has gonococcal conjunctivitis. While awaiting the culture results, the plan of care should be:
A. None; wait for the culture results to determine the course of treatment
B. Ciprofloxacin (Ciloxan) ophthalmic drops
C. IM ceftriaxone
D. High-dose oral amoxicillin
4. Education of women who are being treated with ophthalmic antibiotics for conjunctivitis includes:
A. Throwing away eye makeup and purchasing new
B. Redness and intense burning is normal with ophthalmic antibiotics
C. When applying eye ointment, set the tip of the tube on the lower lid and squeeze in
inch
D. Use a cotton swab to apply ointment, spreading the ointment all over the lid and in the conjunctival sac
5. Sadie was prescribed betaxolol ophthalmic drops by her ophthalmologist to treat her glaucoma. Oral beta blockers should be avoided in patients who use ophthalmic beta blockers due to:
A. There may be an antagonistic reaction between the two
B. The additive effects may include bradycardia
C. They may potentiate each other and cause respiratory depression
D. The additive effects may cause metabolic acidosis
6. David presents to clinic with symptoms of allergic conjunctivitis. He is prescribed cromolyn sodium (Opticrom) eye drops. The education regarding using cromolyn eye drops includes:
A. He should not wear his soft contacts while using the cromolyn eye drops
B. Cromolyn drops are instilled once a day to prevent allergy symptoms
C. Long-term use may cause glaucoma
D. He may experience bradycardia as an adverse effect
7. Choose the type of ophthalmic medication that can result in glaucoma, cataracts, or secondary infection.
A. Sympathomimetics C. Anesthetics
B. Antivirals D. Steroids
8. Prescription of timolol maleate can result in several serious adverse reactions. Select the condition that is considered to be a common side effect of treatment with timolol maleate.
A. Chronic heart failure C. Diabetes
B. Bradycardia D. Blurred vision
9. Which situation shows appropriate use of an ophthalmic anesthetic for a patient with eye pain?
A. Presence of a foreign object in the eye
B. Facilitation of examination of the eye
C. Pain that is worsened by light
D. Underlying problem of a herpes simplex infection
10. The patient is suffering from glaucoma and is scheduled to begin treatment with carbachol (Carboptic). The health care provider knows to monitor the patient closely for evidence of which effect of the drug?
A. Dilation of the iridic sphincter C. Mydriasis
B. Increased outflow of aqueous humor D. Vasoconstriction of collecting
channels
11. The patient is being treated with the drug pilocarpine (Pilocar). He complains of eye irritation. The most appropriate response of the health care provider is:
A. This could be symptomatic of retinal detachment.
B. This is an unexpected, idiosyncratic response to the medication.
C. This is an expected adverse reaction to the medication.
D. This could be symptomatic of iridic cysts.
12. As the patient continues to undergo treatment with pilocarpine (Pilocar), he begins to experience itching of the eye. The most appropriate response of the health care provider is:
A. This could be symptomatic of pinpoint hemorrhaging within the eye.
B. This is an expected adverse reaction to the medication, and treatment to relieve this
symptom will be initiated.
C. This is an unexpected, idiosyncratic response to the medication; the patient must
be switched to a different drug.
D. This could be symptomatic of retinal damage.
13. A patient with an eye injury requires an ocular examination to detect the presence of a foreign body. Which drug would a health care provider expect to be of most use in this examination?
A. Rose bengal C. Fluorexon
B. Fluorocaine D. Isoflurophate
14. Which drug would a health care provider recommend to a patient who complains of dry eyes?
A. Proparacaine (Alcaine) C. Polyvinyl alcohol (Hypotears)
B. Tetracaine (Pontocaine) D. Naphazoline (AK-Con)
Chapter 19. Hypertension
MULTIPLE CHOICE
1. At which stage/classification of hypertension should drug therapy be instituted according to the JNC-7 Report?
A. Prehypertension
B. Stage 1
C. Stage 2
D. Any stage where the blood pressure is greater than 120/80 mm Hg
2. Because primary hypertension has no identifiable cause, treatment is based on interfering with the physiological mechanisms that regulate blood pressure. Thiazide diuretics treat hypertension because they:
A. Increase renin secretion
B. Decrease the production of aldosterone
C. Deplete body sodium and reduce fluid volume
D. Decrease blood viscosity
3. Because of its action on various body systems, the patient taking a thiazide or loop diuretic may also need to receive:
A. Potassium supplements
B. Calcium supplements
C. Magnesium supplements
D. Phosphates supplements
4. All patients with hypertension benefit from diuretic therapy, but those who benefit the most are:
A. Those with orthostatic hypertension
B. African Americans
C. Those with stable angina
D. Diabetics
5. Beta blockers treat hypertension because they:
A. Reduce peripheral resistance
B. Vasoconstrict coronary arteries
C. Reduce norepinephrine
D. Reduce angiotensin II production
6. Which of the following disease processes could be made worse by taking a nonselective beta blocker?
A. Asthma
B. Diabetes
C. Both might worsen
D. Beta blockade does not affect these disorders
7. Disease states in addition to hypertension in which beta blockade is a compelling indication for the use of beta blockers include:
A. Heart failure
B. Angina
C. Myocardial infarction
D. Dyslipidemia
8. ACE inhibitors treat hypertension because they:
A. Reduce sodium and water retention
B. Decrease vasoconstriction
C. Increase vasodilation
D. All of the above
9. Compelling indications for an ACE inhibitor as treatment for hypertension based on clinical trials includes:
A. Pregnancy
B. Renal parenchymal disease
C. Stable angina
D. Dyslipidemia
10. An ACE inhibitor and what other class of drug may reduce proteinuria in patients with diabetes better than either drug alone?
A. Beta blockers
B. Diuretics
C. Nondihydropyridine calcium channel blockers
D. Angiotensin II receptor blockers
11. If not chosen as the first drug in hypertension treatment, which drug class should be added as second step because it will enhance the effects of most other agents?
A. ACE inhibitors
B. Beta blockers
C. Calcium channel blockers
D. Diuretics
12. Treatment costs are important for patients with hypertension. Which of the following statements about cost is NOT true?
A. Hypertension is a chronic disease where patients may be taking drugs for a long
time.
B. Most patients will require more than one drug to treat the hypertension.
C. The cost includes the price of any routine or special lab tests that a specific drug
may require.
D. Few antihypertensive drugs come in generic formulations.
13. Caffeine, exercise, and smoking should be avoided for at least how long before blood pressure measurement?
A. 15 minutes
B. 30 minutes
C. 60 minutes
D. 90 minutes
14. Blood pressure checks in children:
A. Should occur with their annual physical examinations after age 6
B. Require a blood pressure cuff that is one-third the diameter of the child’s arm
C. Should be done during every health-care visit after age 3
D. Require additional lab tests such as serum creatinine
15. Lack of adherence to blood pressure management is very common. Reasons for this lack of adherence include:
A. Lifestyle changes are difficult to achieve and maintain
B. Adverse drug reactions are common and often fall into the categories more
associated with nonadherence
C. Costs of drugs and monitoring with labs can be expensive
D. All of the above
16. Lifestyle modifications for patients with prehypertension or hypertension include:
A. Diet and increase exercise to achieve a BMI greater than 25
B. Drink 4 ounces of red wine at least once per week
C. Adopt the DASH diet
D. Increase potassium intake
Chapter 20. Hyperlipidemia
MULTIPLE CHOICE
1. The overall goal of treating hyperlipidemia is:
A. Maintain an LDL level of less than 160 mg/dL
B. To reduce atherogenesis
C. Lowering apo B, one of the apoliproteins
D. All of the above
2. When considering which cholesterol-lowering drug to prescribe which factor determines the type and intensity of treatment?
A. Total LDL
B. Fasting HDL
C. Coronary artery disease risk level
D. Fasting total cholesterol
3. First-line therapy for hyperlipidemia is:
A. Statins
B. Niacin
C. Lifestyle changes
D. Bile acid-binding resins
4. James is a 45 year old with an LDL level of 120 and normal triglycerides. Appropriate first- line therapy for James may include diet counseling, increased physical activity, and:
A. A statin
B. Niacin
C. Sterols
D. A fibric acid derivative
5. Joanne is a 60 year old with an LDL of 132 and a family history of coronary artery disease. She has already tried diet changes (increased fiber and plant sterols) to lower her LDL and after 6 months her LDL is slightly higher. The next step in her treatment would be:
A. A statin
B. Niacin
C. Sterols
D. A fibric acid derivative
6. Sharlene is a 65 year old who has been on a lipid-lowering diet and using plant sterol margarine daily for the past 3 months. Her LDL is 135 mg/dL. An appropriate treatment for her would be:
A. A statin
B. Niacin
C. A fibric acid derivative
D. Determined by her risk factors
7. Mike is a 47 year old who has been on standard dose atorvastatin for 3 months and his repeat LDL is 124 mg/dL. He is a smoker and has a strong family history of cardiovascular disease. His treatment plan would include reinforcing diet, exercise, plant sterol intake, and:
A. Increasing his dose of atorvastatin
B. Changing to another statin
C. Adding niacin to the treatment regimen
D. Adding a bile acid-binding resin
8. Phil is a 54-year-old male with multiple risk factors who has been on a high dose statin for 3 months to treat his high LDL level. His LDL is 135 mg/dL and his triglycerides are elevated. A reasonable change in therapy would be to:
A. Discontinue the statin and change to a fibric acid derivative
B. Discontinue the statin and change to ezetimibe
C. Continue the statin and add in ezetimibe
D. Refer him to a specialist in managing patients with recalcitrant hyperlipidemia
9. Scott is presenting for follow up on his lipid panel. He had elevated total cholesterol, triglycerides, and an LDL of 122 mg/dL. He has already implemented diet changes and increased physical activity. He has mildly elevated liver studies. An appropriate next step for therapy would be:
A. Atorvastatin (Lipitor)
B. Niacin (Niaspan)
C. Simvastatin and ezetimibe (Vytorin)
D. Gemfibrozil (Lopid)
10. Jamie is a 34-year-old pregnant woman with familial hyperlipidemia and elevated LDL levels. What is the appropriate treatment for a pregnant woman?
A. A statin
B. Niacin
C. Fibric acid derivative
D. Bile acid-binding resins
11. Han is a 48-year-old diabetic with hyperlipidemia and high triglycerides. His LDL is 112
mg/dL and he has not tolerated statins. He warrants a trial of a:
A. Sterol
B. Niacin
C. Fibric acid derivative
D. Bile acid-binding resin
12. Jose is a 12-year-old overweight child with a total cholesterol of 180 mg/dL and LDL of 125 mg/dL. Along with diet education and recommending increased physical activity, a treatment plan for Jose would include with a reevaluation in 6 months.
A. Statins
B. Niacin
C. Sterols
D. Bile acid-binding resins
13. Monitoring of a patient who is on a lipid-lowering drug includes:
A. Fasting total cholesterol every 6 months
B. Lipid profile with attention to serum LDL 6 to 8 weeks after starting therapy then
again in 6 weeks
C. Complete blood count, CRP, and ESR after 6 weeks of therapy
D. All of the above
14. Before starting therapy with a statin, the following baseline laboratory values should be evaluated:
A. Complete blood count
B. Liver function (ALT/AST) and CK
C. C-reactive protein
D. All of the above
15. When starting a patient on a statin, education would include:
A. If they stop the medication their lipid levels will return to pre-treatment levels
B. Medication is a supplement to diet therapy and exercise
C. If they have any muscle aches or pain, they should contact their provider
D. All of the above
Chapter 21. Angina
MULTIPLE CHOICE
1. Angina is produced by an imbalance between oxygen supply (MOS) and demand (MOD) in the myocardium. Which of the following drugs help to correct this imbalance by increasing MOS?
A. Calcium channel blockers
B. Beta blockers
C. ACE inhibitors
D. Aspirin
2. Not all chest pain is caused by myocardial ischemia. Non-cardiac causes of chest pain include:
A. Pulmonary embolism
B. Pneumonia
C. Gastroesophageal reflux
D. All of the above
3. The New York Heart Association and the Canadian Cardiovascular Society have described grading criteria for levels of angina. Angina that occurs with unusually strenuous activity or on walking or climbing stair after meals is:
A. Class I
B. Class II
C. Class III
D. Class IV
4. Patients at high risk for developing significant coronary heart disease are those with:
A. LDL values between 100 and 130
B. Systolic blood pressure between 120 and 130
C. Class III angina
D. Obesity
5. To reduce mortality, all patients with angina, regardless of Class, should be on:
A. Aspirin 81 to 325 mg/d
B. Nitroglycerin sublingually for chest pain
C. ACE inhibitors or ARBs
D. Digoxin
6. Patients who have angina, regardless of Class, who are also diabetic, should be on:
A. Nitrates
B. Beta blockers
C. ACE inhibitors
D. Calcium channel blockers
7. Management of all types and grades of angina includes the use of lifestyle modification to reduce risk factors. Which of these modifications are appropriate for which reason? Both the modification and the reason for it must be true for the answer to be correct.
A. Lose at least 10 pounds of body weight. Excessive weight increases cardiac
workload.
B. Reduce sodium intake to no more than 2,400 mg of sodium. Sodium increases
blood volume and cardiac workload.
C. Increase potassium intake to at least 100 mEq/d. The heart needs higher levels of
potassium to improve contractility and oxygen supply.
D. Intake a moderate amount of alcohol. Moderate intake has been shown by research
to improve cardiac function.
8. Nitrates are especially helpful for patients with angina who also have:
A. Heart failure
B. Hypertension
C. Both A and B
D. Neither A nor B
9. Beta blockers are especially helpful for patients with exertional angina who also have:
A. Arrhythmias
B. Hypothyroidism
C. Hyperlipidemia
D. Atherosclerosis
10. Rapid-acting nitrates are important for all angina patients. Which of the following are true statements about their use?
A. These drugs are useful for immediate symptom relief when the patient is certain it
is angina.
B. The dose is one sublingual tablet or spray every 5 minutes until the chest pain goes
away.
C. Take one nitroglycerine tablet or spray at the first sign of angina; repeat every 5 minutes for no more than three doses. If chest pain is still not relieved, go to the
hospital.
D. All of the above
11. Isosorbide dinitrate is a long-acting nitrate given BID. The schedule for administration is 7 AM and 2 PM because:
A. Long-acting forms have a higher risk for toxicity
B. Orthostatic hypotension is a common adverse effect
C. It must be taken with milk or food
D. Nitrate tolerance can develop
12. Combinations of a long-acting nitrate and a beta blocker are especially effective in treating angina because:
A. Nitrates increase MOS and beta blockers increase MOD
B. Their additive affects permit lower doses of both drugs and their adverse reactions
cancel each other out.
C. They address the pathology of patients with exertional angina who have fixed
atherosclerotic coronary heart disease
D. All of the above
13. Although they are often described as helpful in the lay media, which of the following therapies have not been shown to be helpful based on clinical evidence?
A. Vitamins C and E
B. Co-enzyme Q10
C. Folic acid
D. All of the above
14. Drug choices to treat angina in older adults differ from those of younger adults only in:
A. Consideration of risk factors for diseases associated with and increased in aging
B. The placement of drug therapy as a treatment choice before lifestyle changes are
tried
C. The need for at least three drugs in the treatment regimen because of the
complexity of angina in the older adult
D. Those with higher risk for silent myocardial infarction (MI)
15. Which of the following drugs has been associated with increased risk for myocardial infarction (MI) in women?
A. Aspirin
B. Beta blockers
C. Estrogen replacement
D. Lipid-lowering agents
16. Cost of antianginal drug therapy should be considered in drug selection because of all of the following EXCEPT:
A. Patients often require multiple drugs
B. A large number of angina patients are older adults on fixed incomes
C. Generic formulations may be cheaper but are rarely bioequivalent
D. Lack of drug selectivity may result in increased adverse reactions
17. Five questions should be asked during the follow up of any angina patient. They include:
A. Have there been any changes in lab data since the last visit?
B. Has the level of physical activity associated with the angina changed since the last
visit?
C. Have new risk factors come to light in producing the angina?
D. Is the patient filling prescriptions and taking the drugs as prescribed?
18. Situations that suggest referral to a specialist is appropriate include:
A. When chronic stable angina becomes unpredictable in its characteristics and
precipitating factors
B. When a post-MI patient develops new-onset angina
C. When standard therapy is not successful in improving exercise tolerance or
reducing the incidence of angina
D. All of the above
Chapter 22. Heart Failure
MULTIPLE CHOICE
1. ACE inhibitors are a central part of the treatment of heart failure because they have more than one action to address the pathological changes in this disorder. Which of the following pathological changes in heart failure is NOT addressed by ACE inhibitors?
A. Changes in the structure of the left ventricle so that it dilates, hypertrophies, and
uses energy less efficiently.
B. Reduced formation of cross-bridges so that contractile force decreases.
C. Activation of the sympathetic nervous system that increases heart rate and preload.
D. Decreased renal blood flow that decreases oxygen supply to the kidneys.
2. One of the three types of heart failure involves systolic dysfunction. Potential causes of this most common form of heart failure include:
A. Myocardial ischemia and injury secondary to myocardial infarction
B. Inadequate relaxation and loss of muscle fiber secondary to valvular dysfunction
C. Increased demands of the heart beyond its ability to adapt secondary to anemia
D. Slower filling rate and elevated systolic pressures secondary to uncontrolled
hypertension
3. The American Heart Association and the American College of Cardiology have devised a classification system for heart failure that can be used to direct treatment. Patients with symptoms and underlying disease are classified as:
A. Stage A
B. Stage B
C. Stage C
D. Stage D
4. Diagnosis of heart failure cannot be made by symptoms alone since many disorders share the same symptoms. The most specific and sensitive diagnostic test for heart failure is:
A. Chest x-rays that show cephalization and measure heart size
B. Two-dimensional echocardiograms that identify structural anomalies and cardiac
dysfunction
C. Complete blood count, BUN, and serum electrolytes that facilitate staging for end-
organ damage
D. Measurement of brain natriuretic peptide to distinguish between systolic and
diastolic dysfunction
5. Treatments for heart failure, including drug therapy, are based on the stages developed by the ACC/AHA. Stage A patients are treated with:
A. Drugs for hypertension and hyperlipidemia, if they exist
B. Lifestyle management including diet, exercise, and smoking cessation only
C. ACE inhibitors to directly affect the heart failure only
D. No drugs are used in this early stage
6. Class I recommendations for Stage A heart failure include:
A. Aerobic exercise within tolerance levels to prevent the development of heart
failure
B. Reduction of sodium intake to less than 2,000 mg/day to prevent fluid retention
C. Beta blockers for all patients regardless of cardiac history
D. Treatment of thyroid disorders, especially if they are associated with
tachyarrhythmias
7. Stage B patients should have beta blockers added to their heart failure treatment regimen when:
A. They have an ejection fraction less than 40%
B. They have had a recent MI
C. Both A and B
D. Neither A nor B
8. Increased life expectancy for patients with heart failure has been associated with the use of:
A. ACE inhibitors, especially when started early in the disease process
B. All beta blockers regardless of selectivity
C. Thiazide and Loop diuretics
D. Cardiac glycosides
9. Stage C patients usually require a combination of three to four drugs to manage their heart failure. In addition to ACE inhibitors and beta blockers, diuretics may be added. Which of the following statements about diuretics is NOT true?
A. Diuretics reduce preload associated with fluid retention.
B. Diuretics can be used earlier than Stage C when the goal is control of hypertension.
C. Diuretics may produce problems with electrolyte imbalances and abnormal glucose
and lipid metabolism.
D. Diuretics from the potassium-sparing class should be used when using an ARB.
10. Digoxin has a very limited role in treatment of heart failure. It is used mainly for patients with:
A. Ejection fractions above 40%
B. An audible S3
C. Mitral stenosis as a primary cause for heart failure
D. Renal insufficiency
11. Which of the following classes of drugs is contraindicated in heart failure?
A. Nitrates
B. Long-acting dihydropyridines
C. Calcium channel blockers
D. Alpha-beta blockers
12. Heart failure is a leading cause of death and hospitalization in older adults (greater than 65 years old). The drug of choice for this population is:
A. Aldosterone antagonists
B. Eplerenone
C. ACE inhibitors
D. ARBs
13. ACE inhibitors are contraindicated in pregnancy. While treatment of heart failure during pregnancy is best done by a specialist, which of the following drug classes are considered to be safe, at least in the later parts of pregnancy?
A. Diuretics
B. ARBs
C. Beta blockers
D. Nitrates
14. Heart failure is a chronic condition that can be adequately managed in primary care. However, consultation with or referral to a cardiologist is appropriate when:
A. Symptoms markedly worsen or the patient becomes hypotensive and has syncope
B. There is evidence of progressive renal insufficiency or failure
C. The patient remains symptomatic on optimal doses of an ACE inhibitor, a beta
blocker, and a diuretic
D. Any of the above
Chapter 23. Dysrhythmias
MULTIPLE CHOICE
1. Which of the following cardiac arrhythmias would not be amenable to treatment with digoxin (Lanoxin)?
A. Atrial fibrillation C. Atrial flutter
B. Premature ventricular contractions D. Paroxysmal atrial tachycardia
2. Despite good blood pressure control, a NP might change a patient’s drug from an ACEI to an angiotensin II receptor blocker (ARB) because the ARB:
A. Is stronger than the ACEI
B. Does not produce a dry, hacky cough
C. Has no effect on the renal system
D. Reduces sodium and water retention
3. ACE inhibitors are useful in a variety of disorders. Which of the following statements are true about both its usefulness in the disorder and the reason for its use?
A. Stable angina because it decreases the thickening of vascular walls to decreased
MOD.
B. Heart failure because it reduces remodeling of injured myocardial tissues.
C. Both A and B are true and the reasons are correct
D. Both A and B are true but the reasons are wrong
E. Neither A nor B are true
4. Jacob has hypertension for which a calcium channel blocker has been prescribed. This drug helps control blood pressure because it:
A. Decreases the amount of calcium inside the cell
B. Reduces stroke volume
C. Increases the activity of the Na+/K+/ATPase pump indirectly
D. Decreases heart rate
5. Which of the following adverse effects may occur due to a dihydropyridine-type calcium channel blocker?
A. Bradycardia
B. Hepatic impairment
C. Increased contractility
D. Edema of the hands and feet
6. Patient teaching related to amlodipine includes:
A. Increase calcium intake to prevent osteoporosis from calcium blockade.
B. Do not crush the tablet; it must be given in liquid form if the patient has trouble
swallowing it.
C. Avoid grapefruit juice as it affects the metabolism of this drug.
D. Rise slowly from a supine position to reduce orthostatic hypotension.
7. Larry has heart failure which is being treated with digoxin because it exhibits:
A. Negative inotropism
B. Positive chronotropism
C. Both A and B
D. Neither A nor B
8. Serum digoxin levels are monitored for potential toxicity. Monitoring should occur:
A. Within 6 hours of the last dose
B. Because a reference point is needed in adjusting a dose
C. After three half-lives from the starting of the drug
D. When a patient has stable renal function
9. Which of the following is true about procainamide and its dosing schedule?
A. It produces bradycardia and should be used cautiously in patients with cardiac
conditions that a slower heart rate might worsen.
B. Gastrointestinal adverse effects are common so the drug should be taken with food.
C. Adherence can be improved by using a sustained release formulation that can be
given once daily.
D. Doses of this drug should be taken evenly spaced around the clock to keep an even
blood level.
10. Amiodarone has been prescribed in a patient with a supraventricular dysrhythmia. Patient teaching should include all of the following EXCEPT:
A. Notify your health-care provider immediately if you have visual change
B. Monitor your own blood pressure and pulse daily
C. Take a hot shower or bath if you feel dizzy
D. Use a sunscreen on exposed body surfaces
11. The NP orders a thyroid panel for a patient on amiodarone. The patient tells the NP that he does not have thyroid disease and wants to know why the test is ordered. Which is a correct response?
A. “Amiodarone inhibits an enzyme that is important in making thyroid hormone and
can cause hypothyroidism.”
B. “Amiodarone damages the thyroid gland and can result in inflammation of that
gland causing hyperthyroidism.”
C. “Amiodarone is a broad spectrum drug with many adverse effects. Many different
tests need to be done before it is given.”
D. “Amiodarone can cause corneal deposits in up to 25% of patients.”
12. Isosorbide dinitrate is prescribed for a patient with chronic stable angina. This drug is administered twice daily, but the schedule is 7 AM and 2 PM because:
A. It is a long-acting drug with potential for toxicity
B. Nitrate tolerance can develop
C. Orthostatic hypotension is a common adverse effect
D. It must be taken with milk or food
13. Art is a 55-year-old smoker who has been diagnosed with angina and placed on nitrates. He complains of headaches after using his nitrate. An appropriate reply might be:
A. “This is a parasympathetic response to the vasodilating effects of the drug.”
B. “Headaches are common side effects with these drugs. How severe are they?”
C. “This is associated with your smoking. Let’s work on having you stop smoking.”
D. “This is not related to your medication. Are you under a lot of stress?”
14. In teaching about the use of sublingual nitroglycerine, the patient should be instructed:
A. To swallow the tablet with a full glass of water
B. To place one tablet under the tongue if chest pain occurs and allow it to dissolve
C. To take one tablet every 5 minutes until the chest pain goes away
D. That it should “burn” when placed under the tongue or it is no longer effective
15. Donald has been diagnosed with hyperlipidemia. Based on his lipid profile, atorvastatin is prescribed. Rhabdomyolysis is a rare but serious adverse response to this drug. Donald should be told to:
A. Become a vegetarian since this disorder is associated with eating red meat
B. Stop taking the drug if abdominal cramps and diarrhea develop
C. Report muscle weakness or tenderness and dark urine to his provider immediately
D. Expect “hot flash” sensations during the first 2 weeks of therapy
24 Upper Respiratory Infections
MULTIPLE CHOICE
1. Which of the following conditions would an expectorant drug such as guaifenesin treat effectively?
a. Acute bronchitis c. Smoker's cough
b. Asthma d. Emphysema
2. A younger patient with cystic fibrosis has a new drug order for dornase alpha (Pulmozyme). The health care provider should choose which route of administration for this medication?
a. Oral c. Inhalation via nebulizer
b. Subcutaneous d. Rectal
3. A patient who has just received a new prescription for guaifenesin has been taught about adverse drug effects. The patient should identify which adverse effect as commonly associated with this drug?
a. Diaphoresis c. Muscle aches
b. Lethargy d. Gastrointestinal (GI) distress
4. The patient is scheduled to begin treatment with the alpha1-proteinase inhibitor Prolastin. The health care provider should expect to see what type of changes in the patient’s vital signs approximately 12 hours after drug administration?
a. Tachycardia c. Shortness of breath
b. Hypotension d. Fever
5. A patient who has an upper respiratory infection accompanied by severe cough has been given an antitussive medication with codeine. The patient asks why codeine is part of the prescribed drug. Which is the most appropriate response of the health care provider?
a. Codeine suppresses cough because it has a depressant effect on the sensory cortex
of the brain.
b. Codeine suppresses cough because it has a depressant effect on the cough center in
the medulla.
c. Codeine suppresses cough because it provides local anesthesia on stretch receptors
in the lungs.
d. Codeine suppresses cough because it stimulates the limbic system of the brain.
6. A patient has been instructed to take benzonatate (Tessalon Perles) for nonproductive cough due to bronchial irritation. Which patient instruction should the health care provider give to this patient?
a. Swallow the capsule whole.
b. Chew the capsule as needed to prevent choking.
c. Limit fluid intake when taking the drug.
d. Increase intake of vitamin D while taking the drug.
7. A patient has been instructed to take an antitussive medication to control cough. Which of the following adverse effects is most frequently associated with this group of drugs?
a. Rapid drug dependence c. Nausea and vomiting
b. Drowsiness d. Irritability
MULTIPLE RESPONSE
1. Which of the following medications are considered to be antitussives? Select all that apply.
a. Benzonatate
b. Codeine
c. Diphenhydramine
d. Dornase alpha
e. Guaifenesin
f. Dextromethorphan
Chapter 25. Asthma
MULTIPLE CHOICE
1. Prior to developing a plan for the treatment of asthma, the patient’s asthma should be classified according to the NHLBI Expert Panel 3 guidelines. In adults mild-persistent asthma is classified as asthma symptoms that occur:
A. Daily
B. Daily and limit physical activity
C. Less than twice a week
D. More than twice a week and less than once a day
2. In children age 5 to 11 years mild-persistent asthma is diagnosed when asthma symptoms occur:
A. At nighttime one to two times a month
B. At nighttime three to four times a month
C. Less than twice a week
D. Daily
3. One goal of asthma therapy outlined by the NHLBI Expert Panel 3 guidelines is:
A. Ability to use albuterol daily to control symptoms
B. Minimize exacerbations to once a month
C. Keep nighttime symptoms at a maximum of twice a week
D. Require infrequent use of beta 2 agonists (albuterol) for relief of symptoms
4. A stepwise approach to the pharmacologic management of asthma:
A. Begins with determining the severity of asthma and assessing asthma control
B. Is used when asthma is severe and requires daily steroids
C. Allows for each provider to determine their personal approach to the care of
asthmatic patients
D. Provides a framework for the management of severe asthmatics, but is not as
helpful when patients have intermittent asthma
5. Treatment for mild intermittent asthma is:
A. Daily inhaled medium dose corticosteroids
B. Short-acting beta-2-agonists (albuterol) as needed
C. Long-acting beta-2-agonists every morning as a preventative
D. Montelukast (Singulair) daily
6. The first-line therapy for mild-persistent asthma is:
A. High-dose montelukast
B. Theophylline
C. Low-dose inhaled corticosteroids
D. Long-acting beta-2-agonists
7. Monitoring a patient with persistent asthma includes:
A. Monitoring how frequently the patient has a URI during treatment
B. Monthly in-office spirometry testing
C. Determining if the patient has increased use of his or her long-acting beta-2-
agonist due to exacerbations
D. Evaluating the patient every 1 to 6 months to determine if the patient needs to step up or down in their therapy
8. Asthma exacerbations at home are managed by the patient by:
A. Increasing frequency of beta-2-agonists and contacting their provider
B. Doubling inhaled corticosteroid dose
C. Increasing frequency of beta-2-agonists
D. Starting montelukast (Singulair)
9. Patients who are at risk of a fatal asthma attack include patients:
A. With moderate persistent asthma
B. With a history of requiring intubation or ICU admission for asthma
C. Who are on daily inhaled corticosteroid therapy
D. Who are pregnant
10. Pregnant patients with asthma may safely use _ throughout their pregnancy.
A. Oral terbutaline
B. Prednisone
C. Inhaled corticosteroids (budesonide)
D. Montelukast (Singulair)
11. One goal of asthma management in children is:
A. They independently manage their asthma
B. Participation in school and sports activities
C. No exacerbations
D. Minimal use of inhaled corticosteroids
Chapter 26. Chronic Obstructive Pulmonary Disease
MULTIPLE CHOICE
1. Patients with COPD require monitoring of:
A. Beta-2-agonist use
B. Serum electrolytes
C. Blood pressure
D. All of the above
2. Pregnant patients with asthma may safely use _ throughout their pregnancy.
A. Oral terbutaline
B. Prednisone
C. Inhaled corticosteroids (budesonide)
D. Montelukast (Singulair)
3. Patients with a COPD exacerbation may require:
A. Doubling of inhaled corticosteroid dose
B. Systemic corticosteroid burst
C. Continuous inhaled beta-2-agonists
D. Leukotriene therapy
4. Medications used in the management of patients with COPD include:
A. Inhaled beta-2-agonists
B. Inhaled anticholinergics (ipratropium)
C. Inhaled corticosteroids
D. All of the above
5. One goal of asthma management in children is:
A. They independently manage their asthma
B. Participation in school and sports activities
C. No exacerbations
D. Minimal use of inhaled corticosteroids
6. Education of patients with COPD who use inhaled corticosteroids includes:
A. Doubling dose at the first sign of a URI
B. Use their inhaled corticosteroid first and then their bronchodilator
C. Rinsing mouth after use
D. They should not smoke for at least 30 minutes after using
Chapter 27. Bronchitis and Pneumonia
MULTIPLE CHOICE
1. The most common bacterial pathogen in community acquired pneumonia is:
A. Haemophilus influenzae
B. Staphylococcus aureus
C. Mycoplasma pneumoniae
D. Streptococcus pneumoniae
2. The first-line drug choice for a previously healthy adult patient diagnosed with community acquired pneumonia would be:
A. Ciprofloxacin
B. Azithromycin
C. Amoxicillin
D. Doxycycline
3. The first-line antibiotic choice for a patient with comorbidities or who is immunosuppressed who has pneumonia and can be treated as an outpatient would be:
A. Levofloxacin
B. Amoxicillin
C. Ciprofloxacin
D. Cephalexin
4. If an adult patient with comorbidities cannot reliably take oral antibiotics to treat pneumonia, an appropriate initial treatment option would be:
A. IV or IM gentamicin
B. IV or IM ceftriaxone
C. IV amoxicillin
D. IV ciprofloxacin
5. Samantha is 34 weeks pregnant and has been diagnosed with pneumonia. She is stable enough to be treated as an outpatient. What would be an appropriate antibiotic to prescribe?
A. Levofloxacin
B. Azithromycin
C. Amoxicillin
D. Doxycycline
6. Adults with pneumonia who are responding to antimicrobial therapy should show improvement in their clinical status in:
A. 12 to 24 hours
B. 24 to 36 hours
C. 48 to 72 hours
D. 4 or 5 days
7. Along with prescribing antibiotics, adults with pneumonia should be instructed on lifestyle modifications to improve outcomes, including:
A. Adequate fluid intake
B. Increased fiber intake
C. Bedrest for the first 24 hours
D. All of the above
8. John is a 4-week-old infant who has been diagnosed with chlamydial pneumonia. The appropriate treatment for his pneumonia would be:
A. Levofloxacin
B. Amoxicillin
C. Erythromycin
D. Cephalexin
9. Wing-Sing is a 4 year old who has a suspected bacterial pneumonia. He has a temperature of 102°F, oxygen saturation level of 95%, and is taking fluids adequately. What would be appropriate initial treatment for his pneumonia?
A. Ceftriaxone
B. Azithromycin
C. Cephalexin
D. Levofloxacin
10. Giselle is a 14 year old who presents to clinic with symptoms consistent with mycoplasma pneumonia. What is the treatment for suspected mycoplasma pneumonia in an adolescent?
A. Ceftriaxone
B. Azithromycin
C. Ciprofloxacin
D. Levofloxacin
Chapter 28. Nausea and Vomiting
MULTIPLE CHOICE
1. Which of the following antiemetic drugs would most benefit a patient who experiences nausea and vomiting associated with motion sickness?
a. Prochlorperazine (Compazine) c. Perphenazine (Trilafon)
b. Dimenhydrinate (Dramamine) d. Cisapride (Propulsid)
2. A patient is receiving hydroxyzine (Vistaril) for complaints of nausea and vomiting. Consider the following adverse effects of the drug, and select the one that is most significant.
a. Excessive salivation c. Decreased respiratory rate
b. Increased pulse d. Sedation
3. A patient has been instructed to use meclizine (Bonine) to prevent motion sickness. Select the statement that demonstrates that the patient understands proper use of the drug.
a. Administer at least 30 minutes and preferably 1-2 hours before travel.
b. Administer immediately before travel.
c. Administer during travel if the patient begins to experience dizziness.
d. Administer 1 hour after beginning travel regardless of whether symptoms are felt.
4. A patient who frequently takes diphenhydramine (Benadryl) to prevent motion sickness is scheduled for skin testing to diagnose possible allergies. For what number of days should the patient refrain from taking diphenhydramine before skin testing?
a. 1 c. 4
b. 2 d. 7
5. A patient has a drug order for prochlorperazine (Compazine) for management of nausea and vomiting. Review the following statements, and select the one that most accurately describes the action of the drug.
a. It blocks the action of serotonin in the brain.
b. It blocks the effects of dopamine in the chemoreceptor trigger zone.
c. It stimulates relaxation of smooth muscle in the gastrointestinal (GI) tract.
d. It enhances release of acetylcholine at nerve endings in the mesentery.
6. Which of the following extrapyramidal adverse effects is associated with phenothiazine drugs?
a. Sedation c. Opacity of the lens
b. Hypotension d. Pseudoparkinsonism
7. Phenothiazines most successfully treat nausea and vomiting produced by which of the following?
a. Postoperative gastric distention c. Radiation therapy and chemotherapy
b. Motion sickness d. Gastroparesis
MULTIPLE RESPONSE
1. Which of the following factors are associated with psychogenic vomiting? Select all that apply.
a. Physical syndrome
b. Sexual abuse
c. Alcoholism
d. Posttraumatic stress
e. Eating disorders
Chapter 29. Gastroesophageal Reflux Disease and Peptic Ulcer Disease
MULTIPLE CHOICE
1. Gastroesophageal reflux disease (GERD) may be aggravated by the following medication that effects lower esophageal sphincter (LES) tone:
A. Calcium carbonate
B. Estrogen
C. Furosemide
D. Metoclopramide
2. Lifestyle changes are the first step in treatment of gastroesophageal reflux disease (GERD). Foods that may aggravate GERD include:
A. Eggs
B. White bread
C. Chocolate
D. Chicken
3. Metoclopramide improves GERD symptoms by:
A. Reducing acid secretion
B. Increasing gastric pH
C. Increasing lower esophageal tone
D. Decreasing lower esophageal tone
4. Antacids treat GERD by:
A. Increasing lower esophageal tone
B. Increasing gastric pH
C. Inhibiting gastric acid secretion
D. Increasing serum calcium level
5. When treating patients using the “Step-Down” approach the patient with GERD is started on
first.
A. Antacids
B. Histamine2 receptor antagonists
C. Prokinetics
D. Proton pump inhibitors
6. When using the “Step-Up” approach in caring for patients with GERD, the “step up” from OTC antacid use is:
A. Prokinetic (metoclopramide) for 4 to 8 weeks
B. Proton pump inhibitor (omeprazole) for 12 weeks
C. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks
D. Cytoprotective drug (misoprostol) for 2 weeks
7. When using the “Step-Up” approach in caring for patients with GERD, the “step up” from once daily proton pump inhibitor use is:
A. Prokinetic (metoclopramide) for 8 to 12 weeks
B. Proton pump inhibitor (omeprazole) twice a day for 4 to 8 weeks
C. Histamine2 receptor antagonist (ranitidine) for 4 to 8 weeks
D. Cytoprotective drug (misoprostol) for 4 to 8 weeks
8. When using “Step-Up” therapy for GERD, the next “step up” in treatment when a patient has been on proton pump inhibitors for 12 weeks is:
A. Add a prokinetic (metoclopramide)
B. Referral for endoscopy
C. Switch to another proton pump inhibitor
D. Add a cytoprotective drug
9. Infants with reflux are initially treated with:
A. Histamine2 receptor antagonist (ranitidine)
B. Proton pump inhibitor (omeprazole)
C. Anti-reflux maneuvers (elevate head of bed)
D. Prokinetic (metoclopramide)
10. Long-term use of proton pump inhibitors may lead to:
A. Hip fractures in at-risk persons
B. Vitamin B6 deficiency
C. Liver cancer
D. All of the above
11. An acceptable first-line treatment for peptic ulcer disease with positive H. pylori test is:
A. Histamine2 receptor antagonists for 4 to 8 weeks
B. Proton pump inhibitor BID for 12 weeks until healing is complete
C. Proton pump inhibitor BID plus clarithromycin plus amoxicillin for 14 days
D. Proton pump inhibitor BID and levofloxacin for 14 days
12. Treatment failure in patients with peptic ulcer disease associated with H. pylori may be due to:
A. Antimicrobial resistance
B. Ineffective antacid
C. Overuse of proton pump inhibitors
D. All of the above
:
13. If a patient with H. pylori positive peptic ulcer disease fails first-line therapy the second-line treatment is:
A. Proton pump inhibitor BID plus metronidazole plus tetracycline plus bismuth
subsalicylate for 14 days
B. Test H. pylori for resistance to common treatment regimens
C. Proton pump inhibitor plus clarithromycin plus amoxicillin for 14 days
D. Proton pump inhibitor and levofloxacin for 14 days
14. After H. pylori treatment is completed, the next step in peptic ulcer disease therapy is:
A. Testing for H. pylori eradication with a serum ELISA test
B. Endoscopy by a specialist
C. Proton pump inhibitor for 8 to 12 weeks until healing is complete
D. All of the above
Chapter 30. Constipation Diarrhea and Irritable Bowel Syndrome
MULTIPLE CHOICE
1. Many patients self-medicate with antacids. Which patients should be counseled to not take calcium carbonate antacids without discussing with their provider or a pharmacist first?
A. Patients with kidney stones
B. Pregnant patients
C. Patients with heartburn
D. Post-menopausal women
2. Patients taking antacids should be educated regarding these drugs, including:
A. They may cause constipation or diarrhea
B. Many are high in sodium
C. Separate antacids from other medications by 1 hour
D. All of the above
3. Kelly has diarrhea and is wondering if she can take loperamide (Imodium) for the diarrhea. Loperamide:
A. Can be given to all age patients, including infants and children, for viral
gastroenteritis
B. Slows gastric motility and reduces fluid and electrolyte loss from diarrhea
C. Is the treatment of choice for the diarrhea associated with E. coli 0157
D. May be used in pregnancy and by lactating women
4. Bismuth subsalicylate (Pepto Bismol) is a common OTC remedy for gastrointestinal complaints. Bismuth subsalicylate:
A. May lead to toxicity if taken with aspirin
B. Is contraindicated in children with flu-like illness
C. Has antimicrobial effects against bacterial and viral enteropathogens
D. All of the above
5. Hannah will be traveling to Mexico with her church group over Spring Break to build houses. She is concerned she may develop traveler’s diarrhea. Advice includes normal food and water precautions as well as:
A. Loperamide four times a day throughout the trip
B. Bismuth subsalicylate with each meal and bedtime
C. A prescription for diphenoxylate with atropine to use if she gets diarrhea
D. None of the above
6. Josie is a 5 year old who presents to the clinic with a 48-hour history of nausea, vomiting, and some diarrhea. She is unable to keep fluids down and her weight is 4 pounds less than her last recorded weight. Besides IV fluids, her exam warrants the use of an antinausea medication. Which of the following would be the appropriate drug to order for Josie?
A. Prochlorperazine (Compazine)
B. Meclizine (Antivert)
C. Promethazine (Phenergan)
D. Ondansetron (Zofran)
7. Jim presents with complaints of “heart burn” that is minimally relieved with Tums (calcium carbonate) and is diagnosed with GERD. An appropriate first step therapy would be:
A. Omeprazole (Prilosec) twice a day
B. Ranitidine (Zantac) twice a day
C. Famotidine (Pepcid) once a day
D. Metoclopramide (Reglan) four times a day
8. Patients who are on chronic long-term proton pump inhibitor therapy require monitoring for:
A. Iron deficiency anemia, vitamin B12 and calcium deficiency
B. Folate and magnesium deficiency
C. Elevated uric acid levels leading to gout
D. Hypokalemia and hypocalcemia
9. Sadie is a 72 year old who takes omeprazole for her chronic GERD. Chronic long-term omeprazole use places her at increased risk for:
A. Megaloblastic anemia
B. Osteoporosis
C. Hypertension
D. Strokes
10. Patrick is a 10 year old who presents with constipation. Along with diet changes, a laxative is ordered to provide more rapid relief of constipation. An appropriate choice of medication for a 10 year old would be:
A. PEG 3350 (Miralax)
B. Bisacodyl (Dulcolax) suppository
C. Docusate (Colace) suppository
D. Polyethylene glycol electrolyte solution
Chapter 31 Inflammatory Bowel Disease
MULTIPLE CHOICE
1. Which of the following electrolyte abnormalities would be expected to be present in a patient who has a drug order for a cation-exchange resin?
a. Hypernatremia c. Hyperkalemia
b. Hypocalcemia d. Hypochloremia
2. Which of the following adverse effects would a health care provider expect to see in a patient receiving sodium polystyrene sulfonate resin (Kayexalate)?
a. Peritonitis c. Intussception
b. Nausea and vomiting d. Intestinal necrosis
3. Review the following diagnoses, and select the one that would cause a health care provider to use sodium polystyrene sulfonate resin (Kayexalate) with caution.
a. Kidney stones c. Fractured long bone
b. Heart failure d. Spinal cord injury
4. Which of the following substances is appropriate for mixing with a dose of oral sodium polystyrene sulfonate resin (Kayexalate)?
a. Sorbitol c. Orange juice
b. Magnesium-containing laxative d. Milk
5. Which of the following serum laboratory studies should be evaluated by the health care provider who is determining the effectiveness of lactulose (Cephulac)?
a. Triglycerides c. Uric acid
b. Potassium d. Ammonia
6. Evaluate the following conditions that may be noted in older adults, and select the one that can be treated with lactulose (Cephulac).
a. Constipation c. Peptic ulcer
b. Diarrhea d. Esophageal varices
7. Neomycin (Mycifradin sulfate) is ordered for the patient who is to undergo bowel surgery. Which of the following purposes would accurately explain to the patient the action of this drug and why it is being used preoperatively?
a. To restore electrolyte balance
b. To promote osmotic diuresis
c. To decrease the gastrointestinal (GI) tract bacterial count
d. To inhibit ammonia elimination
Chapter 32. Urinary Tract Infections
MULTIPLE CHOICE
1. The treatment goals when treating urinary tract infection (UTI) include:
A. Eradication of infecting organism
B. Relief of symptoms
C. Prevention of recurrence of UTI
D. All of the above
2. Sally is a 16-year-old female with a urinary tract infection. She is healthy, afebrile, with no use of antibiotics in the previous 6 months and no drug allergies. An appropriate first-line antibiotic choice for her would be:
A. Azithromycin
B. Trimethoprim/sulfamethoxazole
C. Ceftriaxone
D. Levofloxacin
3. Jamie is a 24-year-old female with a urinary tract infection. She is healthy, afebrile, and her only drug allergy is sulfa, which gives her a rash. An appropriate first-line antibiotic choice for her would be:
A. Azithromycin
B. Trimethoprim/sulfamethoxazole
C. Ceftriaxone
D. Ciprofloxacin
4. Juanita is a 28-year-old pregnant woman at 38 weeks gestation who is diagnosed with a lower urinary tract infection. She is healthy with no drug allergies. Appropriate first-line therapy for her UTI would be:
A. Azithromycin
B. Trimethoprim/sulfamethoxazole
C. Amoxicillin
D. Ciprofloxacin
5. Which of the following patients may be treated with a 3-day course of therapy for their urinary tract infection?
A. Juanita, a 28-year-old pregnant woman
B. Sally, a 16-year-old healthy adolescent
C. Jamie, a 24-year-old female
D. Suzie, a 26-year-old diabetic
6. Nicole is a 4-year-old female with a febrile urinary tract infection. She is generally healthy and has no drug allergies. Appropriate initial therapy for her UTI would be:
A. Azithromycin
B. Trimethoprim/sulfamethoxazole
C. Ceftriaxone
D. Ciprofloxacin
7. Monitoring for a healthy, non-pregnant adult patient being treated for a urinary tract infection is:
A. Symptom resolution in 48 hours
B. Follow-up urine culture at completion of therapy
C. “Test of cure” urinary analysis at completion of therapy
D. Follow-up urine culture 2 months after completion of therapy
8. Monitoring for a child who has had a urinary tract infection is:
A. Symptom resolution in 48 hours
B. Follow-up urine culture at completion of therapy
C. “Test of cure” urinary analysis at completion of therapy
D. Follow-up urine culture 2 months after completion of therapy
9. Monitoring for a pregnant woman who has had a urinary tract infection is:
A. Symptom resolution in 48 hours
B. Follow-up urine culture at completion of therapy
C. “Test of cure” urinary analysis at completion of therapy
D. Follow-up urine culture every 2 weeks until delivery
10. Along with an antibiotic prescription, lifestyle education for a non-pregnant adult female who has had a urinary tract infection includes:
A. Increasing her intake of Vitamin C containing orange juice
B. Voiding 10 to 15 minutes after intercourse
C. Avoiding ingesting urinary irritants, such as asparagus
D. All of the above
11. Lisa is a healthy non-pregnant adult woman who recently had a UTI. She is asking about drinking cranberry juice to prevent a recurrence of the UTI. The correct answer to give her would be:
A. “Sixteen ounces per day of cranberry juice cocktail will prevent UTIs.”
B. “100% cranberry juice or cranberry juice extract may decrease UTIs in some
patients.”
C. “There is no evidence that cranberry juice helps prevent UTIs.”
D. “Cranberry juice only works to prevent UTIs in children.”
Chapter 34. Overactive Bladder
MULTIPLE CHOICE
1. Which of the following drug classes is considered to be the drug class of choice for management of overactive bladder (OAB)?
a. Alpha blockers c. Phosphodiasterase inhibitors
b. Urinary tract antispasmodics d. Antimuscarinics
2. The patient has been placed on a treatment regimen that includes bethanechol chloride (Urecholine). Which symptom should the patient be instructed to report because of its potential to be life-threatening?
a. Shortness of breath c. Vomiting
b. Syncope d. Tachycardia
3. The patient has been placed on tadalafil (Cialis) for treatment of erectile dysfunction. The patient should be instructed that the maximum number of doses that may be administered during the course of one day is:
a. 4 c. 2
b. 3 d. 1
4. Which condition would be a contraindication for use of an antimuscarinic agent in a patient?
a. Dysphagia c. Urinary retention
b. Diabetes mellitus d. Gout
5. Which of the following medications is considered to be a nonselective alpha blocker?
a. Alfuzosin c. Doxazosin
b. Tamsulosin d. Prazosin
6. Which of the following drugs is used for benign prostatic hypertrophy (BPH) and has the greatest potential for causing orthostatic hypotension?
a. Alfuzosin c. Doxazosin
b. Tamsulosin d. Prazosin
7. Which of the following medications, if crushed, may have teratogenic effects in a male fetus if the patient’s female sex partner is exposed to it?
a. Dutasteride c. Doxazosin
b. Finasteride d. Prazosin
MULTIPLE RESPONSE
1. Which of the following drugs are considered to be second-generation antimuscarinic drugs? Select all that apply.
a. Darifenacin
b. Oxybutynin
c. Solifenacin
d. Tolterodine
e. Trospium
Chapter 35. Sexually Transmitted Infections
MULTIPLE CHOICE
1. The goals of treatment when prescribing for sexually transmitted infections include:
A. Treatment of infection
B. Prevention of disease spread
C. Prevention of long-term sequelae from the infection
D. All of the above
2. The drug of choice for treatment of primary or secondary syphilis is:
A. Ceftriaxone IM
B. Benzathine penicillin G IM
C. Oral azithromycin
D. Oral ciprofloxacin
3. The drug of choice for treatment of early latent or tertiary syphilis is:
A. Ceftriaxone IM
B. Benzathine penicillin G IM
C. Oral azithromycin
D. Oral ciprofloxacin
4. Demione is a 24 year old who is 32 weeks pregnant and has tested positive for syphilis. The best treatment for her would be:
A. IM ceftriaxone
B. IM benzathine penicillin G
C. Oral azithromycin
D. Any of the above
5. Treatment for suspected gonorrhea is:
A. Ceftriaxone 250 mg IM x 1
B. Ceftriaxone 2 grams IM x 1
C. Ciprofloxacin 500 mg PO x 1
D. Doxycycline 100 mg BID x 7 days
6. When treating suspected gonorrhea in a non-pregnant patient, the patient should be concurrently treated for Chlamydia with:
A. Azithromycin 1 gram PO x 1
B. Amoxicillin 500 mg PO x 1
C. Ciprofloxacin 500 mg PO x 1
D. Penicillin G 2.4 million units IM x 1
7. Ongoing monitoring is essential after treating for gonorrhea. The patient should be rescreened for gonorrhea and Chlamydia in:
A. 4 weeks
B. 3 to 6 weeks
C. 3 to 6 months
D. 1 year
8. A test of cure is recommended after treating Chlamydia in which patient population?
A. Men who have sex with men
B. Adolescent females
C. Pregnant patients
D. All of the above
9. Treatment for chancroid in a non-pregnant patient would be:
A. Oral azithromycin
B. IM ceftriaxone
C. Oral ciprofloxacin
D. Any of the above
10. Jamie was treated for chancroid. Follow-up testing after treatment of chancroid would be:
A. Syphilis and HIV testing at 3-month intervals
B. Chancroid-specific antigen test every 3 months
C. Urine testing for Haemophilus ducreyi in 3 to 6 months for test of cure
D. Annual HIV testing if engaging in high-risk sexual behavior
11. Zoe presents with genital warts present on her labia. Patient-applied topical therapy for warts includes:
A. Podofilox 0.5% gel
B. Podophyllin 10% resin
C. Trichloracetic acid
D. Any of the above
12. In addition to antimicrobial therapy, patients treated for Trichomonas infection should be educated regarding:
A. Necessity of treating sexual partner simultaneously
B. Abstaining from intercourse until both partners are treated
C. Need for retesting in 3 months due to high reinfection rate
D. All of the above
Chapter 36. Osteoarthritis and Rheumatoid Arthritis
MULTIPLE CHOICE
1. The nurse demonstrates understanding of the appropriate use of immunosuppressant therapy by anticipating its use in the client with which disorder?
A. Gout C. Rheumatoid arthritis
B. Exophthalmus D. Cancer
2. The nurse is establishing outcomes for a client with rheumatoid arthritis. What would be an appropriate outcome following three days of immunosuppressant therapy?
A. Decreased serum calcium C. Increased erythrocyte sedimentation rate
B. Reduced joint inflammation D. Increased white cell count
3. In the 1950s, researchers began searching for safer medications to treat rheumatoid arthritis (RA). Prior to this time, RA was treated with aspirin and corticosteroids. Which drug was identified by the researchers to be safer in the treatment of inflammation and pain for RA clients?
A. Gold compounds C. Celecoxib
B. Acetaminophen D. Ibuprofen
4. Which question is most important for the nurse to ask the client who has been diagnosed with osteoporosis?
A. “How much weight have you gained in the last
year?” C. “How many dairy products do you consume
per day?”
B. “Does someone in your household smoke?” D. “What would you estimate your cholesterol
intake to be?”
5. A client with a calcium imbalance has an elevated calcitonin level. The nurse recognizes that the secretion of calcitonin is increased when the client experiences:
A. Hypocalcemia. C. Hyperthyroidism
B. Hypothyroidism. D. Hypercalcemia.
6. A client is prescribed a disease-modifying antirheumatic agent. What will the nurse explain as the mechanism of action for this medication?
A. Provides rapid relief of symptoms C. Reduces damage and delays disease progression
B. Prevents the need for orthopedic surgery D. Allows the client to be more active
7. The nurse should instruct a client with osteoarthritis to engage in low-impact exercise and take:
A. Opioid analgesics C. Acetaminophen
B. Glucosamine and chondroitin agents. D. High anti-inflammatory doses of aspirin.
8. A client with rheumatoid arthritis is prescribed hydroxychloroquine (Plaquenil). The nurse should caution the client to:
A. Report blurred vision or decreased reading ability immediately. C. Take this drug with an antacid to decrease stomach distress.
B.
Continue taking a glass of red wine before dinner to reduce cardiovascular risk. D. Expose skin to sunlight for at least 20 minutes every day to help with bone formation.
Chapter 37. Fibromyalgia
MULTIPLE CHOICE
1. Select the medication that has an unlabeled use as treatment for fibromyalgia.
a. diazepam c. methocarbamol
b. baclofen d. cyclobenzaprine
2. Which of the following medications has an unlabeled use as treatment for Huntington’s chorea?
a. diazepam c. methocarbamol
b. baclofen d. cyclobenzaprine
3. Choose the only benzodiazepine indicated for muscle relaxation.
a. diazepam c. methocarbamol
b. baclofen d. cyclobenzaprine
4. A patient has been started on a treatment regimen that includes cyclobenzaprine (Flexeril). What is the most frequently encountered side effect of this medication?
a. Orthostatic hypotension c. Dry mouth
b. Dizziness d. Weakness
5. The patient needs to have a muscle relaxant added to her treatment regimen. She also is being treated with a monoamine oxidase inhibitor. Select the muscle relaxant that should be avoided when one is prescribing for this patient.
a. diazepam c. methocarbamol
b. baclofen d. cyclobenzaprine
6. Select the maximum length of time that skeletal muscle relaxants should be used.
a. 4 weeks c. 2 weeks
b. 3 weeks d. 1 week
MULTIPLE RESPONSE
1. Select the medications that are considered to be antispasmodics.
a. baclofen
b. metaxalone
c. methocarbamol
d. chlorzoxazone
e. cyclobenzaprine
Ch 38. Headaches
MULTIPLE CHOICE
1. Paige has a history of chronic migraines and would benefit from preventative medication. Education regarding migraine preventive medication includes:
A. Medication is taken at the beginning of the headache to prevent it from getting
worse
B. Medication alone is the best preventative against migraines occurring
C. Medication should not be used more than four times a month
D. The goal of treatment is to reduce migraine occurrence by 50%
2. A first-line drug for abortive therapy in simple migraine is:
A. Sumatriptan (Imitrex)
B. Naproxen (Aleve)
C. Butorphanol nasal spray (Stadol NS)
D. Butalbital and acetaminophen (Fioricet)
3. Vicky, age 56 years, comes to clinic requesting a refill of her Fiorinal (aspirin and butalbital) that she takes for migraines. She has been taking this medication for over 2 years for migraine and states one dose usually works to abort her migraine. What is the best care for her?
A. Switch her to sumatriptan (Imitrex) to treat her migraines
B. Assess how often she is using Fiorinal and refill medication
C. Switch her to a beta-blocker such as propranolol to prevent her migraine
D. Request she return to the original prescriber of Fiorinal as you do not prescribe
butalbital for migraines
4. When prescribing ergotamine suppositories (Wigraine) to treat acute migraine, patient education would include:
A. Ergotamine will briefly make the migraine worse before the migraine resolves
B. The patient may experience bradycardia and dizziness
C. They may need premedication with an antinausea medication
D. Ergotamine works best if the patient starts off with a full suppository to get the full
effect
5. Migraines in pregnancy may be safely treated with:
A. Acetaminophen with codeine (Tylenol #3)
B. Sumatriptan (Imitrex)
C. Ergotamine tablets (Ergostat)
D. Dihydroergotamine (DHE)
6. Xi, a 54-year-old female, has a history of migraine that does not respond well to OTC migraine medication. She is asking to try Maxalt (rizatriptan) because it works well for her friend. Appropriate decision making would be:
A. Prescribe the Maxalt, but only give her four tablets with no refills to monitor the
use
B. Prescribe Maxalt and arrange to have her observed in the clinic or urgent care with
the first dose
C. Explain that rizatriptan is not used for post-menopausal migraines and recommend
Fiorinal (aspirin and butalbital)
D. Prescribe sumatriptan (Imitrex) with the explanation that it is the most effective
triptan
7. Kelly is a 14 year old who presents to clinic with a classic migraine. She says she is having a headache two to three times a month. The initial plan would be:
A. Prescribe NSAIDs as abortive therapy and have her keep a headache diary to
identify her triggers
B. Prescribe zolmitriptan (Zomig) as abortive therapy and recommend relaxation
therapy to reduce her stress
C. Prescribe acetaminophen with codeine (Tylenol #3) for her to take at the first onset
of her migraine
D. Prescribe sumatriptan (Imitrex) nasal spray and arrange for her to receive the first
dose in the clinic
8. Jayla is a 9 year old who has been diagnosed with migraines for almost 2 years. She is missing up to a week of school each month. Her headache diary confirms she averages four or five migraines per month. Which of the following would be appropriate?
A. Prescribe amitriptyline (Elavil) daily, start at a low dose and increase dose slowly
every 2 weeks until effective in eliminating migraines
B. Encourage her mother to give her Excedrin Migraine (aspirin, acetaminophen, and
caffeine) at the first sign of a headache to abort the headache
C. Prescribe propranolol (Inderal) to be taken daily for at least 3 months
D. Explain that it is rare for a 9 year old to get migraines and she needs an MRI to
rule out a brain tumor
9. Amber is a 24 year old who has had migraines for 10 years. She reports a migraine on average of once a month. The migraines are effectively aborted with naratriptan (Amerge). When refilling Amber’s naratriptan education would include:
A. Naratriptan will interact with antidepressants, including SSRIs and St John’s Wort,
and she should inform any providers she sees that she has migraines
B. Continue to monitor her headaches, if the migraine is consistently happening
around her menses there is preventive therapy available
C. Pregnancy is contraindicated when taking a triptan
D. All of the above
10. When prescribing for migraine, patient education includes:
A. Triptans are safe to be used as often as needed as long as the patient is healthy
B. Use triptan before trying OTC meds such as acetaminophen or naproxen
C. Stress reduction and regular sleep are integral to migraine treatment
D. If migraines worsen they are to increase their medication
11. Juanita presents to clinic with a complaint of headaches off and on for months. She reports they feel like someone is “squeezing” her head. She occasionally takes Tylenol for the pain, but usually just “toughs it out.” Initial treatment for tension headache includes asking her to keep a headache diary and a prescription for:
A. Sumatriptan (Imitrex)
B. Naproxen (Aleve)
C. Ergotamine (Ergostat)
D. Tylenol with codeine (Tylenol #3)
12. Nonpharmacologic therapy for tension headaches includes:
A. Biofeedback
B. Stress management
C. Massage therapy
D. All of the above
13. James has been diagnosed with cluster headaches. Appropriate acute therapy would be:
A. Butalbital and aspirin (Fiorinal)
B. Meperidine IM (Demerol)
C. Oxygen 100% for 15 to 30 minutes
D. Indomethacin (Indocin)
14. Preventative therapy for cluster headaches includes:
A. Massage or relaxation therapy
B. Ergotamine nightly before bed
C. Intranasal lidocaine four times a day during “clusters” of headaches
D. Propranolol (Inderal) daily
15. When prescribing any headache therapy, appropriate use of medications needs to be discussed to prevent medication-overuse headaches. The clinical characteristics of medication-overuse headaches include:
A. Headaches are increasing in frequency
B. Headaches are increasing in intensity
C. Headaches recur when medication wears off
D. Headaches begin to “cluster” into a pattern
Chapter 39 Seizure Disorders
MULTIPLE CHOICE
1. Antonia is a 3 year old who has a history of status epilepticus. Along with her routine antiseizure medication, she should also have a home prescription for to be used for an episode of status epilepticus.
A. IV phenobarbital
B. Rectal diazepam (Diastat)
C. IV phenytoin (Dilantin)
D. Oral carbamazepine (Tegretol)
2. Rabi is being prescribed phenytoin for seizures. Monitoring includes:
A. Assessing for phenytoin hypersensitivity syndrome 3 to 8 weeks after starting
treatment
B. Assessing for pedal edema throughout therapy
C. Assessing heart rate at each visit and consider altering therapy if heart rate is less
than 60 bpm
D. Assessing for vision changes, such as red-green blindness, at least annually
3. Dwayne has recently started on carbamazepine to treat seizures. He comes to see you and you note that while his carbamazepine levels had been in the therapeutic range, they are now low. The possible cause for the low carbamazepine levels include:
A. Dwayne hasn’t been taking his carbamazepine because it causes insomnia
B. Carbamazepine auto-induces metabolism, leading to lower levels in spite of good
compliance
C. Dwayne was not originally prescribed the correct amount of carbamazepine
D. Carbamazepine is probably not the right antiseizure medication for Dwayne
4. Carbamazepine has a Black Box warning due to life-threatening:
A. Renal toxicity, leading to renal failure
B. Hepatotoxicity, leading to liver failure
C. Dermatologic reaction, including Steven’s Johnson and toxic epidermal necrolysis
D. Cardiac effects, including supraventricular tachycardia
5. Long-term monitoring of patients who are taking carbamazepine includes:
A. Routine troponin levels to assess for cardiac damage
B. Annual eye examinations to assess for cataract development
C. Monthly pregnancy tests for all women of childbearing age
D. Complete blood count every 3 to 4 months
6. Six-year-old Lucy has recently been started on ethosuximide (Zarontin) for seizures. She should be monitored for:
A. Increased seizure activity, as this drug may auto-induce seizures
B. Altered renal function, including renal failure
C. Blood dyscrasias, which are uncommon but possible
D. Central nervous system excitement, leading to insomnia
7. Selma, who is overweight, recently started taking topiramate for seizures and at her follow-up visit you note she has lost 3 kg. The appropriate action would be:
A. Tell her to increase her caloric intake to counter the effects of the topiramate
B. Consult with a neurologist, as this is not a common adverse effect of topiramate
C. Decrease her dose of topiramate
D. Reassure her that this is a normal side effect of topiramate and continue to monitor
her weight
8. Monitoring of a patient on gabapentin to treat seizures includes:
A. Routine therapeutic drug levels every 3 to 4 months
B. Assessing for dermatologic reactions, including Steven’s Johnson
C. Routine serum electrolytes, especially in hot weather
D. Recording seizure frequency, duration, and severity
9. Scott’s seizures are well controlled on topiramate and he wants to start playing baseball. Education for Scott regarding his topiramate includes:
A. He should not play sports due to the risk of increased seizures
B. He should monitor his temperature and ability to sweat in the heat while playing
C. Reminding him that he may need higher dosages of topiramate when exercising
D. Encouraging him to use sunscreen due to photosensitivity from topiramate
10. Cara is taking levetiracetam (Keppra) to treat seizures. Routine education for levetiracetam includes reminding her:
A. To not abruptly discontinue levetiracetam due to risk for withdrawal seizures
B. To wear sunscreen due to photosensitivity from levetiracetam
C. To get an annual eye exam while on levetiracetam
D. To report weight loss if it occurs
11. Levetiracetam has known drug interactions with:
A. Oral contraceptives
B. Carbamazepine
C. Warfarin
D. Few, if any, drugs
12. Zainab is taking lamotrigine (Lamictal) and presents to the clinic with fever and lymphadenopathy. Initial evaluation and treatment includes:
A. Reassuring her she has a viral infection and to call if she isn’t better in 4 or 5 days
B. Ruling out a hypersensitivity reaction that may lead to multi-organ failure
C. Rapid strep test and symptomatic care if strep test is negative
D. Observation only, with further assessment if she worsens
13. Samantha is taking lamotrigine (Lamictal) for her seizures and requests a prescription for oral contraceptives. Combined oral contraceptives (OCs) interact with lamotrigine and may cause:
A. Contraceptive failure
B. Excessive weight gain
C. Reduced lamotrigine levels, requiring doubling the dose of lamotrigine
D. Induction of estrogen metabolism, requiring higher estrogen content OCs be
prescribed
Chapter 40. Depressive Disorders
MULTIPLE CHOICE
1. Which of the following is the mechanism by which the selective serotonin reuptake inhibitor (SSRI) antidepressant drugs appear to work?
a. Blocking reuptake of gamma-aminobutyric acid (GABA) and substance P
b. Blocking reuptake of serotonin and norepinephrine
c. Enhancing reuptake of serotonin and norepinephrine
d. Enhancing reuptake of GABA and substance P
2. The health care provider teaches a patient beginning tricyclic antidepressant drug therapy about measures to minimize the most serious common adverse drug effects. Which of the following adverse reactions is considered the most serious?
a. Orthostatic hypotension c. Blurred vision
b. Dry mouth d. Urinary retention
3. A patient receiving a tricyclic antidepressant complains of constipation. What is the health care provider’s interpretation of the patient’s complaint?
a. It is a sign of recovery from depression.
b. It is an attention-getting mechanism.
c. It is a common side effect of the drug.
d. It is an indication that this drug should be stopped.
4. A patient has begun taking fluoxetine (Prozac) for depression. When will the effects of the drug first be felt?
a. 5-7 days c. 1-2 months
b. 1-4 weeks d. 3-6 months
5. Phenelzine (Nardil) has been discontinued as a drug order for a patient. How much time must be observed before the patient can start a new drug?
a. 2 days c. 1 week
b. 5 days d. 2 weeks
6. The patient has been started on a treatment regimen which includes the use of lithium. As part of the teaching plan regarding lithium, the patient should be instructed that he should avoid:
a. Becoming sleep-deprived
b. Failing to exercise daily
c. Failing to stay on his prescribed dietary regimen
d. Becoming dehydrated
7. The patient has been started on a treatment regimen for acute mania. As part of the teaching plan for the patient and the family regarding use of the medication, they should be taught to immediately report which of the following symptoms to the primary care provider?
a. Deterioration of mental alertness c. Deterioration of sleep pattern
b. Deterioration of emotional stability d. Deterioration of eating pattern
8. An appropriate first-line drug for the treatment of depression with fatigue and low energy would be:
a. Venlafaxine (Effexor)
b. Escitalopram (Lexapro)
c. Buspirone (Buspar)
d. Amitriptyline (Elavil)
9. The laboratory monitoring required when a patient is on an SSRI is:
a. Complete blood count every 3 to 4 months
b. Therapeutic blood levels every 6 months after steady state is achieved
c. Blood glucose every 3 to 4 months
d. There is no laboratory monitoring required
10. Jaycee has been on escitalopram (Lexapro) for a year and is willing to try tapering off of the SSRI. What is the initial dosage adjustment when starting a taper off antidepressants?
a. Change dose to every other day dosing for a week
b. Reduce dose by 50% for 3 to 4 days
c. Reduce dose by 50% every other day
d. Escitalopram (Lexapro) can be stopped abruptly due to its long half-life
MULTIPLE RESPONSE
1. Which of the following are believed to be risk factors for depression? Select all that apply.
a. Age 20-40 years
b. Positive family history
c. Separation or divorce
d. Death of family member
e. Chronic low self-esteem
f. Experience with abusive relationships
g. Third trimester of pregnancy
h. First 3 months after giving birth
Chapter 40. Depressive Disorders
MULTIPLE CHOICE
1. Which of the following is the mechanism by which the selective serotonin reuptake inhibitor (SSRI) antidepressant drugs appear to work?
a. Blocking reuptake of gamma-aminobutyric acid (GABA) and substance P
b. Blocking reuptake of serotonin and norepinephrine
c. Enhancing reuptake of serotonin and norepinephrine
d. Enhancing reuptake of GABA and substance P
2. The health care provider teaches a patient beginning tricyclic antidepressant drug therapy about measures to minimize the most serious common adverse drug effects. Which of the following adverse reactions is considered the most serious?
a. Orthostatic hypotension c. Blurred vision
b. Dry mouth d. Urinary retention
3. A patient receiving a tricyclic antidepressant complains of constipation. What is the health care provider’s interpretation of the patient’s complaint?
a. It is a sign of recovery from depression.
b. It is an attention-getting mechanism.
c. It is a common side effect of the drug.
d. It is an indication that this drug should be stopped.
4. A patient has begun taking fluoxetine (Prozac) for depression. When will the effects of the drug first be felt?
a. 5-7 days c. 1-2 months
b. 1-4 weeks d. 3-6 months
5. Phenelzine (Nardil) has been discontinued as a drug order for a patient. How much time must be observed before the patient can start a new drug?
a. 2 days c. 1 week
b. 5 days d. 2 weeks
6. The patient has been started on a treatment regimen which includes the use of lithium. As part of the teaching plan regarding lithium, the patient should be instructed that he should avoid:
a. Becoming sleep-deprived
b. Failing to exercise daily
c. Failing to stay on his prescribed dietary regimen
d. Becoming dehydrated
7. The patient has been started on a treatment regimen for acute mania. As part of the teaching plan for the patient and the family regarding use of the medication, they should be taught to immediately report which of the following symptoms to the primary care provider?
a. Deterioration of mental alertness c. Deterioration of sleep pattern
b. Deterioration of emotional stability d. Deterioration of eating pattern
8. An appropriate first-line drug for the treatment of depression with fatigue and low energy would be:
a. Venlafaxine (Effexor)
b. Escitalopram (Lexapro)
c. Buspirone (Buspar)
d. Amitriptyline (Elavil)
9. The laboratory monitoring required when a patient is on an SSRI is:
a. Complete blood count every 3 to 4 months
b. Therapeutic blood levels every 6 months after steady state is achieved
c. Blood glucose every 3 to 4 months
d. There is no laboratory monitoring required
10. Jaycee has been on escitalopram (Lexapro) for a year and is willing to try tapering off of the SSRI. What is the initial dosage adjustment when starting a taper off antidepressants?
a. Change dose to every other day dosing for a week
b. Reduce dose by 50% for 3 to 4 days
c. Reduce dose by 50% every other day
d. Escitalopram (Lexapro) can be stopped abruptly due to its long half-life
MULTIPLE RESPONSE
1. Which of the following are believed to be risk factors for depression? Select all that apply.
a. Age 20-40 years
b. Positive family history
c. Separation or divorce
d. Death of family member
e. Chronic low self-esteem
f. Experience with abusive relationships
g. Third trimester of pregnancy
h. First 3 months after giving birth
Chapter 42 Insomnia and Sleep Disorders
MULTIPLE CHOICE
1. A patient has a drug order for zolpidem (Ambien) written in the medical record. Which of the following conditions would the health care provider expect to see in the progress notes?
a. Anxiety disorder c. Muscle spasticity
b. Insomnia d. Seizure disorder
2. Which of the following is a common adverse effect of benzodiazepines (BZDs)?
a. Mental depression c. Cardiac palpitations
b. Suicidal ideation d. Daytime sedation
3. The patient has been placed on oxazepam (Serax). Which adverse reaction may be expected to occur with this drug?
a. Daytime sedation c. Diarrhea
b. Nausea d. Insomnia
4. Which of the following medications is the only drug available to treat sleep disorders during pregnancy?
a. Diazepam c. Diphenhydramine
b. Clonazepam d. Alprazolam
5. The patient is experiencing a reduction in her dosage of a benzodiazepine after 10 years of heavy use. Select the adverse effect which the health care provider expects will result from such a reduction.
a. Mania c. Constipation
b. Tachycardia d. Bradycardia
Chapter 43. Attention Deficit/Hyperactivity Disorder
Test Bank
MULTIPLE CHOICE
1. A patient is receiving dextroamphetamine (Dexedrine). Review the following symptoms, and select the one for which the health care provider assesses the patient.
a. Bradycardia c. Increased appetite
b. Lethargy d. Irritability
2. Which symptom would the health care provider expect to see in a patient receiving methamphetamine (Desoxyn)?
a. Decreased temperature c. Suppressed appetite
b. Increased blood pressure d. Relief of chest pain
3. A patient is receiving methylphenidate (Ritalin) for the treatment of narcolepsy. What long- term effects should the health care provider expect to monitor in this patient?
a. Drug tolerance c. Tachycardia
b. CNS excitation d. Tremors
4. When prescribing Adderall (amphetamine and dextroamphetamine) to adults with ADHD the nurse practitioner will need to monitor:
a. Blood pressure
b. Blood glucose levels
c. Urine ketone levels
d. Liver function
5. Monitoring for a child on methylphenidate for ADHD includes:
a. ADHD symptoms
b. Routine height and weight checks
c. Amount of methylphenidate being used
d. All of the above
6. Jack, age 8, has attention deficit disorder (ADD) and is prescribed methylphenidate (Ritalin). He and his parents should be educated about the side effects of methylphenidate, which are:
a. Slurred speech and insomnia
b. Bradycardia and confusion
c. Dizziness and orthostatic hypotension
d. Insomnia and decreased appetite
Chapter 44. Alzheimer’s Disease
MULTIPLE CHOICE
1.
1.A patient's medical record contains a drug order for tacrine (Cognex). Which condition would the health care provider expect to see in the patient’s health history?
A. Urinary retention C. Hepatic encephalopathy
B. Dementia of the Alzheimer's type
(DAT) D. Peptic Ulcer Disease
2.
A patient is experiencing an age-related decline in mental functioning. Which of the following substances may be helpful?
A. Echinacea C. Ginkgo
B. Hawthorn D. Ginger
3. Which of the following drugs used to treat Alzheimer’s disease is not an anticholinergic?
A. Donepezil
B. Memantine
C. Rivastigmine
D. Galantamine
4. Taking which drug with food maximizes it bioavailability?
A. Donepezil
B. Galantamine
C. Rivastigmine
D. Memantine
5. Because of their longer life expectancy, women are more likely than men to experience a disabling condition. Common conditions in older women that can produce disability include:
A. Depression
B. Panic disorders
C. Dementia
D. All of the above
Chapter 45. Diabetes Mellitus
MULTIPLE CHOICE
1. Type 1 diabetes results from autoimmune destruction of the beta cells. Eighty-five to 90 percent of Type 1 diabetics have:
A. Autoantibodies to two tyrosine phosphatases
B. Mutation of the hepatic transcription factor on chromosome 12
C. A defective glucokinase molecule due to a defective gene on chromosome 7p
D. Mutation of the insulin promoter factor
2. Type 2 diabetes is a complex disorder involving:
A. Absence of insulin production by the beta cells
B. A suboptimal response of insulin-sensitive tissues in the liver
C. Increased levels of glucagon-like peptide in the post-prandial period
D. Too much fat uptake in the intestine
3. Diagnostic criteria for diabetes include:
A. Fasting blood glucose greater than 140 mg/dl on two occasions
B. Post-prandial blood glucose greater than 140 mg/dl
C. Fasting blood glucose 100 to 125 mg/dl on two occasions
D. Symptoms of diabetes plus a casual blood glucose greater than 200 mg/dl
4. Routine screening of asymptomatic adults for diabetes is appropriate for:
A. Individuals who are older than 45 and have a BMI less than 25 kg/m2
B. Native Americans, African Americans, and Hispanics
C. Persons with HDL cholesterol greater than 100 mg/dl
D. Persons with pre-diabetes confirmed on at least two occasions
5. Screening criteria for children who meet the following criteria should begin at age 10 and occur every 3 years thereafter:
A. BMI above the 85th percentile for age and sex
B. Family history of diabetes in first- or second-degree relative
C. Hypertension based on criteria for children
D. Any of the above
6. Insulin is used to treat both types of diabetes. It acts by:
A. Increasing beta cell response to low blood glucose levels
B. Stimulating hepatic glucose production
C. Increasing peripheral glucose uptake by skeletal muscle and fat
D. Improving the circulation of free fatty acids
7. Adam has Type 1 diabetes and plays tennis for his university. He exhibits a Knowledge deficit about his insulin and his diagnosis. He should be taught that:
A. He should increase his CHO intake during times of exercise
B. Each brand of insulin is equal in bioavailability, so buy the least expensive
C. Alcohol produces hypoglycemia and can help control his diabetes when taken in
small amounts
D. If he does not want to learn to give himself injections, he may substitute an oral
hypoglycemic to control his diabetes
8. Insulin preparations are divided into categories based on onset, duration, and intensity of action following subcutaneous inject. Which of the following insulin preparations has the shortest onset and duration of action?
A. Insulin lispro
B. Insulin glulisine
C. Insulin glargine
D. Insulin detemir
9. The drug of choice for Type 2 diabetics is metformin. Metformin:
A. Decreases glycogenolysis by the liver
B. Increases the release of insulin from beta cells
C. Increases intestinal uptake of glucose
D. Prevents weight gain associated with hyperglycemia
10. Before prescribing metformin, the provider should:
A. Draw a serum creatinine level to assess renal function
B. Try the patient on insulin
C. Prescribe a thyroid preparation if the patient needs to lose weight
D. All of the above
11. Sulfonylureas may be added to a treatment regimen for Type 2 diabetics when lifestyle modifications and metformin are insufficient to achieve target glucose levels. Sulfonylureas have been moved to Step 2 therapy because they:
A. Increase endogenous insulin secretion
B. Have a significant risk for hypoglycemia
C. Address the insulin resistance found in Type 2 diabetics
D. Improve insulin binding to receptors
12. Dipeptidyl peptidase-4 inhibitors (gliptins) act on the incretin system to improve glycemic control. Advantages of these drugs include:
A. Better reduction in glucose levels than other classes
B. Less weight gain than sulfonylureas
C. Low risk for hypoglycemia
D. Can be given twice daily
13. Control targets for patients with diabetes include:
A. HbA1C between 7 and 8
B. Fasting blood glucose levels between 100 and 120 mg/dl
C. Blood pressure less than 130/80 mm Hg
D. LDL lipids less than 130 mg/dl
14. Establishing glycemic targets is the first step in treatment of both types of diabetes. For Type 1 diabetes:
A. Tight control/intensive therapy can be given to adults who are willing to test their
blood glucose at least twice daily
B. Tight control is acceptable for older adults if they are without complications
C. Plasma glucose levels are the same for children as adults
D. Conventional therapy has a fasting plasma glucose target between 120 and 150
mg/dl
15. Treatment with insulin for Type 1 diabetics:
A. Starts with a total daily dose of 0.2 to 0.4 units per kg of body weight
B. Divides the total doses into three injections based on meal size
C. Uses a total daily dose of insulin glargine given once daily with no other insulin
required
D. Is based on the level of blood glucose
16. When the total daily insulin dose is split and given twice daily, which of the following rules may be followed?
A. Give two-thirds of the total dose in the morning and one-third in the evening.
B. Give 0.3 units per kg of premixed 70/30 insulin with one-third in the morning and
two-thirds in the evening.
C. Give 50% of an insulin glargine dose in the morning and 50% in the evening.
D. Give long-acting insulin in the morning and short-acting insulin at bedtime.
17. Studies have shown that control targets that reduce the HbA1C to less than 7% are associated with fewer long-term complications of diabetes. Patients who should have such a target include:
A. Those with long-standing diabetes
B. Older adults
C. Those with no significant cardiovascular disease
D. Young children who are early in their disease
18. Prevention of conversion from pre-diabetes to diabetes in young children must take highest priority and should focus on:
A. Aggressive dietary manipulation to prevent obesity
B. Fostering LDL levels less than 100 mg/dl and total cholesterol less than 170 mg/dl
to prevent cardiovascular disease
C. Maintaining a blood pressure that is less than 80% based on weight and height to
prevent hypertension
D. All of the above
19. The drugs recommended by the American Academy of Pediatrics for use in children with diabetes (depending upon type of diabetes) are:
A. Metformin and insulin
B. Sulfonylureas and insulin glargine
C. Split-mixed dose insulin and GPL-1 agonists
D. Biguanides and insulin lispro
20. Unlike most Type 2 diabetics where obesity is a major issue, older adults with low body weight have higher risks for morbidity and mortality. The most reliable indicator of poor nutritional status in older adults is:
A. Weight loss in previously overweight persons
B. Involuntary loss of 10% of body weight in less than 6 months
C. Decline in lean body mass over a 12-month period
D. Increase in central versus peripheral body adiposity
21. The drugs recommended for older adults with Type 2 diabetes include:
A. Second generation sulfonylureas
B. Metformin
C. Pioglitazone
D. Third generation sulfonylureas
22. Ethnic groups differ in their risk for and presentation of diabetes. Hispanics:
A. Have a high incidence of obesity, elevated triglycerides, and hypertension
B. Do best with drugs that foster weight loss, such as metformin
C. Both A and B
D. Neither A nor B
23. The American Heart Association states that people with diabetes have a 2- to 4-fold increase in the risk of dying from cardiovascular disease. Treatments and targets that do not appear to decrease risk for micro- and macro-vascular complications include:
A. Glycemic targets between 7% and 7.5%
B. Use of insulin in Type 2 diabetics
C. Control of hypertension and hyperlipidemia
D. Stopping smoking
24. All diabetic patients with known cardiovascular disease should be treated with:
A. Beta blockers to prevent MIs
B. ACE inhibitors and aspirin to reduce risk of cardiovascular events
C. Sulfonylureas to decrease cardiovascular mortality
D. Pioglitazone to decrease atherosclerotic plaque buildup
25. All diabetic patients with hyperlipidemia should be treated with:
A. HMG-CoA reductase inhibitors
B. Fibric acid derivatives
C. Nicotinic acid
D. Colestipol
26. Both ACE inhibitors and some Angiotensin-II receptor blockers have been approved in treating:
A. Hypertension in diabetic patients
B. Diabetic nephropathy
C. Both A and B
D. Neither A nor B
27. Protein restriction helps slow the progression of albuminuria, GFR decline, and ESRD is some patients with diabetes. It is useful for patients who:
A. Cannot tolerate ACE inhibitors or ARBs
B. Have uncontrolled hypertension
C. Have HbA1C levels above 7%
D. Show progression of diabetic nephropathy despite optimal glucose and blood
pressure control
28. Diabetic autonomic neuropathy (DAN) is the earliest and most common complication of diabetes. Symptoms associated with DAN include:
A. Resting tachycardia, exercise intolerance, and orthostatic hypotension
B. Gastroparesis, cold intolerance, and moist skin
C. Hyperglycemia, erectile dysfunction, and deficiency of free fatty acids
D. Pain, loss of sensation, and muscle weakness
29. Drugs used to treat diabetic peripheral neuropathy include:
A. Metoclopramide
B. Cholinergic agonists
C. Cardioselective beta blockers
D. Gabapentin
30. The American Diabetic Association has recommended which of the following tests for ongoing management of diabetes?
A. Fasting blood glucose
B. HbA1C
C. Thyroid function tests
D. Electrocardiograms
Chapter 46. Thyroid Disorders
MULTIPLE CHOICE
1. When methimazole is started for hyperthyroidism it may take to see total reversal of hyperthyroid symptoms.
A. 2 to 4 weeks
B. 1 to 2 months
C. 3 to 4 months
D. 6 to 12 months
2. In addition to methimazole, a symptomatic patient with hyperthyroidism may need a prescription for:
A. A calcium channel blocker
B. A beta blocker
C. Liothyronine
D. An alpha blocker
3. After starting a patient with Grave’s disease on an antithyroid agent such as methimazole, patient monitoring includes TSH and free T4 every:
A. 1 to 2 weeks
B. 3 to 4 weeks
C. 2 to 3 months
D. 6 to 9 months
4. A woman who is pregnant and has hyperthyroidism is best managed by a specialty team who will most likely treat her with:
A. Methimazole
B. Propylthiouracil (PTU)
C. Radioactive iodine
D. Nothing, treatment is best delayed until after her pregnancy ends
5. Goals of treatment when treating hypothyroidism with thyroid replacement include:
A. Normal TSH and free T4 levels
B. Resolution of fatigue
C. Weight loss to baseline
D. All of the above
6. When starting a patient on levothyroxine for hypothyroidism the patient will need follow-up measurement of thyroid function in:
A. 2 weeks
B. 4 weeks
C. 2 months
D. 6 months
7. Once a patient who is being treated for hypothyroidism returns to euthyroid with normal TSH levels, he or she should be monitored with TSH and free T4 levels every:
A. 2 weeks
B. 4 weeks
C. 2 months
D. 6 months
8. Treatment of a patient with hypothyroidism and cardiovascular disease consists of:
A. Levothyroxine
B. Liothyronine
C. Liotrix
D. Methimazole
9. Infants with congenital hypothyroidism are treated with:
A. Levothyroxine
B. Liothyronine
C. Liotrix
D. Methimazole
10. When starting a patient with hypothyroidism on thyroid replacement hormones patient education would include:
A. They should feel symptomatic improvement in 1 to 2 weeks
B. Drug adverse effects such as lethargy and dry skin may occur
C. It may take 4 to 8 weeks to get to euthyroid symptomatically and by lab testing
D. Due to its short half-life, levothyroxine doses should not be missed
.Which of the following drugs inhibits the synthesis of thyroid hormones and reduces peripheral conversion of T4 to the more potent T3?
a. Liotrix (Thyrolar) c. Methimazole (Tapazole)
b. Levothyroxine (Synthroid) d. Propylthiouracil (PTU)
11. Which serious adverse effects of propylthiouracil (PTU) would have to be reported to the health care provider immediately?
a. Increased urine output and thirst c. Sore throat and fever
b. Dizziness and hallucinations d. Abdominal pain and constipation
12 Which effect is associated with thyroid replacement hormones such as levothyroxine (Levothroid)?
a. Increase in the metabolic rate of body tissues
b. Inhibition of gluconeogenesis
c. Decrease in utilization and mobilization of glycogen stores
d. Inhibition of protein synthesis and cell growth
13. Which group of symptoms may be indicative of overdosage in a patient taking a thyroid replacement hormone?
a. Bradycardia, somnolence, and ataxia c. Tachycardia, insomnia, and
nervousness
b. Dry skin, tremors, and weight gain d. Sneezing, coughing, and neck pain
14. A patient is undergoing thyroid replacement therapy with levothyroxine (Levothroid). At what time should the health care provider instruct the patient to take this drug?
a. Immediately after breakfast or lunch c. With the last meal of the day
b. Before breakfast on an empty stomach d. At bedtime on an empty stomach
15. A home care patient taking levothyroxine (Synthroid) measures the pulse, finds it to be 110 beats per minute, and notifies his health care provider. Which action would be the most appropriate response of the health care provider?
a. Withhold the dose, and notify the prescriber of the drug.
b. Skip the daily dose, and resume the following day.
c. Take the drug every other day for 1 week.
d. Discontinue the drug altogether.
Chapter 47. Allergies and Allergic Reactions
MULTIPLE CHOICE
1. The term allergy is derived from the word allos
A. Greek C. French
B. Latin D. Russian
2. Your teaching a group of grade-school children about body functions. A student asks, "Why do I sneeze?" The nurse's best response is:
A. "A sneeze is caused by a contraction of your throat and lungs." C. "A sneeze is your body's way of getting rid of something irritating."
B. "The back part of your brain is in charge of sneezes and coughs” D. "You sneeze because your body needs to take a really deep breath."
3. The nurse is planning care for a client with allergies who has an order for a sympathomimetic drug. The nurse is aware that the desired effect for this client is:
A. Relief of nasal dryness. C. Relief of nasal stuffiness.
B. Calming of a wet cough. D. Increased blood flow to the nose.
4. Which assessment data would provide the nurse with the best evidence of allergic rhinitis?
A. Copious thick, green nasal drainage and postnasal drip C. Coughing, sneezing, and watery eyes
B. Productive cough, sneezing, and low- grade fever D. Severe frontal headache and pressure along both sides of the nose
5. The nurse is administering an antihistamine to a client with nasal allergies. The nurse is aware that antihistamines have which distinct limitation?
A. They have potent cholinergic side effects. C. They are most effective when taken prophylactically.
B. They block both H-1 and H-2 receptors. D. They are useful only during acute attacks.
6. The nurse is teaching a client about the use of antihistamines for allergic rhinitis. Which pointer is appropriate for increasing effectiveness?
A. "Take this drug before you are exposed to your allergens." C. "Take this drug when your symptoms are the worst."
B. "Take this drug with the largest meal of the day." D. "Take this drug at the same time every day."
7. Patients with allergic rhinitis may benefit from a prescription of:
A. Fluticasone (Flonase)
B. Cetirizine (Zyrtec)
C. OTC cromolyn nasal spray (Nasalcrom)
D. Any of the above
8. Howard is a 72-year-old male who occasionally takes diphenhydramine for his seasonal allergies. Monitoring for this patient taking diphenhydramine would include assessing for:
A. Urinary retention
B. Cardiac output
C. Peripheral edema
D. Skin for rash
9. First generation antihistamines such as loratadine (Claritin) are prescribed for seasonal allergies because they are:
A. More effective than first generation antihistamines
B. Less sedating than the first generation antihistamines
C. Prescription products, therefore are covered by insurance
D. Able to be taken with CNS sedatives, such as alcohol
Chapter 48. Human Immunodeficiency Virus
MULTIPLE CHOICE
1. The goals of treatment when prescribing antiretroviral medication to patients with HIV include:
A. Prevent vertical HIV transmission
B. Improve quality of life
C. Prolong survival
D. All of the above
2. A challenge faced with antiretroviral therapy (ART) is:
A. Patients abusing ART
B. Drug-resistant mutations of HIV
C. Reduction of transmissibility of HIV
D. Lack of efficacy data
3. Predictors for successful treatment with antiretroviral therapy (ART) in HIV-positive patients include:
A. They respond to low potency treatment regimen
B. They have demonstrated resistance in the past and should respond to newer ART
drugs
C. The patient is strictly adherent to the ART treatment regimen
D. Lower baseline CD4 T-cell count at baseline
4. The goal of antiretroviral therapy (ART) in HIV-positive patients is:
A. Maximum suppression of HIV replication
B. Eradication of HIV virus from the body
C. Determining a treatment regimen that is free of adverse effects
D. Suppression of CD4 T-cell count
5. Pregnant women who are HIV positive:
A. Are treated with AZT alone to prevent birth defects
B. Are treated with a combination ART regimen
C. Should not be treated with ART due to teratogenicity of the drugs
D. Are at high risk of developing resistance to ART drugs
6. Antiretroviral therapy is recommended for HIV-positive patients with:
A. A history of AIDS-defining illness
B. Pregnant women
C. Hepatitis B co-infection
D. All of the above
7. If considering starting a patient on the nucleoside reverse transcriptase inhibitor (NRTI) abacavir, the following testing is recommended prior to prescribing:
A. Renal function
B. HLA B*5701 testing
C. Pancreatic enzyme levels
D. CYP 450 enzyme activity
8. Suzanne is pregnant and has tested HIV positive. Which antiretroviral drug should be avoided in women who are pregnant?
A. Lopinavir/r
B. Zidovudine
C. Ritonavir
D. Lopinavir/ritonavir
9. The cost of HIV treatment can be prohibitive for any patient. Patients can receive assistance from the:
A. Best Pharmaceuticals for HIV/AIDS Patient Act
B. Ryan White HIV/AIDS Treatment Modernization Act
C. National Institute of Health HIV/AIDS Assistance Fund
D. Centers for Disease Control HIV/AIDS Treatment Fund
10. Resistance to antiretroviral therapy (ART) is measured by:
A. Measuring the DNA viral load in the serum
B. Determining plasma viral RNA on two successive measurements
C. Phenotype assays of the combination of ART the patient is on
D. Elevation of T4 counts
11. Phenotype assays are used to measure of antiretroviral therapy (ART).
A. Effectiveness
B. Genotype
C. Sensitivity
D. Hypersensitivity susceptibility
12. Patient factors that contribute to antiretroviral therapy (ART) failure include:
A. Being a male who has sex with males
B. HIV diagnosis in pregnancy
C. Good compliance with ART treatment regimen
D. ART adverse effects
13. Patients who are taking antiretroviral therapy (ART) need to have the following monitored:
A. Lipid levels
B. Sexual functioning
C. Platelet count
D. All of the above
14. Successful antiretroviral therapy (ART) in an HIV-positive patient is determined by:
A. Being able to stop ART therapy due to HIV virus eradication
B. Lowering HIV viral load to unmeasurable amounts
C. Individual measures of success based on their personal situation
D. Normal blood hematologic factors
Chapter 49. Coagulation Disturbances
MULTIPLE CHOICE
1. Assessment for deep vein thrombosis (DVT) is a priority for which client?
a. A client with a gastric ulcer c. A client recovering from a knee replacement
b. A client with hypertension d. A client with pneumonia
2. The nurse is addressing a group of clients who have experienced thromboembolic disorders. One of the clients states, “My dad had a problem with clotting too much and so does my brother.” Before responding to this comment, the nurse considers which information?
a. A genetic deficiency of protein C can produce hypercoagulability.
b. Familial eating habits can result in deficiency of vitamin C that would increase clotting.
c. Genetic deficiency of C peptide is implicated in clotting disorders.
d. If there is a genetic tendency to decreased C reactive protein (CRP) the clotting cascade is enhanced.
3. The client states, "I’ve never had such trouble breathing. What is a pulmonary embolus anyway?" What is the best nursing response?
a. "A pulmonary embolus is a stationary blood clot that formed in your lung."
b. "An embolus is a piece of the injured blood vessel that is moving in your lung."
c. "A pulmonary embolus is a portion of a blood clot that has moved from its original location to your lung."
d. "A pulmonary embolus is an area of tissue in your lung that has lost its blood supply and has become necrotic."
4. The nurse is planning a teaching session for a client newly diagnosed with hemophilia A. Which information should be included?
a. An extra protein is present that breaks down clots too quickly.
b. A substance that is part of the clotting process is missing.
c. The blood is missing a substance that inhibits clotting.
d. There are not enough platelets present.
5. Which class of drugs would the nurse expect to be administered to a client who is bleeding excessively at a surgical site?
a. Thrombolytics c. Anticoagulants
b. Antifibrinolytics d. Prothrombin activators
Question 6
PTS: 1
6. A clinic nurse is developing a teaching handout for clients who are prescribed warfarin (Coumadin) therapy. Which statement should be included in this information? Select all that apply.
a. “Tell your dentist you are taking warfarin prior to any procedures.”
b. “Report to the lab for testing of activated partial thromboplastin time (APTT).”
c. “Avoid strenuous activities.”
d. “Place ice at the injection site if stinging or burning occurs.”
5. “Take nonsteroidal anti-inflammatories (NSAIDs) for minor pain relief.”
PTS: 1
7. A client is receiving intermittent intravenous heparin therapy to treat deep vein thrombosis (DVT). Which laboratory value should the nurse review prior to administering this medication?
a. Prothrombin time (PT) c. Activated partial thromboplastin time (APTT)
b. Fibrinogen level d. Factor VIII level
8. The baseline international normalized ratio (INR) of a client started on warfarin (Coumadin) for atrial fibrillation was A.B. The nurse notes that the INR value is B.5 prior to administration of the next dose of medication. What should the nurse do?
a. Administer the antidote and observe for bleeding.
b. Notify the health care provider so that the dose can be increased.
c. Administer the medication as ordered.
d. Hold medication and contact the health care provider.
Chapter 50. Anemias
MULTIPLE CHOICE
1. Pernicious anemia is treated with:
A. Folic acid supplement
B. Thiamine supplement
C. Vitamin B12
D. Iron
2. Premature infants require iron supplementation with:
A. 10 mg/day of iron
B. 2 mg/kg per day until age 12 months
C. 7 mg/day in diet
D. 1 mg/kg per day until adequate intake of iron from foods
3. Breastfed infants should receive iron supplementation of:
A. 3 mg/kg per day
B. 6 mg/kg per day
C. 1 mg/kg per day
D. Breastfed babies do not need iron supplementation
4. Valerie presents to clinic with menorrhagia. Her hemoglobin is 10.2 and her ferritin is 15 ng/mL. Initial treatment for her anemia would be:
A. 18 mg/day of iron supplementation
B. 6 mg/kg per day of iron supplementation
C. 325 mg ferrous sulfate per day
D. 325 mg ferrous sulfate TID
5. Chee is a 15-month-old male whose screening hemoglobin is 10.4 g/dL. Treatment for his anemia would be:
A. 18 mg/day of iron supplementation
B. 6 mg/kg per day of elemental iron
C. 325 mg ferrous sulfate per day
D. 325 mg ferrous sulfate TID
6. Monitoring for a patient taking iron to treat iron deficiency anemia is:
A. Hemoglobin, hematocrit, and ferritin 4 weeks after treatment is started
B. Complete blood count every 4 weeks throughout treatment
C. Annual complete blood count
D. Reticulocyte count in 4 weeks
7. Valerie has been prescribed iron to treat her anemia. Education of patients prescribed iron would include:
A. Take the iron with milk if it upsets her stomach
B. Antacids may help with the nausea and GI upset caused by iron
C. Increase fluids and fiber to treat constipation
D. Iron is best tolerated if it is taken at the same time as her other medications
8. Allie has just had her pregnancy confirmed and is asking about how to ensure a healthy baby. What is the folic acid requirement during pregnancy?
A. 40 mcg/day
B. 400 mcg/day
C. 800 mcg/day
D. 2 gm/day
9. Kyle has Crohn’s disease and has a documented folate deficiency. Drug therapy for folate deficiency anemia is:
A. Oral folic acid 1 to 2 mg per day
B. Oral folic acid 1 gram per day
C. IM folate weekly for at least 6 months
D. Oral folic acid 400 mcg daily
10. Patients who are being treated for folate deficiency require monitoring of:
A. Complete blood count every 4 weeks
B. Hematocrit and hemoglobin at 1 week and then at 8 weeks
C. Reticulocyte count at 1 week
D. Folate levels every 4 weeks until hemoglobin stabilizes
11. The treatment of vitamin B12 deficiency is:
A. 1,000 mcg daily of oral cobalamin
B. 2 gm per day of oral cobalamin
C. 100 mcg/day Vitamin B12 IM
D. 500 mcg/dose nasal cyanocobalamin 2 sprays once a week
12. The dosage of Vitamin B12 to initially treat pernicious anemia is:
A. Nasal cyanocobalamin 1 gram spray in each nostril daily x 1 week then weekly x 1
month
B. Vitamin B12 IM monthly
C. Vitamin B12 1,000 mcg IM daily x 1 week then 1,000 mg weekly for a month
D. Oral cobalamin 1,000 mcg daily
13. Before beginning IM Vitamin B12 therapy, which laboratory values should be obtained?
A. Reticulocyte count, hemoglobin, and hematocrit
B. Iron
C. Vitamin B12
D. All of the above
14. should be monitored when Vitamin B12 therapy is started.
A. Serum calcium
B. Serum potassium
C. Ferritin
D. C-reactive protein
15. Anemia due to chronic renal failure is treated with:
A. Epoetin alfa (Epogen)
B. Ferrous sulfate
C. Vitamin B12
D. Hydroxyurea
Chapter 51. Immunizations Chapter 53. Travel Medications
MULTIPLE CHOICE
1. Attenuated vaccines are also known as:
A. Killed vaccines
B. Booster vaccines
C. Inactivated vaccines
D. Live vaccines
2. Live attenuated influenza vaccine (FluMist) may be administered to:
A. All patients over 6 months of age
B. Patients between age 2 years and 49 years with no risk factors
C. Patients with a URI or asthma
D. Pregnant women
3. The reason that two MMR vaccines at least a month apart are recommended is:
A. The second dose of MMR “boosts” the immunity built from the first dose
B. Two vaccines 1 month apart is the standard dosing for all live virus vaccines
C. If the two MMR vaccine doses are given too close together there is a greater
likelihood of severe localized reaction to the vaccine
D. Only 95% of patients are fully immunized for measles after the first vaccine, with
99% having immunity after two doses of MMR
4. MMR vaccine is not recommended for pregnant women because:
A. Pregnant women do not build adequate immunity to the vaccine
B. There is a risk of the pregnant women developing measles encephalopathy
C. There is a risk of the fetus developing congenital rubella syndrome
D. Pregnant women can receive the MMR vaccine
5. If the MMRV (measles, mumps, rubella, and varicella) combined vaccine is ordered to be given as the first MMR and varicella dose to a child the CDC recommends:
A. Parents be informed of the increased risk of fever and febrile seizures over the
MMR plus varicella 2 shot regimen
B. Patients must also receive MMRV as the second dose of MMR and varicella in order to build adequate immunity
C. Patients be premedicated with acetaminophen 15 minutes before the vaccine is
given
D. Patients should not be around pregnant women for the first 48 hours after the
vaccine is given
6. The rotavirus vaccine (RotaTeq, Rotarix):
A. Is a live vaccine that replicates in the small intestine, providing active immunity
against rotavirus
B. Should not be administered to infants who are or may be potentially
immunocompromised
C. Is not given to an infant who has a febrile illness (temperature greater than
100.5°F)
D. All of the above
7. Varicella vaccine is recommended to be given to patients who are:
A. HIV positive with a CD4+ T-lymphocyte percentage less than 15 percent
B. Taking corticosteroids (up to 2 mg/kg/day or less than 20 mg/day)
C. Pregnant
D. Immunocompromised
8. Zoster vaccine (Zostavax) is:
A. A live varicella zoster vaccine from the same strain used to develop the varicella
vaccine
B. Effective in preventing varicella zoster in patients of all ages
C. Recommended for patients age 40 to 80 who have had chickenpox
D. Administered at the same time as other live vaccines, as long as they are given the
same day
9. True contraindications to diphtheria, tetanus, and acellular pertussis (DTaP or Tdap) vaccine include:
A. Fever up to 104°F (40.5°C) after previous DTaP vaccine
B. Family history of seizures after DTaP vaccine
C. Adolescent pregnancy
D. Anaphylactic reaction with a previous dose
10. Hepatitis B vaccine (HBV) is contraindicated in patients who:
A. Were born less than 32 weeks gestation (give first dose at age 6 months)
B. Are pregnant
C. Are on hemodialysis
D. Are allergic to yeast
11. Human papillomavirus (HPV) vaccine (Gardasil, Cervarix):
A. Is a live virus vaccine that provides immunity to six strains of HPV virus
B. Has a common adverse effect of syncope within 15 minutes of giving the vaccine
C. Should not be given to males younger than age 12 years
D. May be given to pregnant women
12. Influenza vaccine may be administered annually to:
A. Patients with egg allergy
B. Pregnant patients
C. Patients age 6 weeks or older
D. Patients with acute febrile illness
13. Immune globulin serums (IGs):
A. Provide active immunity against infectious diseases
B. Are contraindicated during pregnancy
C. Are heated to above body temperature to kill most hepatitis, HIV, and other viruses
such as parvovirus
D. Are derived from pooled plasma of adults and contain specific antibodies in
proportion to the donor population
14. Hepatitis B immune globulin (HBIG) is administered to provide passive immunity to:
A. Infants born to HBsAg-positive mothers
B. Household contacts of hepatitis-B virus infected people
C. Persons exposed to blood containing hepatitis B virus
D. All of the above
15. Rho(D) immune globulin (RhoGAM) is given to:
A. Infants born to women who are Rh positive
B. Sexual partners of Rh positive women
C. Rh negative women after a birth, miscarriage, or abortion
D. Rh negative women at 36 weeks gestation
16. Tuberculin purified protein derivative (PPD):
A. Is administered to patients who are known tuberculin-positive reactors
B. May be administered to patients who are on immunosuppressives
C. May be administered 2 to 3 weeks after an MMR or varicella vaccine
D. May be administered the same day as the MMR and/or varicella vaccine
17. Azathioprine has significant adverse drug effects, including:
A. Hypertension
B. Hirsutism
C. Risk of cancer
D. Gingival hyperplasia
Chapter 52. Smoking Cessation
MULTIPLE CHOICE
1. Nicotine withdrawal symptoms include:
A. Nervousness
B. Increased appetite
C. Difficulty concentrating
D. All of the above
2. If a patient wants to quit smoking, nicotine replacement therapy is recommended if the patient:
A. Smokes more than 10 cigarettes a day
B. Smokes within 30 minutes of awakening in the morning
C. Smokes when drinking alcohol
D. All of the above
3. Instructions for a patient who is starting nicotine replacement therapy include:
A. Smoke less than 10 cigarettes a day when starting nicotine replacement
B. Nicotine replacement will help with the withdrawal cravings associated with
quitting tobacco
C. Nicotine replacement can be used indefinitely
D. Nicotine replacement therapy is generally safe for all patients
4. Nicotine replacement therapy should not be used in which patients?
A. Pregnant women
B. Patients with worsening angina pectoris
C. Immediately after an acute myocardial infarction
D. All of the above
5. Instructions for the use of nicotine gum include:
A. Chew the gum quickly to get a peak effect
B. The gum should be “parked” in the buccal space between chewing
C. Acidic drinks such as coffee help with the absorption of the nicotine
D. The highest abstinence rates occur if the patient chews the gum when he or she is
having cravings
6. Patients who choose the nicotine lozenge to assist in quitting tobacco should be instructed:
A. Chew the lozenge well
B. Drink at least 8 ounces of water after the lozenge dissolves
C. Use one lozenge every 1 to 2 hours (at least nine per day with a maximum of
twenty per day)
D. A tingling sensation in the mouth should be reported to the provider
7. Transdermal nicotine replacement (patch) is an effective choice in tobacco cessation because:
A. The patch provides a steady level of nicotine without reinforcing oral aspects of
smoking
B. There is the ability to “fine tune” the amount of nicotine that is delivered to the
patient at any one time
C. There is less of a problem with nicotine toxicity than other forms of nicotine
replacement
D. Transdermal nicotine is safer in pregnancy
8. The most common adverse effect of the transdermal nicotine replacement patch is:
A. Nicotine toxicity
B. Tingling at the site of patch application
C. Skin irritation under the patch site
D. Life-threatening dysrhythmias
9. If a patient is exhibiting signs of nicotine toxicity when using transdermal nicotine, they should remove the patch and:
A. Wash the area thoroughly with soap and water
B. Flush the area with clear water
C. Reapply a new patch in 8 hours
D. Take acetaminophen for the headache associated with toxicity
10. When a patient is prescribed nicotine nasal spray for tobacco cessation, instructions include:
A. Inhale deeply with each dose to ensure deposition in the lungs
B. The dose is one to two sprays in each nostril per hour, not to exceed 40 sprays per
day
C. If they have a sensation of “head rush” this indicates the medication is working
well
D. Nicotine spray may be used for up to 12 continuous months
11. If prescribing bupropion (Zyban) for tobacco cessation, the instructions to the patient include:
A. Bupropion (Zyban) is started 1 to 2 weeks before the quit date
B. Nicotine replacement products should not be used with bupropion
C. If they smoke when taking bupropion they may have increased anxiety and
insomnia
D. Since they are not using bupropion as an antidepressant, they do not need to worry
about increased suicide ideation when starting therapy
12. Varenicline (Chantix) may be prescribed for tobacco cessation. Instructions to the patient who is starting varenicline include:
A. The maximum time varenicline can be used is 12 weeks
B. Nausea is a sign of varenicline toxicity and should be reported to the provider
C. The starting regimen for varenicline is start taking 1 mg twice a day a week before
the quit date
D. Neuropsychiatric symptoms may occur
13. The most appropriate smoking cessation prescription for pregnant women is:
A. Nicotine replacement patch at lowest dose available
B. Bupropion (Zyban)
C. Varenicline (Chantix)
D. Nonpharmacologic measures
Chapter 54. Weight Loss
MULTIPLE CHOICE
1. The most useful estimate of body fat is the patient’s
a. waist circumference. c. overall risk status.
b. body weight. d. BMI.
2. The patient is a morbidly obese woman who has been placed on the anorexiant sibutramine. She tells her primary health care provider that she has noted her level of depression to be improved. The provider tells her that this is
a. indicative that the medication is approaching a toxic level.
b. indicative that the patient is unable to tolerate a sufficient dose of the medication.
c. a desirable side effect of the medication.
d. a hypersensitivity reaction to the medication.
3. The patient has implemented a weight loss program that includes the setting of monthly weight loss goals for monitoring and motivational purposes. The primary health care provider explains to the patient that a realistic goal would be a monthly weight loss of
a. 0.5 to 1 pound. c. 5 to 7 pounds.
b. 2 to 4 pounds. d. 8 to 10 pounds.
4. The patient’s weight loss regimen includes treatment with the anorexiant medication sibutramine. Before beginning treatment with this drug, the primary health care provider instructs the patient that the maximum amount of time that she can remain on the drug is
a. 1 month. c. 1 year.
b. 6 months. d. 2 years.
5. The patient recently has been started on a treatment regimen that includes the drug Orlistat. The primary health care provider instructs the patient that as a side effect of the medication, she should expect
a. constipation. c. soft liquid stool.
b. blood-streaked stool. d. tarry black stool.
6. The patient asks his primary health care provider about his opinion of the over-the-counter weight loss products that contain ephedrine. The provider cautions the patient that ephedrine has been found to cause
a. stroke. c. hypotension.
b. bradycardia. d. chronic heart failure.
MULTIPLE RESPONSE
1. Select the conditions that put the patient at increased risk from obesity or overweight.
a. Diabetes mellitus
b. Sleep apnea
c. Gallstones
d. Kidney stones
e. Coronary artery disease
f. Hypotension
g. Osteoarthritis
Chapter 55. Contraception
MULTIPLE CHOICE
1. Women who are taking an oral contraceptive containing the progesterone drospirenone may require monitoring of:
A. Hemoglobin
B. Serum calcium
C. White blood count
D. Serum potassium
2. The mechanism of action of oral combined contraceptives which prevents pregnancy is:
A. Estrogen prevents the LH surge necessary for ovulation
B. Progestins thicken cervical mucous and slow tubal motility
C. Estrogen thins the endometrium making implantation difficult
D. Progestin suppresses FSH release
3. To improve actual effectiveness of oral contraceptives women should be educated regarding:
A. Use of a back-up method if they have vomiting or diarrhea during a pill packet
B. Doubling pills if they have diarrhea during the middle of a pill pack
C. They will have a normal menstrual cycle if they miss two pills
D. Mid-cycle spotting is not normal and the provider should be contacted immediately
4. A contraindication to the use of combined contraceptives is:
A. Adolescence (not approved for this age)
B. A history of clotting disorder
C. Recent pregnancy
D. Overweight
5. Obese women may have increased risk of failure with which contraceptive method?
A. Combined oral contraceptives
B. Progestin-only oral contraceptive pill
C. Injectable progestin
D. Combined topical patch
6. Ashley comes to clinic with a request for oral contraceptives. She has successfully used oral contraceptives before and has recently started dating a new boyfriend so would like to restart contraception. She denies recent intercourse and has a negative urine pregnancy test in the clinic. An appropriate plan of care would be:
A. Recommend she return to the clinic at the start of her next menses to get a Depo
Provera shot
B. Prescribe oral combined contraceptives and recommend she start them at the
beginning of her next period and use a back-up method for the first 7 days
C. Prescribe oral contraceptives and have her start them the same day with a back-up
method used for the first 7 days
D. Discuss the advantages of using the topical birth control patch and recommend she
consider using the patch
7. When discussing with a patient the different start methods used for oral combined contraceptives, the advantage of a Sunday start over the other start methods is:
A. Immediate protection against pregnancy the first week of using the pill
B. No back-up method is needed when starting
C. Menses occur during the week
D. They can start the pill on the Sunday after the office visit
8. The topical patch combined contraceptive (Ortho Evra) is:
A. Started on the first day of the menstrual cycle
B. Recommended for women over 200 pounds
C. Is not as effective as oral combined contraceptives
D. Has more adverse effects, such as nausea, than the oral combined contraceptives
9. Progesterone-only pills are recommended for women who:
A. Are breastfeeding
B. Have a history of migraine
C. Have a medical history that contradicts the use of estrogen
D. All of the above
10. Women who are prescribed progestin-only contraception need education regarding which common adverse drug effects?
A. Increased migraine headaches
B. Increased risk of developing blood clots
C. Irregular vaginal bleeding for the first few months
D. Increased risk for hypercalcemia
11. An advantage of using the NuvaRing vaginal ring for contraception is:
A. It does not require fitting and is easy to insert
B. It is inserted once a week, eliminating the need to remember to take a daily pill
C. Patients get a level of estrogen and progestin equal to combined oral
contraceptives
D. All of the above
12. Oral emergency contraception (Plan B) is contraindicated in women who:
A. Had intercourse within the past 72 hours
B. May be pregnant
C. Are taking combined oral contraceptives
D. Are using a diaphragm
Chapter 56. Menopause and Menopausal Hormone Therapy
MULTIPLE CHOICE
1. The goals of therapy when prescribing hormone replacement therapy (HRT) include reducing:
A. Cardiovascular risk
B. Risk of stroke or other thromboembolic event
C. Breast cancer
D. Vasomotor symptoms
2. The optimal maximum time frame for hormone replacement therapy (HRT) or estrogen replacement therapy (ERT) is:
A. 2 years
B. 5 years
C. 10 years
D. 15 years
3. Dosage changes of conjugated equine estrogen (Premarin) are made at intervals.
A. 1 to 2 week
B. 2 to 4 week
C. 6 to 8 week
D. 12 week
4. The advantage of vaginal estrogen preparations in the treatment of vulvovaginal atrophy and dryness is:
A. Ability to deliver higher doses of estrogen in a non-oral form
B. The vaginal cream formula provides moisture to the vaginal area
C. Relief of symptoms without increasing cardiovascular risk
D. All of the above
5. Women with an intact uterus should be treated with both estrogen and progestin due to:
A. Increased risk for endometrial cancer if estrogen alone is used
B. Combination therapy provides the best relief of menopausal vasomotor symptoms
C. Reduced risk for colon cancer with combined therapy
D. Lower risk of developing blood clots with combined therapy
6. Ongoing monitoring for women on estrogen replacement therapy (ERT) includes:
A. Lipid levels, repeated annually if abnormal
B. Annual health history and review of risk profile
C. Annual mammogram
D. All of the above
7. Kristine would like to start hormone replacement therapy (HRT) to treat the significant vasomotor symptoms she is experiencing during menopause. Education for a woman considering hormone replacement would include:
A. Explaining that HRT is totally safe if used short term
B. Telling her to ignore media hype regarding HRT
C. Discussing the advantages and risks of HRT
D. Encouraging the patient to use phytoestrogens with the HRT
8. Angela is a black woman who has heard that women of African descent do not need to worry about osteoporosis. What education would you provide Angela about her risk?
A. She is correct, black women do not have much risk of developing osteoporosis due
to their dark skin
B. Black women are at risk of developing osteoporosis due to their lower calcium
intake as a group
C. If she doesn’t drink alcohol, her risk of developing osteoporosis is low
D. If she has not lost more than 10% of her weight lately, her risk is low
Chapter 57. Osteoporosis
MULTIPLE CHOICE
1. Drugs that increase the risk of osteoporosis developing include:
A. Oral combined contraceptives
B. Carbamazepine
C. Calcium channel blockers
D. High doses of Vitamin D
2. Selective estrogen receptor modifiers (SERMs) treat osteoporosis by selectively:
A. Inhibiting magnesium resorption in the kidneys
B. Increasing calcium absorption from the GI tract
C. Acting on the bone to inhibit osteoblast activity
D. Selectively acting on the estrogen receptors in the bone
3. Sallie has been diagnosed with osteoporosis and is asking about the “once a month” pill to treat her condition. How do bisphosphonates treat osteoporosis?
A. By selectively activating estrogen pathways in the bone
B. By reducing bone resorption by inhibiting PTH
C. By reducing bone resorption and inhibiting osteoclastic activity
D. By increasing parathyroid hormone production
4. Inadequate Vitamin D intake can contribute to the development of osteoporosis by:
A. Increasing calcitonin production
B. Increasing calcium absorption from the intestine
C. Altering calcium metabolism
D. Stimulating bone formation
5. Cassie is a 15-year-old female who presents to clinic for a sports physical. Her diet history indicates she drinks less than one glass of milk per day and avoids dairy products to lose weight. What is the recommended daily calcium intake for Cassie?
A. 500 mg
B. 1,000 mg
C. 1,300 mg
D. 1,500 mg
6. Susan is a 52-year-old perimenopausal woman who is lactose intolerant. What is her recommended calcium and vitamin D requirement?
A. 1,500 mg calcium and 200 IU Vitamin D
B. 1,200 mg calcium and 400 IU Vitamin D
C. 1,300 mg calcium and 400 IU Vitamin D
D. 1,000 mg calcium and 400 IU Vitamin D
7. The drug recommended as primary prevention of osteoporosis in women over age 70 years is:
A. Alendronate (Fosamax)
B. Ibandronate (Boniva)
C. Calcium carbonate
D. Raloxifene (Evista)
8. The drug recommended as primary prevention of osteoporosis in men over age 70 years is:
A. Alendronate (Fosamax)
B. Ibandronate (Boniva)
C. Calcium carbonate
D. Raloxifene (Evista)
9. Intranasal calcitonin is used in the treatment of osteoporosis. Calcitonin therapy is appropriate for which patient?
A. Thin, Caucasian perimenopausal women
B. Men over age 65 with osteoporosis
C. Women over age 65 years with osteopenia
D. Women over age 65 with severe osteoporosis
10. The ongoing monitoring for patients over age 65 years taking alendronate (Fosamax) or any other bisphosphonate is:
A. Annual DEXA scans
B. Annual Vitamin D level
C. Annual renal function evaluation
D. Electrolytes every 3 months
58 Vaginitis
MULTIPLE CHOICE
1. Helima presents with a complaint of vaginal discharge that when tested meets the criteria for bacterial vaginosis. Treatment of bacterial vaginosis in a non-pregnant symptomatic women would be:
A. Metronidazole 500 mg PO BID x 7 days
B. Doxycycline 100 mg PO BID x 7 days
C. Intravaginal tinidazole daily x 5 days
D. Metronidazole 2 grams PO x 1 dose
2. Besides prescribing antimicrobial therapy, patients with bacterial vaginosis require education regarding:
A. The most recent partners in the past 60 days should also be treated
B. Alcohol should not be consumed during and for 1 day after metronidazole is taken
C. Condoms should be used during intercourse if intravaginal clindamycin cream is
used
D. Necessity of co-treatment for Chlamydia
3. Sydney presents to clinic with vulvovaginal candidiasis. Appropriate treatment for her would be:
A. OTC intravaginal clotrimazole
B. OTC intravaginal miconazole
C. Oral fluconazole one-time dose
D. Any of the above
4. If a woman presents with recurrent vulvovaginal candidiasis she may be treated with:
A. Weekly intravaginal butoconazole for 3 months
B. Fluconazole 150 mg PO daily x 7 doses then monthly for 6 months
C. Weekly fluconazole 150 mg PO x 6 months
D. Intravaginal tioconazole x 14 days
5. Zoe presents with genital warts present on her labia. Patient-applied topical therapy for warts includes:
A. Podofilox 0.5% gel
B. Podophyllin 10% resin
C. Trichloracetic acid
D. Any of the above
6. Sophie presents to clinic with a malodorous vaginal discharge and is confirmed to have
Trichomonas infection. Treatment for her would include:
A. Metronidazole 2 grams PO x 1 dose
B. Topical intravaginal metronidazole daily x 7 days
C. Intravaginal clindamycin daily x 7 days
D. Azithromycin 2 grams PO x 1 dose
7. In addition to antimicrobial therapy, patients treated for Trichomonas infection should be educated regarding:
A. Necessity of treating sexual partner simultaneously
B. Abstaining from intercourse until both partners are treated
C. Need for retesting in 3 months due to high reinfection rate
D. All of the above
Chapter 59. The Economics of Pharmacotherapeutics
MULTIPLE CHOICE
1. Being competent in the use of information technology in clinical practice is expected in professional nurses. Nurse practitioner competence includes the ability to:
A. Search for information using the most common search engines
B. Serve as content experts in developing, implementing, and evaluating information
systems
C. Write programs to assure the integrity of health information
D. Utilize IT to prescribe drugs
2. You are going to prescribe a drug that has been on the market for less than 2 months. Your best source of drug information at this time (besides calling the pharmacist) is:
A. The Physician’s Desk Reference
B. Any nurse’s drug handbook
C. Micromedix Online
D. Pharmacist’s Drug Reference
3. Which of the following is a primary benefit of the use of computerized physician order entry (CPOE) for patient medications?
A. Reduces time that prescribing drugs takes
B. Eliminates the need to chart drugs prescribed
C. Decreases prescribing and transcription errors
D. Helps keep the number of drugs prescribed to a minimum
4. A number of barriers and concerns exist before the goals of a safe and efficient IT system can be realized. Which of the following is NOT a barrier to adoption and use of IT in prescribing drugs?
A. Cost of initial set up
B. Access to highly skilled experts
C. Compatibility between systems
D. Patient confidentiality risks
5. Electronic Health Records (EHRs):
A. Are bring discouraged by the Centers for Medicare and Medicaid Services due to
cost issues
B. Allow for all patient data to be centralized in one location for access by multiple
providers
C. Use macros and templates to individualize care
D. Use standardized software to facilitate interoperability between systems
6. Factors that facilitate keeping patient information confidential in an EHR system include:
A. Designing software so that only those who need the information can gain access
B. Requiring providers to log-off at the end of the clinical day
C. Keeping a file of the login and password information for each provider in a secure
place
D. Having patients sign informed consent documents to have their data on an EHR
7. Decision support systems often provide medication alerts that tell the prescriber:
A. Patient history data with a summary of their diagnoses
B. The usual dosage for the drug being prescribed
C. The patient’s latest lab values, such as potassium levels
D. Potential drug-to-drug interactions with other medications the patient is taking
8. Prescribers have been shown to override a medication alert about a patient’s allergies when:
A. The history showed that the patient had tolerated the medication in the past
B. The benefit outweighed the risk
C. The medication was therapeutically appropriate and needed
D. All of the above
9. One barrier to use of the Web for both prescribing and for patient teaching is:
A. Lack of free public access to the Internet
B. Age, with older adults rarely understanding how to use a computer
C. Web pages and hyperlinks may change, be deleted, or be replaced
D. Few sites with information about drugs are free
10. IT can be a time-saving device in a busy practice if it is used wisely. One way to make it a help rather than a hindrance is to:
A. Prioritize what is needed information and avoid spending time reading
“interesting” information not central to the problem at hand
B. Integrate professional and person searching so that the same browser does not need
to be accessed repeatedly
C. Check e-mail frequently so that patient questions can be addressed promptly
D. Check for viruses, spyware, and malware
11. Data in the EHR that the provider reviews prior to a patient encounter varies with the clinic setting. In an urgent care clinic, the provider should review:
A. The patient’s current diagnosis and history
B. Drugs the patient is currently taking
C. Any recent previous encounter for the same problem as this visit and what was
done
D. All of the above
12. IT can also be used to interact with a patient between encounters. Which of the following statements about such interactions is true?
A. Patients feel the provider does not care about them if they are not seen in a face-to-
face encounter.
B. Data collected from patients between encounters via IT is less accurate and
complete.
C. Collecting data between encounters via IT may mean a more efficient face-to-face
encounter.
D. Between encounters is a good time to collect screening data.
13. Discharge summaries using IT have several advantages. They can:
A. Replace the need for oral instruction since the patient has printed material to read
at home
B. Be filed with the patient’s chart to document patient teaching
C. Both A and B
D. Neither A nor B
14. IT can also be used for patient teaching during the encounter and after it. The provider can help patients and their families become savvy consumers of health-care information by:
A. Warning them about the questionable quality of health information online
B. Telling them to contact the office about any web sites they have questions about
C. Teaching them how to identify high quality web sites and “red flags” to inaccurate
content
D. All of the above
15. Incorporating IT into a patient encounter takes skill and tact. During the encounter, the provider can make the patient more comfortable with the IT the provider is using by:
A. Turning the screen around so the patient can see material being recorded
B. Not placing the computer screen between the provider and the patient
C. Both A and B
D. Neither A nor B
Chapter 60. Integrative Approaches to Pharmacotherapy – A look at Complex Cases
MULTIPLE CHOICE
1. Patients with chronic illness may struggle with adherence to their treatment regimen. Intelligent non-adherence occurs when the patient:
A. May not understand the specifics of his or her medication regimen
B. Cannot afford to pay for all the medications in his or her regimen
C. Occasionally misses doses of medications due to forgetfulness
D. Chooses to discontinue or alter his or her medication regimen
2. Steps the provider can take to improve medication adherence in the chronically ill patient include:
A. Tell the patient to take the medications as prescribed for optimum health
B. Assess adherence either through self-report or laboratory values
C. Encourage the patient to take the medications regularly
D. If noncompliant with the medication regimen, ask if the patient values good health
3. The Beers Criteria is used to:
A. Determine appropriate prescribing in the elderly
B. Set guidelines for prescribing sedatives for the elderly
C. Assess potentially inappropriate medications in the elderly
D. Provide regulation in the prescribing of potentially dangerous medications
4. The Beers Criteria recommend which muscle relaxant for use in the elderly?
A. Methocarbamol (Robaxin)
B. Carisoprodol (Soma)
C. Cyclobenzaprine (Flexeril)
D. None of the above
5. According to the Beers Criteria list, the elderly should be cautiously prescribed fluoxetine (Prozac) due to:
A. Excessive drowsiness
B. Long half-life
C. Dry mouth and constipation
D. Decreased renal excretion
6. The Beers Criteria states mineral oil is not recommended to be used in the elderly due to:
A. Lack of efficacy in this age group
B. Concern for oil leakage from the anus
C. Potential for aspiration of oil
D. Concern for CNS and extrapyramidal effects
7. Many elderly patients use diphenhydramine (Benadryl) as a sleep aid. The Beers Criteria recommends against the use of diphenhydramine in the elderly due to:
A. Lack of efficacy in the elderly
B. It may cause confusion
C. It may induce depression
D. Orthostatic hypotension
8. The most common prescribing error in long-term care facilities is:
A. The wrong drug is prescribed
B. The wrong dose of medication is prescribed
C. Medications are administered at the wrong time
D. Drugs with known interaction are prescribed
[Show More]




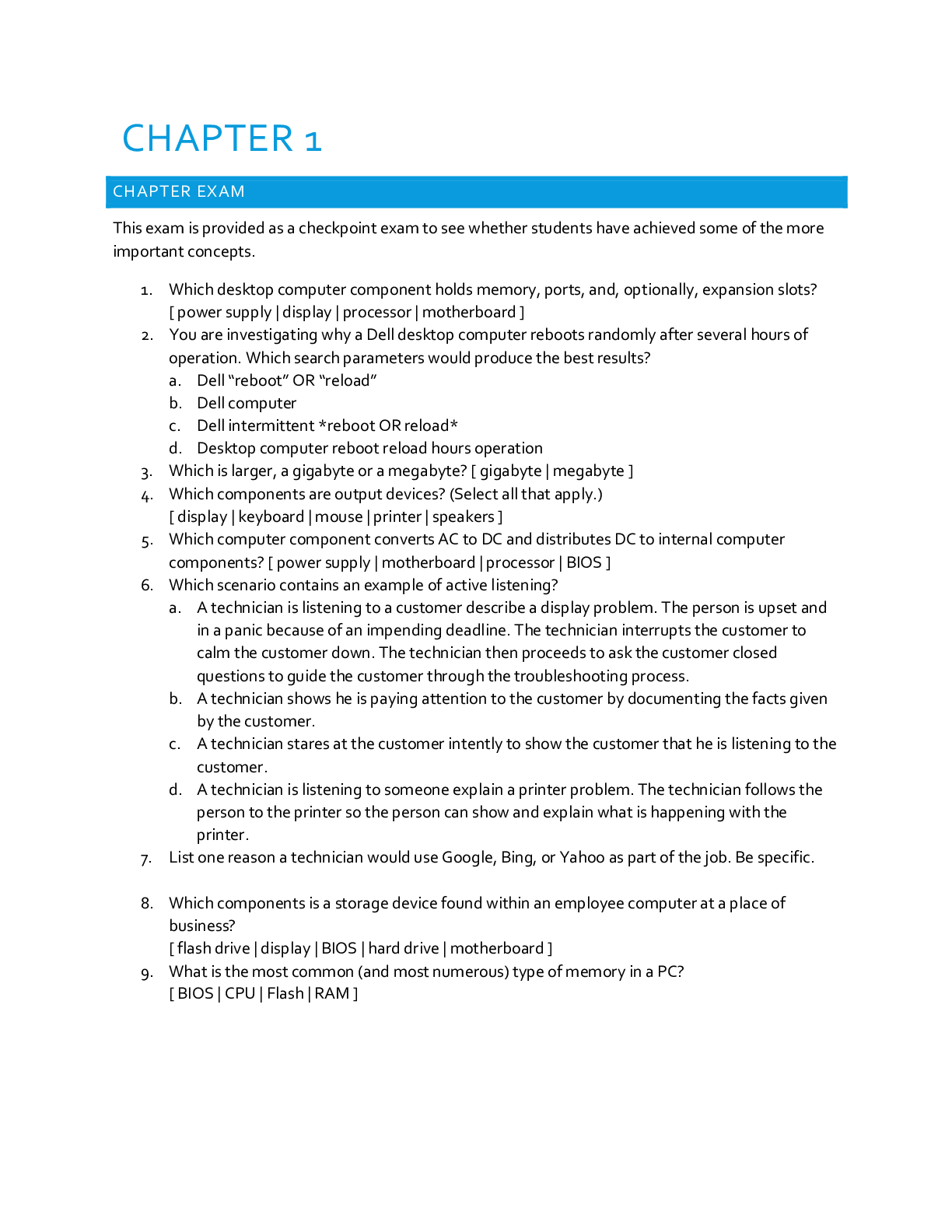
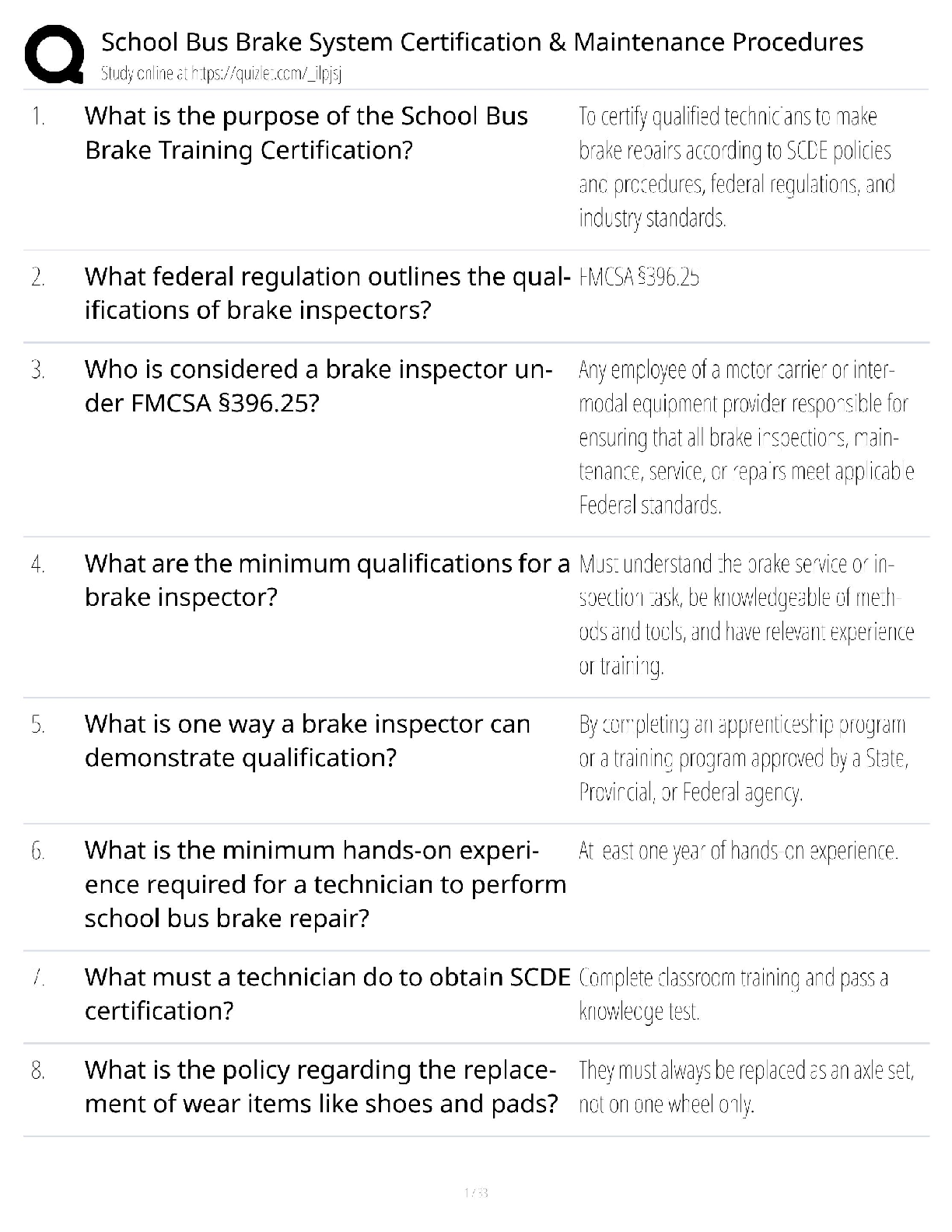
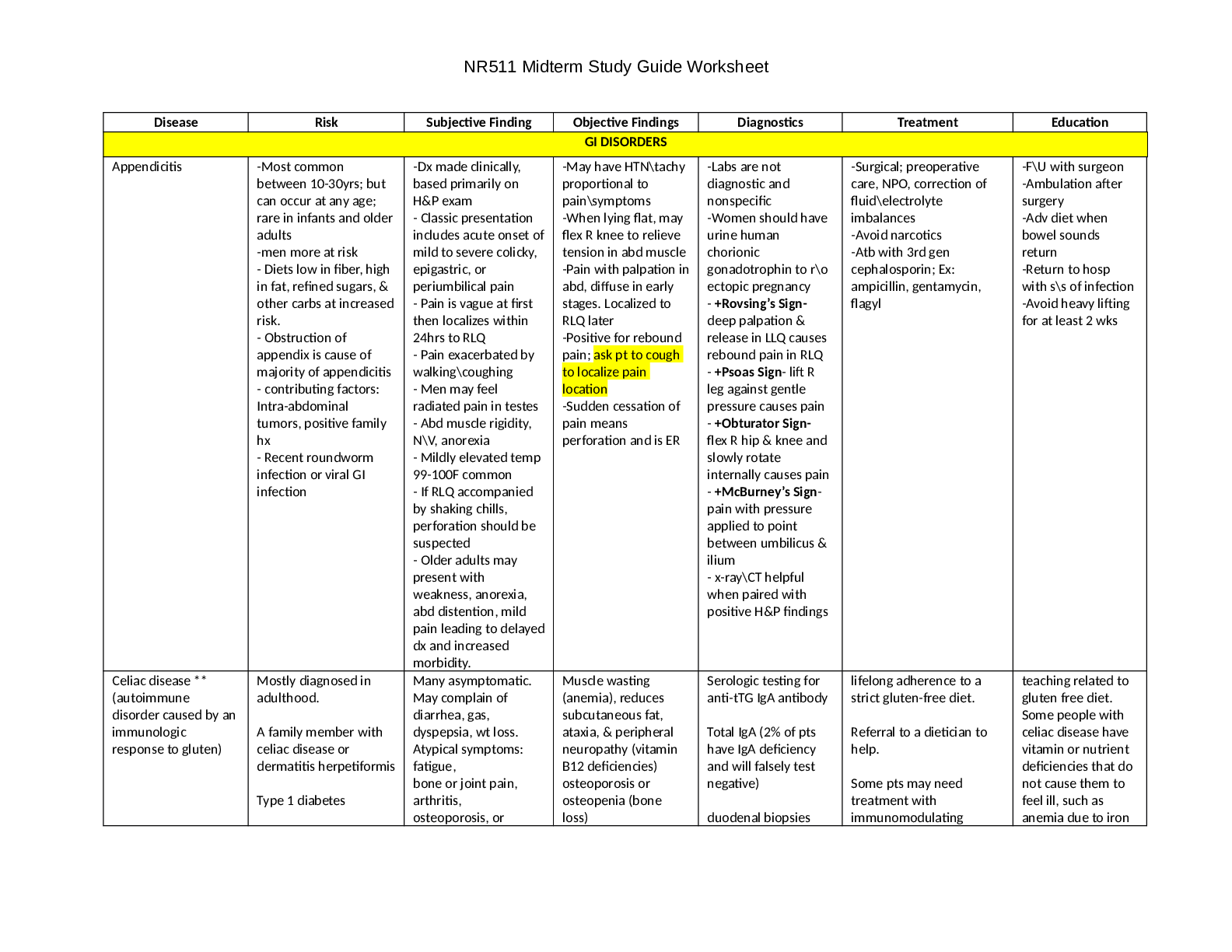
.png)