*NURSING > STUDY GUIDE > NR 565 WEEK 7 and 8 Final Exam Study Guide | Chamberlain College of Nursing | Download To Score An A (All)
NR 565 WEEK 7 and 8 Final Exam Study Guide | Chamberlain College of Nursing | Download To Score An A+
Document Content and Description Below
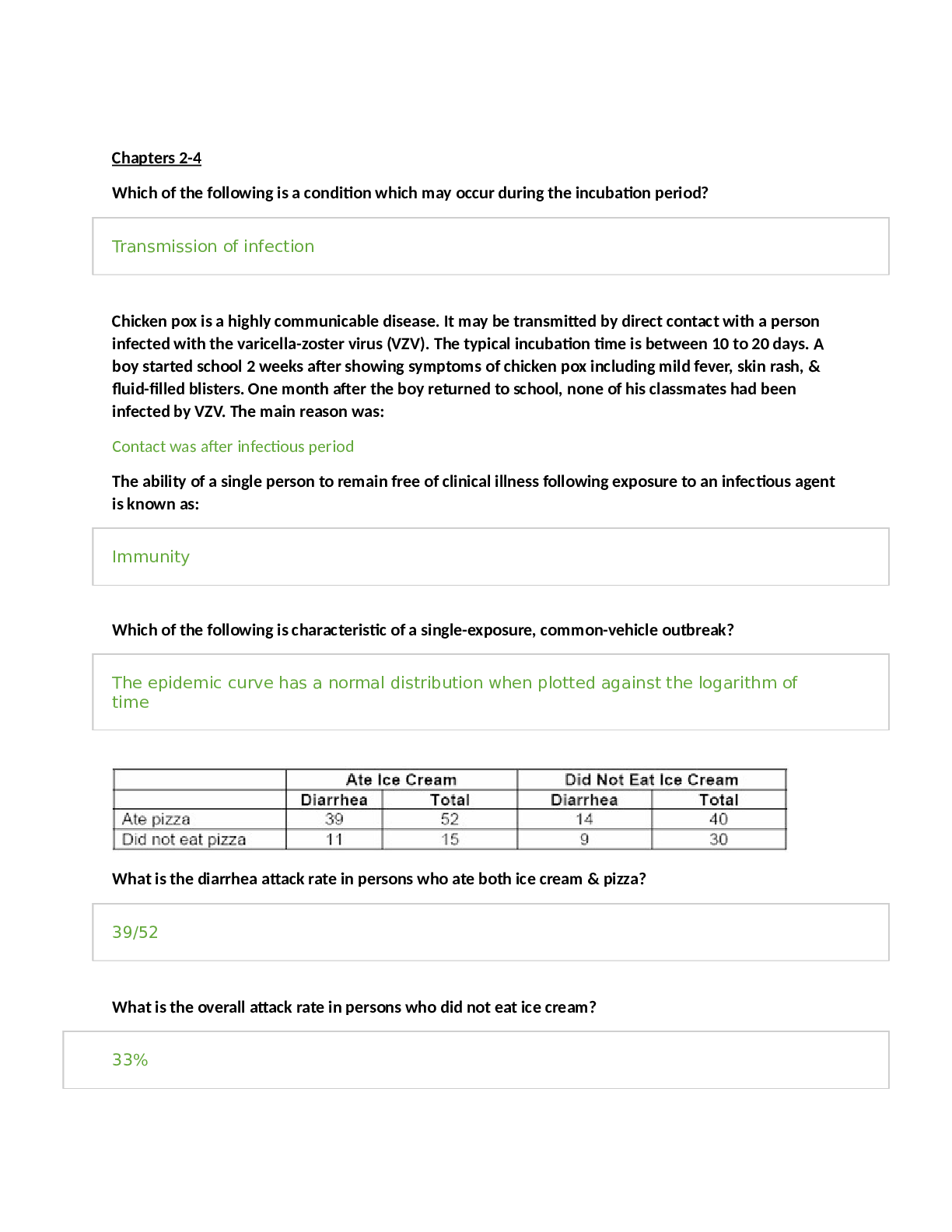
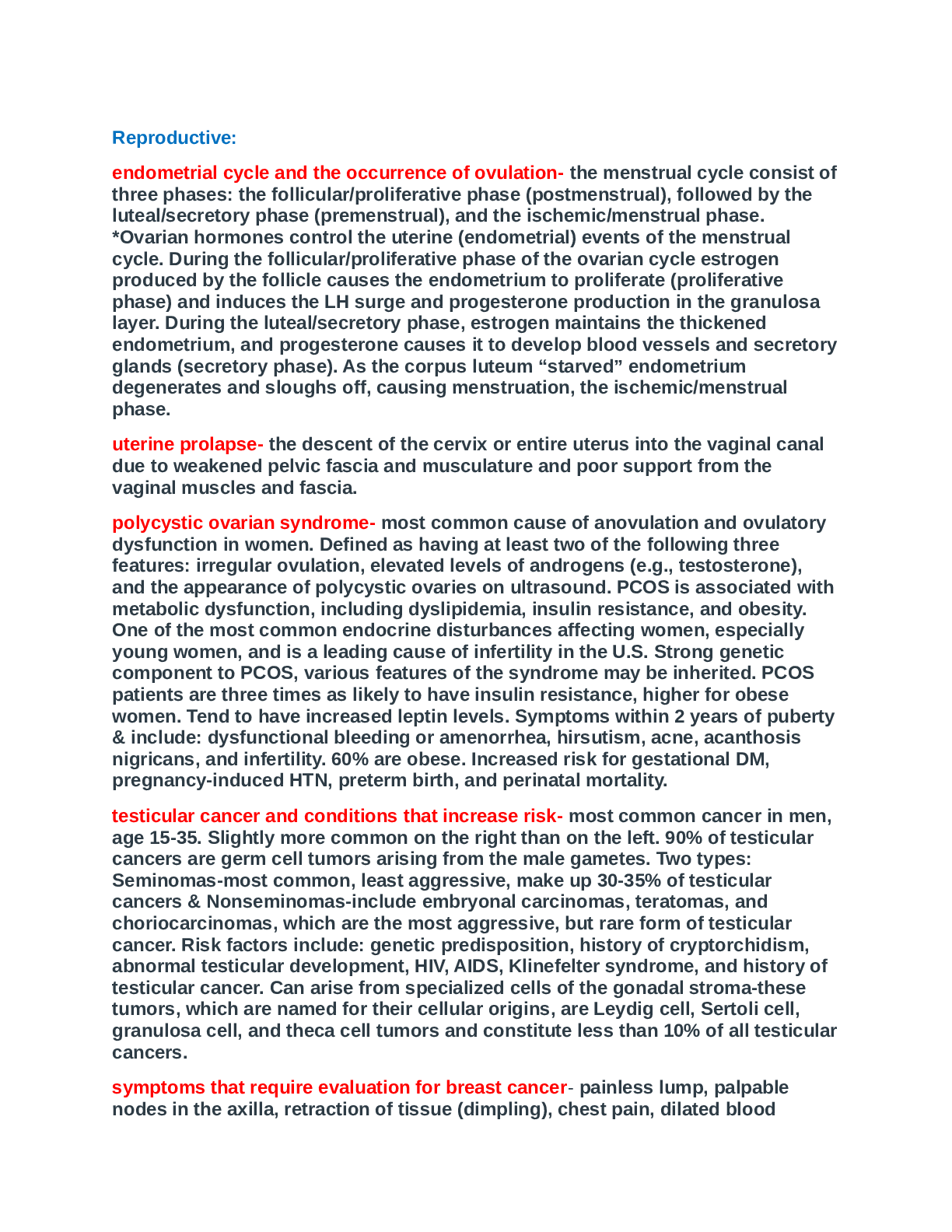
NR 565 Exam Final Study Guide ➢ Antacids: weak bases that react with hydrochloric acid to form salt & water. o Used in the treatment of Hyperacidity, GERD, PUD, hyperphosphatemia, and calcium defi... ciency o Contain combinations of ▪ metallic cation (aluminum, calcium, magnesium, and sodium) ▪ and basic anion (hydroxide, bicarbonate, carbonate, citrate, and trisilicate) ➢ Pharmacodynamics, Pharmacokinetics, Pharmacotherapeutics o Neutralize Gastric Acidity (causes ^pH of the stomach and duodenal bulb) o Inhibit proteolytic activity of pepsin o Increase lower esophageal sphincter tone o Acid-neutralizing capacity ANC varies between products expressed in mEqs o If ingested in a fasting state, antacids reduce acidity for approximately 20 to 40 minutes o If taken 1 hr after a meal, acidity is reduced for 2 to 3 hrs o A second dose taken after a meal maintains reduced acidity for more than 4 hrs after the meal o The action of antacids occurs locally in the GI tract with minimal absorption, minimal metabolism o ALL antacids are contraindicated in the presence of severe abdominal pain of unknown cause, especially if accompanied by fever -HIGH SODIUM content: pts w/ HTN, CHF, marked renal failure, or on low-sodium diets need to use low sodium preparation -Concurrent administration with enteric-coated drugs, destroys the coating= alters absorption, ^ the risk for adverse effects -Administrations should be separated by at least 2 hours to decrease drug/drug interactions 1. Calcium based antacids: TUMS, Caltrate, Calcarb • Prescribed to treat calcium deficient states, i.e. chronic renal failure, post-menopause, and osteoporosis • Used to bind phosphates in CRF • Require Vitamin D for absorption from the GI tract • Excreted mainly in feces, 20% in urine • ADR: Contraindicated in the presence of hypercalcemia and renal calculi • Can cause constipation- increase bulk, fluids and mobility, stool softener • Administered 30min- 1hr on empty stomach or 3hr after meals • Should not be administered with food containing large amounts of oxalic acid (spinach, rhubarb), or phytic acid (bran, cereals), they decrease the absorption of calcium • Taking w/ foods containing phosphorus (milk, dairy) can lead to milk-alkali syndrome (N/V, confusion, headache). • Taking with acidic fruit juice improve absorption 2. Aluminum based: AlternaGEL, Amphojel, Mylanta • Inhibit smooth muscle contraction and slow gastric emptying • Used to bind phosphates in CRF Aluminum is not easily removed by dialysis b/c it is bound to albumin & transferrin = do not cross dialysis membrane • Not absorbable with routine use • Aluminum concentrated in the CNS • Bind with phosphate and excreted in feces • Prolonged use in patients with renal failure may result in dialysis osteomalacia o Aluminum deposits in bone and osteomalacia occurs • Elevated aluminum tissue levels contribute to the development of dialysis encephalopathy • Used to treat hyperphosphatemia in pts w/ renal failure & phosphate renal stone prevention • Can cause constipation- increase bulk, fluids and mobility, stool softener 3. Magnesium based: Milk of mag, Maalox, Mylanta • Can be used to treat magnesium deficiencies from malnutrition, alcoholism, or mag-depleting drugs • Contraindicated in patients with renal failure & used with caution in pts with renal insufficiency The malfunctioning kidney cannot excrete magnesium= hypermagnesemia • Not absorbable with routine use • Excreted in the urine • Contraindicated in patients with renal failure, use with caution for patients with any degree of renal insufficiency o Malfunctioning kidney is unable to excrete magnesium and hypermagnesemia may result • Can cause diarrhea- increase fiber intake (Alkalosis may occur in renal impairment) Clinical Use and Dosing ➢ Rational drug selection o ANC, sodium content, and cost o Combination products with aluminum hydroxide and magnesium hydroxide have the highest ANC (use is moderate to severe disease ➢ Monitoring o Serum phosphate, potassium, and calcium during chronic use o These drugs may cause increased serum calcium and decreased serum phosphate o Chronic magnesium hydroxide use may cause elevated Mg levels in patients with renal failure or the elderly with decreased renal function ➢ Patient education o Take as prescribed, especially related to mealtimes o Take 1-3 hrs after meals and at bedtime o Chewable tablets chew thoroughly and drink half a glass of water o Shake suspensions before administration o Many drug interactions, separate doses by 2 hours apart o Calcium based antacids should not be administer with food containing large amounts of oxalic acid (spinach, rhubarb) or phytic acid (brans, cereals) decrease absorption o Avoid taking with food containing phosphorus (milk, dairy products) can cause milk-alkali syndrome (NV, confusion, HA) o Consult provider: before taking antacids for more than 2 weeks if a problem recurs, if relief is not obtained, or if symptoms of GI bleeding (black, tarry stools, coffee ground emesis o Aluminum and calcium antacids may cause constipation: increase bulk, increase fluid intake, and more mobility, stool softened o Magnesium antacids may cause diarrhea, increase fiber o Avoid smoking, avoid flat lying body position while sleeping, foods that irritate the gastric mucosa (spicy foods), or stimulate acid production (alcohol) and foods that decrease lower esophageal sphincter tone (caffeine, chocolate, fatty foods) ➢ Antidiarrheals: • Diarrhea that lasts for less than 2 weeks is considered acute; if it lasts more than 2 weeks, it is considered chronic. • Pharmacodynamics, Pharmacokinetics • Three main classes absorbent preparations (kaolin and pectin (Kapectolin) and bismuth subsalicylate (Pepto- Bismol, Kaopectate Liquid), opiates (diphenoxylate with atropine (Lomotil), diphenoxin with atropine (Motofen), and loperamide (Imodium)) and anticholinergics (IBD) • Contraindications: Drugs that decrease gastric motility or delay intestinal transit time have induced toxic megacolon, especially in those with inflammatory bowel disease • All antidiarrheals (except Crofelemer) require cautious use in older adults and when there is r/f impaction • Older adults are especially sensitive to diphenoxylate or difenoxin r/t atropine and anticholinergic properties • Not recommended for children under 12, none of the antidiarrheals are safe for children under 2 years old • Antidiarrheals are contraindicated in the Tx of diarrhea in most children • Standard of care: oral rehydration therapy • ADRS Rebound constipation is the main adverse effect -Kaolin-pectin (kapectolin): Acute diarrhea • Kaolin is a clay-like powder that attracts and holds onto bacteria • Pectin thickens the stool by absorbing moisture • Used to treat simple diarrhea • Act locally in the bowel, not systemically absorbed • Pregnancy Category B -Bismuth subsalicylate (Pepto bismol): Acute diarrhea, travelers’ diarrhea ▪ Antisecretory and antimicrobial effects ▪ Also used as part of a multidrug regimen for H. pylori ▪ Undergoes chemical dissociation in GI, salicylate moiety is absorbed ▪ Salicylate is metabolized in the liver and more than 90% is excreted in urine ▪ Contraindicated in children or teenagers during or after recovery from chickenpox or flu-like illness ▪ Contraindicated for patients with ASA hypersensitivity ▪ For bismuth subsalicylate, additional reactions that all patients should be warned about are gray/black stools and black tongue, the results of the bismuth. Patients should be told to expect this reaction and that it does not indicate GI bleeding. ▪ Bismuth subsalicylate may potentiate the risk for toxicity if taken w/ aspirin ▪ R/f hypoglycemia in large doses with insulin or oral hypoglycemics -Crofelemer (fulyzaq): Symptomatic relief of noninfectious diarrhea in adult pts w/ HIV/AIDS on antiretroviral therapy ▪ Botanical blocking chloride secretion from the epithelial cells in the intestinal lumen, decreasing water loss and normalizing the flow of chloride and water in the intestinal tract ▪ Minimal absorption after PO administration ▪ Metabolism and excretion are not known ▪ In clinical trials more likely to have URI, bronchitis, and cough than placebo group ▪ Adverse GI effects flatulence, increased bilirubin, and nausea -diphenoxylate w/atropine (Lomotil): Acute diarrhea ▪ Constipating meperidine congener, lacks analgesic activity ▪ At high doses can produce euphoria and physical dependence ▪ Anticholinergics are useful only with inflammatory bowel disease ▪ Well absorbed from GI tract ▪ The atropine crosses the BBB (produces mild to moderate anticholinergic effects) ▪ Rapidly and extensively metabolized to diphenoxylic acid (it’s metabolite) ▪ Excreted in urine and feces ▪ The atropine component of diphenoxylate and difenoxin contraindicates their use in narrow-angle glaucoma and requires cautious use in prostatic hyperplasia. ▪ Children, especially those with Down syndrome have increased sensitivity to atropine ▪ Use with extreme caution in children, not recommended for use in children younger than 12 y/o ▪ Do not use with E. Coli, Salmonella, Shigella, or in pseudomembranous colitis ▪ ADRs: r/t atropine: anticholinergic effects (dry mouth, flushing, tachycardia, urinary retention) o Crosses BBB=dizziness, drowsiness, sedation, HA, euphoria, or depression ▪ Additive or potentiating CNS effects with other CNS depressants and additive anticholinergic effects with other drugs that share these effects -Difenoxin w/atropine (Motofen): Acute diarrhea9***** ▪ Anticholinergics are useful only with inflammatory bowel disease ▪ Rapidly metabolized to an inactive hydroxylated metabolite ▪ Excreted mainly as conjugates in urine and feces ▪ The atropine component of diphenoxylate and difenoxin contraindicates their use in narrow-angle glaucoma and requires cautious use in prostatic hyperplasia. ▪ Children, especially those with Down syndrome have increased sensitivity to atropine ▪ Use with extreme caution in children, not recommended for use in children younger than 12 y/o ▪ Do not use with E. Coli, Salmonella, Shigella, or in pseudomembranous colitis ▪ ADRs: r/t atropine: anticholinergic effects (dry mouth, flushing, tachycardia, urinary retention) o Crosses BBB=dizziness, drowsiness, sedation, HA, euphoria, or depression ▪ Additive or potentiating CNS effects with other CNS depressants and additive anticholinergic effects with other drugs that share these effects -Loperamide (Imodium): Acute diarrhea, travelers’ diarrhea, chronic diarrhea associated w/inflammatory bowel disease • Binds to opiate receptors of the intestinal wall, slows gastric motility • Reduces fecal volume, increases viscosity and bulk, diminishes loss of fluid and electrolytes • Does not cross BBB, limited CNS ADRs • Partially metabolized by the liver and undergoes enterohepatic recirculation to be completely metabolized • Eliminated in feces • ADRs: r/t atropine: anticholinergic effects (dry mouth, flushing, tachycardia, urinary retention) o To a lesser degree than diphenoxylate and difenoxin o Dizziness and drowsiness (less CNS effects than difenoxin or diphenoxylate • Additive or potentiating CNS effects with other CNS depressants and additive anticholinergic effects with other drugs that share these effects Pharmacotherapeutics • Precaution and contraindications • Drugs that reduce intestinal motility or delay intestinal transit time may cause toxic megacolon, especially in IBD • Diphenoxylate with atropine difenoxin with atropine, and loperamide should be used cautiously in IBD o D/C if ABD distension occurs • Use Diphenoxylate with atropine difenoxin with atropine, and loperamide use with caution in advanced hepatorenal disease and in all patients with abnormal LFTs (hepatic coma may occur) • Atropine: contraindicated in narrow-angle glaucoma and requires cautious use in prostatic hyperplasia • Children (especially those with Downs syndrome) have increased sensitivity to atropine • Clinical Use and Dosing Simple, Acute Diarrhea • Absorbent preparations for adults: Kaolin-pectin or bismuth subsalicylate taken after each loose stool may be effective • Majority of acute diarrhea are self-limiting, hydration important • Maintain hydration o Commercial hydrating fluids (Pedialyte) or powdered salts o A pinch of table salt and a half-teaspoon of honey in 8 oz of fruit juice (older children and adults) o Non-diet colas without carbonations (older children and adults) o Alternate these solutions with 8 oz of water with one-quarter teaspoon baking soda to replenish electrolytes (NA, K, bicarbonate, and Cl) • If the absorbents do not resolve the problem, diphenoxylate or difenoxin or loperamide may be added Chronic Diarrhea Associated with IBD • Steroids and sulfasalazine are needed • Loperamide may be used as adjunct therapy o May significantly improve symptoms especially with added fiber and anticholinergics o If clinical improvement does not occur with doses of 16 mg/day for 10 days, symptoms are unlikely to be controlled by further use Chronic Diarrhea Associated with Pancreatic Insufficiency • Malabsorption r/t pancreatic insufficiency requires enzyme supplements, antidiarrheals not indicated Chronic Infantile Diarrhea • Bismuth subsalicylate: 2.5 mL every 4 hrs for children 2 to 24 months, 5 mL for 24-48 month children, and 10 mL for children 48 to 70 months Diarrhea in HIV/AIDS Patients Taking Antiretroviral Drugs • Crofelemer (Fulyzaq) symptomatic relief of noninfectious diarrhea in adults with HIV/AIDS on ARV therapy • 125 mg tablet twice a day without regard for food Traveler’s Diarrhea • Bismuth subsalicylate: two tablets or 2 Fl oz before each meal and at bedtime (QID) for up to 3 weeks • Prevention and treatment • High-risk areas: Central and South American, Africa, Middle East, Mexico, and Asia • E. Coli is the most common causative agent followed by Campylobacter, Shigella, and Salmonella Rational Drug Selection • Indication: Acute diarrhea, any of the antidiarrheals are appropriate • Subsalicylate and loperamide are the only drugs indicated for traveler’s diarrhea • Loperamide is the only drug with an indication for IBD • Generic and brand name formulations available Monitoring: No specific monitoring Patient Education • Take as directed, do not double doses, do not exceed max number of doses in 24 hrs • Notify provider if diarrhea continues beyond 48 hrs or if ABD pain, fever, or distention occurs • Use calibrated measuring devices for liquids, shake suspensions before measured • Drug interactions may occur, especially with diphenoxylate and loperamide • Do not take any OTC antidiarrheal before contacting your provider if taking digoxin, cephalosporin antimicrobials, warfarin or heparin, or CNS depressants (including ETOH) • R/f salicylate poisoning if taking ASA and bismuth subsalicylate • R/f rebound constipation • Stop drug when s/s of diarrhea are reduced • Bismuth subsalicylate can turn the tongue and stools gray/black • Drugs with atropine: dry mouth, flushing, tachycardia, and urinary retention • Loperamide also exhibits these reactions but to a lesser degree, add fiber and use oral rehydrating solutions • GHWT • Bland food diet, remove milk, could it be lactose intolerance? ➢ Cytoprotective Agents: o Agents used to treat or prevent ulcer formation o Two drugs sucralfate (Carafate) and misoprostol (Cytotec) ❖ Pt should report onset of black tarry stools or severe abdominal pain, which may indicate treatment failure and GI bleeding Sucralfate (Carafate): • Pharmacodynamics-Basic aluminum salt that binds to necrotic ulcer tissue where it acts as a barrier to acid, pepsin, and bile salts. o Action is largely topical, no acid-neutralizing activity, little is absorbed o May directly absorb bile salts and stimulate endogenous prostaglandin synthesis (formation of protective mucosa) • Pharmacokinetics • Minimal absorption, action is largely topical • Essentially not absorbed, 90% excreted in feces • Pharmacotherapeutics • No specific precautions or contraindications • Pregnancy Category B • Safety in children not established • ADRs Minor and rare: constipation, dizziness, gastric discomfort • Drug/Drug interactions: Decrease absorption of other drugs o Separate administration of interacting drugs by 2 hours, give other drug first • Take on an empty stomach • Causes constipation- increased fluids, dietary bulk, and exercise • Do not use with digoxin or warfarin= decreases effectiveness • Indication for active duodenal ulcer x8wks and maintenance after healing x2wks Misoprostol (Cytotec): • Pharmacodynamics: A methyl analogue of prostaglandin E1 • Inhibits gastric secretion through inhibition of histamine-stimulated cyclic adenosis monophosphate (AMP) production • Inhibits basal and nocturnal gastric acid secretion and acid secretion in response to stimuli o meals, histamine, and coffee by binding to prostaglandin E receptors, mucosal protective qualities. • Mucosal protective qualities as well o Binds to prostaglandin E receptors which facilitate mucus and bicarbonate production • Can be taken with food and still be effective • Pharmacokinetics • Rapidly and extensively absorbed after PO administration (distribution unknown) • Rapidly converted into a free acid • Does not affect CYP450 system • Half-life is 20-40 mins however renal impairment doubles its half-life • Metabolite excreted in urine • Pharmacotherapeutics • Use with caution with caution in renal impairment (no routine adjustments) • Use with caution in the elderly r/t decreased renal function • Pregnancy X: Can produce uterine contractions endangering pregnancy causing spontaneous abortion, premature birth, or birth defects. Women of childbearing age should have a negative pregnancy test before prescribed and start misoprostol on day 2 or 3 of menstrual period. If pregnancy is suspected, drug should be stopped immediately. • ADRs GI or gynecological o Most common: diarrhea, ABD pain, nausea, and flatulence o Postmenopausal bleeding, spotting, cramps, hypermenorrhea, menstrual disorder, and dysmenorrhea • Drug/Drug interactions: R/f increased diarrhea when given with magnesium based antacid • Indicated for prophylaxis and treatment of duodenal ulcers associated with NSAID use Clinical Use and Dosing Prophylaxis and Treatment of Duodenal Ulcers Associated with NSAID Use • NSAIDs inhibit prostaglandin synthesis and damage the mucosal lining of the stomach • R/f ulcer formation • Misoprostol is FDA approved for this use (prophylaxis or treatment) • Dosage 200 mcg QID with food ACHS • If unable to tolerate 100 mcg QID with food ACHS Treatment of Duodenal Ulcers from Other Causes • Sucralfate used short term (up to 8 wks) for Tx of an active ulcer • Dosage 1 gram QID on an empty stomach, 1 hr before meals, and HS • Healing usually occurs in 2 weeks • Maintenance therapy after ulcer has healed is 1 g BID • Off label use for treating gastric and esophageal ulcers-same dosing schedule • May have some advantages over antacids and H2Ras in stress ulcer prophylaxis • Misoprostol: less effective for Tx of duodenal ulcers from other causes o Off-label: in doses >400mcg/day, Tx for duodenal ulcers not responsive to H2Ras Rational Drug Selection • Sucralfate: drug of choice for women of childbearing age • Sucralfate preferred over misoprostol for treatment of active duodenal ulcers not caused by NSAIDs Monitoring • No specific monitoring parameters • Negative pregnancy test for misoprostol Patient Education • Take exactly as prescribed • Sucralfate on an empty stomach, Sucralfate is given for 4 to 8 weeks, increase fluid intake, dietary bulk, and exercise to reduce incidence of constipation • Misoprostol with food, Misoprostol given for the duration of NSAID therapy, can cause diarrhea, if persists x1WK notify provider • Continue therapy even if you feel better ➢ Antiemetics: Drug classes with antiemetic properties: antihistamines, phenothiazines, sedative hypnotics, cannabinoids, 5-HT3 receptor antagonist, anticholinergics, and a substance P/neurokinin 1 receptor antagonist Antihistamines: dimenhydrinate (Dramamine), diphenhydramine (Benadryl), hydroxyzine (Vistaril), meclizine (Antivert) • Pharmacodynamics: Antihistamines with significant antiemetic activity have strong anticholinergic effects as well as histamine 1 blocking effects • MOA: Bind to central cholinergic receptors to produce antiemetic effects • especially with motion sickness due to the depression of conduction in the vestibulocerebellar pathway • Pharmacokinetics: All the antiemetic drugs (except for TD scopolamine) are well absorbed after PO administration • Pharmacotherapeutics: Cautious use in narrow-angle glaucoma, seizure disorders, pyloric obstruction, hyperthyroidism, CVD, and prostatic hypertrophy • Contraindicated in severe liver disease r/t extensive liver metabolism • Cautious use in the elderly, dose reductions may be needed • Dimenhydrinate and diphenhydramine are Pregnancy Category B and safe for use in children • Meclizine is pregnancy Category B (safety and efficacy in children less than 12 not established) • Hydroxyzine Pregnancy Category C, has been used safely during labor (safety in children or lactation not established) ADRs: Common adverse reactions: drowsiness, dry mouth, blurred vision & urinary retention • Paradoxical excitation may occur in children • Drug/Drug: additive CNS depression with other drugs that produce CNS depression and additive anticholinergic effects with other drugs that have anticholinergic effects or adverse reactions Phenothiazines: prochlorperazine (Compazine), perphenazine, promethazine (Phenergan) • Pharmacodynamics: block dopamine receptors in the chemoreceptor trigger zone (CTZ) • Also bind to and block cholinergic, alpha 1 adrenergic, and histamine 1 receptors • Use as antiemetics is limited due to sedating and EPM effects • Pharmacotherapeutics: Produce extrapyramidal reaction Contraindicated in Parkinson’s Disease • Contraindicated in narrow-angle glaucoma, bone marrow depression, and sever CVD or hepatic disease • Cautious use in respiratory impairment cause by acute pulmonary infection or chronic respiratory disorders (asthma or emphysema) • May lead to the development of “silent pneumonia” • Suppress cough reflex, aspiration of vomitus is possible • Use with caution in those with r/f aspiration • Pregnancy Category C • Children of all ages are more prone to developing extrapyramidal reactions • Prochlorperazine: avoided in children younger than 5 r/t extrapyramidal reactions • R/f respiratory depression and sudden death in children 2 years of age or older • Adverse reactions: drowsiness, (extrapyramidal reactions) dystonia, akathisia, tardive dyskinesia o Dry mouth, dry eyes, blurred vision, constipation, and urinary retention o ability to mask post-surgical and neurological conditions o potential for agranulocytosis and blood dyscrasias 4-10 weeks after initiation o can cause urine to turn pink to reddish brown (does not indicate hematuria) • Promethazine Black Box Warning: Fatal respiratory depression in children younger than 2 years old • Drug/Drug: additive CNS depression with other drugs that produce CNS depression and additive anticholinergic effects with other drugs that have anticholinergic effects or adverse reactions • Additive hypotensive effects with antihypertensive agents or acute ingestion of ETOH • Concurrent administration of lithium increases r/f extrapyramidal reactions • May mask s/s of lithium toxicity • Antithyroid agents increase r/f agranulocytosis Cabbabinoid: dronabinol (Marinol) • Pharmacodynamics: Work in the CNS like cannabis to prevent NV associated w. chemotherapy & as an appetite stimulant, especially in HIV pts • Pharmacotherapeutics: Use with caution in patient with Hx of seizure disorder r/t lowering of seizure threshold o Cardiac disorders: monitor for hypotension, possible hypertension, syncope, or tachycardia o High potential for abuse o Pregnancy Category C • Adverse reactions: euphoria (should not drive), depression, dizziness, paranoid thoughts, somnolence, and abnormal thoughts o Cardiac effects include palpitations, tachycardia, and hypotension o Seizures and seizure-like activity o Drug/Drug interactions: Interacts with other CNS depressants, additive CNS depression with benzos, barbiturates, ETOH, opioids, antihistamines, muscle relaxants, and other CNS depressants 5- HT3 receptor agonists: palonosetron (Aloxi), dolasetron mesylate (Anzemet), granisetron (Kytril, Sancuso) and ondansetron (Zofran) • Pharmacodynamics: Block serotonin both peripherally and on vagus nerve terminals & the chemoreceptor trigger zone (CTZ) to decrease emesis • Pharmacotherapeutics: Potential to mask progressive ileus o Zofran contains aspartame, use with caution in phenylketonuria o Dolasetron, granisetron, and palonosetron are Pregnancy Category B • Adverse reactions: constipation, headache, fatigue, dizziness, diarrhea. o Less common but concerning rare cases of tachycardia, bradycardia, hypotension, and QT prolongation Anticholinergic: Scopolamine (Transderm Scop) • Pharmacodynamics: Belladonna alkaloid anticholinergic acts as a competitive inhibitor of muscarinic in the parasympathetic nervous system o Blocks cholinergic transmission from the reticular center to the vomiting center in the brain o Anticholinergic effect: decreases secretion of saliva and decreases GI motility • Pharmacotherapeutics: Contraindicated: pts w/ narrow angle glaucoma o Caution: pts with open-angle glaucoma or gastrointestinal or bladder neck obstruction o Use cautiously in the elderly due to CNS effects • Pregnancy Category C, no approved for use in children • Adverse reactions: dry mouth, drowsiness, blurred vision, dilated pupils o Withdraw syndrome: dizziness, NV, HA • Applied in the hairless area behind the ear 4 hours prior to needed effect and can be left in place up to 3 days. Wash hands after handling patch to avoid getting medication in the eyes (can cause blurry vision & pupil dilation) • Decrease secretion of saliva and decrease gastric motility NKI receptor antagonist: Aprepitant (Emend) • Pharmacodynamics: crosses the blood brain barrier and occupies the NK1 receptors to prevent n/v in pts receiving chemotherapy • Pharmacotherapeutics: Contraindicated in patients who are hypersensitive to any component of the product • Inhibits CYP3A4=increase serum concentrations of other drugs that are metabolized by CYP3A4 • Pregnancy Category C and not approved for use in children ▪ Adverse reactions: fatigue, dizziness, hiccups, possible elevated ALT/AST, BUN • Drug/drug interactions: Inducer of CYP3A4 and can increase plasma concentrations of drugs metabolized via CYP3A4 system o Including: hormonal contraceptives and some chemotherapy agents • Concurrent use of Aprepitant and pimozide, terfenadine, astemizole, or cisapride is contraindicated due to potentially life-threatening reactions Misc.: trimethobenzamide (Tigan) • Pharmacodynamics: Inhibits emetic stimulation of the CTZ Rational Drug Selection: Treatment of Nausea and Vomiting Due to Drugs or Gastroenteritis • Often improves with Tx using an antiemetic • 5-HT3 receptor antagonists: low side-effect profile and tolerance • Phenothiazines: also, a good initial and short-term treatment choice, not for children • Trimethobenzamide: also, effective • Antihistamines: can be used, less serious ADRs, better for longer term applications • Dronabinol: only approved for use in chemotherapy associated NV and appetite stimulation • Aprepitant: Approved for post-operative NV and in conjunction with other antiemetic agents for prevention of acute and delayed NV associated with initial and repeated doses of emetogenic CA chemo Motion sickness: • Antihistamines are useful r/t action on vestibular system and CTZ, rapid onset of action and prolonged effect • Dimenhydrinate and meclizine: the most used • Meclizine is also used to treat vertigo • TD scopolamine: indicated for prevention of NV associated with motion sickness in adults and is commonly used in patients on ships Monitoring: • When used as a single dose or very short-term, no specific monitoring required • If Tx for longer than a few days: following monitoring parameters are suggested • Promethazine has been associated with bone marrow depression (CBC prior to initiating therapy) • Phenothiazines associated with blood dyscrasias that occur between week 4-10 of therapy o CBC prior to initiating therapy and after 4 weeks Patient Education • Motion sickness: take 1 to 2 hrs prior to departure (except for ER-12 hrs prior) • ADRs: drowsiness, dry mouth, dry eyes, constipation, and urinary retention • Phenothiazines: turns urine pink to reddish brown: this is not hematuria Do not inhibit ➢ Histamine-2 receptor antagonists: H2Ras o Histamine 2 blockers aka histamine 2 antagonists (H2Ras) acetylcholine, so they reduce gastric acid secretion by only 35%-50% Cimetidine (Tagamet), Famotidine (Pepcid), Nizatidine (Axid), Ranitidine (Zantac) • Used to reduce gastric acid in NPO pts for prophylaxis and management of duodenal and gastric ulcers and GERD (not first-line treatment of GERD), if no esophageal erosive disease is present H2RA’s can be used for maintenance therapy for relief of GERD symptoms • Also used for heart burn, acid indigestion and “sour stomach” • Pharmacodynamics: MOA: Inhibit acid secretion by gastric parietal cells through a reversible blockade of histamine at H2 receptors • potent inhibitors of all phases of gastric acid secretion, including muscarinic agonists and gastrin • Effect volume and H ion concentration of gastric juice, gastric emptying, and lower esophageal sphincter pressure (each drug to varying degrees) o Cimetidine, ranitidine, and famotidine have no effect on gastric emptying o Cimetidine and famotidine have no effect on lower esophageal sphincter pressure o Ranitidine, nizatidine, and famotidine have little or no effect on fasting or postprandial serum gastrin o Ranitidine does not affect pepsin secretion or pentagastrin-stimulated IF secretion • Pharmacokinetics o All drugs are well absorbed with PO administration o All are metabolized to differing degrees by the CYP450 system and excreted in differing percentages unchanged in urine • Pharmacotherapeutics • Caution: Renal impairment (dosage adjustments, r/f CNS ADRs), Elderly (due to decrease in renal function) • Contraindicated: Nizatidine and Ranitidine DO NOT rx for patients w. hx of liver disease (causes hepatocellular injury, hepatitis) elevated ALT AST • Pregnancy Category B, excreted in breast milk, use caution in breastfeeding mothers • Famotidine is labeled safe for infants & neonates (has caused agitation, stopped when drug d/ced) • Cimetidine can cause gynecomastia & impotence o CNS reversible reactions (mental confusion, agitation, psychosis, depression, and disorientation) • Hematological adverse reactions include agranulocytosis, granulocytopenia, thrombocytopenia, and aplastic anemia (rare) • Less Common side effects: drowsiness, dizziness, constipation (increase fiber and fluid intake), or diarrhea & nausea • Drug/Drug Interactions: Related to CYP450 system o Cimetidine is most problematic (metabolized by CYP1A2, CYP2C9, and CYP2D6) o Other drugs metabolism inhibited by cimetidine (r/f increased serum levels and toxicity • Clinical Use and Dosing GERD-most effective if used as on demand therapy for symptoms relief o Tachyphylaxis: Not first line therapy to treat GERD o If not erosive disease, may be used as maintenance therapy after PPI treatment o Infants and children have been successfully treated however no longer recommends H2Ras as empiric treatment in infants • Rational Drug Selection o No specific drug is preferred over another for effectiveness o Consider costs • Monitoring o LFTs r/t potential for hepatocellular damage o Renal impairment: renal function assessment prior to initiation of therapy • Patient Education • Should be taken w/ meals or immediately after & at bedtime, daily doses are best @ bedtime, • take 1 hour away from other drugs, • & two hours away from sucralfate • OTC preparations should not be taken for more than 2 wks without consulting healthcare provider • Report black tarry stools- may indicate GI bleeding. • Sore throat, diarrhea, rash, confusion, or hallucinations should be reported promptly (might need dosage adjustment or discontinuation), • advise pt to stop smoking (interferes with absorption of H2RA & increases gastric secretion) • Prokinetics: metoclopramide (Reglan) o AKA gastrointestinal stimulants o Do not stimulate gastric, biliary, or pancreatic secretions o Used to treat gastroparesis associated with DM, GERD, and emesis with chemotherapy Pharmacodynamics: MOA: Stimulates motility in the upper GI tract, ▪ increases tone and amplitude of gastric contractions, ▪ relaxes the pyloric sphincter and duodenal bulb, ▪ and increases peristalsis of the duodenum and jejunum, ▪ resulting in accelerated gastric emptying and increased speed of gastric transit • Improves gastroesophageal reflux disease symptoms by increasing lower esophageal tone • Also is a dopamine receptor agonist in the CNS, including the chemotherapy trigger zone leading to prevention of emesis • Actions similar to phenothiazines: Produces sedation and may cause tardive dyskinesia or EPS • Induces release of prolactin and transient increases of aldosterone Pharmacokinetics • Well absorbed after PO administration • Injectable formulation is available • High bioavailability, low protein binding • Widely distributed, crosses BBB and placenta, enters breast milk (greater than plasma) • Minimally Metabolized by the liver, liver function is not an issue • Excreted in urine (clearance is affected by renal function) • Renal impairment requires dose adjustment: dose cut in half CCr <40 Pharmacotherapeutics • BLACK BOX WARNING: risk for developing tardive dyskinesia and parkinsonian-like symptoms, the risk increases the longer it’s in use, treatment should not exceed 12 weeks and be discontinued immediately if signs of movement disorder, Report involuntary movement of the eyes, face, or limbs immediately • Contrindicated: in the presence of disorders in which stimulation of GI motility is dangerous (GI hemorrhage, mechanical obstruction, new surgery on the GI tract, or perforation), • dopamine- associated activity affects the CNS & can cause depression (mild- severe w. suicidal ideation), use with caution • Contraindicated in pt.s w. pheochromocytoma b/c the drug can cause hypertensive crisis • Safe to administer to pt.s with hx of impaired hepatic function if renal function is normal • Safety and effectiveness not established in infants and children o EPS is more common in children, use with caution ADRs • Most serious reaction is EPS (dystonic reaction and tardive dyskinesia and parkinsonian-like symptoms d/c in pt. exhibiting movement d/o • Neuroleptic malignant syndrome • More common: Depression, dizziness, diarrhea, and hypoglycemia in DM • Less common: galactorrhea, amenorrhea, gynecomastia, impotence secondary to hyperprolactinemia, and fluid retention r/t elevations in aldosterone • Incidence of ADRs correlated with the dose and duration of therapy Drug interactions: Largely related to its cholinergic and dopaminergic activity • Additive CNS depression • Increased r/f EPS when taking other drugs with a r/f EPS • Drugs with anticholinergic effects reverse the action of metoclopramide • Hypertensive crisis if administered with MAOIs Clinical Use and Dosing: GERD: principal effect is on symptoms of postprandial and daytime heartburn • For adults, for symptoms throughout the day 10 mg taken 30 minutes prior to each meal and at bedtime is recommended • If symptoms are confined to specific situation (after evening meal): 10 to 20 mg dose prior to that meal or at bedtime • Patient who are more sensitive to the therapeutic dose (older adults) 5mg/dose • Neonatal 0.1 to 0.15 mg/kg/dose Q 6 hrs • GERD in infants and children 0.4 to 0.8 mg/kg/day divided in 4 doses (30 minutes prior to teach meal) Nausea and Vomiting • Action on the chemoreceptor trigger zone to prevent NV • Post-op NV in children 14 years old or younger, older children, and adults • For high doses (as with chemo), pretreat with diphenhydramine to prevent EPS Diabetic Gastroparesis • Dose 10 mg 30 minutes AC and HS for 2 to 8 weeks • Route of administration dependent of severity of symptoms • If early: PO is adequate • If more severe: Parenteral therapy 10 mg IV over 1 to 2 minutes for up to 10 days may be needed before PO therapy can be initiated • Rectal formulations available • Be cognizant that renal impairment is common in DM, dose adjustments for CCr <40 Rational Drug Selection • Efficacy: higher cost and increased ADRs, difficult to justify its use in place of H2Ras or PPIs • Length of therapy: Not used for management of GERD is Tx must be long-term (8 weeks) • Concomitant Diseases: Cautious use for those at r/f EPS, renal disease Monitoring • Renal function assessed before therapy • Educate about EPS Patient Education • Drowsiness, avoid driving until response is known • CNS depression with ETOH and additive CNS depression • Notify immediately if involuntary movement of the eyes, face, or limbs occurs • Change in mood should be reported (depression/suicidal ideation) • Avoid ETOH, NSAIDs, large meals, fatty foods, chocolate, caffeine, citrus, ad good or fluid intake within 3 hours of HS ➢ Proton pump inhibitors (PPI’s): Esomeprazole (Nexium), Lansoprazole (Prevacid), Omeprazole (Prilosec), Pantoprazole (Protonix), Rabeprazole (Aciphex), Dexlansoprazole (Dexilant, Kapidex) • Antisecretory drugs used to treat conditions characterized by hyperacidity • Used to treat: erosive gastritis, GERD, and Zollinger-Ellison syndrome, part of the multidrug regiment for short- term treatment of active PUD (especially duodenal ulcers caused by H. pylori) Pharmacodynamics: MOA: • Do not exhibit anticholinergic or H2 blockade but suppress gastric acid secretion • Inhibition of basal and stimulated acid secretion (regardless of stimulus) by suppressing gastric acid secretion via reduction of H+ secretion and inhibition of the H +/K+/ATPase enzyme system at the secretory surface of the parietal cell itself to block the final step of H+ secretion. Pharmacokinetics • PPI’s are ironically acid labile & so most are formulated as EC tablets or granules • All should be taken on an empty stomach before a meal, in the AM if possible o Food decreases absorption • All drugs are distributed to the parietal cells of the stomach • Extensively metabolized by CYP450 system (CYP2C19 and CYP3A4) • Little unchanged drug is excreted in urine, 90% of metabolites excreted in urine • Significant biliary excretion • Older adults have decreased elimination rates of all drugs (decreased renal function, associated with age) Pharmacotherapeutics • Caution: only true contraindication is hypersensitivity to ingredients • Extensively metabolized in the liver (CYP450), use caution hx of hepatic dysfunction & the elderly o No dose adjustments required • Omeprazole is Pregnancy Category C • Lansoprazole, esomeprazole, pantoprazole, and rabeprazole are Pregnancy Category B • Safety and efficacy of pantoprazole and rabeprazole have not been established in children younger than 12 ADRs • Typically, well tolerated when used for short-term treatment o Dizziness, drowsiness, ABD pain, constipation, diarrhea, and flatulence • PPI’s long term can cause nutrient deficiencies such as Iron (iron deficiency anemia), vitamin B12, and calcium (all need an acidic environment for absorption) • places increased risk for megaloblastic anemia and • hip-fractures (osteoporosis) in at risk persons (age & female gender), • concern for cellular level changes increased risk for gastric cancers o Atrophic gastritis with long term omeprazole use is a risk factor for gastric carcinoid tumors • PPI long-term may also increase risk of C.Diff, salmonella, and campylobacter infections • Short-term use ^ risk of pneumonia Drug Interactions • Related to CYP450 system • PPIs may decrease the effects of atazanavir, indinavir, and nelfinavir (coadministration not recommended) • All PPI’s may interfere w/ drugs that need gastric acid for absorption such as ketoconazole, ampicillin, digoxin, and iron salts, • Increased monitoring of INR is required if warfarin is administered w/ PPI’s • Plavix and omeprazole Black Box Warning Regarding poor metabolizers of CYP2C19 and concurrent administration of medications that interfere with CYP2C19. • Co-administration of Plavix and Omeprazole decreases effectiveness of Plavix by 46% • may lead to clot formation- • FDA issued warning DO NOT USE CONCURRENTLY with omeprazole & esomeprazole... • use PPI w/ less CYP2C19 function such as dexlansoprazole, lansoprazole, and pantoprazole Clinical Use and Dosing Duodenal and Gastric Ulcers • Uncomplicated gastric ulcers include testing and treating for H. pylori and acid-suppressive therapy with PPIs • Lansoprazole, omeprazole, esomeprazole, and rabeprazole used for treatment of active duodenal ulcer and active benign gastric ulcer • Once-daily dosing taken before a meal, preferably in the morning • Triple regimens combine a PPI with two antibiotics for 14 days • Quadruple regiment combines a PPI with two antibiotics and bismuth subsalicylate GERD • All should be taken on an empty stomach before a meal, in the AM if possible o Food decreases absorption • Stepwise therapy, Step-up or step-down approach may be used • Steps based on symptom relief and degree of esophageal damage • Treatment begins with lifestyle modifications and OTC antacids or H2Ras (most have tried before seeking care) • ACG recommends, 8 weeks of PPIs for symptoms relief and healing of erosive esophagitis associated with GERD • Standard one a day therapy started and tailored to symptoms relief. • If nighttime symptoms are an issue dosing can be adjusted or twice a day dosing can be used • Another option would be to add an H2RA before bed • Failure to achieve symptom relief after 3 months or s/s of complications refer to GASTRO • PPIs may mask symptoms of gastric CAs • Alarm symptoms (dysphagia, painful swallowing, noncardiac chest pain, weight loss, hematemesis, and choking) suggest endoscopy as part of the initial evaluation • All PPIs are approved to treat GERD • Once daily dosing is taken 30 to 60 minutes before breakfast, Length of therapy is 8 weeks, An addition 4 weeks may be needed • Nonresponsive patients require referral • Patients may need long-term intermittent therapy for GERD Hypersecretory Conditions (Zollinger-Ellison Syndrome) • All PPIs can be used for treatment • Usually requires higher dosing than GERD or PUD Rational Drug Selection • Drug interactions: Lansoprazole is be choice for patients taking drugs metabolized by CYP450 system • All PPIs interaction with atazanavir • Other drugs interfere with Warfarin • Difficulty swallowing: omeprazole, esomeprazole, and lansoprazole capsules can be opened, and intact granules added to applesauce • Do not crush or chew granules • Lansoprazole comes in a quick-dissolve tablet (Prevacid SoluTab) or as granules for suspension • For tube feeding: omeprazole capsules or granules mix with an acidic juice or water Monitoring • Monitor disease being treated • Test for H. pylori • Stop therapy for 2 weeks before undergoing urea breath testing to diagnose H. pylori (false-negative) Patient Education • Take exactly as prescribed • Take before a meal • Drugs taken daily; AM administration preferred • May be taken with antacids • Drowsiness or dizziness • Report onset of black, tarry stools (GI bleed), diarrhea, ABD pain, or persistent HA, may indicate progression of disease or ADRs • Lifestyle modifications Stepped-approach algorithm for peptic ulcer disease. ➢ Laxatives o Six classes of drugs: stimulants, osmotics, bulk-producing laxatives, lubricants, surfactant, and hyperosmolar laxatives (methylnaltrexone (Relistor) mu-opioid receptor antagonist, used for opioid induced constipation) All share contraindication of use in the presence of nausea, vomiting, or undiagnosed abdominal pain, or if bowel obstruction is suspected or diagnosed o All share precautions for dependency, chronic use of laxatives may result in electrolyte imbalances, steatorrhea, osteocalcin, and vitamin and mineral deficiencies o Tartrazine sensitivity- may cause allergic reactions including asthma, seen in pts who also have aspirin sensitivity. o Common adverse reactions: excessive bowel activity, cramping, flatulence, and bloating o Few drug interactions ❖ Stimulants: cascara, senna, Bisacodyl, and castor oil • Pharmacodynamics: MOA: Direct action on intestinal mucosa by stimulating the myenteric plexus, releasing prostaglandins and increase cyclic adenosine monophosphate (cAMP), increasing secretion of electrolytes and peristalsis • Pharmacotherapeutics: o Bisacodyl Caution: patients with cardiovascular disease o bisacodyl is safe during pregnancy o Cascara sagrada: Avoid in patients with alcohol intolerance ▪ Can cause diarrhea in breastfed infant, enters breast milk • Contraindications: Caster oil is contraindicated in pregnancy- can cause uterine contractions • Drug of choice when rapid response is needed • Used most commonly for constipation associated w/ reduced mobility, constipating drugs, reduce motility, neurogenic bowel r/t to spinal cord injury, & IBS. Also used to bowel prep for radiological or surgical procedures • Osmotics: magnesium hydroxide, magnesium citrate, sodium phosphate, polyethylene glycol electrolyte solution, and polyethylene glycol (PEG) 3350 • Pharmacodynamics: MOA: exerts it effects mainly by drawing water into the intestinal lumen to increase intraluminal pressure, hypertonic salt-based solutions that cause the diffusion of fluid from the plasma into the intestine to dilute the solution to an isotonic state. o Magnesium salts also increase cholecystokinin by the duodenum ▪ Pharmacokinetics: 30% may be absorbed ▪ Widely distributed, cross the placenta, and enter breast milk ▪ Metabolized by the liver o Sulfate salts are most powerful o Polyethylene glycol electrolyte solution is used to cleanse the entire GI tract for diagnostic purposes, to flush poisons, and remove parasites • Pharmacotherapeutics: o Contraindications: Magnesium hydroxide is contraindicated in any degree of renal insufficiency (kidney might not be able to excrete the Magnesium) o Contraindications: Hypermagnesemia, hypocalcemia, and heart block o Magnesium hydroxide is Pregnancy Category B o PEG 3350 should not be used in children under the age of 4 o Polyethylene glycol electrolyte solution to treat constipation in children is contraindicated r/t electrolyte disturbance • Second drug of choice when rapid response is needed Bulk- Producing laxatives: psyllium, methylcellulose, polycarbophil • Pharmacodynamics: Safest and most physiological, action is similar to adding fiber into diet • MOA: consist of natural and semisynthetic polysaccharides and cellulose when combined with water in the intestine produces mechanical distension resulting in increased peristalsis • May be used for long term management of simple chronic constipation, situations when straining should be avoided, and management of chronic, watery diarrhea • Pharmacokinetics: No absorption • Pharmacotherapeutics: Caution: pts. w/ narrowed esophageal or intestinal lumen, o avoid in patients who are impacted • • Drug of choice when rapid response is not needed, and long-term management is needed (suited for older adults and pregnancy) Lubricants: Mineral oil • MOA: lubricates the intestine to facilitate passage of stool by retarding colonic absorption of fecal water and soften the stool • Pharmacodynamics: Major concerns of decrease absorption of fat-soluble vitamins • Pharmacokinetics: No distribution, local action • Pharmacotherapeutics: Caution: very young, older adults and those with dysphasia are at high risk for lipid aspiration pneumonia, • avoid use during pregnancy due to decrease in absorption in fat-soluble vitamins = hypothrombinemia in newborn Surfactants: docusate sodium, docusate calcium, docusate potassium • Referred to as stool softeners • Pharmacodynamics: MOA: reduce surface tension of the oil- water interface on the stool and facilitate admixture of fat and water into the stool, producing an emollient action • Most beneficial when feces are hard or dry, situations when passing stool is painful, when straining should be avoided • Can be administered safely to ALL ages and during pregnancy- no precautions or contraindications • Pharmacokinetics: No distribution, local action • Pharmacotherapeutics: No specific contraindications or precautions Hyperosmolar laxatives ‘misc.’: Glycerin, Lactulose • Pharmacodynamics: MOA: hyperosmotic compound that draws water from extravascular spaces into the lumen of the intestine, resulting in more liquid stool • Glycerin is used to treat fecal impactions caused by neurogenic bowel, in which the bowel is filled with feces but cannot be evacuated o Pharmacokinetics: 80% metabolized by the liver • Lactulose is used to treat chronic constipation in the elderly o only laxative used to treat hepatic encephalopathy: lowers the pH of the colon, which in turn inhibits the diffusion of ammonia across colonic membranes • Pharmacokinetics: No distribution, local action • Pharmacotherapeutics: Caution: in volume depletion o Older adults are arf dehydration o lactulose can cause hyperglycemia- caution with DM ❖ Chloride Channel Activators: Lubiprostone (Amitiza) • Pharmacodynamics: MOA: is a bicyclic fatty acid derived from prostaglandin E1 that acts by specifically activating CIC-2-chloride channels on the apical aspect of gastrointestinal epithelial cells, producing a chloride-rich fluid secretion. • These secretions soften the stool, increase motility, and promote spontaneous bowel movements. • Used for chronic idiopathic constipation, IBS with constipation in women aged 18 and older, and chronic opioid-induced constipation in adults with chronic noncancer pain • Pharmacotherapeutics: Most common ADR for Lubiprostone is nausea, may be relieved by administration with food o Adverse effects: nausea (may be relived w. food), diarrhea, dyspnea can occur in patients taking 24mcg BID ❖ Opioid- Receptor Antagonists: Methylnaltrexone • Pharmacodynamics: MOA: Antagonist to the mu-receptor in the GI track and treats the constipation patients experience when taking opioids without affecting the analgesic effect of opioids o Does not cross the BBB therefore does not affect kappa receptor analgesic effect of opioids • Pharmacokinetics: Metabolized in the liver into 5 metabolites • Pharmacotherapeutics: Caution: can cause opioid withdrawal, monitor closely • Adverse reactions: abdominal pain, nausea, diarrhea, hyperhidrosis • Do not take with other opioid antagonists, additive effects Rapid Response and Short Term o Stimulants are the drug of choice when rapid response is needed o All are equally effective, short term o Osmotic laxative work quickly as well o Magnesium hydroxide produces evacuation in 6 to 8 hours and is generally administered before HS o PEG 3350produces a BM in 1 to 3 days o Docusate sodium is the preferred surfactant Slower Response and Long Term o Bulk-forming laxatives are the drug of choice when rapid response is not needed and long term management with the least ADRs o Well suited for older adults o Product choices depends upon patient’s acceptance of texture and taste o Lactulose can be used if the bulk forming laxatives do not work or not well tolerated o Works well in older adults and children Special Indications o Polyethylene glycol electrolyte solutions is the best drug for cleansing the bowel for radiological or surgical procedures o Highly effective and no electrolyte disturbances o Lactulose: effective in reducing ammonia levels in the blood and brain with patient who have hepatic encephalopathy o Lubiprostone is indicated for the treatment of constipation associated with IBS in women aged 18 and older or chronic idiopathic constipation, opioid induced constipation with chronic noncancer pain o Methylnaltrexone is indicated for constipation associated with chronic opioid use Pregnancy o Bulk forming laxatives and surfactant are safe and effective for regular use throughout pregnancy and for lactating women o Magnesium hydroxide is Preg Cat B and can be used intermittently Monitoring o For patients taking laxatives for more than 6 months, laboratory assessment of fluid and electrolytes, K, and Mg l o Careful monitoring r/t hepatic encephalopathy o For older adults taking lactulose for more than 6 months: lab assessment of K, Cl, and CO2 Patient Education o Do not take laxatives with NV or ABD pain, may indicate serious d/o o Rapid acting laxatives are best taken in the morning o Slower acting ones are best taken at bedtime o Taking on an empty stomach with a full glass of water produces more rapid results o Do not crush or chew EC tablets o Liquids can be given with fruit juice o Be careful when pouring bulk forming powder: hypersensitivity reactions have occurred when powder inhaled o Lifestyle management ➢ GERD (Treatment, dosing, and patient education) o Treatment ▪ Goals of treatment: reduce or eliminate symptoms, heal any esophageal lesions, manage, or prevent complications such as stricture, Barret’s esophagus, or esophageal carcinoma, and prevent relapse ▪ Meeting these goals requires both lifestyle modification and drug therapy ▪ Each of the contributing factors (decreased LES tone, acid, peristalsis, and mucosal exposure) are targets for pharmacological management ▪ Drugs to Improve LES tone: • metoclopramide and bethanechol: Not considered for monotherapy o Most useful in combination with aid suppression with gastroparesis o Do not heal esophageal lesions • Antacids: dual purpose: improve LES tone and increase gastric pH ▪ Drugs to Reduce the Amount of Acid • Two main classes: H2RAs and PPIs • H2RA: act on parietal cells to decrease the amount of acid o May be used as maintenance acid suppression or heartburn therapy without erosive GERD o ACG guidelines recommend a trial of nighttime H2Ras for patient taking daytime PPIs to treat nighttime reflux • PPI: First-line therapy for GERD o Improve esophageal healing ▪ Drugs to Improve Peristalsis • A few patients continue to report symptoms despite reduced acid secretion • Prokinetics: improve LES tone and peristalsis • Metoclopramide may provide some benefit but has ADRs ▪ Drugs to Decrease Mucosal Exposure • Cytoprotective agents: sucralfate (Carafate) and misoprostol (Cytotec) o Dosing ▪ PPI therapy: First line therapy for moderate or severe GERD or erosive disease • Length of therapy 8 weeks • No major differences in response between the PPIs • Maintenance PPI should be prescribed for patients who have symptoms that recur after PPI therapy is d/c or complications such as erosive esophagitis or Barrett’s esophagitis • Reassess in 6 to 12 months to determine if weaning can occur • Patients who do not respond to PPIs need referred to GASTRO ▪ H2RA Dosing: • Cimetidine 800 mg BID or 400 mg QID with meals and before bed x 12 weeks • Famotidine 20 mg BID up to 6 to 12 weeks • Nizatidine 150 mg BID • Ranitidine 150 mg BID (no longer available in the US) o Patient Education • PPI Patient Education: o All should be taken on an empty stomach before a meal, in the AM if possible ▪ Food decreases absorption o Stepwise therapy, Step-up or step-down approach may be used o Steps based on symptom relief and degree of esophageal damage o Treatment begins with lifestyle modifications and OTC antacids or H2Ras (most have tried before seeking care) o ACG recommends, 8 weeks of PPIs for symptoms relief and healing of erosive esophagitis associated with GERD o Standard one a day therapy started and tailored to symptoms relief. o If nighttime symptoms are an issue dosing can be adjusted or twice a day dosing can be used o Another option would be to add an H2RA before bed o Failure to achieve symptom relief after 3 months or s/s of complications refer to GASTRO o PPIs may mask symptoms of gastric CAs o Alarm symptoms (dysphagia, painful swallowing, noncardiac chest pain, weight loss, hematemesis, and choking) suggest endoscopy as part of the initial evaluation o All PPIs are approved to treat GERD o Once daily dosing is taken 30 to 60 minutes before breakfast, Length of therapy is 8 weeks, An addition 4 weeks may be needed o Nonresponsive patients require referral o Patients may need long-term intermittent therapy for GERD • H2RA Patient Education: o Should be taken w/ meals or immediately after & at bedtime, daily doses are best @ bedtime, o take 1 hour away from other drugs, o & two hours away from sucralfate o OTC preparations should not be taken for more than 2 wks without consulting healthcare provider o Report black tarry stools- may indicate GI bleeding. o Sore throat, diarrhea, rash, confusion, or hallucinations should be reported promptly (might need dosage adjustment or discontinuation), o advise pt. to stop smoking (interferes with absorption of H2RA & increases gastric secretion) Algorithm for gastroesophageal reflux disease (GERD) PUD (Treatment, Dosing, and Patient Education) o Largely treated in the primary care setting o Risk factors: smoking, habitual NSAID or ETOH use, significantly caused by H. pylori infection which requires eradication o Two categories duodenal ulcers and gastric ulcers o All recommended treatment regimens include a combination of a PPI and antimicrobial therapy o Antimicrobials: clarithromycin, tetracycline, amoxicillin, levofloxacin, and metronidazole o Given in a tiple drug regimen (Two antimicrobials and a PPI x 14 days) or a quadruple drug regimen that includes bismuth subsalicylate o Acid suppression by the PPI in conjunction with the antimicrobial help alleviate ulcer relate symptoms, heals gastric mucosal inflammation, and may enhance the efficacy of antimicrobial agent against H. pylori o Goals of treatment: eradicate H. pylori, heal ulcers, manage, or prevent complications such as GI bleeding or gastric carcinoma, prevent relapse, and reduce or eliminate symptoms o Meeting these goals requires both lifestyle modification and drug therapy o Algorithm: outlines the steps in treating peptic ulcers, consists of healing the ulcer and preventing ulcer recurrence through eradication of H. pylori ▪ Step 1: lifestyle modification, OTC antacids or H2RA ▪ Step 2: h. pylori testing and PPI if uncomplicated Step 3 ▪ Step 3: Treatment for H. pylori with ABX and PPI • PPI continue for 8-12 weeks until healing complete o If low risk: No ongoing therapy o If high risk: Consider chronic suppressive therapy with PPI or H2RA (smokers, >60 y/o, COPD, CAD, Hx of bleeding or perforated ulcer, patients on NSAIDs) ▪ If complicated (bleeding)-Refer to GASTRO for endo-Tx for H. Pylori-Repeat endo in 12 weeks to determine healing o Antacids: Aluminum hydroxide/magnesium hydroxide combination ▪ Maalox 15-30 mL PRN 1 hr and 3 hr after meals and before bed o PPIs-multidrug regimen for ulcers, short-term therapy ▪ Take on an empty stomach before meals o Education: ▪ Stop taking PPIs two weeks before H pylori testing ARF false negative ▪ Take all medications are prescribed ▪ ADRs ▪ Reasons why the drugs are being taken IBS (Treatment, Dosing and Patient Education) ▪ Laxatives: stimulants and chloride channel activators ▪ Stimulants: cascara, sena, bisacodyl, and castor oil o Caster oil: contraindicated in pregnancy ▪ Chloride channel activator: Lubiprostone (Amitiza) o IBS with constipation in women 18 and older o Nausea, take with food o Nausea diarrhea, and dyspnea in doses 24 mcg BID ▪ Do not take laxatives with NV or ABD pain, may indicate serious d/o ▪ Rapid acting laxatives are best taken in the morning ▪ Taking on an empty stomach with a full glass of water produces more rapid results ▪ Do not crush or chew EC tablets ▪ Liquids can be given with fruit juice ▪ Lifestyle management Traveler’s Diarrhea (Treatment, Dosing, and Patient Education) • Bismuth subsalicylate and loperamide (Imodium) • Bismuth subsalicylate: two tablets or 2 Fl oz before each meal and at bedtime (QID) for up to 3 weeks o 524 mg every 30 minutes for up to 8 doses • Prevention and treatment • High-risk areas: Central and South American, Africa, Middle East, Mexico, and Asia • E. Coli is the most common causative agent followed by Campylobacter, Shigella, and Salmonella • Decrease ASA intake while taking bismuth subsalicylate: salicylate toxicity • Can turn the tongue and stool black/gray: not cause for concern, normal finding • Loperamide (Imodium): Adults 4 mg initially, 2 mg after each loose stool, not to exceed 8 mg/day OTC or 16mg/day Rx Black box warning for metoclopramide: • BLACK BOX WARNING: risk for developing tardive dyskinesia and parkinsonian-like symptoms, the risk increases the longer it’s in use, treatment should not exceed 12 weeks and be discontinued immediately if signs of movement disorder, Report involuntary movement of the eyes, face, or limbs immediately Step wise progression of PPIs: antacids and lifestyle modifications followed by PPI trial Effectiveness of different PPIs: No significant differences between effectiveness of PPIs Triple therapy for H.Pylori Eradication: ➢ All include a BID dose of PPI ➢ Most popular ABX are clarithromycin (Biaxin) and amoxicillin ➢ Clarithromycin plus amoxicillin plus a PPI all BID for 10-14 days is most favorable ➢ Pregnant women should not take tetracycline ARF fetal harm ➢ Children younger than 8 should not take tetracycline ARF discoloration of teeth Chapter 34 GERD and PUD Misoprostol use for duodenal ulcer prophylaxis and treatment Misoprostol (Cytotec): Prophylaxis and Treatment of Duodenal Ulcers Associated with NSAID Use: not as reliable for Tx of ulcers from other causes • NSAIDs inhibit prostaglandin synthesis and damage the mucosal lining of the stomach • R/f ulcer formation • Misoprostol is FDA approved for this use (prophylaxis or treatment) • Dosage 200 mcg QID with food ACHS • If unable to tolerate 100 mcg QID with food ACHS • Misoprostol with food, Misoprostol given for the duration of NSAID therapy, can cause diarrhea, if persists x1WK notify provider • Continue therapy even if you feel better • Pharmacodynamics: A methyl analogue of prostaglandin E1 • Inhibits gastric secretion through inhibition of histamine-stimulated cyclic adenosis monophosphate (AMP) production • Inhibits basal and nocturnal gastric acid secretion and acid secretion in response to stimuli o meals, histamine, and coffee by binding to prostaglandin E receptors, mucosal protective qualities. • Mucosal protective qualities as well o Binds to prostaglandin E receptors which facilitate mucus and bicarbonate production • Can be taken with food and still be effective • Pharmacokinetics • Rapidly and extensively absorbed after PO administration (distribution unknown) • Rapidly converted into a free acid • Does not affect CYP450 system • Half-life is 20-40 mins however renal impairment doubles its half-life • Metabolite excreted in urine • Pharmacotherapeutics • Use with caution with caution in renal impairment (no routine adjustments) • Use with caution in the elderly r/t decreased renal function • Pregnancy X: Can produce uterine contractions endangering pregnancy causing spontaneous abortion, premature birth, or birth defects. Women of childbearing age should have a negative pregnancy test before prescribed and start misoprostol on day 2 or 3 of menstrual period. If pregnancy is suspected, drug should be stopped immediately. • ADRs GI or gynecological o Most common: diarrhea, ABD pain, nausea, and flatulence o Postmenopausal bleeding, spotting, cramps, hypermenorrhea, menstrual disorder, and dysmenorrhea • Drug/Drug interactions: R/f increased diarrhea when given with magnesium based antacid • Indicated for prophylaxis and treatment of duodenal ulcers associated with NSAID use Mechanism of action for Lubiprostone • Pharmacodynamics: MOA: is a bicyclic fatty acid derived from prostaglandin E1 that acts by specifically activating CIC-2-chloride channels on the apical aspect of gastrointestinal epithelial cells, producing a chloride-rich fluid secretion. • These secretions soften the stool, increase motility, and promote spontaneous bowel movements. • Used for chronic idiopathic constipation, IBS with constipation in women aged 18 and older, and chronic opioid-induced constipation in adults with chronic noncancer pain [Show More]
Last updated: 2 years ago
Preview 1 out of 37 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 29, 2022
Number of pages
37
Written in
Additional information
This document has been written for:
Uploaded
Jan 29, 2022
Downloads
0
Views
99