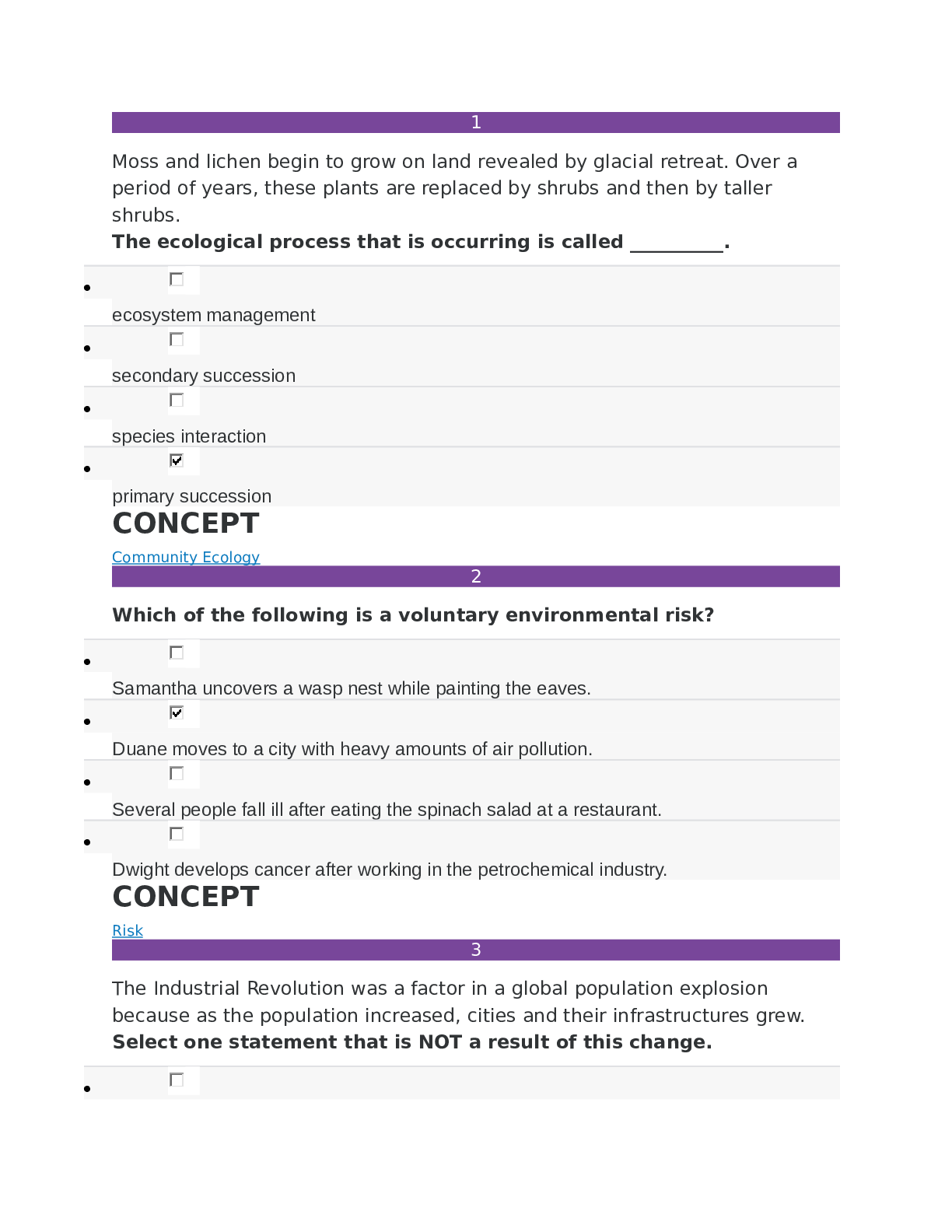
NR 226- Exam 3 Study Guide ALL ANSWERS 100% CORRECT SPRING FALL-2022 LATEST SOLUTION GUARANTEED GRADE A+
Document Content and Description Below
1. Pain in older adults, adults, children and infants; nursing process
Pain in older adults – muscle mass decrease, body fat increases, & percentage body water decreases (means increase concentrati
...
on of water-soluble drugs (morphin) & amount of distribution for fat-soluble drugs increases (fentanyl)); poor eating results in low serum albumin levels (protein made by liver) causing drugs that are high protein to increase the risk for side and/or toxic effect; liver & kidney functions decrease reducing the metabolism & excretion of drugs (means they experience a greater peak effect & longer duration); skin is thinner w/ loss elasticity making absorption of topical analgesic rate faster. ; development of pathological conditions that cause pain (reduces mobility, ADL’s, social activities, & activity tolerance.
Infants – they don’t understand pain and why it happens; they cant express themselves through words; they feel pain before they are born; they have same sensitivity to pain as older children; their pain is observable; very sensitive to drugs (absorb faster, response is intense & prolonged)
Children – they don’t remember how the pain happened or associate it w/ experiences
Nursing process for older adults – aggressive assessment, diagnosis,& management; make detailed assessments when they have more than one source of pain; they have difficulty recalling pain or giving detailed explanations about pain.
Nursing process For infant and children – learn how to assess pain for them; know what to ask; what behaviors to observe; learn how to prepare them for a painful medical procedure.
2. Classifications of pain by location: Superficial/Cutaneous, Deep/Visceral, Referred, and Radiating Superficial/cutaneous - pain on the skin; short duration & localized; sharp sensation
Deep/ visceral pain – pain coming from an organ; diffuse pain & radiates in several directions; duration varies but last longer than superficial; sharp, dull, or unique to organ.
Referred – feeling pain that is distal to the actual site; common in visceral pain because organs have no receptors; sensory from organ goes into spinal cord in same segment as the area where the pain is felt; pain is felt in area that is not effected; different characteristics for pain
Radiating – pain that extends from the pain initial area to another part; traveling pain down or along body; intermittent or constant
3. Pain management; analgesics and nonpharmacological pain relief methods; nursing implications, safety precautions, medication administration
Analgesics –
• Nonopioids - acetaminophen & nonsteroidal anti-inflammatory drugs (NSAIDS); acetaminophen (Tylenol) has no anti-inflammatory effects, most tolerated & safe, hepatotoxicity is an adverse effect; max 24 hr dose is 4g, used w/ opioids to reduce dose for pain relief; NSAIDs (aspirin & ibuprofen) mild- moderate pain relief for acute intermittent pain, postoperative pain begins w/ NSAIDs unless contraindicated, does not depress CNS or interfere w/ bowel & bladder functions, chronic use not recommended for older adults because it causes GI bleed & renal insufficiency, pt w/ asthma or aspirin allergy also allergic to other NSAIDs, since some are OTC discuss w/ pt to tell provider of any use, safe when taken in short periods
• Opioids – narcotic, moderate- severe pain, rare adverse effect in opioid-naïve pt is respiratory depression (only serious if both rate & depth decrease), adverse effect sedation ALWAYS occurs before respiratory depression, other adverse effects nausea, vomiting, constipation , itching, urinary retention, myoclonus & altered mental process; side effects stop after 4-10 days of ATC opiate;
• Adjuvants – variety of meds that enhance analgesics or have analgesic properties that were originally unknown; to treat conditions other than pain but also have analgesic properties.
Nonpharmacological pain relief methods –
• relaxation techniques - (mediation, yoga, zen, guided imagery & progressive exercises) teach only when pt is not distracted by acute discomfort, can use combination for optimal pain relief;
• distraction – (singing, praying, listening to music, laughter, playing games) taking the pt’s attention away from the
pain; works best for short intense pain lasting a few minutes
• music – treat acute, chronic, stress, anxiety & depression; takes attention away from pain; 20 -30 min; they can use headphones to increase concentration & not disturb others
• cutaneous stimulation – (TENS unit, massage, warm bath, ice bag) stimulates skin to reduce pain perception;
releases endorphins & blocks painful stimuli; remove all noises from the environment, put pt in comfortable position, & explain therapy; do not use on sensitive skin areas; when using cold & heat application make sure it is not directly on skin & check temp before putting on skin.
• Herbs – (Echinacea, ginseng, ginkgo, biloba & garlic supplements) can interact w/ analgesics so ask pt if they are taking any
Safety precaution & medication administration – administer ATC instead of PRN to maximize relief & potentially decreasing
drug use. do not use meperidine(Demerol) w/ older adults because it causes seizures. Pt is opioid naïve for first 4-10 days of ATC then become opioid tolerant. use careful assessment & critical thinking. If inflammation, NSAID is more effective than opioid. Oral has longer onset & duration than injectable. Controlled or extended release opioid (morphine, oxycodone, & methadone) are available for 8 to 12 hrs ATC, not PRN. Know potencies of oral or injectable. Know route of admin most effective for pt. know pt’s situation (treatment, disease/condition, &/or organ functions). Safe and effective range orders go according to pt’s age, pain intensity. Sedatives, antianxiety & muscle relaxers have no analgesic effect.
4. Administering analgesics; nursing implications, safety concerns, client education, opioid naïve client
know if pt has allergies; any risk using NSAIDs (GI bleed or renal insufficiency) or opioids (obstructive or sleep apnea); previous dose & route to avoid undertreatment; obtained relief?; nonopioid effective as opioid?. Nonopioid or opioid combination drugs for mild-moderate pain or severe pain because it treats pain peripherally & centrally; can give both together except for older adults; fentanyl patches, morphine or hydromorphone are used long-term for severe pain; IV quicker & relieve within 1 hr and oral takes 2 hrs; avoid IM analgesics especially in older pt; chronic pain give sustained oral ATC. 4 g max in 24hr for acetaminophen & acetylsaliyic acid; 3200mg for ibuprofen. Adjust doses for kids & older pt’s; large dose of opioid is ok for opioid tolerant not opioid naïve. Administer as soon as pain occurs & before it increases in severity; ATC admin is best; give before pain-producing procedures or activities; know average duration of action of drugs & time of admin so the peck happens when pain is worse; use extended release for chronic pain; to not suddenly stop opiates on opioid tolerant pt’s
opioid naïve pt – rare adverse effect is respiratory depression; both rate & depth decrease; sedation always occurs before respiratory depression; closely monitor; if they have it give naloxone (narcan)(0.4mg diluted w/ 9mL saline) IVpush at a rate of 0.5mL every 2 min until respiratory rate is more than 8 breath/min w/ good depth; giving faster than that rate causes severe pain & complications; reassess every 15 min for 2 hours because duration is less than opioid & respiratory depression can come back. If they have PCA do not increase dose or basal and shorten interval time at the same time, this will risk oversedation & respiratory depression.
5. Physical dependence vs addiction vs tolerance
Physical dependence – withdraw symptoms because the person got use to the drug. It happens when they suddenly stop, rapidly decreasing dose, decreased blood levels in the blood and/or when given a antagonist.
Addiction – disease w/ genetic, psychosocial & environmental factors causing it to develop. Not being able to control the use of the drug, overusing, doesn’t care if there is harm they will still use, and craving the drug.
Tolerance – is the level of pain the person is willing to accept
6. Patient controlled analgesics; nursing implications, safety, calculating dosage received, client/family education
is a safe method for pain management; allows pt to self-admin opioid (morphine, hydromorphone & fentanyl) w/ little risk to overdose; goal is to keep rate constant to avoid PRN dosing; most have a locked safety system that prevents tampering by pt
or family & is safe to manage at home; pt has control of pain & doesn’t need to depend on nurse; access med when needed;
decreases anxiety and leads to decreased med use; small dose in small intervals. Pt needs to understand device and physically be able to locate & press button to deliver dose; family member can’t push button for pt; use authorized agent controlled analgesia (AACA) guidelines to “authorize” a family member or nurse to administer med when appropriate. Check IV line & device per institutional policy to ensure proper functioning; very important for nurse to teach so there is no errors related to programmed PCA; for opioid- naïve pt’s do not increase demand or basal dose and shorten the interval time together at the same time because there is a risk of oversedation & respiratory depression; document drug dosage & track med waste according to policy; PCA doses are not recommend for opioid-naïve pt’s after surgery because can cause respiratory depression. Have a second RN confirm order of health care & device setup (they have to independently check not just look at what you are doing). Follow 6 rights! Pt is at highest risk first 12 hrs of use. If pt is not waking up, STOP PCA, elevate head of bed unless contraindicated & asses vitals. DO NOT LEAVE BEDSIDE. Notify healthcare provider &/or call for help. Prepare to give opioid-reversing agent.
Teaching - teach to use PCA before procedure so pt knows what to do after waking up from anesthesia or sedation, reinforce if needed; tell them about purpose & make sure they know that they control the med. Let them know the pump prevent the risk of over dose. Let friends & family know that they CAN’T operate the device for the pt. when done ask pt to tell yout purpose of PCA, watch them give themselves a dose and evaluate pt’s pain while using device.
Bowel Elimination
1. Defecation; Valsalva maneuver
Defecation – begin w/ movement in left colon towards anus; when stool reaches rectum the distention causes relaxation of internal sphincter & awareness of the need to go; when it’s time to poop the external sphincter relaxes, abdominal muscles contract, increasing intrarectal pressure & forcing poop out; normal pooping should be painless w/ soft, formed stool.
Valsalva maneuver – is pressure used when pooping; it’s voluntary contraction of the abdominal muscle while maintaining forced expiration against closed airways; pt’s w/ cardiovascular disease, glaucoma, increased intracranial pressure or new surgical wounds are at greater risk for cardiac dysrhythmias and elevated blood pressure so they need to avoid staining.
2. Factors influencing bowel elimination; common causes of constipation
Common causes of constipation - Ignoring urge to go; irregular bowel habits; chronic illnesses (Parkinson, MS, rheumatoid arthritis, chronic bowel disease, diabetic neuropathy, eating disorders); low-fiber diet & high fat(meats, dairy, eggs); low fluid intake; anxiety, depression, cognitive impairment; no exercise; extended bedrest; misusing laxatives; slowed peristalsis, loss of abdomen muscle elasticity, & reduced intestinal mucus secretion experienced by older pt’s; neuro conditions that block nerve impulses (spinal cord injury, tumor); hypothyroidism, hypocalcemia or hypokalemia; meds (anticholinergics, antispasmodics, anticonvulsants, antidepressants, antihistamines, antihypertensives, antiparkinsonism, bile acid sequestrants, diuretics, antacids, iron supplements, calcium supplements, & opioids)
Factors influencing bowel elimination -
Age – infants poop faster because of small stomach & less digestive enzymes; they have rapid peristalsis; they cant control poop. In older pt’s functional digestion changes are caused by changes in cardiovascular & neuro not because of GI; peristalsis decreases & esophageal emptying slows; impairs digestion & elimination; they lose control of pooping because of lose muscle tome in perineal floor & anal sphincter; nerve impulses in anus slow so they don’t know when they have to go Diet – fiber creates bulk to flush fats and waste easier (whole grains, fresh fruits, & veggies); bowel walls stretch creating peristalsis & keeping stool soft; high-fiber means normal poop pattern; diet high in veggies & fruits linked to decrease risk of colorectal cancer; gas-producing foods stimulate peristalsis by distending the intestines (onions, cauliflower & beans); spicy foods increase peristalsis but also give you indigestion & watery poop; food intolerance is not an allergy it just puts the body in distress within a few hours of eating (diarrhea, cramps or flatulence)
Fluids – not enough intake or fluid loss changes the character of poop; it slows passage in intestines making poop harder(risk for constipation); drink at least 1100-1400mL of fluid daily; increase intake w/ fruit juices (softens poop & increases peristalsis)
Physical activity – promotes peristalsis & immobilization stops it; weak abdominal & pelvic floor muscles impair the ability to
increase intraabdominal pressure & control the external sphincter leading to increase risk for constipation
Psychological factors – emotional stress causes digestion to be faster & peristalsis to increase which leadsd to diarrhea & gaseous distention (diseases associated are ulcerative colitis, IBS, certain gastric & duodenal ulcers and crohn’s); if depressed then ANS slows peristalsis and results in constipation.
Personal habits – busy schedule interrupts your need to go when you urge risking constipation; know best time to go; pt’s that share bathroom or use bedpans become embarrassed because of sight, sound and smell this causes them to become embarrassed and ignore urge to go risking constipation & discomfort.
Position during defecation – squatting is the normal position for ease
Pain – hemorrhoids, rectal surgery, rectal fistulas & abdominal surgery gives discomfort; pt’s avoid urge to avoid pain causing constipation
Pregnancy – fetus is putting pressure on rectum and slowing peristalsis especially during 3rd trimester leading to constipation; from straining and delivery can cause permanent hemorrhoids.
Surgery & anesthesia – general & inhaled anesthesia causes peristalsis to stop temporarily; local or regional is less of a risk to stop peristalsis because it either effects minimally or not at all; condition called paralytic ileus and usually last 24-48 hrs Meds – cause different effects (opioids – constipation, dicyclomine(bentyl) – constipation, anticholingeric – constipation, antibiotics – diarrhea, NSIADs – gi irritation & rectal bleeding, aspirin – gi bleeding, histamine antagonist – suppress hydrochloric acid & interfere w/ digestion, iron – black poop, nausea, vomiting, constipation/diarrhea & abdominal cramps); laxatives & cathartics soften poop and promote peristalsis; laxatives is milder in action but when both use correctly can maintain normal bowel; laxative overuse causes serious diarrhea which leads to dehydration & electrolyte depletion, chronic use of cathartics causes large intestines to become less responsive to the stimulation of laxatives.
Diagnostic testing – for test that require the bowel to be empty they have to use medication, cathartics and/or enemas; pt can’t eat or drink anything several hrs before test; when procedure done they have changes in bowel like increased gas or loose stool until the pt can eat normal again.
3. Constipation/Diarrhea; assessment, nursing implications, client education
Constipation – not a disease, it’s just a symptom; improper diet, reduced fluids, no exercise, & certain meds. signs are infrequent movements (less than every 3 days), hard time passing rectal stool, excessive straining, unable to go at will, hard feces. Do not let a pt that has had resent abdominal, gyno, or surgery try to strain, it can cause sutures to open. Pt’s w/ history of cardiovascular disease, disease causing intraocular pressure (glaucoma) and increased cranial pressure have to prevent constipation and not use Valsalva. If not relieved impaction will occur.
Diarrhea - increased number of times gone & passage of liquid unformed poop; it affects digestion, absorptions & secretion in GI; it passes quickly through both intestines not allowing enough time to absorb fluid & nutrients; unable to hold urge; excess lose causes serious fluid & electrolyte or acid-base imbalances; infants & adults are prone to complications because the repeated stool exposes skin on perineum & butt to be irritated and cause skin breakdown; antibiotics, enteral nutrition, food intolerance & allergies, surgery, and GI diagnostic test also causes diarrhea; the goal is to slow peristalsis & remove causing condition; common agent for diarrhea is Clostridium difficile (C. diff) which can be caused by overgrowth or by contact; foodborne pathogens also cause diarrhea.
4. Bowel diversions; indications, techniques, bowel characteristics
It is a temporary or permeant artificial opening called a stoma on the abdominal wall; Ileum (ileostomy) or colon (colostomy) ends are brought to the surface of abdominal wall.
Ileostomy bypasses the entire large intestine so poop is liquid form & frequent; colostomy in ascending colon is the same type of stool; In the transverse colon it is more solid formed poop; in sigmoid colostomy releases near-normal poop.
Loop colostomy – medical emergency when doctor anticipates closure of colostomy; temporary large stoma in transverse colon; pulling a loop of bowel into
[Show More]
Last updated: 3 years ago
Preview 1 out of 12 pages