*NURSING > EXAM > RNSG 2504 Cardiac Quiz_Spring 2020 – Lone star College | RNSG2504 Cardiac Quiz_Spring 2020 (All)
RNSG 2504 Cardiac Quiz_Spring 2020 – Lone star College | RNSG2504 Cardiac Quiz_Spring 2020
Document Content and Description Below
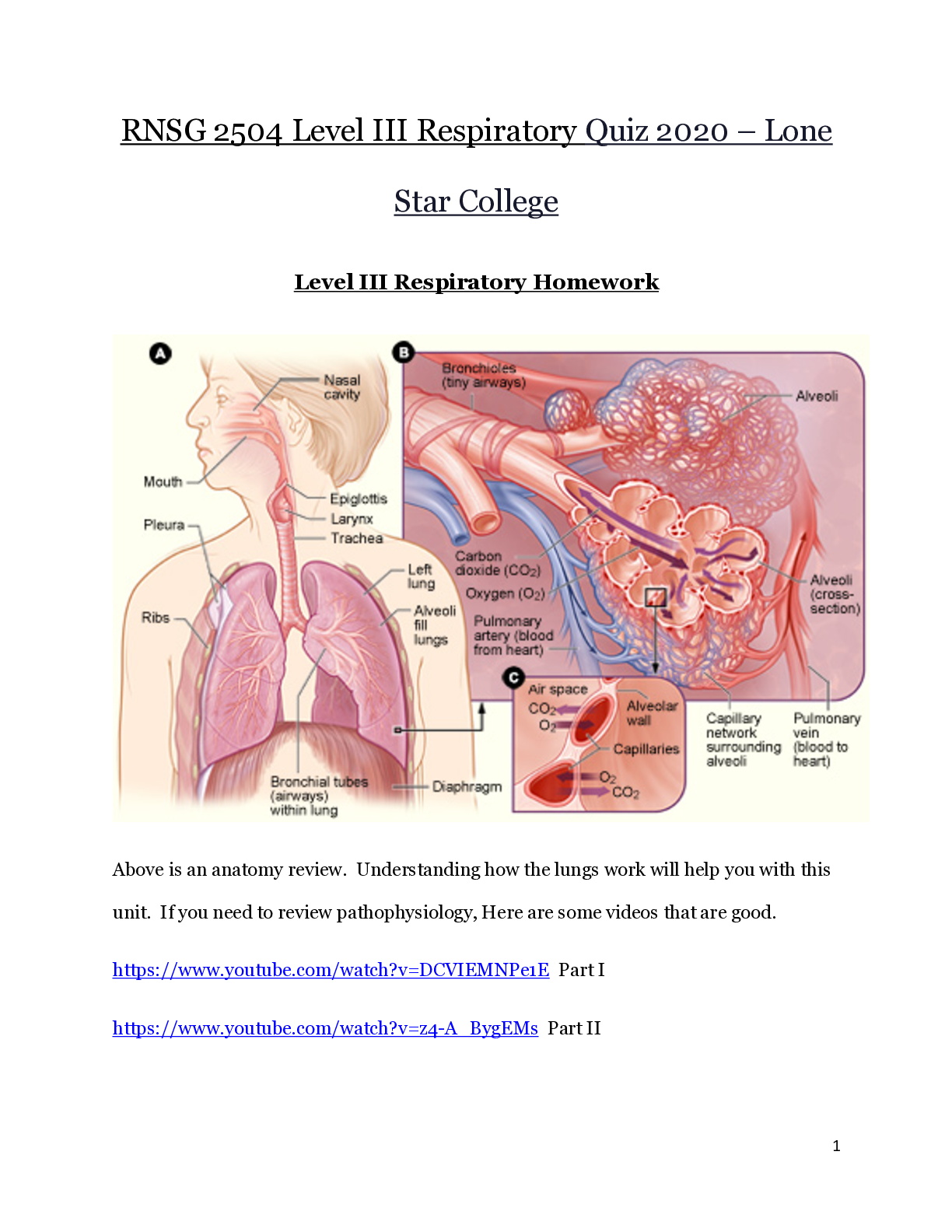
RNSG 2504 Cardiac Quiz_Spring 2020 – Lone star College Cardiac Homework SP2020 Management of Patients With Structural, Infectious, and Inflammatory Cardiac Disorders Watch the following video o... n heart valve disorders https://mendedhearts.org/video/understanding-heart-valve-disease/ Structural, infectious, and inflammatory disorders of the heart present many challenges for the patient, family, and health care team. Problems with heart valves, cardiomyopathies, and infectious diseases of the heart alter cardiac output. Valvular Disorders Atrioventricular valves separate the atria from the ventricles and include the tricuspid valve, which separates the right atrium from the right ventricle, and the mitral valve, which separates the left atrium from the left ventricle. The tricuspid valve has three leaflets; the mitral valve has two Both valves have chordae tendineae that anchor valve leaflets to papillary muscles of the ventricles.- - - - -- - - - - - - - - - - - - - - Mitral regurgitation involves blood flowing back from the left ventricle into the left atrium during systole. Often, edges of mitral valve leaflets do not close completely during systole because leaflets and chordae tendineae have thickened and fibrosed, resulting in their contraction. List three risk factors for mitral valve regurgitation: - Infective endocarditis - Systemic lupus - Rheumatic fever Mitral Stenosis Mitral stenosis is an obstruction to blood flowing from the left atrium into the left ventricle. It most often is caused by rheumatic endocarditis which progressively thickens mitral valve leaflets and chordae tendineae. Leaflets often fuse together. Eventually, the mitral valve orifice narrows and progressively obstructs blood flow into the ventricle. What should a client with mitral stenosis be taught to avoid? - Strenuous activities and competitive sports Aortic Regurgitation/Insufficiency Aortic regurgitation is flow of blood back into the left ventricle from the aorta during diastole. Why are verapamil and diltiazem contraindicated in a client with aortic regurgitation? - Because they decrease ventricular contractility and may cause bradycardia Aortic Stenosis Aortic valve stenosis is narrowing of the orifice between the left ventricle and aorta. Prevention of aortic stenosis is primarily focused on controlling which risk factors? - Controlling risk factors for proliferative and inflammatory responses namely, through treating diabetes, hypertension, hypercholesterolemia, and elevated triglycerides and avoiding tobacco products. Condition Most notable assessment findings Describe Murmur Mitral Prolapse An extra heart sound, referred to as a mitral click. A mitral regurgitation click murmur may be heard if the valve opens during systole and blood flows back into the left atrium Mitral Regurgitation Dyspnea, fatigue, and weakness A systolic murmur is a high-pitched, blowing sound at the apex that may radiate to the left axilla Mitral Stenosis A weak pulse and irregular pulse in the presence of atrial fibrillation A low-pitched, rumbling diastolic murmur is heard at the apex Aortic Regurgitation *note where pulsations might be visible (water hammer ‘Corrigan’s’ pulse) Palpate the patient’s forearm with the patient’s arm above their head. A high-pitched, blowing diastolic murmur is heard at the third or fourth intercostal space at the left sternal border. Aortic Stenosis Vibrations felt over the base of the heart ‘second intercostal space next to the sternum and above the suprasternal notch’ and up along the carotid arteries. Loud, harsh systolic murmur heard over the aortic area ‘the right second intercostal space’ and it may radiate to the carotid arteries and apex of the left ventricle. The murmur is low pitched, crescenodecrescendo, rough, rasping, and vibrating. What medication classes or drug names would help in the management of valvular heart disease? - Diuretics - Inotropic agents - Anticoagulants - Afterload-reducing agents - Ace inhibiters - Beta blockers - - - - - - - - - - - - - - - What are clients with HCM or RCM preventing by limiting physical activity and avoiding excessive weight gain? - It lets the heart rest (ventricle) to avoid increasing the muscle size Infectious Diseases of the Heart Watch https://www.youtube.com/watch?v=8YSfsHjTMx8 Part 1 https://www.youtube.com/watch?v=zVpaTG7VEfk Part 3 List the risk factors for infective endocarditis? (Bacterial) - Microbial infections (staphylococci/streptococci), patients with prosthetic heart valves/cardiac devices/structural cardiac defects/debilitating diseases List the clinical manifestations for endocarditis that uses the mnemonic FROM JANE. - Fever, Roth’s spots, Osler’s nodes, murmur, Janeway lesion, anemia, nail hemorrhage, emboli What type of pathogens are cause myocarditis? (viral) - Coxsackievirus A and B, human immune deficiency virus, influenza A, bacterial, rickettsial, fungal, parasitic, metazoal, protozoal, or spirochetal infection. Which medication should be used cautiously in clients with myocarditis and why? - NSAIDs Should not be used for pain control because they have been shown to be ineffective in relieving the inflammatory process in myocarditis and have been linked to worsening inflammation of the myocardium. This also can contribute to an increased mortality from increased virulence of the pathogen A 50-year-old patient has been admitted to the cardiac unit with pericarditis. Using the nursing process as a framework for care for the patient with pericarditis, what are the key assessments and interventions that need to be completed? - Assess the patient for pain- assess by evaluating the patient’s pain in various positions to identify whether pain is influenced by respiratory movements, while holding an inhaled breath or holding an exhaled breath; by flexion, extension, or rotation of the spine, including the neck; by movements of shoulders and arms; by coughing; or by swallowing. Assess the patient for a pericardial friction rub; the rub is audible on auscultation and is synchronous with the heartbeat. - Relieve pain, and monitor/manage potential complications (cardiac tamponade) What are common clinical manifestations of streptococcal pharyngitis that the nurse needs to assess in this patient? - Chills, fever 101-104f, sore throat, diffuse redness of throat with exudate on oropharynx, petechiae on the roof of mouth, enlarged/tender lymph nodes, abdominal pain, acute sinusitis, acute otitis media, sandpaper like rash. What education would be helpful for clients with endocarditis, myocarditis or pericarditis? - Early treatment of streptococcal infections can prevent rheumatic fever. Prophylactic treatments (including antibiotics for clients who have cardiac defects) can prevent infective endocarditis. Influenza and pneumonia immunizations are important for all clients (especially older adults) in order to decrease the incidence of myocarditis. Pericardial Effusion and Cardiac Tamponade Describe a pericardial effusion: - Pericardial effusion is an accumulation of fluid in the pericardial sac “fluid around the heart” that leads to an increased intrapericardial pressure which compresses on the heart and causes elevated pressure in all cardiac chambers, decreased venous return due to atrial compression, inability of the ventricles to distend and fill adequately, and cause a cardiac tamponade leading to reduced 02. List the most common assessment findings in cardiac tamponade 1.decreased pulse pressure 2.tachycardia 3.tachypnea 4.hypotension 5.neck vein distention 6. dyspnea 7.distant muffled heart sounds 8.decreased arterial pressure What is the treatment for pericardial effusion/cardiac tamponade? - Removal of pericardial fluid to relieve the elevated intrapericardial pressure and improve cardiac output by pericardiocentesis (needle aspiration of the pericardial cavity), pericardial window (surgical creation of an opening), or pericardectomy (resection of a portion or all of the pericardium). Steps for Cardiac Arrest (Do Not Use the Textbook, use your BLS certification) 1. verify scene safety! 2. Check responsiveness & call for help “activate response team and get the AED” 3. Assess the breathing and pulse 4. Begin CPR if pulse is not identified within 10 seconds 30 compressions to every 2 breaths 5. Attempt defibrillation with the AED – check for pulse 6. Return to compressions and breaths if no pulse detected - - - - - - - - - - - - - - - - - - - No qrs CAD, MI, Cardiomyopathy, Valvular heart disease, hypoxia, electrolyte imbalances CPR, Defibrillation Idioventricular Regular Rate 30-40 P wave absent PR not measureable QRS wide >.12 (looks like a PVC) impulses failing to reach AV junction, sinus arrest, third degree heart block, beat after CPR but just before asystole CPR, this is a dying heart, Atropine, Vasopressors 1st Degree AV Block Regular Rate 60-100 P normal PR >.20 QRS normal Ischemia, injury to AV node (inferior wall MI), increased vagal tone, medication effects (beta blockers, calcium channel blockers, digoxin, amiodarone), hyperkalemia, age Treat electrolytes and discontinue mediations Assess and monitor closely 2nd Degree Type I Irregular Rate typically 60-100 P wave normal PR interval progressively longer until QRS drops QRS normal MI of the inferior wall, vagal tone, medications Monitor (asymptomatic), adjust medications Atropine, external or transvenous pacing, dopamine, epinephrine gtts (for symptomatic) 2nd Degree Type II Surprisingly Regular Rate Have to count atrial and Ventricular P wave normal, but too many before a QRS, not next to each other PR interval not measurable QRS Normal Anterior wall MI, myocarditis, degeneration of electrical conduction (elderly) Pacemaker, dopamine (bandald), NO ATROPINE because it may worsen conduction disturbances. Pt susceptible for 3rd degree lethal arrythmias 3rd Degree Heart Block Regular Rate Count Separately (Slow) P wave Normal shape and size, may appear within QRS complexes PR absent QRS normal or wide Anterior Wall MI, Degenerative changes, Lyme disease, Dig toxicity , Inferior Wall MI (typically resolves within hours) Pacemaker, vasopressors, (dobutamine) Explain the difference between Cardioversion and Defibrillation - Cardioversion is an elective procedure. The client is awake an aware Synchronized with QRS Sedated to preform Consent form is required EkG monitoring Preformed chemically to alter flow of electrical activity through the heart USING ADENOSINE or electrically by synchronized shocking to convert an abnormal rhythm to a normal sinus rhythm - Defibrillation is an emergency procedure to shock the heart LIFE saving measure V-Fib/V-tach No cardiac output Begin with 200 Joules up to 360 Client is unconscious Patient cannot consent Pacemakers Watch https://www.youtube.com/watch?v=53_jyoA47Fk A pacemaker is an electronic device that provides electrical stimuli to the heart muscle. Pacemakers are usually used when a patient has a permanent or temporary slower-than-normal impulse formation, or a symptomatic AV or ventricular conduction disturbance. Pacemakers can be permanent or temporary Temporary pacemakers are used to support patients until they improve or receive a permanent pacemaker (e.g., after acute MI or during open heart surgery). The implantable cardioverter defibrillator (ICD) is an electronic device that detects and terminates life-threatening episodes of tachycardia or fibrillation especially those that are ventricular in origin. Some ICDs can respond with (1 antitachycardia pacing, in which the device delivers electrical impulses at a fast rate in an attempt to disrupt the tachycardia, (2) low-energy cardioversion or (3) defibrillation; others may use all three techniques Nursing Management The incision site where the generator was implanted is observed for bleeding, hematoma formation, or infection, which may be evidenced by swelling, unusual tenderness, drainage, and increased warmth. The patient may complain of continuous throbbing or pain. These symptoms are reported to the primary provider. Educating the Patient with an Implantable Cardiac Device Chart 26-9 1. Avoid infetion at the insertion site of the device 2. Adhere to activity restrictions 3. electromagnetic interference: Understand the importance 4. Promote precautions and safety 5. Follow-up care Identify the following rhythms using EKG Analysis Handout: Rhythm Regular Rate ____50____PWave absent PR Interval immeasurable QRS Interval .12Interpretation sinus bradycardia with ST elevation Rhythm regular Rate 80 PWave inversion PR Interval 0.16 QRS Interval 0.08 Interpretation junctional Rhythm regular Rate 50 PWave present PR Interval <0.2 QRS Interval <0.12 Interpretation second degree type II, Mobitz ii Rhythm regular Rate 90 PWave present, consistent, upright PR Interval >0.2 QRS Interval <0.12 Interpretation normal sinus - - - - - - - - - - - - - Administering medications and IV fluids – watch for s/s of fluid overload when administering IV fluids, monitor for side effects of medications/normal effects of medication, assess for IV access, monitor urine output, serum electrolytes, BUN, creatine levels. - Maintain intra-aortic balloon counter pulsation- The nurse makes ongoing timing adjustments of the balloon pump to maximize its effectiveness by synchronizing it with the cardiac cycle. The patient is at risk of circulatory compromise to the leg on the side where the catheter for the balloon has been inserted; therefore, the nurse must check the neurovascular status of the lower extremities frequently. - Enhancing safety and comfort – administering medication to relieve chest pain, preventing infection at the multiple arterial and venous line insertion sites, protect the skin, and monitor renal and respiratory function, proper positioning of patient may reduce anxiety. What is the primary nursing goal for treating cardiogenic shock? Oxygenation – nasal cannula 2-6 L/min Pain control- IV morphine for chest pain relief and dilate vessels Hemodynamic monitoring- assess the patient’s response to treatment/continuous monitoring of BP Laboratory Marker monitoring - Laboratory biomarkers for ventricular dysfunction, cardiac enzyme levels and biomarkers, and serum lactate are measured, a transthoracic echocardiography may be performed at the bedside, and serial 12-lead electrocardiograms are obtained to assess the degree of myocardial damage Fluid therapy – administration of fluids to increase cardiac output and monitor closely for signs of fluid overload Never underestimate the power of emotion to the heart. This is a holistic thought towards treatment for all these problems. https://www.ted.com/talks/sandeep_jauhar_how_your_emotions_change_the_shape_of_your_heart/transcript?language=en [Show More]
Last updated: 2 years ago
Preview 1 out of 26 pages

Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$12.50
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Nov 03, 2020
Number of pages
26
Written in
Additional information
This document has been written for:
Uploaded
Nov 03, 2020
Downloads
0
Views
48







 – University of the People.png)