*NURSING > EXAM > Rasmussen College :NUR 2513/Maternal 2513 Exam 3 Blueprint FINAL 2021/2022,100% CORRECT (All)
Rasmussen College :NUR 2513/Maternal 2513 Exam 3 Blueprint FINAL 2021/2022,100% CORRECT
Document Content and Description Below
Rasmussen College :NUR 2513/Maternal 2513 Exam 3 Blueprint FINAL 2021/2022 Modules: Dosage calc 7 (Chp 34, 38, 40, 41): Interventions for hospitalized peds client, Respiratory, Cardiac Diseases... /Disorders ● What are techniques for administration of ear drops (less than 2 versus older than 2) Turn the child or ask the child to turn onto his or her back or use restraint as necessary. Turn the child’s head to one side. The slant of the ear canal in children. If the child is younger than 2 years of age, straighten the external ear canal by pulling the pinna down and back. If the child is older than 2 years of age, pull the pinna of the ear up and back. Instill the specified number of drops into the ear canal. Hold the child’s head in the sideways position to ensure the medication fills the entire ear canal. Praise the child for cooperating during this difficult procedure ● What are tips for helping a child take oral medication? Available in preparations (liquids, chewables, and meltaways). Determine the child’s ability to swallow pills. Use the smallest measuring device for doses of liquid medication. Use an oral medication syringe for smaller amounts, and a medication cup for larger amounts. Avoid measuring liquid medication in a teaspoon or tablespoon. Use rigid plastic cups instead of paper cups for liquid medications. Avoid mixing medication with formula or putting it in a bottle of formula because the infant might not take the entire feeding, and the medication can alter the taste of the formula. Hold the infant in a semi-reclining position similar to a feeding position. Hold the small child in an upright position to prevent aspiration. Administer the medication in the side of the mouth in small amounts. This allows the infant or child to swallow. Only use the droppers that come with the medication for measurement. Stroke the infant under the chin to promote swallowing while holding cheeks together. Teach the child to swallow tablets that aren’t available in liquid form and can’t be crushed. Teach in short sessions using verbal instruction, demonstration, and positive reinforcement. Provide atraumatic care. Mix the medication in a small amount of sweet nonessential food (applesauce or sherbet). Offer juice, a soft drink, or snack after administration. Add flavoring to medications as available. Use a nipple to allow the infant to suck the medication. Reward small child with a prize or sticker afterwards. Administer medications via a feeding tube. Confirm placement. Use liquid formulation. Do not add medication to the formula bag. If administering several medications, flush tubing with water after the administration of each medication. ● What are teaching tips for use of a metered-dose inhaler? A metered-dose inhaler (MDI) is a handheld device that provides a route for medication administration directly to the respiratory tract. The child inhales while depressing a trigger on the apparatus. For successful use, children need to follow five general rules: shake the canister, exhale deeply, activate the inhaler and place it in their mouth as they begin to inhale, take a long slow inhalation, and then hold their breath for 5 to 10 seconds. Caution them to take only one puff at a time, with a 1-minute wait between puffs. Coordinating inhalation with MDI use can be difficult; therefore, use of an aerochamber (spacer) is generally recommended to prevent deposition on the posterior pharynx. Younger children can use an MDI attached to an aerochamber with a mask. All children using inhaled corticosteroids need an aerochamber to prevent deposition of the medication in the mucous membranes of the mouth and pharynx, which can contribute to the development of thrush. Instruct the child and guardians to clean the MDI and spacer after each use and to have the child rinse out the mouth and expectorate. -Do not shake the device. -Take the cover off the mouthpiece. -Follow the directions of the manufacturer for preparing the medication (turning the wheel of the inhaler). -Exhale completely. Place the mouthpiece between the lips and take a deep breath through the mouth. -Hold breath for 5 to 10 seconds. -Take the inhaler out of the mouth and slowly exhale through pursed lips. Resume normal breathing. -If more than one puff is prescribed, wait the length of time directed before administering the second puff. -Remove the canister and rinse the inhaler, cap, and spacer once a day with warm running water. Dry the inhaler before reuse. ● What’s important to know about the newborn/infant nose and breathing? What assessments are important? p. 932 Infants are obligate nose breathers. They cannot coordinate mouth breathing, so they become disturbed when the nose is temporarily blocked to check for patency; do this only momentarily to avoid discomfort. Most newborns have milia (i.e., small white papules) on the surface of the nose, which are of no consequence and disappear without treatment. Observe the nose for flaring of the nostrils (a sign of a need for oxygen). Using an otoscope light, observe the mucous membrane of the nose for color—it should be pink; pale suggests allergies, and redness suggests infection. Note and describe any discharge. Document the septum is in the midline because a displaced septa such as those that occur after facial injuries can interfere with respiration and make nasal intubation in emergencies difficult. Gently press one nostril closed and ask the child to inhale. Repeat on the opposite side to ensure both sides of the nose are patent; that is, no choanal atresia or membrane obstructing the posterior nares exists. Sinuses do not fully develop until about 6 years. ● What are signs of dehydration? (see below) -Mild WEIGHT LOSS 3% to 5% in infants, 3% to 4% in children MANIFESTATIONS: Behavior, mucous membranes, anterior fontanel, pulse, and blood pressure within expected findings, Capillary refill greater than 2 seconds, Possible slight thirst -Moderate WEIGHT LOSS 6% to 9% in infants, 6% to 8% in children MANIFESTATIONS: Capillary refill between 2 and 4 seconds, Possible thirst and irritability, Pulse slightly increased with normal to orthostatic blood pressure, Dry mucous membranes and decreased tears and skin turgor, Slight tachypnea, Normal to sunken anterior fontanel on infants -Severe WEIGHT LOSS Greater than 10% in infants, 10% in children MANIFESTATIONS: Capillary refill greater than 4 seconds, Tachycardia present, and orthostatic blood pressure can progress to shock,Extreme thirst, Very dry mucous membranes and tented skin, Hyperpnea, No tearing with sunken eyeballs, Sunken anterior fontanel ● What are interventions for mild/moderate versus severe dehydration from gastroenteritis? pp. 1062-1063; https://www.aafp.org/afp/2009/1001/p692.html NURSING ACTIONS -Oral rehydration is attempted first for mild and moderate cases of dehydration. Mild: 50 mL/kg rehydration fluid within 4 hr Moderate: 100 mL/kg rehydration fluid within 4 hr Replacement of diarrhea losses with 10 mL/kg each stool -Administer parenteral fluid therapy as prescribed. Initiate when a child is unable to drink enough oral fluids to correct fluid losses, and those with severe dehydration or continued vomiting. -Isotonic solution at 20 mL/kg IV bolus with possible repeat for isotonic and hypotonic dehydration. Hypertonic dehydration: rapid fluid replacement is contraindicated because of the risk of cerebral edema. Administer maintenance IV fluids as prescribed. Avoid potassium replacement until kidney function is verified. -Assess capillary refill. Assess vital signs. Monitor weight. Maintain accurate I&O. ● What are therapeutic interventions to manage croup (bronchiolitis)? Cool moist air combined with a corticosteroid, such as dexamethasone, or racemic epinephrine, given by nebulizer, usually reduces inflammation and produces effective bronchodilation to open the airway. The provider may prescribe dexamethasone for home administration but racemic epinephrine needs to be administered in a healthcare setting. ● What are symptoms of streptococcal pharyngitis and complications/risks? Group A β-hemolytic streptococcus is the organism most frequently involved in bacterial pharyngitis in children, particularly those between the ages of 5 and 15 years. Onset is abrupt and characterized by pharyngitis, headache, fever and abdominal pain. Tonsils and pharynx can be inflamed and covered with exudate, usually appears by second day of illness. Streptococcal infections are generally more severe and present more suddenly than viral infections. The back of the throat and palatine tonsils are usually markedly erythematous (bright red); the tonsils are enlarged, and there may be a white exudate in the tonsillar crypts. Petechiae may be present on the palate. A child typically appears ill, with a fever, sore throat, headache, stomach ache, and difficulty swallowing. Other respiratory symptoms are generally absent, such as cough, congestion, rhinorrhea, or conjunctivitis. A rapid antigen test and/or throat culture should be done to confirm the presence of the Streptococcus bacteria. These findings may vary depending on the child’s age and make it difficult to distinguish it from a viral illness. Some children may develop a sandpaper-like rash (scarlatiniform rash) on the body. Although rare, streptococcal infections can lead to acute rheumatic fever and glomerulonephritis if not treated. ● What are post-tonsillectomy nursing cares? POSTOPERATIVE NURSING ACTIONS Positioning: Place in position to facilitate drainage. Elevate head of bed when child is fully awake. Assessment: Assess for evidence of bleeding, which includes frequent swallowing, clearing the throat, restlessness, bright red emesis, tachycardia, and/or pallor. Assess the airway and vital signs. Monitor for difficulty breathing related to oral secretions, edema, and/or bleeding. Comfort measures: Administer liquid analgesics or tetracaine lollipops as prescribed. Provide an ice collar. Offer ice chips or sips of water to keep throat moist. Administer pain medication on a regular schedule. Diet: Encourage clear liquids and fluids after a return of the gag reflex, avoiding red-colored liquids, citrus juice, and milk-based foods initially. Advance the diet with soft, bland foods. Instruction: Discourage coughing, throat clearing, and nose blowing in order to protect the surgical site. Avoid straws as they can damage the surgical site Alert guardians that there can be clots or blood-tinged mucus in vomitus. ● What are signs/clinical manifestations/assessment findings in a child with pneumonia? Bacterial pneumonia: Streptococcus pneumoniae, Group A streptococci, Staphylococcus aureus, Mycoplasma catarrhalis, Mycoplasma pneumoniae Assessment: High fever, Cough that can be unproductive or productive of white sputum, Tachypnea, Retractions and nasal flaring, Chest pain, Dullness with percussion, Adventitious breath sounds (rhonchi, fine crackles), Pale color that progresses to cyanosis, Irritability, restless, lethargic, Abdominal pain, diarrhea, lack of appetite, and vomiting. Children may often appear acutely ill, with high fever, tachycardia, chest or abdominal pain, chills, and signs of respiratory distress. Breath sounds are often diminished, and crackles (rales) may be present. Dullness on percussion indicates total consolidation. Chest radiography will often reveal consolidation, and laboratory studies will indicate leukocytosis. Bacterial pneumonia treatment: Encourage rest. Administer IV antibiotics. Promote increased oral intake. Monitor I&O. Administer antipyretics for fever. CPT and postural drainage can be helpful. Administer IV fluids. Administer oxygen. Monitor continuous oximetry ● What are signs/symptoms and treatments of viral pneumonia? Viral pneumonia is generally caused by viral infections of the upper respiratory tract. Symptoms begin as an upper respiratory tract infection and may progress to diminished breath sounds and fine rales on auscultation. Antibiotic therapy is not effective against viral infections. Rest and antipyretics are used for treatment. Similar to bacterial pneumonia, fatigue often occurs following the acute phase of illness. Viral pneumonia treatment: Administer oxygen with cool mist. Monitor continuous oximetry. Administer antipyretics for fever. Monitor I&O. CPT and postural drainage ● What are treatments and teaching topics for management of cystic fibrosis? NURSING CARE TREATMENT: Assess lung sounds and respiratory status. Vital signs with oxygen saturation. Obtain IV access. Use of a peripherally inserted central catheter or IV port allows for home IV antibiotic therapy. Obtain sputum for culture and sensitivity. Provide support to the child and family. -Pulmonary management: Assist in providing airway clearance therapy (ACT) to promote expectoration of pulmonary secretions. Usually prescribed twice a day in the morning and evening. Avoid ACT immediately before or after meals. Several methods of ACT are available. Chest physiotherapy (CPT) with postural drainage as prescribed (manual or mechanical percussion). Positive expiratory therapy (PEP) uses a device (a flutter mucus clearance device) to encourage the client to breathe with forceful exhalations. Active-cycle-of-breathing techniques (“huffing” or forced expiration), are encouraged. Autogenic drainage uses an electronic chest vibrator or handheld percussor along with breathing techniques. High-frequency chest compression uses a mechanical chest device combined with nebulization therapy. Administer aerosol therapy as prescribed (bronchodilator, human deoxyribonuclease). Often recommended prior to ACT. Administer IV or aerosolized antibiotics. Encourage physical aerobic exercise. Provide oxygen as prescribed (assess for carbon dioxide retention). Monitor for hemoptysis or pneumothorax. -Gastrointestinal management: Provide a well-balanced diet high in protein and calories. Give three meals a day with snacks. Encourage oral fluid intake. Administer pancreatic enzymes within 30 min of eating a meal or snack. Administer water soluble vitamin supplements: multivitamin; vitamins A, D, E, and K. Administer laxatives or stool softeners for constipation. Polyethylene-glycol electrolyte solution is administered orally or via nasogastric tube. Administer histamine-receptor antagonist and motility medications for GERD. Administer possible formula supplements in addition to breastfeedings or via gastric tube. Encourage to add salt to food during hot weather- (dehydration). Consult a dietitian. Children should receive regular nutritional evaluations. -Endocrine management: Cystic fibrosis related diabetes (CFRD) necessitates monitoring of blood glucose levels. Administer insulin. Oral glycemic medications are not effective for CFRD. Medications: Respiratory medications: Short-acting beta2 agonists (albuterol). Cholinergic antagonists (anticholinergics [ipratropium bromide]). Fluticasone propionate/salmeterol. NURSING ACTIONS: Monitor for tremors and tachycardia when the child is taking albuterol. Observe for dry mouth when the child is taking ipratropium. CLIENT EDUCATION: Understand how to properly use an MDI, PEP, or nebulizer. Rinse mouth after fluticasone propionate/salmeterol. Dornase alfa (aerosol): Decreases the viscosity of mucus and improves lung function. NURSING ACTIONS: Monitor sputum thickness and ability of client to expectorate. Monitor the child for improvement in PFTs. CLIENT EDUCATION: Understand how to use a nebulizer.Administer once or twice a day. This medication can cause laryngitis. Antibiotics: Administer through IV or aerosol. Specific to treat pulmonary infection. Common medications include tobramycin, ticarcillin, or gentamicin. NURSING ACTIONS: Assess for allergies. High doses may be prescribed. Collect blood specimens before and after some IV antibiotics to maintain therapeutic levels. Pancreatic enzymes: Pancrelipase treats pancreatic insufficiency associated with cystic fibrosis. NURSING ACTIONS: Monitor stools for adequate dosing (1 to 2 stools/day). Monitor weight. Administer capsules with all meals and snacks. Child can swallow or sprinkle capsules on food. Do not sprinkle on hot foods or add to bottles or formula. Increase dosage of enzymes when eating high-fat foods. INTERPROFESSIONAL CARE: Respiratory and physical therapy, social services, pulmonologist, pharmacist, pediatrician, infectious disease specialists, and dietitians may be involved in the care of the child who has cystic fibrosis. Transplantation of heart, lung, pancreas, and liver for adolescents who have advanced disease can be a consideration. ● What are the mechanisms of asthma and assessment findings you will note? p. 1114 Asthma primarily affects the small airways. The relationship of inflammation to airway hyperresponsiveness and airway obstruction contributes to clinical symptoms. This complex interplay of factors presents as recurrent wheezing, breathlessness, chest tightness, and coughing. Asthma is a chronic inflammatory disorder of the respiratory track and is the most common chronic illness in children. Typically, asthma presents before 5 years of age, although it may be difficult to make a definitive diagnosis in these early years. Typically, an episode begins with a dry cough. Children then develop increasing difficulty exhaling as it becomes more and more difficult for them to force air through the narrowed lumen of the bronchioles that are not only inflamed and swollen but also filled with mucus. Typical dyspnea and wheezing (the sound caused by air being pushed forcibly past obstructed bronchioles) associated with the disorder begin. Wheezing is heard primarily upon expiration because the lumen of bronchioles are narrower during exhalation than inhalation, but it may be absent with severe asthma exacerbations. In some children, the initial wheezing is evident only by stethoscope auscultation; in others, it is so loud it can be heard by simply listening. Air-filled lungs are hyperresonant to percussion or they make a louder, more hollow noise on percussion than usual. With normal respiration, the inspiration phase of breathing is longer than the expiration phase. During an asthma attack, however, a child must work so hard to exhale due to air trapping that the expiration phase becomes longer than the inspiration phase. Time the two phases to demonstrate this. Also, observe for retractions (the chest wall is drawn inward with breaths) because children have to use intercostal accessory muscles to achieve full breaths. As constriction becomes acute, the sound of wheezing may decrease because so little air can leave the alveoli. During attacks, children with asthma are generally more comfortable in a sitting or standing position rather than lying down and should be allowed to be in a position of comfort. If seated in a chair, they lean forward and raise their shoulders to give themselves more breathing space. Children who do agree to lie down are either at the end of an attack and beginning to feel less threatened by the dyspnea or are so exhausted by the paroxysms of coughing that they no longer have the strength to sit upright. EXPECTED FINDINGS: Chest tightness. History regarding current and previous asthma exacerbations (Onset and duration, Precipitating factors, Changes in medication regimen, Medications that relieve manifestations, Other medications, Self-care methods used to relieve manifestations,Home/school environment, Heating/cooling source in the home) PHYSICAL ASSESSMENT FINDINGS: Dyspnea, Cough, Audible wheezing, Coarse lung sounds, wheezing throughout possible crackles, Mucus production, Restlessness, irritability, Anxiety, Sweating, Use of accessory muscles, Decreased oxygen saturation (low SaO2), Tripod positioning, Sitting retractions, Inaudible breath sounds or crackles (severe obstruction) ● When would digoxin be used for a heart condition and what effect/action does it have???? Cardiomyopathy and congenital heart disease are causes of heart failure. Children with CHF are often prescribed digoxin (Lanoxin). Improves myocardial contractility. Digoxin may be used for its positive inotropic and negative chronotropic effects. ● What are safety considerations when caring for a child with a chest tube? (Can read on CTs in book, pp. 1152-1153, but you’ll probably find this answer in your ATIs). Endotracheal suctioning is necessary while a child is receiving ventilatory assistance to prevent secretion accumulation in the lungs or obstruction of the endotracheal tube. Assist with chest physiotherapy (percussion and vibration) as needed to help keep lung secretions mobile. As soon as the endotracheal tube and ventilator are removed, encourage the child to cough and breathe deeply or use an incentive spirometer at hourly intervals as a way to mobilize secretions. Although children may have practiced such procedures preoperatively, they may have difficulty carrying them out postoperatively because coughing and deep breathing after cardiac surgery can be very painful. To minimize pain, administer prescribed analgesia or alert the child to use the patient-controlled analgesia (PCA) pump 10 to 15 minutes before it is time to breathe deeply. Teach children how to use a pillow as a splint while coughing and deep breathing. Be certain parents understand that games such as blowing cotton balls or bubbles, or using the incentive spirometer, are important exercises to help achieve lung expansion. Encourage them to work with the child throughout the day to perform these exercises. Chest tube drainage systems are used after complex cardiac surgeries to collect air from the pleural space, and fluid, typically blood, from the mediastinum, but may be used in other situations such as isolated pleural effusions, chylothorax, or pneumothorax. After surgery, typically one tube in the mediastinal space collects blood and another in the pleural space collects air. Nursing concerns when working with a child who has a chest drainage system include: Keeping the system closed and below chest level Ensuring suction control chambers are filled or set for the ordered amount of suction. If a fluid-filled system, ensure bubbles are in the chamber. Making sure the water seal chamber is filled to manufacturer’s recommended level Monitoring for bubbles in the water seal chamber, which can indicate either a leak in the drainage system or an air leak from the patient’s lungs Assessing and documenting the amount, color, and consistency in the drainage system routinely and as ordered. Report any drainage that changes in volume, color, or bloodiness. NOT aggressively milking or stripping chest tubes, as this can cause very high levels of negative pressure. But it is important to keep the tubes freely draining, which can be difficult if the drainage is frank blood, which may have clots in it. Ensuring adequate pain control. Chest tubes can be very uncomfortable, but it is important for the child to get out of bed, ambulate, cough, or perform pulmonary toilet maneuvers. It is important to obtain a level of pain control that allows the child to be awake and interactive. ● What will heart sounds sound like with a patent ductus arteriosus? Where can this murmur be heard? P. 1140 and https://www.youtube.com/watch?v=LduIjbtF7kA A condition in which the normal fetal circulation conduit between the pulmonary artery and the aorta fails to close and results in increased pulmonary blood flow (left-to-right shunt). Systolic murmur (machine hum) This defect produces a systolic murmur early in life and a continuous murmur as the child ages. The murmur is noted at the second intercostal space, left upper sternal border, or out to the left clavicular area. If the defect is large enough, the flow to the lungs will be significant and can cause rales, congestion, increased work of breathing, difficulty feeding, or failure to thrive. Over time, the left heart can become dilated. The severity of the symptoms depends on the amount of blood shunting to the lungs. A PDA is confirmed with an echocardiogram. ● What are signs you’ll note in a newborn with coarctation of the aorta (CoA) and what are important assessments to do to help confirm your suspicions of this anomaly? A narrowing of the lumen of the aorta, usually at or near the ductus arteriosus, that results in obstruction of blood flow from the ventricle. Elevated blood pressure in the arms, Bounding pulses in the upper extremities, Decreased blood pressure in the lower extremities, Cool skin of lower extremities, Weak or absent femoral pulses, Heart failure in infants, Dizziness, headaches, fainting, or nosebleeds in older children. The common coarctation of the aorta (CoAo) typically causes a discrete narrowing of the aorta. Frequently, children are not diagnosed with a coarctation until they grow and are noted to be hypertensive. The narrowed area is most frequently distal to the right subclavian artery, so the pressures before that area increase and refer out these vessels. This causes elevated blood pressures to be noted in the right arm. Occasionally, a murmur may be noted in these children. If the narrowing is significant, it can cause a systolic murmur heard along the left sternal border and the left midscapular area. This narrowing increases the resistance to the left ventricle and can lead to left ventricular hypertension and hypertrophy over time. Coarctation noted in infancy is usually more critical and can produce heart failure within weeks of birth. These emergencies require immediate surgical intervention. To further identify the presence of a coarctation defect, you must assess the patient for the presence of pulse equality in the upper and lower extremities. While a child is lying supine, the right radial and femoral pulses are palpated concurrently. The pulses in both areas should be felt simultaneously without delay. There should be no absence or weakness in the femoral pulses compared with the radial or brachial pulse. Another method to evaluate for the presence of a significant coarctation is to obtain blood pressures in the right arm and either leg. If the correct cuff size is used for each extremity and the child is demonstrating a similar behavior during both measurements (not crying for either reading), the pressures should be fairly equal, with the systolic pressure in the lower extremity reading slightly higher than that in the upper extremity. If the systolic pressure reading in the right upper extremity is 10 mmHg higher than that in the lower extremity, this is an indicator of potential CoAo and requires further evaluation. The exact location of the coarctation can vary but is rarely before the right subclavian branch off of the aorta. This is why using the right arm and any leg for blood pressure comparison is effective. ● What is a position to have a child with Tetralogy of Fallot (TOF) go into if they show signs of respiratory distress/altered oxygenation? Why does this help? Occasionally, the area below the pulmonary valve may spasm, thereby increasing the resistance to flow through this area even more. This will cause a greater than usual amount of blood to shunt from right to left across the VSD, and the child will be more deoxygenated. This is termed a hypercyanotic spell, or a “tet spell.” The exact etiology of these episodes is unclear, although a number of mechanisms have been proposed, including increased infundibular contractility, peripheral vasodilatation, hyperventilation, and stimulation of right ventricular mechanoreceptors. During a spell, the child becomes distressed and irritable, possibly without reason. This period of lower saturation is temporary and can be managed by the family by soothing the child if he or she is upset and bringing the child’s knees tightly to the chest in an effort to increase systemic vascular resistance. This increase in the pressure on the left side of the heart (the systemic side) will help force blood back through the pulmonic valve, thereby oxygenating more blood. ● What are teaching points/assessments/nursing cares for post-cardiac catheterization? pp. 1155-1156 Once the catheterization is completed and the access catheters are removed, the child is at risk for bleeding from the insertion site. Children typically remain supine with their legs straight for 2 to 4 hours after the procedure to ensure hemostasis at the site. If the access points were in the neck or arm, the activity restrictions will be less. It is imperative that you understand the child’s underlying cardiac anatomy and physiology as well as the purpose of the catheterization before the child returns from the procedure. Recovery of a child after a catheterization must include monitoring of the respiratory status including the airway, rate, and depth of respirations as well as monitoring for the hemodynamic effects of sedative agents and the catheterization process itself. Children will have frequent vital signs initially that will include heart rate, rhythm, respiratory rate, oxygen saturation, blood pressure, and temperature. With each set of vital signs, distal perfusion to the effected extremity should be included. Oxygen may be continued for a period of time after the procedure as the child recovers from the sedation or anesthesia. Once the child has been observed and is deemed stable, oxygen may be weaned off as long as oxygen saturations remain normal for the child. The child will have activity restrictions upon discharge. They will typically need to miss a day or two of school while the leg site continues to heal. Depending on the procedure performed, they may be restricted from physical activities for several months after device closure of a septal defect POST PROCEDURE NURSING ACTIONS: Provide for continuous cardiac monitoring and oxygen saturation to assess for bradycardia, dysrhythmias, hypotension, and hypoxemia. Assess heart and respiratory rate for 1 full minute. Assess pulses for equality and symmetry. Assess temperature and color of affected extremity. A cool extremity with skin that blanches can indicate arterial obstruction. Assess insertion site (femoral or antecubital area) for bleeding or hematoma. Maintain clean dressing. Prevent bleeding by maintaining the affected extremity in a straight position for 4 to 8 hr. Monitor I&O for adequate urine output, hypovolemia, or dehydration. Monitor for hypoglycemia. IV fluids with dextrose can be necessary. Encourage oral intake, starting with clear liquids. Encourage the child to void to promote excretion of the contrast medium 8 (Chp 16-21, 37): Prioritized interventions for GI, Immune, Infectious, Hematological, Sensory, Neuro, Musculoskeletal Disorders Note: The chapters addressing these topics are Chapters 42-45, 49, 51 ● In illness, when are antibiotics used, and when are they not used? Antibiotics DO NOT work on viruses. Continue antibiotics for the entire treatment or the bacteria will come back stronger? ● What are priority questions to ask in obtaining a health history on a child presenting with illness? ask about immunizations?? ● What are some teaching points for parents of an immunocompromised child? Caution parents, while children are receiving chemotherapy, not to give them nonsteroidal anti-inflammatory drugs as they may interfere with blood coagulation, a problem that may already be present because of lowered thrombocyte levels. Instead, suggest they use acetaminophen (Tylenol) to relieve a headache or to reduce fever and ensure they inform their oncology team of fever because infection in a child receiving cancer treatment may be life-threatening and is considered an emergency while immunocompromised. A parent who wants to give a child vitamins should check with their child’s primary healthcare provider to be certain the vitamin preparation will not interfere with a chemotherapeutic agent. Administration of a vitamin that contains folic acid, for example, could interfere with the effectiveness of methotrexate, a folic acid antagonist. A child receiving chemotherapy is particularly susceptible to contracting an infection and thus should be kept away from people with known infections. Zoster immune globulin may be administered if the child has not been immunized against varicella and is exposed to chickenpox during chemotherapy. Caution parents that live-virus vaccines should not be given during chemotherapy because, if the child’s immune mechanism is deficient, these vaccines could cause widespread viral disease. Non-live vaccines are also not given while receiving chemotherapy since the immune system cannot mount the response necessary to create immunity. Do not administer live virus vaccines (varicella or MMR) to a child who is severely immunocompromised, pregnant, or has received treatment that provide acquired passive immunity (blood products) within 3 months ● When would bronchoscopy be used? What are important assessments/cares surrounding this procedure? p. 1035 Bronchoscopy is the direct visualization of the larynx, trachea, and bronchi through a lit, flexible, fiberoptic tube (i.e., a bronchofiberscope) that is passed through the naris or trachea. The procedure is used with children who have aspirated a foreign object, to instill certain medications, or to take culture and or biopsy specimens. Typically, the throat is sprayed with a local pharyngeal anesthetic to numb the area. Moderate sedation is then administered, and continuous monitoring of vital signs is standard care. Different types of bronchoscopes are used depending on the age of the child and/or the size of the endotracheal tube being used. Procedural complications are not common but may include compromise to the airway such as hemorrhage, pneumothorax and airway edema. After the procedure, continue to assess the child’s respiratory function and airway patency. Post Procedure complications may include bronchospasm, stridor, desaturation, or respiratory distress. Observe children carefully the first time they drink after the procedure to assess that their gag reflex is intact and they do not choke. ● What’s important to know about stool specimen collection? p. 1040 Stool specimens are frequently obtained to be analyzed for blood, bacterial or viral infections, or ova and parasites. Ask children who are toilet trained to use a potty seat or to place a collector cap device on a toilet. Transfer the specimen to a laboratory collection cup using tongue depressor blades. To obtain a specimen from a child who is not toilet trained, scrape stool from a diaper using tongue depressor blades and place it in a stool collection cup. Some stool specimens need a preservative added to the container. If it is important to keep urine from contaminating the stool specimen, place a separate urine collector bag on the infant. Ask an older child to void first into the toilet and then defecate into the potty seat or collection device. Specimens should be sent to the laboratory promptly so they do not dry and have to be collected a second time because most children need at least 24 more hours to produce a stool specimen. If the stool specimen is for ova and parasites, do not refrigerate it because refrigeration destroys the organisms to be analyzed. ● What are signs of anaphylaxis and what are treatments for anaphylactic shock? p. 1184-1186 Symptoms of anaphylaxis may include: -Breathing: wheezing, shortness of breath, throat tightness, cough, hoarse voice, chest pain/tightness, trouble swallowing, itchy mouth/throat, nasal stuffiness/congestion -Circulation: pale/blue color, low pulse, dizziness, light-headedness/passing out, low blood pressure, shock, loss of consciousness -Skin: hives, swelling, itch, warmth, redness, rash -Stomach: nausea, pain/cramps, vomiting, diarrhea -Other: anxiety, feeling of impending doom, itchy/red/watery eyes, headache, cramping of the uterus Anaphylaxis is a true emergency, so fast interventions are necessary. • Administer aqueous epinephrine (Adrenalin) 1:1,000 intramuscularly at a dosage of 0.01 mg/kg of body weight up to 0.3 mg. This relieves laryngeal edema and severe bronchospasm by widening the airway. • Initiate 911 emergency or notify the cardiac arrest team because both respiratory and cardiac arrest may occur. • If hypoxia is present, administer oxygen by mask or nasal cannula. • Anticipate the need for an intravenous (IV) fluid line as a route for a vasopressor such as dopamine and fluid to help restore blood pressure. • If an insect sting was the cause of the condition, a tourniquet, applied above the site of the bite, may be prescribed to limit absorption of the insect venom into the bloodstream. • Anticipate use of a nebulized bronchodilator such as albuterol to halt wheezing or diphenhydramine (Benadryl) intramuscularly or IV if urticaria (itching and swelling) is present. • If the child is experiencing seizures, turn the child onto his or her side and prepare to administer an antiseizure medication such as phenobarbital or diazepam. • A corticosteroid may be administered as a second-line drug. This does not act immediately but does reduce inflammation. IV methylprednisolone is a typical drug given. • Keep the child and family members calm; anxiety adds to bronchospasm and decreases breathing ability. ● What is atopic dermatitis and what are therapeutic managements for it? pp. 1189-1191 Atopic dermatitis (AD) is a type of eczema (eczema describes a category of integumentary disorders, not a specific disorder with a determined etiology) that is characterized by pruritus and associated with a history of allergies that are of an inherited tendency (atopy). Classifications of atopic dermatitis are based on the child’s age, how the lesions are distributed, and the appearance of the lesions. AD cannot be cured but can be well- controlled. Keep skin hydrated with tepid baths (with/without mild soap or emulsifying oil), then apply an emollient within 3 min of bathing. Two or three baths may be given daily with one prior to bedtime. After bathing, pat, do not rub, skin. Dress the child in cotton clothing. Avoid wool and synthetic fabrics. Avoid excessive heat and perspiration, which increases itching. Avoid irritants (bubble baths, soaps, perfumes, fabric softeners). Provide support to the child and family. Wash skin folds and genital area frequently with water. Assist in identifying causative agent. Keep client’s nail short and filed smooth to eliminate sharp edges. ● What personal protective equipment (PPE) is needed for various infection control precautions? p. 1204 Standard and Transmission-Based Precautions for Infection Control To decrease the transmission of infectious agents in the healthcare setting: 1. Wash hands for at least 20 seconds immediately with a non- antimicrobial soap and water or alcohol-based hand sanitizers before and after examining patients and after any contact with blood, body fluids, excretions, secretions, and contaminated items despite the use of gloves. Soap and water is always used if the hands are visibly dirty or contaminated. 2. Wear clean, nonsterile gloves anytime contact with blood, body fluids, mucous membranes, or broken skin is likely. Hand hygiene should be done before and after glove use. Change gloves between tasks or procedures on the same patient. Before going to another patient, remove gloves, wash hands, and then put on new gloves. 3. Wear a mask, protective eyewear, gowns, and face shields during any patient care activity when splashes or sprays of body fluids, excretions, secretions, or blood are likely. Remove the soiled gown and wash hands as soon as possible. Remove the gown and gloves in the room of the patient before moving to the next patient. 4. Make sure contaminated nondisposable equipment is not reused with another patient until it has been cleaned, disinfected, and sterilized properly. Do not recap needles. Dispose of nonreusable needles, syringes, and other sharp patient care instruments in puncture-resistant containers. 5. Ensure housekeeping routinely clean and disinfect frequently touched surfaces including beds, bed rails, examination tables, and bedside tables. 6. Do not touch linens soiled with blood or body fluids with bare hands. Use plastic bags to transport soiled linen. 7. Place a patient whose blood or body fluids are likely to contaminate surfaces or other patients in an isolation room or area. 8. Minimize the use of invasive procedures to avoid the potential for injury and accidental exposure. Use oral rather than injectable medications whenever possible. 9. When a specific diagnosis is made, find out how the disease is transmitted. Use precautions according to the transmission risk. AIRBORNE PRECAUTIONS Airborne precautions reduce the risk of small-particle organisms being transmitted through the air as microorganisms carried by this route can be carried widely. If airborne transmission is possible: 1. Place the patient in a single-patient isolation room that is not air-conditioned or where air is not circulated to the rest of the healthcare facility. Make sure the room has a door that can be closed. 2. Wear a high-efficiency particulate air (HEPA) or other biosafety mask when in the patient’s room. 3. Limit movement of the patient from the room to other areas. Place a surgical mask on a patient who must be moved. DROPLET PRECAUTIONS Droplet precautions reduce the risk of pathogens being spread through large-particle droplet contact by acts such as coughing, sneezing, and talking or through procedures such as suctioning or bronchoscopy. Large droplets do not remain suspended in the air for long periods and generally travel only short distances, so close proximity is required for the spread of disease. Respiratory viruses, Bordetella pertussis, and patients within the first 24 hours of meningococcal infections or group A streptococcal infections can be transmitted by droplets. If droplet transmission is possible: 1. Place the patient in a single-patient isolation room. 2. Wear a HEPA or other biosafety mask when caring for the patient. 3. Limit movement of the patient from the room to other areas. If the patient must be moved, place a surgical mask on the patient. CONTACT PRECAUTIONS Contact precautions reduce the risk of transmission of pathogens by direct contact such as skin-to-skin contact (shaking hands) or indirect contact through an intermediate object such as a comb or soiled dressing. If contact transmission is possible: 1. Place the patient in an isolation room and limit access. 2. Wear gloves during contact with the patient and with infectious body fluids or contaminated items. 3. Wear a disposable gown when in the patient’s room. 4. Limit movement of the patient from the isolation room to other areas. 5. Avoid sharing equipment between patients. Designate equipment for each patient if supplies allow. If sharing equipment is unavoidable, clean and disinfect it before use with the next patient. ● What are important teaching points for iron supplementation for iron-deficiency anemia? pp. 1240-1242 Give 1 hr before or 2 hr after milk, tea, or antacid to prevent decreased absorption. Gastrointestinal (GI) upset (diarrhea, constipation, nausea) is common at the start of therapy. These will decrease over time. If tolerated, administer iron supplements on an empty stomach. Give with meals and start with reduced dose and gradually increase if GI distress occurs. Give with vitamin C to increase absorption. Use a straw with liquid preparation to prevent staining of teeth. Use a Z-track into deep muscle for parenteral injections. Do not massage after injection. Nursing Implications: • Instruct parents to administer the drug on an empty stomach with water to enhance absorption. If this causes gastrointestinal irritation, administer it after meals. Avoid giving it with milk or tea because these interfere with absorption. • If the liquid preparation is ordered, advise parents to mix it with water or juice to mask the taste. Have the child drink the medication through a straw to avoid staining the teeth. • Remember that iron is absorbed best in the presence of an acid. Suggest parents give the iron with a citrus juice such as orange juice to help absorption. Some children may be prescribed vitamin C to take concurrently to increase absorption. • Inform the child and parents that iron may turn stools black. • Encourage parents to include high-fiber foods in the child’s diet to minimize the risk of constipation. • Reinforce the need for thorough brushing of teeth to prevent staining. • Remind parents about the need for follow-up blood studies to evaluate the effectiveness of the drug. CLIENT EDUCATION: Expect stools to turn a tarry green color if dose is adequate. Brush teeth after oral dose to minimize or prevent staining. ● What are important interventions for a child in sickle cell crisis ?The child in a sickle-cell crisis has three primary needs: pain relief, adequate hydration, and oxygenation to prevent further sickling and halt the crisis. Bed rest: reduces the need for oxygen in body cells. Administer prescribed analgesic as needed. Administer oxygen by nasal prongs to keep oxygen saturation above 95% or as prescribed.Administer medications to initiate red blood cell (RBC) production as prescribed such as folic acid and hydroxyurea; Begin oral rehydration or intravenous (IV) therapy as prescribed. Restoring hydration reduces sickle-cell clotting ● What are ways to decrease risk for a crisis in a child with sickle cell anemia (SCA)?pp. 1243-1248, especially 1247-1248 Between crises, parents need to focus care on preventing recurring crises. Although the hemoglobin level of children may remain as low as 6 to 9 g/100 ml, children adjust well to this chronic state. Caution parents that children who receive frequent blood transfusions should not be given supplementary iron or iron-fortified formula or vitamins because they may receive too much iron; high levels of excess iron are deposited in body tissues (hemochromatosis) to a point of staining body tissue or being incorporated into body tissue with fibrotic scarring (hemosiderosis). Oral folic acid may be prescribed to help rebuild hemolyzed RBCs. They need to monitor urine output and may be asked to test urine for specific gravity and hematuria to detect the extent or presence of kidney damage occurring from minor infarcts. Some children who have had kidney infarcts and a lessened ability to concentrate urine have chronic nocturnal enuresis (bed-wetting). Be certain that children receive childhood immunizations so they are not vulnerable to common childhood infections such as measles or pertussis and receive meningococcal, pneumococcal, and Hib vaccines to prevent those specific infections. If children are prescribed oral penicillin as prophylaxis against infection, help the parents determine a method to remember or remind conscientious administration of this. Caution parents to bring their child to a healthcare facility at the first indication of infection.Children should attend regular school and should be allowed to participate in all school activities except contact sports (such as football), which could result in rupture of an enlarged spleen or liver. Long-distance running is also inadvisable because it can lead to dehydration. During the summer, parents need to offer the child frequent drinks to prevent dehydration.Caution parents that even for a simple operation such as tooth extraction, they must alert healthcare personnel about their child’s condition. What are signs of increased intracranial pressure? What are early signs? What are signs of increasing pressure? What vital sign changes will occur? p. 1384 Because symptoms are subtle at first, the initial signs children may show are headache, irritability, or restlessness. Growing pressure on the brainstem, which controls respiration and cardiac activity, soon causes pulse and respiration rates to slow. Compression of cranial vessels leads to a compensatory increase in blood pressure (or pulse pressure, the gap between the systolic and diastolic blood pressures). Pressure on the hypothalamus, the temperature-regulating center of the body, causes an increase in body temperature. An older child may be able to report symptoms such as diplopia (double vision). On funduscopic examination, papilledema may be detected. Compare a new assessment against all recordings taken in the last 24 hours so a progressive change can be detected. Increased head circumference- An increase >2 cm per month in first 3 months of life, >1 cm per month in the second 3 months, and >0.5 cm per month for the next 6 months. Fontanelle changes- Anterior fontanelle tense and bulging; closing late; Vomiting Occurring in the absence of nausea, on awakening in morning or after nap; possibly projectile. Eye changes -Diplopia (double vision) from pressure on abducens nerves; white of sclera evident over pupil (setting sun sign); limited visual fields, papilledema. Vital sign changes- Elevated temperature and blood pressure; decreased pulse and respiration rates. Pain Headache, often present on awakening and standing; increasing with straining at stool (Valsalva maneuver) or holding breath. Mentation Irritability, altered consciousness such as sleepiness. ● What is cerebral palsy (CP)? pp. 1388-1389; Cerebral palsy (CP) is a group of nonprogressive disorders of upper motor neuron impairment that result in motor dysfunction. Affected children also may have speech or ocular difficulties, seizures, cognitive challenges, or hyperactivity. Muscle spasticity can lead to orthopedic or gait difficulties. CP is caused by abnormal brain development or damage to the developing brain, leading to cell destruction of the motor tracts. Nutritional deficiencies, drug use, and maternal infections such as cytomegalovirus or toxoplasmosis, as well as direct birth injury, may also contribute to the cause. Regarding the spastic type of CP, what newborn reflexes persist? Spasticity is excessive tone in the voluntary muscles that results from loss of upper motor neurons. A child with spastic CP has hypertonic muscles, abnormal clonus, exaggeration of deep tendon reflexes, abnormal reflexes such as a positive Babinski reflex, and continuation of neonatal reflexes, such as the tonic neck reflex, well past the age at which these usually disappear. If infants with CP are held in a ventral suspension position, they arch their backs and extend their arms and legs abnormally. They fail to demonstrate a parachute reflex if lowered suddenly and tend to assume a “scissors gait” because tight adductor thigh muscles cause their legs to cross when held upright. This involvement may be so severe that it leads to a subluxated hip. By school age, tightening of the heel cord can become so severe that children walk on their toes, unable to stretch their heel to touch the ground ● https://www.cerebralpalsy.org/about-cerebral-palsy/sign-and-symptoms#:~:text=Hyperreflexia%20are%20excessive%20reflex %20responses,abnormal%20development%2C%20including%20Cerebral%20Palsy. ● What are assessment findings in a child with meningitis? p. 1391 Children usually have had 2 or 3 days of upper respiratory tract infection prior to the development of meningitis. They then grow increasingly irritable because of an intense headache. They experience sharp pain when they bend their head forward. In the newborn, symptoms such as poor sucking, weak cry, or lethargy develop. As the disease progresses, signs of meningeal irritability then occur, as evidenced by positive Brudzinski and Kernig signs. Children may hold their back arched and their neck hyperextended (opisthotonos). If third and sixth cranial nerve paralysis occurs, a child will not be able to follow a light through full visual fields. If the fontanelles are open, they bulge upward and feel tense; if they are closed, papilledema may develop. If the meningitis is caused by H. influenzae, the child may develop septic arthritis. If it is caused by Neisseria meningitidis, a papular or purple petechial skin rash may occur. After this beginning of a myriad of general symptoms, sudden cardiovascular shock, seizures, nuchal rigidity, or apnea can occur. Because the infant has open fontanelles, nuchal rigidity appears late and is not as useful a sign for diagnosis as in the older child. As a rule, a child with a high temperature who then has a seizure is assumed to have meningitis until CSF findings prove otherwise. CSF analysis obtained by lumbar puncture confirms the diagnosis. CSF results indicative of meningitis include increased white blood cell and protein levels, increased ICP, and a glucose level less than 60% of blood glucose. ● What are safety measures during a seizure? p. 1399 Remain calm. • Move away furniture or any sharp objects. • Turn your child gently on her side, or on her abdomen with her head turned to the side, to prevent aspiration of unswallowed mouth secretions. • Do not restrain her other than to keep her head turned to the side. Restraining a child could result in injury because of the amount of force necessary. • Do not attempt to place an object between the child’s teeth to prevent tongue biting. Trying to force an object into the mouth could break or loosen teeth. • Be aware that a child having this type of seizure may have some slight cyanosis during the tonic and clonic stages, but these stages are so short that administering oxygen is not needed. • After any seizure, telephone your primary care provider about the seizure so arrangements for any necessary follow-up care can be initiated. • If your child should pass rapidly from one seizure into another (status epilepticus), she may need supplemental oxygen or medicine to stop the seizure. If this happens, telephone your emergency medical service number (911). ● Review pp. 1396-1397 re: seizure types. Partial seizures originate from a specific brain area. A typical partial seizure with motor signs begins in the fingers and spreads to the wrist, arm, and face in a clonic contraction. If the movement remains localized, there will be no loss of consciousness. If the spread is extensive, the seizure can cross the midline and become generalized and, at that point, is impossible to differentiate from a full generalized tonic–clonic seizure. This makes it important, therefore, to observe children carefully as a seizure begins to distinguish whether it began with local signs such as numbness, tingling, paresthesia, or pain all associated with one brain area. Documenting the spread can help localize the spot in the brain that first initiated the abnormal electrical discharge or be instrumental in detecting the location of a rapidly growing brain tumor. Typical tonic–clonic seizures (formerly termed grand mal seizures) are generalized seizures usually consisting of three stages: a prodromal period of hours or days or an aura, or warning, immediately before the seizure that a seizure is about to occur; a tonic–clonic stage; and, finally, a postictal stage. The prodromal period may consist of drowsiness, dizziness, malaise, lack of coordination, or tension. The next phase is the tonic stage. All muscles of the body contract, extremities stiffen, the face distorts, air is pushed through the glottis from contraction of the chest muscles to produce a guttural cry, and the child falls to the ground. Although this phase lasts only about 20 seconds because the respiratory muscles remain contracted during this time, the child may experience hypoxia and begin to appear cyanotic. Contraction of the throat prevents swallowing, so saliva collects in the mouth. A few children bite their tongue when the jaws contract and thus have bleeding from their mouth. Clonic stage, in which muscles of the body rapidly contract and relax, producing quick, jerky motions. The child may blow bubbles from foamy or bloody saliva and will be incontinent of stool and urine. This phase usually lasts 20 to 30 seconds.Following this tonic–clonic period, the child falls into a sound sleep, the postictal period. He or she will sleep soundly for 1 to 4 hours rousing only to painful stimuli. When children awake, they often experience a severe headache. They have no memory of the seizure.What are behaviors for an absence seizure?Absence seizures are one form of generalized seizures, consist of a staring spell that lasts for a few seconds. A child might be reciting in class, for example, when he or she pauses and stares for 1 to 5 seconds and then continues the recitation as if he or she is unaware time has passed. Rhythmic blinking and twitching of the mouth or an extremity may accompany the staring. As many as 100 seizures can occur during a day. ● What would be signs of child/family coping/transition with cares for a spinal cord injury. p. 1406-As soon as possible, children should be introduced to self-help methods for activities of daily living. You may need to encourage parents to allow a child to become as self- sufficient as possible or not to take over complete care. The child may well outlive them and will someday need to be able to function as independently as possible without them. The second recovery phase is the time for parents and children to begin thinking about what this degree of disability will mean to them as a family and to face what adjustments they will need to make. Children and parents typically react to the initial diagnosis with grief. They may still be in denial or shock when the second phase begins. With no sudden miracle cure in sight, they may begin to move through stages of anger, bargaining, depression, and then acceptance (the injury happened; we must go on from this point). They need assistance and support to work through all of these feelings, however. Both the parents and the child may need counseling to reach acceptance. ● What are important teaching points for family when a child with epilepsy is taking valproate (Depakene)/valproic acid? Review the “How should this medicine be used?”: https://medlineplus.gov/druginfo/meds/a682412.html:Take valproic acid at around the same time(s) every day. Take valproic acid with food to help prevent the medication from upsetting your stomach. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take valproic acid exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor. -Swallow the regular capsules, delayed-release capsule, and extended-release tablets whole; do not split, chew, or crush them. -You can swallow the sprinkle capsules whole, or you can open the capsules and sprinkle the beads they contain on a teaspoonful of soft food, such as applesauce or pudding. Swallow the mixture of food and medication beads right after you prepare it. Be careful not to chew the beads. Do not store unused mixtures of food and medication. -Do not mix the syrup into any carbonated drink. -Divalproex sodium, valproate sodium, and valproic acid products are absorbed by the body in different ways and cannot be substituted for one another. If you need to switch from one product to another, your doctor may need to adjust your dose. Valproic acid may help to control your condition but will not cure it. Continue to take valproic acid even if you feel well. Do not stop taking valproic acid without talking to your doctor, even if you experience side effects such as unusual changes in behavior or mood or if you find out that you are pregnant. If you suddenly stop taking valproic acid, you may experience a severe, long-lasting and possibly life-threatening seizure. Your doctor will probably decrease your dose gradually. ● What assessments should be performed after casting is done for a fracture? What are teaching points for cast care at home? p. 1438-1439 If an extremity has been casted, keep it elevated by a pillow to prevent edema. Check circulation frequently, such as every 15 minutes during the first hour, hourly for the next 4 hours, and then every 4 hours throughout the first day. Assess for color, warmth, presence of pedal or radial pulses, and sensations of numbness or tingling. Signs of impaired neurovascular function include pallor (including blueness or coldness of the distal part), pulselessness, pain in the casted part, paresthesia (numbness or tingling in the part, as if it were “asleep”), and paralysis. Children younger than 6 or 7 years of age have difficulty describing paresthesia; however, they may whine or cry with the discomfort of the sensation. Edema that does not improve with elevation is also an important sign. Any of these symptoms requires immediate attention because neurovascular impairment can lead to nerve ischemia and destruction, possibly causing permanent paralysis of an extremity.Preventing the flow of urine under the edges of a cast can be a problem with full-body or high-leg casts in non–toilet-trained children. If a cast surrounds the genital area, cover the edges with plastic or waterproof material to help keep it dry. Keeping children in a semi-Fowler position by using pillows or raising the head of the bed helps to direct urine and feces downward and away from the cast. Because a cast is heavy, infants tend to slip down in bed a great deal, so they need frequent repositioning to remain in this raised position. ● If young children have a body cast, make certain they have a bib or cover over the top edge of their cast so crumbs or fluids do not spill inside. Choose toys carefully so small parts cannot drop inside. A piece of food inside a cast will mold and macerate the skin; a small part of a toy could cause irritation and a pressure ulcer. If food or fluid is spilled on the outside of the cast, the cast can be cleaned with a damp cloth. If a child has an upper extremity cast, be certain the parents understand how to position the extremity properly, such as with a sling. If the cast is on a lower extremity, be certain parents and the child understand the amount of weight bearing allowed on the affected extremity and how to use crutches safely, if prescribed. Handling a child in a large cast can seem so overwhelming for parents that they do not see how they will be able to care for their child at home. Assure them the child is quite comfortable in the cast despite its awkward, constricting appearance. Role model moving the child to show them that it is not an impossible task. Be sure to caution them that if an abduction bar is used with a cast, it must never be used as a handle for lifting. Such use can break the bar from the cast or weaken its support. Parents need to use good body mechanics (lift with the thighs, not the back) when turning or positioning the child in a full-body cast. They may appreciate suggestions on ways to move the child from room to room, such as using a toy wagon with a flat board on top or using a skateboard for children to propel themselves forward. Point out that all children thrive on being touched. Children in large body casts need their head and arms stroked (or any areas of the body that are not covered by the cast) so they receive this. Demonstrate how even a child in a large hip spica cast can be held, cuddled, and supported for feeding. Many children report a sensation of itching inside a cast at about the end of the first week. If the area is immediately under the edge of the cast, the itching is probably the result of dry skin caused by the drying effect of the cast. Reaching a hand under the edge of the cast and massaging the area usually relieves the itching. Applying hand lotion may relieve the dryness. If the area is unreachable, blowing cool air through the cast with a fan or a hair dryer set on cool air may relieve the uncomfortable feeling. Caution both the child and parents not to use implements such as a coat hanger or knitting needle to scratch the area. These can injure the skin, causing an infection under the cast ● When would skeletal traction be used and what are some creative nursing interventions to help? pp. 1442-1443 If longer period of traction or greater strength of traction pull is needed. Cotton gauze squares Cleanse with hydrogen peroxide Use sterile technique Observe pin site for drainage ● What is Legg-Calve-Perthes Disease? What are treatments based on age? pp. 1446-1447 Childhood disorder of the hip that causes avascular necrosis ● What is osteomyelitis and how is it treated? pp. 1447-1448 Acute osteomyelitis is often the result of a hematogenous spread of bacteria such as Staphylococcus aureus in older children and by Streptococcus pyogenes in younger children. Children with sickle-cell anemia have a special susceptibility to Salmonella invasion in long bones. The infection may occur after extensive impetigo, burns, or something as simple as a furuncle (skin abscess) when the infectious organism is then carried through the blood supply to the bone. It also may occur directly by outside invasion from a penetrating wound, open fracture, or contamination during surgery (bone infection) Malaise/ lethargy/ irritability Fever High HR Warmth, edema, pain TX. Limit weight bearing Bedrest Immobilization IV antibiotic Oxacillin ● What are treatments of a fractured femur? p. 1462 Surgery to insert intramedullary rod ● What signs will you see if infection happens post-surgery? pp. 1447-1448. (S/S of osteomyelitis) Malaise Fever Irritability Sharp pain Warm skin edema OB/Newborn ● What does GTPAL mean? “G”- Gravida - # of times a woman has been pregnant, “T”- Term babies - # of times women carried pregnancy to at least 37 weeks and delivered; “P” - Preterm - # of deliveries before 37 weeks gestation; “A” - Abortion - # of abortions, whether elective or spontaneous, before 20 weeks; “L” - Living children - # of live births. In a case scenario, how will you number a woman’s pregnancy/birth history? ● How is a due date calculated by Naegele’s rule? Add 7 days to the last day of your last menstrual period and then subtract 3 months, remember to change year if need be ● If Leopold’s maneuvers help us determine how baby laying/presenting so we know where the head and back are to monitor baby’s heart tones best, what part of the abdomen would the best place be to hear if the baby is vertex versus breech? Left lower quadrant ● What are the differences between placenta previa and placental abruption? Placenta Previa- when placenta covers the cervix= bright red blood with no pain, Placental abruption- placenta detaches from the uterus = dark red blood with severe pain. How will each manifest/what signs will you notice with each? ● What are the assessment criteria for each component of the Apgar score? pp. 436-437 Appearance. skin color. blue, pale. Pink and blue. pink Pulse. absent. < 100. >100 Grimacing. floppy. Minimal response. Prompt response Activity… absent. Flexed arms and legs. Active Respiration… absent. / slow and irregular. vigorous cry ● If the purpose of the infant’s fontanelle (3-4 cm anterior opening) and cranial bones is to be movable for the birthing process, when does the anterior fontanelle close? p. 445 closes at 12-18 months of age ● What is the Moro reflex? Startle reflex. Loud noise or jamming the bassinet. Hold the baby in supine, allow head to drop back. In response to this backward head movement, the baby will first extend the arms and legs, swing the arms into embrace position and pull up legs against the abdomen. How is it elicited and how long before it fades (as neuromuscular maturity increases)? p. 434 Should go away by 4-5 months of age ● If a mother is using a substance (either Rx or illicit), what are the risks to baby? Withdrawal. Besides the need to assess toxicology on mom and baby, what other assessments/cares are necessary? pp. 584, 709-710. urinology o Here’s an interesting link about urine testing for drugs in pregnancy (and possible legal consequences). Urinalysis for toxicology… https://womensmentalhealth.org/posts/how-do-we-respond-to-mothers-who-use-drugs-during-pregnancy/ ● What are risk factors for postpartum hemorrhage? Think of reasons that make the uterus have to work harder to contract back down to size. Large baby Multiple babies Long labor Induction labor Use of Pitocin ● What are signs of respiratory distress in a newborn? Intercostal retractions Nares dilation Expiratory grunt Xiphoidal retraction Chest movement (seesaw respiration). Is acrocyanosis a normal finding? YES. Why? Because of premature peripheral circulation. ● Pitocin (oxytocin) can be used to induce (or augment) labor. If too much is given, little rest time between contractions (we like at least 1 minute) means baby will have less circulation since a contraction really slows blood flow through the uterus. It’s like baby is holding their breath during the contraction. Think back to your discussion on Pitocin. What are safe ways to use this high-risk medication? pp. 603-604 (Note: Hyperstimulation is now called tachysystole, and in real life, laying to the right or left side helps uteroplacental circulation/prevent supine hypotension…not just the left side). Use infusion pump Regulate infusion rate Monitor frequency pulse and BP: watch for hypotension: discontinue Monitor FHR Monitor I/O Prepare woman for birth 9 (Chp 46, 48, 53): Renal, Urinary, Reproductive, Endocrine, Metabolic Disorders, Chronic/Terminal Illness Note: The topic of reproductive chapter 47 was not in the assigned reading. ● What are the Kubler-Ross stages of grief and examples of each? pg 1583 Denial- difficulty realizing what has occurred. “How could this have happened?” Anger- feeling of injustice of being singled out this way. “it’s isn’t fair this is happening” Bargaining-an attempt to work out a deal. “if my child gets well, i will devote the rest of my life to doing good” Depression- the feeling of sadness and fatigued. ex. Parents develop low self-confidence, self confidence in their parenting abilities because they could not prevent this from happening. Acceptance-finally coming to terms with the reality of the situation. “yes this is happening and it's all right that it is happening” ● What are treatments/recommendations for the treatment of UTIs? pg 1304 o Tx would be to utilize broad-spectrum antibiotics(Bactrim, amoxicillin, nitrofurantoin), hydration,frequent use of bathroom(do not hold urine in ) Proper wiping(from front to back ladies especially), cotton underwear(ladies), no bubble baths. Urination after sex. Take all of the prescribed medication for UTI treatment. ● What is a voiding cystourethrogram (VCUG) and how is it performed? pg 1296 o a study of the lower urinary tract, reveals the structure of the urethra and bladder and the presence of reflux into the ureters. After bladder catheterization, a radiopaque dye is injected into the bladder, and the catheter is then removed. The child is asked to void into a bedpan while serial X-ray films are taken. o VCUG should not be performed if there is a case of an active UTI. This creates danger of the radiopaque material injected into the bladder could spread bacteria from the bladder up the ureters and up to the kidneys (pyelonephritis). ● Regarding post-op kidney transplant care, what are important teaching points? (p. 1317-1319) found info on pg 1318 o sterile environment as much as possible due to them being on immunosuppressive therapy drugs (cyclosporine, azathioprine, Methyprednisolone) o hemodialysis( until kidney can fully function) ● What is the etiology (cause) of acute glomerulonephritis? pg1308 o Streptococcal infection. typically occur w/ 5-10 y/o children who just recovered from or has a hx of respiratory infection, impetigo(all caused by streptococcal infxn) ● What is the therapeutic management for growth hormone (GH) deficiency? pg 1350 o admin of IM recombinant human growth hormone, typically given at bedtime(time of day in which its growth hormone peaks). some children may need suppression of luteinizing hormone-releasinghormone releasing hormone LHRH or gonadotropin- releasing hormone GnRH to delay epiphyseal closure. ● What are comfort measures (pharmacological/non-pharmacological) for dysmenorrhea(painful periods)? p. 1329-1330 ▪ Pharm o NSAID(ibuprofen, Advil, Motrin) do not take on an empty stomach. o oral contraceptives. Can also use long-acting oral contraceptives that only allow periods q 3 months. o eval for possible endometriosis. o Yoga, ● What causes “salt-losing form of congenital adrenogenital hyperplasia” and what are the consequences/manifestations? (p. 1357) o blockage of cortisol formation which leads to aldosterone deficiency. Without aldosterone salt is not retained and neither is water. Consequences are vomiting, diarrhea, anorexia, weight loss and extreme dehydration. Untreated= death in 48-72hrs after birth. ● What are manifestations (signs) noted with Cushing syndrome?pg 1357 increased glucOse prOduction(fat accumulation on cheeks, chin, trunk causing mOOn fac, stOcky appearance.) PrOtein wasting→ muscle wasting(thin extremities) OsteopOrOsis, suppressed immune system, vasOcOnstriction→ extreme HTN. Hyperpigmentation(especially On cheeks), abnormal saculinaztaion or feminization(OverprOduction of andrOgen or estrOgen), pOOr wOund healing, purple striae (On hips, abdOmen, thighs), pOlyuria. ● What is the disease process/what manifestations will occur with the onset and progression of Type 1 Diabetes Mellitus prior to diagnosis and management? pg 1359 o Type 1 DM is of idiopathic or autoimmune destruction origin. Destruction of the beta cell in the pancreas→ absOlute insulin deficiency(no insulin prOduction). pg 514 table 20.2 & pg 1359 o Manifestation & onset= equal incidence in boys and girls 1/500 children in the USA. Age of onse 5-7 y/O. Marked weight loss is initial sign, polydipsia, polyphagia, polyuria( bed wetting in previous potty trained child), fatigue, blurred vision, mood changes, electrolyte imbalance, short stature. ● What are risk factors for Type 2 Diabetes? o overweight, family hx, race(African, hispanic, asian, or native indian), has a high fat diet, high carbohydrate diet, sedentary lifestyle. ● What is pathophysiology compared to Type 1 DM? o diminished insulin secretion( some pancreatic islet cells still function, produce small amounts of insulin) as opposed to type 1(no insulin production, islets do not function). Type 2 DM patients do not always need daily insulin, their blood sugar can be managed with diet alone or with insulin and diet combo. ● What are the details of the therapeutic management of diabetes with insulin? pg 1360 o Types of insulin vary based on onset, peak and duration. o Children can be regulated on a variety of insulin programs, but typically receive a combined insulin dose of 0.4 to 0.7 units per kilogram of body weight daily in two divided doses (one before breakfast and one before dinner); adolescents may need as much as 1.2 units per kilogram daily divided into the two doses. The most common mixture of insulin used with children is a combination of an intermediate-acting insulin and a regular insulin, usually in a 2:1 ratio or 0.75 units of the intermediate-acting insulin to 0.33 units regular insulin, and given in the same syringe, although this prescription varies for individual children. The morning dose is two thirds of the total daily dose; the evening dose is the remaining one third. ● How/what types of insulin are used to manage glucose levels and what are techniques for administration? pp. 1360-1366 o always injected SubQ unless in cases of emergencies(given IV), rotate sites or lipodystropy will occur and no sensation will be available here and insulin will no longer be absorbed on this site. Admin insulin at room temp( dec subQ atrophy & increase peak effectiveness.) Preparation Onset Peak Effect Duration of Effect (hr) Lispro (Humalog) Immediate 30 min–1 hr 3–4 Aspart 15 min 30–40 min 3–5 Regular (Humulin-R) 0.5–1.0 hr 2–4 hr 5–7 Lantus 1 hr 5 hr 24 Humulin-N 1–2 hr 4–12 hr 24+ Humulin-L 1–3 hr 6–14 hr 24+ Humulin-U 6 hr 16–18 hr 36+ o injection sites ● Why can hypocalcemia occur in newborns and how will it manifest (what will you see)? p. 1369 o newborn before they begin sucking well. Typically occur in infants who experienced birth anoxia, immature infants (immature parathyroid gland), mom hx of DM (infants will experience hypoglycemia shortly after birth), Also caused by change in either calcium or phosphorus(inverse relationship). o Manifestation- neuromuscular irritability(latent tetany blood Ca < 7.5mg/dl), jitters when held, crying for extended period of time. Trousseau, Pedal spasm( foot extended, toes flex, sole of foot cups.) Chvostek. Without therapy- high pitched, crowning sound on inspiration, respiration may cease. ● What are recommended cares for a child with neutropenia? pg 1511 o minimize contact with family/friends who might have infection. limit large crowds. Wash hands before providing care to child, have child wash hand as well, daily bath or shower, oral hygiene, monitor for candida infxn(moisturize lips to avoid cracks), daily temp, monitor skin for possible s/sx of infxn, stool softeners, high protein diets, avoid raw fruits/veggies. Assess for respiratory tract infxn, monitor for GU infxn, avoid vaccines until the immune system has recovered( ok to give flu vaccine). ● What’s the best way to take a temp? Consider neutropenia, stomatitis…p. 1511 o Best way found is temporal. DO NOT TAKE RECTAL TEMP. Oral temp may be inaccurate due to mouth irritation, nausea, vomiting = not a good way to take temp if this is happening. ● What are ways to prevent skin cancer? pg 1525 & pages in my brain lol o Minimize direct sun exposure, sunscreen, protective clothing, avoid peak sunlight hours. ● What increases risk for skin cancer? 1525-1526 o excessive sun exposure(sunburn). Unprotected sun exposure. Tanning beds/ultraviolet light. o https://www.skincancer.org/risk-factors/sunburn/ 10 (Chp 55): Health Promotion Strategies, Mental and Behavioral Health Disorders, Current Issues in Peds Health Care ● What are topics of education/support for preschool health screening from Healthy People 2020? The mark of a developed nation is the ability to protect the health of its most vulnerable members. This makes both child maltreatment and intimate partner violence national health concerns. Examples of 2020 National Health Goals that specifically address these issues are: • Reduce the rate of maltreatment of children younger than 18 years of age from a baseline of 9.4 per 1,000 to a target level of 8.5 per 1,000. • Reduce the rate of child maltreatment fatalities from a baseline of 2.4 per 100,000 to a target level of 2.2 per 100,000. • Reduce the rate of physical, sexual, and psychological violence by current or former intimate partners. • Reduce stalking by former or present intimate partners. • Reduce abusive sexual conduct and rape (U.S. Department of Health and Human Services, 2010; see www.healthypeople.gov). Nurses can help the nation achieve these goals by educating parents about how to parent more effectively and by identifying children or adults in school or healthcare agency settings who have been maltreated, neglected, or victim of violence. ● What is nursing’s responsibility with suspected abuse? If child maltreatment is suspected, talk with the parents first, without the child, and then interview the child separately to help uncover any inconsistencies in the parents’ explanations. Remember, however, you are not investigating the concern—you are doing an initial screening to assess the need for referral and reporting. Your agency’s patient protective services department will do the actual investigation.Planning must center first on ensuring the safety of the maltreated family member and minimizing the effects of trauma. Second comes reporting the discovery to authorities as nurses are mandated by law to report child maltreatment. ***Mandatory reporters are professionals who are mandated by law to report child maltreatment. Nurses are included in the mandatory category in most states; this means they must report suspected child maltreatment when they identify it. Failure to do so can result in a fine, jail time, or loss of nursing licensure. ● What are car seat safety measures to educate families about per child age?????????????? -Newborns should always be transported in rear facing car seats placed in the back seat;The ideal model has a five-point harness with broad straps, which helps spread the force of a collision over the chest and hips, and a shield, which cushions the head. ● What are STI risk factors for adolescents? only condoms (both male and female) provide protection against sexually transmitted infections (STIs) or HIV—an important concern if a relationship is not a monogamous one. Websites set up by health professionals can be an ideal method for adolescents to learn more about their bodies and safer sex practices because they can do this in a private, nonjudgmental setting Educating adolescents about safer sex practices, including the need for condom use (see Chapter 5) and the importance of health screening for these disorders, is an important nursing responsibility. Pay particular attention to adolescents who do not have a strong family support system because it may be particularly difficult for these youth to receive correct information about preventing STIs (Hudson, 2012). ● What is failure to thrive (FTT)? p. 1567-1568 Failure to thrive is a unique syndrome in which an infant falls below the 5th percentile for weight and height on a standard growth chart or is falling in percentiles on a growth chart. The condition is usually divided into two categories: One where severe loss of weight can be explained because of organic causes, such as cardiac disease, and a second that occurs because of a disturbance in the parent–child relationship, resulting in maternal role insufficiency (a nonorganic cause). Sometimes, both forms combine to play a role in failure to thrive. o What are nursing diagnoses and goals for FTT? Imbalanced nutrition, less than body requirements, related to inadequate intake secondary to emotional deprivation Goals:Child shows interest in bottle feedings; child is able to establish a regular eating pattern; child begins to gain weight. ● What are ways in which physical neglect can occur? pp. 1566-1567 A neglected child may appear unwashed, thin, and malnourished or be dressed inappropriately, such as without mittens, a coat, or shoes in cold weather. In some families, no one has a warm coat to wear or receives enough food because there is no money for these things; that is, different from the family in which parents do have these things, but the children or one particular child does not. Failing to bring a child for medical attention or failing to seek early medical care for an infection are other signs of neglect. Not requiring a child to attend school, deliberately keeping a child out of school without setting up a home school program, or allowing a child to go unsupervised after school may also be interpreted as neglect. Such actions may be willful or they may occur if parents simply do not realize the developmental needs of a child ● What are signs of sexual abuse? p. 1570-1571 Here are some general indications that a child is being sexually maltreated: • The child reports she has had sexual activity with an adult. • The child demonstrates an awareness of sex or a sexual vocabulary beyond her age expectations. • The child participates in sexual expression with dolls. • A girl younger than 15 years of age is pregnant. • A perineal, vaginal, or anal exam reveals inflammation or vaginal tears or anal fissures. • A child younger than 15 years of age has a sexually transmitted infection. • A child has a history of symptoms of increased anxiety such as a sleep disturbance, development of nervous tics, nail biting, or stuttering. • There is a change in school performance, school phobia, or truancy. • The child voices a fear of being left alone with a certain adult. • A child reports vague abdominal pain or demonstrates acting-out behavior. From Module 6: Growth and Development ● What are ways a parent can respond to a child to help them achieve the Erickson’s developmental task of their age? (Infant, toddler) Infant:Developmental task is to form a sense of trust versus mistrust. Child learns to love and be loved. Provide a primary caregiver. Provide experiences that add to security. Toddler: Developmental task is to form a sense of autonomy versus shame. Child learns to be independent and make decisions for self. Provide opportunities for independent decision making, such as choosing own clothes. o How might the nurse incorporate the developmental perceptions into explaining a test or procedure to a preschool-aged child? Use age appropriate language, demonstrate to the child what is going to happen, show pictures ● What growth assessments are done at clinic visits? To assess growth (defined as an increase in physical size, typically measured as height, weight and head circumference), measure and plot height and weight on a standard growth chart for children at all well-child care visits. Measurement of the head circumference is included for children age 2 years and younger. Growth charts are available through the Centers for Disease Control and Prevention (CDC; www.cdc.gov/growthcharts/) and the World Health Organization (WHO; www.who.int/childgrowth/standards). This will aid in determining if the child’s growth is following the predicted pattern. Obtain a developmental health history from both parents (if they are available) and the child (if age-appropriate). Development refers to the progression toward maturity in mental, physical, and social markers of normal development. Observe what specific activities the child can accomplish to establish whether developmental milestones (major markers of normal development) are achieved (Fig. 28.1). Document a 24-hour recall history for nutritional intake, sleep, and a description of school and play behaviors (see Chapter 34). Periodic screening tests such as the Ages & Stages Questionnaires (http://agesandstages.com/) and routine screening, including hearing and vision, should be scheduled following the periodicity schedule of the American Academy of Pediatrics Bits and Pieces ● What are rules for making medical decisions or giving consent with single or divorced parents? p. 45 If there has been a divorce, one parent may have been given legal custody of the children or both parents may share custody. Either way, both parents often participate in decision making. At a time of illness, both may stay with an ill child in the hospital and be eager to receive reports of the child’s progress. Identifying who is the custodial parent is especially important when consent forms for care need to be signed, so be certain this is clearly marked in the child’s healthcare records. ● Have a general understanding of reproduction technology. If there are genetic risks with either the male or female, what are options? p. 145-148 -Alternative or IUI is the instillation of sperm from a masturbatory sample into the female reproductive tract by means of a cannula to aid conception at the time of ovulation (Kop, van Wely, Mol, et al., 2015). The sperm can either be instilled into the cervix (intracervical insemination) or directly into the uterus (IUI) at the time of predicted ovulation. BBT charting, mucus analysis, or urinary test kits for LH can be used to detect the day of ovulation (Hamilton, 2012). -In vitro fertilization (IVF) is most often used for couples who have not been able to conceive because the woman has obstructed or damaged fallopian tubes. It is also used when the man has oligospermia or a very low sperm count. IVF may also be helpful for couples when an absence of cervical mucus prevents sperm from entering the cervix or antisperm antibodies cause immobilization of sperm. In addition, couples with unexplained subfertility of long duration may be helped by IVF. For the procedure, one or more mature oocytes are removed from a woman’s ovary by laparoscopy and fertilized by exposure to sperm in a laboratory. About 40 hours after fertilization, the laboratory-grown fertilized ova (now zygotes) are inserted into a woman’s uterus, where, ideally, one or more of them will implant and grow. -In gamete intrafallopian transfer (GIFT) procedures, ova are obtained from ovaries exactly as in IVF. Instead of waiting for fertilization to occur in the laboratory, however, both ova and sperm are instilled, within a matter of hours, using a laparoscopic technique, into the open end of a patent fallopian tube. Fertilization then occurs in the tube, and the zygote moves to the uterus for implantation. It requires at least one patent fallopian tube; it may be a preferred procedure by some couples because conception occurs in the fallopian tube and so is not contradictory to their religious beliefs. -Surrogate embryo transfer is an assisted reproductive technique for a woman who does not produce ova. For the process, the oocyte is donated by a friend, relative, or an anonymous donor (Check, Wilson, Levine, et al., 2015). The menstrual cycles of the donor and recipient are synchronized by administration of gonadotropic hormones. At the time of ovulation, the donor’s ovum is removed by a transvaginal, ultrasound-guided procedure. The oocyte is then fertilized in the laboratory by the recipient woman’s partner’s sperm (or donor sperm) and placed in the recipient woman’s uterus by embryonic transfer. Once pregnancy occurs, it progresses the same as an unassisted pregnancy. -Adoption is an alternative for subfertile and LGBT couples, those individuals who have genetic-related health conditions or health conditions that would make pregnancy high risk; Child-free living is another option available to both fertile and subfertile couples ● How quickly does a baby grow? p. 782 As a rule, most infants double their birth weight by 4 to 6 months and triple it by 1 year. During the first 6 months, infants typically average a weight gain of 2 lb per month. During the second 6 months, weight gain is approximately 1 lb per month. The average 1-year-old boy weighs 10 kg (22 lb); the average girl weighs 9.5 kg (21 lb). An infant increases in height during the first year by 50%, or grows from the average birth length of 20 in. to about 30 in. ● What are teaching topics for positive ideas to help in decreasing obesity in the school-aged child? p. 882, 1167 The type of weight-reduction program that will probably work best is one that emphasizes long-term lifestyle changes and contains features such as: • An intake of about 1,200 calories a day (no more than 30% as fat), with lifestyle changes such as a structured family meal, eliminating eating or snacking in front of the television, decreasing portion sizes, and eliminating sugar-rich drinks. • An active exercise program, including monitoring and limiting time spent in physical inactivity (e.g., watching television, playing computer and video games, surfing the Internet, texting). • A counseling program to discuss aspects such as self-image and motivation to reduce weight. Total caloric intake should not be reduced too drastically in children because they need calories to form new body tissue for continued growth. Caution children not to try faddish high-protein diets (as most adults should not) because such diets do not supply enough carbohydrates and may produce a heavy renal solute load (the breakdown product of proteins) to the kidneys. It helps if children aim to lose 5 lb over a short time rather than 50 lb over a year. This short-term goal coincides better with the task of developing industry. Nurses must use every opportunity to provide education for children and their families by encouraging them to choose healthy lifestyle behaviors such as: • Consuming low-fat diets • Eliminating sweetened beverages and other sugary foods • Increasing physical activity • Decreasing screen time It is important for these behaviors to be implemented by the entire family. It is also important to note that restricting calories is not a first-line management choice for children because they have significant metabolic needs as they grow. Childhood obesity and its risk factors must be addressed early to prevent premature cardiovascular disease in adulthood. ● When does growth stop of girls/boys? p. 887 The major milestones of physical development in the adolescent period are the onset of puberty at 8 to 12 years of age and the cessation of body growth around 16 to 20 years (Sass & Kaplan, 2013). Between these milestones, physiologic growth and development of adult coordination occur. At first, the gain in physical growth is mostly in weight, leading to the stocky, slightly obese appearance of prepubescence; later comes the thin, gangly appearance of late adolescence. Most girls are 1 to 2 in. (2.4 to 5 cm) taller than boys coming into adolescence but generally stop growing within 3 years from menarche and so are shorter than boys by the end of adolescence. Boys typically grow about 4 to 12 in. (10 to 30 cm) in height and gain about 15 to 65 lb (7 to 30 kg) during their teenage years. Girls grow 2 to 8 in. (5 to 20 cm) in height and gain 15 to 55 lb (7 to 25 kg). Growth stops with closure of the epiphyseal lines of the long bones, which occurs at about 16 or 17 years of age in females and about 18 to 20 years of age in males. ● What are some teaching points for adolescents with interest in being sexually active? p. 901 When discussing sexuality with adolescents, the nurse should avoid assumptions about the gender of the adolescent’s partner. Ask open- ended questions when providing education on health promoting behaviors. This will also help the adolescent feel more open to asking questions. Counseling can assist adolescents improve their perspective and also learn how to say no. For adolescents who agree to have intercourse but who do not really want to, the primary reasons given are peer pressure, curiosity, and affection for their partner. Here are a few common guidelines: • It is your choice whether to participate in sexual relations. Do not be influenced by friends who may be exaggerating stories to impress you or who ask you to do something you do not want to do. When you say no, be firm and clear about your wishes. • There is no 100% method to prevent pregnancy or a sexually transmitted infection (STI) except abstinence. Be direct with a sexual partner in discussing abstinence or reproductive and infection prevention measures. • Sexual relations neither add to nor detract from your physical strength or general wellness. • The mark of an adult sexual relationship is that the activity is pleasurable to both partners. If sexual partners are not interested in your enjoyment as well as their own, you should reconsider the relationship. • There is no “normal” mode of sexual expression. Any activity that is pleasurable to both partners is “normal.” • Learn about safer sex techniques and practice them. ● What are suicide risk factors and warning signs? What interventions can be helpful in preventing suicide? 906-909. Assess at these visits signs of depression such as anorexia, insomnia, excessive fatigue, or weight loss (Gampetro, Wojciechowski, & Amer, 2012). In younger adolescents, depression may be manifested not so much by appearing sad, but by behavior problems such as disobedience, temper tantrums, truancy, and running away. Self-destructive behavior or injury proneness; difficulties in school; acting out with chemicals, alcohol, or sexual promiscuity; or trouble with legal authorities may be further clues. Depressed adolescents find it so hard to be alone that they seek constant activity as a means of escape. Others may withdraw from contact with other people and become completely isolated. Either behavior needs to be detected through assessing activity and interaction levels. Loners or have difficulty expressing their feelings to others and, therefore, do not receive emotional support from friends or family. Others appear to be “perfect” students, so friends or family do not see a need to counsel them. The stress of trying to continually achieve at a high level, however, is the trigger that provokes suicide. LGBT youths appear to have higher levels of suicide than others, reflecting the level of stress they may be experiencing. Assess for LGBTs as well. If another member of a family or a close friend commits suicide, the chance an adolescent will also do so is greater than usual. The anniversary of a family member’s suicide is an especially vulnerable time because wishing to join the dead family member may appear attractive. The following are commonly seen clues: • Giving away prized possessions • Organ donation questions, such as “How do you leave your body to a medical school?” • Sudden, unexplained elevation of mood, which may indicate the individual has reached a decision about the suicide and feels relief • Injury proneness, carelessness, and death wishes • Decrease in verbal communication or a statement such as “This is the last time you will see me” • Withdrawal from peer activities or previously enjoyed events • Previous attempt (80% of all completed suicides have been preceded by a failed attempt) • Preference for art, music, and literature with themes of death • Recent increase in interpersonal conflict with significant others • Running away from home • Recent experience of a friend or famous person committing suicide • Inquiring about the hereafter • Asking for information (supposedly for a friend) about suicide prevention and intervention • Almost any sustained deviation from the normal pattern of behavior. PREVENTING: Crisis intervention for adolescents who are contemplating suicide includes trying to alleviate their pain and depression and counseling them in an effort to help them change their perspective on the value of life. Be aware that establishing expected outcomes with adolescents who are contemplating suicide or who have made an attempt will be difficult because they are often too depressed to come up with alternative solutions to their problems (their goal was to kill themselves, not solve problems). As another measure, try to find out the things in the child’s life that are still viewed as important; build a plan that will help view life as worth living enough to work through difficulties. Show them how no one can change everything, but everyone can make one or two changes that can make a difference. After these small changes are made, a domino effect can be created to change more and more of one’s circumstances. Helping all adolescents learn better problem-solving skills is a prime intervention strategy. Ask “what would happen if” questions such as “Suppose you did fail a course; what would be the worst that could happen?” ● How can nurses support the developmental needs of an ill and/or hospitalized adolescent? pp. 1006-1007 If possible, help adolescents to continue to participate in activities they did before becoming hospitalized to help them feel that their world is not totally changing. Encourage them to maintain self-care activities and good hygiene practices to help preserve self-esteem. Illness can be especially difficult for adolescents also because peer relationships are so important to them and a hospitalization automatically interferes with those. To help avoid feelings of exclusion and hurt, urge them to welcome visitors from their peer group. Suggest electronic communication formats such as texting or emailing as easy ways to keep in contact with friends and maintain relationships with individuals who are important to them while separated from them. Adolescents usually appreciate being hospitalized in a special adolescent unit or at least in a room free of childish decor.Often, adolescents convey a blasé attitude toward procedures (e.g., having an X-ray taken is nothing, surgery is a cinch, a cast change is a snap). Listen carefully to make certain adolescents really feel this way and are not trying to convince themselves that a procedure is harmless. Remember that adolescents are extremely worried about their body image. Explain to them what is going to happen in surgery or in other departments because it is easy to assume from their attitude they know more than they do. ● What are some interventions to help with separation anxiety in a toddler? Pp. 825-826 Most toddlers react best to separation if a regular babysitter is employed or if the day care center has consistent caregivers. It helps if toddlers have fair warning they will have a babysitter. It helps if parents say goodbye firmly, repeat the explanation they will be there when the child wakes in the morning, and then leave. 994-995--When hospitalizations such as elective surgeries are scheduled, advance preparation is possible with programs such as preoperative orientation. The preparations parents make for a child obviously vary depending on the child’s developmental age and experiences. As a rule, therefore, children between 2 and 7 years of age should be told about a scheduled ambulatory or inpatient hospitalization as many days before the procedure as the child’s age in years. For example, a 2-year-old should be informed 2 days before hospitalization; a 4-year-old, 4 days before; and so forth. 1002-1003-Hospitalized children should have one nurse who is “theirs” to minimize the effect of separation from parents (primary care nursing). When possible, young children should have a parent room-in with them when they are in the hospital (Fig. 36.5). Remind parents that it is not uncommon for this age group to go through three different phases: protest, despair, and detachment. Parents often need help in saying goodbye when it is time to leave a child. If the parents of a toddler or preschooler have to leave, urge them first to give a warning they will soon have to go: “I have to leave in a minute to fix dinner for Daddy.” When the time to go has come, the parent should say firmly that it is time to go and then explain the time he or she will return. Time for a preschooler is best measured in terms of events rather than clock hours. “I’ll be back after you’ve eaten supper,” is better than “I’ll be back at seven”; and “after you wake up tomorrow,” is better than 8 AM as these times give the child a concrete event by which to measure time. Like infants, toddlers need someone with them when their parents leave; they like to be held or played with so they know they are not alone. ● When is myringotomy used and how does this impact hearing? pp. 1430-1431- Treatment for otitis media-,normally, the middle ear is an air-filled cavity; air is supplied to it each time the eustachian tube opens with swallowing, yawning, or chewing. If this source of air to the middle ear is closed off due to inflammation or edema of the eustachian tube, the epithelial cells of the middle ear begin to secrete a thin, watery mucus. Over time, the compartment becomes so filled with this and the fluid becomes so thick and tenacious that it appears glue- like. Some children notice a feeling of fullness or the sound of popping or ringing in their ears. There may be a drop in hearing of 20 to 40 dB because of the inability of the ossicles to function effectively. Involvement is usually bilateral. A source of air can be supplied to the middle ear by the insertion of small plastic (Teflon) tubes inserted through the tympanic membrane (tympanostomy). The insertion of such tubes is done by a myringotomy at a point in the tympanic membrane that is not instrumental for hearing, so the tube does not interfere with hearing (Fig. 50.10). Myringotomy tubes can be placed in one or both ears as an ambulatory procedure after the local injection of lidocaine (Xylocaine). Tubes tend to be extruded after 6 to 12 months. For most children, this period is long enough to halt the secretory process of the middle ear. Because the course of the process is long term, the hearing impairment associated with the condition may also be long term. Urge parents to notify the school nurse that their child has compromised hearing because of the middle ear fluid and has myringotomy tubes in place. Children may need to move to the front of the class to mitigate difficulty hearing and encourage participation in class until the condition improves What will a burn victim feel with superficial versus deeper burns? p. 1487 First degree(Superficial)- Involves the epidermis or outer layer of skin. Appears reddened, dry, and feels mildly painful. Heals by simple regeneration so takes 1–10 days to heal. Second degree- Involves the epidermis and part of the dermis layer of skin. Appears red, blistered, and may be swollen. Very painful. Third degree- Involves the epidermis and full extent of the dermis. Appears white or charred and lacks sensation as the nerve endings are destroyed. ● What are nursing interventions in caring for a child needing burn treatments? pp. 1490-1491: -The child with a third-degree or fourth-degree burn is critically injured and requires immediate care. Sure care, including fluid therapy, systemic antibiotic therapy, pain management, and physical therapy. The goal is to prevent disability caused by scarring, infection, or contracture. Because pain and anxiety often accompany burn care, relieving them is always an important concern in burn care. Deficient fluid volume related to fluid shifts from severe burn-To detect whether extreme hypovolemia is occurring, monitor vital signs closely even with relatively minor burns; lactated Ringer’s solution is the commercially available solution most compatible with extracellular fluid, so that or normal saline will be administered for fluid replacement. A child may also need plasma replacement and a source of glucose such as 5% dextrose in water. Do not administer a potassium additive immediately after a burn until kidney function is evaluated to be certain extra potassium can be eliminated. What is debridement and its purpose? p. 1493-1494-Debridement is the removal of necrotic tissue on which microorganisms could thrive from a burned area to reduce the possibility of infection.If burned areas are debrided, granulation tissue forms underneath. When a full bed of granulation tissue is present (about 2 weeks after the injury), the area is ready for skin grafting. ● What is a child’s reaction to impending death? What may their anxieties be? pp. 1589-1592 Infants and Toddlers Infants and toddlers are certainly too young to appreciate that their death is imminent. If the person who cared for them dies, they experience a deep loss and a void in their life. If such a loss interferes with the development of a sense of trust, its implications for the child’s ability to achieve warm, close relationships could last a lifetime. Preschoolers Preschoolers cannot always differentiate what is real from what is make-believe play. This is a normal part of development and extends to abstract concepts such as illness and death. They envision death as temporary and therefore may not have the same fears adults may have about death. This view of death is sometimes interpreted as unfeeling. For example, the first response of a child who is told his brother has just been killed in an automobile accident might be to ask if he can have his brother’s cell phone. This happens because he thinks of his brother as being gone for only a short time, making this a chance to take advantage of his property. The understanding of death as temporary may be strengthened by fictional depictions of death in children’s animation or stories in which sometimes characters that are killed come back to life. The separation anxiety preschoolers experience can complicate their response to death. When confronted with their own death, their main concern may be separation from their parents. Constant reassurances and having a caregiver present with the child helps mitigate these fears. School-Age Children School-age children begin to have additional experiences with death, so their knowledge of its finality increases. They may think of it, however, as something that happens only to adults. Children’s books tend to deal only superficially with the subject, although many books that deal specifically with death are available for children (Box 56.5). As children near 8 or 9 years of age, they begin to appreciate that death is permanent. They may experience the same feeling of loneliness experienced when they went away to camp or just for a weekend, but this time, the separation will be permanent. Physical Exam Skills for dehydration May not have most current baseline weight prior to illness, so need to go by assessments Assessment Area Mild Dehydration 3-5% decrease in weight Moderate Dehydration 6-9% decrease in weight Severe Dehydration decrease in weight: ≥10% Pulses Full Weak Weak or unable to palpate HR Normal Elevated Elevated SBP Lower limit=70 + age x 2 Normal Normal to low Low Respirations Normal Deep, rate may be increased Deep, tachypnea, or decreased… apnea Buccal Mucosa Tacky, slightly dry Dry Parched Anterior Fontanel Normal Sunken Markedly sunken Eyes Normal Sunken Markedly sunken Skin Turgor Normal Reduced Tenting Skin Normal Cool Cool, mottled, acrocyanosis UOP Normal or mildly reduced Markedly reduced Anuric Mental Status Increased thirst Listless or irritable Grunting, lethargy, coma [Show More]
Last updated: 2 years ago
Preview 1 out of 47 pages
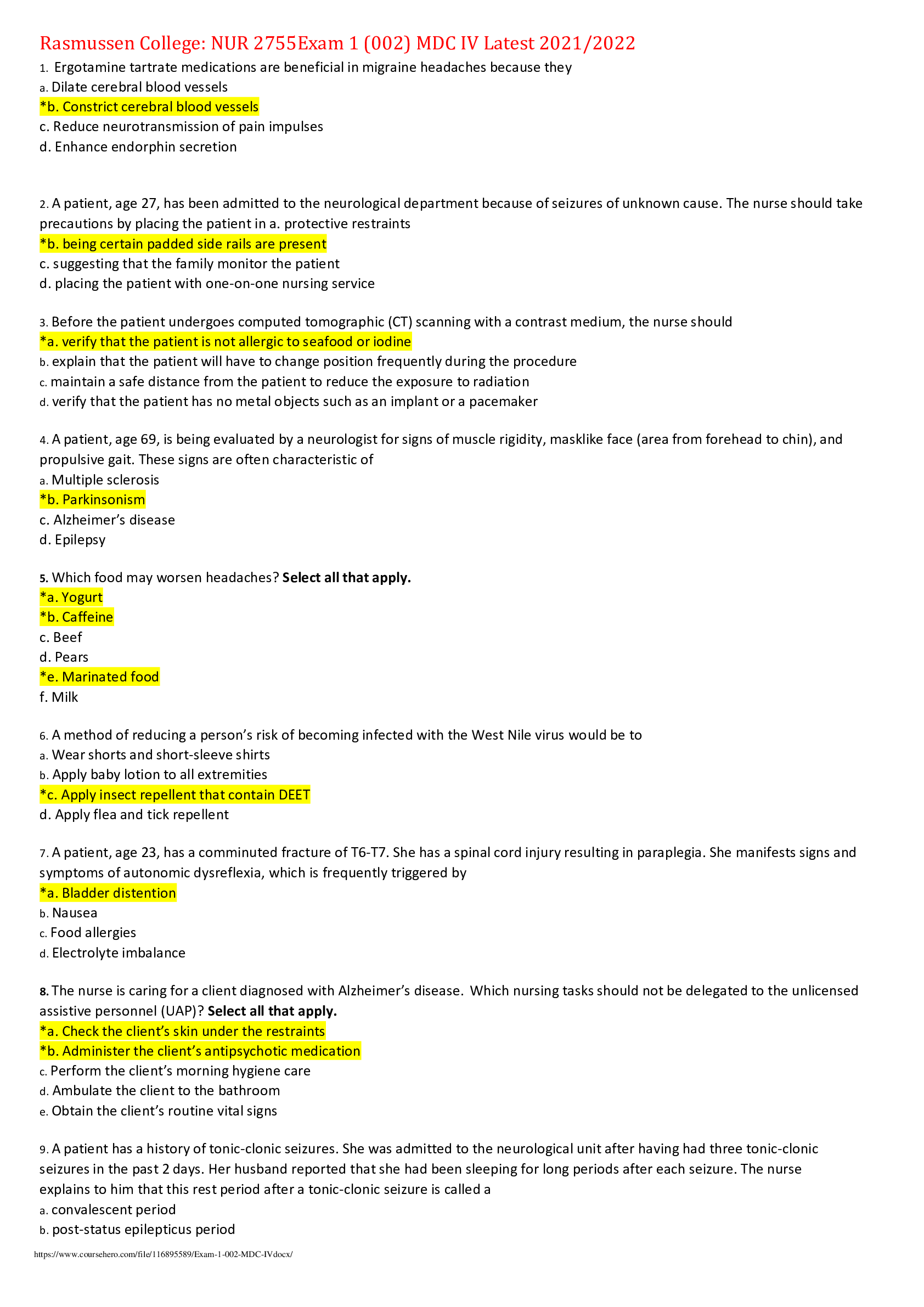
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$16.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
May 02, 2022
Number of pages
47
Written in
Additional information
This document has been written for:
Uploaded
May 02, 2022
Downloads
0
Views
103


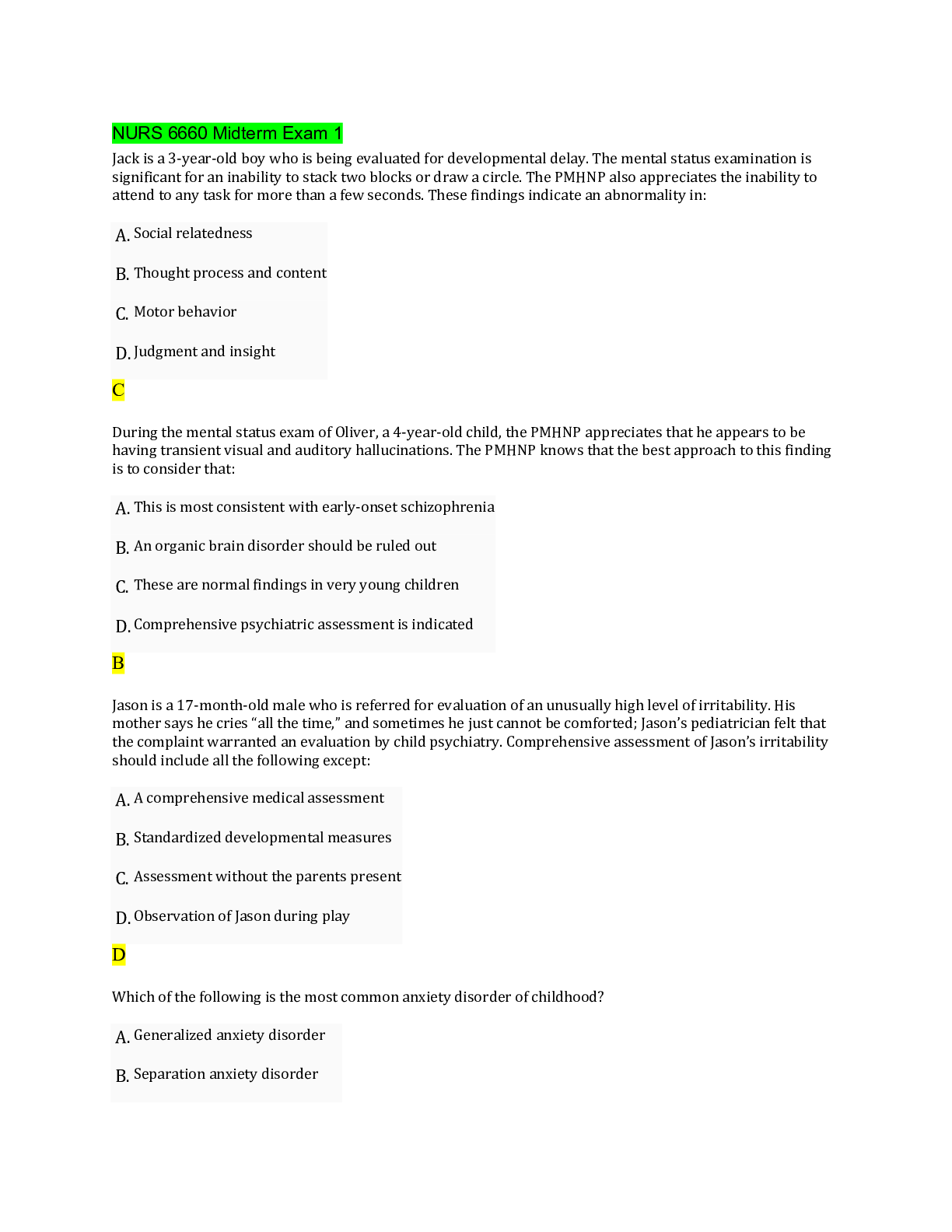
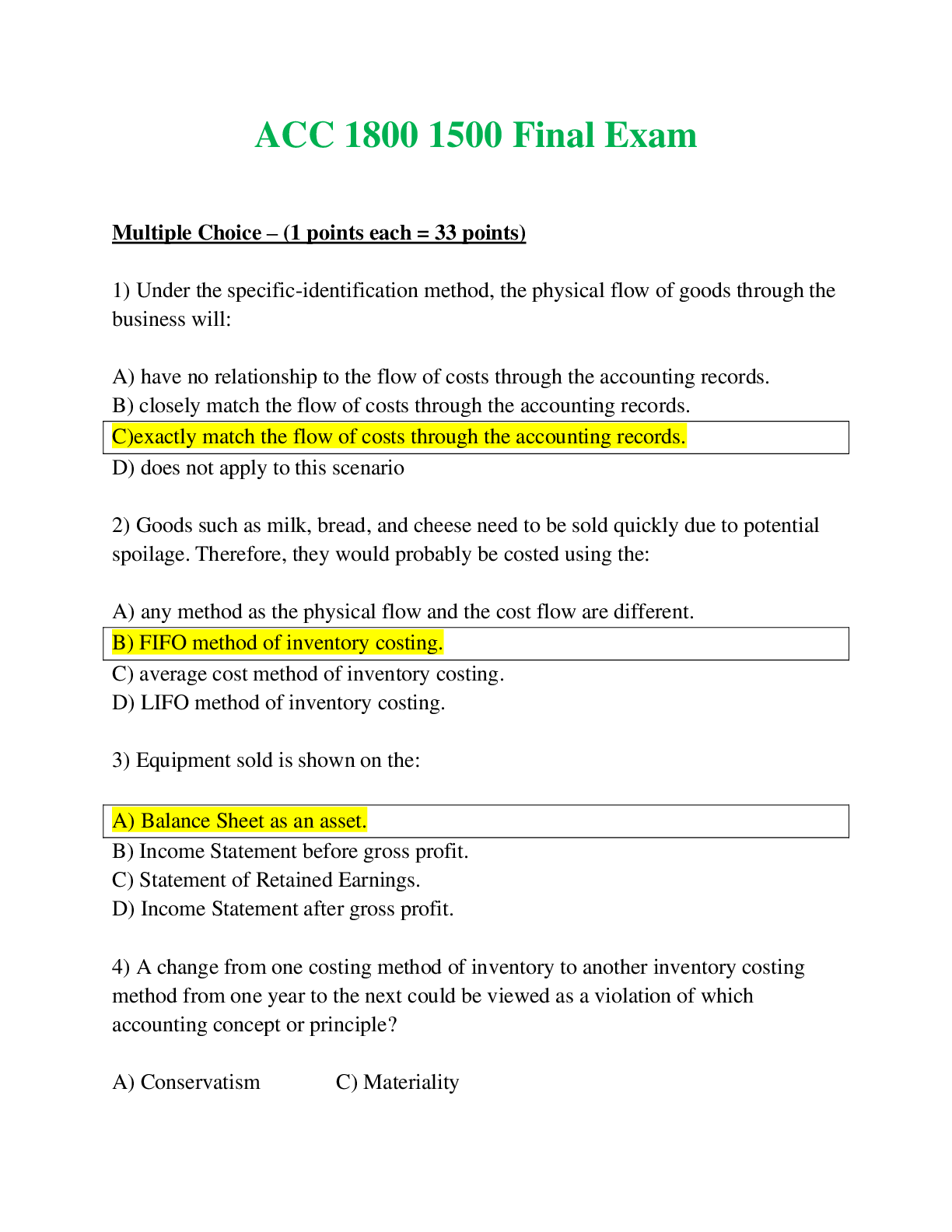

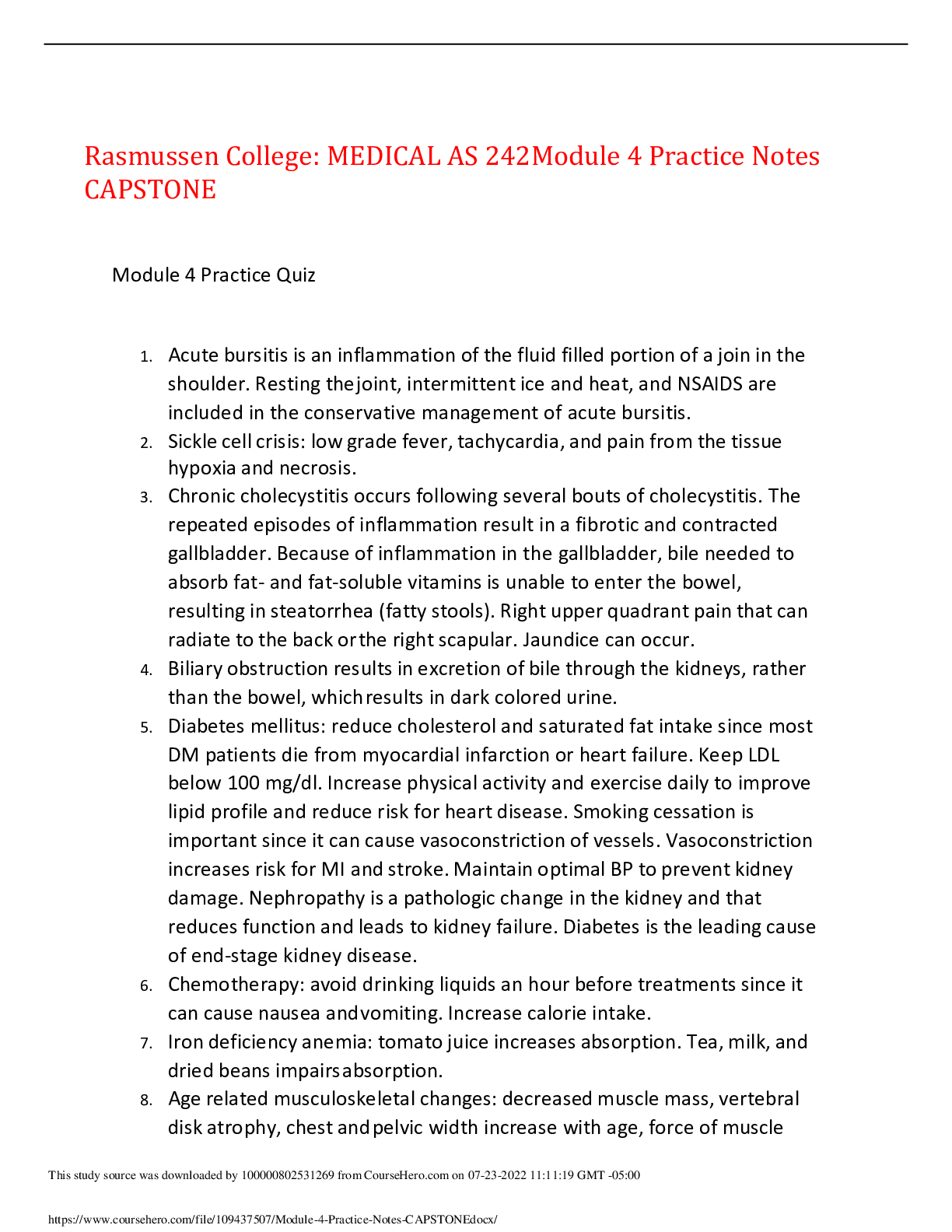

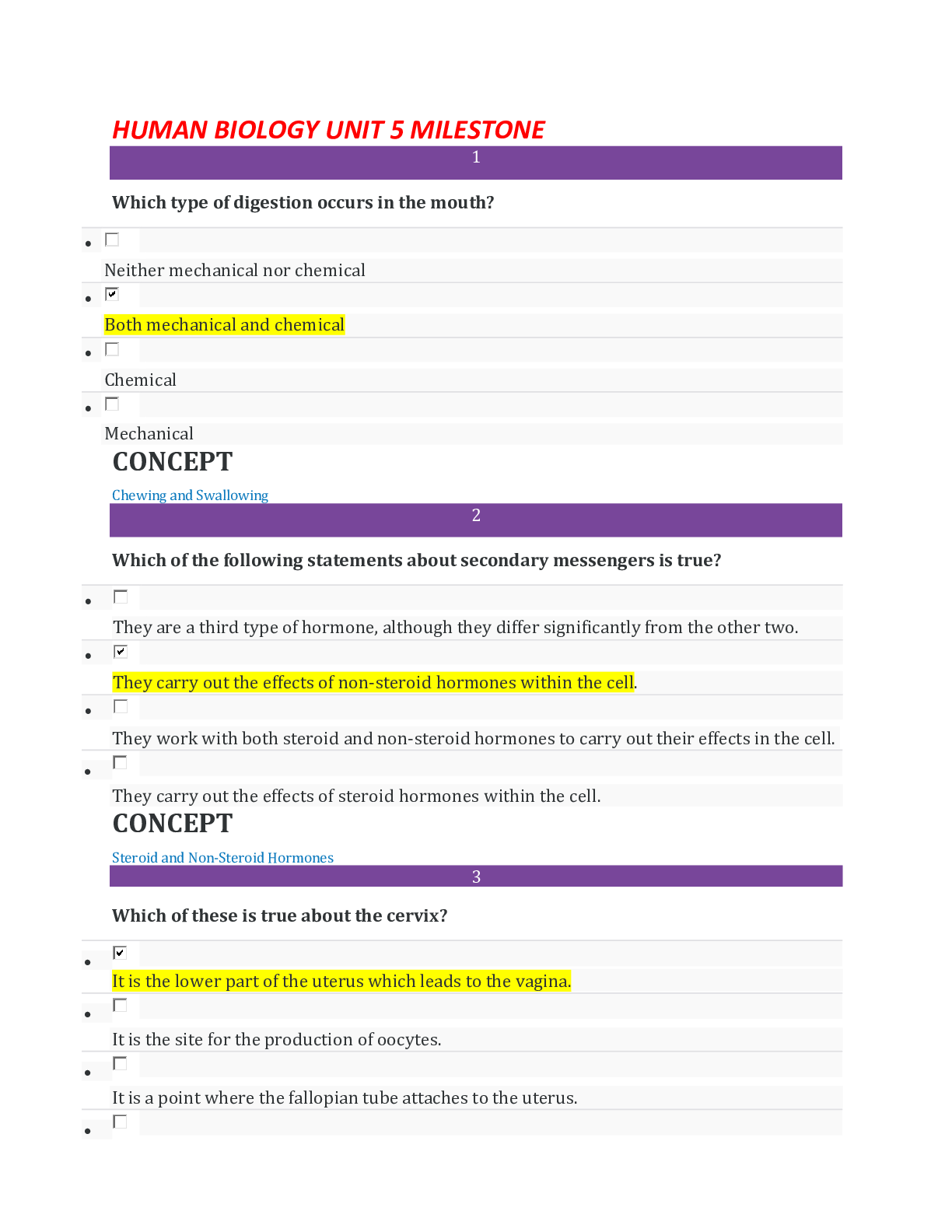




 AG21.png)