*NURSING > EXAM > NR 293 Week 4 Quiz 2 Take Home Assignment ( Pre-class questions Week 4) | Already GRADED A (All)
NR 293 Week 4 Quiz 2 Take Home Assignment ( Pre-class questions Week 4) | Already GRADED A
Document Content and Description Below
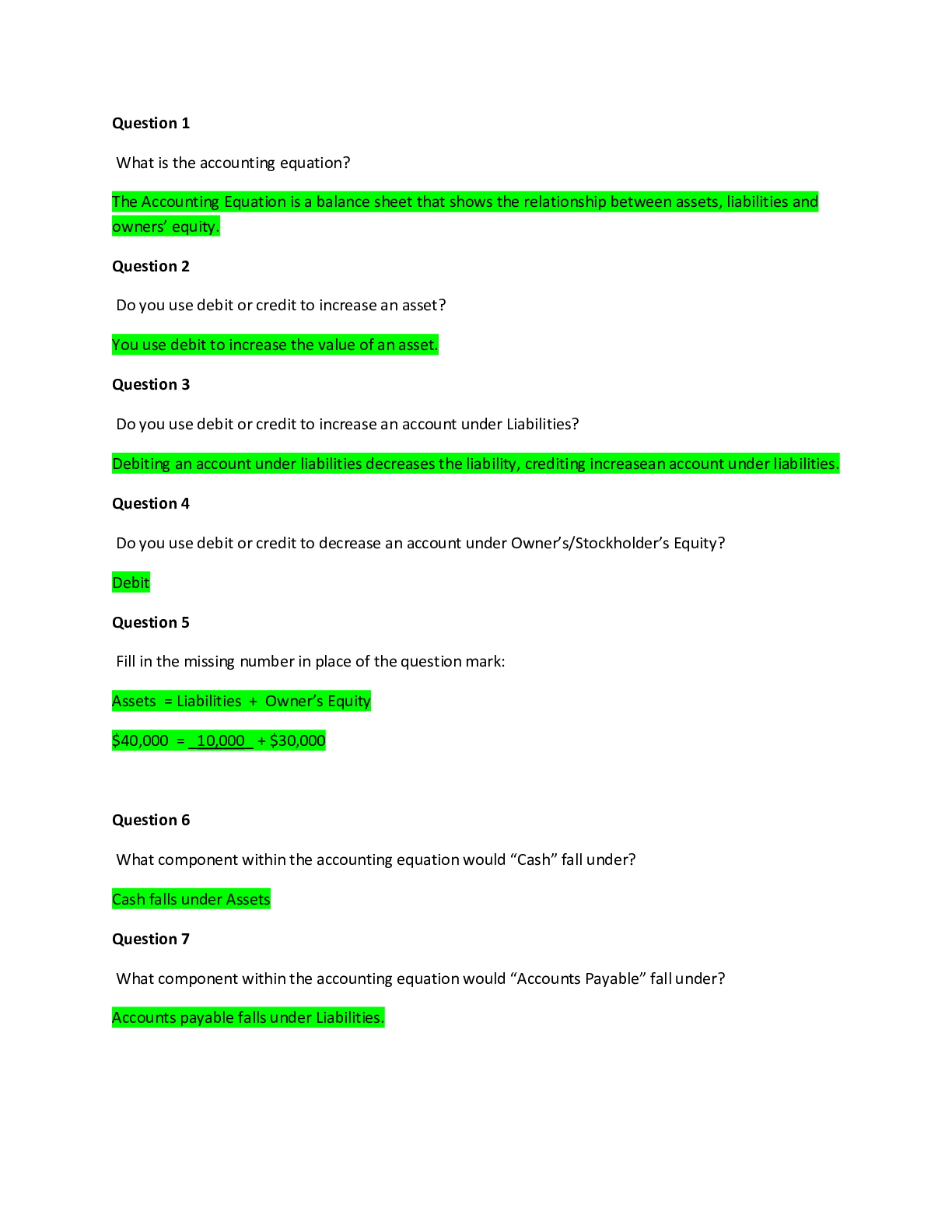
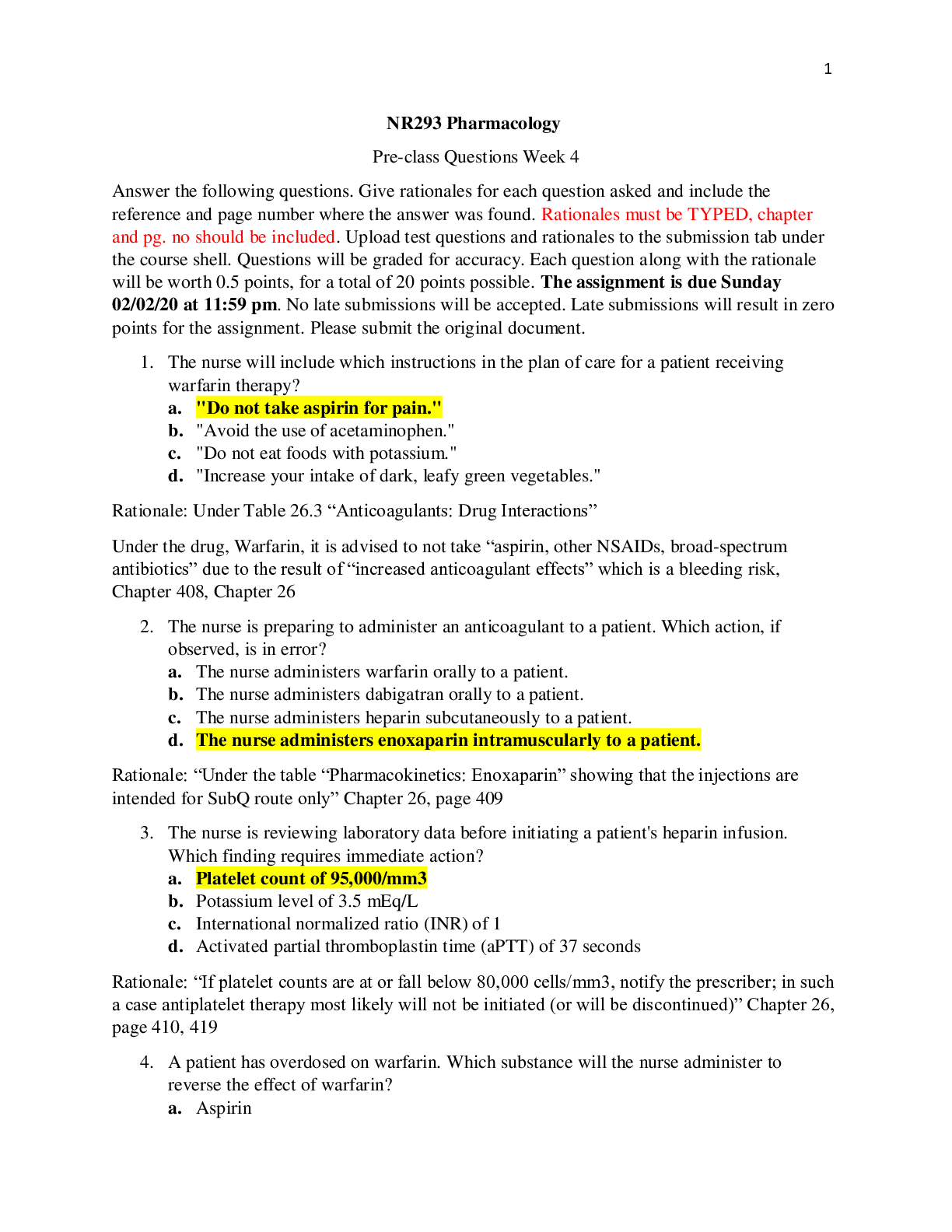
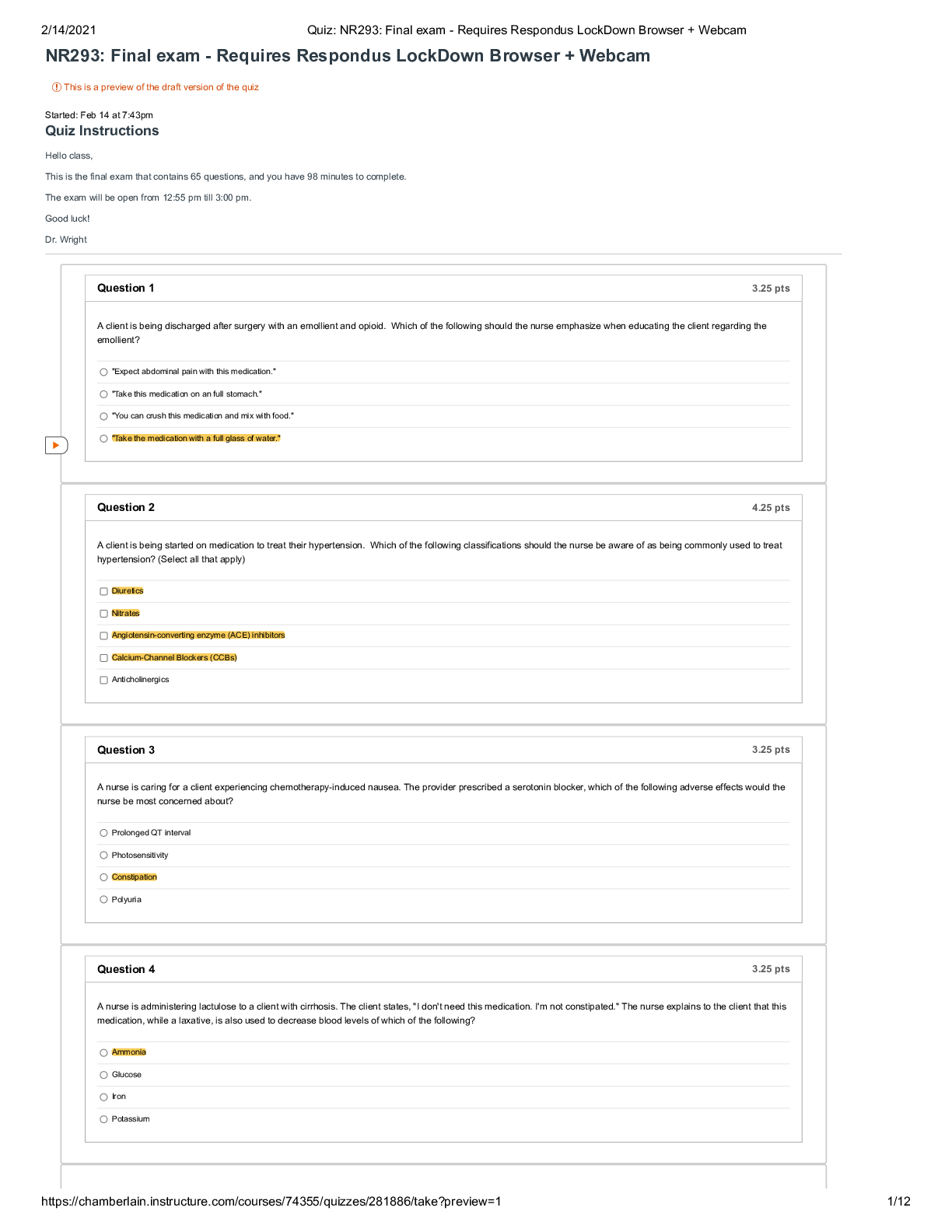
NR293 Pharmacology Pre-class Questions Week 4 Answer the following questions. Give rationales for each question asked and include the reference and page number where the answer was found. Rationales... must be TYPED, chapter and pg. no should be included. Upload test questions and rationales to the submission tab under the course shell. Questions will be graded for accuracy. Each question along with the rationale will be worth 0.5 points, for a total of 20 points possible. The assignment is due Sunday 02/02/20 at 11:59 pm. No late submissions will be accepted. Late submissions will result in zero points for the assignment. Please submit the original document. 1. The nurse will include which instructions in the plan of care for a patient receiving warfarin therapy? a. "Do not take aspirin for pain." b. "Avoid the use of acetaminophen." c. "Do not eat foods with potassium." d. "Increase your intake of dark, leafy green vegetables." Rationale: Under Table 26.3 “Anticoagulants: Drug Interactions” Under the drug, Warfarin, it is advised to not take “aspirin, other NSAIDs, broad-spectrum antibiotics” due to the result of “increased anticoagulant effects” which is a bleeding risk, Chapter 408, Chapter 26 2. The nurse is preparing to administer an anticoagulant to a patient. Which action, if observed, is in error? a. The nurse administers warfarin orally to a patient. b. The nurse administers dabigatran orally to a patient. c. The nurse administers heparin subcutaneously to a patient. d. The nurse administers enoxaparin intramuscularly to a patient. Rationale: “Under the table “Pharmacokinetics: Enoxaparin” showing that the injections are intended for SubQ route only” Chapter 26, page 409 3. The nurse is reviewing laboratory data before initiating a patient's heparin infusion. Which finding requires immediate action? a. Platelet count of 95,000/mm3 b. Potassium level of 3.5 mEq/L c. International normalized ratio (INR) of 1 d. Activated partial thromboplastin time (aPTT) of 37 seconds Rationale: “If platelet counts are at or fall below 80,000 cells/mm3, notify the prescriber; in such a case antiplatelet therapy most likely will not be initiated (or will be discontinued)” Chapter 26, page 410, 419 4. A patient has overdosed on warfarin. Which substance will the nurse administer to reverse the effect of warfarin? a. Aspirin b. Calcium c. Potassium d. Vitamin K Rationale: “In the event of warfarin toxicity or overdose, the first step is to discontinue the warfarin. As with heparin, the toxicity associated with warfarin is an extension of its therapeutic effects on the clotting cascade. However, because warfarin inactivates the vitamin K–dependent clotting factors and these clotting factors are synthesized in the liver, it may take 36 to 42 hours before the liver can resynthesize enough clotting factors to reverse warfarin’s effects. Giving vitamin K1 (phytonadione) can hasten the return to normal coagulation” Chapter 27, page 407 5. The nurse is caring for a patient who is scheduled to begin warfarin treatment and is currently being treated with amiodarone. Based on this information, the nurse anticipates which change will be made to the medication regimen? a. The dosage of the warfarin will be increased by half. b. The dosage of the warfarin will be decreased by half. c. The dosage of the amiodarone will be increased by half. d. The dosage of the amiodarone will be decreased by half. Rationale: “Combining warfarin and amiodarone will lead to a 50% increase in the INR. When amiodarone is added to warfarin therapy, it is recommended that the warfarin dose be cut in half” Chapter 26, page 411 6. The nurse is caring for a newly admitted patient who will begin heparin therapy. While documenting the patient history, the nurse notes that the patient is currently undergoing treatment with enoxaparin. What is the nurse's highest priority? a. Notify the provider that the patient is at risk for an allergic reaction. b. Notify the provider that heparin should not be started on the patient. c. Notify the provider that the dosage of heparin will need to be increased. d. Notify the provider that the dosage of heparin will need to be decreased. Rationale: Also, “a potentially deadly medication error is to give heparin in combination with enoxaparin (or any LMWH, dabigatran, rivaroxaban, apixaban, edoxaban or betrixaban). Always double-check that enoxaparin and other anticoagulants are never given to the same patient.” “LMWHs, especially enoxaparin, are also routinely used as anticoagulant bridge therapy in situations in which a patient must stop warfarin for surgery or other invasive medical procedures. The term bridge therapy refers to the fact that enoxaparin acts as a bridge to provide anticoagulation while the patient must be off of his or her warfarin therapy” Chapter 26, Page 406, 407, 409 7. A patient who has been receiving intravenous heparin as treatment for a deep vein thrombosis requires immediate surgery for a suspected bowel perforation. Which intervention is essential at this time? a. Administer vitamin K b. Administer protamine sulfate c. Assess the INR before surgery d. Provide patient teaching about the heparin Rationale: “Protamine is a specific heparin antidote and forms a complex with heparin, completely reversing its anticoagulant properties. This occurs in as little as 5 minutes. In general, 1 mg of protamine can reverse the effects of 100 units of heparin” Chapter 26, page 407 8. A patient is started on warfarin therapy while also receiving intravenous heparin. The patient is concerned about the risk for bleeding. What will the nurse tell the patient? a. "Your concern is valid. I will call the doctor to discontinue the heparin." b. "Because you are now up and walking, you have a higher risk of blood clots and therefore need to be on both medications." c. "It usually takes about 3 days to achieve a therapeutic effect for warfarin, so the heparin is continued until the warfarin is therapeutic." d. "Because of your valve replacement, it is especially important for you to be anticoagulated. The heparin and warfarin together are more effective than either one alone." Rationale: “Home therapy with parenteral anticoagulants may require injections for a period of time, and LMWHs are generally used. If there is a switch from heparin to warfarin (Coumadin), there will be an overlap period of at least 5 days during which both drugs are taken to allow therapeutic levels of the oral warfarin to be reached before the heparin is discontinued. This process may occur in the hospital or at home” “Recommendations for overlapping therapy of heparin and warfarin are for at least 5 days; the heparin is stopped after 5 days when the INR is above 2” Chapter 26, page 421, 424 9. A patient with a serum cholesterol level of 275 mg/dL is prescribed simvastatin. What instructions should the nurse provide to the patient? Select all that apply. a. "Avoid taking the drug with grapefruit juice." b. "Take aspirin 30 minutes before taking simvastatin." c. "Notify your health care provider if your urine becomes discolored." d. "Notify your health care provider if muscle pain occurs within 1 day." e. "Notify your health care provider if muscle pain occurs after 3 days." Rationale: Under “Patient-Centered Care: Patient Teaching” • Drug and food interactions associated with the statin drugs that must be avoided include oral anticoagulants, erythromycin, verapamil, some antifungal drugs, and grapefruit juice. • With the HMG-CoA reductase inhibitors or statin drugs, any muscle soreness, change in color of the urine, fever, nausea, vomiting, and/or malaise must be reported to the prescriber immediately. • Chapter 27, page 441 10. The nurse is caring for a patient who has elevated triglyceride levels and is unresponsive to HMG-CoA reductase inhibitors. What does the nurse expect the primary health care provider to prescribe to the patient? a. Colestipol b. Simvastatin c. Gemfibrozil d. Cholestyramine Rationale: “The fibric acid derivatives, gemfibrozil and fenofibrate, are prescription-only drugs and are the only two drugs available in this class. They are both classified as pregnancy category C drugs and are contraindicated in patients with a known hypersensitivity, preexisting gallbladder disease, significant hepatic or renal dysfunction, and primary biliary cirrhosis. Both drugs decrease the triglyceride levels and increase the HDL levels by as much as 25%” Chapter 27, page 437 11. A patient with hyperlipidemia has been prescribed simvastatin. The nurse instructs the patient to undergo a liver function test and kidney function test every 3 to 6 months. Which drug therapy–related complication in the patient is the nurse trying to prevent? a. Hepatitis b. Cirrhosis c. Nephritis d. Rhabdomyolysis Rationale: “A clinically important adverse effect is myopathy (muscle pain), which may progress to a serious condition known as rhabdomyolysis. This is the breakdown of muscle protein accompanied by myoglobinuria, which is the urinary elimination of the muscle protein myoglobin. Rhabdomyolysis can lead to acute renal failure and even death” “When recognized reasonably early, rhabdomyolysis is usually reversible with discontinuation of the statin drug. Risk factors for myopathy include age older than 65 years, hypothyroidism, renal insufficiency, and drug interactions. Instruct patients to immediately report any signs of toxicity, including muscle soreness or changes in urine color” Chapter 27, page 433 12. A patient with hyperlipidemia is treated with atorvastatin. On the follow-up visit, the nurse discovers that the patient has had no improvement in cholesterol levels. What could be the reason for this? a. The patient has a history of rhabdomyolysis. b. The patient took atorvastatin with gemfibrozil. c. The patient is taking the medication in the morning. d. The patient consumed more than 8 ounces of grapefruit juice per day. Rationale: “Atorvastatin has also been shown to raise levels of “good” cholesterol, the HDL component. All statins are dosed once daily, usually with the evening meal or at bedtime. Bedtime dosing provides peak drug levels in a time frame that correlates better with the natural diurnal (daytime) rhythm of cholesterol production in the body” Chapter 27, page 434 13. The nurse teaches the nursing student about statin drugs. Which statements by the student indicate effective learning? Select all that apply. a. "Statins can be used along with gemfibrozil." b. "Fluvastatin with warfarin increases the risk of bleeding." c. "Simvastatin is the least potent inhibitor of the CYP3A4 enzyme." d. "Atorvastatin with cyclosporine decreases the risk of rhabdomyolysis." e. "Pravastatin is not as effective as simvastatin for the inhibition of CYP3A4." Rationale: Statins are related to bleeding and CYP3A4. Statins are used for managing cholesterol and other bleeding diseases. Chapter 27, page 433 14. The nurse would question an order for colesevelam if the patient has which condition in the medical history? a. Impaction b. Glaucoma c. Renal disease d. Hepatic disease Rationale: “The adverse effects of colestipol, cholestyramine, and colesevelam are similar; however, colesevelam is reported to have fewer gastrointestinal adverse effects and drug interactions. Constipation is a common problem and may be accompanied by heartburn, nausea, belching, and bloating” 15. Which statement made by the patient indicates an understanding of discharge instructions on antihyperlipidemic medications? a. "I will stop taking the medication if it causes nausea and vomiting." b. "It is important to double my dose if I miss one in order to maintain therapeutic blood levels." c. "I will continue my exercise program to help increase my high-density lipoprotein serum levels." d. "Antihyperlipidemic medications will replace the other interventions I have tried to decrease my cholesterol." Rationale: “The therapeutic effects of both nonpharmacologic and pharmacologic measures are evidenced by a decrease in cholesterol and triglyceride levels to within normal ranges (see previous presentations of serum laboratory values). Nonpharmacologic measures include a low- fat, low-cholesterol diet; supervised, moderate exercise; weight loss; cessation of smoking and drinking; and relaxation therapy” “The AHA also strongly emphasizes the substantial therapeutic benefits of even modest weight reduction and exercise in both improvement of lipid profiles and reduction of the likelihood of heart disease” Chapter 27, page 430, 440 16. A patient is taking pravastatin sodium. Which assessment finding requires immediate action by the nurse? a. Headache b. Muscle pain c. Constipation d. Slight nausea Rationale: “A clinically important adverse effect is myopathy (muscle pain), which may progress to a serious condition known as rhabdomyolysis. This is the breakdown of muscle protein accompanied by myoglobinuria, which is the urinary elimination of the muscle protein myoglobin. Rhabdomyolysis can lead to acute renal failure and even death” “Pravastatin and fluvastatin inhibit CYP3A4 to a much smaller degree than the other statins, whereas lovastatin and simvastatin are the most potent inhibitors of this enzyme. The use of gemfibrozil and statins together is not recommended owing to an increased risk for rhabdomyolysis” Chapter 27, page 433 17. A patient is prescribed dextromethorphan for treatment of cough. What instruction should the nurse give to the patient for safe administration of the drug? a. "Use a humidifier while sleeping." b. "Elevate your bed while sleeping." c. "Increase your fluid intake to 3000 mL per day." d. "Restrict activities that require mental alertness." Rationale: “Although dextromethorphan failed as an opioid, it is widely used as an over-the- counter (OTC) cough suppressant. It is becoming an increasingly popular drug of abuse. It can produce a “high” associated with very large doses. It also produces hallucinations, which is documented to be similar to phencyclidine (PCP)” Chapter 17, 276 18. A patient is prescribed guaifenesin for treatment of productive cough. What instruction should the nurse give to the patient for maximum therapeutic effect? a. "Increase your fluid intake." b. "Increase your fiber intake." c. "Increase your protein intake." d. "Increase your carbohydrate intake." Rationale: “Educate patients that all dosage forms are to be taken as instructed and with an increase in fluid intake of up to 3000 mL per day, unless contraindicated. The fluid helps to liquefy secretions, assists in breaking up thick secretions, and makes it easier to cough up secretions” Chapter 36, page 563 19. For which adverse drug effect is the nurse alert in an older adult patient taking diphenhydramine? a. Hay fever b. Insomnia c. Hypertension d. Urinary retention Rationale: Under Table 36.3 “Antihistamines: Reported Adverse Effects” • [Body System] Other—dryness of mouth, nose, and throat; urinary retention; vertigo; visual disturbances; tinnitus; headache. • Chapter 36, page 557 20. A patient who takes several medications experiences a troublesome cough associated with allergic rhinitis. Which is the best choice of treatment to manage the cough? a. Loratadine b. Guaifenesin c. Benzonatate d. Dextromethorphan Rationale: “Guaifenesin (Mucinex) is a commonly used expectorant that is available in several different oral dosage forms: capsules, tablets, solutions, and granules. It is used in the symptomatic management of coughs of varying origin. It is beneficial in the treatment of productive coughs because it thins mucus in the respiratory tract that is difficult to cough up” Chapter 36, page 562 21. Which is the most effective antitussive? a. Codeine b. Benzonatate c. Diphenhydramine d. Dextromethorphan Rationale: “Codeine is a popular opioid antitussive drug. It is used in combination with many other respiratory medications to control coughs. Because it is an opioid, it is potentially addictive and can depress respirations as part of its CNS depressant effects. For this reason, codeine- containing cough suppressants are controlled substances” Chapter 36, page 561 22. The nurse is caring for a patient who is taking a traditional antihistamine. What is the most important information for the nurse to teach the patient? a. "Do not drive after taking this medication." b. "Take this medication on an empty stomach." c. "Do not take this medication for more than 2 days." d. "Make sure you drink a lot of liquids while on this medication." Rationale: “Educate about the sedating effects of traditional antihistamines. The patient needs to avoid activities that require mental alertness until tolerance to sedation occurs or until he or she accurately judges that the drug has no impact on motor skills or responses to motor activities. Include a list of drugs the patient must avoid, such as alcohol and CNS depressants” Chapter 36, page 564 23. The nurse is assessing a toddler who is unconscious after consumption of over-the- counter cold medication. What other assessment findings should the nurse expect to see in this child? Select all that apply. a. Seizures b. Tachycardia c. Hypocalcemia d. Hyperuricemia e. Hyperglycemia Rationale: “In 2008, the US Food and Drug Administration (FDA) issued recommendations that over-the-counter (OTC) cough and cold products not be given to children younger than 2 years of age. This followed numerous case reports of symptoms such as oversedation, seizures, tachycardia, and even death in toddlers” Chapter 36, page 554 24. The nurse is teaching a patient about the use of an expectorant. What is the most important instruction for the nurse to include in the patient teaching? a. "Take the medication once a day only, at bedtime." b. "Restrict your fluids to decrease mucus production." c. "Increase your fiber and fluid intake to prevent constipation." d. "Increase your fluid intake to decrease viscosity of secretions." Rationale: “Educate patients that all dosage forms are to be taken as instructed and with an increase in fluid intake of up to 3000 mL per day, unless contraindicated. The fluid helps to liquefy secretions, assists in breaking up thick secretions, and makes it easier to cough up secretions” Chapter 36, page 563 25. A patient with a history of asthma is short of breath and says, “I feel like I’m having an asthma attack.” What is the nurse’s highest priority action? a. Calling a code b. Administering a beta2-adrenergic agonist c. Administering a long-acting glucocorticoid d. Asking the patient to describe the symptoms Rationale: “The beta2 agonists are helpful in treating conditions such as asthma and bronchitis. Common bronchodilators that are classified as predominantly beta2 albuterol, ephedrine, formoterol, levalbuterol, metaproterenol, pirbuterol, salmeterol, and terbutaline” Chapter 18, page 292 26. For what side effects should the nurse ask the patient to be watchful when administering mixed alpha/beta agonists? Select all that apply. a. Anorexia b. Drowsiness c. Hypoglycemia d. Vascular headache e. Cardiac stimulation Rationale: “Mixed alpha/beta agonists produce the most adverse effects because they are nonselective. These include insomnia, restlessness, anorexia, cardiac stimulation, hyperglycemia, tremor, and vascular headache” Chapter 37, page 571 27. A patient is prescribed albuterol. The nurse is explaining the most common route of administration of albuterol to the patient. Which route should the nurse discuss? a. Inhalation b. Intravenous c. Subcutaneous d. Intramuscular Rationale: “Albuterol is available for both oral and inhalational use. Inhalational dosage forms include metered-dose inhalers (MDIs) as well as solutions for inhalation” Chapter 37, page 571 28. A patient received methylprednisolone intravenously for 4 days for acute asthma. The nurse is preparing for the discharge of the patient with a prescription for fluticasone. Which priority instruction should the nurse include while educating the patient before discharge? a. "Take fluticasone exactly as it is prescribed." b. "Rinse your mouth with water after using fluticasone." c. "Avoid situations that can expose you to the infections." d. "Administer albuterol before other asthma medications." Rationale: “Inhaled corticosteroids (glucocorticoids) are yet another group of drugs that must be used as prescribed and with cautions regarding overuse. Advise the patient to take the medication as ordered every day regardless of whether or not he or she is feeling better” Chapter 37, page 580 29. A patient is prescribed theophylline for the treatment of chronic bronchitis. What instruction should the nurse give to the patient for safe administration of theophylline? a. "Avoid consumption of citrus fruit." b. "Avoid intake of a high-protein diet." c. "Increase fluid intake up to 3 L per day." d. "Increase intake of low-carbohydrate food." Rationale: “In patients taking xanthine derivatives (e.g., theophylline), identify any contraindications and cautions…Perform a dietary assessment, including questions about consumption of a low-carbohydrate, high-protein diet, and intake of charcoal-broiled meat. These dietary practices may lead to increased theophylline elimination and decreased therapeutic levels of the drug” Chapter 37, page 578-579 30. A patient is prescribed inhaled corticosteroids. Why should the nurse ask the patient to rinse the mouth after each dose? a. To relieve the patient’s dry mouth b. To minimize the chance of nasal congestion c. To reduce the risk of sore throat and infection d. To prevent the development of oral candidiasis Rationale: “Recommend rinsing the mouth immediately after use of the inhaler or nebulizer dosage forms of corticosteroids to help prevent overgrowth of oral fungi and subsequent development of oral candidiasis (thrush)” Chapter 37, page 581 31. A patient on theophylline therapy complains of gastroesophageal reflux during sleep. What other complications should the nurse anticipate in the patient? Select all that apply. a. Vomiting b. Insomnia c. Dry mouth d. Increased urination e. Ventricular dysrhythmias Rationale: “The common adverse effects of the xanthine derivatives include nausea, vomiting, and anorexia. Cardiac adverse effects include sinus tachycardia, extrasystole, palpitations, and ventricular dysrhythmias. Transient increased urination and hyperglycemia are other possible adverse effects” Chapter 37, page 573 32. The health care provider prescribes albuterol and beclomethasone inhalers for a patient. What is the nurse’s best action? a. Administer each inhaler at 30-minute intervals. b. Question the prescription; two inhalers should not be given at one time. c. Administer beclomethasone, wait 2 minutes, and then administer albuterol. d. Administer the albuterol, wait 5 minutes, and then administer beclomethasone. Rationale: “If a second puff of the same drug is ordered, instruct the patient to wait 1 to 2 minutes between puffs. If a second type of inhaled drug is ordered, instruct the patient to wait 2 to 5 minutes between the medications or as prescribed” Chapter 37, page 580 33. Which is a common expected adverse effect of iron supplementation? a. Flatus b. Fatigue c. Heartburn d. Constipation Rationale: Under Table 51.3 “Causes of Constipation” Analgesics, anticholinergics, iron supplements, aluminum antacids, calcium antacids, opiates, calcium channel blockers are listed examples under adverse drug effects that can cause constipation” Chapter 51, page 800 34. Which route of administration results in a slow onset of action of epoetin alfa? a. Oral b. Intravenous c. Intramuscular d. Subcutaneous Rationale: “Epoetin alfa (Epogen) is indicated for anemias associated with end-stage renal disease and chemotherapy. It requires very careful use. Always check for route of administration, with the subcutaneous route having a slower onset of action than the intravenous route” Chapter 54, page 851 35. A child who accidently ingested an enteric-coated iron supplement develops seizures and is immediately hospitalized. The serum iron concentration is found to be 350 mcg/dL. What intervention should the nurse expect the provider to prescribe to reduce the serum iron levels? a. Bowel irrigation b. An electrolyte infusion c. Abdominal radiographs d. Administration of deferoxamine Rationale: “In patients with severe symptoms of iron intoxication, such as coma, shock, or seizures, chelation therapy with deferoxamine is initiated” Chapter 54, page 847 36. A patient informs the nurse she must take her iron with a meal to prevent stomach upset. To increase the uptake of oral iron, which food group will the nurse instruct the patient to avoid? a. Dairy b. Fruits c. Proteins d. Vegetables Rationale: “Other oral forms of iron must be given with plenty of fluids but not with antacids or milk and preferably not with meals, because of the risk for decreased absorption of the drug. However, most individuals find that they do need to take oral iron products with meals or food because of the commonly encountered adverse effect of gastrointestinal upset. If antacids or milk products are used, schedule them at least 2 hours before or after the oral dose of iron” Chapter 54, page 850 37. What intervention will the provider prescribe to increase the effectiveness of epoetin alfa? a. Administer folic acid along with epoetin alfa. b. Administer folic acid 1 to 2 hours after epoetin alfa. c. Administer ferrous fumarate along with epoetin alfa. d. Administer ferrous fumarate 1 to 2 hours after epoetin alfa. Rationale: This medication, epoetin alfa, should be given with ferrous fumarate in order to increase the effectiveness of the medication. Chapter Page 486, 487 38. Iron dextran is prescribed for a patient with severe iron-deficiency anemia. How will the nurse administer the drug? a. Administer a test dose by the intravenous route. b. Administer a test dose by the subcutaneous route. c. Administer the full dose by the intravenous route. d. Administer the full dose by the subcutaneous route. Rationale: “Iron dextran (INFeD, Dexferrum) is a colloidal solution of iron (as ferric hydroxide) and dextran. It is intended for intravenous or intramuscular use for the treatment of iron deficiency. Anaphylactic reactions to iron dextran, including major orthostatic hypotension and fatal anaphylaxis, have been reported in 0.3% of patients. Because of this, a test dose of 25 mg of iron dextran is administered before injection of the full dose” Chapter 54, page 848 39. What precautions will the nurse take before starting intravenous (IV) iron therapy? Select all that apply. a. Flush the IV line with normal saline. b. Monitor blood pressure periodically. c. Keep resuscitative equipment available. d. Suggest exercising right before the injection. e. Administer the injection using the Z-track method. Rationale: “Intramuscularly administrated iron must be given deep in a large muscle mass using the Z- track method. Iv iron dextran must be given after the IV line is flushed with 10 mL normal saline. Keep epinephrine and resuscitative equipment available in case of an anaphylactic reaction.” Chapter 54, page 851 40. Which drug is used to treat iron overdose? a. Deferiprone b. Tetracycline c. Methotrexate d. Trimethoprim Rationale: “In 2011, the FDA approved deferiprone, which can also be used to treat iron overload” Chapter 54, page 847 [Show More]
Last updated: 2 years ago
Preview 1 out of 12 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jun 27, 2022
Number of pages
12
Written in
Additional information
This document has been written for:
Uploaded
Jun 27, 2022
Downloads
0
Views
85


 Questions and Answers 100% VERIFIED.png)
 Questions and Answers 100% correct Solutions.png)






.png)