Pathophysiology Final Study Guide
Patho Section 1
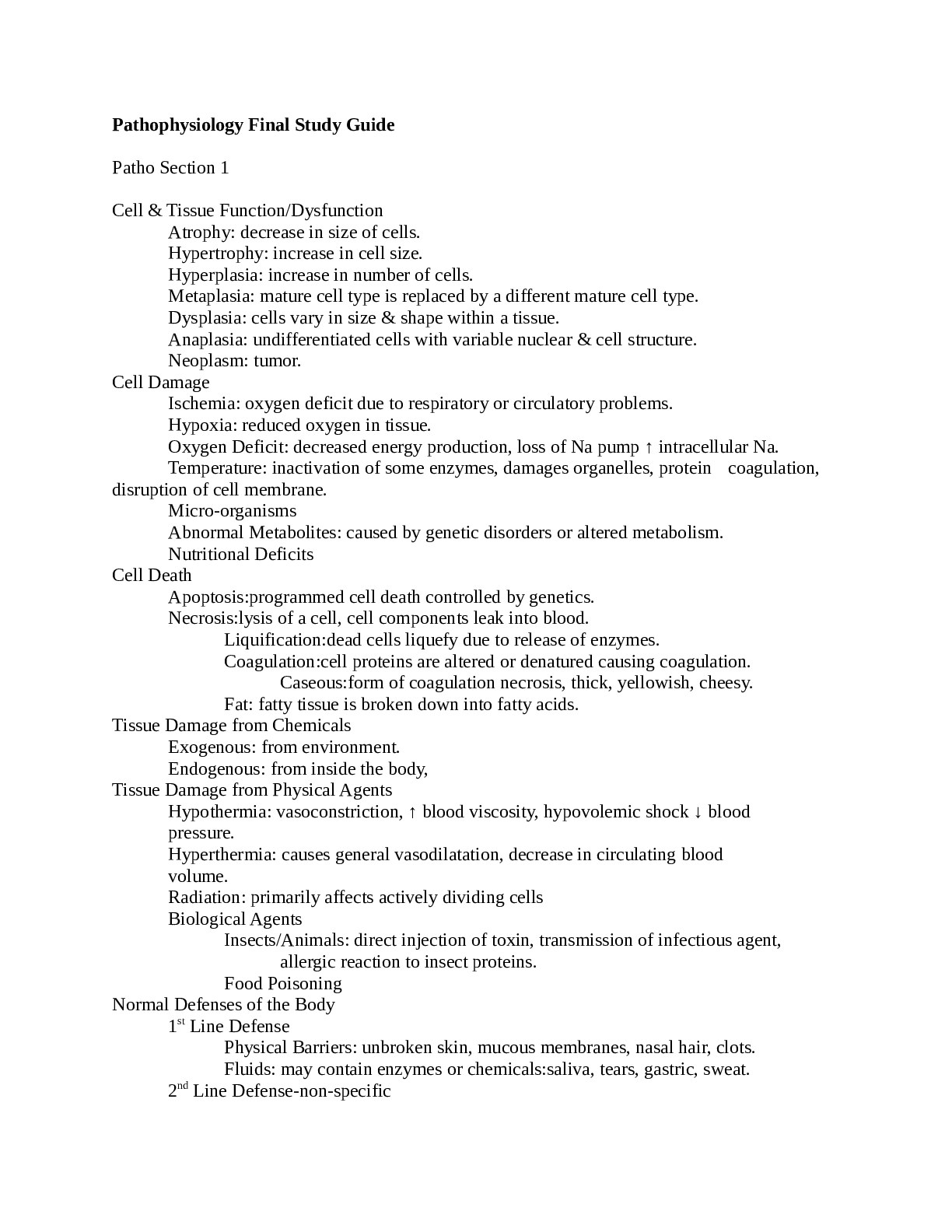
Cell & Tissue Function/Dysfunction
Atrophy: decrease in size of cells.
Hypertrophy: increase in cell size.
Hyperplasia: increase in number of cells.
Metaplasia: mat
...
Pathophysiology Final Study Guide
Patho Section 1
Cell & Tissue Function/Dysfunction
Atrophy: decrease in size of cells.
Hypertrophy: increase in cell size.
Hyperplasia: increase in number of cells.
Metaplasia: mature cell type is replaced by a different mature cell type.
Dysplasia: cells vary in size & shape within a tissue.
Anaplasia: undifferentiated cells with variable nuclear & cell structure.
Neoplasm: tumor.
Cell Damage
Ischemia: oxygen deficit due to respiratory or circulatory problems.
Hypoxia: reduced oxygen in tissue.
Oxygen Deficit: decreased energy production, loss of Na pump ↑ intracellular Na.
Temperature: inactivation of some enzymes, damages organelles, protein coagulation,
disruption of cell membrane.
Micro-organisms
Abnormal Metabolites: caused by genetic disorders or altered metabolism.
Nutritional Deficits
Cell Death
Apoptosis:programmed cell death controlled by genetics.
Necrosis:lysis of a cell, cell components leak into blood.
Liquification:dead cells liquefy due to release of enzymes.
Coagulation:cell proteins are altered or denatured causing coagulation.
Caseous:form of coagulation necrosis, thick, yellowish, cheesy.
Fat: fatty tissue is broken down into fatty acids.
Tissue Damage from Chemicals
Exogenous: from environment.
Endogenous: from inside the body,
Tissue Damage from Physical Agents
Hypothermia: vasoconstriction, ↑ blood viscosity, hypovolemic shock ↓ blood
pressure.
Hyperthermia: causes general vasodilatation, decrease in circulating blood
volume.
Radiation: primarily affects actively dividing cells
Biological Agents
Insects/Animals: direct injection of toxin, transmission of infectious agent,
allergic reaction to insect proteins.
Food Poisoning
Normal Defenses of the Body
1st Line Defense
Physical Barriers: unbroken skin, mucous membranes, nasal hair, clots.
Fluids: may contain enzymes or chemicals:saliva, tears, gastric, sweat.
2nd Line Defense-non-specific
Phagocytosis:neutrophils & macrophages engulf cells, debris, foreign mat.
Inflammation: automatic response to cell injury.
3rd Line Defense-specific defense produced by
Antibodies
Cell Mediated Immunity
Cellular Defenses
Mast Cells: located in tissue & release histamine & bradykinin.
Macrophages: monocytes that enter tissue & act as phagocytes.
Interferons: small proteins made by lymphocytes to prevent virus replication.
White Blood Cells
Granulocytes
Neutrophils: work by phagocytosis.
Basophils: release histamine leading to inflammation.
Eosinophils:combat the effects of histamine.
Agranulocytes
Monocytes:can enter tissue to become macrophages which
function as phagocyte.
Lymphocytes: B & T
Acute Inflammation
Vascular Response: vasodilatation & increased capillary permeability.
Cellular Response: migration of inflammatory cells through chemotaxis to injury site to
destroy ineffective organism, remove damaged cells, released inflammation mediators.
Exudate
Serous: watery, mostly fluids, some proteins and WBC’s.
Fibrinous: thick, sticky, high fibrin content.
Purulent: thick, yellow-green, contains leukocytes, cell debris & microorganisms.
Abscess: Pocket of purulent exudates or pus in a solid tissue.
Local Effects of Inflammation-Cardinal Signs of Inflammation
Redness & Warmth: due to increased blood flow to area.
Swelling: shift of protein & fluid into interstitial space.
Pain: pressure on free nerve endings, chemical mediators irritate nerves.
Loss of Function: edema may restrict movement.
Systemic Effects of Inflammation
Mild Fever: due to resetting of hypothalamic thermoregulatory set point, release of
endogenous pyrogens.
Malaise
Fatigue
Headache
Anorexia
Treatment of Inflammation: drugs may decrease capillary permeability, reduce number of
leukocytes & mast cells.
Types of Healing
Resolution: minimal tissue damage, cells can repair themselves.
Regeneration: damaged tissue is replaced by identical tissue.
Replacement: functional tissue replaced by scar or fibrous tissue.
1st Intention: wound is clean, edges are close together with minimal gap.
2nd Intention: large break in tissue, longer healing process with more scar tissue.
Scar Formation: fibroblasts proliferate, abnormal amount of collagen.
Hypertrophic: overgrowth of fibrous tissue, keloid.
Ulceration: blood supply around scar is impaired resulting in tissue
breakdown.
Wound Staging
1. Partial thickness ulcer-red or pink ie. Sunburn.
2. Partial thickness ulcer-blister, scrape, abrasion.
3. Full thickness ulcer- through dermis.
4. Full thickness ulcer that includes muscle or bone.
Drainage
Transudate: clear & watery.
Serosanginous: clear w/ tinge of red/brown. Contains serum/blood thin & watery.
Exudate: creamy yellowish. Contains proteins & WBC’s Thick.
Purulent: yellowish. Contains leukocytes and necrotic debris, thick.
Infected Pus: hues of yellow, green or blue. Contains pathogens, thick.
Venous Insufficiency Clinical Presentation
Incompetent Valves medial leg area
Inefficient Calf Pump edema
Distended Capillary Bed wet wound
Decreased Fibrolysis scaring, red base
Fibrin Leakage hemosiderin deposits(purple/brown on leg)
Trauma Ulcer
Documentation of Pulses
Normal: 2+
Diminished: 1+
Absent: 0
Arterial Insufficiency: decreased arterial blood supply.
Acute(thrombosis) vs Chronic(arteriosclerosis)
Characteristics
Dry Gangrene: nonviable dry tissue.
Wet Gangrene: tissue necrosis + bacterial infection. Drainage w/ odor.
Black Gangrene: gangrenous borders, mummified skin.
Pain w/ walking=Claudication
Skin is atrophic(no hair) slow nail growth & Diminished Pulse
Ankle Pressure Index: SBP LE/SBP UE
>1 no arterial occlusive disease
.9-1 min sx in LE
.5-.9 claudication pain(leg pain w/ walking)
.3-.5 ischemic rest pain
<.3 ischemic w/ tissue necrosis
Assessment of arterial flow, skin color w/ elevation/dependency
1. LE Elevation to 60º for 1 minute. Normal=no color change.
2. Lower the LE & record time for color to return.>30seconds
means arterial insufficiency. Will look hyperemic(bright red).
Immune Response-Third Body Defense
Humeral Immunity: antibodies are produced to protect body & stored in blood.
Cell Mediated Immunity:lymphocytes are programmed to attack non-self cells.
Antigens:immunogens, proteins, polysaccharides, glycoproteins on cell surface.
Cells
Macrophages:present throughout the body, derived from monocytes,
initiate immune response, engulf foreign materialprocess & display
foreign antigens & present them to lymphocytes, secrete monokines &
interleukins .
Lymphocytes:primary cell in immune response,
T: has 3 subgroups made in bone marrow & differentiate in
thymus, cell mediated immunity, can target certain cells.
1.Cytotoxic T:cells destroy cells bind to antigen & release enzymes
2.Helper T: facilitate immune response by activating & regulating
3.Memory T: remember antigens.
B:Made in bone marrow, located in spleen & lymphoid tissue,
produce antibodies.
Natural Killer:kill tumor or virus infected cells w/o prior exposure
Antibodies
IgG:most common, can activate compliment, cross placenta, primary &
secondary immune response.
IgM:can activate compliment, natural antibodies ie. Involved in blood type
IgA:not in blood, is in tears, saliva & colostrums.
IgE
IgD
Compliment System:antigen-antibody complex, activated during immune rxn w/ IgG or
IgM. Causes cell damage when activated, causes macrophages to release enzymes.
Immune Response
Primary: 1st exposure to antigen, 1-2 weeks needed for effective antibodies
Secondary:repeat exposure to same antigen, effective response in 1-3 days
Immunity: Innate-always present. Or acquired.
Hypersensitivity Reactions
Type 1 Hypersensitivity:allergic rxn, exposed to allergen causes development of
IgE’s,activate mast cells and causes inflammation. Ie. Hay fever, allergies, asthma
Type 2 Hypersensitivity:cytotoxic hypersensitivity. Antigen on cell membrane reacts
w/ circulating IgG’s, activates compliment, cells w/ antigen destroyed. Ie incompatible blood
type exposure.
Type 3: Immune complex hypersensitivity-antigen & antibody combine forming
immune complexes that cause inflammation & tissue destruction.
Type 4:Cell Mediated or delayed response by T-lymphocytes. No antibodies
present. Ie. Tb test, contact dermatitis.
Immune System Malfunction
Hypersensitivity: full system immune response to non-noxious stimulus.
Asthma: central windpipe or airway disorder.
[Show More]