UWORLD NCLEX RATIONALES/INFORMATION TO KNOW
CARDIAC RATIONALES:
Hypovolemic shock most commonly occurs from blood loss but can occur in any condition that reduces intravascular volume. Hypovolemia is classified as eit
...
UWORLD NCLEX RATIONALES/INFORMATION TO KNOW
CARDIAC RATIONALES:
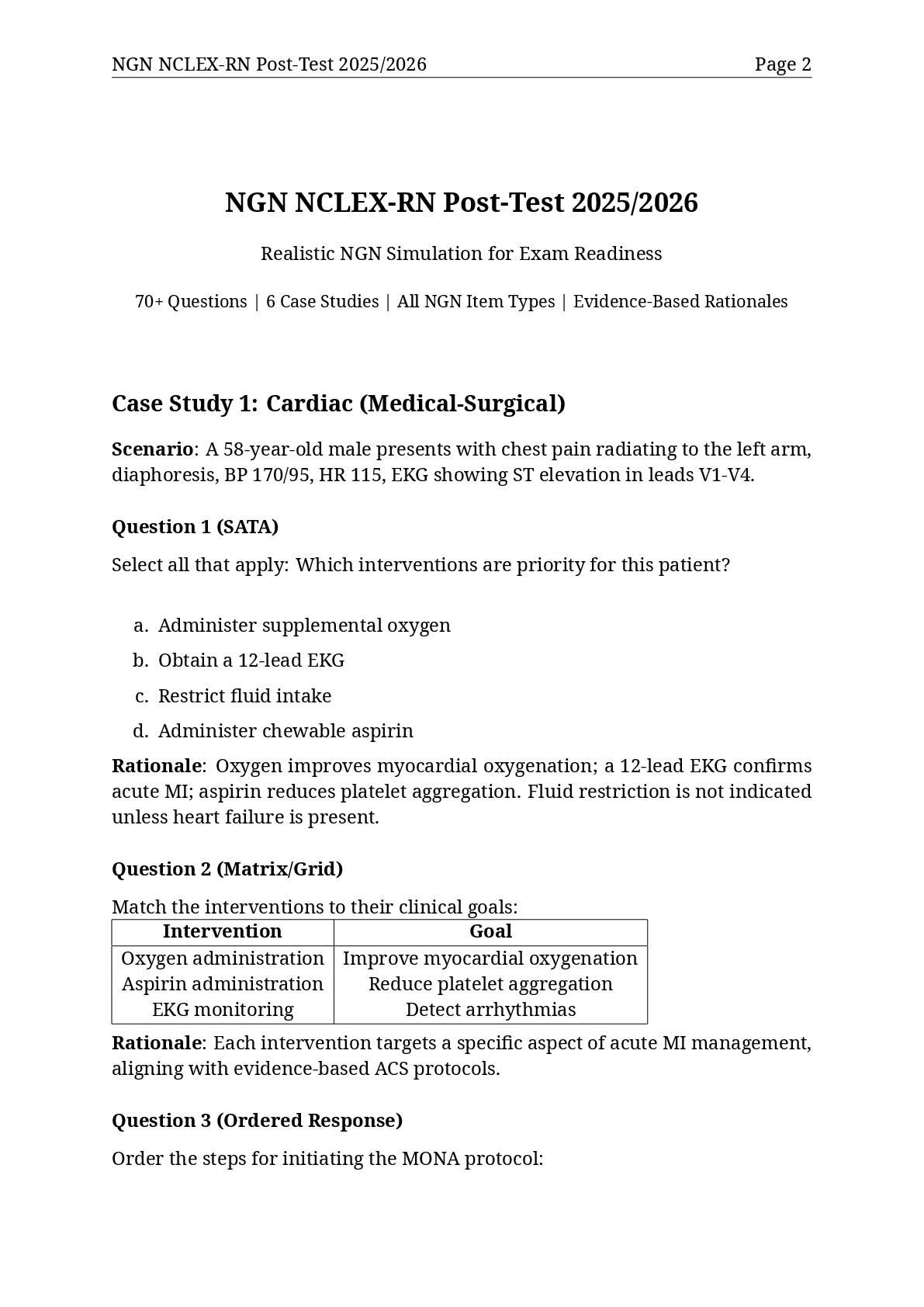
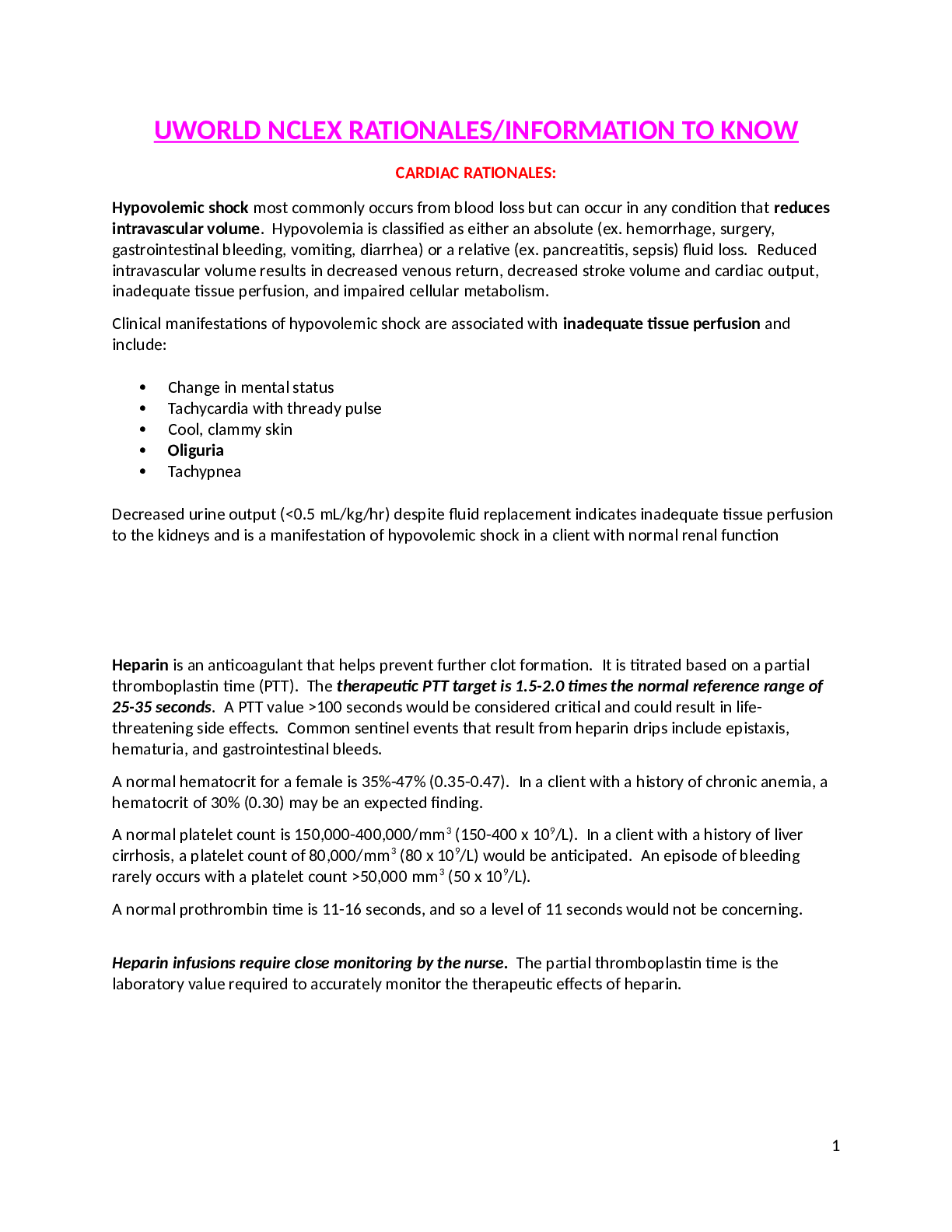
Hypovolemic shock most commonly occurs from blood loss but can occur in any condition that reduces intravascular volume. Hypovolemia is classified as either an absolute (ex. hemorrhage, surgery, gastrointestinal bleeding, vomiting, diarrhea) or a relative (ex. pancreatitis, sepsis) fluid loss. Reduced intravascular volume results in decreased venous return, decreased stroke volume and cardiac output, inadequate tissue perfusion, and impaired cellular metabolism.
Clinical manifestations of hypovolemic shock are associated with inadequate tissue perfusion and include:
• Change in mental status
• Tachycardia with thready pulse
• Cool, clammy skin
• Oliguria
• Tachypnea
Decreased urine output (<0.5 mL/kg/hr) despite fluid replacement indicates inadequate tissue perfusion to the kidneys and is a manifestation of hypovolemic shock in a client with normal renal function
Heparin is an anticoagulant that helps prevent further clot formation. It is titrated based on a partial thromboplastin time (PTT). The therapeutic PTT target is 1.5-2.0 times the normal reference range of 25-35 seconds. A PTT value >100 seconds would be considered critical and could result in life-threatening side effects. Common sentinel events that result from heparin drips include epistaxis, hematuria, and gastrointestinal bleeds.
A normal hematocrit for a female is 35%-47% (0.35-0.47). In a client with a history of chronic anemia, a hematocrit of 30% (0.30) may be an expected finding.
A normal platelet count is 150,000-400,000/mm3 (150-400 x 109/L). In a client with a history of liver cirrhosis, a platelet count of 80,000/mm3 (80 x 109/L) would be anticipated. An episode of bleeding rarely occurs with a platelet count >50,000 mm3 (50 x 109/L).
A normal prothrombin time is 11-16 seconds, and so a level of 11 seconds would not be concerning.
Heparin infusions require close monitoring by the nurse. The partial thromboplastin time is the laboratory value required to accurately monitor the therapeutic effects of heparin.
Ventricular paced rhythms are seen in clients with ventricular pacemakers. Ventricular pacemakers typically have one lead placed in the right ventricle. The pacer spike just before the QRS complex signals electrical stimulation of the ventricle by the pacemaker lead (Option 3). The pacemaker lead depolarizes the right ventricle first, and electricity travels across the heart to depolarize the left ventricle. This atypical electrical pathway distorts and widens the QRS complex. The T wave can be seen immediately after the wide QRS complex.
Implanted permanent pacemakers are often placed in clients with symptomatic bradycardia or heart block. Demand pacemakers are the most common type of implanted permanent pacemaker. The demand pacemaker sends an electrical impulse (pacer spike) only if the pacemaker does not sense an intrinsic heartbeat occurring at the programmed threshold rate (eg, 40/min).
Ventricular paced rhythms have a pacer spike just before the QRS complex, which is usually distorted and wide. Implanted permanent pacemakers are often placed in clients with symptomatic bradycardia or heart block.
Electrical cardioversion is a treatment modality considered for A. Fib that has been unresponsive to drug therapy. A Fib (rapid, irregular atrial contractions) results in ineffective atrial kick and predisposes to thrombus formation (blood clots) in the left atrium. If a client is in A. Fib for more than 48 hours, anticoagulation therapy is needed for 3-4 weeks before cardioversion. Anticoagulation therapy is necessary as cardioversion may dislodge an atrial thrombus, putting the client at risk for a stroke or other sequelae of thromboembolism. If 4 weeks of anticoagulation is not an option, TEE must be performed prior to cardioversion.
A TEE (Transesophageal Echocardiogram) is indicated prior to cardioversion for a client who has been in AF for more than 48 hours, as cardioversion is contraindicated in the presence of an atrial thrombus.
In peripheral artery disease (PAD), the arteries of the extremities become atherosclerotic (progressive thickening and hardening due to chronic vascular damage). PAD reduces tissue perfusion and can cause ischemic pain of the lower extremities with movement or exercise (intermittent claudication). Pain with PAD can also occur at rest and manifests in the lower extremities as burning, aching, or numbness. Factors that cause chronic vascular changes and increase risk for PAD include:
• Hypertension: Vessel damage from chronically elevated vascular resistance
• Diabetes mellitus: Inflammatory vascular changes from hyperglycemia
• Hyperlipidemia: Increased plaque formation (ex. atherosclerosis)
• Smoking: Chronic vasoconstriction from nicotine inhalation
Elevated estrogen levels (ex. oral contraceptive use, pregnancy, hormone replacement therapy) make blood hypercoagulable. However, elevated estrogen levels are more likely to form thrombi in veins than in arteries due to lower venous pressure and slower blood flow (ex. venous stasis).
Unlike chronic venous insufficiency, in which vessels ineffectively return blood from the feet to the central circulation, standing is not a risk factor for PAD, as standing facilitates blood flow by gravity to the lower extremities.
In peripheral artery disease, arteries in the extremities become atherosclerotic (progressive thickening and hardening due to chronic damage). Peripheral tissue perfusion is impaired, causing pain with exercise (ex. intermittent claudication) and at rest. Risk factors include hypertension, diabetes mellitus, hyperlipidemia, and smoking.
Endovascular abdominal aortic aneurysm repair is a minimally invasive procedure that involves the placement of a sutureless aortic graft inside the aortic aneurysm via the femoral artery. It does not require an abdominal incision. The nurse will need to monitor the puncture sites in the groin area for bleeding or hematoma formation. Peripheral pulses should be palpated and monitored frequently in the early post-op period and routinely afterward. Renal artery occlusion can occur due to graft migration or thrombosis so careful monitoring of urine output and kidney function should be part of nursing care.
NO abdominal incision is required in endovascular repair.
Chest tubes are NOT required in endovascular repair.
The nurse needs to monitor groin puncture sites, peripheral pulses, urine output, and kidney function in the client who has had minimally invasive endovascular repair of an abdominal aneurysm.
The client is experiencing failure to capture from the permanent pacemaker with subsequent bradycardia and hypotension. Failure to capture appears on the cardiac monitor as pacemaker spikes that are not followed by QRS complexes. Pacemaker malfunction may be caused by a failing battery, malpositioned lead wires, or fibrosis at the tip of lead wire(s) preventing adequate voltage for depolarization.
This client is symptomatic (ex. hypotension, dizziness) from insufficient perfusion. The nurse's priority is to use transcutaneous pacemaker pads to normalize the heart rate, stabilize blood pressure, and adequately perfuse organs until the permanent pacemaker is repaired or replaced (Option 3). Administer analgesia and/or sedation as prescribed as transcutaneous pacing is very uncomfortable for the client.
Atropine is administered to clients with symptomatic bradycardia; however, this client's symptoms are caused by failure to capture. Therefore, obtaining capture via transcutaneous pacing should resolve the client's symptoms.
Dopamine is an inotrope used to treat hypotension due to bradycardia. This client is bradycardic and hypotensive due to failure to capture. If hypotension persists after transcutaneous pacing is initiated, an inotrope may be necessary.
The health care provider needs to be notified, but the nurse should first use the transcutaneous pacemaker to stabilize the client.
Signs and symptoms of a failing pacemaker include failure to capture (pacer spikes without associated QRS complexes) with bradycardia and hypotension. The nurse should use a transcutaneous pacemaker to stabilize the client until the internal pacemaker can be repaired or replaced
Mitral valve regurgitation is the result of a disrupted papillary muscle(s) or ruptured chordae tendineae, allowing a backflow of blood from the left ventricle through the mitral valve into the left atrium. This backflow can lead to dilation of the left atrium, reduced cardiac output, and pulmonary edema. Clients are often asymptomatic but are instructed to report any new symptoms indicative of heart failure (ex. dyspnea, orthopnea, weight gain, cough, fatigue). This client should be assessed first due to possible heart failure, which would require immediate intervention.
Kidney transplant recipients are on an immunosuppressant regimen to prevent rejection of the transplanted organ, which can leave them susceptible to infections such as candidiasis (thrush) of the oral cavity.
The client with a spider bite is displaying signs and symptoms of infection, and further assessment is required to evaluate for conditions such as cellulitis. This client should be called second.
Clients with hypertension who develop sinus or nasal congestion have limited options for symptom relief. Decongestants containing a vasoconstrictor (ex. pseudoephedrine) can exacerbate hypertension.
Chronic mitral valve regurgitation is often asymptomatic, but many clients eventually develop heart failure; therefore, early recognition of symptoms is a priority. Mitral regurgitation causes a backflow of blood from the left ventricle to the left atrium, resulting in pulmonary edema (ex. dyspnea, orthopnea) and decreased cardiac output (ex. fatigue). Left atrial enlargement can also result in atrial fibrillation (ex. palpitations).
Clients with an implanted permanent pacemaker should be assessed for both electrical capture of heart rhythm and mechanical capture of heart rate. In atrial pacing, pacer spikes precede P waves, whereas in ventricular pacing, pacer spikes precede QRS complexes. Pacing spikes should be immediately followed by their appropriate electrical waveform, indicating electrical capture.
Checking for mechanical capture is essential to ensure that the electrical activity of the heart corresponds to a pulsatile rhythm. The best method for checking for a pulsatile rhythm is to assess a central pulse (ex. auscultation of apical, palpation of femoral). This rate should be compared to the electrical rate displayed on the cardiac monitor to assess for pulse deficit.
Blood pressure is an important assessment relating to cardiac output and organ perfusion, but it does not determine if the client's pacemaker is capturing the mechanical activity of the heart.
A 12-lead ECG does not assess mechanical capture of cardiac activity via the client's pacemaker.
Peripheral pulses (ex. radial, pedal, popliteal) are not the best indicators of mechanical action of the heart. Peripheral vasculature may have anatomical changes that impair pulse quality, leading to false perception of a pulse deficit.
For clients with a newly implanted permanent pacemaker, the nurse should assess for electrical capture of heart rhythm (ex. ECG) and mechanical capture of heart rate (ex. pulse). A central pulse (ex. auscultation of apical, palpation of femoral) should be assessed to determine mechanical capture
Acute pericarditis is inflammation of the membranous sac (pericardium) surrounding the exterior of the heart, which can cause an increase in the amount of fluid in the pericardium (ex. pericardial effusion). If pericardial effusions accumulate rapidly or are very large, they may compress the heart, altering the mechanics of the cardiac cycle (ex. cardiac tamponade). Cardiac tamponade decreases atrioventricular filling and impairs the heart's ability to contract and eject blood; it is life-threatening without prompt recognition and treatment.
Clinical features of cardiac tamponade include hypotension or narrow pulse pressure, muffled heart sounds, and neck vein distension (Beck triad). In addition, pulsus paradoxus (ie, systolic blood pressure decrease >10 mm Hg during inhalation), chest pain, tachypnea, and tachycardia may be present.
Cardiac tamponade is a possible complication of acute pericarditis that impairs cardiac output and is life-threatening without immediate intervention. Clinical features of cardiac tamponade include hypotension, muffled heart sounds, and neck vein distension (Beck triad).
Peripheral artery disease (PAD [previously called peripheral vascular disease]) refers to arteries that have thickened, have lost elasticity due to calcification of the artery walls, and are narrowed by atherosclerotic plaques (made up of fat and fibrin). Pain due to decreased blood flow is the most common symptom of PAD. Cramping pain in the muscles of the legs during exercise, known as intermittent claudication, is usually relieved with rest. However, with critical arterial narrowing, pain can be present at rest and is typically described as "burning pain" that is worsened by elevating the legs and improved when the legs are dependent. Skin becomes cool, dry, shiny, and hairless (due to lack of oxygen). Ulcers and gangrene occur usually at the most distal part of the body, where circulation is poorest. Clients should be advised that a progressive walking program will aid the development of collateral circulation.
Chronic venous insufficiency refers to inadequate venous blood return to the heart. Too much venous blood remains in the lower legs, and venous pressure increases. This increased venous pressure inhibits arterial blood flow to the area, resulting in inadequate supply of oxygen and nutrients to area cells and the development of stasis ulcers, which are typically found around the medial side of the ankle. By the end of the day or after prolonged standing, the legs become edematous with dull pain due to venous engorgement. The skin of the lower leg becomes thick with a brown pigmentation.
The pain of peripheral artery disease is arterial in nature and results from decreased blood flow to the legs. It is made worse with leg elevation. Arterial ulcers are formed at the most distal end of the body. Venous ulcers form over the medial malleolus, and compression bandaging is needed to reduce the pressure
***********************************************CONTINUED*************************************************
[Show More]





.png)