*NURSING > QUESTIONS & ANSWERS > Neuro-Senses-Onco-Ortho-Copy.docx mostly selected exam questions questions and answers solution (All)
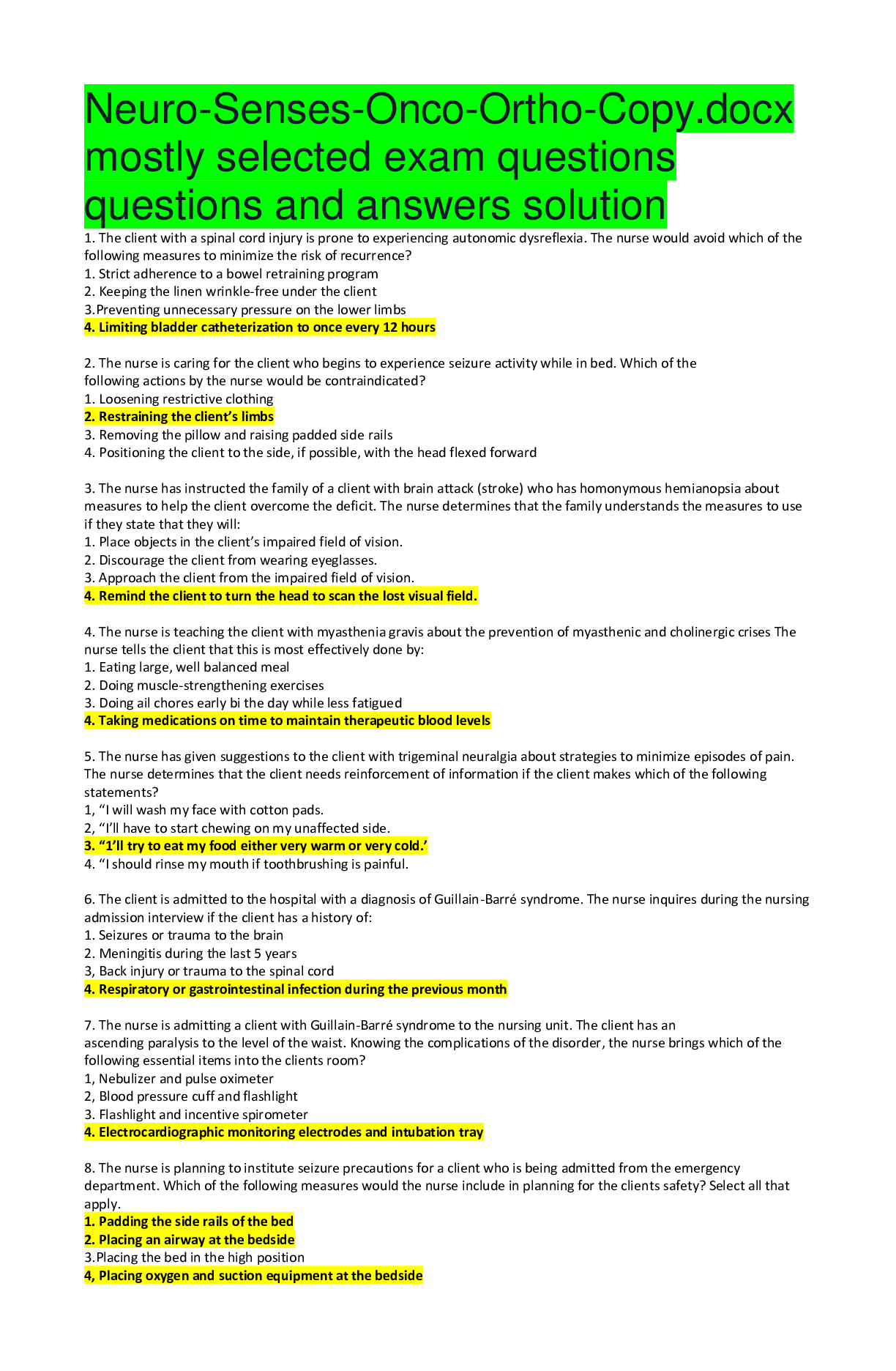
Neuro-Senses-Onco-Ortho-Copy.docx mostly selected exam questions questions and answers solution
Document Content and Description Below
Neuro-Senses-Onco-Ortho-Copy.docx mostly selected exam questions questions and answers solution 1. The client with a spinal cord injury is prone to experiencing autonomic dysreflexia. The nurse woul... d avoid which of the following measures to minimize the risk of recurrence? 1. Strict adherence to a bowel retraining program 2. Keeping the linen wrinkle-free under the client 3.Preventing unnecessary pressure on the lower limbs 4. Limiting bladder catheterization to once every 12 hours 2. The nurse is caring for the client who begins to experience seizure activity while in bed. Which of the following actions by the nurse would be contraindicated? 1. Loosening restrictive clothing 2. Restraining the client’s limbs 3. Removing the pillow and raising padded side rails 4. Positioning the client to the side, if possible, with the head flexed forward 3. The nurse has instructed the family of a client with brain attack (stroke) who has homonymous hemianopsia about measures to help the client overcome the deficit. The nurse determines that the family understands the measures to use if they state that they will: 1. Place objects in the client’s impaired field of vision. 2. Discourage the client from wearing eyeglasses. 3. Approach the client from the impaired field of vision. 4. Remind the client to turn the head to scan the lost visual field. 4. The nurse is teaching the client with myasthenia gravis about the prevention of myasthenic and cholinergic crises The nurse tells the client that this is most effectively done by: 1. Eating large, well balanced meal 2. Doing muscle-strengthening exercises 3. Doing ail chores early bi the day while less fatigued 4. Taking medications on time to maintain therapeutic blood levels 5. The nurse has given suggestions to the client with trigeminal neuralgia about strategies to minimize episodes of pain. The nurse determines that the client needs reinforcement of information if the client makes which of the following statements? 1, “I will wash my face with cotton pads. 2, “I’ll have to start chewing on my unaffected side. 3. “1’ll try to eat my food either very warm or very cold.’ 4. “I should rinse my mouth if toothbrushing is painful. 6. The client is admitted to the hospital with a diagnosis of Guillain-Barré syndrome. The nurse inquires during the nursing admission interview if the client has a history of: 1. Seizures or trauma to the brain 2. Meningitis during the last 5 years 3, Back injury or trauma to the spinal cord 4. Respiratory or gastrointestinal infection during the previous month 7. The nurse is admitting a client with Guillain-Barré syndrome to the nursing unit. The client has an ascending paralysis to the level of the waist. Knowing the complications of the disorder, the nurse brings which of the following essential items into the clients room? 1, Nebulizer and pulse oximeter 2, Blood pressure cuff and flashlight 3. Flashlight and incentive spirometer 4. Electrocardiographic monitoring electrodes and intubation tray 8. The nurse is planning to institute seizure precautions for a client who is being admitted from the emergency department. Which of the following measures would the nurse include in planning for the clients safety? Select all that apply. 1. Padding the side rails of the bed 2. Placing an airway at the bedside 3.Placing the bed in the high position 4, Placing oxygen and suction equipment at the bedside 5.Putting a padded tongue blade at the head of the bed 6. Having intravenous equipment ready for insertion of an intravenous catheter 9. An unconscious client with multiple injuries ar¬rives in the emergency room. Which nursing intervention receives the highest priority? 1. Establishing an airway. 2. Replacing blood loss. 3. Stopping bleeding from open wounds. 4. Checking for a neck fracture. 10. A client is at risk for increased intracranial pres¬sure (ICP). Which of the following would be the priority for the nurse to monitor? 1. Unequal pupil size. 2. Decreasing systolic blood pressure. 3. Tachycardia. 4. Decreasing body temperature. 11. A client has signs of increased ICP. Which of the following is an early indicator of deterioration in the client's condition? 1. Widening pulse pressure. 2. Decrease in the pulse rate. 3. Dilated, fixed pupil. 4. Decrease in level of consciousness. 12. The client has a sustained ICP of 20 mm Hg. Which client position would be most appropriate? 1. The head of the bed elevated 30 to 45 degrees. 2. Trendelenburg's position. 3. Left Sim's position. 4. The head elevated on two pillows. 13. The nurse administers mannitol (Osmitrol) to the client with increased ICP. Which parameter requires close monitoring? 1. Muscle relaxation. 2. Intake and output. 3. Widening of the pulse pressure. 4. Pupil dilation. 14. Which activity would the nurse encourage the client to avoid when there is a risk for increased ICP? 1. Deep breathing. 2. Turning. 3. Coughing. 4. Passive range-of-motion exercises. 15. Which of the following describes decerebrate pos¬turing? 1. Internal rotation and adduction of arms with flexion of elbows, wrists, and fingers. 2. Back hunched over, rigid flexion of all four ex¬tremities with supination of arms and plantar flexion of feet. 3. Supination of arms, dorsiflexion of the feet. 4. Back arched, rigid extension of all four, extremi¬ties. 16. In planning the care for a client who has had a posterior fossa (infratentorial) craniotomy, which of the following is contraindicated when positioning the client? 1. Keeping the client flat on one side or the other. 2. Elevating the head of the bed to 30 degrees. 3. Log rolling or turning as a unit when turning. 4. Keeping the neck in a neutral position. 17. Which of the following is contraindicated for a client with seizure precautions? 1. Encouraging him to perform his own personal hygiene. 2. Allowing him to wear his own clothing. 3. Assessing oral temperature with a glass ther¬mometer. 4. Encouraging him to be out of bed. 18. For breakfast on the morning a client is to have an electroencephalogram (EEG), the client is served a soft-boiled egg, toast with butter and marmalade, orange juice, and coffee. Which of the following would the nurse do? 1. Remove all the food. 2. Remove the coffee. 3. Remove the toast, butter, and marmalade only. 4. Substitute vegetable juice for the orange juice. 19. Which clinical manifestation does the nurse as¬sess as a typical reaction to long-term phenytoin sodi¬um (Dilantin) therapy? 1. Weight gain. 2. Insomnia. 3. Excessive growth of gum tissue. 4. Deteriorating eyesight. 20. During the first 24 hours after thrombolytic treat¬ment for an ischemic CVA, the primary goal is to ¬ control the client's 1. pulse. 2. respirations. 3. blood pressure. 4. temperature. 21. What is a priority nursing assessment in the first 24 hours after admission of the client with a thrombotic CVA? 1. Cholesterol level. 2. Pupil size and pupillary response. 3. Bowel sounds. 4. Echocardiogram. 22. Which food-related behaviors would the nurse observe in a client who has had a CVA that has left him with homonymous hemianopia? 1. Increased preference for foods high in salt. 2. Eating food on only half of the plate. 3. Forgetting the names of foods. 4. Inability to swallow liquids. 23. What is the expected outcome of thrombolytic drug therapy for CVA? 1. Increased vascular permeability. 2. Vasoconstriction. 3. Dissolved emboli. 4. Prevention of hemorrhage. 24. A nurse is performing an assessment on a client who is unconscious after sustaining a head injury. The nurse should avoid performing the oculocephalicresponse (dolls-eyes maneuver) if which condition is present in the client? 1. A cervical cord injury 2. Lumbar trauma 3.Dilated pupils 4. Altered level of consciousness 25. A nurse develops a plan of care for a client with a brain aneurysm who will be placed on aneurysm precautions. Which of the following should be included in the plan? Select all that apply 1. Allow the client to drink one cup of caffeinated coffee a day. 2. Allow the client to ambulate four times a day with assistance. 3. Place a blood pressure cuff at the client’s bedside. 4. Close the shades in the client’s room during the day. 5. Leave the lights on in the client’s room at night. 26. A nurse is developing a plan of care for a client with dysphagia following a brain attack (stroke). Which of the following should the nurse include in the plan? Select all that apply. 1. Thicken liquids. 2. Provide ample time for the client to chew and swallow. 3. Assess for the presence of a swallow reflex. 4, Place the food on the affected side of the mouth. 5. Assist the client with eating. 27. A nurse is caring for a client after a craniotomy and monitors the client for signs of increased intracranial pressure (ICP). Which of the following, if noted in the client, would indicate an early sign of increased ICP? 1. Confusion 2. Bradycardia 3. Widening of pulse pressure 4. Hyperthermia 28. An emergency department nurse is caring for a client with a suspected diagnosis of meningitis. The nurse will prepare the client for which of the following tests to confirm the diagnosis? 1. CT Scan 2. Lumbar Puncture 3. Blood Culture 4. White Blood Cell count 29. A thymectomy accomplished via a median sternotomy approach is performed in a client with a diagnosis of myasthenia gravis. The nurse has developed a postoperative plan of care for the client that includes which of the following? 1. Avoid administering pain medication Lo prevent respiratory depression. 2. Monitor the chest tube drainage. 3. Maintain intravenous infusion of lactated Ringer’s solution. 4. Restrict visitors for 24 hours postoperatively. 30. A home care nurse is visiting a client with a diagnosis of Parkinson’s disease. The client is taking benztropinemesylate (Cogentin) orally daily. The nurse provides information to the spouse regarding the side effects of this medication and tells the spouse to report which side effect if it occurs? 1. Inability to urinate 2. Decreased appetite 3.Shuffling gait 4. Irregular bowel movements 31. A client arrives in the hospital emergency department with a closed head injury to the right side of the head caused by an assault with a baseball bat. The nurse assesses the client neurologically. Looking primarily for motor response deficits that involve: 1. The left side of the body 2. The right side of the body 3.Both sides of the body equally 4. Cranial nerves only, such as speech and pupillary response 32. A nurse is caring for a client who is on bed rest as part of aneurysm precautions. The nurse would avoid doing which of the following when giving respiratory care to this client to prevent atelectasis? 1. Reposition gently side to side every 2 hours. 2. Assist with incentive spirometer. 3. Encourage hourly coughing. 4. Encourage hourly deep breathing. 33. A nurse is assisting with caloric testing of the oculovestibular reflex in an unconscious client. Cold water is injected into the left auditory canal. The client exhibits eye conjugate movements toward the left, followed by eye movement back to midline. The nurse understands that this indicates the client has: 1. Brain death 2. A cerebral lesion 3.A temporal lesion 4. An intact brainstem 34. A nurse is assessing a client’s extraocular eye movements as part of the neurologic examination. The nurse is assessing which cranial nerves? Select all that apply. 1. Cranial nerve II 2. Cranial nerve III 3.Cranial nerve IV 4.Cranial nerve V 5.Cranial nerve VI 6. Cranial nerve VIII 35. A nurse is assessing a client diagnosed with multiple sclerosis (MS). Which symptom does the nurse expect to find? 1. Vision changes 2. Absent deep tendon reflexes 3.Tremors at rest 4. Flaccid muscles 36. A client has a cerebral aneurysm. The physician orders hydralazine (Apresoline), 15 mg I.V., every 4 hours as needed to keep the systolic blood pressure under 140 mm Hg. The label on the hydralazine vial reads “hydralazine 20 mg/ml.” To administer the correct dose, how many milliliters of medication should the nurse draw up in the syringe? Record your answer using two decimal places. Answer 0.75ml 37. A client is admitted to the hospital after sustaining a closed head injury in a skiing accident. The physician ordered neurologic assessments to be performed every 2 hours. The client’s neurologic assessments have been unchanged since admission, and the client is complaining of a headache. Which intervention by the nurse is best? 1. Administer codeine 30 mg by mouth as ordered and continue neurologic assessments as ordered. 2. Assess the client’s neurologic status for subtle changes, administer acetaminophen, and then reassess the client in 30 minutes. 3. Reassure the client that a headache is expected and will go away without treatment. 4. Notify the physician; a headache is an early sign of worsening neurologic status. 38. A registered nurse (RN) and licensed practical nurse (LPN) are administering medications on the neurologic floor. The LPN prepares to administer phenytoin (Dilantin) to a client with a history of seizures. As the LPN walks into the room, she hands the medication to a nursing assistant. The LPN asks the nursing assistant to give the client the medication after completing the client’s morning care. What should the registered nurse do? 1. Remind the LPN that she must administer the medications herself. 2. Do nothing because the client has been taking the medication for a long time. 3. Allow the nursing assistant to administer this dose and tell the LPN later that it’s her responsibility to administer the medication. 4. Take the medication from the nursing assistant and administer it. 39. A nurse caring for a group of clients on the neurological floor is working with a nursing assistant and a licensed practical nurse (LPN). Their client care assignment consists of a client with new-onset seizure activity, a client with Alzheimer’s disease, and a client who experienced a stroke. While administering medications, the registered nurse receives a call from the intensive care unit (ICU), saying a client who underwent a craniotomy 24 hours ago must be transferred to make room for a new admission. The ancillary staff is providing morning care and assisting clients with breakfast. How should the nurse direct the staff to facilitate a timely transfer? 1. Tell the ICU they have to wait to transfer the client because everyone is too busy to accept the client. 2. Ask the nursing assistant to finish providing care to the clients and the LPN to administer the remaining medications so the registered nurse can accept the client from the ICU. 3. Administer the medications quickly and ask the nursing assistant and LPN to finish providing care for the clients. 4. Notify the supervisor that the client care assignment is unsafe with the addition of the new client, and insist she assist with the assignment. 40. During morning care, a nurse notes that a client who’s had a spinal cord injury has experienced a change in level of consciousness and isn’t answering questions appropriately. The nurse checks the client’s vital signs and measures his blood pressure at 180/110 mm Hg and his heart rate at 125 beats/minute. She determines that the client may be experiencing dysreflexia. What other assessments should the nurse make? Select all that apply. 1. Most recent bowel movement 2. Urine output 3. Percentage of meals taken 4. Medications ordered for hypertension 5. Pain level 41. After striking his head on a tree while falling from a ladder, a client is admitted to the emergency department. He’s unconscious and his pupils are nonreactive. Which intervention should the nurse question? 1. Giving him a barbiturate 2. Placing him on mechanical ventilation 3.Performing a lumbar puncture 4. Elevating the head of his bed 42. A nurse is teaching a client who was recently diagnosed with myasthenia gravis. Which statement should the nurse include in her teaching? 1. “You’ll continue to experience progressive muscle weakness and sensory deficits.” 2. “You’ll need to take edrophonium (Tensilon) to treat the disease.” 3. “The disease is a disorder of motor and sensory dysfunction.” 4. “This disease doesn’t cause sensory impairment.” 43. A client with respiratory complications of multiple sclerosis (MS) is admitted to the medical-surgical unit. Which equipment is most important for the nurse to keep at the client’s bedside? 1. Sphygmomanometer 2. Padded tongue blade 3. Nasal cannula and oxygen 4. Suction machine with catheters 44. For a client who has had a stroke, which intervention can help prevent contracture in the lower legs? 1. Putting slippers on the client’s feet 2. Crossing the client’s ankles every 2 hours 3. Placing hand rolls on the balls of each foot 4. Attaching braces or splints to each foot and leg RATIONALE: Attaching braces or splints to each foot and leg prevents footdrop (a lower leg contracture) by supporting the feet in proper alignment. Putting slippers on the client’s feet can’t prevent footdrop because slippers are too soft to support the ankle joints. Crossing the ankles every 2 hours is contraindicated because it can cause excess pressure and damage veins, promoting thrombus formation. Placing hand rolls on the balls of each foot doesn’t prevent contractures because hand rolls are too soft to support and hold the feet in proper alignment. 45. A nurse received a shift report on four clients. Which should she assess first? 1. An older adult returning to the unit after having a carotid endarterectomy 2. An older adult admitted 3 hours earlier for observation because of possible transient ischemic attack 3. A middle-age adult who had a rhizotomy 2 days earlier 4. A young adult admitted for observation and management of migraine headaches 46. Three hours after injuring the spinal cord at the C6 level, a client receives high doses of methylprednisolone sodium succinate (Solu-Medrol) to suppress breakdown of the neurologic tissue membrane at the injury site. To help prevent adverse effects of this drug, the nurse expects the physician to order: 1. naloxone (Narcan). 2. famotidine (Pepcid). 3. nitroglycerin (N,tro-8id). 4. atracurium (Tracrium). 47. Friends come to visit a client admitted with new-onset ischemic stroke. The stroke has caused aphasia and right-sided weakness. The client has an advance directive and an identified health care power of attorney. The friends ask the nurse about the client’s condition. How should the nurse respond? 1. “I’m not at liberty to discuss his condition with you. You’ll have to speak to his power of attorney if you’d like information.” 2. “I can’t tell you anything about his condition.” 3. “You’ll have to ask him how he is feeling.” 4. “He is unable to communicate as a result of a stroke, so I’ll tell you what I think he’d want you to know.” 48. A client was seen and treated in the hospital emergency department for treatment of a concussion. The nurse determines that the family needs reinforcement of the discharge instructions if they verbalize to call the physician for which client sign or symptom? 1 Difficulty speaking 2.Difficulty awakening 3.Vomiting 4. Minor headache 49. A client with myasthenia gravis arrives at the hospital emergency department in suspected crisis. The physician plans to administer edrophonium (Tensilon) to differentiate between myasthenic and cholinergic crises. The nurse prepares to administer which medication as prescribed if the client is in cholinergic crisis? 1. Atropine sulfate 2. Morphine sulfate 3. Pyridostigmine bromide (Mestinon) 4. Protamine sulfate 50. A nurse is preparing to care for a client who had a supratentorial craniotomy. The nurse plans to place the client in which position? 1. Prone 2. Supine 3. Side lying 4. Semi fowlers Special Senses 1. After an eye examination, a client is diagnosed with open-angle glaucoma. The physician orders pilocarpine ophthalmic solution (Pilocar), 0.25% gtti, OU q.i.d. Based on this prescription, the nurse should teach the client or a family member to administer the drug by: 1. instilling one drop of pdocarpine 0.25% into both eyes daily. 2. instilling one drop of pilocarpine 0.25% into both eyes four times daily. 3. instilling one drop of pdocarpine 0.25% into the right eye daily. 4. instilling one drop of pdocarpine 0.25% into the left eye four times daily. 2. A client has just been diagnosed with early glaucoma. During a teaching session, the nurse should: 1. provide instructions on eye patching. 2. assess the client’s visual acuity. 1. provide instructions on eye patching. 2. assess the client’s visual acuity. 3. demonstrate eye drop instillation. 4. teach about intraocular lens cleaning. 3. The nurse is performing an admission assessment on a client with a diagnosis of detached retina. Which of the following is associated with this eye disorder? 1. Total loss of vision 2. Pain in the affected eye 3.A yellow discoloration of the sclera 4. A sense of a curtain falling across the field of vision 4. A woman was working in her garden. She accidentally sprayed insecticide into her right eye. She calls the emergency department frantic and screaming for help. The nurse should instruct the woman to take which immediate action? 1. Call the physician. 2. Irrigate the eyes with water. 3. Come to the emergency room. 4. Irrigate the eyes with diluted hydrogen peroxide. 5. The nurse is preparing a teaching plan for a client who is undergoing cataract extraction with intraocular implantation. Which home care measures will the nurse include in the plan? Select all that apply. 1. Avoid activities that require bending over. 2. Contact the surgeon if eye scratchiness occurs. 3. Place an eye shield on the surgical eye at bedtime. 4. Episodes of sudden severe pain in the eye are expected. 5. Contact the surgeon if a decrease in visual acuity occurs, 6. Take acetaminophen (Tylenol) for minor eye discomfort. 6. Betaxolol hydrochloride (Betoptic) eye drops have been prescribed for the client with glaucoma. Which of the following nursing actions is most appropriate related to monitoring for the side effects of this medication? 1. Monitoring temperature 2. Monitoring blood pressure 3, Assessing peripheral pulses 4. Assessing blood glucose level 7. In preparation for cataract surgery. the nurse is to administer cyclopentolate (Cyclogyl) eye drops. The nurse administers the eye drops, knowing that the purpose of this medication is to: 1. Produce miosis of the operative eye. 2. Dilate the pupil of the operative eye. 3. Provide lubrication to the operative eye. 4. Constrict the pupil of the operative eye. 8. A client asks, "What does the lens of my eye do?" The nurse should explain that the lens of the eye 1. produces aqueous humor. 2. holds the rods and cones. 3. focuses light rays onto the retina. 4. regulates the amount of light entering the eye. 9. A client is admitted to outpatient surgery for a cataract extraction on the right eye. The client asks the nurse, "What causes cataracts in old people?" Which of the following statements should form the basis for the nurse's response? Cataracts most commonly 1. are a result of chronic systemic disease. 2. are a result of the aging process. 3. are a result of injuries sustained early in life. 4. are a result of the prolonged use of drugs. 10. A client with a cataract would most likely com¬plain of which symptoms? 1. Halos and rainbows around lights. 2. Eye pain and irritation that worsens at night. 3. Blurred and hazy vision. 4. Eye strain and headache when doing close work. 11. A client is admitted through the emergency de¬partment with a diagnosis of detached retina in the right eye. As the nurse completes the admission history, the client reports that before the physician patched his eye, he saw many spots, or "floaters." The nurse should explain to the client that these spots were caused by: 1. pieces of the retina floating in the eye. 2. blood cells released into the eye by the detachment. 3. contamination of the aqueous humor. 4. spasms of the retinal blood vessels traumatized by the detachment. 12. Scleral buckling, a procedure used to treat retinal detachment, involves 1. removing the torn segment of the retina and stitching down the remaining segment. 2. replacing the torn segment of the retina with a strip of retina from a donor. 3. stitching the retina firmly to the optic nerve to give it support. 4. creating a splint to hold the retina together until a scar can form and seal off the tear. 13. The client who has been treated for chronic open-angle glaucoma (COAG) for 5 years asks the clinic nurse,"How does glaucoma damage my eyesight?" The nurse's reply should be based on theknowledge that COAG 1. results from chronic eye inflammation. 2. causes increased intraocular pressure. 3. leads to detachment of the retina. 4. is caused by decreased blood flow to the retina. 14. Which of the following signs or symptoms is most commonly experienced by clients with COAG? 1. Eye pain. 2. Excessive lacrimation. 3. Colored light flashes. 4. Decreasing peripheral vision. 15. Miotics are frequently used in the treatment of glaucoma. The nurse should understand that miotics work by 1. paralyzing ciliary muscles. 2. constricting intraocular vessels. 3. constricting the pupil. 4. relaxing ciliary muscles. 16. The client with glaucoma is scheduled for a minor surgical procedure. Which of the following orders would require clarification or correction before the nurse carries it out? 1. Administer morphine sulfate. 2. Administer atropine sulfate. 3. Teach deep breathing exercises. 4. Teach leg exercises. 17. Which of the following clinical manifestations would the nurse associate with acute angle-closure glaucoma? 1. Gradual loss of central vision. 2. Acute light sensitivity. 3. Loss of color vision. 4. Sudden eye pain. 18. The best method to remove cerumen from a client's ear involves 1. inserting a cotton-tipped applicator into the ex¬ternal canal. 2. irrigating the ear gently. 3. using aural suction. 4. using a cerumen curette. 19. A 50-year-old man has been taking aspirin regu¬larly for 6 months to prevent a heart attack. He informs the nurse that he has noticed a constant "ringing" in both ears. How should the nurse respond to the client's comment? 1. Tell the client that tinnitus is associated with the aging process. 2. Inform the client he needs a Weber test done. 3. Schedule the client for audiometric testing. 4. Inform the client that the "ringing" may be re¬lated to the aspirin he has been taking for his heart. 20. The classic triad of symptoms associated with Meniere's disease is vertigo, tinnitus, and 1. headache. 2. otitis media. 3. fluctuating hearing loss. 4. vomiting. Answer: 3. Meniere's disease involves the inner ear and is characterized by episodes of acute vertigo, tinnitus, and fluctuating, progressive hearing loss. The severe vertigo can lead to nausea and vomiting, but vomiting is not considered one of the classic triad of symptoms. Headache is not associated with Meniere's disease. Oti¬tis media is an inflammation of the middle ear. 21. The client with Meniere's disease is instructed to modify his diet. The nurse would explain that the most frequently recommended diet modification for Meniere's disease is 1. low sodium. 2. high protein. 3. low carbohydrate. 4. low fat. 22. Which of the following statements by the client would indicate that she understands the expected course of Meniere's disease? 1. "The disease process will gradually extend to the eyes." 2. "Control of the episodes is usually possible, but a cure is not yet available." 3. "Continued medication therapy will cure the disease." 4. "Bilateral deafness is an inevitable outcome of the disease." 23. The nurse would anticipate that all of the follow¬ing drugs may be used in the attempt to control the symptoms of Meniere's disease excep? 1. antihistamines. 2. antiemetics. 3. diuretics. 4. glucocorticoids. 24. When assessing an older adult with macular de¬generation the nurse would expect to find 1. loss of central vision. 2. loss of peripheral vision. 3. total blindness. 4. blurring of vision. 25. A client states that she was told she has sen¬sorineural hearing loss and asks the nurse what this means. The nurse's response is based on the knowledge that sensorineural hearing loss results from which of the following conditions? 1. Presence of fluid and cerumen in the external canal. 2. Sclerosis of the bones of the middle ear. 3. Damage to the cochlear or vestibulocochlear nerve. 4. Emotional disturbance resulting in a functional hearing loss. Oncology 1. The nurse is caring for a client with an internal radiation implant. When caring for the client, the nurse should observe which principle? 1. Limit the time with the client to 1 hour per shift. 2. Do not allow pregnant women into the client’s room. 3. Remove the dosimeter film badge when entering the clients room. 4. Individuals younger than 16 years old may be allowed to go in the room as long as they are 6 feet away from the client. 2. The female client who has been receiving radiation therapy for bladder cancer tells the nurse that it feels as if she is voiding through the vagina, The nurse interprets that the client may be experiencing: 1. Rupture of the bladder 2. The development of a vesicovaginal fistula 3. Extreme stress caused by the diagnosis of cancer 4. Altered perineal sensation as a side effect of radiation therapy 3. A gastrectomy is performed on a client with gastric cancer In the immediate postoperative period, the nurse notes bloody drainage from the nasogastric tube. Which of the following is the appropriate nursing intervention? 1. Notify the physician. 2. Measure abdominal girth. 3. Irrigate the nasogastric tube. 4. Continue to monitor the drainage. 4. The nurse is teaching a client about the risk factors associated with colorectal cancer. The nurse determines that further teaching related to colorectal cancer is necessary if the client identifies which of the following as an associated risk factor? 1. Age younger than 50 years 2. History of colorectal polyps 3.Family history of colorectal cancer 4. Chronic inflammatory bowel disease 5. A nurse is caring for a client who had a prostatectomy for prostate cancer. The nurse is reviewing the client’s vital signs and intake and output as documented by a nursing assistant. Which documented finding requires immediate action? 1. Blood pressure 2. Heart rate 3. Ventricular standstill 4. Temperature 6. A client tells the nurse that she has found a painless lump in her right breast during her monthly self-examination. Which assessment finding would strongly suggest that this client’s lump is cancerous? 1. Eversion of the right nipple and mobile mass 2. Non-mobile mass with irregular edges 3. Mobile mass that is soft and easily delineated 4. Non-palpable right axillary lymph nodes 7. After being seen in the oncology clinic, a client with severe bone marrow suppression is admitted to the hospital. The client’s cancer therapy consisted of radiation and chemotherapy. When developing the care plan for this client, which nursing diagnosis takes priority? 1. Risk for injury 2. Imbalanced nutrition: Less than body requirements 3. Risk for infection 4. Anxiety 8. While being prepared for a biopsy of a lump in the right breast, the patient asks the nurse what the difference is between a benign tumor and a malignant tumor. The nurse explains that a benign tumor differs from a malignant tumor in that benign tumors a. do not cause damage to adjacent tissue. b. do not spread to other tissues and organs. c. are simply an overgrowth of normal cells. d. frequently recur in the same site. 9. A patient who has been told by the health care provider that the cells in a bowel tumor are poorly differentiated asks the nurse what is meant by "poorly differentiated." Which response should the nurse make? a. "The cells in your tumor do not look very different from normal bowel cells." b. "The tumor cells have DNA that is different from your normal bowel cells." c. "Your tumor cells look more like immature fetal cells than normal bowel cells." d. "The cells in your tumor have mutated from the normal bowel cells." 10. A patient who smokes tells the nurse, "I want to have a yearly chest x-ray so that if I get cancer, it will be detected early." Which response by the nurse is most appropriate? a. "Chest x-rays do not detect cancer until tumors are already at least a half-inch in size." b. "Annual x-rays will increase your risk for cancer because of exposure to radiation." c. "Insurance companies do not authorize yearly x-rays just to detect early lung cancer." d. "Frequent x-rays damage the lungs and make them more susceptible to cancer." 11. In teaching about cancer prevention to a community group, the nurse stresses promotion of exercise, normal body weight, and low-fat diet because a. most people are willing to make these changes to avoid cancer. b. dietary fat and obesity promote growth of many types of cancer. c. people who exercise and eat healthy will make other lifestyle changes. d. obesity and lack of exercise cause cancer in susceptible people. 12. During a routine health examination, a 30-year-old patient tells the nurse about a family history of colon cancer. The nurse will plan to a. teach the patient about the need for a colonoscopy at age 50. b. ask the patient to bring in a stool specimen to test for occult blood. c. schedule a sigmoidoscopy to provide baseline data about the patient. d. have the patient ask the doctor about specific tests for colon cancer. 13. When reviewing the chart for a patient with cervical cancer, the nurse notes that the cancer is staged as Tis, N0, M0. The nurse will teach the patient that a. the cancer cells are well-differentiated. b. it is difficult to determine the original site of the cervical cancer. c. further testing is needed to determine the spread of the cancer. d. the cancer is localized to the cervix. 14. Which statement by a patient who is scheduled for a needle biopsy of the prostate indicates that the patient understands the purpose of a biopsy? a. "The biopsy will tell the doctor whether the cancer has spread to my other organs." b. "The biopsy will help the doctor decide what treatment to use for my enlarged prostate." c. "The biopsy will determine how much longer I have to live." d. "The biopsy will indicate the effect of the cancer on my life." 15. The nurse is teaching a postmenopausal patient with breast cancer about the expected outcomes of her cancer treatment. The nurse evaluates that the teaching has been effective when the patient says a. "After cancer has not recurred for 5 years, it is considered cured." b. "I will need to have follow-up examinations for many years after I have treatment before I can be considered cured." c. "Cancer is considered cured if the entire tumor is surgically removed." d. "Cancer is never considered cured, but the tumor can be controlled with surgery, chemotherapy, and radiation." 16. A patient with a large stomach tumor that is attached to the liver is scheduled to have a debulking procedure. The nurse explains that the expected outcome of this surgery is a. control of the tumor growth by removal of malignant tissue. b. promotion of better nutrition by relieving the pressure in the stomach. c. relief of pain by cutting sensory nerves in the stomach. d. reduction of the tumor burden to enhance adjuvant therapy. 17. External-beam radiation is planned for a patient with endometrial cancer. The nurse teaches the patient that an important measure to prevent complications from the effects of the radiation is to a. test all stools for the presence of blood. b. inspect the mouth and throat daily for the appearance of thrush. c. perform perianal care with sitz baths and meticulous cleaning. d. maintain a high-residue, high-fat diet. 18. Which action by a nursing assistant (NA) caring for a patient with a temporary radioactive cervical implant indicates that the RN should intervene? a. The NA places the patient's bedding in the laundry container in the hallway. b. The NA flushes the toilet once after emptying the patient's bedpan. c. The NA stands by the patient's bed for an hour talking with the patient. d. The NA gives the patient an alcohol-containing mouthwash for oral care. 19. A patient with Hodgkin's lymphoma is undergoing external radiation therapy on an outpatient basis. After 2 weeks of treatment, the patient tells the nurse, "I am so tired I can hardly get out of bed in the morning." An appropriate intervention for the nurse to plan with the patient is to a. exercise vigorously when fatigue is not as noticeable. b. consult with a psychiatrist for treatment of depression. c. establish a time to take a short walk every day. d. maintain bed rest until the treatment is completed. 20. Which information obtained by the nurse about a patient with colon cancer who is scheduled for external radiation therapy to the abdomen indicates a need for patient teaching? a. The patient swims a mile 5 days a week. b. The patient eats frequently during the day. c. The patient showers with Dove soap daily. d. The patient has a history of dental caries. 21. A patient undergoing external radiation has developed a dry desquamation of the skin in the treatment area. The nurse knows that teaching about management of the skin reaction has been effective when the patient says a. "I can use ice packs to relieve itching in the treatment area." b. "I can buy a steroid cream to use on the itching area." c. "I will expose the treatment area to a sun lamp daily." d. "I will scrub the area with warm water to remove the scales." 22. A patient with metastatic cancer of the colon experiences severe vomiting following each administration of chemotherapy. An important nursing intervention for the patient is to a. teach about the importance of nutrition during treatment. b. have the patient eat large meals when nausea is not present. c. administer prescribed antiemetics 1 hour before the treatments. d. offer dry crackers and carbonated fluids during chemotherapy. 23. When the nurse is administering a vesicant chemotherapeutic agent intravenously, an important consideration is to a. stop the infusion if swelling is observed at the site. b. infuse the medication over a short period. c. administer the chemotherapy through small-bore catheter. d. hold the medication unless a central venous line is available. 24. A chemotherapeutic agent known to cause alopecia is prescribed for a patient. To maintain the patient's self-esteem, the nurse plans to a. suggest that the patient limit social contacts until regrowth of the hair occurs. b. encourage the patient to purchase a wig or hat and wear it once hair loss begins. c. have the patient wash the hair gently with a mild shampoo to minimize hair loss. d. inform the patient that hair loss will not be permanent and that the hair will grow back. 25. A patient with ovarian cancer tells the nurse, "I don't think my husband cares about me anymore. He rarely visits me." On one occasion when the husband was present, he told the nurse he just could not stand to see his wife so ill and never knew what to say to her. An appropriate nursing diagnosis in this situation is a. compromised family coping related to disruption in lifestyle and role changes. b. impaired home maintenance related to perceived role changes. c. risk for caregiver role strain related to burdens of caregiving responsibilities. d. interrupted family processes related to effect of illness on family members. 26. A patient receiving head and neck radiation and systemic chemotherapy has ulcerations over the oral mucosa and tongue and thick, ropey saliva. An appropriate intervention for the nurse to teach the patient is to a. remove food debris from the teeth and oral mucosa with a stiff toothbrush. b. use cotton-tipped applicators dipped in hydrogen peroxide to clean the teeth. c. gargle and rinse the mouth several times a day with an antiseptic mouthwash. d. rinse the mouth before and after each meal and at bedtime with a saline solution. 27. A 40-year-old divorced mother of four school-age children is hospitalized with metastatic cancer of the ovary. The nurse finds the patient crying, and she tells the nurse that she does not know what will happen to her children when she dies. The most appropriate response by the nurse is a. "Why don't we talk about the options you have for the care of your children?" b. "Many patients with cancer live for a long time, so there is time to plan for your children." c. "For now you need to concentrate on getting well, not worry about your children." d. "Perhaps your ex-husband will take the children when you can't care for them." 28. Which information noted by the nurse reviewing the laboratory results of a patient who is receiving chemotherapy is most important to report to the health care provider? a. Hemoglobin of 10 g/L b. WBC count of 1700/µl c. Platelets of 65,000/µl d. Serum creatinine level of 1.2 mg/dl 29. After the nurse has explained the purpose of and schedule for chemotherapy to a 23-year-old patient who recently received a diagnosis of acute leukemia, the patient asks the nurse to repeat the information. Based on this assessment, which nursing diagnosis is most likely for the patient? a. Acute confusion related to infiltration of leukemia cells into the central nervous system b. Knowledge deficit: chemotherapy related to a lack of interest in learning about treatment c. Risk for ineffective health maintenance related to anxiety about new leukemia diagnosis d. Risk for ineffective adherence to treatment related to denial of need for chemotherapy 30. A hospitalized patient who has received chemotherapy for leukemia develops neutropenia. Which observation by the RN caring for the patient indicates that the nurse should take action? a. The patient's visitors bring in some fresh peaches from home. b. The patient ambulates several times a day in the room. c. The patient uses soap and shampoo to shower every other day. d. The patient cleans with a warm washcloth after having a stool. 31. Which action by a nursing assistant (NA) when caring for a patient who is pancytopenic indicates a need for the nurse to intervene? a. The NA assists the patient to use dental floss after eating. b. The NA makes an oral rinse using 1 teaspoon of salt in a liter of water. c. The NA adds baking soda to the patient's saline oral rinses. d. The NA puts fluoride toothpaste on the patient's toothbrush. 32. A with tumor lysis syndrome (TLS) is taking allopurinol (Xyloprim). Which laboratory value should the nurse monitor to determine the effectiveness of the medication? a. Blood urea nitrogen (BUN) b. Serum phosphate c. Serum potassium d. Uric acid level 33. When assessing a patient's needs for psychologic support after the patient has been diagnosed with stage I cancer of the colon, which question by the nurse will provide the most information? a. "Can you tell me what has been helpful to you in the past when coping with stressful events?" b. "How long ago were you diagnosed with this cancer?" c. "Are you familiar with the stages of emotional adjustment to a diagnosis like cancer of the colon?" d. "How do you feel about having a possibly terminal illness?" 34. A client who’s receiving chemotherapy for breast cancer develops myelosuppression. Which instructions should the nurse include in the client’s discharge teaching plan? Select all that apply. 1. Avoid people who have recently received attenuated vaccines. 2. Avoid activities that may cause bleeding. 3. Wash hands frequently. 4. Increase intake of fresh fruits and vegetables. 5. Avoid crowded places such as shopping malls. 6. Treat a sore throat with over-the-counter (OTC) products. 35. A client suspected of having colorectal cancer requires which diagnostic study to confirm the diagnosis? 1. Stool Hematest 2. Carcinoembryonic antigen (CEA) 3. Sigmoidoscopy 4. Abdominal computed tomography (CT) scan 36. To combat the most common adverse effects of chemotherapy, a nurse should administer an: 1. antiemetic. 2. antimetabolite. 3. antibiotic. 4. anticoagulant. 37. Which statement by a client undergoing external radiation therapy indicates the need for further teaching? 1. “I’ll wash my skin with mild soap and water only.” 2. “I’ll not use my heating pad during my treatment.” 3. “I’ll wear protective clothing when outside.” 4. “I’m worried I’ll expose my family members to radiation.” 38. A client with metastatic ovarian cancer is ordered cisplatin (Platinol). Before administering the first dose, the nurse reviews the client’s medication history for drugs that may interact with cisplatin. Which drug may cause significant interactions when given concomitantly with cisplatin? 1. Erythromycin 2. A tetracycline 3.A cephalosporin 4. An aminoglycoside 39. A client receiving external radiation to the left thorax to treat lung cancer has a nursing diagnosis of Risk for impaired skin integrity. Which intervention should be part of this client’s care plan? 1. Avoiding using soap on the irradiated areas 2. Applying talcum powder to the irradiated areas daily after bathing 3.Wearing a lead apron during direct contact with the client 4. Removing thoracic skin markings after each radiation treatment 40. A client is receiving chemotherapy to treat breast cancer. Which assessment finding indicates a chemotherapy-induced complication? 1. Urine output of 400 ml in 8 hours 2. Serum potassium level of 2.6 mEq/L 3. Blood pressure of 120/64 to 130/72 mm Hg 4. Sodium level of 142 mhq/L 41. A client receives a sealed radiation implant to treat cervical cancer. When caring for this client, the nurse should: 1. consider the client’s urine, feces, and vomitus to be highly radioactive. 2. consider the client to be radioactive for 10 days after implant removal. 3. allow soiled linens to remain in the room until after the client is discharged. 4. maintain the client on complete bed rest 42. A client is undergoing a left modified radical mastectomy for breast cancer. Postoperatively, blood pressure should be obtained from the right arm, and the client’s left arm and hand should be elevated as much as possible to prevent which condition? 1. Lymphedema 2. Trousseau’s sign 3.I.V. infusion infiltration 4. Muscle atrophy 42. A client with stage II ovarian cancer undergoes a total abdominal hysterectomy and bilateral salpingo-oophorectomy with tumor resection, omentectomy, appendectomy, and lymphadenectomy. During the second postoperative day, which assessment finding requires immediate intervention? 1. Abdominal pain 2. Hypoactive bowel sounds 3. Serous drainage from the incision 4. Shallow breathing and increasing lethargy 43. A client who will have his last chemotherapy cycle in 11 days becomes neutropenic. The client understands his condition when he states: 1. “I’ll monitor my temperature frequently and go to the nearest emergency department if my temperaturerises above 100.4°F. 2. “I’ve found that eating fresh fruit and vegetables reduces the side effects of chemotherapy and also gives me more energy.” 3. “I find that going out for a quiet dinner and a movie relieves the stress and anxiety of my cancer treatment.” 4. “I love working in my garden; it gives me a lot of inner peace and tranquility.” 44. A nurse is administering daunorubicin (Daunoxome) through a peripheral I.V. line when the client complains of burning at the insertion site. The nurse notes no blood return from the catheter and redness at the IV. site. The client is most likely experiencing which complication? 1. Erythema 2. Flare 3. Extravasation 4. Thrombosis 45. For a client newly diagnosed with radiation-induced thrombocytopenia, the nurse should include which intervention in the care plan? 1. Administering aspirin if the temperature exceeds 102° F (38.8° C) 2. Inspecting the skin for petechiae once every shift 3.Providing for frequent rest periods 4. Placing the client in strict isolation 46. A client is scheduled to receive methotrexate (Trexall), 0.625 mg/kg P.O. daily, to treat malignant lymphoma. Before administering the drug, the nurse reviews the client’s medication history. Which drug might interact with methotrexate? 1. Digoxin (Lanoxin) 2. Theophylline (Slo-Phyllin) 3. Probenecid (Probalan) 4. Famotidine (Pepcid) 47. A client with a nagging cough makes an appointment to see the physician after reading that this symptom is one of the seven warning signs of cancer. What is another warning sign of cancer? 1. Persistent nausea 2. Rash 3.Indigestion 4. Chronic ache or pain 48. A client with laryngeal cancer has undergone laryngectomy and is now receiving radiation therapy to the head and neck. The nurse should monitor the client for which adverse effects of external radiation? Select all that apply. 1. Xerostomia 2. Stomatitis 3.Thrombocytopenia 4.Cystitis 5.Dysgeusia 6. Leukopenia 49. A client with carcinoma of the lung develops syndrome of inappropriate antidiuretic hormone (SIADH) as a complication of the cancer. The nurse anticipates that which of the following may be prescribed? Select all that apply. 1. Radiation 2. Chemotherapy 3.Increased fluid intake 4. Serum sodium levels 5. Decreased oral sodium intake 6. Medication that is antagonistic to antidiuretic hormone 50. A nurse is preparing a list of home care instructions regarding stoma and laryngectomy care to a client who had a laryngectomy. Which instructions would be included in the list? Select all that apply. 1. Avoid swimming and use care when showering. 2. Keep the humidity in the home low. 3. Avoid exposure to people with infections. 4. Restrict fluid intake. 5. Obtain a Medic-Alert bracelet. 6. Prevent debris from entering the stoma. Ortho 1. A client complains that he experiences pain and numbness in his fingers when he types on a computer keyboard. Which action will help the nurse assess for Phalen’s sign? 1. Having the client hold both hands above his head with his arms straight for 30 seconds 2. Having the client hold both wrists in acute flexion with the dorsal surfaces touching for 60 seconds 3.Tapping gently over the median nerve in the wrist 4. Having the client extend his wrists while the nurse provides resistance 2. A nurse is managing the care of a client with osteoarthritis. Appropriate treatment strategies for osteoarthritìs include: 1. administration of opioids for pain control. 2. administration of nonsteroidal anti-inflammatory drugs (NSAIDs) and initiation of an exercise program. 3. administration of monthly intra-articular injections of corticosteroids. 4. vigorous physical therapy for the joints. 3. A nurse is caring for a client with burns on his legs. Which nursing intervention will help to prevent contractures? 1. Applying knee splints 2.Elevating the foot of the bed 3. Hyperextending the client’s legs 4. Performing shoulder range-of-motion (ROM) exercises 4. A client is in the emergency department with a suspected fracture of the right hip. Which assessment findings should the nurse expect? Select all that apply. 1. The right leg is longer than the left leg. 2. The right leg is shorter than the left leg. 3. The right leg is abducted. 4. The right leg is adducted. 5. The right leg is externally rotated. 6. The right leg is internally rotated. 5. After a car accident, a client is admitted to an acute care facility with multiple traumatic injuries, including a fractured pelvis. For 24 to 48 hours after the accident, the nurse must monitor the client closely for which potential complication of a fractured pelvis? 1. Compartment syndrome 2. Fat embolism 3.Infection 4. Volkmann’s ischemic contracture [Show More]
Last updated: 2 years ago
Preview 1 out of 16 pages
Buy this document to get the full access instantly
Instant Download Access after purchase
Buy NowInstant download
We Accept:

Reviews( 0 )
$14.00
Can't find what you want? Try our AI powered Search
Document information
Connected school, study & course
About the document
Uploaded On
Jan 12, 2021
Number of pages
16
Written in
Additional information
This document has been written for:
Uploaded
Jan 12, 2021
Downloads
0
Views
55

 answers.png)
























